Abstract
The ability to protect mice against respiratory infections with virulent Francisella tularensis has been problematic and the role of antibody-versus-cell-mediated immunity controversial. In this study, we tested the hypothesis that protective immunity can develop in mice that were given antibiotic therapy following infection via the respiratory tract with Francisella tularensis SCHU S4. We show that mice infected with a lethal dose of SCHU S4, via an intra-nasal challenge, could be protected with levofloxacin treatment. This protection was evident even when levofloxacin treatment was delayed 72 hours post-infection. At early time points after levofloxacin treatment, significant numbers of bacteria could be recovered from the lungs and spleens of mice, which was followed by a dramatic disappearance of bacteria from these tissues. Mice successfully treated with levofloxacin were later shown to be almost completely resistant to rechallenge with SCHU S4 by the intra-nasal route. Serum antibody appeared to play an important role in this immunity. Normal mice, when given sera from animals protected by levofloxacin treatment, were solidly protected from a lethal intra-nasal challenge with SCHU S4. The protective antiserum contained high titers of SCHU S4 specific IgG2a, indicating that a strong Th1 response was induced following levofloxacin treatment. Thus, this study describes a potentially valuable animal model for furthering our understanding of respiratory tularemia and provides suggestive evidence that antibody can protect against respiratory infections with virulent F. tularensis.
Introduction
Francisella tularensis is a small, gram-negative, bacterium that is the causative agent of tularemia, a zoonotic disease. It is an aerobic, non-spore-forming coccobacillus, that infects the host as a facultative intracellular pathogen. It has been considered one of the most infectious pathogens known, since very few bacteria can result in infection leading to significant pathology, disease, and death (1). Since it can be aerosolized, is extremely infectious, and is surprisingly stable in different environments for long periods of time, F. tularensis is considered a Category A bioweapon (2–5).
Human pathogenic F. tularensis has been divided into two major subspecies. F. tularensis subspecies tularensis or Type A is highly virulent to humans and animals and is the most common biotype isolated in North America. In contrast, Francisella tularensis subsp. holarctica (Type B) is less virulent to humans and common in Europe and Asia but also found in North America (4,6,7). A relatively well characterized strain of the subspecies holarctica was shown to be immunogenic and protective when injected into animals and was denoted F. tularensis live vaccine strain (LVS). This strain has been used in humans, but because its attenuation is uncharacterized, it is not licensed. However, mice challenged with LVS have served as a valuable model for examining the immune response to this bacterium (8,9). The bacteria have a thin capsule that appears unique from those of other gram-negative bacteria (10,11). Additionally, lipopolysaccharide (LPS) from this bacterium seems to differ significantly from that of other gram-negative bacteria (12–14). No protein toxins have been found to be associated with this bacterium (15,16) and only recently has progress been made in understanding some of the virulence factors that may be important for the high infectivity and pathogenesis (17–20).
There is now significant evidence that the best protective immune responses against respiratory bacterial infections are induced via intra-nasal or inhalation vaccination (21–24). Thus, understanding the lung immune response and developing a vaccine that would protect against this route of infection would be crucially important, given that any biological weapon using Francisella would use this mechanism for dispersal. In fact, it is now well established that many different mouse strains can be immunized by systemic administration of LVS against subsequent intradermal challenge with virulent Francisella, but these mice do not survive exposure to low doses of aerosols of virulent Francisella (25). Although much knowledge has been gained about the role of different immune functions with regard to systemic LVS infections, it has been only recently that new insights have been gained into how LVS and virulent Francisella interact with different host immune functions following intra-nasal or inhalation infection (26–29). However, the role of antibody-versus-cell-mediated immunity in establishing protective immunity to inhalation infection with virulent Francisella is still not completely understood. Conlan et al. (30) have shown that mice immunized via aerosol exposure to LVS had enhanced protection against virulent type A Francisella, which was T cell-dependent. Lyons and co-workers (31) have also shown that intra-nasal vaccination with LVS could protect Balb/c mice, but not C57BL/6 mice, against intra-nasal or subcutaneous challenges with virulent Francisella. In this study, protection was dependent upon T cells. A recent study by Kirimanjeswara et al (32) has shown that antiserum generated in Balb/c mice by intraperitoneal immunization with LVS was protective, via passive transfer to normal mice, against a lethal respiratory infection with LVS. Interestingly, this protection was dependent upon T cells and cell-mediated immunity.
In this study, we have shown that mice infected via intra-nasal challenge with virulent F. tularensis SCHU S4 and then treated with levofloxacin developed protective immunity against subsequent intra-nasal challenge with SCHU S4. Interestingly, sera from mice challenged with SCHU S4 that had been treated with levofloxacin was shown to be protective when passively transferred to normal, naive, mice. The most abundant class of immunoglobulin in this protective serum was IgG2a, suggesting that a Th1 type of immune response was dominant. We believe that this mouse model could be helpful in identifying F. tularensis antigens that elicit the formation of protective antibodies. The model might also yield valuable insight into a number of questions still unanswered with regard to protective immunity against inhalation infection with virulent Francisella.
Materials and Methods
Mice and bacteria
BALB/c female mice, 5–6 weeks old, were purchased from The Jackson Laboratory. F. tularensis SCHU S4 was obtained from U.S. Army DPG, Life Sciences Division, Dugway, UT. IsoVitaleX was purchased from Becton Dickinson (Cockeysville, MD). Brain heart infusion (BHI) medium was purchased from Difco Laboratories (Detroit, MI). Bacteria were stored frozen at −85°C, until used in experiments. Bacteria from frozen stock were grown in modified Muller Hinton broth (MHB; Difco Laboratories) enriched with IsoVitaleX. The bacteria were grown for 15–18 h, at which times, bacteria consistently reached 2 × 109 – 3 × 109 colony forming units per ml (CFU/ml). We used bacteria from cultures at this growth phase in each experiment below and the actual concentration of bacteria was verified by a Petroff-Hausser counting chamber and viable plate counts after growing aliquots on BHI plates. All animal procedures were approved by the UTMB institutional animal care and use committee.
Intra-nasal infection of mice and passive transfer of serum
Mice were anesthetized with ketamine-HCl (35 mg/kg) and xylazine-HCl (5 mg/kg) by intraperitoneal injection (i.p.) and were then suspended vertically by the upper incisors using commercial fishing line looped behind the upper incisors and connected to a support platform. Ten microliters of phosphate-buffered saline (PBS) containing approximately 99 CFU of SCHU S4 (3 LD50 doses) were then placed at the anterior of each naris, and the mice then allowed to inhale the bacteria (33). The number of SCHU S4 given to mice in different experiments did sometimes differ and the actual dose is noted in the figure legends. Following intra-nasal administration, the mice were given 10 μl of sterile PBS per naris to ensure that the bacteria were washed into the lungs. Mice were then returned to their cages, and then at varying times, given either levofloxacin (i.p.) or PBS. In some experiments, mice were given sera from either immune or control mice. For these experiments, pooled sera were obtained and 250 μl transferred to mice via the i.p. route.
Analysis of bacterial load in different tissues of infected mice
Mice were sacrificed at varying times post intra-nasal infection and spleen and lungs obtained aseptically. Spleen and lungs from individual mice were homogenized in 1 ml of PBS, and various dilutions plated on BHI agar plates.
ELISA for detecting different classes of Immunoglobulins
F. tularensis SCHU S4 cultures were resuspended, at concentration of 5×108 CFU/ml, in PBS, 0.5% glutaraldehyde and incubated for 1 hour at room temperature. High-binding 96-well plates (Evergreen Scientific) were coated with 50 μl of 10 μg/ml poly-l-lysine (Sigma) in PBS for 30 minutes at room temperature. After removing the poly-l-lysine, 50 μl of bacteria were added per well. Plates were sealed and centrifuged at 250 x g for 5 minutes. Plates were washed once by immersion in PBS then, 200 μl per well of 0.1M Glycine, 0.1% BSA in water was added for 30 minutes at room temperature. Plates were washed twice in PBS and then 50 μl of 0.1% BSA in PBS was added to the wells and the plates were frozen at −20°C until use.
