Abstract
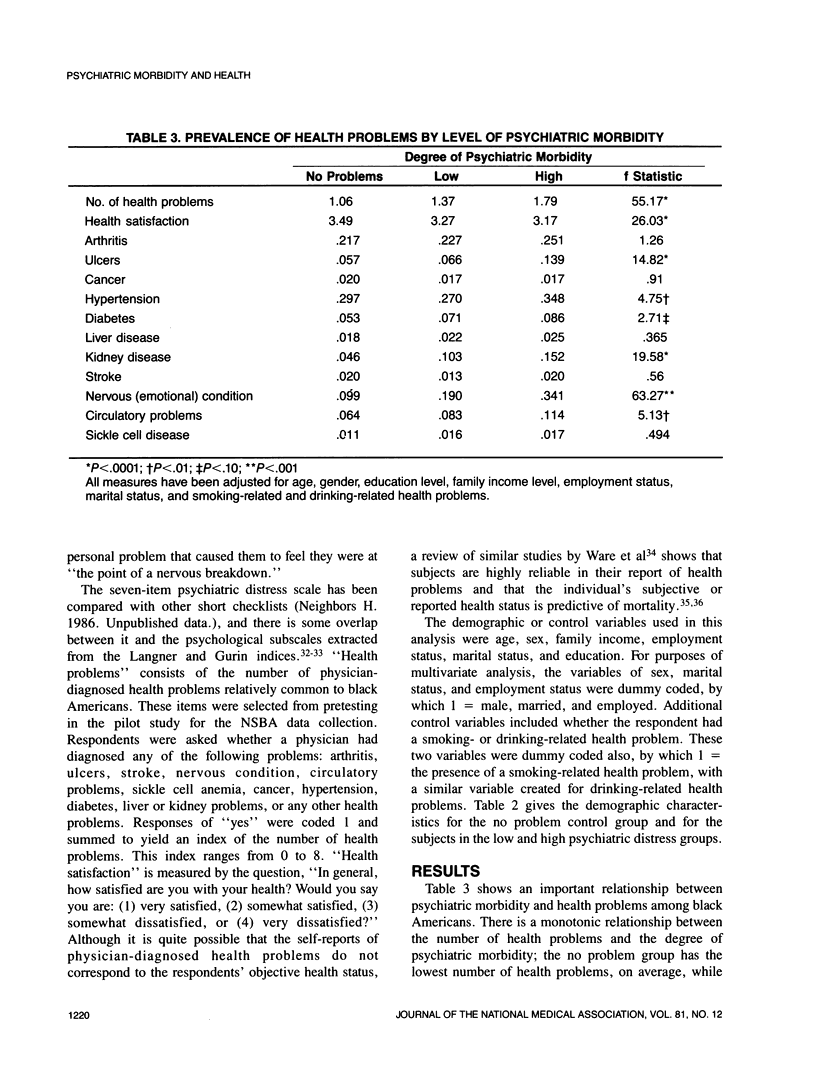
This study examined the relationship between symptoms of psychiatric morbidity and health problems among a nationally representative, cross-sectional sample of 2107 black adults from the National Survey of Black Americans. Subjects experiencing a high level of psychiatric symptomatology had a significantly higher number of health problems and reported a lower level of satisfaction with their overall health than blacks with low levels of psychiatric symptoms or those who never experienced emotional problems. Individuals with the highest level of psychiatric symptomatology were more likely to have been physician-diagnosed as having ulcers, hypertension, diabetes, kidney problems, nervous-emotional problems, and circulatory system difficulties. These relationships persisted after controlling for age, gender, socioeconomic factors, and traditional risk factors for health problems, such as smoking and alcohol use. Although generally consistent with previous research on predominantly white samples, these specific findings underscore the complexities involved in drawing inferences from associations between psychiatric symptomatology and health problems observed in cross-sectional surveys. Prospective psychiatric epidemiologic studies, utilizing better measures of psychological distress and objective health outcome measures, are needed to clarify the relationship between psychiatric difficulties and health problems among black Americans.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andrews G., Tennant C., Hewson D. M., Vaillant G. E. Life event stress, social support, coping style, and risk of psychological impairment. J Nerv Ment Dis. 1978 May;166(5):307–316. doi: 10.1097/00005053-197805000-00001. [DOI] [PubMed] [Google Scholar]
- Brand R. J., Rosenman R. H., Sholtz R. I., Friedman M. Multivariate prediction of coronary heart disease in the Western Collaborative Group Study compared to the findings of the Framingham study. Circulation. 1976 Feb;53(2):348–355. doi: 10.1161/01.cir.53.2.348. [DOI] [PubMed] [Google Scholar]
- Cochrane R. Hostility and neuroticism among unselected essential hypertensives. J Psychosom Res. 1973 Jul;17(3):215–218. doi: 10.1016/0022-3999(73)90026-3. [DOI] [PubMed] [Google Scholar]
- Diamond E. L. The role of anger and hostility in essential hypertension and coronary heart disease. Psychol Bull. 1982 Sep;92(2):410–433. [PubMed] [Google Scholar]
- Eaton W. W., Kessler L. G. Rates of symptoms of depression in a national sample. Am J Epidemiol. 1981 Oct;114(4):528–538. doi: 10.1093/oxfordjournals.aje.a113218. [DOI] [PubMed] [Google Scholar]
- Engel G. L. The concept of psychosomatic disorder. J Psychosom Res. 1967 Jun;11(1):3–9. doi: 10.1016/0022-3999(67)90051-7. [DOI] [PubMed] [Google Scholar]
- Greenberg R. P., Dattore P. J. Do alexithymic traits predict illness? J Nerv Ment Dis. 1983 May;171(5):276–279. doi: 10.1097/00005053-198305000-00003. [DOI] [PubMed] [Google Scholar]
