Abstract
Diverse functions of eukaryotic cells are optimized by organization of compatible chemistries into distinct compartments defined by the structures of lipid-containing membranes, multiprotein complexes and oligomeric structures of saccharides and nucleic acids. This structural and chemical organization is coordinated, in part, through cysteine residues of proteins which undergo reversible oxidation-reduction and serve as chemical/structural transducing elements. The central thiol/disulfide redox couples, thioredoxin-1, thioredoxin-2, GSH/GSSG and cysteine/cystine (Cys/CySS), are not in equilibrium with each other and are maintained at distinct, non-equilibrium potentials in mitochondria, nuclei, the secretory pathway and the extracellular space. Mitochondria contain the most reducing compartment, have the highest rates of electron transfer and are highly sensitive to oxidation. Nuclei also have more reduced redox potentials but are relatively resistant to oxidation. The secretory pathway contains oxidative systems which introduce disulfides into proteins for export. The cytoplasm contains few metabolic oxidases and this maintains an environment for redox signaling dependent upon NADPH oxidases and NO synthases. Extracellular compartments are maintained at stable oxidizing potentials. Controlled changes in cytoplasmic GSH/GSSG redox potential are associated with functional state, varying with proliferation, differentiation and apoptosis. Variation in extracellular Cys/CySS redox potential is also associated with proliferation, cell adhesion and apoptosis. Thus, cellular redox biology is inseparable from redox compartmentalization. Further elucidation of the redox control networks within compartments will improve the mechanistic understanding of cell functions and their disruption in disease.
1. INTRODUCTION
The compartmentalization of peroxide-metabolizing systems within peroxisomes has long been recognized to provide a means to utilize hydrogen peroxide as a metabolic reagent while at the same time protect redox-sensitive cell components in other cell compartments from oxidative damage. Accumulating knowledge of redox characteristics in mitochondria, cytoplasm, nuclei and the secretory pathway indicate that unique redox characteristics have evolved with each of the major compartments in mammalian cells.
Elucidation of details has been advanced by improved sensitivity and spatial resolution of redox indicators in living cells but remains somewhat limited by difficulties in calibration and ability to confirm with fractionation due to auto-oxidation and redistribution artifacts. However, methods are progressively being improved so that an understanding of subcellular redox characteristics is emerging [1, 2]. In particular, development of redox western blot techniques for measuring redox states of proteins [3, 4] has allowed quantification of steady-state redox potentials of proteins in different subcellular compartments [2, 4, 5]. By creating constructs to target accumulation of proteins in specific compartments, systematic mapping of redox potentials in different compartments has become possible. Targeting has been achieved using mitochondrial localization sequences (MLS), nuclear localization signals (NLS), nuclear export signals (NES), and endoplasmic reticulum retention signals. The approaches have been complemented by techniques to measure redox potential in living cells, largely based upon partitioning of lipophilic cationic fluorescent chemicals into mitochondria dependent upon the high mitochondrial membrane potential (Δψ) [6] and development of redox-sensitive forms of green fluorescent protein [7]. Detection of disulfide reduction in the endosome has also been achieved by use of FRET [8]. Application of these methods to diverse systems has begun to clarify structural and chemical aspects of cellular functions which depend upon thiol/disulfide redox elements.
2. Mitochondrial redox regulation
Mitochondria are the most redox-active compartment of mammalian cells, accounting for more than 90% of electron transfer to O2 as the terminal electron acceptor. The predominant electron transfer occurs through a central redox circuit which uses the potential energy available from oxidation of various metabolic substrates (e.g., pyruvate, fatty acids) to generate ATP. The mitochondrial inner membrane contains 5 multiprotein complexes with central functions in oxidative phosphorylation. Three of these complexes are redox-driven proton pumps: complex I (NADH-quinone oxidoreductase), complex III (coenzyme Q: cytochrome reductase), and complex IV (cytochrome oxidase). Complex II (succinate dehydrogenase) transfers electrons into the chain from succinate, and complex V (ATP synthase), is a reversible proton pump which uses the electrochemical proton gradient (ΔμH +) to drive ATP synthesis.
Regulation of this process is central to cell function because cells must produce ATP while at the same time maintaining an appropriate homeostasis in terms of supply of non-essential amino acids, eliminating excess amino acids, supplying glucose and interconverting energy precursors to allow for long-term energy supply in the face of variable and intermittent food intake. Part of the regulation appears to occur through a continuous low rate of reactive oxygen species (ROS) generation, which regulates the magnitude of ΔμH + through control of Fe-S containing dehydrogenases and uncoupling proteins [9]. The molecular sensors and associated redox circuitry for this regulation remain poorly defined, but such regulation requires a specialized redox environment. In addition, the molecular machinery required for oxidative phosphorylation is highly dependent upon critical cysteine residues of proteins for enzymatic and transport activities [10], and the mitochondrial genome is susceptible to oxidative damage [11, 12]. These processes are directly relevant to mitochondrial oxidative stress-related diseases such as Parkinson’s disease [13], Friedreich’s ataxia [14], Huntington disease [15], and [16], and improved understanding can be expected to aid development of improved therapies for these diseases.
2.1 Oxidants in mitochondria
ROS, principally superoxide anion radical (O2 .−) and its dismutation product H2O2, are derived from several sources in mitochondria. Within the electron transport chain, Complex I and III are the main sites of electron transfer to O2 to produce O2 .− [17]. Inhibitors of complex I and III, rotenone and antimycin A, respectively, stimulate O2 .− generation at these sites [18, 19]. In addition to the electron transport chain, mitochondrial ROS may also be generated by pyruvate, α-ketoglutarate dehydrogenase, glycerol-3-phosphate dehydrogenase, and monoamine oxidase [20–23]. In apoptotic signaling, release of cytochrome c from mitochondria results in stimulated ROS generation [24]. Under excessive oxidative stress, simultaneous collapse of the mitochondrial membrane potential and a transient increase in ROS generation by the electron transfer chain can result in mitochondrial release of ROS to cytosol. This can trigger “ROS-induced ROS release” in neighboring mitochondria [25]. Thus, although a low rate of ROS generation is a normal process in mitochondria, disruption of electron flow with excessive ROS generation can activate cell death.
In addition to ROS, reactive nitrogen species (RNS) including nitric oxide (NO) and peroxynitrite (ONOO−), formed from reaction of NO with O2 .−, are present. The interaction of NO with mitochondria is also a potential mechanism for mitochondrial redox regulation. NO at physiological levels in cells does not appear to be directly toxic but can be converted to more reactive species [26]. Similar to ROS reactivity to protein thiols (-SH in cysteine residue), NO is also reactive to protein thiols and glutathione (GSH) to form nitrosothiols [27]. NO-modified proteins or other NO metabolites play a key role in regulating cellular redox signaling [27].
In support of a possible role for NO within mitochondria, mitochondrial nitric oxide synthase (mtNOS) has been identified and its function of NO generation in the mitochondria has been reported [28, 29]. In addition to stimulation of mitochondrial NO production by calcium-stimulated mtNOS activation, specific interaction of NO with cytochrome oxidase (complex IV) was shown to affect mitochondrial function [30]. Subsequent research demonstrated that mitochondrial function was affected by interactions of mitochondrial NO and its derivatives with glutathione (GSH) and with protein thiols [31].
NO reacts with O2 .− to produce peroxynitrite at a diffusion controlled rate. Peroxynitrite reacts with tyrosine residues in proteins to form nitrotyrosine residues [32, 33]. Similar to NO, ONOO− has a very short half-life, and its effect on cells is dependent on the concentration and proximity to the target molecule.
The mechanisms of ROS and RNS and their control by free radical scavengers have been extensively reviewed [34–37]. In the present review, we primarily discuss only the thiol/disulfide redox-regulated antioxidant systems. Mitochondria have two major thiol antioxidant systems dependent upon GSH and the small protein thioredoxin-2 (Trx2), and each has several associated proteins, e.g., glutaredoxin-2 (Grx2), glutathione peroxidases 1 and 4 (Gpx1, Gpx4), and thioredoxin reductase-2 (TrxR2) and peroxiredoxins 3 and 5 (Prx3, Prx5), respectively.
2.2. NADPH/NADP+ system as reducing power for Trx and GSH system
In contrast to the respiratory electron transport chain in the mitochondria which is dependent upon NADH/NAD+, both Trx and GSH systems are dependent on the reducing power of NADPH/NADP+. Most mitochondrial dehydrogenases are linked to NAD+ rather than NADP+, so the rate of electron flow through the NADH/NAD+ couple is significantly greater than that for the NADPH/NADP+ couple. Despite this, available evidence, which is principally only for rat liver, indicates that the steady-state redox potential of NADPH/NADP+ (−415 mV) is considerably more negative (reducing) than NADH/NAD+ (−300 mV) [38]. Mitochondrial NADPH functions in biosynthetic and detoxification reactions, including supply of reducing equivalents to the redox pathways containing GSH and thioredoxins [9]. Earlier studies showed mitochondrial reduction of NADP+ by the energy-linked transhydrogenase [39] as well as a limited number of dehydrogenases [40], but additional studies are needed to allow conclusions concerning the endogenous rates of these reactions in different cell types.
2.3. Mitochondrial GSH/GSSG redox state
Estimation of mitochondrial GSH/GSSG redox state is technically challenging due to loss and/or oxidation of GSH/GSSG during isolation of mitochondria. The GSH/GSSG pool has been estimated from GSH and GSSG concentrations following selective permeabilization of cells and also from isolated mitochondria incubated with respiratory substrates. Steady-state redox potential (electromotive force, Eh) is calculated using the Nernst equation and provides a measure of the tendency of a chemical species to accept or donate electrons. This tendency is quantitatively expressed in volts or millivolts relative to the standard hydrogen electrode reaction (H2/2H+ + 2e−). The Eh for an oxidation/reduction couple (e.g., GSH/GSSG) is dependent upon the inherent tendency of the chemical species to accept/donate electrons (Eo) and the concentration of the respective acceptors and donors, defined by the Nernst equation (e.g., for the GSH/GSSG couple, Eh = Eo + RT/NF ln([GSSG]/[GSH]2). The steady-state redox potential, also referred to as the "redox state", of mitochondrial GSH/GSSG, is about −280 mV [24, 41]. This value is more reduced than the cytoplasmic values (−260 mV to −200 mV) but not as reduced as measured in isolated mouse liver mitochondria (−330 mV to −300 mV, [42]). The latter redox potential values may be more negative due to an artificially high concentration of respiratory substrates, but both cellular and subcellular approaches indicate that mitochondrial GSH/GSSG redox state is more reduced than total cellular GSH/GSSG redox potential.
The GSH/GSSG redox potential in mitochondria is dependent upon concentrations of GSH and GSSG. Because mitochondrial GSH is not synthesized in mitochondria, it must rely on synthesis in the cytoplasm and subsequent transport into mitochondria [43, 44]. Therefore, GSH transport is a key determinant of GSH/GSSG redox state [45, 46]. Transport is stimulated by mitochondrial substrates, e.g., malate or pyruvate, and inhibited by excessive glutamate or disruption of the protonmotive force with proton ionophores. Two transporters, the dicarboxylate carrier and 2-oxoglutarate carrier, are major carriers for GSH transport [46]. These anion exchange systems use the energy available from the mitochondrial membrane potential to drive the uptake of the anion GSH against the prevailing membrane potential. Over-expression of these two carriers in eukaryotic cells caused increased mitochondrial GSH uptake and protected from oxidant-induced apoptosis [47, 48]. In addition to the presence of specific carriers, the mitochondrial inner membrane, the prevailing membrane potential, and the pH gradient from cytoplasm to mitochondrial matrix are important factors to determine mitochondrial GSH/GSSG redox [46].
Animal models for disease, including alcoholic liver disease (ALD) and Parkinson’s disease, provide evidence for the importance of GSH transport and GSH redox potential in the mitochondrial compartment [49, 50]. These studies show that the mitochondrial GSH/GSSG redox potential is affected by cellular pathological and toxicological conditions [49, 50]. For instance, the ALD study shows that the mitochondrial GSH/GSSG couple was decreased by up to 60% in ALD, and GSH transport was inhibited in rats with ALD [49]. A variety of studies using cell culture models also support the crucial role played by GSH in mitochondria as a protective effect in apoptotic cell death [51–53]. In apoptosis, oxidation of mitochondrial GSH/GSSG stimulated cytochrome c release [52], and GSH depletion resulted in increased ROS which was generated from complex III, suggesting a role for GSH in controlling mitochondrial ROS generation.
2.4. Mitochondrial GSH-dependent systems
Mitochondria contain several GSH-dependent enzymes including glutathione peroxidase-1 and 4 (Gpx1, Gpx4), glutathione reductase (GR) and glutaredoxin-2 (Grx2) [54, 55]. Studies involving Gpx1 knockout mice showed that susceptibility to mitochondrial oxidative stress was enhanced by Gpx1 depletion [56]. Cell lines derived from Gpx4 knockout mice (Gpx4+/−) showed an increased sensitivity to diquat-induced mitochondrial dysfunction and loss of the membrane potential [57], suggesting that both Gpx1 and Gpx4 in mitochondria have a protective role against oxidative stress.
While Grx1 is found in cytoplasm, Grx2 is principally localized in mitochondria and catalyzes the reversible oxidation and glutathionylation (Pr-SSG) of mitochondrial membrane proteins [58]. Molecular biological studies show that Grx2 has a central role in GSH-dependent redox regulation in mitochondria [59]. Over-expression of Grx2 in HeLa cells decreased susceptibility to 2-deoxy-D-glucose-induced apoptosis and prevented loss of cardiolipin, the phospholipids anchoring cytochrome c to the inner mitochondrial membrane [60]. Although evidence in now accumulating for Trx2, see below, most of the evidence to date indicates that GSH-dependent systems, including Gpx1, Gpx4, and Grx2, are essential for protection of mitochondria against oxidative stress.
2.5. Mitochondrial Trx2 redox state and Trx2-dependent system
Trx2 is a member of the Trx family of small redox proteins that contains a conserved thioredoxin active site of Trp-Cys-Gly-Pro-Cys-Lys [61]. Similar to the Trx1 system found in cytoplasm and nucleus, the Trx2 system includes Trx2, thioredoxin reductase-2 (TrxR2), and mitochondrial peroxiredoxin-3 (Prx3) and peroxiredoxin-5 (Prx5) [61–64]. The active site cysteines of Trx2 are maintained in the reduced form by electron transfer from NADPH, catalyzed by TrxR2. Overexpression of Trx2 in mammalian cells, i.e., osteosarcoma 143B cells and HEK-293 cells, protected against t-butylhydroperoxide and etoposide-induced apoptosis and mitochondrial membrane potential elevation [3, 65]. More recently, Trx2 overexpression in vascular endothelial cells showed that Trx2 plays an important role in vascular relaxation by NO [66]. Depletion of Trx2 in a chicken B cell line resulted in ROS increase, cytochrome c release, and apoptosis [67]. Heterozygous Trx2 deficient mice (Trx2+/−), did not have gross phenotype changes while Trx2−/− was embryonic lethal with massive apoptosis [68].
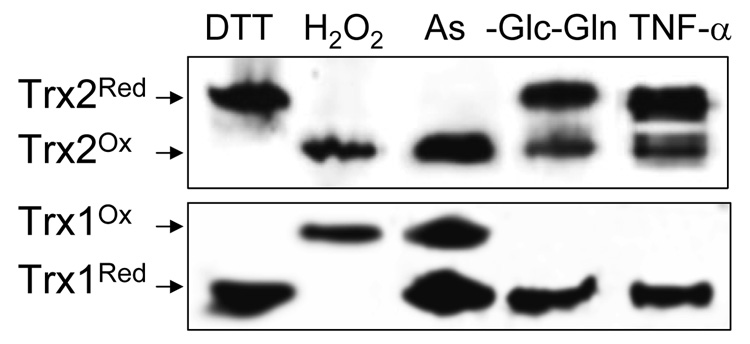
Because Trx2 is specific to the mitochondria, redox western blot analysis of Trx2 has been useful for the selective determination of mitochondrial redox potential by the redox Western blot method [5, 69]. Based on the redox potential value obtained using this technique, mitochondria are more reduced than other compartments in the cell [2], which is consistent with the data obtained using the redox sensitive green fluorescent protein [70]. The mitochondrial Trx2 has a much more reduced redox value (−330 mV at pH 7.6) than cytoplasmic and nuclear Trx1 (−280 mV to −300 mV at pH 7.0, [42]). The fraction of Trx2 present in the reduced form is variable in different cell types and under different metabolic conditions, with redox potential normally in the range of −360 mV to − 340 mV [42]. Increasing evidence that the redox state of mitochondrial Trx2 is distinct from Trx1 in cytoplasm and nucleus is listed in Table 1. The distinct differences of Trx2 and Trx1 in redox sensitivity are shown by different treatments, including metal ion (arsenic), restriction of glucose (Glc) and glutamine (Gln), and exposure to an inflammatory cytokine (TNF-α) (Fig 1) [69, 71, 72].
Table 1.
Evidence that mitochondrial Trx2 is regulated independently of Trx1
| Glc- and Gln-free medium selectively oxidizes cytoplasmic Trx1 and mitochondrial Trx2. | [71] |
| Chemical toxicants targeting mitochondrial electron transport show differential effects on Trx1 and Trx2 | [222] |
| Toxic metals oxidize Trx2 much greater than Trx1 | [72] |
| Trx2 but not Trx1 is oxidized by TNF-α. | [69] |
| tBH preferentially oxidizes Trx2 as compared to Trx1 | [223] |
Figure 1.
