Abstract
Compelling evidence suggests that major depression is associated with dysfunction of the brain glutamatergic transmission, and that the glutamatergic N-methyl-D-aspartate (NMDA) receptor plays a role in antidepressant activity. Recent postmortem studies demonstrate that depression is associated with altered concentrations of proteins associated with NMDA receptor signaling in the brain. The present study investigated glutamate signaling proteins in the amygdala from depressed subjects, given strong evidence for amygdala pathology in depression. Lateral amygdala samples were obtained from 13-14 pairs of age- sex-, and postmortem-interval matched depressed and psychiatrically healthy control subjects. Concentrations of NR1 and NR2A subunits of the NMDA receptor, as well as NMDA receptor-associated proteins such as postsynaptic density protein-95 (PSD-95) and neuronal nitric oxide synthase (nNOS) were measured by Western immunoblotting. Additionally, levels of enzymes involved in glutamate metabolism, including glutamine synthetase and glutamic acid decarboxylase (GAD-67), were measured in the same amygdala samples. NR2A protein levels were markedly and significantly elevated (+115%, p=0.03) in depressed subjects as compared to controls. Interestingly, PSD-95 levels were also highly elevated (+128%, p=0.01) in the same depressed subjects relative to controls. Amounts of NR1, nNOS, glutamine synthetase, and GAD-67 were unchanged. Increased levels of NR2A and PSD-95 suggest that glutamate signaling at the NMDA receptor in the amygdala is disrupted in depression.
Keywords: NMDA receptor; postsynaptic density protein-95; neuronal nitric oxide synthase; glutamate metabolizing enzymes, amygdala
Introduction
A rapidly growing body of research studies provides evidence that major depressive disorder (MDD) is associated with a dysfunction of the glutamate signaling. Numerous clinical studies demonstrate altered brain indices of glutamate transmission in depressed subjects. Altered brain glutamate or glutamate/glutamine levels have been observed in magnetic resonance spectroscopy (MRS) studies in depressed patients (Auer et al., 2000; Hasler et al., 2007; Michael et al., 2003a; Michael et al., 2003b; Mirza et al., 2004; Pfleiderer et al., 2003; Sanacora et al., 2004) and in serum or plasma of medicated depressed subjects (Altamura et al., 1993; Kim et al., 1982; Mauri et al., 1998). Postmortem brain findings demonstrate a depression-associated reduction in the expression of genes for glutamate transporters (EAAT-1, EAAT-2) and the glutamate synthesizing enzyme, glutamine synthase, in the temporal lobe (Choudary et al., 2005). A role of glutamate in depression is also supported by numerous preclinical studies demonstrating that drugs that alter glutamate signaling have antidepressant activity in laboratory animals, and demonstration of antidepressant-like behavior in transgenic animals lacking specific glutamate receptors (see Pittenger et al., 2007; Witkin et al., 2007 for reviews).
Of multiple receptors for glutamate, the N-methyl-D-aspartate (NMDA) receptor has received the most attention with respect to the biology of depression and its treatment (Kugaya and Sanacora, 2005; Pittenger et al., 2007). The NMDA receptor is a heterooligomeric structure composed of the NR1 subunit, NR2(A-D) subunits, and less common NR3 (A-B) subunits. NMDA receptors are embedded in the postsynaptic density (PSD) of the postsynaptic membrane where they are anchored by PSD-95 and coupled to cytoplasmic signaling molecules, including neuronal nitric oxide synthase (nNOS; Kornau et al., 1995; Sheng and Kim 2002). Activation of NMDA receptors results in Ca2+ entry and subsequent activation nNOS. Human postmortem studies provide evidence that radioligand binding to the NMDA receptor is altered in cerebral cortex from suicide victims and from depressed subjects (Beneyto et al., 2007; Nowak et al.,1995; Nudmamud-Thanoi and Reynolds, 2004). In addition, low levels of nNOS and elevated levels of the NR2C subunit of the NMDA receptor have been reported in the noradrenergic locus coeruleus in MDD (Karolewicz et al., 2004; Karolewicz et al., 2005b). Interestingly, several antagonists of NMDA receptor activation demonstrate antidepressant activity in behavioral models in laboratory animals (Kugaya and Sanacora, 2005). Of particular relevance is the demonstration that ketamine, a NMDA receptor antagonist, exhibits rapid and sustained antidepressant activity in humans (Berman et al., 2000; Zarate et al., 2006). Together, these findings demonstrate compelling evidence that glutamate signaling through the NMDA receptor is disrupted in depression.