For assays, plates were blocked with 200 μl PBS, 10% fetal calf serum (FCS) for 1 hour. Two-fold dilutions of sera were incubated in the plates for 2 hours at room temperature. This was followed by washing in PBS, 0.05% Tween 20 (PBST), and the addition of 0.5 g/ml biotinylated primary goat anti-mouse IgG, IgM, IgG1, IgG2a, IgG2b, or IgG3 (Caltag Laboratories) for 1 hour at room temperature. Plates were washed with PBST, and 50 μl of Avidin peroxidase (Sigma) was added per well for 30 minutes at room temperature. Plates were again washed with PBST, and 100 μl of 2,2′3 azino-bis(3-ethylbenzthiazoline-6-sulfonic acid) (ABTS) substrate solution (Sigma) was added per well. After color development, the reaction was stopped by the addition of 50 μl per well of 1% SDS and the OD was read at 405 nm. The titers of different SCHU S4-specific antibodies were calculated as the lowest dilution of serum that gave an OD of 0.1 above the normal serum control.
Statistical Analysis
Survival experimental results were assessed using Kaplan Meier Survival analysis using GraphPad Prism Program. Additional analysis was also performed using the Students T Test.
Results
Levofloxacin rescues mice from lethal intra-nasal infections with SCHU S4
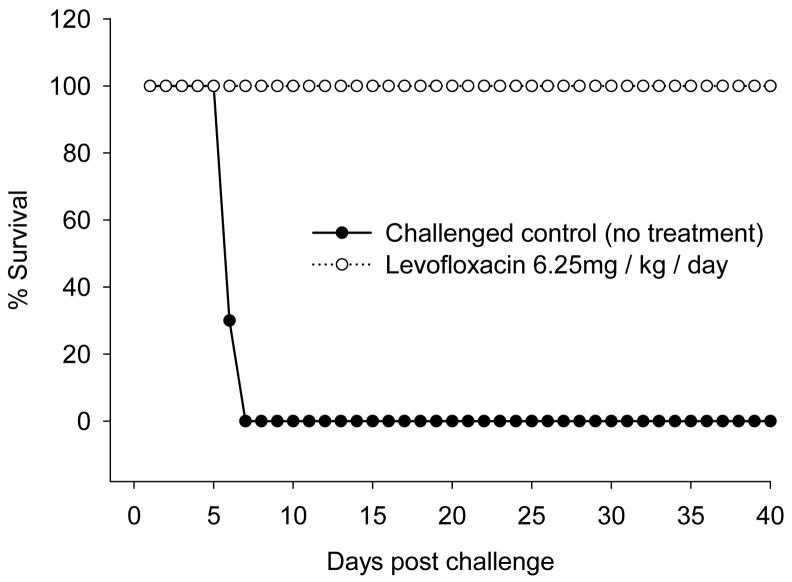
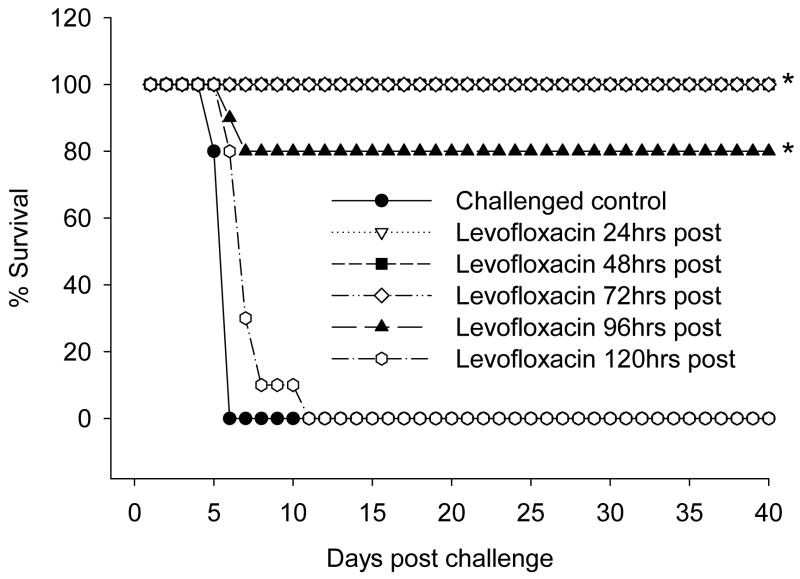
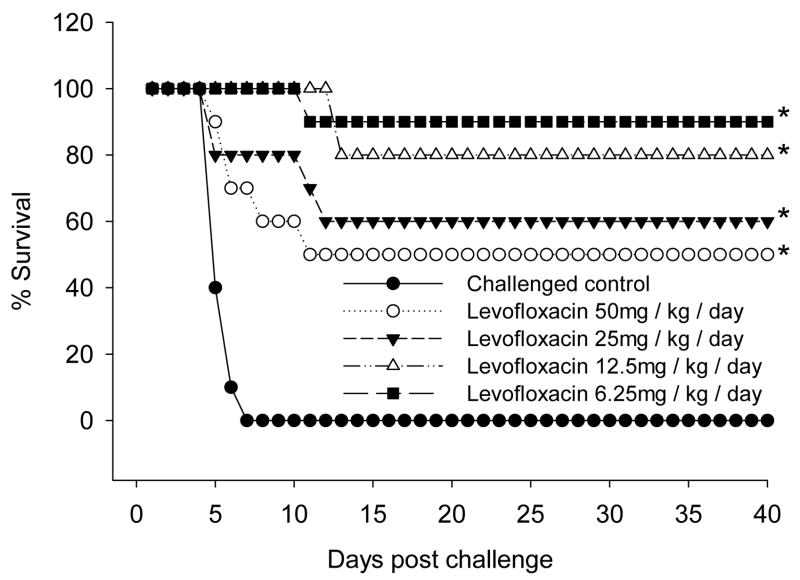
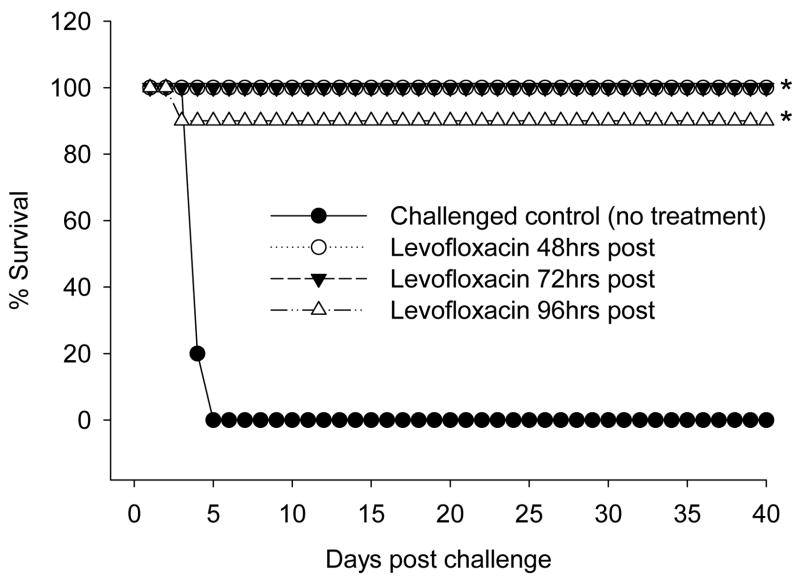
In initial experiments, mice were infected with 3 LD50 doses of SCHU S4 (103 CFU) via intra-nasal challenge, and then 24 hours later given (via intraperitoneal injection) varying doses of levofloxacin (50, 25, 12.5, and 6.25 mg/kg/day) daily for 13 days. Control mice received daily injections of PBS. All doses of levofloxacin offered 100% protection from the SCHU S4 challenge. In contrast, control treated mice, infected but not given levofloxacin, started to die at five days post-infection, with 100% mortality being observed at day seven post challenge. Data from a representative experiment are presented in Figure 1, using the lowest dose of levofloxacin. We then investigated how long we could delay levofloxacin treatment following intra-nasal challenge and still provide protection. For these experiments, we used a high dose of levofloxacin, i.e. 40 mg/kg/day. Mice were challenged intra-nasally with 3 LD50 doses (116 CFU)of SCHU S4 and then divided into six groups (10 mice per group). The control group was infected but received no levofloxacin. The remaining mice were then divided into four groups (10 mice per group), with each group given levofloxacin starting at different times post challenge as follows: 48 hours, 72 hours, 96 hours, and 120 hours post challenge, with continued daily injections for thirteen days as above. Results from this experiment are presented in Figure 2. Levofloxacin treatment could be postponed for up to 72 hours post challenge with 100% of the mice surviving and appearing healthy for up to two months. Delaying treatment with levofloxacin for 96 hours post-challenge still afforded an 80% survival rate for mice. However, levofloxacin failed to reverse a lethal infection if postponed until 120 hours post-infection.