Mitochondrial Trx2 is more sensitive to oxidants than Trx1. Cells were exposed to arsenic (As), glucose and glutamine depletion (-Glc-Gln), or TNF-α. To provide reduced and oxidized controls, cells were treated with DTT (5 mM) and H2O2 (2 mM), respectively. Redox analyses of Trx2 and Trx1 were obtained by redox western blot methods [4, 5]. Briefly, the separation of Trx2 redox forms was obtained by difference in molecular weight due to alkylation of thiol in reduced Trx2 with AMS (4-acetoamido-4-maleimidylstilbene-2,2-disulphonic acid, 500 Da) under non-reduced condition of SDS-PAGE (Fig. 1, top). For Trx1 redox analysis, thiol alkylation of reduced Trx1 by IAA (iodoacetic acid) introduces extra negative charges, thereby giving rise to faster mobility in reduced form than oxidized form under native condition of PAGE (Fig.1, bottom). Using these methods, the results show that Trx2 with 100 µM As [72], Glc and Gln depletion [71], or TNF-α (20 ng/ml) [69] is significantly more oxidized than Trx1 (Fig. 1).
2.6. Thioredoxin reductase-2
Thioredoxin reductases (TrxR) are NADPH-dependent members of the nucleotide-disulfide oxidoreductase family which function to reduce thioredoxins. TrxR's are ubiquitously found in mammalian tissues, are homodimeric and contain a C-terminal selenocysteine necessary for catalytic activity. Three isoforms have been identified, the cytosolic TrxR1, mitochondrial TrxR2, and testis-specific Trx and GSSG reductase [73]. Cytosolic TrxR1 and mitochondrial TrxR2 function independently [74, 75], and elimination of either TrxR1 or TrxR2 gene results in an embryonic lethal phenotype [76, 77]. TrxR2−/− fibroblasts were much more sensitive to GSH deprivation induced-oxidative stress than TrxR2+/+ [76]. The phenotype of the mice after inactivation of TrxR2 was less severe than that in Trx2 knockout mice [78], which may suggest that other systems including TrxR1 or GSH-dependent redox systems substitute for the TrxR2 deficiency in mitochondria.
2.7. Mitochondrial peroxiredoxins
The mitochondria also contain peroxiredoxins (Prx), members of a super-family of selenium-free and heme-free peroxidases which function as Trx peroxidases to catalyze the reduction of H2O2, alkyl hydroperoxide, and peroxynitrite [79]. In mammals, six different peroxiredoxins (Prxs) have been identified. Prx3 is exclusively localized in mitochondria, and Prx5 has been found in mitochondria [80, 81] and other compartments, e.g., peroxisomes, cytosol and nucleus [82]. Banmeyer et al. [82] showed that Prx5 protected mitochondrial DNA from oxidative attack, suggesting an important role for Prx5 in mitochondrial genome stability. Prx3 decreased cell growth by regulating H2O2 level and protected cells from peroxide-induced apoptosis [68]. Similar to the results from the functional studies for Trx2 and TrxR2, the results from over-expression and depletion studies for mitochondrial Prxs suggest that Prx3 and Prx5 play an important role in mitochondrial redox regulation by functioning as antioxidants [66, 83].
3. Nuclear redox regulation
3.1. Nuclear protective functions of GSH and Trx1
ROS and RNS serve as messengers in cell signaling but also cause oxidative damage to macromolecules, including DNA damage. Sequestration of DNA within nuclei protects the genome from reactive chemicals generated in other parts of the cells; however, H2O2, organic hydroperoxides, and NO can diffuse across membranes, thus posing a potential damage from normal signaling events. Similar to other cellular organelles, nuclei also contain two major antioxidant systems dependent upon GSH and Trx1.
Studies to evaluate nuclear compartmentalization of GSH are contradictory due to artifacts resulting from perturbations during measurement [84–87]. However, an indirect estimation of nuclear GSH/GSSG, can be obtained by measuring nuclear S-glutathionylated protein (Pr-SSG), which is less subject to artifactual redistribution. Pr-SSG can be formed from reaction of GSSG with protein thiols (PrSH) and reaction of oxidized proteins with GSH. In principle, PrSSG could also be formed by GSH S-transferases or thiol peroxidases. Pr-SSG concentrations in nuclear and cytoplasmic compartments can be measured following reduction of nuclear and cytoplasmic proteins fractions with DTT, releasing GSH for HPLC measurement [88]. Results from this approach showed that cytoplasmic proteins have a higher content of S-glutathionylation than nuclear proteins. Stimulated nuclear production of H2O2 by targeting D-amino acid oxidase to nuclei resulted in increased protein glutathionylation in the nuclei but not in the cytosol [89]. In contrast, culture of cells in media devoid of Glc and Gln resulted in increased protein S-glutathionylation in the cytosol but not in nuclei [71]. Thus, the data show that protein S-glutathionylation is independently controlled in the cytoplasmic and nuclear compartments and indicate that the GSH/GSSG redox potential is likely to be more reduced in nuclei than in cytoplasm.
Compared to the GSH/GSSG redox measurement, measuring Trx1 redox in nuclei is less challenging. Trx-1 can translocate into the nucleus in response to a variety of stimuli including oxidants, UV irradiation, cytokines, lipopolysaccharide [90, 91], and Trx1 in nuclei has been shown in both cell culture and animal models [92, 93]. The reason for the increase in nuclear Trx1 in response to stress has not been established; however, it may be due to its antioxidant and repair functions against oxidant-induced damage. Alternatively, the increase in nuclear Trx1 concentration may provide a more reducing environment required for DNA binding by transcription factors (see below). Transport has recently been shown to be dependent upon importin-α [94], and retention could be maintained by binding to thioredoxin binding protein-2 (TBP-2), a nuclear protein also identified as Vitamin D3-binding protein-1 [95].
3.2. Nuclear Trx1 is functionally autonomous from cytoplasmic Trx1
A distinct nuclear pool of Trx1 is evident from immunohistochemical studies demonstrating that Trx1 is imported into the nucleus during oxidative stress [90, 94, 96, 97]. Although studies by Schroeder showed that lysine residues K81 and K82 of Trx1 play a key role in nuclear transport [94], the detailed mechanisms for nuclear localization of Trx1 remain to be identified. The existence of Trx1 in both compartments, cytoplasm and nucleus, provides the basis for its use in the study of nuclear and cytoplasmic redox states. Several lines of evidence now indicate that the redox state of Trx1 in the nucleus is distinct from that in the cytoplasm (see Table 2 and Fig. 2). Quantitative measurements show that reduced:oxidized ratios for Trx1 differ by 5- to 6-fold under basal conditions in different cell lines [2].
Table 2.
Evidence that nuclear Trx1 is regulated independently of cytoplasmic Trx1
| Trx1 accumulates in nuclei following oxidative stress and other stimuli | [90,119,224] |
| Steady-state redox is about 20 mV more reduced than cytoplasmic values | [4] |
| High-dose peroxide causes more extensive oxidation of nuclear than cytosolic Trx1 | [225] |
| The time course of recovery of nuclear Trx1 is slower than cytosolic Trx1 | [225] |
| EGF stimulates oxidation of cytosolic Trx1 but not nuclear Trx1 | [5] |
| Transfection with NLS-Trx1 stimulates transcriptional activation more than Trx1 | [133] |
| Glc- and Gln-free medium selectively oxidizes cytoplasmic Trx1 | [71] |
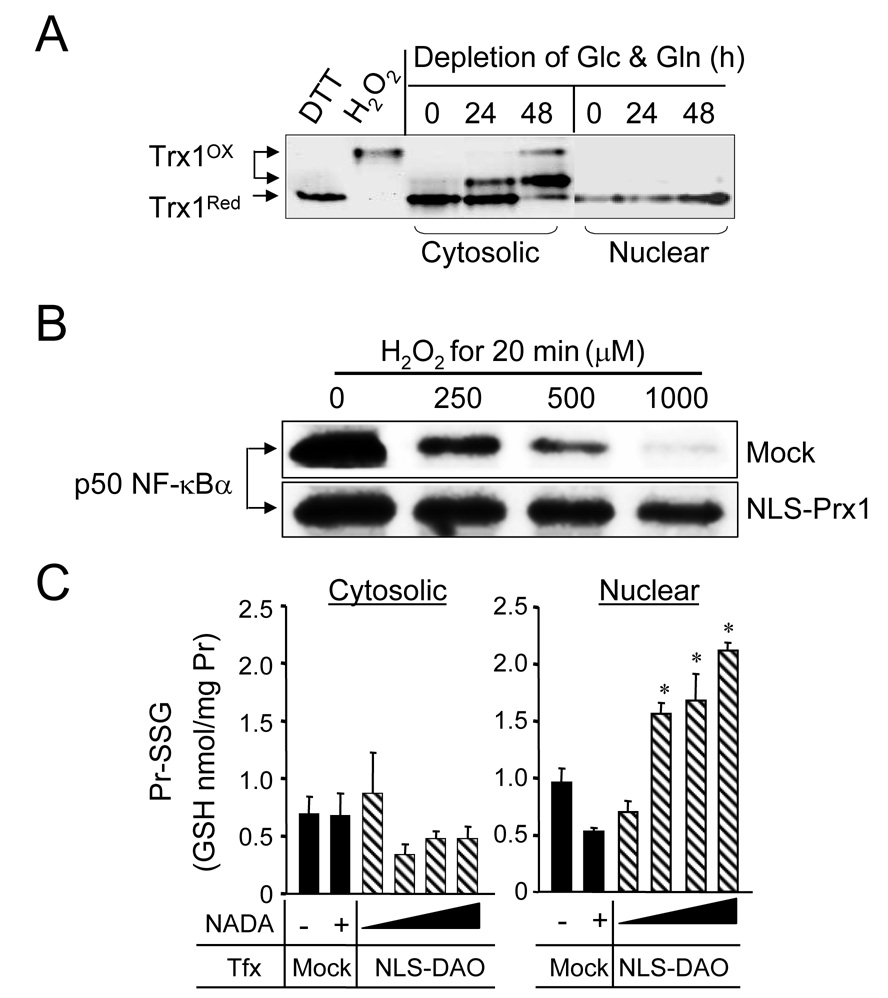
Figure 2.
Nuclear redox system is distinct from cytoplasm and is protected from oxidation. A. Redox state of Trx1 shows that oxidation of cytosolic but not nuclear Trx1 occurs in Glc- and Gln-free media [71]. B. Cells transfected with vector control or nuclear-targeted Prx1 (NLS-Prx1) for 24 h were exposed to H2O2 for 20 min with indicated amounts. BIAM (biotinylated iodoacetamide) labeling followed by immunoprecipitation for p50 NF-κB was used to determine reduced p50 NF-κB [124]. NLS-Prx1 expression inhibited oxidation of p50 compared with vector control (Mock). C. Cells were transfected with vector control (Mock) or nuclear targeted-D-amino acid oxidase (NLS-DAO) and treated with N-acetyl-D-alanine (NADA, 0 – 1 mM) to stimulate H2O2 production in the nuclei of cells [89]. NLS-DAO/NADA-induced ROS caused significant oxidation of the nuclear but not the cytosolic GSH pool, as measured by protein-S-glutathionylation (Pr-SSG).
3.3. Cysteine (Cys)-containing proteins and GSH in cell nuclei are critical for cell function
Cys-containing proteins control the genome, and include enzymes, transport machinery, structural proteins and transcription factors with conserved cysteine in zinc fingers and DNA-binding domains. Many of these nuclear systems depend upon the abundant, low molecular weight thiol antioxidant, GSH. GSH is important in the regulation of the nuclear matrix organization [98], maintenance of Cys residues on zinc-finger DNA binding motifs in a reduced and functional state [99]; chromosome consolidation [100]; DNA synthesis [101]; DNA protection from oxidative stress [102] and protection of DNA-binding proteins [103]. GSH supports GSH S-transferases (GST) in protection against oxidative DNA damage [104]. GSTpi in nuclei is increased in some cancers and is associated with anticancer drug resistance [105, 106]. Moreover, GSTpi forms a complex with peroxiredoxins [107] and catalyzes S-glutathionylation of Prx5 [108].
3.4. Redox-dependent activation of transcription factors by GSH and Trx1 systems
Regulation of transcription factor activity is among the most actively studied and important aspects of nuclear redox control. Several important transcription factors, including AP-1, NF-κB, Nrf2, p53 and glucocorticoid receptor [109–114] contain a critical Cys in the DNA binding region which is required for DNA binding. Accumulating evidence indicates that both GSH and Trx1 are important in regulation of transcription factor activity, apparently by different mechanisms.
3.4.1. Activating protein-1 (AP-1) activation
Early studies of activator protein-1 (AP-1) showed that oxidative stress signals phosphorylation of Jun to activate AP-1 [115–117]. In contrast, AP-1 binding to DNA is inhibited by high oxidant conditions due to a redox-sensitive thiol in the DNA binding region [109, 118]. Redox factor-1 (Ref-1) restores DNA binding using Trx1 as a reductant [119, 120]. Thus, AP-1 has two opposing redox-sensitive steps, 1) an upstream oxidative activation of the signaling kinase pathway and 2) a downstream Trx1-dependent reduction of the Cys of the DNA-binding domain. In addition, an indirect effect of Trx1 in cell nuclei can occur due to Trx1-dependent peroxide metabolism through peroxiredoxins (Prx1, Prx2, Prx5)[121].
3.4.2. Nuclear factor-κB (NF-κB) activation
Similar opposing responses in cytoplasm and nuclei also occur for NF-κB. NF-κB activation in the cytoplasm is initiated by I-κB kinase, which phosphorylates I-κB causing dissociation and release of NF-κB for translocation into the nucleus [122]. Many activators of NF-κB, such as TNF-α and phorbol esters, stimulate ROS production, and activation can be blocked by reducing agents [113, 123] showing that activation of NF-κB is regulated by redox-dependent mechanisms. Over-expression of Trx2 in mitochondria blocked TNF-α-dependent activation, indicating that mitochondrial ROS can function to activate in the cytoplasm [124]. However, excessive ROS production, as well as NO generation by SNP (sodium nitroprusside) and GSNO (S-nitrosoglutathione), modifies a critical Cys62 in the DNA binding region of NF-κB p50 and inhibits DNA binding [125–127]. Thus, as with AP-1, there is a dual effect of ROS and RNS on NF-κB activity. Transfection with Trx1, which is principally present in cytoplasm, inhibited NF-κB activation, but nuclear-targeted Trx1 enhanced DNA binding [90]. As with AP-1, this process is mediated by Ref-1 [128, 129]. Targeted expression of a nuclear export signal-containing Prx-1 in the cytoplasm resulted in inhibited NF-κB reporter activity while the corresponding construct with a nuclear localization signal stimulated activity [124]. This experiment indicated that Prx-1-dependent H2O2 metabolism in the nucleus is important in controlling the NF-κB reporter activity [124]. However, in contrast to this, direct stimulation of H2O2 production in nuclei by targeted increase in D-amino acid oxidase resulted in inhibition of a NF-κB reporter activity but occurred without Trx1 oxidation [89]. The latter inhibition of NF-κB reporter activity was associated with increased nuclear protein S-glutathionylation. Thus, even though Trx1 provides a primary redox regulation of NF-κB in nuclei, this system also appears to be controlled by the GSH system [89].
3.4.3. Nuclear factor (erythroid-derived 2)-like 2 (Nrf2) activation
Control of Nrf2 is similarly complex [130, 131], with kinase control mechanisms as well as redox control [132]. Similar to Fos, Jun and NF-κB, Nrf2 has a critical Cys508, which must be in the reduced form to bind to DNA [111]. Oxidation of Nrf2 blocks its ability to increase gene expression. As shown with AP-1 and NF-κB, Trx1 reduces Cys508 in a Nrf2-dependent reaction and restores gene expression [111]. Recent studies further support compartment-specific redox control of Nrf-2 signaling. Cytoplasmic activation of Nrf-2 was regulated by GSH and not by Trx1 [133]. However, nuclear expression of an ARE reporter was controlled by nuclear-targeted Trx1 and not by GSH [133]. Thus, the GSH and Trx1 systems have distinct functions in the two compartments in control of transcription by Nrf2.
4. Cytoplasmic redox regulation is different from that in nuclear compartment
Redox regulation, like phosphorylation, is a covalent regulatory system that controls normal cellular functions of cells and organisms. It controls how cells respond to stress involving oxidants and free radicals, which underlie many degenerative diseases, including heart disease, cancer, stroke, diabetes, Alzheimer's disease, and kidney disease. Growth factors, such as epidermal growth factor (EGF), bind to their receptors and stimulate tyrosine kinase activity, initiating a phosphorylation cascade that activates DNA replication and cell division as downstream effects [134]. An increase in ROS accompanies EGF binding to its receptor, which appears to be a critical component for proper signal transduction. Recent studies on EGF stimulation evaluated ROS production, phosphorylation of the receptor, and oxidation of redox couples in different subcellular compartments [5]. Under this system, nuclear Trx1, mitochondrial Trx2, and cellular GSH did not show any significant oxidation following EGF stimulation while cytoplasmic Trx1 was oxidized by nearly 20 mV [5]. Although the effects of specific cytoplasmic oxidation of Trx1 are not known, these findings demonstrated that physiologic stimulation at the plasma membrane can cause the oxidation of specific redox couples in the cytoplasm without affecting other subcellular compartments.
