Abstract
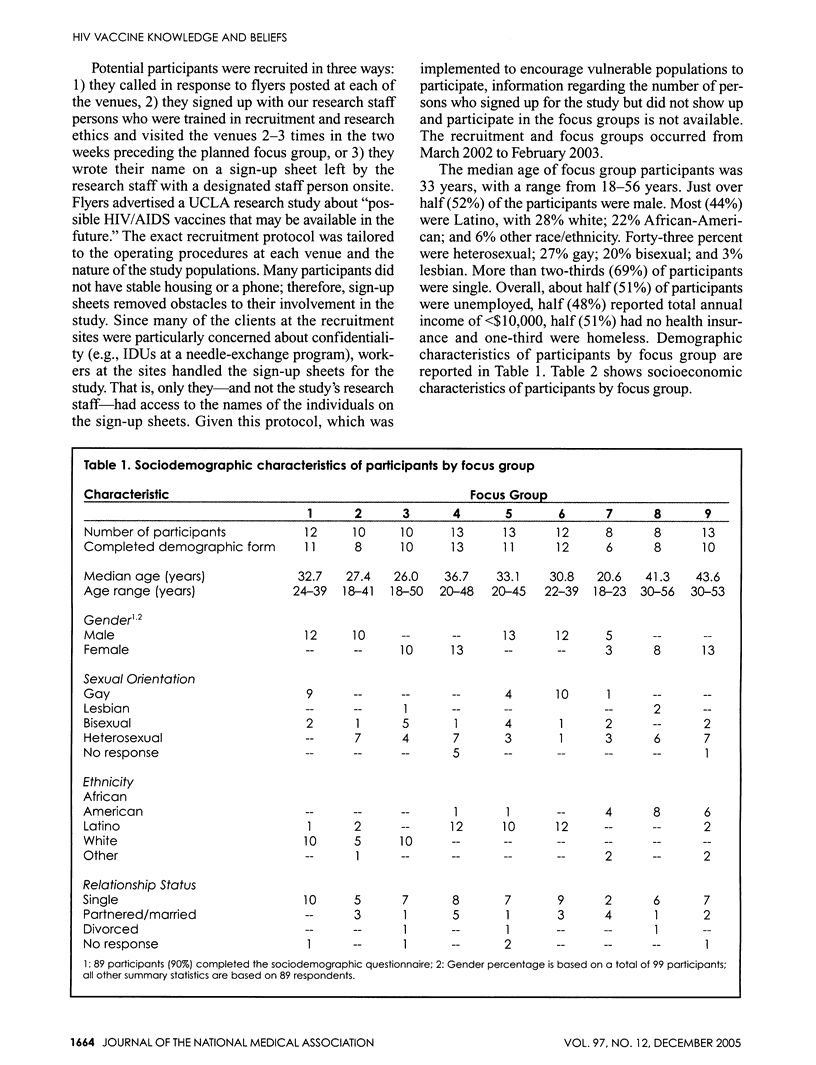
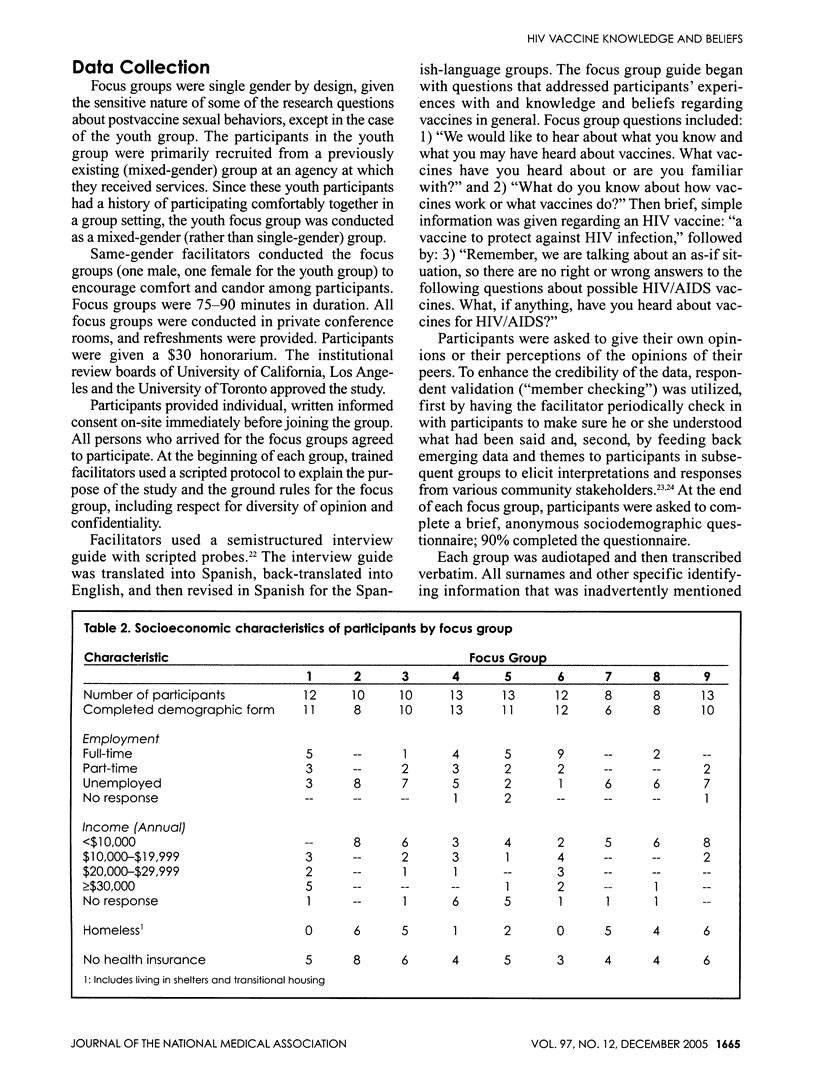
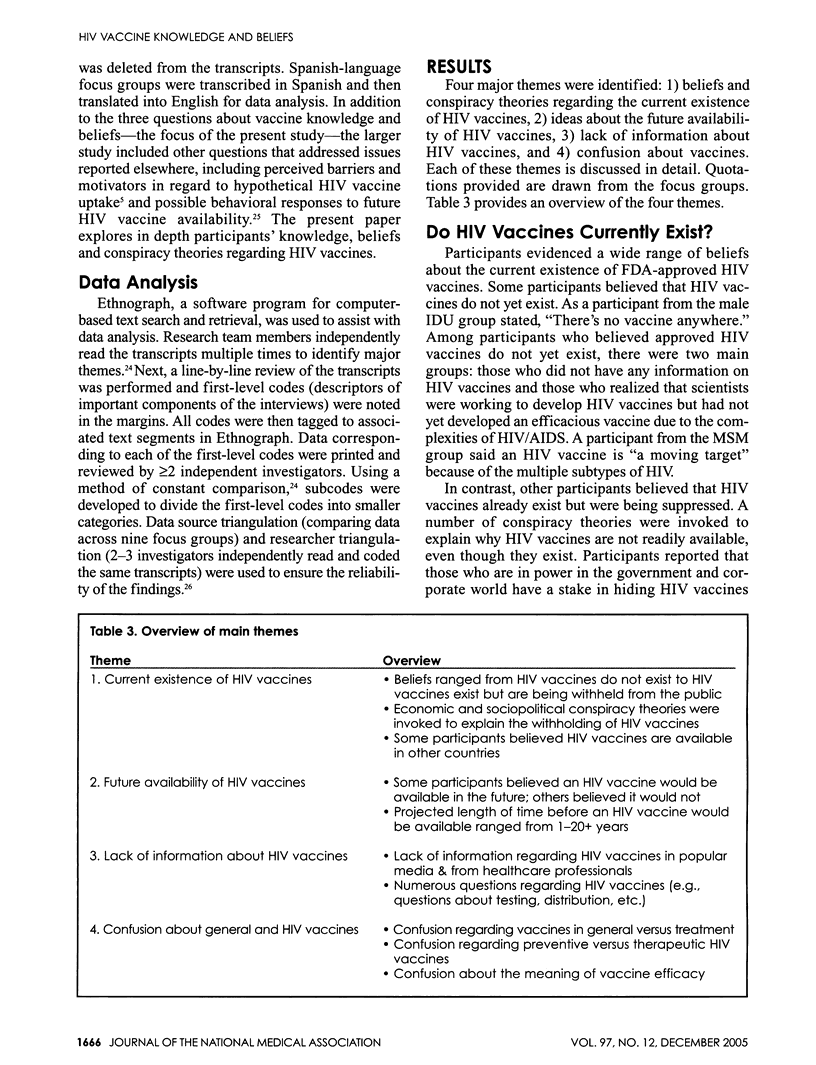
HIV vaccines offer the best long-term hope of controlling the AIDS pandemic. We explored HIV vaccine knowledge and beliefs among communities at elevated risk for HIV/AIDS. Participants (N=99; median age=33 years; 48% female; 22% African-American; 44% Latino; 28% white; 6% other) were recruited from seven high-risk venues in Los Angeles, California, using purposive, venue-based sampling. Results from nine focus groups revealed: 1) mixed beliefs and conspiracy theories about the existence of HIV vaccines; 2) hopefulness and doubts about future HIV vaccine availability; 3) lack of information about HIV vaccines; and 4) confusion about vaccines and how they work. Tailored HIV vaccine education that addresses the current status of HIV vaccine development and key vaccine concepts is warranted among communities at risk. Ongoing dialogue among researchers, public health practitioners and communities at risk may provide a vital opportunity to dispel misinformation and rumors and to cultivate trust, which may facilitate HIV vaccine trial participation and uptake of future HIV vaccines.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson R. M., Garnett G. P. Low-efficacy HIV vaccines: potential for community-based intervention programmes. Lancet. 1996 Oct 12;348(9033):1010–1013. doi: 10.1016/s0140-6736(96)07100-0. [DOI] [PubMed] [Google Scholar]
- Bates Benjamin R., Harris Tina M. The Tuskegee Study of Untreated Syphilis and public perceptions of biomedical research: a focus group study. J Natl Med Assoc. 2004 Aug;96(8):1051–1064. [PMC free article] [PubMed] [Google Scholar]
- Blower S. M., McLean A. R. Prophylactic vaccines, risk behavior change, and the probability of eradicating HIV in San Francisco. Science. 1994 Sep 2;265(5177):1451–1454. doi: 10.1126/science.8073289. [DOI] [PubMed] [Google Scholar]
- Bogart Laura M., Bird Sheryl Thorburn. Exploring the relationship of conspiracy beliefs about HIV/AIDS to sexual behaviors and attitudes among African-American adults. J Natl Med Assoc. 2003 Nov;95(11):1057–1065. [PMC free article] [PubMed] [Google Scholar]