Figure 1. Levofloxacin treatment rescues mice from intranasal SCHU S4 infection.
Balb/c mice were given 3 LD50 doses (103 CFU) of SCHU S4 via intra-nasal challenge, and then 24 hours later given 6.25 mg/kg body weight of levofloxacin via intra-peritoneal injections. As a control, mice were injected with PBS. Mice (10 mice per group) were given levofloxacin or PBS daily for thirteen days. Mice were monitored twice daily for up to two months.
Figure 2. Levofloxacin treatment given at 96 hours post-infection can rescue mice from intra-nasal SCHU S4 infection.
Balb/c mice were given approximately 3 LD50 doses (114 CFU) of SCHU S4 via intra-nasal challenge and then given levofloxacin (i. p., 40 mg/kg body weight) starting at one of the following times post-infection (Post): 48, 72, 96, or 120 hours. As a control, mice were injected with PBS. Mice (10 mice per group) were given levofloxacin or PBS daily for thirteen days. Mice were monitored twice daily for up to two months. Asterisk indicates statistically significant survival with p<0.0001
Bacterial load in tissues of levofloxacin-treated mice
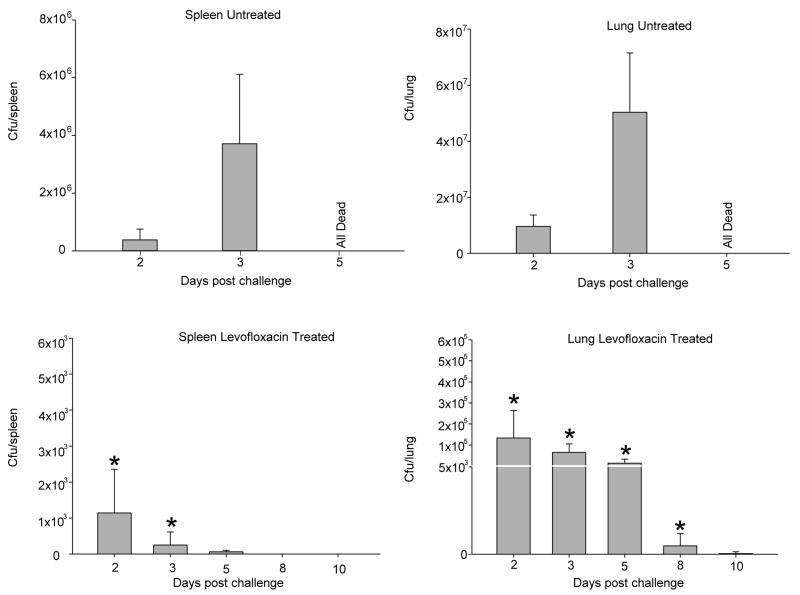
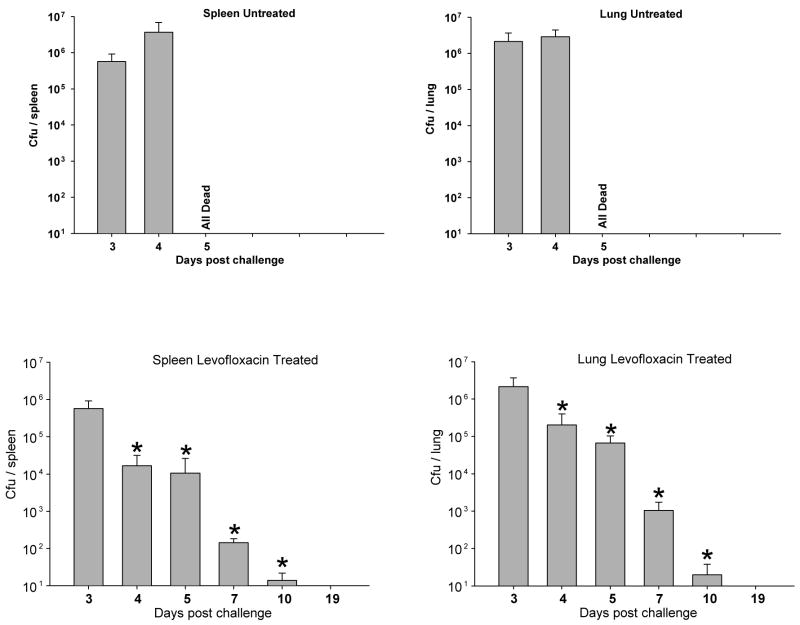
To investigate the mechanism of protection afforded by levofloxacin, we examined SCHU S4-infected control-versus-levofloxacin treated mice for the numbers of viable SCHU S4 present in their spleens and lungs at varying times post challenge. For these experiments, we treated mice with either 6.25 mg/kg/day, starting 24 hours post-infection, or with 40 mg/kg/day, starting at 72 hours post-challenge. Spleen and lungs were then obtained from four individual mice from each group at varying times and homogenized and plated for determining the number of CFU per tissue. The results of these experiments are presented in Figures 3 and 4. Mice receiving no levofloxacin and challenged with SCHU S4 had very high numbers of bacteria in their spleens and lungs at all time points up until time of death. In contrast, mice receiving levofloxacin at 6.25 mg/kg/day starting 24 hours post challenge (Figure 3) had low numbers of SCHU S4 in their lungs and spleens. This was several logs less then what was recovered from infected mice not treated with levofloxacin. At ten days following treatment, there were no detectable bacteria in spleens, and barely detectable numbers in lungs from these treated mice. In contrast, in mice that received levofloxacin at 72 hours post-infection, there were significant numbers of bacteria in their spleens and lungs early after levofloxacin treatment (day 4 and 5). However, the bacterial load in these tissues diminished over time to barely detectable numbers. These results are presented in Figure 4, and demonstrate that there was a low level background bacterial presence/growth in levofloxacin treated mice, and that this was most dramatic when levofloxacin-treatment was delayed until 72 hours post-infection.
Figure 3. Bacterial load in spleen and lungs of mice given levofloxacin starting at 24 hours post-infection.
Mice were infected via intra-nasal challenge (122 CFU) and treated with levofloxacin at 24 hours post-infection as described in Figure 1. At varying times (3, 5, 8, and 10 days) post-infection, mice were sacrificed and the spleen and lungs removed and assessed for the number of SCHU S4 in each tissue by plating. Data is expressed as the mean plus/minus SD from four mice per group. Asterisk indicates statistically different from untreated control mice at same time point. p<0.01
Figure 4. Bacterial load in spleen and lungs of mice given levofloxacin starting at 72 hours post-infection.
