Abstract
Understanding T cell immunodominance hierarchies is fundamental to the development of cellular-based vaccines and immunotherapy. A combination of influenza virus infection in C57BL/6J mice and reverse genetics is used here to dissect the role of T cell antigen receptor (TCR) repertoire in the immunodominant DbNP366CD8+ T cell response. Infection with an engineered virus (NPM6A) containing a single alanine (A) mutation at the critical p6 NP366–374 residue induced a noncross-reactive CD8+ T cell response characterized by a novel, narrower TCR repertoire per individual mouse that was nonetheless equivalent in magnitude to that generated after WT virus challenge. Although of lower overall avidity, the levels of both cytotoxic T lymphocyte activity and cytokine production were comparable with those seen for the native response. Importantly, the overdominance profile characteristic of secondary DbNP366-specific clonal expansions was retained for the NPM6A mutant. The primary determinants of immunodominance in this endogenous, non-TCR-transgenic model of viral immunity are thus independent of TCR repertoire composition and diversity. These findings both highlight the importance of effective antigen dose for T cell vaccination and/or immunotherapy and demonstrate the feasibility of priming the memory T cell compartment with engineered viruses to protect against commonly selected mutants viral (or tumor) escape mutants.
Keywords: avidity, viral escape, pMHC structure, TCR diversity, reverse genetics
Virus-specific CD8+ T cells play an essential role in limiting infectious process by killing virus-infected cells and/or producing proinflammatory cytokines (1). Because this CD8+ T cell-mediated immunity tends to be directed at 1 or 2 immunodominant epitopes and a number of subdominant determinants (2), we need to identify the major factors controlling immunodominance if we are to develop optimized T cell vaccines and immunotherapy protocols. Influenza A virus infection of C57BL/6J (B6, H2b) mice provides a well-characterized “natural” [non-T cell receptor (TCR)-transgenic] system for dissecting CD8+ T cell immunodominance hierarchies. Although there are at least 6 epitopes distributed between H2Db and H2Kb (3), the most prominent CD8+ sets that emerge after an initial encounter with an influenza A virus are specific for H2Db-bound peptides from the viral nucleoprotein (DbNP366–374) and acid polymerase (DbPA224–233) proteins (4). These DbNP366+CD8+ and DbPA224+CD8+ populations reach essentially comparable sizes after primary infection, although the DbPA224+CD8+ set peaks 1–2 days earlier (5), reflecting a higher naïve T cell precursor frequency (6, 7). After secondary challenge, the DbNP366+CD8+ T cells are massively overdominant, constituting up to 80% of the total virus-specific CD8+ response (8). This emphasis on DbNP366 in the recall response has been attributed to differences in the spectrum of antigen-presenting cell involvement (9), protein/peptide abundance, and T cell precursor frequency (7).
TCR repertoires selected by DbNP366 and DbPA224 differ in both extent and character. Analysis of TCR CDR3β sequence variability and clonal prevalence shows that DbPA224 recruits a predominantly “private” (specific for individual mice) and diverse range of TCRβ sequences (10), whereas CD8+ T cell recognition of DbNP366 is mediated via a narrower, “public” (conserved between individuals) TCR repertoire (11). Could selection of optimal public clones by DbNP366 but not DbPA224 explain the dramatic divergence in CD8+ T cell response magnitude, especially after secondary challenge? To date, the role of TCR fine specificity and particular TCR clones in establishing immunodominance hierarchies remains unclear. The present analysis asks whether the limited, public TCR repertoire characteristic of the DbNP366+CD8+ T cell response is a primary determinant of immunodominance.
Results
Residues Critical for TCR Recognition by DbNP366+CD8+ T Cells.
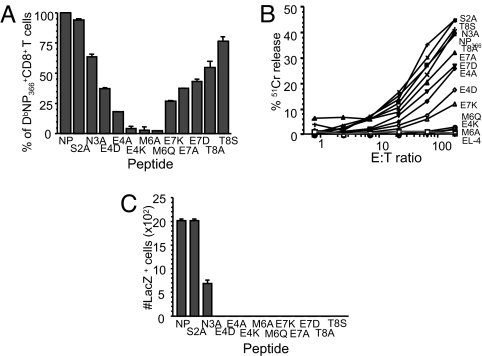
To determine critical residues for recognition of the NP366 peptide by H2Db-restricted CD8+ T cells, single amino acid mutations were made at different positions within the viral NP366 peptide, excluding the anchor amino acid (p5, p9). These included A substitutions (S2A, N3A, E4A, M6A, E7A, T8A), conserved (E4D, M6Q, E7D, T8S), and reverse charge (E4K, E7K) mutations. Mutant NP366 peptides were used to probe CD8+ T cells by intracellular cytokine secretion (ICS), a 51Cr-release assay and stimulation of DbNP366+LacZ-inducible T cell hybridomas. The recognition profiles of polyclonal DbNP366+CD8+ T cells obtained from mice infected with the WT virus were variably modified by different amino acid substitutions (Fig. 1 A and B). p6M appeared to be critical for TCR recognition, as stimulation with 2 different amino acid substitutions (M6A, M6Q) resulted in a complete loss of peptide-induced IFN-γ production (Fig. 1A) and 51Cr-mediated lysis (Fig. 1B). This finding is in accord with data showing that the emergence of viral escape mutants in mice transgenic for a DbNP366+ TCR resulted from a p6M mutation (12). The p4E position was also important, while substitutions at p3, p7, and p8 led to a partial loss of TCR recognition (Fig. 1A). Stimulating 3 distinct DbNP366+ LacZ-inducible hybridomas expressing 1 of the DbNP366+ public TCRβ sequences, SGGGNTGQL (11), with NP-mutant peptides led to different results. Monoclonal, public-TCR, DbNP366+ T cells responded optimally to only WT NP366 and NPS2A peptides and partially to the NPN3A peptide (Fig. 1C). Thus, although polyclonal DbNP366CD8+ T cells can recognize a spectrum of mutant NP366 peptides, the public DbNP366+ hybridomas do not tolerate mutations at p4, p6, p7, and p8, supporting the idea that limiting the diversity of antigen-specific TCRs has the potential to facilitate the emergence of mutant viruses (13).