- Bogart Laura M., Thorburn Sheryl. Are HIV/AIDS conspiracy beliefs a barrier to HIV prevention among African Americans? J Acquir Immune Defic Syndr. 2005 Feb 1;38(2):213–218. doi: 10.1097/00126334-200502010-00014. [DOI] [PubMed] [Google Scholar]
- Bojak Alexandra, Deml Ludwig, Wagner Ralf. The past, present and future of HIV-vaccine development: a critical view. Drug Discov Today. 2002 Jan 1;7(1):36–46. doi: 10.1016/s1359-6446(01)02081-5. [DOI] [PubMed] [Google Scholar]
- Celentano D. D., Beyrer C., Natpratan C., Eiumtrakul S., Sussman L., Renzullo P. O., Khamboonruang C., Nelson K. E. Willingness to participate in AIDS vaccine trials among high-risk populations in northern Thailand. AIDS. 1995 Sep;9(9):1079–1083. doi: 10.1097/00002030-199509000-00015. [DOI] [PubMed] [Google Scholar]
- Corbie-Smith Giselle, Thomas Stephen B., St George Diane Marie M. Distrust, race, and research. Arch Intern Med. 2002 Nov 25;162(21):2458–2463. doi: 10.1001/archinte.162.21.2458. [DOI] [PubMed] [Google Scholar]
- Cummings K. M., Becker M. H., Maile M. C. Bringing the models together: an empirical approach to combining variables used to explain health actions. J Behav Med. 1980 Jun;3(2):123–145. doi: 10.1007/BF00844986. [DOI] [PubMed] [Google Scholar]
- Daniels Nicholas A., Juarbe Teresa, Rangel-Lugo Martha, Moreno-John Gina, Pérez-Stable Eliseo J. Focus group interviews on racial and ethnic attitudes regarding adult vaccinations. J Natl Med Assoc. 2004 Nov;96(11):1455–1461. [PMC free article] [PubMed] [Google Scholar]
- Edgeworth Rebecca L., San Juan Homero, Rosenzweig Jason A., Nguyen Nang L., Boyer Jean D., Ugen Kenneth E. Vaccine development against HIV-1: current perspectives and future directions. Immunol Res. 2002;25(1):53–74. doi: 10.1385/ir:25:1:53. [DOI] [PubMed] [Google Scholar]
- Esparza José, Chang Marie-Louise, Widdus Roy, Madrid Yvette, Walker Neff, Ghys Peter D. Estimation of "needs" and "probable uptake" for HIV/AIDS preventive vaccines based on possible policies and likely acceptance (a WHO/UNAIDS/IAVI study). Vaccine. 2003 May 16;21(17-18):2032–2041. doi: 10.1016/s0264-410x(02)00775-2. [DOI] [PubMed] [Google Scholar]