Mice were infected via intra-nasal challenge (147 CFU) and treated with levofloxacin at 72 hours post-infection as described in Figure 2. At varying times (3, 4, 5, 7, and 10 days) post infection, mice were sacrificed and the spleen and lungs removed and assessed for the number of SCHU S4 present in each tissue by plating. Data is expressed as the mean plus/minus SD from four mice per group. Asterisk indicates statistically different from untreated control mice at same time point. p<0.01
Levofloxacin treatment results in the generation of protective immunity
Since levofloxacin treatment provided protection from a lethal challenge of Francisella, we next investigated whether these mice, that had been given levofloxacin and protected from a lethal dose of bacteria, had developed any protective immunity against rechallenge with a lethal dose of SCHU S4. In the first series of experiments to address this question, we used mice that had been challenged with SCHU S4 and then treated 24 hours post challenge with different doses of levofloxacin as described above. Thus, mice were challenged intra-nasally with SCHU S4 (90 CFU) and then assigned into groups, with each group being given a different dose of levofloxacin 24 hours after challenge (50, 25, 12.5, or 6.25 mg/kg/day for 13 days), as described above (Figure 1). These mice, which were fully protected by levofloxacin treatment, were then housed for 50 days and then again re-challenged intra-nasally with 3 LD50 doses of SCHU S4. Results of this experiment are shown in Figure 5. Mice given the lower doses of levofloxacin showed immunity/protection towards re-infection/challenge with SCHU S4. Mice initially treated with 6.25 mg/kg/day of levofloxacin had 90% survival following re-challenge. However, the higher the initial dose of levofloxacin used in the treatment, the less protected the mice were from re-challenge. Only 50% survival was achieved in mice that had been treated with the highest dose of levofloxacin, 50 mg/kg/day. As a control for the possible effects of levofloxacin, we treated normal, not infected, mice with 50 mg/kg/day for 13 days and rested these mice for 50 days and then tested them for their susceptibility to SCHU S4 infection. These mice acted identically to control mice with regard to being fully susceptible to the initial challenge dose of SCHU S4, 100% mortality at days 5–6 post-infection (data not presented).
Figure 5. Mice given levofloxacin at 24 hours post-infection are immune to subsequent challenge with SCHU S4.
Mice were infected via intra-nasal challenge (90 CFU) and treated with varying concentrations of levofloxacin at 24 hours post-infection as described in Figure 1. At 24 hours post-infection, mice were divided into groups (ten mice per group) and given one of the following doses of levofloxacin: 6.25, 12.50, 25, or 50 mg/kg body weight. Mice were then housed for 50 days, and then challenged intra-nasally with 3 LD50 doses of SCHU S4. Mice (10 per group) were monitored twice daily for up to one month. Asterisk indicates statistically significant survival with p<0.0007
We then tested mice for protective immunity to Francisella after they had been treated with levofloxacin at varying times post-infection, as described in Figure 2. For these experiments, mice were challenged intra-nasally with a lethal dose of SCHU S4 (88 CFU) and not given levofloxacin treatment (40 mg/kg/day) until 48, 72, or 96 hours post-infection. These mice were housed for 55 days and then again re-challenged intra-nasally with 3 LD50 doses of SCHU S4 (119 CFU). Protective immunity developed in all these mice, as shown in Figure 6. Mice challenged with SCHU S4 and treated with levofloxacin starting at 48 or 72 hours post-infection were completely immune to re-challenge. Mice in these groups had a 100% survival rate. Mice that received levofloxacin at 96 hours post-infection also showed immunity to re-challenge, with 90% survival.
Figure 6. Mice given levofloxacin at 72 hours post-infection are immune to subsequent challenge with SCHU S4.
Mice were infected via intra-nasal challenge (88 CFU) and treated with levofloxacin at varying times post-infection (Post) as described in Figure 2. At 72, 96, and 120 hours post-infection, mice were divided into groups (ten mice per group) and given levofloxacin 40 mg/kg/body weight. Mice were then housed for 55 days, and then challenged intra-nasally with approximately 3 LD50 doses (116 CFU) of Schu 4. Mice (10 per group) were monitored twice daily for up to one month.
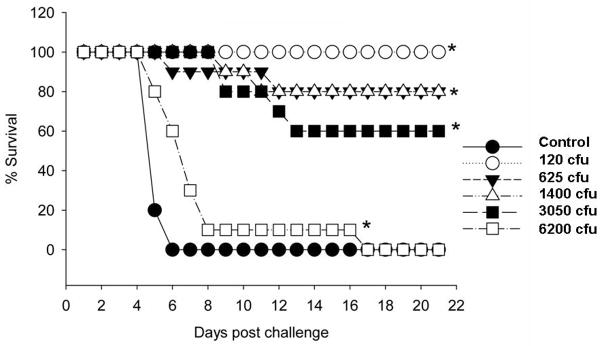
We next assessed the level of immunity induced by levofloxacin treatment. For these experiments, mice were challenged intra-nasally with a lethal dose of SCHU S4 and then given levofloxacin treatment (40 mg/kg/day) starting at 72 hours post-infection, as described in Figure 2. These mice were housed for 50 days and then again re-challenged intra-nasally with varying amounts (120 CFU vs 625 CFU vs 1400 CFU vs 3050 CFU vs 6200 CFU) of SCHU S4. The results from a representative experiment are presented in Figure 7. Significant protection was observed in these mice following re-challenge with up to 90 LD50 (3050 CFU) doses of SCHU S4, 60% survival. Eighty percent survival was observed in these mice follow challenge with 40 LD50 (1400 CFU) doses of SCHU S4.
Figure 7. Assessment of immunity in mice given levofloxacin at 72 hours post-infection.
Mice were challenged intra-nasally with SCHU S4 and then treated with levofloxacin at 72 hours post-infection (40 mg/kg/body weight), as described in Figure 2.
; Mice were then housed for 50 days, and then challenged intra-nasally with varying numbers of SCHU S4 (120, 625, 1400, 3050, and 6200 CFU). Mice (10 per group) were monitored twice daily for up to one month. Asterisk indicates statistically significant survival with p<0.0005
In summary, these results clearly indicated that levofloxacin treatment of Francisella-infected mice can not only rescue these mice from a lethal intra-nasal infection, but more importantly, it allows the mice to develop protective immunity. All of the above experiments have been repeated at least twice with identical results.
