Abstract
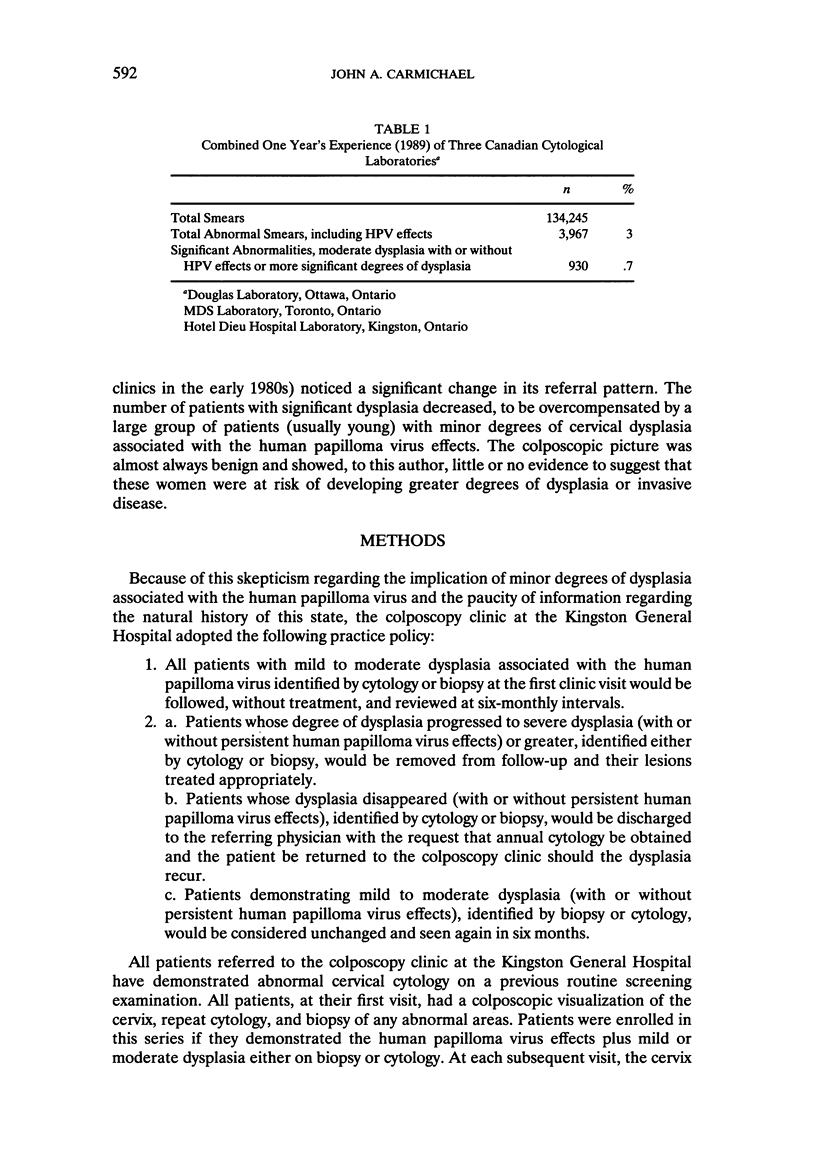
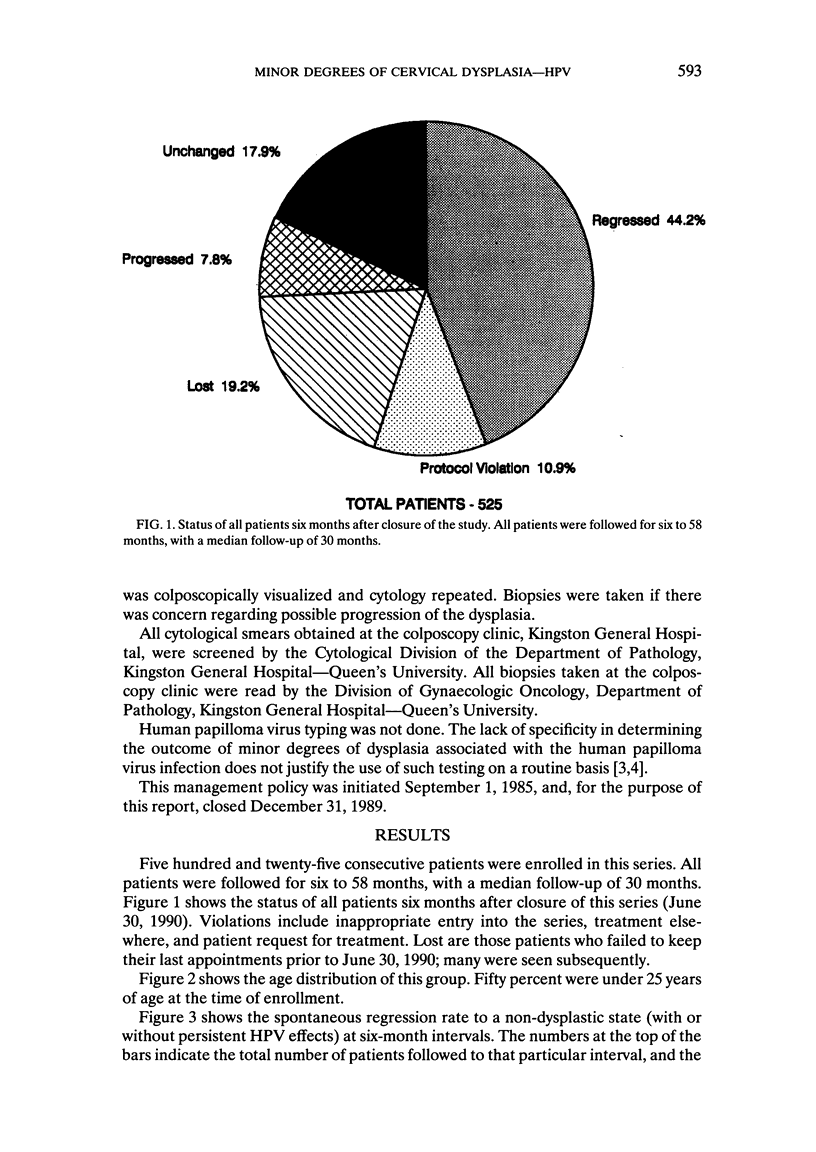
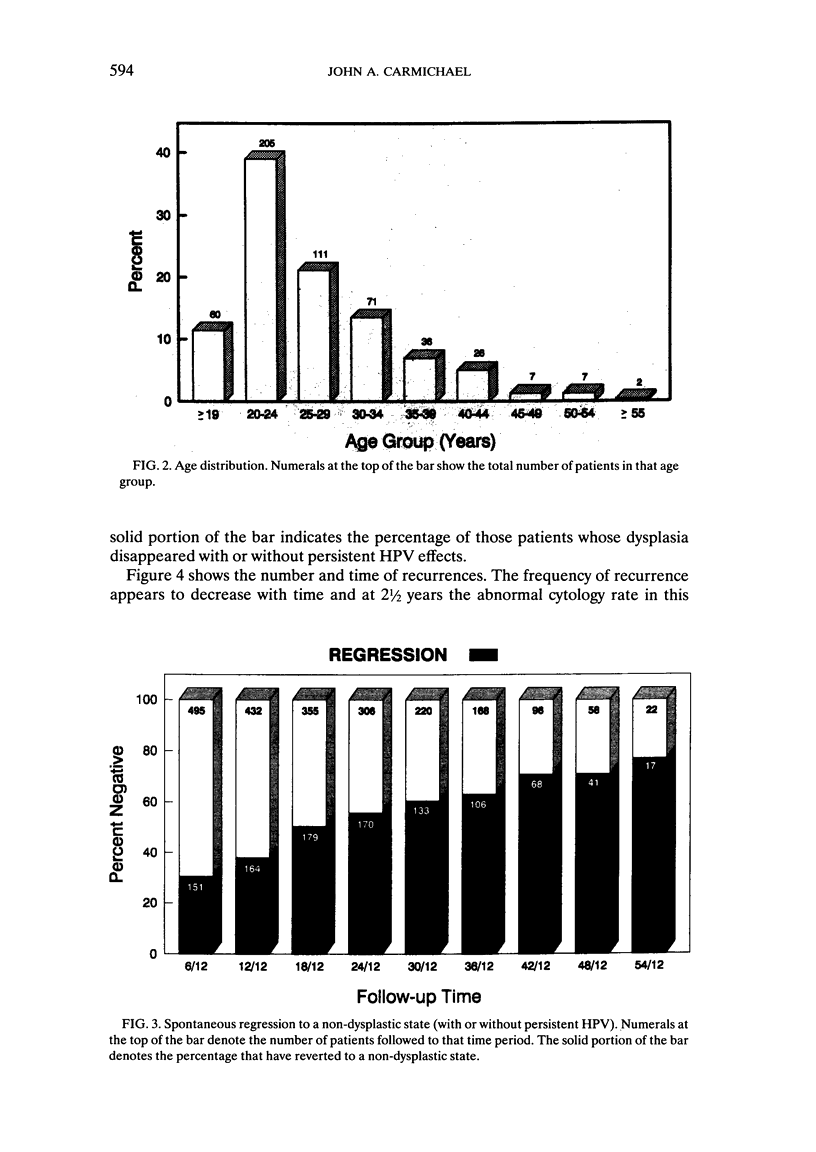
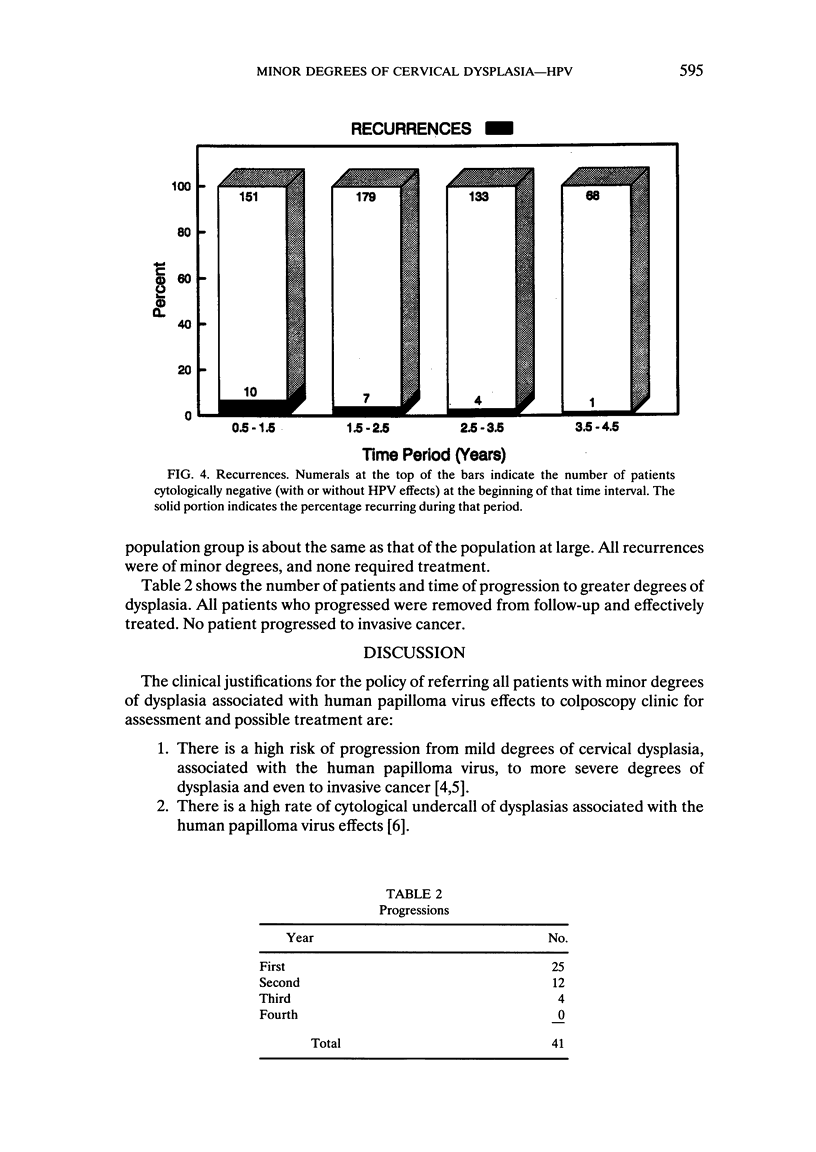
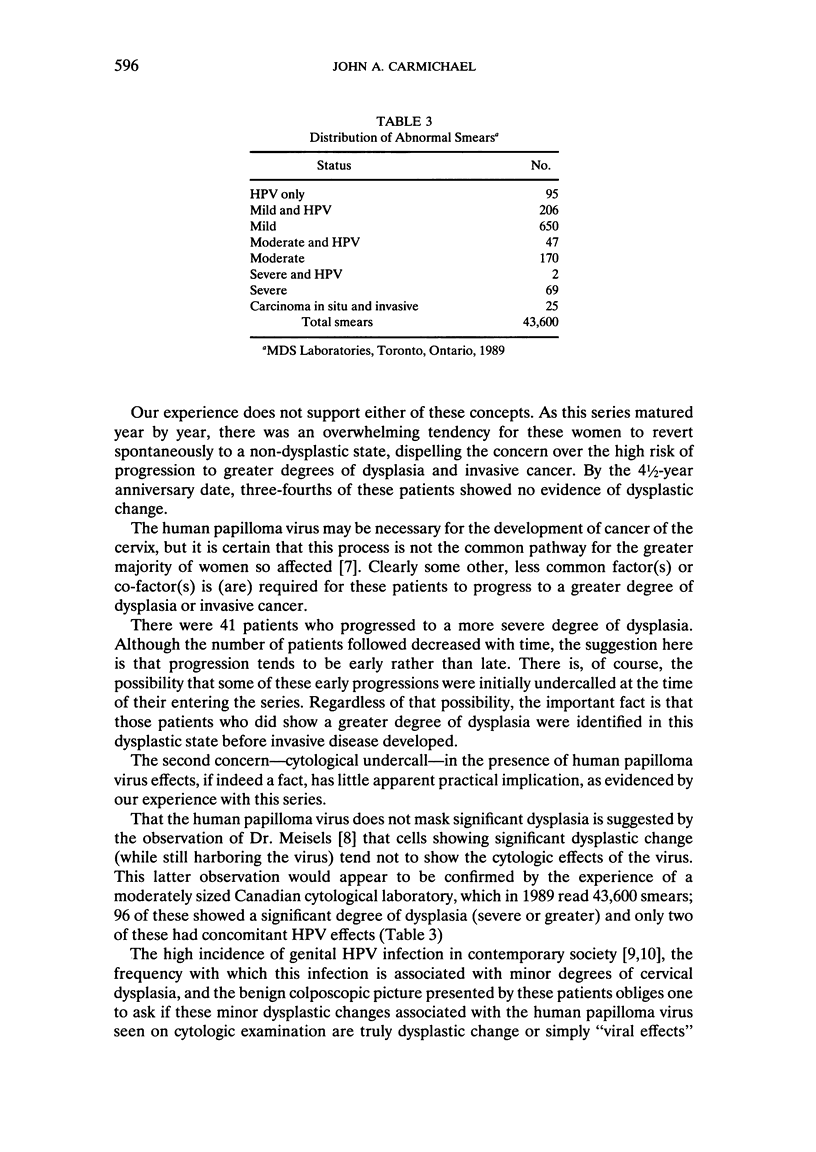
This report attempts to define further the natural history of minor degrees of cervical dysplasia associated with human papilloma virus (HPV). Five hundred and twenty-five patients with a diagnosis of mild to moderate cervical dysplasia and HPV effects were followed without treatment for six months to five years. Those patients who progressed to a greater degree of dysplasia were removed from follow-up and treated appropriately. Those patients who regressed to a non-dysplastic state were returned