Abstract
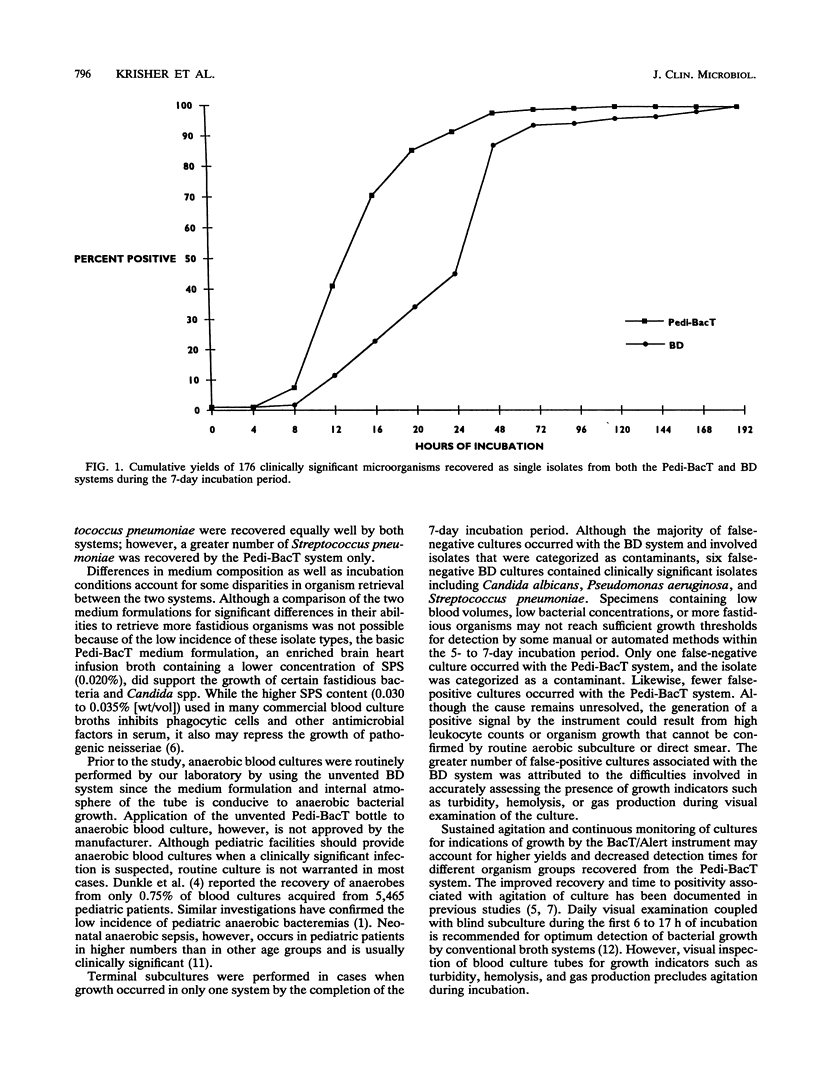
The performance of the Pedi-BacT system, the BacT/Alert (Organon Teknika Corp., Durham, N.C.) pediatric blood culture bottle, was compared with that of a conventional 20-ml supplemented peptone broth tube (Becton-Dickinson Corp., Cockeysville, Md.) (BD system) in matched aerobic cultures. The tubes of the BD system were visually examined daily for 7 days and were subcultured during the first 24 h of incubation. Pedi-BacT cultures were mechanically agitated and continuously monitored for growth by the instrument. Of the 6,628 compliant pairs, 331 (5.0%) were positive in both systems, 220 (3.3%) were positive in the Pedi-BacT system only, and 170 (2.6%) were positive in the BD system only. One (0.02%) false-negative culture and 15 (0.2%) false-positive cultures occurred with the Pedi-BacT system while 20 (0.3%) false-negative cultures and 35 (0.5%) false-positive cultures occurred with the BD system. Of 288 clinically significant organisms detected in matched pairs from which a single isolate was recovered, 176 (61%) were recovered from both systems, 83 (29%) were recovered from the Pedi-BacT system only (P < 0.0001), and 29 (10%) were recovered from the BD system only. Members of the family Enterobacteriaceae (P < 0.01), miscellaneous nonfermenters (P < 0.05), and Candida spp. (P < 0.01) were isolated more frequently in the Pedi-BacT system than in the BD system. No significant difference in recovery of other organisms was found between the systems. The average time to detection for the Pedi-BacT system ranged from 11.5 h for streptococci to 29.7 h for enterococci, while that for the BD system ranged from 20.3 h for streptococci to 66.4 h for some nonfermenters. The BacT/Alert system is a reliable, labor-saving alternative to conventional blood culture methods.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bryan C. S., Reynolds K. L., Derrick C. W., Jr Patterns of bacteremia in pediatrics practice: factors affecting mortality rates. Pediatr Infect Dis. 1984 Jul-Aug;3(4):312–316. doi: 10.1097/00006454-198407000-00007. [DOI] [PubMed] [Google Scholar]
- Campos J. M. Detection of bloodstream infections in children. Eur J Clin Microbiol Infect Dis. 1989 Sep;8(9):815–824. doi: 10.1007/BF02185854. [DOI] [PubMed] [Google Scholar]
- Carey R. B. Clinical comparison of the Isolator 1.5 microbial tube and the BACTEC radiometric system for detection of bacteremia in children. J Clin Microbiol. 1984 May;19(5):634–638. doi: 10.1128/jcm.19.5.634-638.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkle L. M., Brotherton T. J., Feigin R. D. Anaerobic infections in children: a prospective study. Pediatrics. 1976 Mar;57(3):311–320. [PubMed] [Google Scholar]