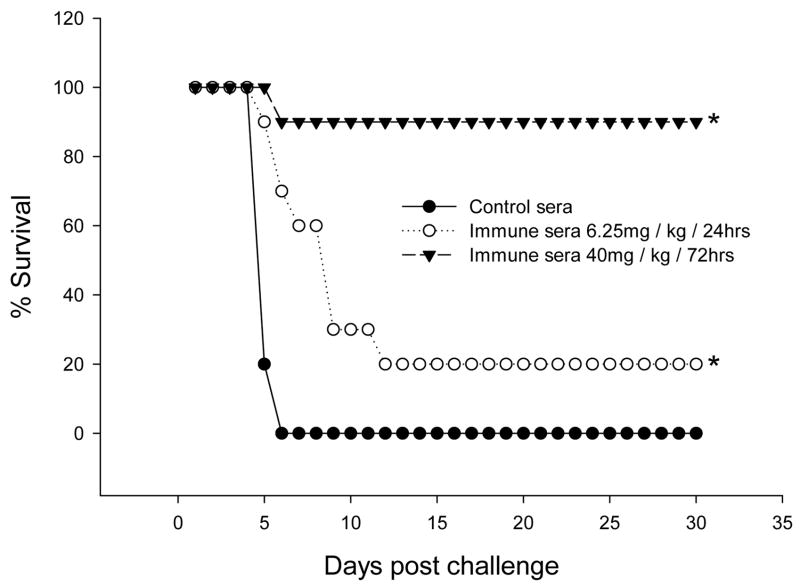
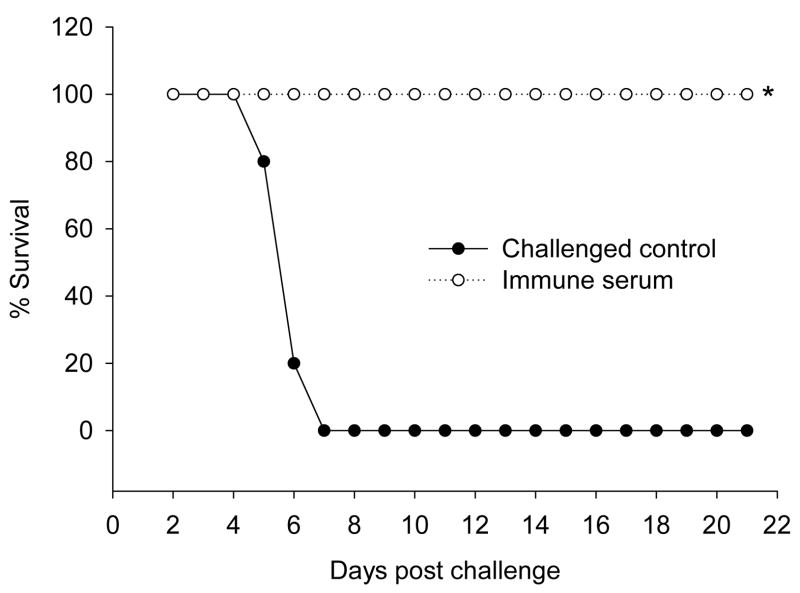
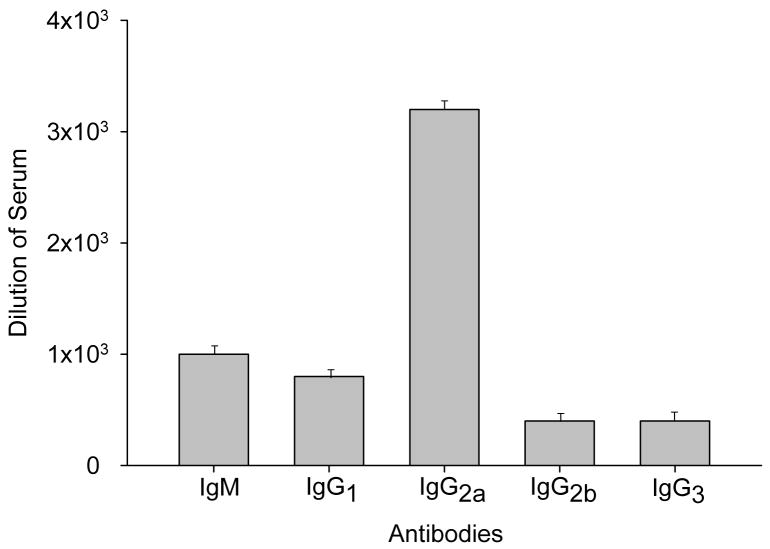
Sera from Levofloxacin-induced immune mice protect normal mice against intra-nasal infection with SCHU S4
Since levofloxacin treatment of SCHU S4 infected mice was found to lead to the development of protective immunity, we investigated whether sera from these mice could provide protection to normal, naïve, mice. Thus, serum was obtained from two different groups of mice. One group of mice was challenged with SCHU S4, and then treated with levofloxacin (6.25 mg/kg/day) starting at 24 hours post-infection as described above (Figure 1). A second group of mice was challenged with SCHU S4, but then treated with levofloxacin (40mg/kg/day) at 72 hours post challenge (Figure 2). These mice were then sacrificed at 30 days post-infection and sera obtained and pooled. As a control, non-infected mice were housed identically and then also sacrificed and sera obtained and pooled. Normal, untreated, mice were then given 250 μl of sera (normal vs immune) and then challenged (intra-nasal) four hours later with 5 LD50 doses (172 CFU) of SCHU S4. Results from one of two identical experiments are presented in Figure 8. Sera from mice treated with levofloxacin at 72 hours post-infection offered almost complete protection to normal, naïve, mice. There was one death in this group of ten mice (10% mortality). These mice stayed disease free for two months before being sacrificed. In contrast, little protection was transferred using sera from mice challenged with SCHU S4 and then given levofloxacin at 24 hours post-infection. There was 80% mortality in this group. As expected, control sera failed to transfer any protection against SCHU S4. Protective sera from mice treated with levofloxacin at 72 hours post-infection offered almost complete protection to normal, naïve, mice even when administered 24 hours post infection (Figure 9). When protective sera were analyzed for the amount of different classes of immunoglobulin, IgG2a was the most dominant SCHU S4-specific antibody present in this sera (Figure 10). This suggested that levofloxacin induced immunity is associated with a Th1 type antibody response. Since sera from mice given levofloxacin at 24 hours post-infection did not give significant protection, we next compared this sera vs the protective sera from mice given levofloxacin at 72 hours post infection. As seen in Figure 11, IgG2a and IgM were significantly higher in the protective serum when compared to the less protective sera obtained from mice given levofloxacin at 24 hours post-infection.
Figure 8. Normal mice are protected from intra-nasal challenge with SCHU S4 by passive transfer of sera from levofloxacin protected mice.
Mice were challenged intra-nasally with SCHU S4 and then treated with levofloxacin at either 24 hours post-infection (6.25 mg/kg body weight) or at 72 hours post-infection (40 mg/kg/body weight), as described in Figures 1 and 2. Thirty days following intra-nasal challenge, mice were sacrificed and sera obtained. Serum was also obtained from control mice, not challenged with SCHU S4. Sera from mice were pooled and then used for passive transfer into normal mice. Normal, naïve, mice were then given 250 μl of serum from either control mice or from mice challenged with SCHU S4 and treated with levofloxacin at 24 vs 72 hours post challenge. Four hours after the transfer of sera, mice were challenged with 5 LD50 doses (172 CFU) of SCHU S4. Mice were monitored twice daily for up to one month. Asterisk indicates statistically significant survival with p<0.0005
Figure 9. Immune sera can protect normal mice even when given 24 hours post-infection.
Mice (normal/naïve) were challenged intra-nasally with approximately 3 LD50 doses (109 CFU) of SCHU S4. At 24 hours post-infection, mice were then given 250 μl of serum from either control mice or immune sera from mice challenged with SCHU S4 and treated with levofloxacin at 72 hours post challenge, as described in Figure 8. Mice were monitored twice daily for up to one month. Asterisk indicates statistically significant survival with p<0.0005
Figure 10. Characterization of protective immune serum.
Immune sera obtained from mice treated with levofloxacin at 72 hours post-infection, which showed protection in passive transfer experiments (Figures 8 and 9), was characterize by ELISA for SCHU S4 specificity. Titers were calculated as the lowest dilution of serum that gave an OD of 0.1 above the normal serum control.
Figure 11. Comparison of protective vs non-protective serums for levels of different Igs.
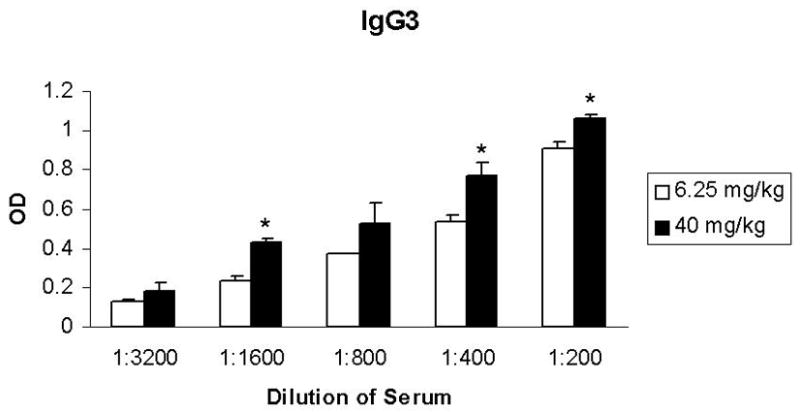
Immune sera obtained from mice treated with levofloxacin at 72 post-infection (protective) was compared with immune sera obtained from mice treated with levofloxacin at 24 hours post-infection (non-protective) by ELISA for the levels of different classes of immunoglobulin specific for SCHU S4. The OD units from control sera were subtracted from the OD units obtained from the corresponding dilution of immune sera and the resultant OD units plotted for each serum dilution. Asterisk indicates statistically significant differences between protective versus non-protective sera.