In the present study, levels of several proteins involved in glutamate signaling through the NMDA receptor were measured in brain tissue from subjects who had clinically defined depressed mood at the time of death, and psychiatrically normal control subjects. The NMDA receptor signaling proteins chosen for study were relevant subunits of the NMDA receptor (NR1 and NR2A), a major anchoring and scaffolding protein associated with the receptor (PSD-95), and an intracellular signaling protein (nNOS) linked to the receptor. In addition two major glutamate metabolic enzymes glutamine synthetase (GS) and glutamic acid decarboxylase (GAD-67) were investigated. The area of the brain chosen for study was the lateral nucleus of amygdala. The amygdala has long been implicated in the pathobiology of depressive disorders and suicide (Bowley et al., 2002; Cheetham et al., 1989; Drevets et al., 2002; Klimek et al., 2002; Sheline et al., 1998). Glutamatergic inputs from the prefrontal cortex and thalamus enter amygdala at the lateral level (Carmichael and Price, 1995; McDonald, 1998), making this amygdala subregion a key brain region in receiving and processing cortical and thalamic information transmitted via glutamatergic transmission. The NR1 and NR2A subunits were specifically chosen for study because the NMDA receptor in the mature lateral amygdala is largely composed of these two subunits (Lopez de Armentia and Sah, 2003; Radley et al., 2007).
Materials and methods
Psychiatric autopsy and tissue collection
Postmortem brain samples were collected at autopsy from a total of 28 subjects at the Cuyahoga County Coroner's Office in Cleveland, OH. Informed written consent was obtained from the legal next-of-kin of all subjects. Next-of-kin were interviewed and retrospective psychiatric assessments were conducted in accordance with Institutional Review Board policies at Case Western Reserve University and the University of Mississippi Medical Center. A trained interviewer administered the Schedule for Affective Disorders and Schizophrenia: lifetime version (SADS-L) and/or the Structured Clinical Interview for DSM-IV Psychiatric Disorders (SCID-IV) to knowledgeable next-of-kin of subjects in the study.
A total of 14 subjects were studied that had the common feature of depressed mood: 11 subjects met clinical criteria for MDD and 3 subjects met criteria for adjustment disorder with depressed mood based on the Diagnostic and Statistic Manual of Mental Disorders – Revised DSM-IV. One MDD subject had co-existing diagnosis of dysthymic disorder, and one MDD subject had diagnosis of alcohol abuse (Table 1).
Table 1.
Demographic characteristics of subjects
| Parameter | Controls (n=14) | Depressed (n=14) |
| Age (years)* | 53 ± 4 | 54 ± 4 |
| Age range | 27 − 74 | 30 − 73 |
| PMI (hours)* | 18 ± 1 | 19 ± 2 |
| PMI range | 6 − 26 | 5 − 33 |
| pH* | 6.68 ± 0.07 | 6.55 ± 0.07 |
| pH range | 5.99 − 6.96 | 6.15 − 6.91 |
| Time in freezer (months)* |
121 ± 5 | 132 ± 8 |
| Time in freezer range | 81 − 158 | 61 − 181 |
| Gender (F/M) | 1/13 | 1/13 |
| Medication historya | 0/14 | 2/14 (sertraline) |
| Toxicology | Clean, n=7 Drugs detected, n=5 (brompheniramine, lidocaine, diazepam, chlorpheniramine) Ethanol, n=1 CO, n=1 |
Clean, n=8 Drugs detected, n=3 (codeine, phenobarbital, phenytoin) Ethanol, n=1 CO, n=2 |
| Cause of death | Heart disease, n=9 Hypertension, n=1 Aneurysm, n=1 Accidental CO poisoning, n=1 Homicide, n=1 Thrombophlebitis, n=1 |
Suicide, n=12 (shot gun, n=5; CO poisoning, n=3; hanging, n=2; drowning, n=1; slit wrists, n=1), Other causes, n=2 (pulmonary embolism, homicide) |
| Diagnosis | Alcohol dependence, n=1 Phobia (heights), n=1 |
MDD, n=9 MDD and dysthymic disorder, n=1 MDD and alcohol abuse, n=1 Adjustment disorder with depressed mood, n=3 |
| Smoking | Smokers, n=6 History of smoking, n=3 |
Smokers, n=6 History of smoking, n=3 |
PMI, postmortem interval; F, female; M, male; CO, carbon monoxide; MDD, major depressive disorder;
mean ± S.E.M.