- Ellner P. D., Kiehn T. E., Beebe J. L., McCarthy L. R. Critical analysis of hypertonic medium and agitation in detection of bacteremia. J Clin Microbiol. 1976 Sep;4(3):216–224. doi: 10.1128/jcm.4.3.216-224.1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eng J., Iveland H. Inhibitory effect in vitro of sodium polyanethol sulfonate on the growth of Neisseria meningitidis. J Clin Microbiol. 1975 May;1(5):444–447. doi: 10.1128/jcm.1.5.444-447.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins B. L., Peterson E. M., de la Maza L. M. Improvement of positive blood culture detection by agitation. Diagn Microbiol Infect Dis. 1986 Sep;5(3):207–213. doi: 10.1016/0732-8893(86)90003-9. [DOI] [PubMed] [Google Scholar]
- La Scolea L. J., Jr, Dryja D., Sullivan T. D., Mosovich L., Ellerstein N., Neter E. Diagnosis of bacteremia in children by quantitative direct plating and a radiometric procedure. J Clin Microbiol. 1981 Mar;13(3):478–482. doi: 10.1128/jcm.13.3.478-482.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morello J. A., Matushek S. M., Dunne W. M., Hinds D. B. Performance of a BACTEC nonradiometric medium for pediatric blood cultures. J Clin Microbiol. 1991 Feb;29(2):359–362. doi: 10.1128/jcm.29.2.359-362.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noel G. J., Laufer D. A., Edelson P. J. Anaerobic bacteremia in a neonatal intensive care unit: an eighteen-year experience. Pediatr Infect Dis J. 1988 Dec;7(12):858–862. [PubMed] [Google Scholar]
- Sullivan T. D., LaScolea L. J., Jr, Neter E. Relationship between the magnitude of bacteremia in children and the clinical disease. Pediatrics. 1982 Jun;69(6):699–702. [PubMed] [Google Scholar]
- Thorpe T. C., Wilson M. L., Turner J. E., DiGuiseppi J. L., Willert M., Mirrett S., Reller L. B. BacT/Alert: an automated colorimetric microbial detection system. J Clin Microbiol. 1990 Jul;28(7):1608–1612. doi: 10.1128/jcm.28.7.1608-1612.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washington J. A., 2nd, Ilstrup D. M. Blood cultures: issues and controversies. Rev Infect Dis. 1986 Sep-Oct;8(5):792–802. doi: 10.1093/clinids/8.5.792. [DOI] [PubMed] [Google Scholar]
- Welch D. F., Scribner R. K., Hensel D. Evaluation of a lysis direct plating method for pediatric blood cultures. J Clin Microbiol. 1985 Jun;21(6):955–958. doi: 10.1128/jcm.21.6.955-958.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]


