Abstract
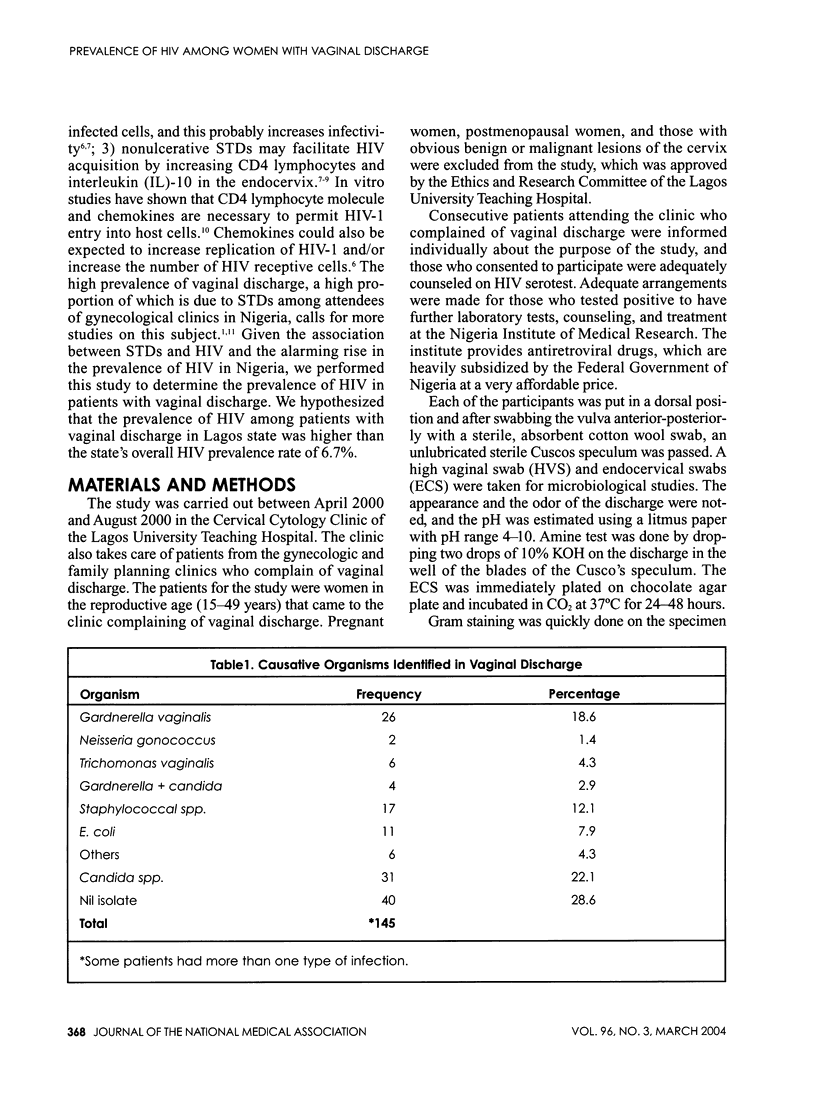
OBJECTIVE: Vaginal discharge is a common complaint among women with sexually transmitted diseases (STDs) in Nigeria. Given the association between STDs and HIV and the alarming rise in the prevalence of HIV in Nigeria, we performed this study to determine the prevalence of HIV in patients with vaginal discharge. STUDY DESIGN: Between April 2000 and August 2000, women who attended the Lagos University Teaching Hospital and complained of vaginal discharge were adequately counseled for HIV serotest. High vaginal/endocervical swabs and venous blood were taken for microbiological studies and HIV serotest, respectively. RESULTS: Out of the 230 women counseled for HIV serotest 140 (60.9%) consented. The mean age of the 140 was 31.1+/-6.9 years (range 18-50 years). In 31 (22.1%), Candida albicans was isolated, in 26 Gardnerella vaginalis (18.8%), in 17 Staphylococcal spp. (12.1%); and E. coli, Trichomonas vaginalis, and Neisseria gonococcus in 7.9%, 4.3%, and 1.4%, respectively. Four (2.9%) of the 140 patients were HIV seropositive, and all had Candida albicans isolated. The prevalence of HIV among patients with Candida albicans was 12.9%. Association between HIV seropositivity and Candida albicans infection is significant (X2=14.48; p=0.002). CONCLUSION: Candida albicans is a common cause of vaginal discharge among HIV-seropositive women in Lagos.