Discussion
In this report, we show that treatment with levofloxacin can rescue mice from a lethal intra-nasal challenge with virulent SCHU S4. More importantly, we demonstrate that these rescued mice developed protective immunity against intra-nasal rechallenge with SCHU S4. These findings offer a unique model for investigating what potential immune functions are generated in mice infected with virulent Francisella as opposed to LVS, which has been traditionally used in studies for investigating the immune responses associated with tularemia. More importantly, we show that SCHU S4-infected mice treated with levofloxacin develop protective antibody, as assessed by passive transfer to normal mice.
Levofloxacin is in the quinolone family of antibiotics. Quinolones have been shown to be an effective treatment against tularemia (34). This has been documented in animal studies and in some clinical studies (34–36). Quinolones reversibly trap gyrases on DNA as complexes in which the DNA is broken. The complexes block DNA replication, leading to a bactericidal activity. Quinolones have also been shown to alter different functions of the immune system (for review see reference (34)). Usually, immunosuppressive effects have been reported, but some studies have also reported enhancement of different immune functions, e.g., the production of select cytokines. In general, most fluoroquinoloine derivatives appear to be suppressive toward the production of inflammatory cytokines (34,35). The therapeutic benefits of quinolones are assumed to be mediated via direct action on Francisella. Thus, the possibility that Quinolone treatment and resolution of tularemia might result in the generation of protective immunity has not previously been reported.
Mice given levofloxacin either at 24 hours post-infection or at 72 hours post-infection developed protective immunity when rechallenged with 3 LD50 doses of SCHU S4. We did assess the degree of immunity generated in mice given levofloxacin at 72 hours post-infection. These mice showed significant immunity towards 40–90 LD50 doses of Francisella. The degree of immunity induced in mice following multiple immunizations is currently under investigation. However, mice treated at 72 hours post-infection generated protective antibody, while little protective antibody was present in serum from mice treated at 24 hours post-infection. Interestingly, antibody could protect mice even when given 24 hours post-infection. It is probably not a coincidence that protective antibody was generated in mice that had the greatest bacterial burden, but were capable of surviving. Mice given levofloxacin at 72 hours post-infection had significant numbers of SCHU S4 in their spleen and lungs when compared to mice given levofloxacin at 24 hours post-infection. This finding might explain the difference between these different strategies, and suggests that the magnitude of the immune response generated in these mice was greater then that of mice given levofloxacin at 24 hours post-infection. This could also be coupled with the possibility that levofloxacin treatment could expose determinants not routinely seen during a live infection, where no antibiotic is present. The predominant class of immunoglobulin in the protective serum was shown to be IgG2a, leading to the conclusion that a Th1 type of immune response was dominant in mice that were rescued by levofloxacin. Additionally, higher levels of IgG2a and IgM were present in the protective sera then in the non-protective sera. Thus, we cannot rule out a potentially important role for IgM in the protection mediated via passive transfer of the sera from mice given levofloxacin at 72 hours post infection. However, both groups (those in which 24 hour and 72 hour strategies were used) were immune to rechallenge with SCHU S4, indicating that a protective memory immune response was induced upon rechallenge.
The immune functions involved in the protective immunity generated in levofloxacin treated mice are unknown, but currently under investigation. Clearly, antibody must be considered a potentially important mechanism, since serum from mice given the 72 hours strategy was protective. However, many investigators now believe that the adaptive immune response against Francisella is likely mediated by both CMI and humoral immunity. In fact, there is convincing evidence that antibody can protect against many important intracellular pathogens (37). CMI is a crucial arm in host defense against Francisella, but specific antibody (IgG, IgA, and IgM) responses are nevertheless mounted within 10 days during natural Francisella infections or following vaccination (38–46). In this regard, LVS fails to induce protective immunity in B cell-deficient mice, although these mice have normal levels of T cells (47,48). In contrast, depletion of either CD4 or CD8 T cells or neutralization of IFNγ at the time of challenge in LVS-vaccinated mice was shown to result in loss of protection, even though these mice had normal serum antibody levels (30,31). Conlan et al. (30) have shown that mice immunized via aerosol exposure to LVS did have enhanced protection against virulent type A Francisella. However, in this study, not all mice were protected and mice were only followed for 21 days, but IFNγ and CD4 and CD8 T cells were essential for the expression of immunity in the lungs. Lyons and co-workers (31) have shown that intra-nasal vaccination with LVS could protect Balb/c mice, but not C57BL/6 mice, against intra-nasal or subcutaneous challenges with virulent Francisella. This response was shown to be dependent upon T cells and specific for Francisella, but the role for antibody in this protection was not investigated. Additionally, protection was only observed when low doses of virulent Francisella were used for intra-nasal re-challenge. Intra-nasal challenge doses above 2 × 102 CFU proved lethal for such intra-nasally immunized mice. However, boosting intra-nasal LVS-vaccinated mice with a sub-lethal dose of virulent Francisella significantly increased resistance to subsequent challenge with virulent Francisella. This finding was the first real demonstration that mice could be significantly protected from intra-nasal exposure to virulent Francisella. However, neither the protective antigens nor the role of serum antibody in this protection was investigated. KuoLee et al. (49) have also shown that oral immunization of mice with LVS results in protection against respiratory challenge with virulent Francisella. Interestingly, this was successful using Balb/c mice but not C57Bl/6 mice. In this study, oral immunization resulted in detection of antibody in the serum and bronchoalveolar lavage fluids and cytokine production by splenic T cells.
A recent study by Kirimanjeswara et al. (32) has provided new insights into the role of antibody and T cells in protection against respiratory infections with LVS. In this study, antiserum was generated in Balb/c mice by i.p. immunization with LVS. This antiserum, which had high levels of IgG2a, was then investigated for its ability to passively transfer protection to naïve mice against respiratory infection with LVS. It was found that the passively transferred immune sera protected mice from a lethal respiratory infection with LVS. This protection was dependent upon T cells, FcγR bearing cells (bone marrow derived cells), and IFNγ production. Collectively, these results suggested that both antibody and T cells (CMI) are necessary for optimal mucosal protection against pulmonary infections with Francisella. It is not yet known whether T cells, FcγR-bearing cells, and IFNγ are also playing a crucial role in our mouse model where immune sera can protect Balb/c mice from a lethal respiratory infection with virulent SCHU S4.
We have not identified the specific Francisella antigens crucial for generating serum capable of mediating protection via passive transfer. Serum antibodies against both LPS and outer membrane proteins have been detected in humans naturally infected or immunized with LVS (38,40). Mice given repeated large doses of LVS LPS were also shown to be protected against lethal LVS infection but not virulent Francisella (50). In early studies, attempts were made to treat tularemia in humans with immune sera. Reports from these studies yielded conflicting results. Some workers showed that immune serum could successfully be used to treat individuals suffering from tularemia (41), while others reported it as having no value for the treatment in either humans or animals (42,51). Unfortunately, the protective antibody passively transferred in these previously reported studies was not characterized. It was suggested that the conflicting results in humans might have reflected differences in the virulence of the infecting strains, and it may be significant that most of the recent studies demonstrating protection with immune sera have used mice challenged mainly with the low-virulence LVS strain. In this regard, Pasetti et al (53) have recently shown that rabbits immunized with an improved Francisella tularensis live vaccine strain generated antibody that could recognized both LVS and SCHU S4 antigens. In fact, from a number of studies in mice and humans, it is clear that protection against low-virulence strains of Francisella can be mediated by antibody (43,53). But, the only protective antigen of Francisella that has been identified is lipopolysaccharide (LPS). Historically, immunization with LPS provides good protection against only type B strains of Francisella (53,54). Recently, Lu et al (55) have reported that a monoclonal IgG2a specific for LVS LPS conferred full protection in mice against intra-nasal infection with LVS. Thus, the possibility of LPS being an important antigen recognized by protective serum in our passive transfer model is under investigation.