- Haynes S. G., Feinleib M., Levine S., Scotch N., Kannel W. B. The relationship of psychosocial factors to coronary heart disease in the Framingham study. II. Prevalence of coronary heart disease. Am J Epidemiol. 1978 May;107(5):384–402. doi: 10.1093/oxfordjournals.aje.a112557. [DOI] [PubMed] [Google Scholar]
- Haynes S. G., Levine S., Scotch N., Feinleib M., Kannel W. B. The relationship of psychosocial factors to coronary heart disease in the Framingham study. I. Methods and risk factors. Am J Epidemiol. 1978 May;107(5):362–383. doi: 10.1093/oxfordjournals.aje.a112556. [DOI] [PubMed] [Google Scholar]
- Johnson E. H., Broman C. L. The relationship of anger expression to health problems among black Americans in a national survey. J Behav Med. 1987 Apr;10(2):103–116. doi: 10.1007/BF00846419. [DOI] [PubMed] [Google Scholar]
- Kathol R. G., Petty F. Relationship of depression to medical illness. A critical review. J Affect Disord. 1981 Jun;3(2):111–121. doi: 10.1016/0165-0327(81)90036-7. [DOI] [PubMed] [Google Scholar]
- Lolas F., Heerlein A. Content category analysis of affective expression in irritable bowel, duodenal ulcer and anxiety disorder patients. Psychopathology. 1986;19(6):309–316. doi: 10.1159/000284454. [DOI] [PubMed] [Google Scholar]
- Lyketsos G., Arapakis G., Psaras M., Photiou I., Blackburn I. M. Psychological characteristics of hypertensive and ulcer patients. J Psychosom Res. 1982;26(2):255–262. doi: 10.1016/0022-3999(82)90044-7. [DOI] [PubMed] [Google Scholar]
- MIRSKY I. A., REISER M. F., THALER M., WEINER H. Etiology of duodenal ulcer. I. Relation of specific psychological characteristics to rate of gastric secretion (serum pepsinogen). Psychosom Med. 1957 Jan-Feb;19(1):1–10. doi: 10.1097/00006842-195701000-00001. [DOI] [PubMed] [Google Scholar]
- Magni G., Di Mario F., Trinciarelli G., Conlon P., Donzella G. Personality pattern of patients with chronic gastric ulcer: a case control study. Psychother Psychosom. 1986;46(3):152–156. doi: 10.1159/000287977. [DOI] [PubMed] [Google Scholar]
- Mossey J. M., Shapiro E. Self-rated health: a predictor of mortality among the elderly. Am J Public Health. 1982 Aug;72(8):800–808. doi: 10.2105/ajph.72.8.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors H. W. Socioeconomic status and psychologic distress in adult blacks. Am J Epidemiol. 1986 Nov;124(5):779–793. doi: 10.1093/oxfordjournals.aje.a114454. [DOI] [PubMed] [Google Scholar]
- SCHMALE A. H., Jr Relationship of separation and depression to disease. I. A report on a hospitalized medical population. Psychosom Med. 1958 Jul-Aug;20(4):259–277. doi: 10.1097/00006842-195807000-00001. [DOI] [PubMed] [Google Scholar]
- Salber E. J., Beza A. G. The health interview survey and minority health. Med Care. 1980 Mar;18(3):319–326. doi: 10.1097/00005650-198003000-00006. [DOI] [PubMed] [Google Scholar]
- Tennant C. Psychosocial causes of duodenal ulcer. Aust N Z J Psychiatry. 1988 Jun;22(2):195–201. doi: 10.3109/00048678809158960. [DOI] [PubMed] [Google Scholar]