to the original referring physician to be followed with annual cytology. Regression to a non-dysplastic state was 30.5 percent at six months, 50.4 percent at 1 1/2 years, 60.5 percent at 2 1/2 years, 70.9 percent at 3 1/2 years, 77.3 percent at 4 1/2 years, 7.8 percent have progressed to a greater degree of cervical dysplasia, removed from follow-up, and treated, and 22 patients have recurred, all with minor degrees of dysplasia. No invasive cancer has been diagnosed in this group of patients. From these results, we conclude that patients with minor degrees of dysplasia associated with HPV can be followed in a routine screening program with the anticipation that the great majority will, over time, convert to a non-dysplastic state. A small number of patients will progress to a higher degree of dysplasia and will be effectively identified, to be referred for colposcopic assessment and appropriate treatment.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Koutsky L. A., Galloway D. A., Holmes K. K. Epidemiology of genital human papillomavirus infection. Epidemiol Rev. 1988;10:122–163. doi: 10.1093/oxfordjournals.epirev.a036020. [DOI] [PubMed] [Google Scholar]
- Meisels A., Fortin R. Condylomatous lesions of the cervix and vagina. I. Cytologic patterns. Acta Cytol. 1976 Nov-Dec;20(6):505–509. [PubMed] [Google Scholar]