In summary, we describe in this report a mouse model for investigating intra-nasal infection with virulent Francisella. This model offers an opportunity to investigate the immune functions and antigens that are important for mediating protection against respiratory infections with virulent Francisella. Finally, we demonstrated that antibody can play an important role in mediating protection against respiratory infections with virulent Francisella.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dennis DT, Inglesby TV, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Fine AD, Friedlander AM, Hauer J, Layton M, Lillibridge SR, McDade JE, Osterholm MT, O’Toole T, Parker G, Perl TM, Russell PK, Tonat K. Tularemia as a biological weapon: medical and public health management. Jama. 2001;285:2763–73. doi: 10.1001/jama.285.21.2763. [DOI] [PubMed] [Google Scholar]
- 2.Jacobs RF. Tularemia. Adv Pediatr Infect Dis. 1996;12:55–69. [PubMed] [Google Scholar]
- 3.McCrumb FR. Aerosol Infection of Man with Pasteurella Tularensis. Bacteriol Rev. 1961;25:262–7. doi: 10.1128/br.25.3.262-267.1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McLendon MK, Apicella MA, Allen LA. Francisella tularensis: taxonomy, genetics, and Immunopathogenesis of a potential agent of biowarfare. Annu Rev Microbiol. 2006;60:167–85. doi: 10.1146/annurev.micro.60.080805.142126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saslaw S, Eigelsbach HT, Prior JA, Wilson HE, Carhart S. Tularemia vaccine study. II Respiratory challenge. Arch Intern Med. 1961;107:702–14. doi: 10.1001/archinte.1961.03620050068007. [DOI] [PubMed] [Google Scholar]
- 6.Ellis J, Oyston PC, Green M, Titball RW. Tularemia. Clin 2 Microbiol Rev. 2002;15:631–46. doi: 10.1128/CMR.15.4.631-646.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sandstrom G, Sjostedt A, Tarnvik A. The first international conference on Tularemia: Umea, Sweden, 23–25 August 1995 -Introduction. Fems Immunology and Medical Microbiology. 1996;13:179–179. doi: 10.1111/j.1574-695X.1996.tb00232.x. [DOI] [PubMed] [Google Scholar]
- 8.Elkins KL, Cowley SC, Bosio CM. Innate and adaptive immune responses to an intracellular bacterium, Francisella tularensis live vaccine strain. Microbes Infect. 2003;5:135–42. doi: 10.1016/s1286-4579(02)00084-9. [DOI] [PubMed] [Google Scholar]
- 9.Fortier AH, Slayter MV, Ziemba R, Meltzer MS, Nacy CA. Live vaccine strain of Francisella tularensis: infection and immunity in mice. Infect Immun. 1991;59:2922–8. doi: 10.1128/iai.59.9.2922-2928.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jantzen E, Berdal BP, Omland T. Cellular fatty acid composition of Francisella tularensis. J Clin Microbiol. 1979;10:928–30. doi: 10.1128/jcm.10.6.928-930.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nichols PD, Mayberry WR, Antworth CP, White DC. Determination of monounsaturated double-bond position and geometry in the cellular fatty acids of the pathogenic bacterium Francisella tularensis. J Clin 2 Microbiol. 1985;21:738–40. doi: 10.1128/jcm.21.5.738-740.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ancuta P, Pedron T, Girard R, Sandstrom G, Chaby R. Inability of the Francisella tularensis lipopolysaccharide to mimic or to antagonize the induction of cell activation by endotoxins. Infect Immun. 1996;64:2041–6. doi: 10.1128/iai.64.6.2041-2046.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cole LE, Elkins KL, Michalek SM, Qureshi N, Eaton LJ, Rallabhandi P, Cuesta N, Vogel SN. Immunologic consequences of Francisella tularensis live vaccine strain infection: role of the innate immune response in infection and immunity. J Immunol. 2006;176:6888–99. doi: 10.4049/jimmunol.176.11.6888. [DOI] [PubMed] [Google Scholar]
- 14.Telepnev M, Golovliov I, Grundstrom T, Tarnvik A, Sjostedt A. Francisella tularensis inhibits Toll-like receptor-mediated activation of intracellular signalling and secretion of TNF-alpha and IL-1 from murine macrophages. Cell Microbiol. 2003;5:41–51. doi: 10.1046/j.1462-5822.2003.00251.x. [DOI] [PubMed] [Google Scholar]
- 15.Hood AM. Virulence factors of Francisella tularensis. J Hyg (Lond) 1977;79:47–60. doi: 10.1017/s0022172400052840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Skrodzki E. Investigations on the pathogenesis of tularemia. VII. Attempts to discover F. tularensis toxins. Biul Inst Med Morsk Gdansk. 1968;19:69–76. [PubMed] [Google Scholar]
- 17.Lauriano CM, Barker JR, Yoon SS, Nano FE, Arulanandam BP, Hassett DJ, Klose KE. MglA regulates transcription of virulence factors necessary for Francisella tularensis intraamoebae and intramacrophage survival. Proc Natl Acad Sci USA. 2004;101:4246–9. doi: 10.1073/pnas.0307690101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Su J, Yang J, Zhao D, Kawula TH, Banas JA, Zhang JR. Genome-Wide Identification of Francisella tularensis Virulence Determinants 7. Infect Immun. 2007;75:3089–101. doi: 10.1128/IAI.01865-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Twine S, Bystrom M, Chen W, Forsman M, Golovliov I, Johansson A, Kelly J, Lindgren H, Svensson K, Zingmark C, Conlan W, Sjostedt A. A mutant of Francisella tularensis strain SCHU S4 lacking the ability to express a 58-kilodalton protein is attenuated for virulence and is an effective live vaccine. Infect Immun. 2005;73:8345–52. doi: 10.1128/IAI.73.12.8345-8352.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weiss DS, Brotcke A, Henry T, Margolis JJ, Chan K, Monack DM. In vivo negative selection screen identifies genes required for Francisella virulence. Proc Natl Acad Sci USA. 2007;104:6037–42. doi: 10.1073/pnas.0609675104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barclay WR, Busey WM, Dalgard DW, Good RC, Janicki BW, Kasik JE, Ribi E, Ulrich CE, Wolinsky E. Protection of monkeys 12 against airborne tuberculosis by aerosol vaccination with bacillus Calmette 13 Guerin. Am Rev Respir Dis. 1973;107:351–8. doi: 10.1164/arrd.1973.107.3.351. [DOI] [PubMed] [Google Scholar]
- 22.Eigelsbach HT, Tulis JJ, Overholt EL, Griffith WR. Aerogenic immunization of the monkey and guinea pig with live tularemia vaccine. Proc Soc Exp Biol Med. 1961;108:732–4. doi: 10.3181/00379727-108-27049. [DOI] [PubMed] [Google Scholar]
- 23.Lefford MJ. Induction and expression of immunity after BCG immunization. Infect Immun. 1977;18:646–53. doi: 10.1128/iai.18.3.646-653.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tulis JJ, Eigelsbach HT, Kerpsack RW. Host-parasite relationship in monkeys administered live tularemia vaccine. Am J Pathol. 1970;58:329–36. [PMC free article] [PubMed] [Google Scholar]
- 25.Shen H, Chen W, Conlan JW. Susceptibility of various mouse strains to systemically-or aerosol-initiated tularemia by virulent type A Francisella tularensis before and after immunization with the attenuated live vaccine strain of the pathogen. Vaccine. 2004;22:2116–21. doi: 10.1016/j.vaccine.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 26.Bosio CM, Dow SW. Francisella tularensis induces aberrant activation of pulmonary dendritic cells. J Immunol. 2005;175(6):792–801. doi: 10.4049/jimmunol.175.10.6792. [DOI] [PubMed] [Google Scholar]
- 27.Conlan JW, Chen W, Shen H, Webb A, KuoLee R. Experimental tularemia in mice challenged by aerosol or intradermally with virulent strains of Francisella tularensis: bacteriologic and histopathologic studies. Microb Pathog. 2003;34:239–48. doi: 10.1016/s0882-4010(03)00046-9. [DOI] [PubMed] [Google Scholar]