- Francis Donald P., Heyward William L., Popovic Vladimir, Orozco-Cronin Patti, Orelind Karin, Gee Carolyn, Hirsch Adrian, Ippolito Tina, Luck Aimee, Longhi Michael. Candidate HIV/AIDS vaccines: lessons learned from the World's first phase III efficacy trials. AIDS. 2003 Jan 24;17(2):147–156. doi: 10.1097/01.aids.0000050786.28043.62. [DOI] [PubMed] [Google Scholar]
- Freeman V. A., Freed G. L. Parental knowledge, attitudes, and demand regarding a vaccine to prevent varicella. Am J Prev Med. 1999 Aug;17(2):153–155. doi: 10.1016/s0749-3797(99)00063-x. [DOI] [PubMed] [Google Scholar]
- Freimuth V. S., Quinn S. C., Thomas S. B., Cole G., Zook E., Duncan T. African Americans' views on research and the Tuskegee Syphilis Study. Soc Sci Med. 2001 Mar;52(5):797–808. doi: 10.1016/s0277-9536(00)00178-7. [DOI] [PubMed] [Google Scholar]
- Gifford Allen L., Cunningham William E., Heslin Kevin C., Andersen Ron M., Nakazono Terry, Lieu Dale K., Shapiro Martin F., Bozzette Samuel A., HIV Cost and Services Utilization Study Consortium Participation in research and access to experimental treatments by HIV-infected patients. N Engl J Med. 2002 May 2;346(18):1373–1382. doi: 10.1056/NEJMsa011565. [DOI] [PubMed] [Google Scholar]
- Guinan M. E. Black communities' belief in "AIDS as genocide". A barrier to overcome for HIV prevention. Ann Epidemiol. 1993 Mar;3(2):193–195. doi: 10.1016/1047-2797(93)90136-r. [DOI] [PubMed] [Google Scholar]
- Halpern S. D., Metzger D. S., Berlin J. A., Ubel P. A. Who will enroll? Predicting participation in a phase II AIDS vaccine trial. J Acquir Immune Defic Syndr. 2001 Jul 1;27(3):281–288. doi: 10.1097/00126334-200107010-00011. [DOI] [PubMed] [Google Scholar]
- Haynes B. F. Scientific and social issues of human immunodeficiency virus vaccine development. Science. 1993 May 28;260(5112):1279–1286. doi: 10.1126/science.8493572. [DOI] [PubMed] [Google Scholar]
- Herek G. M., Capitanio J. P. Conspiracies, contagion, and compassion: trust and public reactions to AIDS. AIDS Educ Prev. 1994 Aug;6(4):365–375. [PubMed] [Google Scholar]