- Melchers W., van den Brule A., Walboomers J., de Bruin M., Burger M., Herbrink P., Meijer C., Lindeman J., Quint W. Increased detection rate of human papillomavirus in cervical scrapes by the polymerase chain reaction as compared to modified FISH and southern-blot analysis. J Med Virol. 1989 Apr;27(4):329–335. doi: 10.1002/jmv.1890270413. [DOI] [PubMed] [Google Scholar]
- Mitchell H., Drake M., Medley G. Prospective evaluation of risk of cervical cancer after cytological evidence of human papilloma virus infection. Lancet. 1986 Mar 15;1(8481):573–575. doi: 10.1016/s0140-6736(86)92807-2. [DOI] [PubMed] [Google Scholar]
- Soutter W. P., Wisdom S., Brough A. K., Monaghan J. M. Should patients with mild atypia in a cervical smear be referred for colposcopy? Br J Obstet Gynaecol. 1986 Jan;93(1):70–74. doi: 10.1111/j.1471-0528.1986.tb07816.x. [DOI] [PubMed] [Google Scholar]
- Young L. S., Bevan I. S., Johnson M. A., Blomfield P. I., Bromidge T., Maitland N. J., Woodman C. B. The polymerase chain reaction: a new epidemiological tool for investigating cervical human papillomavirus infection. BMJ. 1989 Jan 7;298(6665):14–18. doi: 10.1136/bmj.298.6665.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Villiers E. M., Wagner D., Schneider A., Wesch H., Miklaw H., Wahrendorf J., Papendick U., zur Hausen H. Human papillomavirus infections in women with and without abnormal cervical cytology. Lancet. 1987 Sep 26;2(8561):703–706. doi: 10.1016/s0140-6736(87)91072-5. [DOI] [PubMed] [Google Scholar]