Fig. 1.
Residues important for TCR recognition by DbNP366+CD8+ T cells. (A and B) Splenocytes obtained from PR (H1N1)-primed mice secondarily-infected with the WT HK (H3N2) influenza virus were stimulated with either the WT NP366–374 or a panel of mutant peptides with single amino acid substitutions. The extent of TCR recognition was assessed by IFN-γ production in the ICS assay (A) and 51Cr cytotoxicity after incubation with target EL-4 cells pulsed with 1 μM peptides and 750 μCi 51Cr (B). (C) The response profiles of monoclonal DbNP366+ LacZ-inducible hybridomas expressing the public SGGGNTGQL CDR3β (11) to WT NP366 and NP-mutant peptides are shown.
Characteristics of Infection and CD8+ T Cell Response Magnitude for the NPM6A Virus.
Having shown that p6M is critical for TCR recognition of DbNP366, we expressed the M6A mutation within the viral NP366 sequence to determine whether it would abrogate the WT DbNP366+CD8+ T cell response. What TCR repertoire might the new DbNPM6A epitope select after infection? Would the utilization of a novel TCR repertoire for DbNPM6A modify quantitative and qualitative aspects of the influenza NP-specific CD8+ T cell response? A single A substitution at p6 was engineered to create an M6A mutation within the viral NP366 peptide. Two serologically distinct viruses with the NPM6A change were generated by using the standard HKx31 (HK-NPM6A) and PR8 (PR-NPM6A) strains, to facilitate prime/boost experiments in the absence of cross-reactive antibodies.
The WT and mutant NPM6A viruses replicated to equivalent titers in B6 mice (Fig. 2A), suggesting no diminution in viral fitness (and thus NP amount and kinetics of production) as a consequence of the single amino acid change in this virus structural protein. In fact, the lung titers for HK-NPM6A were significantly (P > 0.05) higher on days 3 and 6, although both viruses were cleared with equivalent kinetics. This finding indicates that the level and duration of viral protein production is broadly comparable for the NPM6A and WT NP proteins. Furthermore, because NP366 and NPM6A peptides bind to the H-2Db MHC glycoprotein with equivalent affinity (14) and the thermostability [supporting information (SI) Fig. S1] of H2Db-NPM6A midpoint of thermal denaturation (Tm) of 63.3 ± 0.7 °C] is higher than that for the native H2Db-NP366 (Tm of 51.8 ± 0.7 °C), there is no reason to think that the mutant NPM6A peptide is any less “fit” than the WT NP366 when it comes to the generation of an immunogenic epitope.
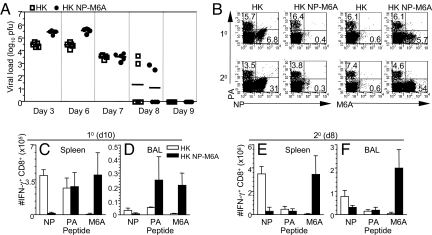
Fig. 2.
Virus clearance and CD8+ T cell profiles after infection with the WT HK and mutant HK-NPM6A viruses. Mice were infected with WT HK or the mutant HK-NPM6A virus. (A) Lungs were sampled at days 3, 6, 7, 8, and 9 after infection and titrated in a plaque assay. The results are log10 pfu per lung (n = 5). (B) CD8+ T cell responses were measured after 10 (day 10) or 20 (day 8) i.n. challenge of naïve or PR- or PR-NPM6A-primed mice with the homologous HK WT of HK-NPM6A virus. Cells were stained with the DbNP366-APC, DbNP-M6A-APC, or DbPA-PE tetramers.(C–F) The response magnitude was assessed for spleen (C and E) and BAL (D and F) sets by ICS. Datasets are mean ± SD for n = 5.