4.1. Trx1 and GSH/GSSG redox couples in cytoplasm are not in equilibrium
The redox state of cytoplasm has been measured using cytosolic Trx1 and GSH/GSSG. The total cellular GSH/GSSG couple largely represents the cytoplasmic GSH/GSSG pool. However, the total cellular GSH/GSSG redox potential is more reduced in cultured cells and tissues in vivo than values obtained for red blood cells, where there are no intracellular organelles. In red blood cells, the Eh value for GSH/GSSG was estimated to be −193 mV [135]. This value is more positive (oxidized) than estimates for cells with nuclei and mitochondria, which are typically lower than −200 mV, indicating that organelles with more negative value could introduce an error when using a cellular value to estimate the cytoplasm value. Alternatively, the content of disulfide forms in the secretory pathway could result in total cellular values being more oxidized than cytoplasmic values. The magnitude of the latter error was estimated to be about 10 mV for the Cys/CySS couple from digitonin fractionation studies [136].
The standard potential (Eo) of the active site dithiol/disulfide couple of Trx1 was estimated to be −230 mV [4]. Using this value and measuring the percentage reduction with a redox western blot [4], cellular Trx1 has a steady-state redox potential of −280 mV. The value was more negative (reduced) than the GSH/GSSG redox couple, and the couples were not in redox equilibrium (see Fig. 3) [5, 133, 137]. The Trx1 and GSH/GSSG couples were found to vary independently during growth transitions [137], redox signaling [5, 133], and metal-induced toxicity [69]. Additional results by Hansen et al. show that GSH and Trx1 systems have unique functions in Nrf2 activation in the cytoplasm supporting differential roles of Trx1 and GSH in activation of transcription factor in cytoplasm [133]. Thus, the data show that the major redox systems consisting of Trx1 and GSH are distinct both between and within compartments.
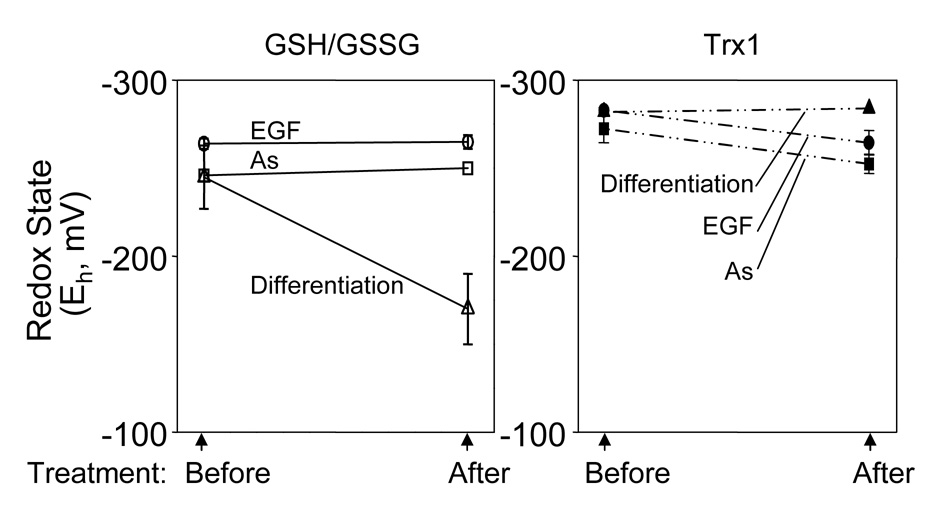
Figure 3.
Independent redox regulation of cellular (cytoplasmic) GSH/GSSG and cytoplasmic Trx1 by EGF, As, and differentiation. Redox states of cellular GSH/GSSG (left, open symbols with solid lines) and Trx1 (right, filled symbols with dashed lines) were measured in cells treated with EGF (circle, [5]) and arsenic (As) (rectangle, [72]), and in cells progressing from proliferation to differentiation (triangle, [137]). EGF treatment caused significant oxidation of cytoplasmic Trx1 redox state (20 mV) but had no effect in GSH/GSSG redox state. Similarly, arsenic oxidized Trx1 but not GSH/GSSG. GSH/GSSG but not Trx1 redox state was significantly oxidized during cellular differentiation.
5. Extracellular redox state
5.1. Cys/CySS couple is the major low molecular weight thiol/disulfide redox couple in most extracellular compartments
Cys and its disulfide, cystine (CySS) pool constitute the major low-molecular weight thiol/disulfide couple in mammalian plasma [138], and the Cys/CySS pool is one of the central redox control nodes in the biological signaling [136]. As described earlier [2, 9, 139, 140], the redox state of Cys/CySS in the extracellular compartment plays a major role in redox communication between cells and tissues. This function is in contrast to GSH in extracellular fluids, which appears to principally function in detoxification of reactive oxidants in the lung [141] and electrophiles in the small intestine [135].
Although we focus here on plasma Cys/CySS because cells in culture regulate the redox potential in the culture media to values similar to plasma Cys/CySS [142, 143], Eh data for plasma GSH/GSSG are also available and show that the redox potential of GSH/GSSG also correlates with health parameters [135, 144, 145]. Albumin also contains a redox-active Cys residue which is normally about 50% present as the S-cysteinyl disulfide form. This thiol has been suggested to function as a carrier of NO and also to function in detoxification [146, 147]. The content of this disulfide was also found to correlate with the plasma Cys/CySS redox potential [138]. Smaller amounts of S-GSH and S-cysteinylglycine disulfides were also present, but these did not correlate with plasma GSH/GSSG redox potential [138], consistent with earlier radiotracer studies which showed that S-cysteinylation is much more rapid than S-glutathionylation in plasma [88]. Trx1 is also present in plasma principally in the oxidized state [148].
The mean plasma GSH/GSSG redox value is approximately −140 mV in young healthy individuals [138]. This value is 90 mV more oxidized than the cytoplasmic pool; the difference is roughly equivalent in energetic terms to the membrane potential across the plasma membrane in an electrically excited tissue. The mean plasma Cys/CySS redox state is approximately −80 mV, about 60 mV more oxidized than cytoplasmic Cys/CySS redox. Particularly noteworthy, the plasma Cys/CySS redox is not in equilibrium with the plasma GSH/GSSG pool. A recent study of the diurnal variation of these pools showed that the Cys/CySS redox state becomes reduced after meals, with maximal values 2–3 h after eating [149]. GSH/GSSG also became more reduced, but this occurred 6–7 h after maximal changes in Cys/CySS [149]. Other studies show that the plasma redox potentials are oxidized in association with age [138, 150], but with different characteristics. GSH/GSSG is unchanged until about 45 years, then becomes oxidized at a rate of 0.7 mV/year; whereas, Cys/CySS becomes oxidized by about 0.2 mV/year over the entire age range from 18 to 93 years [138]. In addition to aging, plasma thiol/disulfide redox state is oxidized with oxidative stress involved circumstances such as chemotherapy [145], diabetes [135], cardiovascular disease [144], and smoking [151]. Alcohol abuse has recently been shown to result in oxidation of the redox potential in the lung lining fluid [141]. The lining fluid has a high GSH concentration and the GSH/GSSG redox state is similar to tissue redox values, i.e., −200 mV, perhaps reflecting the functional need to protect against oxidative toxicity and/or to avoid formation of protein disulfide. Fluidity of mucus is decreased by an oxidized redox state [152, 153], and crosslinking of proteins on the cell surface or in the lining fluid could also occur due to oxidation of the redox state. Thus, maintenance of a highly reduced redox state in the lining fluid would appear to be necessary to maintain deformability of the alveolar structures as well as signaling and other homeostatic functions. The plasma redox value correlates with plasma protein S-glutathionylation [154, 155], and age-associated oxidation of plasma redox couple can be prevented by antioxidant supplements [156].
5.2. The effects of changes in extracellular Cys/CySS redox on intracellular signaling
Recent advances have been made in understanding the mechanisms and functional consequences of redox changes in the extracellular compartment, as summarized in Table 3. These studies have addressed the potential consequences of variation in plasma Cys/CySS redox state by systematically varying this parameter in cell culture. In human gut epithelial (Caco-2) cells and normal human retinal pigment epithelial (hRPE) cells, cell proliferation was greater at more reduced Eh values (Fig. 4, [143, 157]). In studies to identify the mechanism of extracellular Cys/CySS redox state regulated cell growth in Caco-2 cells, alteration of the extracellular Cys/CySS redox state was sufficient to alter phosphorylation of p44/p42 MAPK through EGFR phosphorylation, with the greatest phosphorylation observed at the most reducing conditions (−150 mV) [158]. On the other hand, a lung fibroblast model relevant to pulmonary fibrosis showed that oxidized Eh values stimulate fibroblast proliferation and matrix expression through upregulation of transforming growth factor-β (Fig. 4, [159]). These results suggest that extracellular Cys/CySS redox-dependent cell proliferation is cell type specific and is mediated by intracellular kinase (e.g. p44/p42 MAPK) activation.
Table 3.
Thiol/disulfide redox controls in human plasma and extracellular compartment
| Association of oxidative stress- mediated pathologic circumstances with plasma thiol/disulfide redox state in human studies | |
|---|---|
| Decreased glutathione availability, oxidation of GSH/GSSG redox in the alcoholic lung | [141] |
| Antioxidant supplementation decreases CySS concentration in human plasma | [156] |
| Diurnal variation of Cys/CySS and GSH/GSSG redox states in human plasma: age-dependent diurnal variation in Cys/CySS redox state | [149] |
| Plasma Cys/CySS and GSH/GSSG redox state in early atherosclerosis | [144] |
| Age-dependent oxidation of GSH/GSSG and Cys/CySS pools in human plasma | [138] |
| Plasma antioxidant status after high-dose chemotherapy | [145] |
| Plasma GSH/GSSG redox state: association with aging, age-related macular degeneration, and diabetes | [135] |
| Effects of variation in extracellular Cys/CySS redox state on cell functions in in vitro studies | |
| GSH-independent control of extracellular Cys/CySS redox control in human colon cancer cells, HT-29 | [226] |
| Extracellular Cys/CySS redox controls lung fibroblast proliferation and matrix expression | [159] |
| Oxidized extracellular Cys/CySS redox promotes monocyte adhesion to vascular endothelial cells | [142] |
| Oxidation of extracellular Cys/CySS in human retinal pigment epithelial cells (hRPE) sensitizes oxidant-induced apoptosis | [143] |
| Extracellular Cys/CySS redox-dependent cell growth signaling in colon carcinoma cells is mediated by a metalloproteinase-dependent mechanism involving EGFR | [158] |
| Cell proliferation in human colonial epithelial cells (Caco2) and hRPE cells were greater at more reduced Eh values | [143,157] |
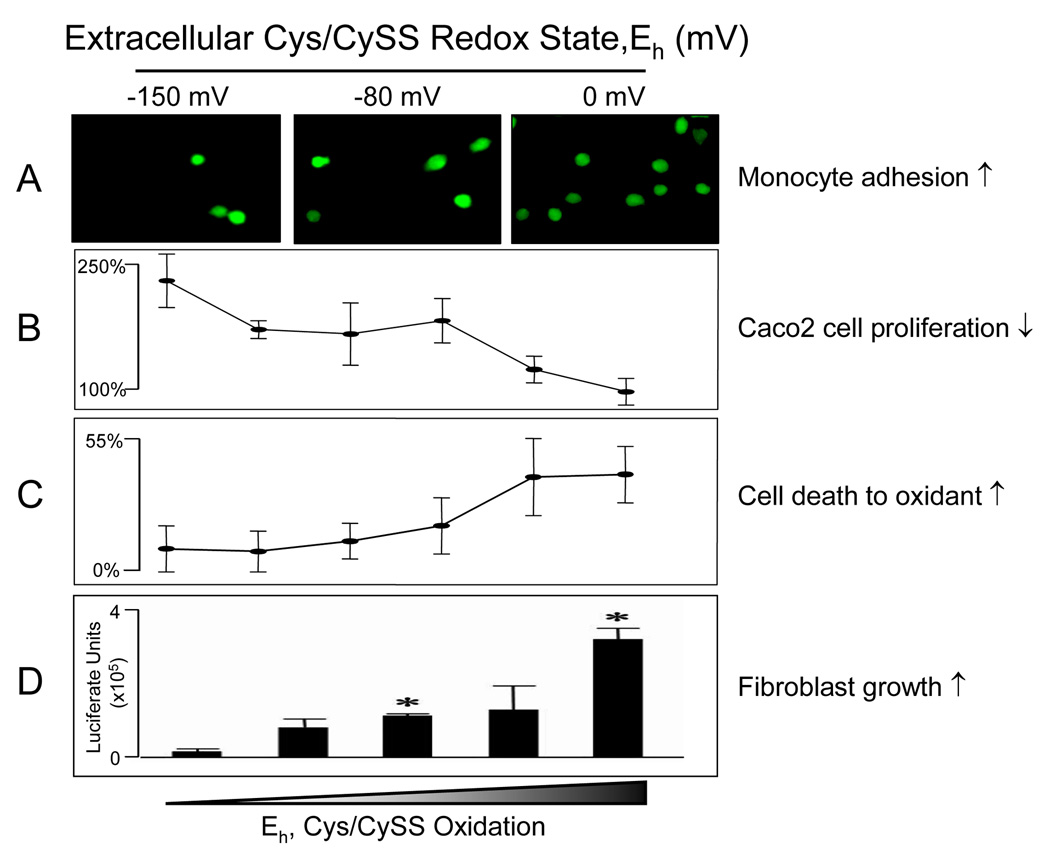
Figure 4.
Extracellular Cys/CySS redox-controlled changes in cellular mechanisms. Cells exposed to Cys/CySS redox-controlled media, varying from most reduced (−150 mV) to most oxidized (0 mV) stimulated monocyte adhesion to endothelial cells (A, [142]), reduced proliferation in colonial epithelial cells, Caco2 (B, [157]), increased cell death due to oxidants (C, [143]), and stimulated fibroblast growth (D, [159]).
The cell type specificity may reflect differences in cell responses to physiologic conditions, wherein fibroblasts respond to proliferate for tissue repair following immune cell-induced oxidative conditions, while reducing conditions are most stimulatory to other cells. Importantly, many studies show that there is growth stimulation both due to low levels of ROS and in association with increased cellular GSH and/or a more reduced extracellular thiol/disulfide redox state [157]. This apparent contradiction occurs because thiol/disulfide changes affect an upstream redox signaling step while the ROS affects a more downstream (intermediate) signaling step. Activation of these signaling molecules-dependent cell growth and proliferation mechanisms has been shown in a broad range of eukaryotic cells including cancer-derived and primary cells [158–161] and these mechanisms have been shown redox sensitive [162, 163].
Although there are relatively small numbers of studies available on extracellular Cys/CySS redox-dependent changes, the available data show that cell growth control is mediated by intracellular kinase activation [142, 158, 159]. The different responses among cell types, however, indicate that underlying mechanisms of signaling in response to extracellular Cys/CySS redox controlled cell growth and proliferation will require further elucidation.
While proliferation rate of hRPE cells were greater at reduced extracellular condition, these cells were more sensitive to oxidant-induced apoptosis than at more oxidized Eh values (Fig. 4, [143]). Additional studies to examine whether extracellular Cys/CySS redox state controls vascular biology using cultured vascular endothelial cells and human THP1 monocytes showed that ROS production was increased in cells exposed to a more oxidized Eh value ([142]). Also, increased numbers of adherent THP1 cells were observed when endothelial cells where exposed to culture medium containing oxidized Cys/CySS Eh (Fig. 4 [142]). Thus, the data show that the factors controlling the balance of plasma or extracellular Cys/CySS are important in determining cell functions, with general characteristics that a more reduced state stimulates cell proliferation while a more oxidized state sensitizes cells to oxidative stress and other stress responses.
5.3. Trx1 in extracellular compartments
Within the cytoplasm, nucleus, and mitochondria, Trx1 regulates redox signaling molecules and antioxidant functions as described in earlier sections of this review. In addition to translocation into the nucleus, Trx1 is secreted to the extracellular compartment where it can serve as a biomarker of disease and also can exert important protective functions [164–166]. Trx1 found in the extracellular compartment exists in two forms including intact Trx1 (12 kD) and a truncated form (10 kD). Intact Trx1 was found predominantly in an oxidized form [148, 167] and its truncated form (Trx-80, 10 kD) was found containing only N-terminal 1–80 (or 1–84) residues of Trx1. Truncated Trx1 can be released by cells [168] and functions with both cytokine-like and chemokine-like activities [169, 170]. Extracellular Trx1 prevents LPS- and chemokine-induced neutrophil chemotaxis in mice [165] and decreases reperfusion-induced arrhythmias [171] and adriamycin-induced cytotoxic injury [172]. Extracellular Trx1 suppresses autoimmune myocarditis via its antioxidative damage and anti-inflammatory functions [173] and prevents ischemic reperfusion injury [174]. Although the mechanism that mediates secretion of Trx1 to extracellular compartment and related effects need to be elucidated, Trx1 secretion occurs predominantly under conditions associated with oxidative stress, apoptosis, and inflammation [148, 167]. Consistently, plasma Trx1 concentrations were raised in patients with several cardiovascular risk factors [175] and with acute lung injury [176]. Hoshino et al. suggested that secreted Trx1 in extracellular compartment, plasma/serum Trx1, can be a useful biomarker for a wide variety of diseases.
6. Peroxisomes
Peroxisomes are ubiquitous organelles that perform biochemical functions of lipid metabolism and a number of oxidative reactions involving H2O2. The activities in mammalian peroxisomes include α-oxidation of specific fatty acids, catabolism of purines, polyamines, and prostaglandins, the biosynthesis of plasmalogens and sterols, and regulation of ROS and NO metabolism [177]. Peroxisomal enzymes generating ROS, primarily H2O2, found in eukaryotes were summarized in recent reviews [178, 179]. ROS generating enzymes include acyl-CoA oxidase, urate oxidase, xanthine oxidase, D-amino acid oxidase, pipecolic acid oxidase, D-aspartate oxidase, sarcosine oxidase, glycolate oxidase, hydroxyacid oxidase 2 and 3, and polyamine oxidase [178, 179]. NO production in peroxisomes has been shown and NO generation was regulated by inducible nitric oxide synthase detected in peroxisomes [180]. Therefore, it is clear that peroxisomes are another source of oxidants, ROS and NO, due to the presence of these enzymes besides mitochondria.
