Abstract
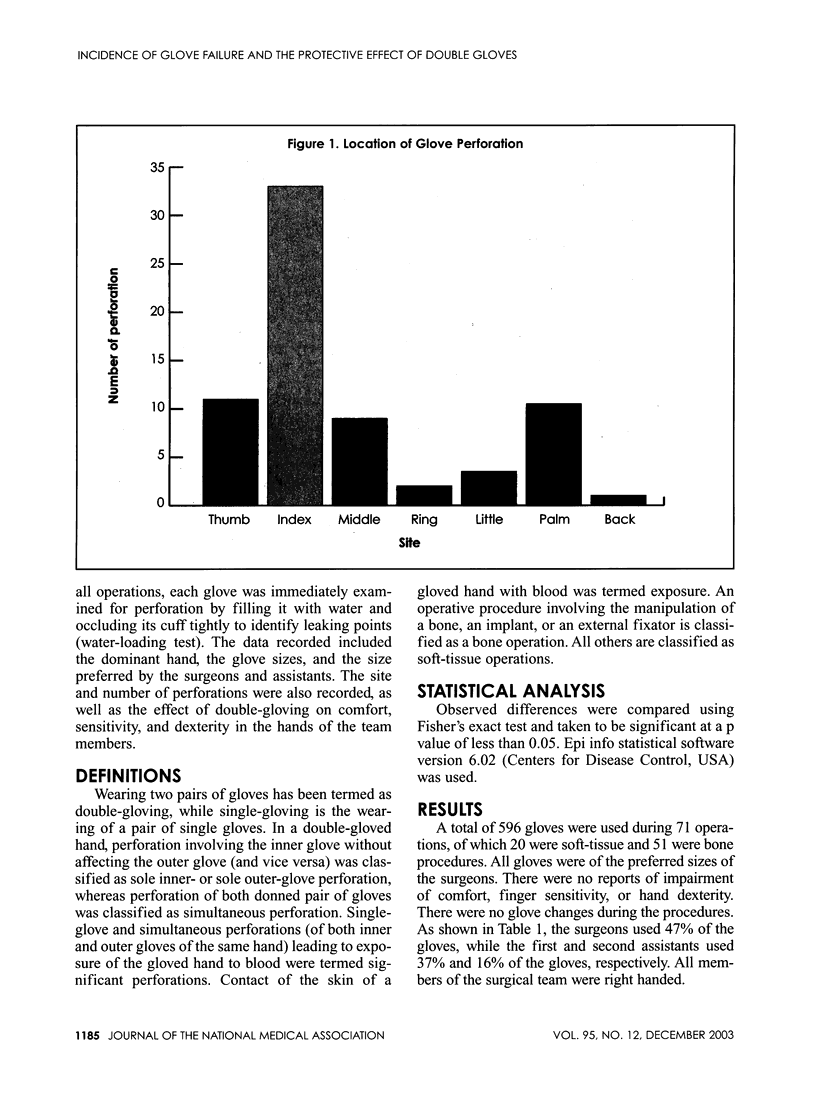
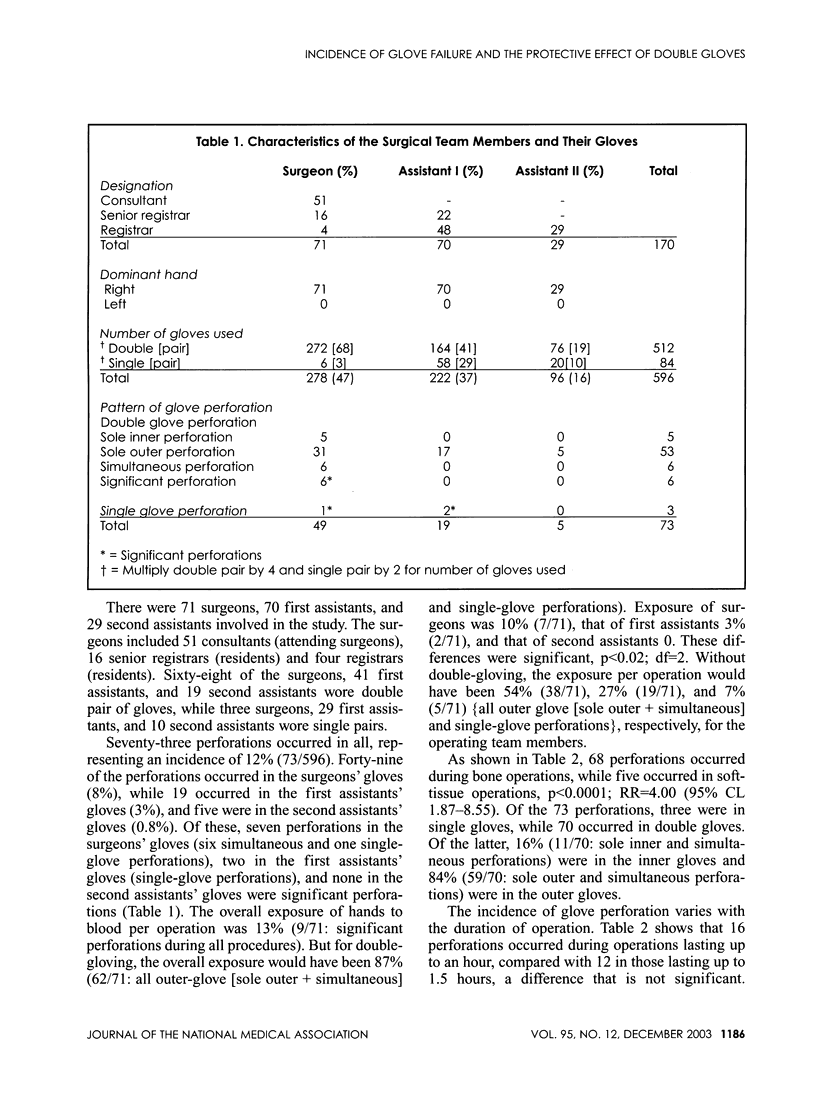
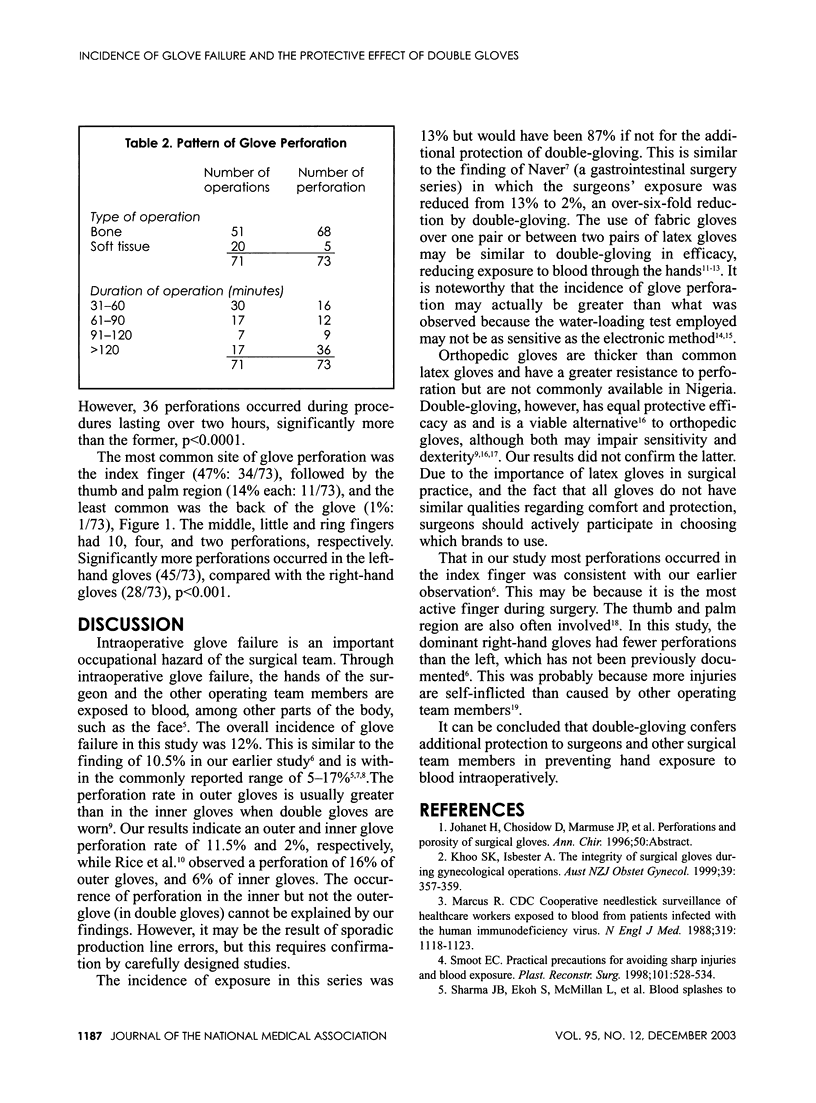
OBJECTIVE: To determine the usefulness of double gloves in protecting against the exposure of surgical team members' hands to blood. METHODOLOGY: Five-hundred-ninety-six gloves were studied during 71 orthopedic operations using the water-loading test (filling a glove with water and occluding its cuff tightly to identify leaking points). RESULTS: In all, 73 glove perforations occurred, but only nine resulted in exposure to blood (blood touching the skin). The incidence of glove perforation was 12% (73/596), and overall exposure (blood touching the skin) per operation was 13% (9/71). The latter would have been 87% (62/71) but for the use of double gloves. Sixteen percent of the perforations in double gloves were in the inner gloves, while 84% were in the outer gloves. Exposure of surgeons was reduced from 54% to 10%, first assistants from 27% to 3%, and second assistants from 7% to 0 (p < 0.02, df = 2) by double-gloving. Significantly more perforations occurred during operations on bone, compared with soft tissue operations, p < 0.0001, RR = 4 (95% CL 1.87-8.55). The most common sites of glove perforation were the index finger (47%), thumb, and the palm region: 14% each. More glove perforations occurred in nondominant hands. CONCLUSION: Double-gloving offers additional protection to surgeons and assistants by preventing hand exposure to blood intraoperatively.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Caillot J. L., Côte C., Abidi H., Fabry J. Electronic evaluation of the value of double gloving. Br J Surg. 1999 Nov;86(11):1387–1390. doi: 10.1046/j.1365-2168.1999.01266.x. [DOI] [PubMed] [Google Scholar]