Primary and recall CD8+ T cell responses were generated by infecting naïve and PR i.p.-immunized B6 mice intranasally (i.n.) with the HK variants. Spleen (Fig. 2 B, C, and E) and bronchoalveolar lavage (BAL) (Fig. 2 D and F) CD8+ T cells were analyzed on day 10 (10) or day 8 (20) by staining with the DbNP366 and DbNPM6A tetramers (Fig. 2B) or stimulation with peptide (Fig. 2 C–F). The viruses carrying the NPM6A mutation induced the recruitment and expansion of naïve (Fig. 2 B, C, and E) and memory (Fig. 2 B, E, and F) DbNPM6A-specific CD8+ T cells at levels equivalent to the WT DbNP366+CD8+ set (8) (Fig. 2 B–F). It seems that the M-to-A substitution at p6 in the NP366 peptide created a novel peptide/MHC I complex (pMHCI) that is antigenically distinct from, but as immunogenic as, the WT epitope. Although the response magnitudes were similar in spleen (a good reflection of immunodominance), slightly larger NPM6A+CD8+ T cell numbers were recovered from the site of infection (BAL), perhaps reflecting the elevated antigen load on days 3 and 6 after viral exposure (Fig. 2A). Furthermore, the characteristic WT CD8+ T cell immunodominance hierarchies were maintained after exposure to viruses carrying the NPM6A mutation. As found for WT infections that induce expansion of the DbNP366CD8+ set, the primary responses to DbNPM6A and DbPA224 in lymphoid tissue look to be essentially comparable in size (Fig. 2 C and E). However, the secondary response to DbNPM6A showed the massive overdominance (relative to DbPA224) found invariably for the WT DbNP366+CD8+ set. Thus, although CD8+ T cells induced by the DbNP366 and DbM6A epitopes show little evidence of cross-reactivity, the responses to these 2 epitopes are similar, at least in the numerical sense of immunodominance.
Consequences for CD8+ T Cell Recognition and Function.
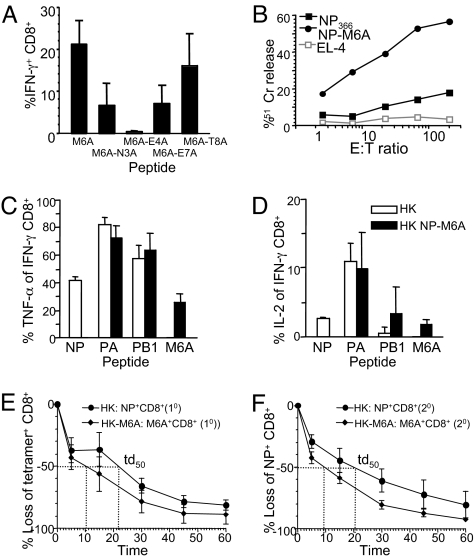
Analysis of response profiles with mutated peptides (Fig. 1A) was repeated (Fig. 3A) for the responding NPM6A+CD8+ T cells. Starting with NPM6A, we made a panel of single A substitutions (M6A-N3A, M6A-E4A, M6A-E7A, M6A-T8A) to identify the residues critical for TCR recognition. Stimulation of T cells recovered directly from mice infected with the HK-NPM6A virus established that polyclonal NPM6A+CD8+ T cells respond equivalently to the M6A and M6A-T8A peptides, respond partially to M6A-N3A and M6A-E7A, and cannot recognize the M6A-E4A mutation (Fig. 3A). This finding shows that the residue critical for TCR recognition by DbNPM6A+CD8+ T cells is now shifted to p4 E.
Fig. 3.
Functional quality of the emerging M6A+CD8+ sets. DbNPM6A+CD8+ T cells generated after challenge with the HK-NPM6A virus were assessed for important residues in TCR recognition (A), 51Cr-mediated killing (B), production of IFN-γ, TNF-α, and IL-2 (C and D), and TCR avidity for the pMHC complex (E and F). (A) Cells obtained from mice infected with NPM6A viruses were incubated with the NPM6A (or mutant peptides with further A mutations) to stimulate IFN-γ production. (B) Cells of mice secondarily challenged with the HK-NPM6A virus were cultured for 4 h. 51Cr-labeled EL-4 cells were pulsed with 1 μM of NP366 or NPM6A peptides. (C and D) Data (n = 5, mean ± SD) for hierarchical production of IFN-γ, TNF-α, and IL-2 after 10 or 20 infection with either WT HK or mutant HK-NPM6A viruses. (E and F) Tetramer dissociation as a measure of TCR avidity. Cells were stained with the DbNP336 or DbNPM6A tetramers and incubated with a mAb to H2Db to prevent rebinding of dissociated tetramer. The progressive diminution in tetramer staining was measured. Td50 defines time to 50% tetramer loss. Data represent mean± SD, n = 5.