Earlier studies to evaluate H2O2 metabolism in rat hepatocytes showed that at low rates of generation by glycolate oxidase, most of the peroxide was metabolized by catalase within the peroxisomes [181]. However, at rates of generation >6 nmol/106 cells per min, H2O2 generation was sufficient to cause loss of cellular GSH, indicating that GSH-dependent metabolism was stimulated [181]. Peroxisomal H2O2 concentrations under these conditions were approximately 40 nM. In contrast, stimulation of H2O2 production in the endoplasmic reticulum resulted in substantial GSH loss with less peroxisomal H2O2. These data show that at low rates of production, peroxisomal and non-peroxisomal H2O2 metabolism are largely separated according to the respective sites of generation [181]. Steady-state infusion of H2O2 under anaerobic conditions allowed calibration of catalase and GSH peroxidase activities (without consideration of peroxiredoxin contribution) [182]. Results showed that non-catalase dependent metabolism represented a substantial fraction of the total elimination at low rates of infusion. However, at high rates, H2O2 was nearly stoichiometrically converted to O2 according to the catalatic reaction [182], indicating that the compartmentalization of H2O2 metabolism under physiologic conditions is due to rapid kinetics compared to diffusion.
Eukaryotic peroxisomes also contain antioxidants in addition to catalase, including glutathione peroxidase (Gpx), manganese superoxide dismutase (SOD2), copper/zinc superoxide dismutase (SOD1), epoxide hydrolase, peroxiredoxin-1 (Prx1), and Prx5 (also known as PMP20) [179]. However, as indicated above, catalase is the major peroxisomal enzyme responsible for the metabolism of H2O2. Inhibition and mislocation of catalase resulted in multiple peroxisomal enzymatic dysfunctions and deficiencies [183, 184]. Deficiency of peroxisomal catalase caused developmental abnormalities while its overexpression in transgenic mice resulted in extended life span suggesting that catalase in peroxisomes has an important role in cell survival and aging mechanisms [185].
While numerous studies have focused on catalase and its function, relatively little is known about other antioxidant enzymes, such as Gpx and Prxs, and their roles in mammalian peroxisomes, even though these enzymes are important in plant peroxisomes [186]. Since these enzymes are members of the GSH/GSSG and Trx systems, additional studies in mammalian peroxisomes are needed to evaluate their functions and also to estimate peroxisomal redox state.
7. Endoplasmic reticulum (ER)
While mitochondria can be generalized as a compartment utilizing oxidation for energy production and the peroxisomes as one utilizing H2O2 as an oxidative reagent, the ER is specialized with different oxidative functions in different cell types. In liver and steroidogenic cells, ER contains hemoproteins of the cytochrome P450 (Cyp) family which function to activate O2 to a reagent form used for steroid synthesis and oxidative detoxification of foreign compounds [187]. Many of these are highly inducible. The ER, as well as many other cell membranes, contains high amounts of cytochrome b5, a component of stearyl-CoA desaturase and a number of other oxidase enzymes [188]. Each of these hemoprotein systems is associated with flavoprotein reductases, and these systems can generate considerable amounts of O2 −. and H2O2 under some conditions. In muscle, redox reactions function in regulation of Ca2+ signaling through the ryanodine receptor [189].
In addition to these more specialized oxidative functions, the ER has a more general oxidative function to introduce structural disulfides in protein folding for membranal and exported proteins [190]. Central redox proteins for these functions include the endoplasmic reticulum oxidase-1 (Ero-1) and protein disulfide isomerases (PDI). Ero-1 proteins are flavoproteins which are oxidized by O2 and in turn oxidize dithiols in PDI to disulfides. Ero-1α is a constitutive form while Ero-1β is an inducible form produced under conditions of increased secretory demand or when processing results in excessive improperly folded protein, termed the unfolded protein response [191]. Ero-1p contains two catalytically inactive cysteines which serve as a built-in “off” mechanism, becoming oxidized and inactivating the enzyme under excessively oxidizing conditions [191]. Many PDI homologs function in the folding and processing pathways in the ER, and the appropriate function of these proteins requires a dynamic condition of partial reduction in the cyclic process of introduction of disulfides. Exposed reactive cysteines of processed proteins serve as retention signals within the ER [192] and a critical Cys29 of ERp44, a protein located more distally in the secretory pathway, functions in quality control for the proper folding [193].
In addition to the oxidative mechanisms [194], ER also contains a reductase system regulated by GSH transported by isolated microsomes [195]. GSH in the ER is used to reduce incorrect proteins disulfides. In the process, GSH content is depleted and this diminishes the capacity of the ER to counteract ROS [196]. Thus, ER contains both oxidative and reductive mechanisms which allow dynamic control of redox state in association with processing and secretory functions [197].
The GSH/GSSG ratio in the ER varies between 3/1 and 1/1 and is considerably more oxidized than cytoplasmic GSH/GSSG ratio (30/1 to 100/1). Based upon these values the ER redox potential has been estimated to be −189 mV, which is relatively oxidizing compared to other cellular compartments [198]. A significant amount of GSH in the ER was detected as protein mixed disulfides, which appears to regulate the activity of redox-active thiol-containing proteins and protect against hyperoxidizing conditions [196]. Interestingly, in an animal model for study of elastase regulation in lung function, the ER redox state in α1-antitrypsin transgenic mice was more reduced by expression of α1-antitrypsin, and this was accompanied with a higher GSH/GSSG ratio compared to the cytoplasm. The results indicated that changes in ER redox state to a more reduced environment resulted in a more protective role of ER against oxidative stress [199].
8. Lysosomes
Conditions for degradation of proteins to small peptides in lysosomes include an acidic pH and reduction of inter- and intrachain disulfide bonds. Due to the low pH, disulfide reduction in this compartment may not be favored by Trx or GSH redox systems that normally act in a neutral environment. There has been no enzyme found to catalyze reduction of the disulfide bond besides gamma- interferon (IFN-γ)- inducible lysosomal thiol reductase, GILT [200]. GILT, a unique lysosomal thiol reductase induced by IFN-γ, contains an active site with two cysteines like Trx family members and shows disulfide reduction activity at acidic pH. The redox potential of lysosomes has been measured in PC3 cells by expressing a redox-sensitive variant of GFP fused to various endocytic proteins (roGFP) [70]. The results showed that lysosomal redox potential was at least as oxidized as −240 mV, while mitochondrial redox potential was measured as −318 mV using roGFP, suggesting that lysosomes are relatively oxidized compared to other subcellular organelles [70]. In addition, deficiency in mechanisms to reduce disulfides in lysosomes was also shown by earlier studies in cystinosis, where a mutation results in loss of CySS transport and an accumulation of CySS within lysosomes [201, 202].
Non-thiol-dependent mechanisms also exist in the secretory pathway, and investigation of the interaction of these systems with thiol/disulfide systems is needed. Coenzyme Q, ubiquinone (UQ) is widely distributed in cell membranes and could play a role in antioxidant function and proton transport in other membranes including plasma membrane, golgi vesicles, and lysosomes [203, 204]. In lysosomes, a redox chain exists which carries electrons in the sequence of NADH > FAD > cytochrome b > UQ > oxygen, and regulates acidification of the lysosomal matrix. High levels of UQ exist in the reduced state in lysosomes and this contributes to distribute protons and to ROS generation [204, 205]. On the other hand, reduced UQ restores antioxidant function to oxidized tocopherol while no enzymes are available for reduction of oxidized tocopherol, directly suggesting that UQ has a dual function, antioxidant and oxidant, in lysosomal redox cycling systems.
9. Endocytic pathway
In opposition to secretory mechanisms, uptake and activation of toxins, such as diphtheria toxin, cholera toxin and Pseudomonas exotoxin, through the endocytic pathway involves reduction of disulfides [206–209]. Studies with a disulfide-containing radiolabeled polymer showed that the process in Chinese hamster ovary cells was partially blocked by thiol reagents and occurred over a several hour time course [210]. The process was inhibited by antibody to PDI, indicating that cell surface PDI was involved in the process, but the several hour time course indicated that intracellular reduction also occurred. The dynamics of this process have been studied with FRET using a folate-BODIPY disulfide with rhodamine which allowed real-time imaging of reduction in killer butterfly (KB) cells [8]. Results showed that reduction occurred with a half-life of 6 h, began in endosomes, did not depend significantly on extracellular surface thiols or redox machinery within lysosomes or Golgi, and yielded products which were sorted into different endosomal pathways. Thus, cells possess pathways to regulate the redox gradient of thiol/disulfide components in both release and uptake directions.
10. Summary and Perspectives
The available evidence shows that the concept of a simple redox balance within biologic systems is an inadequate description because each compartment of cells has different redox characteristics and, within each compartment, the major thiol/disulfide control systems are not in thermodynamic equilibrium. The redox characteristics of the compartments appear to have evolved in conjunction with the functions of the organelles, with mitochondria optimized for high-flux electron transfer reactions which are well insulated from other redox processes both within mitochondria and in other parts of the cell. Redox communication between the mitochondria and other compartments occurs via small reactive species, eg O2 −./H2O2, but the quantification and specificity of this communication mechanism requires further clarification. The nuclear compartment is relatively reducing and resistant to oxidative stress, perhaps reflecting a function of oxidative reactions as an off mechanism for central transcription factors. The secretory pathway and endocytic pathway have opposing redox systems which respectively oxidize and reduce thiol/disulfide couples in association with movement out or in. Because of the critical nature of folding, the secretory pathway contains quality control mechanisms dependent upon thiol/disulfide state. The very high rates of oxidation required for cells with high secretory function appear to require this compartmentalization to preserve a more reduced state in other regions of the cell. The cytoplasm is relatively devoid of enzymes which generate reactive oxygen species as part of normal metabolic function. This can serve two purposes. First, it can provide a buffer zone between mitochondria, ER and nuclei, so that each organelle is protected against aberrant ROS production by the others. Second, it can allow a very low background of ROS and RNS so that these can be used for sensitive and specific signaling dependent upon NADPH oxidases and NO synthases [211]. Finally, the extracellular compartments provide defensive barriers against external oxidants, a medium for communication between cells and appropriate conditions for receptor and transporter functions in the plasma membranes. Redox state measurements within the extracellular compartments are emerging as a useful biomarker of disease risk and provide a means to both monitor disease progress and response to interventions.
Detection methods with sufficient sensitivity, spatial resolution and chemical/biochemical specificity remain a major limit to progress in understanding redox compartmentalization. However, rapid advances with genetically engineered redox-sensitive GFP’s as well as fluorescent probes and new nanosensors appear likely to overcome these limitations. Much of what is known has been obtained with cell lines under a very limited range of conditions. One can expect that evolution of highly differentiated functions of organs and tissues will have resulted in associated variations which are critical to function of specific cell types. Thus, while the general features of subcellular redox compartmentalization have been elucidated, there remain many unanswered questions concerning the details in different biologic and pathologic conditions.
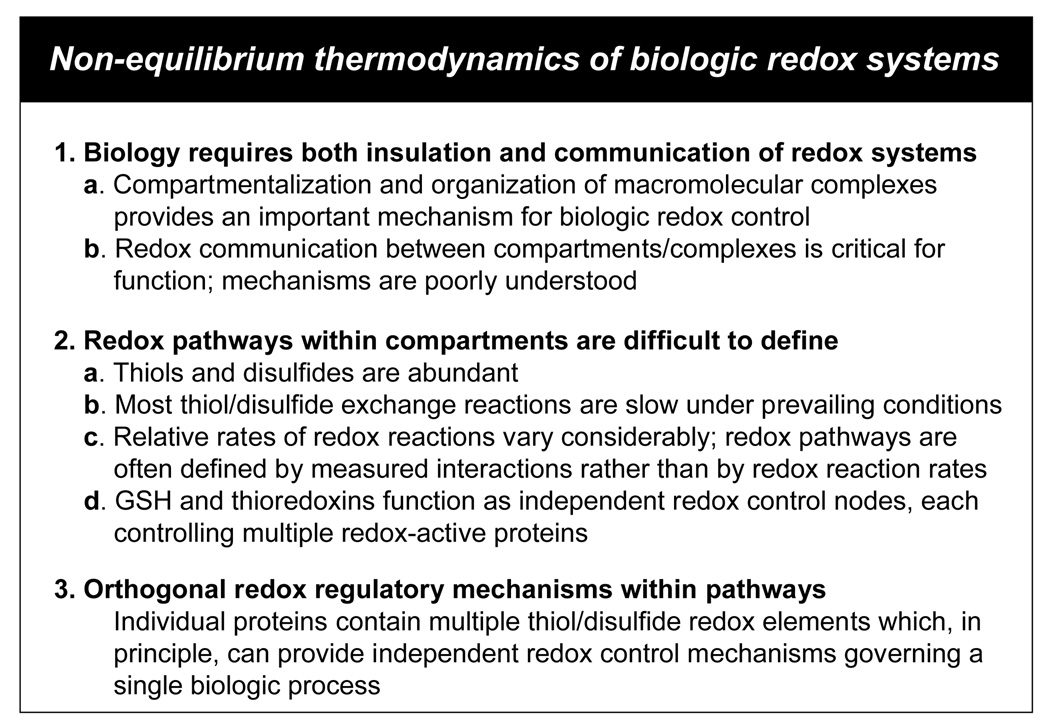
The thermodynamic disequilibrium of redox couples within and between compartments was recently considered from the perspective of redox systems biology [42]. A central principle is that electron transfer rates between thiol/disulfide systems are slow under prevailing conditions in cells. Key aspects for systems biological descriptions are summarized in Fig 5. Insulation of different redox components occurs by compartmentalization and also by organization of macromolecular complexes. Redox communication between compartments and complexes is poorly understood and represents an important subject for investigation. Within compartments and complexes, definition of pathways remains uncertain because of the differences in rates of thiol/disulfide reactions. In principle, this subject can be clarified by more specific consideration of proteins in terms of redox control by thioredoxin and GSH-dependent systems. Apoptosis signal-regulated kinase-1 (Ask-1), Nrf2 and NF-κB are controlled differently by Trx1 and GSH [89, 133, 212]. Additional studies are needed to understand these mechanisms, which appear to be orthogonal redox control mechanisms operating through different redox-sensitive elements.
Figure 5.
Non-equilibrium thermodynamics of biologic redox systems. A recent review of thiol/disulfide systems from the perspective of developing mathematical models for the dynamics of redox regulation identified three important areas for investigation [42]. The insulation of redox systems due to compartmentalization and macromolecular complexes identifies a need to understand redox communication between these compartments/complexes. Because there are many thiol/disulfide elements in proteins and their interaction rates are highly variable, effort is needed to develop a standardized means to define redox pathways. This problem may be addressed by functionally mapping protein cysteines according to their interactions with GSH and thioredoxin systems. Finally, there is a need to address the existence of orthogonal redox control elements. Many proteins and functional pathways have multiple redox-sensitive elements. Separate control by GSH and Trx allow different regulatory events to be controlled independently. Hence, different regulatory mechanisms can be considered to be orthogonal. Several examples are now known for such orthogonal regulation, but additional studies are needed to determine the generality of this type of regulation.
Finally, there is considerable need to integrate these concepts of thiol/disulfide compartmentalization into the broader context of the biologic consequences of redox signaling. Enhanced generation of oxidants is a common feature of cell proliferation, and the coordinated oxidant generation with changes in thiol/disulfide redox status may be an important aspect of the context-dependent regulation of cell function [213, 214]. This subject has been extensively studied and is relevant to neurotrophin signaling in neurons [215] and to oncogenic signaling by H Ras [216–218]. A similar connection occurs between oxidative stress in mitochondria and the stimulation of apoptosis or senescence [219, 220]. At the molecular level, these aspects are integrated by diffusible ROS species, which provide communication between compartments. For instance, mitochondria-derived H2O2 provides a transmembranal redox signal for cytoplasmic activation of c-Jun N-terminal kinase through Ask-1 [221]. A review on the specificity of ROS in signaling has recently become available [211] and provides many additional examples and details of these mechanisms. Additional investigation of the cell biology of the ROS and kinase signaling mechanisms within the developing knowledge of compartmentalization of thiol/disulfide redox systems provides an opportunity to improve understanding of these critical pathways in disease.