Treatment with antidepressants within 4 weeks of time of death. The average ages, PMI, pH and times in freezer of depressed and control subjects were not statistically different.
Fourteen subjects did not meet criteria for Axis I disorder (termed psychiatrically healthy controls) except for nicotine dependence as noted (see Table 1). Among 14 depressed individuals, 12 were suicide victims, and two died due to the other causes such as a homicide or pulmonary embolism (Table 1). Blood and urine samples from all subjects were examined by the coroner's office for psychotropic medications and substances of abuse, including ethanol (Table 1). No antidepressant drugs were detected in the postmortem toxicology screening of subjects in the present study (Table 1). Fourteen depressed subjects and 14 psychiatrically healthy controls were arranged into 14 pairs, matched as closely as possible for age, gender, postmortem interval, tissue pH and smoking history. As specified above, one MDD subject had a diagnosis of alcohol abuse; this subject was matched with an alcohol-dependent control subject with no other psychiatric disorders.
Dissection and anatomical positioning of measurements
Tissue was collected from frozen blocks containing the right amygdaloid complex. Frozen blocks were cut into 50 μm-thick sections for collecting tissue for Western blotting and 20 μm-thick sections for histology. The 20 μm-thick tissue sections collected at 1 mm intervals along the anterior-posterior extent of the amygdala were processed for acetylcholinesterase. Acetylcholinestrease histology (as described previously by Biegon and Wolff, 1986 and Karolewicz et al., 2005a) was used to create anatomical templates for anatomical positioning and as a guide for the dissection of the lateral nucleus. For all subjects, the anatomical position for collection of tissue punches of the lateral amygdala for Western blotting was established approximately midway along the anterior-posterior extent of the amygdala (Figure 1). Tissue punches (diameter 5 mm) containing the lateral nucleus were collected in centrifuge tubes and stored at −80° C until assayed.
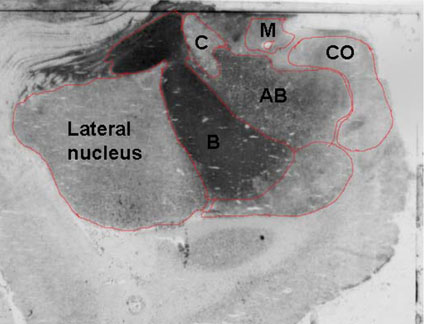
Figure 1.
Digital image of a coronal section of the amygdala stained histochemically for acetylcholinesterase. The acetycholinesterase staining preparation was used to visualize the lateral amygdala and to distinguish it from neighboring nuclei: basal (B), accessory basal (AB), central (C), medial (M), cortical (CO).
Western blotting
Tissue samples were prepared as published previously (Karolewicz et al., 2005b). Samples were homogenized in ice-cold TE buffer (10 mM Tris-HCl and 1 mM ethylene-diaminetetraacetate, EDTA) containing protease inhibitors (Protease Inhibitor Cocktail Tablets - Complete™, Boehringer Mannheim GmbH, Mannheim, Germany). Total protein concentrations for all samples were determined using the bicinchoninic acid (BCA) method (Pierce Biotechnology Inc., Rockford, IL, USA). Samples were mixed with sample buffer (125 mM Tris base, 20% glycerol, 4% SDS, 10% mercaptoethanol, 0.05% bromophenol blue, pH 6.8) and heated at 95°C for 8 min. Solubilized protein (20 μg per lane) was subjected to 10 % Criterion Precast Tris-HCl gel electrophoresis (Bio-Rad Laboratories, Hercules, CA, USA) and transferred to nitrocellulose membranes (Hybond ECL; Amersham Biosciences, Piscataway, NJ, USA). Membrane blots were blocked in 5% non-fat milk/TBS (20 mM Tris base and 0.5 M NaCl, pH 7.5) or 5% non-fat milk/PBS (137 mM NaCl, 2.7 mM KCl, 8 mM Na2HPO4 and KH2PO4, pH 7.4) for 2 h, then incubated (overnight at 4° C) with primary antibody (see Antibodies). Membranes were washed two times for 15 min in TBS (or PBST) buffer and incubated with secondary anti-mouse antibody for NR1, PSD-95, nNOS, glutamine synthetase, actin (diluted 1:2000; Amersham Biosciences, no. NA931) and anti-rabbit secondary antibody for NR2A and beta-tubulin (diluted 1:5000; Amersham Biosciences, no. NA934). After incubation, blots were washed 3 times for 15 min and developed using enhanced chemiluminescence detection (ECL; Perkin-Elmer Life Sciences, Inc., Boston, MA, USA) and immediately exposed to film (Hyperfilm-ECL; Amersham Biosciences).