The inference from the in vivo response experiments (Fig. 2) and the mutational analysis (Fig. 3A) that DbNP366 and DbNPM6A are distinct epitopes was further supported by the lack of cross-reactivity for cytotoxic T lymphocyte (CTL) populations when tested in a 51Cr release assay (Fig. 3B). The capacity to produce multiple cytokines (4) simultaneously (IFN-γ, TNF-α, and IL-2) showed that frequencies of double producers (IFN-γ/TNF-α) and triple producers (IFN-γ/TNF-α/IL-2) within the DbNPM6A+CD8+ set were equivalent to those found for the DbNP366+CD8+ populations but were significantly lower than the values for DbPA224+CD8+ T cells stimulated by the WT or NPM6A influenza viruses (Fig. 3 C and D). This finding, together with the CTL results (Fig. 3B), suggests that the DbNPM6A+CD8+ and DbNP366+CD8+ T cells are functionally comparable, although they differ in specificity. Binding avidities were compared by the tetramer dissociation rate (measuring the “off” rate component of avidity) (4) for DbNPM6A+CD8+ and DbNP366+CD8+ populations. The tetramer dissociation curves were compared for DbNPM6A+CD8+ and DbNP366+CD8+ TCRs after primary (Fig. 3E) and secondary (Fig. 3F) infection. The td50 value (the time to 50% tetramer loss) was much shorter for the DbNPM6A+CD8+ (t = 10.1 min and t = 10.0 min for 10 and 20 responses) than for the WT DbNP366+CD8+ T cells (t = 21.8 min and t = 22.0 min] for 10 and 20, respectively), indicating that, on a population basis, the DbNPM6A epitope selects TCRs that bind less strongly. Furthermore, TCR/pMHCI avidity was found to be lower for DbNPM6A by 2 other measures, tetramer dilution and CD8β dependence assays (Fig. S2). In addition, there was no evidence of pMHC–TCR avidity maturation from the primary to the secondary response.
DbNPM6A Selects a Distinct and Less Diverse TCRVβ Repertoire.
To show that the novel DbNPM6A epitope selects an array of TCRs different to the native DbNP336, we defined the DbNPM6A+CD8+ repertoire at the clonal level. First, the DbNPM6A+CD8+ T cell sets were analyzed for Vβ usage. The strong Vβ8.3 bias characteristic of DbNP366+CD8+ T cells was not apparent for the DbNPM6A+CD8+ sets (Fig. S3), which use a broader and less consistent spectrum of TCRVβ elements. Unlike DbNP366+CD8+ T cells, DbNPM6A did not select consistent TCRVβ profiles. The responses were individualized, with an average (per mouse) of 2.8 (10) and 2.2 (20) prominent TCRVβ elements after HK-NPM6A infection (Tables S1). and S2). Clonal analysis of 996 sequences from specific Vβ segments showed that, although the DbNPM6A+CD8+ T cells used multiple Vβ regions, the extent of TCR repertoire selection within an individual TCRVβ+ set was quite restricted (Table S1 and S2). An average of 3.3 and 2.4 clonotypes were identified for each DbNPM6A+CD8+ TCRVβ after 10 or 20 challenge (Table S2), which is lower than the average of 7.9 clonotypes characteristic of the DbNP366+Vβ8.3+CD8+ T cell responses (10, 11). Because Vβ8.3 constitutes 30–50% of the WT DbNP366+CD8+ response and other subdominant Vβs (6) are also prominent, clonal diversity of DbNPM6A+CD8+ T cells with ≈2 prominent TCRVβs and an average of ≈3 clonotypes per Vβ is lower that the WT DbNP366+CD8+ response. Analysis of the average number of clonotypes per mouse showed that, taking into account all Vβs analyzed, DbNPM6A elicited an average of 9.0 (10) and 5.0 (20) clonotypes per mouse. Relatively few clonotypes were found repeatedly in >1 mouse. Thus, this response (unlike DbNP366) is not public in character. Interestingly, although TCR diversity per 1 individual mouse was ≈2 lower for NPM6A+CD8+ T cells, the overall TCR diversity within the population (all of the mice tested) was, because of the public nature of DbNP366+CD8+ repertoire, greater for NPM6A+CD8+ T cells than for the DbNP366+CD8+ sets.
Crystal Structure of the DbNPM6A Complex.
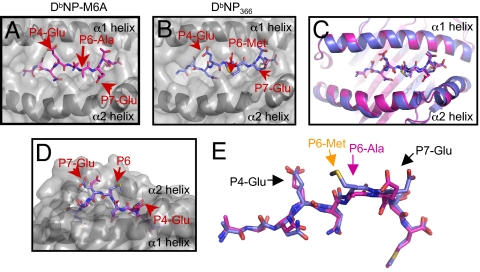
To gain a greater understanding of the impact of the M6A mutation, we determined the crystal structure of H2Db-NPM6A to 2.5-Å resolution (Fig. 4A and Table S3), refined to a final Rfactor and Rfree of 22.0% and 28.5%, respectively. The electron density corresponding to the NPM6A peptide was unambiguous, as were the residues within the Ag-binding cleft. As for DbNP366 (15), the NPM6A peptide adopted an extended conformation (Fig. 4 A and B) within the H2Db Ag-binding cleft. p3-Asn, p5-Asn, and p9-Met represent the anchor residues, and p4-Glu, p6-Ala, p7-Glu, and p8-Thr are solvent-exposed and available for contact by the TCR. The contacts between the WT NP366 and mutant NPM6A peptides with H2-Db are similar, consistent with the epitopes being presented equally. In the WT DbNP366, p6-Met interacts extensively with the side chain of His-155 of H-2Db. However, in the DbNPM6A complex, the shorter side chain of Ala results in a loss of contact between p6 of the peptide and H2Db, resulting in notable alterations in the substructure of the pMHC around this position. The M6A substitution generated a flatter topology with respect to DbNP366 (Fig. 4A). Although the structures of the NP366 and NPM6A Ag-binding clefts were in general very similar (rmsd = 0.80 Å), more notable structural changes were located in a region of the α2 helix between residues 148–152, with a 1.2-Å shift in the Cα position of 151. Such shifts in the helical backbone of the Ag-binding cleft have been shown to impact profoundly on TCR recognition (16, 17). Also, although the overall conformation of the DbNP366 and DbNPM6A epitopes are similar, the p6 position differs substantially (rmsd of 1.1 Å), with the p6A moving toward the α2 helix compared with the p6M (Fig. 4C). On account of the “cavity” created by the M6A substitution, the p7-Glu side chain reorientates toward and contacts Ala-152, whereas in the DbNP366 epitope, the p7-Glu is orientated toward Lys-146. Thus, the observed changes in DbNPM6A topology and structure are consistent with the lack of DbNP366+CTL cross-reactivity.