Full text
PDF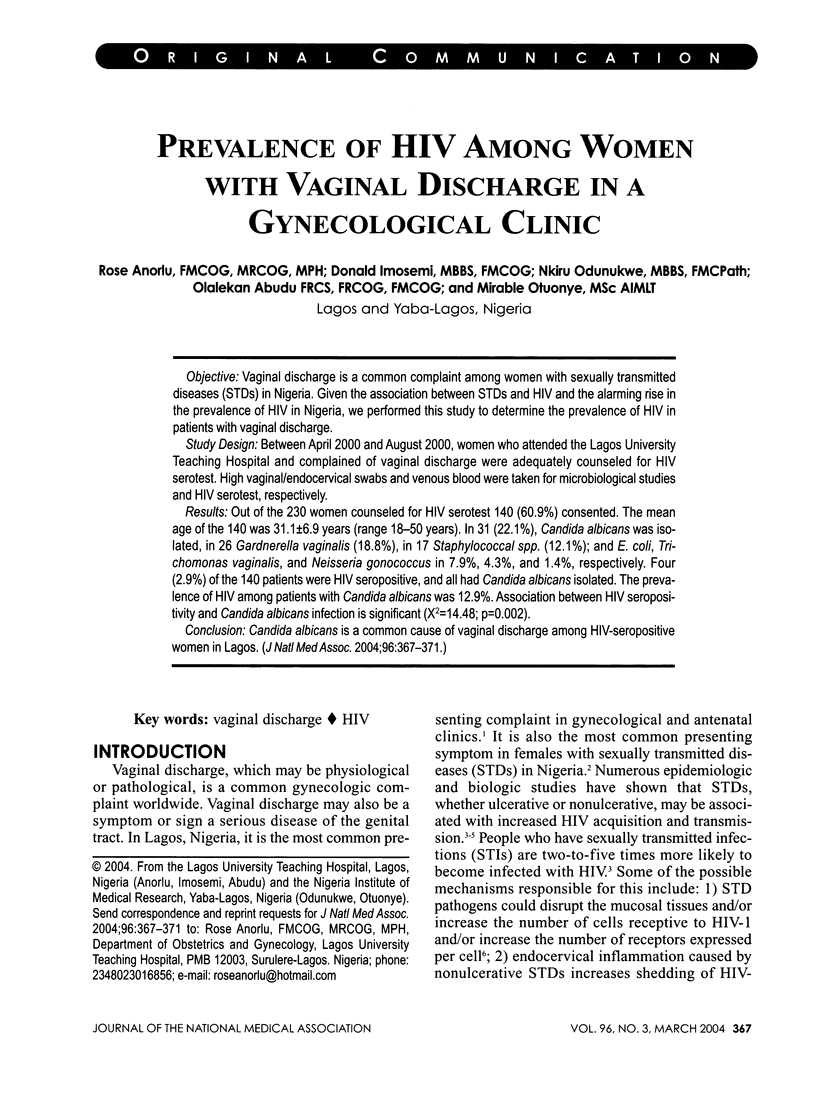

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Clemetson D. B., Moss G. B., Willerford D. M., Hensel M., Emonyi W., Holmes K. K., Plummer F., Ndinya-Achola J., Roberts P. L., Hillier S. Detection of HIV DNA in cervical and vaginal secretions. Prevalence and correlates among women in Nairobi, Kenya. JAMA. 1993 Jun 9;269(22):2860–2864. [PubMed] [Google Scholar]
- Cohen M. S. Sexually transmitted diseases enhance HIV transmission: no longer a hypothesis. Lancet. 1998;351 (Suppl 3):5–7. doi: 10.1016/s0140-6736(98)90002-2. [DOI] [PubMed] [Google Scholar]
- Cu-Uvin S., Hogan J. W., Warren D., Klein R. S., Peipert J., Schuman P., Holmberg S., Anderson J., Schoenbaum E., Vlahov D. Prevalence of lower genital tract infections among human immunodeficiency virus (HIV)-seropositive and high-risk HIV-seronegative women. HIV Epidemiology Research Study Group. Clin Infect Dis. 1999 Nov;29(5):1145–1150. doi: 10.1086/313434. [DOI] [PubMed] [Google Scholar]
- Dragic T., Litwin V., Allaway G. P., Martin S. R., Huang Y., Nagashima K. A., Cayanan C., Maddon P. J., Koup R. A., Moore J. P. HIV-1 entry into CD4+ cells is mediated by the chemokine receptor CC-CKR-5. Nature. 1996 Jun 20;381(6584):667–673. doi: 10.1038/381667a0. [DOI] [PubMed] [Google Scholar]
- Duerr A., Sierra M. F., Feldman J., Clarke L. M., Ehrlich I., DeHovitz J. Immune compromise and prevalence of Candida vulvovaginitis in human immunodeficiency virus-infected women. Obstet Gynecol. 1997 Aug;90(2):252–256. doi: 10.1016/S0029-7844(97)00253-6. [DOI] [PubMed] [Google Scholar]