Antibodies
All antibodies used in this study were commercially available and have been used previously to detect NR1, NR2A, PSD-95, nNOS, GS, and GAD-67 in numerous regions of the human and rat brain as well as in vitro studies (Gerlach et al., 2001; Karolewicz et al., 2004, 2005b, 2008; Ling et al., 2005; Kristiansen et al., 2006; Kronfeld et al., 2000). Mouse monoclonal antibodies were used to label NR1 subunit (1:1000; BD Biosciences/Pharmingen, San Diego, CA, USA; no. 556308), PSD-95 (1:1000; Upstate Biotechnology, Lake Placid, NY, USA; no. 05-494), nNOS (1:1000; BD Biosciences/Transduction Laboratories, Franklin Lakes, NJ, USA; no. 610309), GS (1:1000; BD Biosciences/Transduction Laboratories; no. 610518), and GAD-67 (1:1000; Chemicon, Temecula, CA, USA, no. MAB5406). NR2A subunit was labeled using rabbit polyclonal antibodies diluted 1:500 (Novus Biologicals, Littleton, CO, USA; no. NB 300-105). As a control for transfer and loading, actin or β-tubulin was detected on blots using an anti-actin (Chemicon, no. MAB1501) or anti-tubulin (Abcam Inc., Cambridge, MA, USA; no. ab6046) antibody.
Experimental design and data analysis
Immunoreactivities of glutamate-related proteins were investigated in 13-14 depressed subjects and 13-14 matched normal control subjects. Pairs of subjects were immunoblotted on the same gel (maximum 4-5 pairs) with duplicates on separate gels. In order to minimize inter-blot variability and to aid in quantifying blots, each gel was loaded with 3 concentrations of a cortical tissue standard consisting of 10, 20, and 40 μg of total protein. The tissue standard was dissected from anterior PFC of one control subject and the same cortical tissue standard was used for all experimental gels. Band densities were analyzed using MCID Elite 7.0 (Imaging Research, St. Catherines, Ontario, Canada). Linear regression (GraphPad Prism 4.0) was used to plot a standard curve for each gel, from which relative optical density (ROD) values of samples were converted to cortical standard protein units for each experimental sample for each gel. In order to control for accuracy of tissue loading and efficiency of transfer, data were normalized to actin or tubulin detected on the same blots. The final data are expressed in cortical standard protein units and presented as a ratio of [protein of interest]/[actin or tubulin].
Statistical analyses
Data were analyzed statistically using a two-tailed paired Student's t-test (GraphPad Prism 4.0). Linear regression analysis was performed to test for associations between age, pH, postmortem interval (PMI), time in freezer (TF) and each protein investigated. If a significant correlation between protein immunoreactivities and ones of these variables was observed (p<0.05), analysis of covariance (ANCOVA) was used to correct the test for the effect of diagnosis on the protein expression. Summary statistics are reported as the mean ± S.E.M. A p-value <0.05 was considered significant.
Results
Relationship between optical density and total protein concentration
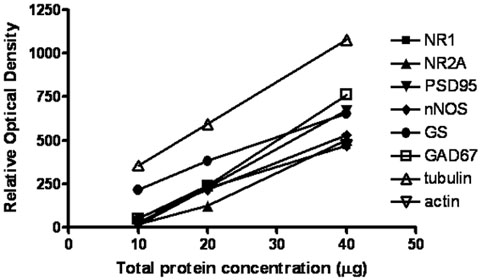
In order to determine the relationship between optical density values and the concentrations of protein immunoreactivities, 10, 20, and 40 μg of total cortical protein (standard) was immunoblotted with all antibodies used in this study. Analyses of blots revealed a linear relationship between optical density values and protein concentrations (Figure 2). All measurements of control and depressed samples fell within the linear range of these standard plots.