Fig. 4.
Crystal structure of the M6A peptide bound to H-2Db. (A and B) The crystal structure of DbNPM6A (A), solved to 2.5 Å, compared with DbNP366 structure (B). The structures are positioned with the peptide C terminus on the right, the α2 helix at the front, and the α1 helix at the back. The most-exposed amino acids side chains predicted to be critical for specific TCR recognition are indicated by red arrows. (C) Ribbon representation of the superposition of the structure of DbNP-M6A (pink) and DbNP366 (blue) viewed from the perspective of a TCR. (D) The structure are positioned with the peptide C terminus on the left and the α2 helix at the back. (E) Superposition of the NP-M6A peptide (pink) and the NP366 peptide (blue) positioned with the C terminus on the right.
Discussion
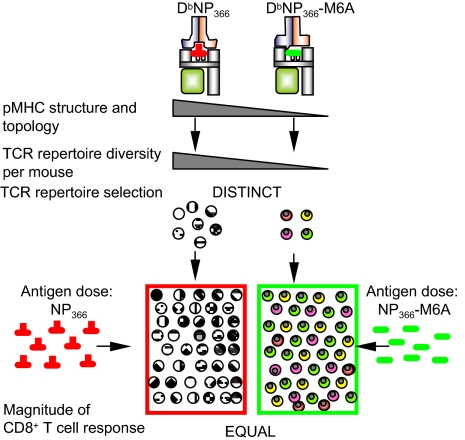
Understanding the nature of antigenicity and CD8+ T cell immunodominance hierarchies should help us to develop better vaccines and immunotherapy protocols. Immunodominance has been variously attributed to TCR (repertoire, avidity, and precursor frequency) and epitope dose (including antigen processing and presentation) effects (2, 7), although there is no precise understanding of how the various elements function together to determine response magnitude. We dissected the role of TCR repertoire in immunodominance by using a mutant virus engineered by reverse genetics. Our conclusions are that changing the character of the TCR response does not modify a well-defined and dramatic CD8+ T cell immunodominance hierarchy. We showed that a mutated viral peptide selects epitope-specific CD8+ T cells that differ in specificity, the character and diversity of their TCR repertoire, and the level of TCR/pMHCI avidity, but otherwise retains the response magnitude and immunodominance profile characteristics of the native epitope (Fig. 5). These findings provide unique insights into both virus-specific CD8+ T cell recognition and the selection of immunodominant T cell responses. The fact that p6A-for-M substitution in the influenza virus NP366 peptide fundamentally alters the interface that the H2Db MHCI glycoprotein presents to the TCR is emphasized by the finding that recognition by DbNPM6A T cells is disrupted by an additional change at p4. Looking at the structure of the DbNPM6A complex we see that it indeed differs from DbNP366 in that there are significant conformational changes at p7E and a region of the MHC α2 helix. Together with loss of the p6M side chain, DbNPM6A exhibits a pMHC topology that is even more “flat and featureless” than the original WT DbNP366 complex. Clearly, though, the M6A change has in no way compromised peptide binding to the groove of the MHCI molecule.
Fig. 5.
Complete modification of TCR specificity and repertoire selection does not affect the CD8+ T cell immunodominance hierarchy. A single amino acid substitution within the viral NP protein at the critical residue p6M was engineered. In the DbNPM6A complex, the shorter side chain of A results in a loss of contact between p6 of NPM6A and H2Db, resulting in a flatter topology than that seen for DbNP366. These changes are consistent with lack of DbNP366+CD8+ cross-reactivity and lower TCR diversity. Despite the complete modification of TCR specificity and selection, the magnitude (and immunodominance hierarchies) for WT DbNP366 and mutant NPM6A+CD8+ responses are equal. Thus, the primary determinant of immunodominance is antigen dose rather than TCR repertoire composition.
The TCR repertoire specific for this novel DbNPM6A epitope is more diverse overall for the spectrum of selected TCR Vβs, while lacking the public TCRS (using fewer CDR3βs within each Vβ) than the predominant Vβ8.3+DbNP366CD8+ set (11). Thus, the TCR repertoire for DbNPM6A per individual mouse (but not within the population) is a little more limited in range than that found for the WT DbNP336 response, although the differential is at most 2-fold and the results conform with the earlier conclusion that flat and featureless pMHC–TCR interfaces (p6A is less prominent than p6M) tend to recruit a restricted TCR repertoire (10), although excessively “bulged” epitopes can be also associated with very limited TCR usage (17, 18). This further indicates that the public versus private character of a selected TCR repertoire is irrelevant when it comes to response magnitude and immunodominance hierarchies but is important for TCR diversity within the population. There must presumably be a sufficient number of “naïve” TCRs to select into a response, but whether these are more individualized or shared between mice may be of no consequence. Thus, although the topology of the pMHCI determines the diversity of the TCR repertoire, the public or private character of that repertoire is determined by the availability of naïve clonotypes in all of the animals.