Acknowledgements
Research in the authors’ laboratory, upon which a portion of this review is based, was supported by NIH Grants ES009047 and ES011195.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Halvey PJ, Hansen JM, Lash LH, Jones DP. Compartmentation of Redox Signaling and Control: Discrimination of Oxidative Stress in Mitochondria, Cytoplasm. Nuclei and Endoplasmic Reticulum. 2007 In Press. [Google Scholar]
- 2.Hansen JM, Go YM, Jones DP. Nuclear and mitochondrial compartmentation of oxidative stress and redox signaling. Annual review of pharmacology and toxicology. 2006;46:215–234. doi: 10.1146/annurev.pharmtox.46.120604.141122. [DOI] [PubMed] [Google Scholar]
- 3.Damdimopoulos AE, Miranda-Vizuete A, Pelto-Huikko M, Gustafsson JA, Spyrou G. Human mitochondrial thioredoxin. Involvement in mitochondrial membrane potential and cell death. The Journal of biological chemistry. 2002;277:33249–33257. doi: 10.1074/jbc.M203036200. [DOI] [PubMed] [Google Scholar]
- 4.Watson WH, Pohl J, Montfort WR, Stuchlik O, Reed MS, Powis G, Jones DP. Redox potential of human thioredoxin 1 and identification of a second dithiol/disulfide motif. The Journal of biological chemistry. 2003;278:33408–33415. doi: 10.1074/jbc.M211107200. [DOI] [PubMed] [Google Scholar]
- 5.Halvey PJ, Watson WH, Hansen JM, Go YM, Samali A, Jones DP. Compartmental oxidation of thiol-disulphide redox couples during epidermal growth factor signalling. The Biochemical journal. 2005;386:215–219. doi: 10.1042/BJ20041829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murphy MP, Smith RA. Targeting antioxidants to mitochondria by conjugation to lipophilic cations. Annual review of pharmacology and toxicology. 2007;47:629–656. doi: 10.1146/annurev.pharmtox.47.120505.105110. [DOI] [PubMed] [Google Scholar]
- 7.Hanson GT, Aggeler R, Oglesbee D, Cannon M, Capaldi RA, Tsien RY, Remington SJ. Investigating mitochondrial redox potential with redox-sensitive green fluorescent protein indicators. The Journal of biological chemistry. 2004;279:13044–13053. doi: 10.1074/jbc.M312846200. [DOI] [PubMed] [Google Scholar]
- 8.Yang J, Chen H, Vlahov IR, Cheng JX, Low PS. Evaluation of disulfide reduction during receptor-mediated endocytosis by using FRET imaging. Proceedings of the National Academy of Sciences of the United States of America. 2006;103:13872–13877. doi: 10.1073/pnas.0601455103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones DP. Disruption of mitochondrial redox circuitry in oxidative stress. Chem Biol Interact. 2006;163:38–53. doi: 10.1016/j.cbi.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 10.Hurd TR, Prime TA, Harbour ME, Lilley KS, Murphy MP. Detection of reactive oxygen species-sensitive thiol proteins by redox difference gel electrophoresis: implications for mitochondrial redox signaling. The Journal of biological chemistry. 2007;282:22040–22051. doi: 10.1074/jbc.M703591200. [DOI] [PubMed] [Google Scholar]
- 11.Suliman HB, Carraway MS, Piantadosi CA. Postlipopolysaccharide oxidative damage of mitochondrial DNA. American journal of respiratory and critical care medicine. 2003;167:570–579. doi: 10.1164/rccm.200206-518OC. [DOI] [PubMed] [Google Scholar]
- 12.Wei YH, Lu CY, Lee HC, Pang CY, Ma YS. Oxidative damage and mutation to mitochondrial DNA and age-dependent decline of mitochondrial respiratory function. Annals of the New York Academy of Sciences. 1998;854:155–170. doi: 10.1111/j.1749-6632.1998.tb09899.x. [DOI] [PubMed] [Google Scholar]
- 13.Cohen G. Oxidative stress, mitochondrial respiration, and Parkinson's disease. Annals of the New York Academy of Sciences. 2000;899:112–120. doi: 10.1111/j.1749-6632.2000.tb06180.x. [DOI] [PubMed] [Google Scholar]
- 14.Lodi R, Tonon C, Calabrese V, Schapira AH. Friedreich's ataxia: from disease mechanisms to therapeutic interventions. Antioxidants & redox signaling. 2006;8:438–443. doi: 10.1089/ars.2006.8.438. [DOI] [PubMed] [Google Scholar]
- 15.McGill JK, Beal MF. PGC-1alpha, a new therapeutic target in Huntington's disease? Cell. 2006;127:465–468. doi: 10.1016/j.cell.2006.10.023. [DOI] [PubMed] [Google Scholar]
- 16.Donath MY, Ehses JA, Maedler K, Schumann DM, Ellingsgaard H, Eppler E, Reinecke M. Mechanisms of beta-cell death in type 2 diabetes. Diabetes. 2005;54 Suppl 2:S108–S113. doi: 10.2337/diabetes.54.suppl_2.s108. [DOI] [PubMed] [Google Scholar]
- 17.St-Pierre J, Buckingham JA, Roebuck SJ, Brand MD. Topology of superoxide production from different sites in the mitochondrial electron transport chain. The Journal of biological chemistry. 2002;277:44784–44790. doi: 10.1074/jbc.M207217200. [DOI] [PubMed] [Google Scholar]
- 18.Chen Q, Vazquez EJ, Moghaddas S, Hoppel CL, Lesnefsky EJ. Production of reactive oxygen species by mitochondria: central role of complex III. The Journal of biological chemistry. 2003;278:36027–36031. doi: 10.1074/jbc.M304854200. [DOI] [PubMed] [Google Scholar]
- 19.Kushnareva Y, Murphy AN, Andreyev A. Complex I-mediated reactive oxygen species generation: modulation by cytochrome c and NAD(P)+ oxidation-reduction state. The Biochemical journal. 2002;368:545–553. doi: 10.1042/BJ20021121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miwa S, St-Pierre J, Partridge L, Brand MD. Superoxide and hydrogen peroxide production by Drosophila mitochondria. Free radical biology & medicine. 2003;35:938–948. doi: 10.1016/s0891-5849(03)00464-7. [DOI] [PubMed] [Google Scholar]
- 21.Sandri G, Panfili E, Ernster L. Hydrogen peroxide production by monoamine oxidase in isolated rat-brain mitochondria: its effect on glutathione levels and Ca2+ efflux. Biochimica et biophysica acta. 1990;1035:300–305. doi: 10.1016/0304-4165(90)90092-b. [DOI] [PubMed] [Google Scholar]
- 22.Starkov AA, Fiskum G, Chinopoulos C, Lorenzo BJ, Browne SE, Patel MS, Beal MF. Mitochondrial alpha-ketoglutarate dehydrogenase complex generates reactive oxygen species. J Neurosci. 2004;24:7779–7788. doi: 10.1523/JNEUROSCI.1899-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tretter L, Adam-Vizi V. Generation of reactive oxygen species in the reaction catalyzed by alpha-ketoglutarate dehydrogenase. J Neurosci. 2004;24:7771–7778. doi: 10.1523/JNEUROSCI.1842-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cai J, Jones DP. Superoxide in apoptosis. Mitochondrial generation triggered by cytochrome c loss. The Journal of biological chemistry. 1998;273:11401–11404. doi: 10.1074/jbc.273.19.11401. [DOI] [PubMed] [Google Scholar]
- 25.Zorov DB, Juhaszova M, Sollott SJ. Mitochondrial ROS-induced ROS release: an update and review. Biochimica et biophysica acta. 2006;1757:509–517. doi: 10.1016/j.bbabio.2006.04.029. [DOI] [PubMed] [Google Scholar]
- 26.Levonen AL, Patel RP, Brookes P, Go YM, Jo H, Parthasarathy S, Anderson PG, Darley-Usmar VM. Mechanisms of cell signaling by nitric oxide and peroxynitrite: from mitochondria to MAP kinases. Antioxidants & redox signaling. 2001;3:215–229. doi: 10.1089/152308601300185188. [DOI] [PubMed] [Google Scholar]
- 27.Stamler JS, Hausladen A. Oxidative modifications in nitrosative stress. Nat Struct Biol. 1998;5:247–249. doi: 10.1038/nsb0498-247. [DOI] [PubMed] [Google Scholar]
- 28.Elfering SL, Sarkela TM, Giulivi C. Biochemistry of mitochondrial nitric-oxide synthase. The Journal of biological chemistry. 2002;277:38079–38086. doi: 10.1074/jbc.M205256200. [DOI] [PubMed] [Google Scholar]
- 29.Ghafourifar P, Schenk U, Klein SD, Richter C. Mitochondrial nitric-oxide synthase stimulation causes cytochrome c release from isolated mitochondria. Evidence for intramitochondrial peroxynitrite formation. The Journal of biological chemistry. 1999;274:31185–31188. doi: 10.1074/jbc.274.44.31185. [DOI] [PubMed] [Google Scholar]
- 30.Moncada S, Erusalimsky JD. Does nitric oxide modulate mitochondrial energy generation and apoptosis? Nature reviews. 2002;3:214–220. doi: 10.1038/nrm762. [DOI] [PubMed] [Google Scholar]
- 31.Costa NJ, Dahm CC, Hurrell F, Taylor ER, Murphy MP. Interactions of mitochondrial thiols with nitric oxide. Antioxidants & redox signaling. 2003;5:291–305. doi: 10.1089/152308603322110878. [DOI] [PubMed] [Google Scholar]
- 32.Beckman JS, Koppenol WH. Nitric oxide, superoxide, and peroxynitrite: the good, the bad, and ugly. Am J Physiol. 1996;271:C1424–C1437. doi: 10.1152/ajpcell.1996.271.5.C1424. [DOI] [PubMed] [Google Scholar]
- 33.Laskin JD, Heck DE, Gardner CR, Laskin DL. Prooxidant and antioxidant functions of nitric oxide in liver toxicity. Antioxidants & redox signaling. 2001;3:261–271. doi: 10.1089/152308601300185214. [DOI] [PubMed] [Google Scholar]
- 34.Abrescia P, Golino P. Free radicals and antioxidants in cardiovascular diseases. Expert review of cardiovascular therapy. 2005;3:159–171. doi: 10.1586/14779072.3.1.159. [DOI] [PubMed] [Google Scholar]
- 35.Kowluru RA. Diabetic retinopathy: mitochondrial dysfunction and retinal capillary cell death. Antioxidants & redox signaling. 2005;7:1581–1587. doi: 10.1089/ars.2005.7.1581. [DOI] [PubMed] [Google Scholar]
- 36.Le Prell CG, Hughes LF, Miller JM. Free radical scavengers vitamins A, C, and E plus magnesium reduce noise trauma. Free radical biology & medicine. 2007;42:1454–1463. doi: 10.1016/j.freeradbiomed.2007.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Valentine JS, Doucette PA, Zittin Potter S. Copper-zinc superoxide dismutase and amyotrophic lateral sclerosis. Annual review of biochemistry. 2005;74:563–593. doi: 10.1146/annurev.biochem.72.121801.161647. [DOI] [PubMed] [Google Scholar]
- 38.Sies H. Nicotinamide nucleotide compartmentation. London: A Subsidiary of Harcourt Brace Jovanovich; 1982. [Google Scholar]
- 39.Wanders RJ, van Doorn HE, Tager JM. The energy-linked transhydrogenase in rat liver in relation to the reductive carboxylation of 2-oxoglutarate. European journal of biochemistry / FEBS. 1981;116:609–614. doi: 10.1111/j.1432-1033.1981.tb05379.x. [DOI] [PubMed] [Google Scholar]
- 40.Hatefi Y, Galante YM. Dehydrogenase and transhydrogenase properties of the soluble NADH dehydrogenase of bovine heart mitochondria. Proceedings of the National Academy of Sciences of the United States of America. 1977;74:846–850. doi: 10.1073/pnas.74.3.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rebrin I, Sohal RS. Comparison of thiol redox state of mitochondria and homogenates of various tissues between two strains of mice with different longevities. Exp Gerontol. 2004;39:1513–1519. doi: 10.1016/j.exger.2004.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kemp M, Go YM, Jones DP. Nonequilibrium thermodynamics of thiol/disulfide redox systems: A perspective on redox systems biology. Free radical biology & medicine. 2007 doi: 10.1016/j.freeradbiomed.2007.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Griffith OW, Meister A. Origin and turnover of mitochondrial glutathione. Proceedings of the National Academy of Sciences of the United States of America. 1985;82:4668–4672. doi: 10.1073/pnas.82.14.4668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kurosawa K, Hayashi N, Sato N, Kamada T, Tagawa K. Transport of glutathione across the mitochondrial membranes. Biochem Biophys Res Commun. 1990;167:367–372. doi: 10.1016/0006-291x(90)91774-m. [DOI] [PubMed] [Google Scholar]
- 45.Chen Z, Putt DA, Lash LH. Enrichment and functional reconstitution of glutathione transport activity from rabbit kidney mitochondria: further evidence for the role of the dicarboxylate and 2-oxoglutarate carriers in mitochondrial glutathione transport. Archives of biochemistry and biophysics. 2000;373:193–202. doi: 10.1006/abbi.1999.1527. [DOI] [PubMed] [Google Scholar]
- 46.Lash LH. Mitochondrial glutathione transport: physiological, pathological and toxicological implications. Chem Biol Interact. 2006;163:54–67. doi: 10.1016/j.cbi.2006.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen Z, Lash LH. Evidence for mitochondrial uptake of glutathione by dicarboxylate and 2-oxoglutarate carriers. J Pharmacol Exp Ther. 1998;285:608–618. [PubMed] [Google Scholar]
- 48.Lash LH, Putt DA, Matherly LH. Protection of NRK-52E cells, a rat renal proximal tubular cell line, from chemical-induced apoptosis by overexpression of a mitochondrial glutathione transporter. J Pharmacol Exp Ther. 2002;303:476–486. doi: 10.1124/jpet.102.040220. [DOI] [PubMed] [Google Scholar]
- 49.Fernandez-Checa JC, Hirano T, Tsukamoto H, Kaplowitz N. Mitochondrial glutathione depletion in alcoholic liver disease. Alcohol. 1993;10:469–475. doi: 10.1016/0741-8329(93)90067-x. [DOI] [PubMed] [Google Scholar]
- 50.Przedborski S, Jackson-Lewis V. Mechanisms of MPTP toxicity. Mov Disord. 1998;13 Suppl 1:35–38. [PubMed] [Google Scholar]
- 51.Armstrong JS, Jones DP. Glutathione depletion enforces the mitochondrial permeability transition and causes cell death in Bcl-2 overexpressing HL60 cells. Faseb J. 2002;16:1263–1265. doi: 10.1096/fj.02-0097fje. [DOI] [PubMed] [Google Scholar]
- 52.Ghibelli L, Coppola S, Fanelli C, Rotilio G, Civitareale P, Scovassi AI, Ciriolo MR. Glutathione depletion causes cytochrome c release even in the absence of cell commitment to apoptosis. Faseb J. 1999;13:2031–2036. doi: 10.1096/fasebj.13.14.2031. [DOI] [PubMed] [Google Scholar]
- 53.Troyano A, Fernandez C, Sancho P, de Blas E, Aller P. Effect of glutathione depletion on antitumor drug toxicity (apoptosis and necrosis) in U-937 human promonocytic cells. The role of intracellular oxidation. The Journal of biological chemistry. 2001;276:47107–47115. doi: 10.1074/jbc.M104516200. [DOI] [PubMed] [Google Scholar]
- 54.Arai M, Imai H, Koumura T, Yoshida M, Emoto K, Umeda M, Chiba N, Nakagawa Y. Mitochondrial phospholipid hydroperoxide glutathione peroxidase plays a major role in preventing oxidative injury to cells. The Journal of biological chemistry. 1999;274:4924–4933. doi: 10.1074/jbc.274.8.4924. [DOI] [PubMed] [Google Scholar]
- 55.Lundberg M, Johansson C, Chandra J, Enoksson M, Jacobsson G, Ljung J, Johansson M, Holmgren A. Cloning and expression of a novel human glutaredoxin (Grx2) with mitochondrial and nuclear isoforms. The Journal of biological chemistry. 2001;276:26269–26275. doi: 10.1074/jbc.M011605200. [DOI] [PubMed] [Google Scholar]
- 56.Esposito LA, Kokoszka JE, Waymire KG, Cottrell B, MacGregor GR, Wallace DC. Mitochondrial oxidative stress in mice lacking the glutathione peroxidase-1 gene. Free radical biology & medicine. 2008;28:754–766. doi: 10.1016/s0891-5849(00)00161-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yant LJ, Ran Q, Rao L, Van Remmen H, Shibatani T, Belter JG, Motta L, Richardson A, Prolla TA. The selenoprotein GPX4 is essential for mouse development and protects from radiation and oxidative damage insults. Free radical biology & medicine. 2003;34:496–502. doi: 10.1016/s0891-5849(02)01360-6. [DOI] [PubMed] [Google Scholar]
- 58.Holmgren A. Antioxidant function of thioredoxin and glutaredoxin systems. Antioxidants & redox signaling. 2000;2:811–820. doi: 10.1089/ars.2000.2.4-811. [DOI] [PubMed] [Google Scholar]
- 59.Beer SM, Taylor ER, Brown SE, Dahm CC, Costa NJ, Runswick MJ, Murphy MP. Glutaredoxin 2 catalyzes the reversible oxidation and glutathionylation of mitochondrial membrane thiol proteins: implications for mitochondrial redox regulation and antioxidant DEFENSE. The Journal of biological chemistry. 2004;279:47939–47951. doi: 10.1074/jbc.M408011200. [DOI] [PubMed] [Google Scholar]