- Herek Gregory M., Capitanio John P., Widaman Keith F. HIV-related stigma and knowledge in the United States: prevalence and trends, 1991-1999. Am J Public Health. 2002 Mar;92(3):371–377. doi: 10.2105/ajph.92.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmberg S. D. The estimated prevalence and incidence of HIV in 96 large US metropolitan areas. Am J Public Health. 1996 May;86(5):642–654. doi: 10.2105/ajph.86.5.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Dale J., Vitek Charles R., Bartholow Bradford, Mastro Timothy D. Key issues for a potential human immunodeficiency virus vaccine. Clin Infect Dis. 2003 Feb 17;36(5):638–644. doi: 10.1086/367891. [DOI] [PubMed] [Google Scholar]
- Israsena S., Kamolratanakul P., Sakulramrung R. Factors influencing acceptance of hepatitis B vaccination by hospital personnel in an area hyperendemic for hepatitis B. Am J Gastroenterol. 1992 Dec;87(12):1807–1809. [PubMed] [Google Scholar]
- Klonoff E. A., Landrine H. Do blacks believe that HIV/AIDS is a government conspiracy against them? Prev Med. 1999 May;28(5):451–457. doi: 10.1006/pmed.1999.0463. [DOI] [PubMed] [Google Scholar]
- Koblin B. A., Heagerty P., Sheon A., Buchbinder S., Celum C., Douglas J. M., Gross M., Marmor M., Mayer K., Metzger D. Readiness of high-risk populations in the HIV Network for Prevention Trials to participate in HIV vaccine efficacy trials in the United States. AIDS. 1998 May 7;12(7):785–793. doi: 10.1097/00002030-199807000-00015. [DOI] [PubMed] [Google Scholar]
- Koblin B. A., Holte S., Lenderking B., Heagerty P. Readiness for HIV vaccine trials: changes in willingness and knowledge among high-risk populations in the HIV network for prevention trials. The HIVNET Vaccine Preparedness Study Protocol Team. J Acquir Immune Defic Syndr. 2000 Aug 15;24(5):451–457. doi: 10.1097/00126334-200008150-00010. [DOI] [PubMed] [Google Scholar]
- Levy J. A. What can be achieved with an HIV vaccine? Lancet. 2001 Jan 20;357(9251):223–224. doi: 10.1016/S0140-6736(00)03601-1. [DOI] [PubMed] [Google Scholar]
- Liau A., Zimet G. D. The acceptability of HIV immunization: examining vaccine characteristics as determining factors. AIDS Care. 2001 Oct;13(5):643–650. doi: 10.1080/09540120120075275. [DOI] [PubMed] [Google Scholar]
- Mantell Joanne E., Myer Landon, Carballo-Diéguez Alex, Stein Zena, Ramjee Gita, Morar Neetha S., Harrison Polly F. Microbicide acceptability research: current approaches and future directions. Soc Sci Med. 2005 Jan;60(2):319–330. doi: 10.1016/j.socscimed.2004.05.011. [DOI] [PubMed] [Google Scholar]