Figure 2.
Relationship between the optical density values of Western blotted protein immunoreactivities and total protein concentration for NR1, NR2A, PSD95, nNOS, glutamine synthetase (GS), GAD67, actin, and tubulin. Wells were loaded with three concentrations of cortical standard (dissected from a healthy control subject) consisting of 10, 20, and 40 μg of total protein.
NMDA receptor subunits
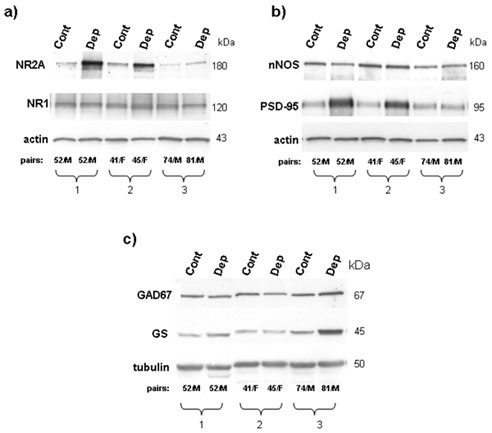
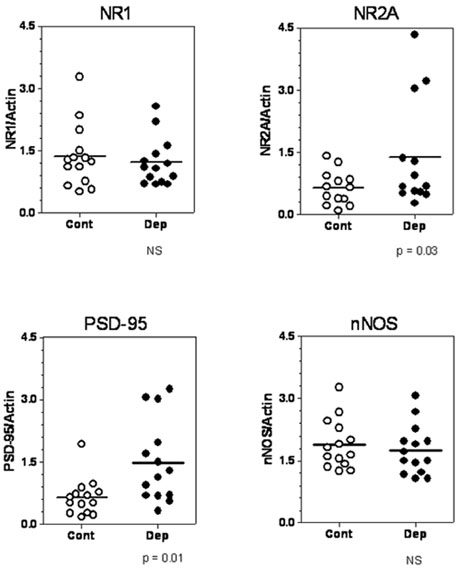
For NMDA receptor subunits, immunoreactive bands corresponding to molecular masses of 120 and 180 kDa for NR1 and NR2A, respectively, were observed in homogenates of lateral amygdala (Figure 3a). Averaged NR1 immunoreactivities from depressive (1.22 ± 0.15) and control subjects (1.36 ± 0.20) were not statistically different (t=1.1, df=13, p=0.28). There were no significant correlations between amounts of NR1 and pH, postmortem interval (PMI), age or time in freezer. The amount of NR2A immunoreactivity from depressed subjects (1.38 ± 0.36) was significantly higher (+115%) than that from control subjects (0.64 ± 0.11; t=2.4; df=12; p=0.03). A significant negative correlation was found between time in freezer and amounts of NR2A immunoreactivity in depressed subjects (r2=0.48, p=0.008). Using ANCOVA with time in freezer as a covariate for NR2A, an effect of diagnosis on this subunit was still detected (p=0.011).
Figure 3.
Immunoblots of NR1, NR2A, and actin (a) nNOS, PSD-95, and actin (b) as well as glutamine synthetase (GS), GAD67, and tubulin (c) from 3 representative pairs of controls (Cont) and depressed subjects (Dep) used in the analysis. Each well was loaded with 20 μg of total protein
NMDA receptor – interacting proteins
PSD-95 and nNOS immunoreactivities appeared as bands with molecular masses of 95 and 160 kDa, respectively (Figure 3b). Averaged PSD-95 immunoreactivities from depressive (1.49 ± 0.26) and control subjects (0.65 ± 0.12) were statistically different (+128 %; t=2.9; df=13; p=0.01; Figure 4). Linear regression analysis showed negative correlations between PMI and amounts of PSD-95 immunoreactivity in controls (r2=0.32; p=0.04) and between time in freezer and PSD-95 immunoreactivity in depressed subjects (r2=0.32; p=0.03). Nevertheless, using ANCOVA with PMI and time in freezer as a covariates, a significant effect of depression for PSD-95 was still detected (p=0.002).
Figure 4.