- 60.Enoksson M, Fernandes AP, Prast S, Lillig CH, Holmgren A, Orrenius S. Overexpression of glutaredoxin 2 attenuates apoptosis by preventing cytochrome c release. Biochem Biophys Res Commun. 2005;327:774–779. doi: 10.1016/j.bbrc.2004.12.067. [DOI] [PubMed] [Google Scholar]
- 61.Spyrou G, Enmark E, Miranda-Vizuete A, Gustafsson J. Cloning and expression of a novel mammalian thioredoxin. The Journal of biological chemistry. 1997;272:2936–2941. doi: 10.1074/jbc.272.5.2936. [DOI] [PubMed] [Google Scholar]
- 62.Chae HZ, Robison K, Poole LB, Church G, Storz G, Rhee SG. Cloning and sequencing of thiol-specific antioxidant from mammalian brain: alkyl hydroperoxide reductase and thiol-specific antioxidant define a large family of antioxidant enzymes. Proceedings of the National Academy of Sciences of the United States of America. 1994;91:7017–7021. doi: 10.1073/pnas.91.15.7017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chae HZ, Uhm TB, Rhee SG. Dimerization of thiol-specific antioxidant and the essential role of cysteine 47. Proceedings of the National Academy of Sciences of the United States of America. 1994;91:7022–7026. doi: 10.1073/pnas.91.15.7022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Miranda-Vizuete A, Damdimopoulos AE, Spyrou G. cDNA cloning, expression and chromosomal localization of the mouse mitochondrial thioredoxin reductase gene(1) Biochimica et biophysica acta. 1999;1447:113–118. doi: 10.1016/s0167-4781(99)00129-3. [DOI] [PubMed] [Google Scholar]
- 65.Chen Y, Cai J, Murphy TJ, Jones DP. Overexpressed human mitochondrial thioredoxin confers resistance to oxidant-induced apoptosis in human osteosarcoma cells. The Journal of biological chemistry. 2002;277:33242–33248. doi: 10.1074/jbc.M202026200. [DOI] [PubMed] [Google Scholar]
- 66.Zhang H, Luo Y, Zhang W, He Y, Dai S, Zhang R, Huang Y, Bernatchez P, Giordano FJ, Shadel G, Sessa WC, Min W. Endothelial-specific expression of mitochondrial thioredoxin improves endothelial cell function and reduces atherosclerotic lesions. Am J Pathol. 2007;170:1108–1120. doi: 10.2353/ajpath.2007.060960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tanaka T, Hosoi F, Yamaguchi-Iwai Y, Nakamura H, Masutani H, Ueda S, Nishiyama A, Takeda S, Wada H, Spyrou G, Yodoi J. Thioredoxin-2 (TRX-2) is an essential gene regulating mitochondria-dependent apoptosis. The EMBO journal. 2002;21:1695–1703. doi: 10.1093/emboj/21.7.1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Nonn L, Berggren M, Powis G. Increased expression of mitochondrial peroxiredoxin-3 (thioredoxin peroxidase-2) protects cancer cells against hypoxia and drug-induced hydrogen peroxide-dependent apoptosis. Mol Cancer Res. 2003;1:682–689. [PubMed] [Google Scholar]
- 69.Hansen JM, Zhang H, Jones DP. Mitochondrial thioredoxin-2 has a key role in determining tumor necrosis factor-alpha-induced reactive oxygen species generation, NF-kappaB activation, and apoptosis. Toxicol Sci. 2006;91:643–650. doi: 10.1093/toxsci/kfj175. [DOI] [PubMed] [Google Scholar]
- 70.Austin CD, Wen X, Gazzard L, Nelson C, Scheller RH, Scales SJ. Oxidizing potential of endosomes and lysosomes limits intracellular cleavage of disulfide-based antibody-drug conjugates. Proceedings of the National Academy of Sciences of the United States of America. 2005;102:17987–17992. doi: 10.1073/pnas.0509035102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Go YM, Ziegler TR, Johnson JM, Gu L, Hansen JM, Jones DP. Selective protection of nuclear thioredoxin-1 and glutathione redox systems against oxidation during glucose and glutamine deficiency in human colonic epithelial cells. Free radical biology & medicine. 2007;42:363–370. doi: 10.1016/j.freeradbiomed.2006.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hansen JM, Zhang H, Jones DP. Differential oxidation of thioredoxin-1, thioredoxin-2, and glutathione by metal ions. Free radical biology & medicine. 2006;40:138–145. doi: 10.1016/j.freeradbiomed.2005.09.023. [DOI] [PubMed] [Google Scholar]
- 73.Nakamura H. Thioredoxin and its related molecules: update 2005. Antioxidants & redox signaling. 2005;7:823–828. doi: 10.1089/ars.2005.7.823. [DOI] [PubMed] [Google Scholar]
- 74.Nalvarte I, Damdimopoulos AE, Nystom C, Nordman T, Miranda-Vizuete A, Olsson JM, Eriksson L, Bjornstedt M, Arner ES, Spyrou G. Overexpression of enzymatically active human cytosolic and mitochondrial thioredoxin reductase in HEK-293 cells. Effect on cell growth and differentiation. The Journal of biological chemistry. 2004;279:54510–54517. doi: 10.1074/jbc.M408494200. [DOI] [PubMed] [Google Scholar]
- 75.Patenaude A, Ven Murthy MR, Mirault ME. Mitochondrial thioredoxin system: effects of TrxR2 overexpression on redox balance, cell growth, and apoptosis. The Journal of biological chemistry. 2004;279:27302–27314. doi: 10.1074/jbc.M402496200. [DOI] [PubMed] [Google Scholar]
- 76.Conrad M, Jakupoglu C, Moreno SG, Lippl S, Banjac A, Schneider M, Beck H, Hatzopoulos AK, Just U, Sinowatz F, Schmahl W, Chien KR, Wurst W, Bornkamm GW, Brielmeier M. Essential role for mitochondrial thioredoxin reductase in hematopoiesis, heart development, and heart function. Molecular and cellular biology. 2004;24:9414–9423. doi: 10.1128/MCB.24.21.9414-9423.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jakupoglu C, Przemeck GK, Schneider M, Moreno SG, Mayr N, Hatzopoulos AK, de Angelis MH, Wurst W, Bornkamm GW, Brielmeier M, Conrad M. Cytoplasmic thioredoxin reductase is essential for embryogenesis but dispensable for cardiac development. Molecular and cellular biology. 2005;25:1980–1988. doi: 10.1128/MCB.25.5.1980-1988.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nonn L, Williams RR, Erickson RP, Powis G. The absence of mitochondrial thioredoxin 2 causes massive apoptosis, exencephaly, and early embryonic lethality in homozygous mice. Molecular and cellular biology. 2003;23:916–922. doi: 10.1128/MCB.23.3.916-922.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Dubuisson M, Vander Stricht D, Clippe A, Etienne F, Nauser T, Kissner R, Koppenol WH, Rees JF, Knoops B. Human peroxiredoxin 5 is a peroxynitrite reductase. FEBS letters. 2004;571:161–165. doi: 10.1016/j.febslet.2004.06.080. [DOI] [PubMed] [Google Scholar]
- 80.Knoops B, Clippe A, Bogard C, Arsalane K, Wattiez R, Hermans C, Duconseille E, Falmagne P, Bernard A. Cloning and characterization of AOEB166, a novel mammalian antioxidant enzyme of the peroxiredoxin family. The Journal of biological chemistry. 1999;274:30451–30458. doi: 10.1074/jbc.274.43.30451. [DOI] [PubMed] [Google Scholar]
- 81.Watabe S, Kohno H, Kouyama H, Hiroi T, Yago N, Nakazawa T. Purification and characterization of a substrate protein for mitochondrial ATP-dependent protease in bovine adrenal cortex. J Biochem (Tokyo) 1994;115:648–654. doi: 10.1093/oxfordjournals.jbchem.a124390. [DOI] [PubMed] [Google Scholar]
- 82.Banmeyer I, Marchand C, Verhaeghe C, Vucic B, Rees JF, Knoops B. Overexpression of human peroxiredoxin 5 in subcellular compartments of Chinese hamster ovary cells: effects on cytotoxicity and DNA damage caused by peroxides. Free radical biology & medicine. 2004;36:65–77. doi: 10.1016/j.freeradbiomed.2003.10.019. [DOI] [PubMed] [Google Scholar]
- 83.Fujii J, Ikeda Y. Advances in our understanding of peroxiredoxin, a multifunctional, mammalian redox protein. Redox Rep. 2002;7:123–130. doi: 10.1179/135100002125000352. [DOI] [PubMed] [Google Scholar]
- 84.Bellomo G, Vairetti M, Stivala L, Mirabelli F, Richelmi P, Orrenius S. Demonstration of nuclear compartmentalization of glutathione in hepatocytes. Proceedings of the National Academy of Sciences of the United States of America. 1992;89:4412–4416. doi: 10.1073/pnas.89.10.4412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Briviba K, Fraser G, Sies H, Ketterer B. Distribution of the monochlorobimane-glutathione conjugate between nucleus and cytosol in isolated hepatocytes. The Biochemical journal. 1993;294(Pt 3):631–633. doi: 10.1042/bj2940631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cotgreave IA. Analytical developments in the assay of intra- and extracellular GSH homeostasis: specific protein S-glutathionylation, cellular GSH and mixed disulphide compartmentalisation and interstitial GSH redox balance. Biofactors. 2003;17:269–277. doi: 10.1002/biof.5520170126. [DOI] [PubMed] [Google Scholar]
- 87.Voehringer DW, McConkey DJ, McDonnell TJ, Brisbay S, Meyn RE. Bcl-2 expression causes redistribution of glutathione to the nucleus. Proceedings of the National Academy of Sciences of the United States of America. 1998;95:2956–2960. doi: 10.1073/pnas.95.6.2956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lash LH, Jones DP. Distribution of oxidized and reduced forms of glutathione and cysteine in rat plasma. Archives of biochemistry and biophysics. 1985;240:583–592. doi: 10.1016/0003-9861(85)90065-7. [DOI] [PubMed] [Google Scholar]
- 89.Halvey PJ, Hansen JM, Johnson JM, Go YM, Samali A, Jones DP. Selective oxidative stress in cell nuclei by nuclear-targeted D-amino acid oxidase. Antioxidants & redox signaling. 2007;9:807–816. doi: 10.1089/ars.2007.1526. [DOI] [PubMed] [Google Scholar]
- 90.Hirota K, Murata M, Sachi Y, Nakamura H, Takeuchi J, Mori K, Yodoi J. Distinct roles of thioredoxin in the cytoplasm and in the nucleus. A two-step mechanism of redox regulation of transcription factor NF-kappaB. The Journal of biological chemistry. 1999;274:27891–27897. doi: 10.1074/jbc.274.39.27891. [DOI] [PubMed] [Google Scholar]
- 91.Wiesel P, Foster LC, Pellacani A, Layne MD, Hsieh CM, Huggins GS, Strauss P, Yet SF, Perrella MA. Thioredoxin facilitates the induction of heme oxygenase-1 in response to inflammatory mediators. The Journal of biological chemistry. 2000;275:24840–24846. doi: 10.1074/jbc.M000835200. [DOI] [PubMed] [Google Scholar]
- 92.Makino Y, Yoshikawa N, Okamoto K, Hirota K, Yodoi J, Makino I, Tanaka H. Direct association with thioredoxin allows redox regulation of glucocorticoid receptor function. The Journal of biological chemistry. 1999;274:3182–3188. doi: 10.1074/jbc.274.5.3182. [DOI] [PubMed] [Google Scholar]
- 93.Takagi Y, Mitsui A, Nishiyama A, Nozaki K, Sono H, Gon Y, Hashimoto N, Yodoi J. Overexpression of thioredoxin in transgenic mice attenuates focal ischemic brain damage. Proceedings of the National Academy of Sciences of the United States of America. 1999;96:4131–4136. doi: 10.1073/pnas.96.7.4131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Schroeder P, Popp R, Wiegand B, Altschmied J, Haendeler J. Nuclear redox-signaling is essential for apoptosis inhibition in endothelial cells--important role for nuclear thioredoxin-1. Arteriosclerosis, thrombosis, and vascular biology. 2007;27:2325–2331. doi: 10.1161/ATVBAHA.107.149419. [DOI] [PubMed] [Google Scholar]
- 95.Oka S, Masutani H, Liu W, Horita H, Wang D, Kizaka-Kondoh S, Yodoi J. Thioredoxin-binding protein-2-like inducible membrane protein is a novel vitamin D3 and peroxisome proliferator-activated receptor (PPAR)gamma ligand target protein that regulates PPARgamma signaling. Endocrinology. 2006;147:733–743. doi: 10.1210/en.2005-0679. [DOI] [PubMed] [Google Scholar]
- 96.Hirota K, Matsui M, Murata M, Takashima Y, Cheng FS, Itoh T, Fukuda K, Yodoi J. Nucleoredoxin, glutaredoxin, and thioredoxin differentially regulate NF-kappaB, AP-1, and CREB activation in HEK293 cells. Biochem Biophys Res Commun. 2000;274:177–182. doi: 10.1006/bbrc.2000.3106. [DOI] [PubMed] [Google Scholar]
- 97.Wei SJ, Botero A, Hirota K, Bradbury CM, Markovina S, Laszlo A, Spitz DR, Goswami PC, Yodoi J, Gius D. Thioredoxin nuclear translocation and interaction with redox factor-1 activates the activator protein-1 transcription factor in response to ionizing radiation. Cancer Res. 2000;60:6688–6695. [PubMed] [Google Scholar]
- 98.Dijkwel PA, Wenink PW. Structural integrity of the nuclear matrix: differential effects of thiol agents and metal chelators. J Cell Sci. 1986;84:53–67. doi: 10.1242/jcs.84.1.53. [DOI] [PubMed] [Google Scholar]
- 99.Klug A, Rhodes D. Zinc fingers: a novel protein fold for nucleic acid recognition. Cold Spring Harb Symp Quant Biol. 1987;52:473–482. doi: 10.1101/sqb.1987.052.01.054. [DOI] [PubMed] [Google Scholar]
- 100.De Capoa A, Ferraro M, Lavia P, Pelliccia F, Finazzi-Agro A. Silver staining of the nucleolus organizer regions (NOR) requires clusters of sulfhydryl groups. J Histochem Cytochem. 1982;30:908–911. doi: 10.1177/30.9.6182186. [DOI] [PubMed] [Google Scholar]
- 101.Suthanthiran M, Anderson ME, Sharma VK, Meister A. Glutathione regulates activation-dependent DNA synthesis in highly purified normal human T lymphocytes stimulated via the CD2 and CD3 antigens. Proceedings of the National Academy of Sciences of the United States of America. 1990;87:3343–3347. doi: 10.1073/pnas.87.9.3343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sandstrom BE, Marklund SL. Effects of variation in glutathione peroxidase activity on DNA damage and cell survival in human cells exposed to hydrogen peroxide and t-butyl hydroperoxide. The Biochemical journal. 1990;271:17–23. doi: 10.1042/bj2710017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sen CK, Packer L. Antioxidant and redox regulation of gene transcription. Faseb J. 1996;10:709–720. doi: 10.1096/fasebj.10.7.8635688. [DOI] [PubMed] [Google Scholar]
- 104.Kamada K, Goto S, Okunaga T, Ihara Y, Tsuji K, Kawai Y, Uchida K, Osawa T, Matsuo T, Nagata I, Kondo T. Nuclear glutathione S-transferase pi prevents apoptosis by reducing the oxidative stress-induced formation of exocyclic DNA products. Free radical biology & medicine. 2004;37:1875–1884. doi: 10.1016/j.freeradbiomed.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 105.Goto S, Kamada K, Soh Y, Ihara Y, Kondo T. Significance of nuclear glutathione S-transferase pi in resistance to anti-cancer drugs. Jpn J Cancer Res. 2002;93:1047–1056. doi: 10.1111/j.1349-7006.2002.tb02482.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Moffat GJ, McLaren AW, Wolf CR. Involvement of Jun and Fos proteins in regulating transcriptional activation of the human pi class glutathione S-transferase gene in multidrug-resistant MCF7 breast cancer cells. The Journal of biological chemistry. 1994;269:16397–16402. [PubMed] [Google Scholar]
- 107.Ralat LA, Manevich Y, Fisher AB, Colman RF. Direct evidence for the formation of a complex between 1-cysteine peroxiredoxin and glutathione S-transferase pi with activity changes in both enzymes. Biochemistry. 2006;45:360–372. doi: 10.1021/bi0520737. [DOI] [PubMed] [Google Scholar]
- 108.Manevich Y, Feinstein SI, Fisher AB. Activation of the antioxidant enzyme 1-CYS peroxiredoxin requires glutathionylation mediated by heterodimerization with pi GST. Proceedings of the National Academy of Sciences of the United States of America. 2004;101:3780–3785. doi: 10.1073/pnas.0400181101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Abate C, Patel L, Rauscher FJ, 3rd, Curran T. Redox regulation of fos and jun DNA-binding activity in vitro. Science (New York, N.Y. 1990;249:1157–1161. doi: 10.1126/science.2118682. [DOI] [PubMed] [Google Scholar]
- 110.Allen RG, Tresini M. Oxidative stress and gene regulation. Free radical biology & medicine. 2000;28:463–499. doi: 10.1016/s0891-5849(99)00242-7. [DOI] [PubMed] [Google Scholar]