- Doll G. M., Zentner A., Balan R., Sergl H. G. Efficacy of protection by latex gloves during orthodontic therapy. J Orofac Orthop. 2000;61(2):80–90. doi: 10.1007/BF01300350. [DOI] [PubMed] [Google Scholar]
- Herscovici D., Jr, DiPasquale T., Sanders R. Comparison of cloth gloves used in orthopaedic surgery: a clinical and experimental evaluation. J Orthop Trauma. 1998 Feb;12(2):106–110. doi: 10.1097/00005131-199802000-00007. [DOI] [PubMed] [Google Scholar]
- Jackson E. M., Neal J. G., Williams F. M., Stern C. A., Suber F., Thacker J. G., Edlich R. F. Biomechanical performance of orthopedic gloves. J Biomed Mater Res. 1999;48(2):193–198. doi: 10.1002/(sici)1097-4636(1999)48:2<193::aid-jbm14>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- Khoo S. K., Isbester A. The integrity of surgical gloves during gynaecological operations. Aust N Z J Obstet Gynaecol. 1999 Aug;39(3):357–359. doi: 10.1111/j.1479-828x.1999.tb03415.x. [DOI] [PubMed] [Google Scholar]
- Kovavisarach E., Vanitchanon P. Perforation in single- and double-gloving methods for cesarean section. Int J Gynaecol Obstet. 1999 Dec;67(3):157–161. doi: 10.1016/s0020-7292(99)00159-9. [DOI] [PubMed] [Google Scholar]
- Leslie L. F., Woods J. A., Thacker J. G., Morgan R. F., McGregor W., Edlich R. F. Needle puncture resistance of surgical gloves, finger guards, and glove liners. J Biomed Mater Res. 1996 Spring;33(1):41–46. doi: 10.1002/(SICI)1097-4636(199621)33:1<41::AID-JBM7>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- Louis S. S., Steinberg E. L., Gruen O. A., Bartlett C. S., Helfet D. L. Outer gloves in orthopaedic procedures: a polyester/stainless steel wire weave glove liner compared with latex. J Orthop Trauma. 1998 Feb;12(2):101–105. doi: 10.1097/00005131-199802000-00006. [DOI] [PubMed] [Google Scholar]