Analysis of virus growth characteristics indicated that the NPM6A substitution did not diminish viral fitness, and thus the amount of NP produced during the infectious process. The influenza virus NP is a key and abundant structural protein (7). Given that DbNPM6A generates a response that is of equivalent magnitude to that long recognized for DbNP366 it seems reasonable to argue that the M6A change had no effect on the antigen-processing pathway. Thus, we are left with the conclusion that, if the protein/peptide load is equivalent for 2 different pMHCI epitopes, then the relationship will be maintained for the response magnitude and the resultant, numerical immunodominance hierarchy. The diminished TCR/pMHCI avidity profile associated with the NPM6A change indicates either that TCR avidity has no effect on response magnitude or, alternatively, that both interactions exceed a necessary threshold. The higher (with respect to DbNP366) TCR/pMHCI avidity associated with recognition of DbPA224 is also correlated with a different “functional avidity” profile (more TNF-α and IL-2 expression). Although TCR avidities varied for DbNP366 and DbNPM6A, the strength of the TCR/pMHCI interaction was evidently sufficient in both cases to promote an effective cytokine and CTL response. The relative efficacies might have changed if, for example, the mutant had shown the “higher” TCR/pMHCI avidity profile associated with DbPA224.
The present results also emphasize that useful insights into the nature of relative epitope quality, or “fitness”, are unlikely to emerge from experiments that use only TCR-transgenic mice. Under those conditions there is, of course, no alternative TCR repertoire available for selection. We might also ask, though, whether a new TCR repertoire to a spontaneously arising mutant virus can emerge effectively during the course of infection with a persistent virus like HIV (13). If a preexisting, primed TCR memory pool to common mutations generated by the virus was to be elicited by preemptive vaccination, would this act to promote the control of persistent viruses or work against the emergence of tumor variants?
In conclusion, these experiments with the NPM6A mutation highlight that achieving an effective antigen dose is likely to be important for CD8+ T cell vaccination and/or immunotherapy protocols. What is more intriguing, though, is that the results presented here suggest that immunization with at least some of these mutants will establish effective CD8+ T cell memory. It may thus be possible to prime against the emergence of commonly selected mutants and thus diminish the possibility of virus (or tumor) escape.
Methods
Mice and Viral Infection.
C57BL/6J mice at 6 weeks of age were lightly anesthetized by methoxyfluorane inhalation and infected i.n. with 104 plaque-forming units (pfu) of the HKx31 (H3N2; HK) influenza A viruses in 30 μL of PBS. Memory mice were primed i.p. with 1.5 × 107 pfu of the serologically distinct PR8 (H1N1) influenza A viruses that share the internal NP and PA proteins of HK. Mice were challenged i.n. with the HK viruses 6 weeks later to generate a secondary response.
Generation and Titration of Recombinant Viruses.
Recombinant viruses were produced by an 8-plasmid reverse genetics system. A single amino acid mutation (M6A) was introduced into the NP366 peptide, ASNENMETM, by PCR (primers available on request). PCR products were digested with BsmB1 and ligated into pHW2000 vector. The recombinant HK and PR8 viruses (HK-NPM6A and PR-NPM6A) were rescued after transfection of 8 plasmids encoding influenza segments into 293T and MDCK cells. Viruses were grown in embryonated eggs, and viral titers were determined by plaque assay.
Tissue Sampling and Cell Preparation.
Spleen and BAL were recovered from mice at acute phases of 10 (day 10) and 20 (day 8) infections. Spleens were enriched for CD8+ T cells by using anti-mouse IgG and IgM antibodies (Jackson ImmunoResearch Laboratories). Lungs were sampled on days 3, 6, 7, 8, or 9 after infection and homogenized, and the virus-containing supernatant was harvested. Infectious virus in lung supernatants was determined by plaque assay on MDCK cells.
Tetramer Staining and Tetramer Dissociation Analysis.
CD8+ T cells were stained with the DbNP366, DbPA224, or Db-NPM6A tetramers conjugated to Streptavidin-phycoerythrin (PE) (Molecular Probes) for 60 min at room temperature. Cells were washed twice in FACS buffer (10% BSA/0.02% NaAz in PBS), stained with a FITC-conjugated mAb to CD8α (BD Biosciences Pharmingen) for 30 min on ice, washed, and analyzed by flow cytometry. As a measure of TCR avidity, splenic T cells were used in tetramer dissociation assay (4). After staining with tetramer, T cells were washed and incubated with anti-H2Db antibody at 5 μg/mL to prevent tetramer rebinding. Cells were always stained and washed in the presence of NaAz to prevent tetramer internalization. Loss of tetramer+CD8+ T cells at particular time points was calculated compared with tetramer staining at t = 0 min.