- McGrath J. W., George K., Svilar G., Ihler E., Mafigiri D., Kabugo M., Mugisha E. Knowledge about vaccine trials and willingness to participate in an HIV/AIDS vaccine study in the Ugandan military. J Acquir Immune Defic Syndr. 2001 Aug 1;27(4):381–388. doi: 10.1097/00126334-200108010-00009. [DOI] [PubMed] [Google Scholar]
- Newman Peter A., Duan Naihua, Rudy Ellen T., Johnston-Roberts Kathleen. HIV risk and prevention in a post-vaccine context. Vaccine. 2004 May 7;22(15-16):1954–1963. doi: 10.1016/j.vaccine.2003.10.031. [DOI] [PubMed] [Google Scholar]
- Newman Peter A., Duan Naihua, Rudy Ellen T., Roberts Kathleen J., Swendeman Dallas. Posttrial HIV vaccine adoption: concerns, motivators, and intentions among persons at risk for HIV. J Acquir Immune Defic Syndr. 2004 Nov 1;37(3):1393–1403. doi: 10.1097/01.qai.0000127064.84325.ad. [DOI] [PubMed] [Google Scholar]
- Rudy Ellen T., Detels Roger, Douglas Wendy, Greenland Sander. Factors affecting hepatitis vaccination refusal at a sexually transmitted disease clinic among men who have sex with men. Sex Transm Dis. 2003 May;30(5):411–418. doi: 10.1097/00007435-200305000-00007. [DOI] [PubMed] [Google Scholar]
- Shavers V. L., Lynch C. F., Burmeister L. F. Knowledge of the Tuskegee study and its impact on the willingness to participate in medical research studies. J Natl Med Assoc. 2000 Dec;92(12):563–572. [PMC free article] [PubMed] [Google Scholar]
- Smith Kimberly Y., Orgain Javette, Scott Robert. Disparities and gaps in HIV research and care. J Natl Med Assoc. 2004 Feb;96(2 Suppl):5S–7S. [PMC free article] [PubMed] [Google Scholar]
- Thomas S. B., Quinn S. C. The Tuskegee Syphilis Study, 1932 to 1972: implications for HIV education and AIDS risk education programs in the black community. Am J Public Health. 1991 Nov;81(11):1498–1505. doi: 10.2105/ajph.81.11.1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walensky Rochelle P., Paltiel A. David, Goldie Sue J., Gandhi Rajesh T., Weinstein Milton C., Seage George R., 3rd, Smith Heather E., Zhang Hong, Freedberg Kenneth A. A therapeutic HIV vaccine: how good is good enough? Vaccine. 2004 Sep 28;22(29-30):4044–4053. doi: 10.1016/j.vaccine.2004.03.059. [DOI] [PubMed] [Google Scholar]