- Marcus R. Surveillance of health care workers exposed to blood from patients infected with the human immunodeficiency virus. N Engl J Med. 1988 Oct 27;319(17):1118–1123. doi: 10.1056/NEJM198810273191703. [DOI] [PubMed] [Google Scholar]
- Muralidhar A., Bishu R. R. Safety performance of gloves using the pressure tolerance of the hand. Ergonomics. 2000 May;43(5):561–572. doi: 10.1080/001401300184251. [DOI] [PubMed] [Google Scholar]
- Naver L. P., Gottrup F. Incidence of glove perforations in gastrointestinal surgery and the protective effect of double gloves: a prospective, randomised controlled study. Eur J Surg. 2000 Apr;166(4):293–295. doi: 10.1080/110241500750009113. [DOI] [PubMed] [Google Scholar]
- Rice J. J., McCabe J. P., McManus F. Needle stick injury. Reducing the risk. Int Orthop. 1996;20(3):132–133. doi: 10.1007/s002640050048. [DOI] [PubMed] [Google Scholar]
- Smoot E. C. Practical precautions for avoiding sharp injuries and blood exposure. Plast Reconstr Surg. 1998 Feb;101(2):528–534. doi: 10.1097/00006534-199802000-00045. [DOI] [PubMed] [Google Scholar]
- Sohn R. L., Murray M. T., Franko A., Hwang P. K., Dulchavsky S. A., Grimm M. J. Detection of surgical glove integrity. Am Surg. 2000 Mar;66(3):302–306. [PubMed] [Google Scholar]
- Wilson S. J., Sellu D., Uy A., Jaffer M. A. Subjective effects of double gloves on surgical performance. Ann R Coll Surg Engl. 1996 Jan;78(1):20–22. [PMC free article] [PubMed] [Google Scholar]