- 28.Duckett NS, Olmos S, Durrant DM, Metzger DW. Intra-nasal interleukin-12 treatment for protection against respiratory infection with the Francisella tularensis live vaccine strain. Infect Immun. 2005;73:2306–11. doi: 10.1128/IAI.73.4.2306-2311.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Metzger DW, Bakshi CS, Kirimanjeswara G. Mucosal Immunopathogenesis of Francisella tularensis. Ann N Y Acad Sci. 2007 doi: 10.1196/annals.1409.007. [DOI] [PubMed] [Google Scholar]
- 30.Conlan JW, Shen H, Kuolee R, Zhao X, Chen W. Aerosol-, but not intradermal-immunization with the live vaccine strain of Francisella tularensis protects mice against subsequent aerosol challenge with a highly virulent type A strain of the pathogen by an alphabeta T cell-and interferon gamma-dependent mechanism. Vaccine. 2005;23:2477–85. doi: 10.1016/j.vaccine.2004.10.034. [DOI] [PubMed] [Google Scholar]
- 31.Wu TH, Hutt JA, Garrison KA, Berliba LS, Zhou Y, Lyons CR. Intra-nasal vaccination induces protective immunity against intra-nasal infection with virulent Francisella tularensis biovar A. Infect Immun. 2005;73:2644–54. doi: 10.1128/IAI.73.5.2644-2654.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kirimanjeswara GS, Golden JM, Bakshi CS, Metzger DW. Prophylactic and therapeutic use of antibodies for protection against respiratory infection with Francisella tularensis. J Immunol. 2007;179:532–9. doi: 10.4049/jimmunol.179.1.532. [DOI] [PubMed] [Google Scholar]
- 33.Comer JE, Noffsinger DM, McHenry DJ, Weisbaum DM, Chatuev BM, Chopra AK, Peterson JW. Evaluation of the protective effects of quinacrine against Bacillus anthracis Ames. J Toxicol Environ Health A. 2006;69:1083–95. doi: 10.1080/15287390500360281. [DOI] [PubMed] [Google Scholar]
- 34.Dalhoff A, Shalit I. Immunomodulatory effects of quinolones 2. Lancet Infect Dis. 2003;3:359–71. doi: 10.1016/s1473-3099(03)00658-3. [DOI] [PubMed] [Google Scholar]
- 35.Aranda EA. Treatment of tularemia with levofloxacin. Clin Microbiol Infect. 2001;7:167–8. doi: 10.1046/j.1469-0691.2001.00234.x. [DOI] [PubMed] [Google Scholar]
- 36.Piercy T, Steward J, Lever MS, Brooks TJ. In vivo efficacy of fluoroquinolones against systemic tularaemia infection in mice. J Antimicrob Chemother. 2005;56:1069–73. doi: 10.1093/jac/dki359. [DOI] [PubMed] [Google Scholar]
- 37.Casadevall A, Pirofski LA. A reappraisal of humoral immunity based on mechanisms of antibody-mediated protection against intracellular pathogens. Adv Immunol. 2006;91:1–44. doi: 10.1016/S0065-2776(06)91001-3. [DOI] [PubMed] [Google Scholar]
- 38.Bevanger L, Maeland JA, Naess AI. Agglutinins and antibodies to Francisella tularensis outer membrane antigens in the early diagnosis of disease during an outbreak of tularemia. J Clin Microbiol. 1988;26:433–7. doi: 10.1128/jcm.26.3.433-437.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carlsson HE, Lindberg AA, Lindberg G, Hederstedt B, Karlsson KA, Agell BO. Enzyme-linked immunosorbent assay for immunological diagnosis of human tularemia. J Clin Microbiol. 1979;10:615–21. doi: 10.1128/jcm.10.5.615-621.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Drabick JJ, Narayanan RB, Williams JC, Leduc JW, Nacy CA. Passive protection of mice against lethal Francisella tularensis (live tularemia vaccine strain) infection by the sera of human recipients of the live tularemia vaccine. Am J Med Sci. 1994;308:83–7. doi: 10.1097/00000441-199408000-00003. [DOI] [PubMed] [Google Scholar]
- 41.Foshay L. A comparative study of the treatment of tularemia with immune serum, hyperimmune serum and streptomycin. Am J Med. 1946;1:180–188. doi: 10.1016/0002-9343(46)90036-8. [DOI] [PubMed] [Google Scholar]
- 42.Francis E, Foshay L. Antitularemic serum. Public Health Rep. 1942;957:44–55. [Google Scholar]
- 43.Fulop M, Mastroeni P, Green M, Titball RW. Role of antibody to lipopolysaccharide in protection against low-and high-virulence strains of Francisella tularensis. Vaccine. 2001;19:4465–72. doi: 10.1016/s0264-410x(01)00189-x. [DOI] [PubMed] [Google Scholar]
- 44.Koskela P, Salminen A. Humoral immunity against Francisella tularensis after natural infection. J Clin Microbiol. 1985;22:973–9. doi: 10.1128/jcm.22.6.973-979.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Saslaw S, Carhart S. Studies with tularemia vaccines in volunteers. III Serologic aspects following intracutaneous or respiratory challenge in both vaccinated and nonvaccinated volunteers. Am J Med Sci. 1961;241:689–99. [PubMed] [Google Scholar]
- 46.Saslaw S, Eigelsbach HT, Wilson HE, Prior JA, Carhart S. Tularemia vaccine study. I. Intracutaneous challenge. Arch Intern Med. 1961;107:68922–701. doi: 10.1001/archinte.1961.03620050055006. [DOI] [PubMed] [Google Scholar]
- 47.Bosio CM, Elkins KL. Susceptibility to secondary Francisella tularensis live vaccine strain infection in B-cell-deficient mice is associated with neutrophilia but not with defects in specific T-cell-mediated immunity. Infect Immun. 2001;69:194–203. doi: 10.1128/IAI.69.1.194-203.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Elkins KL, Bosio CM, Rhinehart-Jones TR. Importance of B cells, but not specific antibodies, in primary and secondary protective immunity to the intracellular bacterium Francisella tularensis live vaccine strain. Infect Immun. 1999;67:6002–7. doi: 10.1128/iai.67.11.6002-6007.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kuolee R, Harris G, Conlan JW, Chen W. Oral immunization of mice with the live vaccine strain (LVS) of Francisella tularensis protects mice against respiratory challenge with virulent type A F. tularensis. Vaccine. 2007;25:3781–91. doi: 10.1016/j.vaccine.2007.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fulop M, Manchee R, Titball R. Role of lipopolysaccharide and a major outer membrane protein from Francisella tularensis in the induction of immunity against tularemia. Vaccine. 1995;13:1220–5. doi: 10.1016/0264-410x(95)00062-6. [DOI] [PubMed] [Google Scholar]
- 51.Ruchman I, Foshay L. Immune response in mice after vaccination with bacterium tularense. J immunol. 1949;61:229–234. [PubMed] [Google Scholar]
- 52.Tarnvik A. Nature of protective immunity to Francisella tularensis. Rev Infect Dis. 1989;11:440–51. [PubMed] [Google Scholar]
- 53.Pasetti MF, Cuberos L, Horn HL, Shearer JD, Matthews SJ, House RV, Sztein MB. An Improved Franceisella tularensis live vaccine strain (LVS) is well tolerated and highly immunogenic when administered to rabbits in escalating doses using various immunization routes. Vaccine. 2008;26:1773–1785. doi: 10.1016/j.vaccine.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Overholt EL, Tigertt WD, Kadull PJ, Ward MK, Charkes ND, Rene RM, Salzman TE, Stephens M. An analysis of forty-two cases of laboratory-acquired tularemia. Treatment with broad spectrum antibiotics. Am J Med. 1961;30:785–806. doi: 10.1016/0002-9343(61)90214-5. [DOI] [PubMed] [Google Scholar]
- 55.Lu Z, Roche MI, Hui JH, Unal B, Felgner PL, Gulati S, Madico G, Sharon J. Generation and characterization of hybridoma antibodies for immunotherapy of tularemia. Immunol Lett. 2007 doi: 10.1016/j.imlet.2007.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]