- 111.Bloom D, Dhakshinamoorthy S, Jaiswal AK. Site-directed mutagenesis of cysteine to serine in the DNA binding region of Nrf2 decreases its capacity to upregulate antioxidant response element-mediated expression and antioxidant induction of NAD(P)H:quinone oxidoreductase1 gene. Oncogene. 2002;21:2191–2200. doi: 10.1038/sj.onc.1205288. [DOI] [PubMed] [Google Scholar]
- 112.Bodwell JE, Holbrook NJ, Munck A. Evidence for distinct sulfhydryl groups associated with steroid- and DNA-binding domains of rat thymus glucocorticoid receptors. Biochemistry. 1984;23:4237–4242. doi: 10.1021/bi00313a034. [DOI] [PubMed] [Google Scholar]
- 113.Galter D, Mihm S, Droge W. Distinct effects of glutathione disulphide on the nuclear transcription factor kappa B and the activator protein-1. European journal of biochemistry / FEBS. 1994;221:639–648. doi: 10.1111/j.1432-1033.1994.tb18776.x. [DOI] [PubMed] [Google Scholar]
- 114.Hainaut P, Milner J. Redox modulation of p53 conformation and sequence-specific DNA binding in vitro. Cancer Res. 1993;53:4469–4473. [PubMed] [Google Scholar]
- 115.Bauskin AR, Alkalay I, Ben-Neriah Y. Redox regulation of a protein tyrosine kinase in the endoplasmic reticulum. Cell. 1991;66:685–696. doi: 10.1016/0092-8674(91)90114-e. [DOI] [PubMed] [Google Scholar]
- 116.Cerutti PA, Trump BF. Inflammation and oxidative stress in carcinogenesis. Cancer Cells. 1991;3:1–7. [PubMed] [Google Scholar]
- 117.Devary Y, Gottlieb RA, Lau LF, Karin M. Rapid and preferential activation of the c-jun gene during the mammalian UV response. Molecular and cellular biology. 1991;11:2804–2811. doi: 10.1128/mcb.11.5.2804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Abate C, Luk D, Gagne E, Roeder RG, Curran T. Fos and jun cooperate in transcriptional regulation via heterologous activation domains. Molecular and cellular biology. 1990;10:5532–5535. doi: 10.1128/mcb.10.10.5532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Hirota K, Matsui M, Iwata S, Nishiyama A, Mori K, Yodoi J. AP-1 transcriptional activity is regulated by a direct association between thioredoxin and Ref-1. Proceedings of the National Academy of Sciences of the United States of America. 1997;94:3633–3638. doi: 10.1073/pnas.94.8.3633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Xanthoudakis S, Curran T. Identification and characterization of Ref-1, a nuclear protein that facilitates AP-1 DNA-binding activity. The EMBO journal. 1992;11:653–665. doi: 10.1002/j.1460-2075.1992.tb05097.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Immenschuh S, Baumgart-Vogt E. Peroxiredoxins, oxidative stress, and cell proliferation. Antioxidants & redox signaling. 2005;7:768–777. doi: 10.1089/ars.2005.7.768. [DOI] [PubMed] [Google Scholar]
- 122.Sen R, Baltimore D. Inducibility of kappa immunoglobulin enhancer-binding protein Nf-kappa B by a posttranslational mechanism. Cell. 1986;47:921–928. doi: 10.1016/0092-8674(86)90807-x. [DOI] [PubMed] [Google Scholar]
- 123.Baeuerle PA, Henkel T. Function and activation of NF-kappa B in the immune system. Annu Rev Immunol. 1994;12:141–179. doi: 10.1146/annurev.iy.12.040194.001041. [DOI] [PubMed] [Google Scholar]
- 124.Hansen JM, Moriarty-Craige S, Jones DP. Nuclear and cytoplasmic peroxiredoxin-1 differentially regulate NF-kappaB activities. Free radical biology & medicine. 2007;43:282–288. doi: 10.1016/j.freeradbiomed.2007.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Matthews JR, Botting CH, Panico M, Morris HR, Hay RT. Inhibition of NF-kappaB DNA binding by nitric oxide. Nucleic Acids Res. 1996;24:2236–2242. doi: 10.1093/nar/24.12.2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Toledano MB, Ghosh D, Trinh F, Leonard WJ. N-terminal DNA-binding domains contribute to differential DNA-binding specificities of NF-kappa B p50 and p65. Molecular and cellular biology. 1993;13:852–860. doi: 10.1128/mcb.13.2.852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Toledano MB, Leonard WJ. Modulation of transcription factor NF-kappa B binding activity by oxidation-reduction in vitro. Proceedings of the National Academy of Sciences of the United States of America. 1991;88:4328–4332. doi: 10.1073/pnas.88.10.4328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Angkeow P, Deshpande SS, Qi B, Liu YX, Park YC, Jeon BH, Ozaki M, Irani K. Redox factor-1: an extra-nuclear role in the regulation of endothelial oxidative stress and apoptosis. Cell death and differentiation. 2002;9:717–725. doi: 10.1038/sj.cdd.4401025. [DOI] [PubMed] [Google Scholar]
- 129.Nishi T, Shimizu N, Hiramoto M, Sato I, Yamaguchi Y, Hasegawa M, Aizawa S, Tanaka H, Kataoka K, Watanabe H, Handa H. Spatial redox regulation of a critical cysteine residue of NF-kappa B in vivo. The Journal of biological chemistry. 2002;277:44548–44556. doi: 10.1074/jbc.M202970200. [DOI] [PubMed] [Google Scholar]
- 130.Jeyapaul J, Jaiswal AK. Nrf2 and c-Jun regulation of antioxidant response element (ARE)-mediated expression and induction of gamma-glutamylcysteine synthetase heavy subunit gene. Biochem Pharmacol. 2000;59:1433–1439. doi: 10.1016/s0006-2952(00)00256-2. [DOI] [PubMed] [Google Scholar]
- 131.Sankaranarayanan K, Jaiswal AK. Nrf3 negatively regulates antioxidant-response element-mediated expression and antioxidant induction of NAD(P)H:quinone oxidoreductase1 gene. The Journal of biological chemistry. 2004;279:50810–50817. doi: 10.1074/jbc.M404984200. [DOI] [PubMed] [Google Scholar]
- 132.Kensler TW, Curphey TJ, Maxiutenko Y, Roebuck BD. Chemoprotection by organosulfur inducers of phase 2 enzymes: dithiolethiones and dithiins. Drug Metabol Drug Interact. 2000;17:3–22. doi: 10.1515/dmdi.2000.17.1-4.3. [DOI] [PubMed] [Google Scholar]
- 133.Hansen JM, Watson WH, Jones DP. Compartmentation of Nrf-2 redox control: regulation of cytoplasmic activation by glutathione and DNA binding by thioredoxin-1. Toxicol Sci. 2004;82:308–317. doi: 10.1093/toxsci/kfh231. [DOI] [PubMed] [Google Scholar]
- 134.Carpenter G, Cohen S. Epidermal growth factor. The Journal of biological chemistry. 1990;265:7709–7712. [PubMed] [Google Scholar]
- 135.Samiec PS, Drews-Botsch C, Flagg EW, Kurtz JC, Sternberg P, Jr, Reed RL, Jones DP. Glutathione in human plasma: decline in association with aging, age-related macular degeneration, and diabetes. Free radical biology & medicine. 1998;24:699–704. doi: 10.1016/s0891-5849(97)00286-4. [DOI] [PubMed] [Google Scholar]
- 136.Jones DP, Go YM, Anderson CL, Ziegler TR, Kinkade JM, Jr, Kirlin WG. Cysteine/cystine couple is a newly recognized node in the circuitry for biologic redox signaling and control. Faseb J. 2004;18:1246–1248. doi: 10.1096/fj.03-0971fje. [DOI] [PubMed] [Google Scholar]
- 137.Nkabyo YS, Ziegler TR, Gu LH, Watson WH, Jones DP. Glutathione and thioredoxin redox during differentiation in human colon epithelial (Caco-2) cells. Am J Physiol Gastrointest Liver Physiol. 2002;283:G1352–G1359. doi: 10.1152/ajpgi.00183.2002. [DOI] [PubMed] [Google Scholar]
- 138.Jones DP, Mody VC, Jr, Carlson JL, Lynn MJ, Sternberg P., Jr Redox analysis of human plasma allows separation of pro-oxidant events of aging from decline in antioxidant defenses. Free radical biology & medicine. 2002;33:1290–1300. doi: 10.1016/s0891-5849(02)01040-7. [DOI] [PubMed] [Google Scholar]
- 139.Jones DP. Redefining oxidative stress. Antioxidants & redox signaling. 2006;8:1865–1879. doi: 10.1089/ars.2006.8.1865. [DOI] [PubMed] [Google Scholar]
- 140.Moriarty-Craige SE, Jones DP. Extracellular thiols and thiol/disulfide redox in metabolism. Annu Rev Nutr. 2004;24:481–509. doi: 10.1146/annurev.nutr.24.012003.132208. [DOI] [PubMed] [Google Scholar]
- 141.Brown LA, Ping XD, Harris FL, Gauthier TW. Glutathione availability modulates alveolar macrophage function in the chronic ethanol-fed rat. Am J Physiol Lung Cell Mol Physiol. 2007;292:L824–L832. doi: 10.1152/ajplung.00346.2006. [DOI] [PubMed] [Google Scholar]
- 142.Go YM, Jones DP. Intracellular proatherogenic events and cell adhesion modulated by extracellular thiol/disulfide redox state. Circulation. 2005;111:2973–2980. doi: 10.1161/CIRCULATIONAHA.104.515155. [DOI] [PubMed] [Google Scholar]
- 143.Jiang S, Moriarty-Craige SE, Orr M, Cai J, Sternberg P, Jr, Jones DP. Oxidant-induced apoptosis in human retinal pigment epithelial cells: dependence on extracellular redox state. Invest Ophthalmol Vis Sci. 2005;46:1054–1061. doi: 10.1167/iovs.04-0949. [DOI] [PubMed] [Google Scholar]
- 144.Ashfaq S, Abramson JL, Jones DP, Rhodes SD, Weintraub WS, Hooper WC, Vaccarino V, Harrison DG, Quyyumi AA. The relationship between plasma levels of oxidized and reduced thiols and early atherosclerosis in healthy adults. J Am Coll Cardiol. 2006;47:1005–1011. doi: 10.1016/j.jacc.2005.09.063. [DOI] [PubMed] [Google Scholar]
- 145.Jonas CR, Puckett AB, Jones DP, Griffith DP, Szeszycki EE, Bergman GF, Furr CE, Tyre C, Carlson JL, Galloway JR, Blumberg JB, Ziegler TR. Plasma antioxidant status after high-dose chemotherapy: a randomized trial of parenteral nutrition in bone marrow transplantation patients. Am J Clin Nutr. 2000;72:181–189. doi: 10.1093/ajcn/72.1.181. [DOI] [PubMed] [Google Scholar]
- 146.Ng ES, Kubes P. The physiology of S-nitrosothiols: carrier molecules for nitric oxide. Canadian journal of physiology and pharmacology. 2003;81:759–764. doi: 10.1139/y03-078. [DOI] [PubMed] [Google Scholar]
- 147.Tellez-Sanz R, Cesareo E, Nuccetelli M, Aguilera AM, Baron C, Parker LJ, Adams JJ, Morton CJ, Lo Bello M, Parker WM, Garcia-Fuentes L. Calorimetric and structural studies of the nitric oxide carrier S-nitrosoglutathione bound to human glutathione transferase P1-1. Protein Sci. 2006;15:1093–1105. doi: 10.1110/ps.052055206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Hoshino Y, Shioji K, Nakamura H, Masutani H, Yodoi J. From oxygen sensing to heart failure: role of thioredoxin. Antioxidants & redox signaling. 2007;9:689–699. doi: 10.1089/ars.2007.1575. [DOI] [PubMed] [Google Scholar]
- 149.Blanco RA, Ziegler TR, Carlson BA, Cheng PY, Park Y, Cotsonis GA, Accardi CJ, Jones DP. Diurnal variation in glutathione and cysteine redox states in human plasma. Am J Clin Nutr. 2007;86:1016–1023. doi: 10.1093/ajcn/86.4.1016. [DOI] [PubMed] [Google Scholar]
- 150.Hildebrandt W, Kinscherf R, Hauer K, Holm E, Droge W. Plasma cystine concentration and redox state in aging and physical exercise. Mech Ageing Dev. 2002;123:1269–1281. doi: 10.1016/s0047-6374(02)00013-1. [DOI] [PubMed] [Google Scholar]
- 151.Moriarty SE, Shah JH, Lynn M, Jiang S, Openo K, Jones DP, Sternberg P. Oxidation of glutathione and cysteine in human plasma associated with smoking. Free radical biology & medicine. 2003;35:1582–1588. doi: 10.1016/j.freeradbiomed.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 152.Bai C, Jones DP. GSH transport and GSH-dependent detoxication in small intestine of rats exposed in vivo to hypoxia. Am J Physiol. 1996;271:G701–G706. doi: 10.1152/ajpgi.1996.271.4.G701. [DOI] [PubMed] [Google Scholar]
- 153.Neu J, Roig JC, Meetze WH, Veerman M, Carter C, Millsaps M, Bowling D, Dallas MJ, Sleasman J, Knight T, Auestad N. Enteral glutamine supplementation for very low birth weight infants decreases morbidity. J Pediatr. 1997;131:691–699. doi: 10.1016/s0022-3476(97)70095-7. [DOI] [PubMed] [Google Scholar]
- 154.Pastore A, Tozzi G, Gaeta LM, Bertini E, Serafini V, Di Cesare S, Bonetto V, Casoni F, Carrozzo R, Federici G, Piemonte F. Actin glutathionylation increases in fibroblasts of patients with Friedreich's ataxia: a potential role in the pathogenesis of the disease. The Journal of biological chemistry. 2003;278:42588–42595. doi: 10.1074/jbc.M301872200. [DOI] [PubMed] [Google Scholar]
- 155.Piemonte F, Pastore A, Tozzi G, Tagliacozzi D, Santorelli FM, Carrozzo R, Casali C, Damiano M, Federici G, Bertini E. Glutathione in blood of patients with Friedreich's ataxia. Eur J Clin Invest. 2001;31:1007–1011. doi: 10.1046/j.1365-2362.2001.00922.x. [DOI] [PubMed] [Google Scholar]
- 156.Moriarty-Craige SE, Ha KN, Sternberg P, Jr, Lynn M, Bressler S, Gensler G, Jones DP. Effects of long-term zinc supplementation on plasma thiol metabolites and redox status in patients with age-related macular degeneration. Am J Ophthalmol. 2007;143:206–211. doi: 10.1016/j.ajo.2006.09.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Jonas CR, Gu LH, Nkabyo YS, Mannery YO, Avissar NE, Sax HC, Jones DP, Ziegler TR. Glutamine and KGF each regulate extracellular thiol/disulfide redox and enhance proliferation in Caco-2 cells. Am J Physiol Regul Integr Comp Physiol. 2003;285:R1421–R1429. doi: 10.1152/ajpregu.00702.2002. [DOI] [PubMed] [Google Scholar]
- 158.Nkabyo YS, Go YM, Ziegler TR, Jones DP. Extracellular cysteine/cystine redox regulates the p44/p42 MAPK pathway by metalloproteinase-dependent epidermal growth factor receptor signaling. Am J Physiol Gastrointest Liver Physiol. 2005;289:G70–G78. doi: 10.1152/ajpgi.00280.2004. [DOI] [PubMed] [Google Scholar]
- 159.Ramirez A, Ramadan B, Ritzenthaler JD, Rivera HN, Jones DP, Roman J. Extracellular cysteine/cystine redox potential controls lung fibroblast proliferation and matrix expression through upregulation of transforming growth factor-{beta} Am J Physiol Lung Cell Mol Physiol. 2007 doi: 10.1152/ajplung.00010.2007. [DOI] [PubMed] [Google Scholar]
- 160.Razidlo GL, Kortum RL, Haferbier JL, Lewis RE. Phosphorylation regulates KSR1 stability, ERK activation, and cell proliferation. The Journal of biological chemistry. 2004;279:47808–47814. doi: 10.1074/jbc.M406395200. [DOI] [PubMed] [Google Scholar]
- 161.Schubert SY, Benarroch A, Ostvang J, Edelman ER. Regulation of endothelial cell proliferation by primary monocytes. Arteriosclerosis, thrombosis, and vascular biology. 2008;28:97–104. doi: 10.1161/ATVBAHA.107.157537. [DOI] [PubMed] [Google Scholar]
- 162.Aw TY. Cellular redox: a modulator of intestinal epithelial cell proliferation. News Physiol Sci. 2003;18:201–204. doi: 10.1152/nips.01448.2003. [DOI] [PubMed] [Google Scholar]
- 163.Berk BC. Vascular smooth muscle growth: autocrine growth mechanisms. Physiological reviews. 2001;81:999–1030. doi: 10.1152/physrev.2001.81.3.999. [DOI] [PubMed] [Google Scholar]
- 164.Nakamura H, De Rosa SC, Yodoi J, Holmgren A, Ghezzi P, Herzenberg LA, Herzenberg LA. Chronic elevation of plasma thioredoxin: inhibition of chemotaxis and curtailment of life expectancy in AIDS. Proceedings of the National Academy of Sciences of the United States of America. 2001;98:2688–2693. doi: 10.1073/pnas.041624998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Nakamura H, Herzenberg LA, Bai J, Araya S, Kondo N, Nishinaka Y, Herzenberg LA, Yodoi J. Circulating thioredoxin suppresses lipopolysaccharide-induced neutrophil chemotaxis. Proceedings of the National Academy of Sciences of the United States of America. 2001;98:15143–15148. doi: 10.1073/pnas.191498798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Sahaf B, Rosen A. Secretion of 10-kDa and 12-kDa thioredoxin species from blood monocytes and transformed leukocytes. Antioxidants & redox signaling. 2000;2:717–726. doi: 10.1089/ars.2000.2.4-717. [DOI] [PubMed] [Google Scholar]
- 167.Billiet L, Furman C, Larigauderie G, Copin C, Brand K, Fruchart JC, Rouis M. Extracellular human thioredoxin-1 inhibits lipopolysaccharide-induced interleukin-1beta expression in human monocyte-derived macrophages. The Journal of biological chemistry. 2005;280:40310–40318. doi: 10.1074/jbc.M503644200. [DOI] [PubMed] [Google Scholar]