ICS.
Cells were stimulated with NP366, PA224, PB1703, or an array of NP-mutant peptides for 5 h in 200 μL of cRPMI medium containing 1 μg/ml Golgi-Plug (BD Biosciences Pharmingen), washed in FACS buffer, and stained with a PerCP-Cy5.5 conjugated mAb to CD8. Cells were fixed, permeabilized with a BD Cytofix/Cytoperm kit, stained with mAbs to IFN-γ (FITC), TNF-α [allophycocyanin (APC)], and IL-2 (PE) (BD Biosciences Pharmingen) for 30 min, washed, and analyzed by flow cytometry.
Ex Vivo 51Cr Release Assay.
Effector T cells were prepared from spleens of mice infected with HK or HK-NPM6A viruses. Cells were diluted across a range of effector-to-target ratios. EL-4 targets were pulsed with 1 μM of NP366 or NPM6A peptides and 750 μCi 51Cr (Amersham Biosciences) for 1 h at 37 °C, washed, and adjusted to 105 cells per ml. One-hundred microliters was dispensed into plates, and effectors and targets were incubated for 4 h at 37 °C. Supernatants were transferred to Lumina plates (Packard Instruments). Gamma irradiation was measured, and percentage of specific lysis was calculated.
Hybridoma LacZ Assay.
LacZ-inducible T cell hybridomas specific for NP366 peptide (9) were dispensed into 96-well plates together with 5 × 105 naïve splenocytes. Cells were cultured in the presence of NP366 or NP mutant peptides at 10−6 M for 18 h at 37 °C. Cells were washed, fixed, and incubated with X-Gal for 16 h at 37 °C. LacZ+ hybridomas were counted.
TCR Repertoire Analysis.
CD8+ T cell populations were stained with the DbNPM6A tetramer, then anti-CD8-FITC. Cells were isolated by using a MoFlo sorter (Cytomation). DbNPM6A+CD8+ T cells were sorted, and RNA was prepared by using TRIzol (Invitrogen). cDNA was reverse-transcribed with an Omniscript RT kit (Qiagen). PCR products were cloned into pCR2.1-TOPO (Invitrogen). Colonies containing inserts were sequenced on an Applied Biosystems Prism 3700 sequence analyzer.
Protein Expression, Purification, Crystallization, and Structure Determination.
H2-Db and β2-microglobulin molecules were expressed in Escherichia coli as inclusion bodies, refolded with the NP-M6A peptide, and purified (19, 20). DbNPM6A complex crystals were obtained at 7.4 mg/mL by the hanging-drop vapor diffusion technique at 20 °C. Crystals were grown with a reservoir containing 0.1 M potassium thiocianate, 30% PEG 2000 (wt/vol). The crystals belong to space group P1, and the unit cell dimensions were consistent with 2 molecules per asymmetric units (Table S3). The crystals were flash-frozen to a temperature of 100 K before data collection in-house on a R-Axis IV++ detector. Data were processed and scaled with the XDS (21). The crystal structure was solved using the molecular replacement method. The search probe used to solve the structure was the structure of mouse MHC class I H2-Db minus the peptide (Protein Data Bank ID code 1YN7) (10). The progress of refinement was monitored by the Rfree value with neither a sigma nor a low-resolution cutoff being applied to the data. The refinement protocol used includes several cycles of refinement with REFMAC followed by manual model rebuilding with the O program (22). Refinement statistics are in Table S3.
Supplementary Material
Acknowledgments.
We thank Drs. N. La Gruta and J. Stambas for review of the manuscript, Ken Field for sorting, and Dina Stockwell for technical assistance. This work was funded by National Health and Medical Research Council Project Grants AI454595 (to P.C.D.), Al508929 (to A.W.P. and S.J.T.) and AI454312 (to K.K.), a University of Melbourne Early Career Researcher Grant (to K.K.), and National Institutes of Health Grant AI170251. K.K. is a National Health and Medical Research Council R.D. Wright Fellow. S.J.T. is a Pfizer Senior Research Fellow. C.G. is a Marie Curie International Fellow (040840). J.R. is an Australian Research Council Federation Fellow. A.W.P. is a National Health and Medical Research Council Senior Research Fellow.
Footnotes
The authors declare no conflict of interest.
Data deposition: The atomic coordinates have been deposited in the Protein Data Bank, www.pdb.org (PDB ID code 3CPL).
This article contains supporting information online at www.pnas.org/cgi/content/full/0810274105/DCSupplemental.