Amounts of NR1, NR2A, PSD-95, and nNOS immunoreactivities in the lateral amygdala from control subjects (open circles; n=13-14) and depressed subjects (filled circles; n=13-14). Significant increases in the NR2A and PSD-95 immunoreactivities (+115% and +128%, respectively) were observed in depressed subjects as compared to controls. Normalized optical density values for the individual subjects (circles) and mean values (horizontal lines) are presented.
Amounts of nNOS immunoreactivity in depressives (1.75 ± 0.16) and control subjects (1.89 ± 0.16) were not significantly different (t=0.68; df=13; p=0.5). There was a significant negative correlation between PMI and amounts of nNOS immunoreactivity in depressed subjects (r2=0.45; p=0.008). Using ANCOVA with pH as a covariate for nNOS did not change the statistical outcome of the analysis (p=0.998).
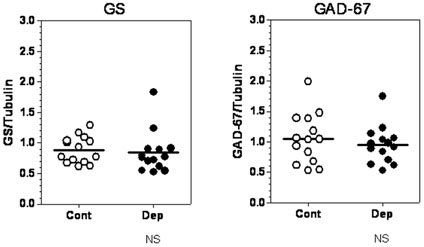
Glutamate metabolizing enzymes
Glutamine synthetase immunoreactivity appeared as a band at 45 kDa (Figure 3c) and amounts of glutamine synthetase immunoreactivity were unchanged in depressed (0.84 ± 0.09) as compared to control subjects (0.89 ± 0.06; t=0.43, df=13; p=0.67; Figure 5). There was a significant positive correlation between pH and amounts of glutamine synthetase immunoreactivity in control subjects (r2=0.36; p=0.02). Using ANCOVA with pH as a covariate for glutamine synthetase, a main effect for diagnosis on glutamine synthetase was not detected (p=0.98). GAD-67 was revealed as a single band at 67 kDa (Figure 3c). Average amounts of GAD-67 immunoreactivity in control subjects (1.05 ± 0.11) and in depressed subjects (0.95 ± 0.08) were not statistically different (t=0.89; df=13; p=0.38; Figure 5). There were no significant correlations between amounts of GAD-67 and pH, age, PMI or TF.
Figure 5.
Amount of glutamine synthetase (GS) and GAD67 immunoreactivity from control subjects (open circles; n=14) and depressed subjects (filled circles; n=14) in the lateral amygdala. Normalized optical density values for the individual subjects (circles) and mean value (horizontal lines) are presented.
Correlations of immunoreactivities
The possibility that amounts of certain proteins in the NMDA receptor signaling cascade would correlate was investigated. Amounts of NR2A immunoreactivity were highly positively correlated with PSD-95 immunoreactivity only in depressed subjects (r2=0.79; p<0.0001). There were no significant correlations between NR2A and nNOS or PSD-95 and nNOS in both control and depressed subjects (data not shown).
Discussion
The present study is the first to analyze the levels of several glutamate signalingrelated biological markers in postmortem amygdala from depressed subjects. Evidence is provided that amounts of the NR2A subunit and its anchoring protein, PSD-95, are robustly elevated in the lateral amygdala of depressed subjects as compared to psychiatrically healthy control subjects. Increased expression of NR2 subunits of the NMDA receptor may be a common pathology in depression since higher levels of the NR2C subunit were previously reported in the noradrenergic locus coeruleus in depressed subjects (Karolewicz et al., 2005b). Interestingly, recent research points to clinical efficacy of NMDA receptor antagonism in depression, i.e. recent clinical studies have shown that a single intravenous dose of ketamine, an NMDA receptor antagonist, produces robust, rapid, and relatively sustained antidepressant effects in treatment-resistance depression (Berman et al., 2000; Zarate et al., 2006). Preclinical research also suggests that inhibition of NMDA receptor, as well as inhibition of intracellular signaling cascades including nNOS that are linked to the NMDA receptor, exhibit antidepressant-like effects in animal screening procedures (Paul, 2001; Paul and Skolnick, 2003). Interestingly, NR2A knockout mice show antidepressant-like profiles in animal models, as compared to wild-type controls (Boyce-Rustay and Holmes, 2006). Moreover, a selective NR2B antagonist Ro25-6981 exhibits antidepressant-like properties in mice (Maeng et al., 2007). A preliminary clinical study has demonstrated the benefit of supplementation with zinc, a non-selective NMDA receptor antagonist, in antidepressant therapy (Nowak et al., 2003). Collectively, current research suggests that the NMDA receptor complex is abnormal in depression and regulation of NMDA receptor signaling in critical brain circuits may represent a strategy for the development of effective and rapid-acting antidepressants.