- 168.Silberstein DS, McDonough S, Minkoff MS, Balcewicz-Sablinska MK. Human eosinophil cytotoxicity-enhancing factor. Eosinophil-stimulating and dithiol reductase activities of biosynthetic (recombinant) species with COOH-terminal deletions. The Journal of biological chemistry. 1993;268:9138–9142. [PubMed] [Google Scholar]
- 169.Gon Y, Sasada T, Matsui M, Hashimoto S, Takagi Y, Iwata S, Wada H, Horie T, Yodoi J. Expression of thioredoxin in bleomycin-injured airway epithelium: possible role of protection against bleomycin induced epithelial injury. Life Sci. 2001;68:1877–1888. doi: 10.1016/s0024-3205(01)00980-8. [DOI] [PubMed] [Google Scholar]
- 170.Hagg D, Englund MC, Jernas M, Schmidt C, Wiklund O, Hulten LM, Ohlsson BG, Carlsson LM, Carlsson B, Svensson PA. Oxidized LDL induces a coordinated up-regulation of the glutathione and thioredoxin systems in human macrophages. Atherosclerosis. 2006;185:282–289. doi: 10.1016/j.atherosclerosis.2005.06.034. [DOI] [PubMed] [Google Scholar]
- 171.Aota M, Matsuda K, Isowa N, Wada H, Yodoi J, Ban T. Protection against reperfusion-induced arrhythmias by human thioredoxin. J Cardiovasc Pharmacol. 1996;27:727–732. doi: 10.1097/00005344-199605000-00016. [DOI] [PubMed] [Google Scholar]
- 172.Shioji K, Kishimoto C, Nakamura H, Masutani H, Yuan Z, Oka S, Yodoi J. Overexpression of thioredoxin-1 in transgenic mice attenuates adriamycin-induced cardiotoxicity. Circulation. 2002;106:1403–1409. doi: 10.1161/01.cir.0000027817.55925.b4. [DOI] [PubMed] [Google Scholar]
- 173.Liu W, Nakamura H, Shioji K, Tanito M, Oka S, Ahsan MK, Son A, Ishii Y, Kishimoto C, Yodoi J. Thioredoxin-1 ameliorates myosin-induced autoimmune myocarditis by suppressing chemokine expressions and leukocyte chemotaxis in mice. Circulation. 2004;110:1276–1283. doi: 10.1161/01.CIR.0000141803.41217.B6. [DOI] [PubMed] [Google Scholar]
- 174.Okubo K, Kosaka S, Isowa N, Hirata T, Hitomi S, Yodoi J, Nakano M, Wada H. Amelioration of ischemia-reperfusion injury by human thioredoxin in rabbit lung. J Thorac Cardiovasc Surg. 1997;113:1–9. doi: 10.1016/S0022-5223(97)70393-3. [DOI] [PubMed] [Google Scholar]
- 175.Miwa K, Kishimoto C, Nakamura H, Makita T, Ishii K, Okuda N, Yodoi J, Sasayama S. Serum thioredoxin and alpha-tocopherol concentrations in patients with major risk factors. Circ J. 2005;69:291–294. doi: 10.1253/circj.69.291. [DOI] [PubMed] [Google Scholar]
- 176.Callister ME, Burke-Gaffney A, Quinlan GJ, Nicholson AG, Florio R, Nakamura H, Yodoi J, Evans TW. Extracellular thioredoxin levels are increased in patients with acute lung injury. Thorax. 2006;61:521–527. doi: 10.1136/thx.2005.053041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Fagarasanu A, Fagarasanu M, Rachubinski RA. Maintaining peroxisome populations: a story of division and inheritance. Annual review of cell and developmental biology. 2007;23:321–344. doi: 10.1146/annurev.cellbio.23.090506.123456. [DOI] [PubMed] [Google Scholar]
- 178.Schrader M, Fahimi HD. Peroxisomes and oxidative stress. Biochimica et biophysica acta. 2006;1763:1755–1766. doi: 10.1016/j.bbamcr.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 179.Wanders RJ, Waterham HR. Biochemistry of mammalian peroxisomes revisited. Annual review of biochemistry. 2006;75:295–332. doi: 10.1146/annurev.biochem.74.082803.133329. [DOI] [PubMed] [Google Scholar]
- 180.Loughran PA, Stolz DB, Vodovotz Y, Watkins SC, Simmons RL, Billiar TR. Monomeric inducible nitric oxide synthase localizes to peroxisomes in hepatocytes. Proceedings of the National Academy of Sciences of the United States of America. 2005;102:13837–13842. doi: 10.1073/pnas.0503926102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Jones DP. Intracellular inhibition of catalase by alpha-methyldopa. Research communications in chemical pathology and pharmacology. 1981;33:215–222. [PubMed] [Google Scholar]
- 182.Jones DP. Intracellular catalase function: analysis of the catalatic activity by product formation in isolated liver cells. Archives of biochemistry and biophysics. 1982;214:806–814. doi: 10.1016/0003-9861(82)90087-x. [DOI] [PubMed] [Google Scholar]
- 183.Sheikh FG, Pahan K, Khan M, Barbosa E, Singh I. Abnormality in catalase import into peroxisomes leads to severe neurological disorder. Proceedings of the National Academy of Sciences of the United States of America. 1998;95:2961–2966. doi: 10.1073/pnas.95.6.2961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Zoeller RA, Allen LA, Santos MJ, Lazarow PB, Hashimoto T, Tartakoff AM, Raetz CR. Chinese hamster ovary cell mutants defective in peroxisome biogenesis. Comparison to Zellweger syndrome. The Journal of biological chemistry. 1989;264:21872–21878. [PubMed] [Google Scholar]
- 185.Terlecky SR, Koepke JI, Walton PA. Peroxisomes and aging. Biochimica et biophysica acta. 2006;1763:1749–1754. doi: 10.1016/j.bbamcr.2006.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Noctor G, Veljovic-Jovanovic S, Foyer CH. Peroxide processing in photosynthesis: antioxidant coupling and redox signalling. Philosophical transactions of the Royal Society of London. 2000;355:1465–1475. doi: 10.1098/rstb.2000.0707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Hughes AL, Powell DW, Bard M, Eckstein J, Barbuch R, Link AJ, Espenshade PJ. Dap1/PGRMC1 binds and regulates cytochrome P450 enzymes. Cell metabolism. 2007;5:143–149. doi: 10.1016/j.cmet.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 188.Henderson MP, Hwang YT, Dyer JM, Mullen RT, Andrews DW. The C-terminus of cytochrome b5 confers endoplasmic reticulum specificity by preventing spontaneous insertion into membranes. The Biochemical journal. 2007;401:701–709. doi: 10.1042/BJ20060990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Coussin F, Macrez N, Morel JL, Mironneau J. Requirement of ryanodine receptor subtypes 1 and 2 for Ca(2+)-induced Ca(2+) release in vascular myocytes. The Journal of biological chemistry. 2000;275:9596–9603. doi: 10.1074/jbc.275.13.9596. [DOI] [PubMed] [Google Scholar]
- 190.Sen CK. Cellular thiols and redox-regulated signal transduction. Current topics in cellular regulation. 2000;36:1–30. doi: 10.1016/s0070-2137(01)80001-7. [DOI] [PubMed] [Google Scholar]
- 191.Cenci S, Sitia R. Managing and exploiting stress in the antibody factory. FEBS letters. 2007;581:3652–3657. doi: 10.1016/j.febslet.2007.04.031. [DOI] [PubMed] [Google Scholar]
- 192.Sitia R, Neuberger M, Alberini C, Bet P, Fra A, Valetti C, Williams G, Milstein C. Developmental regulation of IgM secretion: the role of the carboxyterminal cysteine. Cell. 1990;60:781–790. doi: 10.1016/0092-8674(90)90092-s. [DOI] [PubMed] [Google Scholar]
- 193.Anelli T, Ceppi S, Bergamelli L, Cortini M, Masciarelli S, Valetti C, Sitia R. Sequential steps and checkpoints in the early exocytic compartment during secretory IgM biogenesis. The EMBO journal. 2007;26:4177–4188. doi: 10.1038/sj.emboj.7601844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Gross E, Sevier CS, Heldman N, Vitu E, Bentzur M, Kaiser CA, Thorpe C, Fass D. Generating disulfides enzymatically: reaction products and electron acceptors of the endoplasmic reticulum thiol oxidase Ero1p. Proceedings of the National Academy of Sciences of the United States of America. 2006;103:299–304. doi: 10.1073/pnas.0506448103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Chakravarthi S, Jessop CE, Bulleid NJ. The role of glutathione in disulphide bond formation and endoplasmic-reticulum-generated oxidative stress. EMBO Rep. 2006;7:271–275. doi: 10.1038/sj.embor.7400645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Cuozzo JW, Kaiser CA. Competition between glutathione and protein thiols for disulphide-bond formation. Nat Cell Biol. 1999;1:130–135. doi: 10.1038/11047. [DOI] [PubMed] [Google Scholar]
- 197.Gorlach A, Klappa P, Kietzmann T. The endoplasmic reticulum: folding, calcium homeostasis, signaling, and redox control. Antioxidants & redox signaling. 2006;8:1391–1418. doi: 10.1089/ars.2006.8.1391. [DOI] [PubMed] [Google Scholar]
- 198.Hwang C, Sinskey AJ, Lodish HF. Oxidized redox state of glutathione in the endoplasmic reticulum. Science (New York, N.Y. 1992;257:1496–1502. doi: 10.1126/science.1523409. [DOI] [PubMed] [Google Scholar]
- 199.Papp E, Szaraz P, Korcsmaros T, Csermely P. Changes of endoplasmic reticulum chaperone complexes, redox state, and impaired protein disulfide reductase activity in misfolding alpha1-antitrypsin transgenic mice. Faseb J. 2006;20:1018–1020. doi: 10.1096/fj.05-5065fje. [DOI] [PubMed] [Google Scholar]
- 200.Arunachalam B, Phan UT, Geuze HJ, Cresswell P. Enzymatic reduction of disulfide bonds in lysosomes: characterization of a gamma-interferon-inducible lysosomal thiol reductase (GILT) Proceedings of the National Academy of Sciences of the United States of America. 2000;97:745–750. doi: 10.1073/pnas.97.2.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Cherqui S, Kalatzis V, Trugnan G, Antignac C. The targeting of cystinosin to the lysosomal membrane requires a tyrosine-based signal and a novel sorting motif. The Journal of biological chemistry. 2001;276:13314–13321. doi: 10.1074/jbc.M010562200. [DOI] [PubMed] [Google Scholar]
- 202.Forestier L, Jean G, Cherqui S, Lewis C, van't Hoff W, Broyer M, Town C. Antignac, Molecular characterization of CTNS deletions in nephropathic cystinosis: development of a PCR-based detection assay. Am J Hum Genet. 1999;65:353–359. doi: 10.1086/302509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Gille L, Nohl H. The existence of a lysosomal redox chain and the role of ubiquinone. Archives of biochemistry and biophysics. 2000;375:347–354. doi: 10.1006/abbi.1999.1649. [DOI] [PubMed] [Google Scholar]
- 204.Nohl H, Gille L. The bifunctional activity of ubiquinone in lysosomal membranes. Biogerontology. 2002;3:125–131. doi: 10.1023/a:1015288220217. [DOI] [PubMed] [Google Scholar]
- 205.Crane FL. Discovery of ubiquinone (coenzyme Q) and an overview of function. Mitochondrion. 2007;7 Suppl:S2–S7. doi: 10.1016/j.mito.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 206.Blewitt MG, Chung LA, London E. Effect of pH on the conformation of diphtheria toxin and its implications for membrane penetration. Biochemistry. 1985;24:5458–5464. doi: 10.1021/bi00341a027. [DOI] [PubMed] [Google Scholar]
- 207.Falnes PO, Olsnes S. Cell-mediated reduction and incomplete membrane translocation of diphtheria toxin mutants with internal disulfides in the A fragment. The Journal of biological chemistry. 1995;270:20787–20793. doi: 10.1074/jbc.270.35.20787. [DOI] [PubMed] [Google Scholar]
- 208.Falnes PO, Sandvig K. Penetration of protein toxins into cells. Current opinion in cell biology. 2000;12:407–413. doi: 10.1016/s0955-0674(00)00109-5. [DOI] [PubMed] [Google Scholar]
- 209.Ryser HJ, Mandel R, Ghani F. Cell surface sulfhydryls are required for the cytotoxicity of diphtheria toxin but not of ricin in Chinese hamster ovary cells. The Journal of biological chemistry. 1991;266:18439–18442. [PubMed] [Google Scholar]
- 210.Feener EP, Shen WC, Ryser HJ. Cleavage of disulfide bonds in endocytosed macromolecules. A processing not associated with lysosomes or endosomes. The Journal of biological chemistry. 1990;265:18780–18785. [PubMed] [Google Scholar]
- 211.D'Autreaux B, Toledano MB. ROS as signalling molecules: mechanisms that generate specificity in ROS homeostasis. Nature reviews. 2007;8:813–824. doi: 10.1038/nrm2256. [DOI] [PubMed] [Google Scholar]
- 212.Saitoh M, Nishitoh H, Fujii M, Takeda K, Tobiume K, Sawada Y, Kawabata M, Miyazono K, Ichijo H. Mammalian thioredoxin is a direct inhibitor of apoptosis signal-regulating kinase (ASK) 1. The EMBO journal. 1998;17:2596–2606. doi: 10.1093/emboj/17.9.2596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Kirlin WG, Cai J, Thompson SA, Diaz D, Kavanagh TJ, Jones DP. Glutathione redox potential in response to differentiation and enzyme inducers. Free radical biology & medicine. 1999;27:1208–1218. doi: 10.1016/s0891-5849(99)00145-8. [DOI] [PubMed] [Google Scholar]
- 214.Schafer FQ, Buettner GR. Redox environment of the cell as viewed through the redox state of the glutathione disulfide/glutathione couple. Free radical biology & medicine. 2001;30:1191–1212. doi: 10.1016/s0891-5849(01)00480-4. [DOI] [PubMed] [Google Scholar]
- 215.Bedogni B, Pani G, Colavitti R, Riccio A, Borrello S, Murphy M, Smith R, Eboli ML, Galeotti T. Redox regulation of cAMP-responsive element-binding protein and induction of manganous superoxide dismutase in nerve growth factor-dependent cell survival. The Journal of biological chemistry. 2003;278:16510–16519. doi: 10.1074/jbc.M301089200. [DOI] [PubMed] [Google Scholar]
- 216.Irani K, Xia Y, Zweier JL, Sollott SJ, Der CJ, Fearon ER, Sundaresan M, Finkel T, Goldschmidt-Clermont PJ. Mitogenic signaling mediated by oxidants in Ras-transformed fibroblasts. Science (New York, N.Y. 1997;275:1649–1652. doi: 10.1126/science.275.5306.1649. [DOI] [PubMed] [Google Scholar]
- 217.Lee AC, Fenster BE, Ito H, Takeda K, Bae NS, Hirai T, Yu ZX, Ferrans VJ, Howard BH, Finkel T. Ras proteins induce senescence by altering the intracellular levels of reactive oxygen species. The Journal of biological chemistry. 1999;274:7936–7940. doi: 10.1074/jbc.274.12.7936. [DOI] [PubMed] [Google Scholar]
- 218.Santillo M, Mondola P, Seru R, Annella T, Cassano S, Ciullo I, Tecce MF, Iacomino G, Damiano S, Cuda G, Paterno R, Martignetti V, Mele E, Feliciello A, Avvedimento EV. Opposing functions of Ki- and Ha-Ras genes in the regulation of redox signals. Curr Biol. 2001;11:614–619. doi: 10.1016/s0960-9822(01)00159-2. [DOI] [PubMed] [Google Scholar]
- 219.Passos JF, von Zglinicki T, Saretzki G. Mitochondrial dysfunction and cell senescence: cause or consequence? Rejuvenation research. 2006;9:64–68. doi: 10.1089/rej.2006.9.64. [DOI] [PubMed] [Google Scholar]
- 220.Skulachev VP. Bioenergetic aspects of apoptosis, necrosis and mitoptosis. Apoptosis. 2006;11:473–485. doi: 10.1007/s10495-006-5881-9. [DOI] [PubMed] [Google Scholar]
- 221.Nemoto S, Takeda K, Yu ZX, Ferrans VJ, Finkel T. Role for mitochondrial oxidants as regulators of cellular metabolism. Molecular and cellular biology. 2000;20:7311–7318. doi: 10.1128/mcb.20.19.7311-7318.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Ramachandiran S, Hansen JM, Jones DP, Richardson JR, Miller GW. Divergent mechanisms of paraquat, MPP+, and rotenone toxicity: oxidation of thioredoxin and caspase-3 activation. Toxicol Sci. 2007;95:163–171. doi: 10.1093/toxsci/kfl125. [DOI] [PubMed] [Google Scholar]
- 223.Chen Y, Cai J, Jones DP. Mitochondrial thioredoxin in regulation of oxidant-induced cell death. FEBS letters. 2006;580:6596–6602. doi: 10.1016/j.febslet.2006.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Tanaka T, Nishiyama Y, Okada K, Hirota K, Matsui M, Yodoi J, Hiai H, Toyokuni S. Induction and nuclear translocation of thioredoxin by oxidative damage in the mouse kidney: independence of tubular necrosis and sulfhydryl depletion. Lab Invest. 1997;77:145–155. [PubMed] [Google Scholar]
- 225.Watson WH, Jones DP. Oxidation of nuclear thioredoxin during oxidative stress. FEBS letters. 2003;543:144–147. doi: 10.1016/s0014-5793(03)00430-7. [DOI] [PubMed] [Google Scholar]
- 226.Anderson CL, Iyer SS, Ziegler TR, Jones DP. Control of extracellular cysteine/cystine redox state by HT-29 cells is independent of cellular glutathione. Am J Physiol Regul Integr Comp Physiol. 2007;293:R1069–R1075. doi: 10.1152/ajpregu.00195.2007. [DOI] [PubMed] [Google Scholar]