- Fleming D. T., Wasserheit J. N. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect. 1999 Feb;75(1):3–17. doi: 10.1136/sti.75.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imam N., Carpenter C. C., Mayer K. H., Fisher A., Stein M., Danforth S. B. Hierarchical pattern of mucosal candida infections in HIV-seropositive women. Am J Med. 1990 Aug;89(2):142–146. doi: 10.1016/0002-9343(90)90291-k. [DOI] [PubMed] [Google Scholar]
- Levine W. C., Pope V., Bhoomkar A., Tambe P., Lewis J. S., Zaidi A. A., Farshy C. E., Mitchell S., Talkington D. F. Increase in endocervical CD4 lymphocytes among women with nonulcerative sexually transmitted diseases. J Infect Dis. 1998 Jan;177(1):167–174. doi: 10.1086/513820. [DOI] [PubMed] [Google Scholar]
- Minkoff H. L., Eisenberger-Matityahu D., Feldman J., Burk R., Clarke L. Prevalence and incidence of gynecologic disorders among women infected with human immunodeficiency virus. Am J Obstet Gynecol. 1999 Apr;180(4):824–836. doi: 10.1016/s0002-9378(99)70653-8. [DOI] [PubMed] [Google Scholar]
- Mostad S. B., Overbaugh J., DeVange D. M., Welch M. J., Chohan B., Mandaliya K., Nyange P., Martin H. L., Jr, Ndinya-Achola J., Bwayo J. J. Hormonal contraception, vitamin A deficiency, and other risk factors for shedding of HIV-1 infected cells from the cervix and vagina. Lancet. 1997 Sep 27;350(9082):922–927. doi: 10.1016/S0140-6736(97)04240-2. [DOI] [PubMed] [Google Scholar]
- Sewankambo N., Gray R. H., Wawer M. J., Paxton L., McNaim D., Wabwire-Mangen F., Serwadda D., Li C., Kiwanuka N., Hillier S. L. HIV-1 infection associated with abnormal vaginal flora morphology and bacterial vaginosis. Lancet. 1997 Aug 23;350(9077):546–550. doi: 10.1016/s0140-6736(97)01063-5. [DOI] [PubMed] [Google Scholar]
- Williams A. B., Andrews S., Tashima K., Mezger J., Yu C. Factors associated with vaginal yeast infections in HIV-positive women. J Assoc Nurses AIDS Care. 1998 Sep-Oct;9(5):47–52. doi: 10.1016/S1055-3290(98)80032-0. [DOI] [PubMed] [Google Scholar]