References
- 1.Doherty PC, Turner SJ, Webby RG, Thomas PG. Influenza and the challenge for immunology. Nat Immunol. 2006;7:449–455. doi: 10.1038/ni1343. [DOI] [PubMed] [Google Scholar]
- 2.Irvine K, Bennink J. Factors influencing immunodominance hierarchies in TCD8+-mediated antiviral responses. Exp Rev Clin Immunol. 2006;2:135–147. doi: 10.1586/1744666X.2.1.135. [DOI] [PubMed] [Google Scholar]
- 3.Zhong W, Reche PA, Lai CC, Reinhold B, Reinherz EL. Genomewide characterization of a viral cytotoxic T lymphocyte epitope repertoire. J Biol Chem. 2003;278:45135–45144. doi: 10.1074/jbc.M307417200. [DOI] [PubMed] [Google Scholar]
- 4.La Gruta NL, Turner SJ, Doherty PC. Hierarchies in cytokine expression profiles for acute and resolving influenza virus-specific CD8+ T cell responses: Correlation of cytokine profile and TCR avidity. J Immunol. 2004;172:5553–5560. doi: 10.4049/jimmunol.172.9.5553. [DOI] [PubMed] [Google Scholar]
- 5.Kedzierska K, et al. Early establishment of diverse TCR profiles for influenza-specific CD62Lhi CD8+ memory T cells. Proc Natl Acad Sci USA. 2006;103:9184–9189. doi: 10.1073/pnas.0603289103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kedzierska K, et al. Quantification of repertoire diversity of influenza-specific epitopes with predominant public or private TCR usage. J Immunol. 2006;177:6705–6712. doi: 10.4049/jimmunol.177.10.6705. [DOI] [PubMed] [Google Scholar]
- 7.La Gruta NL, et al. A virus-specific CD8+ T cell immunodominance hierarchy determined by antigen dose and percursor frequencies. Proc Natl Acad Sci USA. 2006;103:994–999. doi: 10.1073/pnas.0510429103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flynn KJ, et al. Virus-specific CD8+ T cells in primary and secondary influenza pneumonia. Immunity. 1998;8:683–691. doi: 10.1016/s1074-7613(00)80573-7. [DOI] [PubMed] [Google Scholar]
- 9.Crowe SR, et al. Differential antigen presentation regulates the changing patterns of CD8+ T cell immunodominance in primary and secondary influenza virus infections. J Exp Med. 2003;198:399–410. doi: 10.1084/jem.20022151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Turner SJ, et al. Lack of prominent peptide-major histocompatibility complex features limits repertoire diversity in virus-specific CD8+ T cell populations. Nat Immunol. 2005;6:382–389. doi: 10.1038/ni1175. [DOI] [PubMed] [Google Scholar]
- 11.Kedzierska K, Turner SJ, Doherty PC. Conserved T cell receptor usage in primary and recall responses to an immunodominant influenza virus nucleoprotein epitope. Proc Natl Acad Sci USA. 2004;101:4942–4947. doi: 10.1073/pnas.0401279101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Price GE, Ou R, Jiang H, Huang L, Moskophidis D. Viral escape by selection of cytotoxic T cell-resistant variants in influenza A virus pneumonia. J Exp Med. 2000;191:1853–1867. doi: 10.1084/jem.191.11.1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Price DA, et al. T cell receptor recognition motifs govern immune escape patterns in acute SIV infection. Immunity. 2004;21:793–803. doi: 10.1016/j.immuni.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 14.Sigal LJ, Wylie DE. Role of nonanchor residues of Db-restricted peptides in class I binding and TCR triggering. Mol Immunol. 1996;33:1323–1333. doi: 10.1016/s0161-5890(96)00099-5. [DOI] [PubMed] [Google Scholar]
- 15.Young AC, Zhang W, Sacchettini JC, Nathenson SG. The three-dimensional structure of H-2Db at 2.4-Å resolution: Implications for antigen-determinant selection. Cell. 1994;76:39–50. doi: 10.1016/0092-8674(94)90171-6. [DOI] [PubMed] [Google Scholar]
- 16.Macdonald WA, et al. A naturally selected dimorphism within the HLA-B44 supertype alters class I structure, peptide repertoire, and T cell recognition. J Exp Med. 2003;198:679–691. doi: 10.1084/jem.20030066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tynan FE, et al. High-resolution structures of highly bulged viral epitopes bound to major histocompatibility complex class. I. Implications for T cell receptor engagement and T cell immunodominance. Nat Immunol. 2005;6:1114–1122. doi: 10.1074/jbc.M503060200. [DOI] [PubMed] [Google Scholar]
- 18.Gras S, Kjer-Nielsen L, Burrows SR, McCluskey J, Rossjohn J. T cell receptor bias and immunity. Curr Opin Immunol. 2008;20:119–125. doi: 10.1016/j.coi.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 19.Clements CS, et al. The production, purification, and crystallization of a soluble heterodimeric form of a highly selected T cell receptor in its unliganded and liganded state. Acta Crystallogr D. 2002;58:2131–2134. doi: 10.1107/s0907444902015482. [DOI] [PubMed] [Google Scholar]
- 20.Macdonald W, et al. Identification of a dominant self-ligand bound to three HLA B44 alleles and the preliminary crystallographic analysis of recombinant forms of each complex. FEBS Lett. 2002;527:27–32. doi: 10.1016/s0014-5793(02)03149-6. [DOI] [PubMed] [Google Scholar]
- 21.Kabsch W. Automatic processing of rotation diffraction data from crystals of initially unknown symmetry and cell constants. J Appl Crystallogr. 1993;26:795–800. [Google Scholar]
- 22.Jones T, Zou J, Cowan S, Kjeldgaard M. Improved methods for building protein models in electron density maps and the location of errors in these models. Acta Crystallogr A. 1991;1991:110–119. doi: 10.1107/s0108767390010224. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.