The abnormalities at the excitatory synapse, as revealed by our postmortem research, may occur in response to abnormal levels of glutamate in depression. Several lines of evidence indicate altered glutamate or glutamate/glutamine levels in multiple brain regions in depressed patients (Auer et al., 2000; Hasler et al., 2007; Michael et al., 2003a; Michael et al., 2003b; Mirza et al., 2004; Pfleiderer et al., 2003; Sanacora et al., 2004). It has been well established that glia play a key role in glutamate neurotransmission, including glutamate metabolism and recycling, therefore depression-associated reductions in the density of these cells in prefrontal cortex (Miguel-Hidalgo et al., 2000; Ongur et al., 1998; Rajkowska et al., 1999; Si et al., 2004) and amygdala (Bowley et al., 2002; Hamidi et al., 2004) may also contribute to altered synaptic glutamate in depression. Glutamine synthetase gene expression has been shown to be reduced in the prefrontal cortex in depression (Choudary et al., 2005), which could also contribute to altered glutamate levels and compensatory changes in glutamate receptors. Since glutamine synthetase is exclusively expressed in astrocytes and a reduced density of astrocytes has been consistently reported in depression (see above); we hypothesized that glutamine synthetase protein immunoreactivity would be reduced in the amygdala. However, the present findings demonstrate unaltered levels of glutamine synthetase in the lateral amygdala in depression. It is conceivable that unchanged levels of glutamine synthetase may indicate (1) unchanged density of astrocytes in the amygdala in depression, (2) a compensatory increase in glutamine synthetase protein expression in remaining astrocytes, or (3) glutamine synthetase expression may be turned on in cells other than astrocytes during depression. One other study has also reported unchanged glutamine synthetase immunoreactivity in the prefrontal cortex in depression (Toro et al., 2006).
Glutamate is an immediate precursor for GABA, and reductions in GABA levels are consistently reported in neuroimaging studies in depression (Hasler et al., 2007; Sanacora et al., 1999; Sanacora et al., 2004). In addition, postmortem analyses demonstrate a significant reduction in the density and size of GABAergic interneurons immunoreactive for calbindin in the dorsolateral prefrontal cortex in depression (Rajkowska et al., 2007). Reduced levels of GAD-67 and GAD-65 were previously reported in cerebellum in major depressive subjects (Fatemi et al., 2005). We expected to find lower GAD-67 protein levels in depression in the present study. However, GAD-67 levels in the lateral amygdala were unchanged in depressed subjects. Further studies aimed to investigate protein levels and/or activity of GAD-65, another isoforms of GAD (Bu et al., 1992) are needed to fully address the status of GABA synthesis in the amygdala in depression.
The NMDA receptor in the mature lateral amygdala is largely composed of the NR1 subunit, a mandatory subunit, and the regulatory NR2A subunit (Lopez de Armentia and Sah, 2003; Radley et al., 2007). To date, few studies have investigated NMDA receptors in postmortem brain from depressed subjects. In this study, NR1 subunit immunoreactivity was unchanged in the amygdala in depression, despite a significant elevation of NR2A subunit immunoreactivity. Unchanged levels of NR1 subunit in amygdala in depression is consistent with our previous observations in the LC and cerebellum of depressed subjects (Karolewicz et al., 2005b) and no changes in NR1 immunoreactivity in subregions of the hippocampal dentate gyrus and in the orbitofrontal cortex (Toro and Deakin, 2005).
Only two previous investigations have measured PSD-95 in brain tissues form depressed subjects. Normal levels in depressed subjects were reported for PSD-95 mRNA in the striatum (Kristiansen and Meador-Woodruff, 2005) and for PSD-95 protein in the hippocampus and orbitofrontal cortex (Toro and Deakin, 2005). In the lateral amygdala, we found markedly elevated levels of PSD-95 in depressives as compared to matched control subjects. These findings suggest that PSD-95 involvement in depression is neuroanatomically limited. PSD-95 belongs to the large family of membrane - associated guanylate kinases (MAGUKs) and is exclusively localized to dendritic spines at glutamatergic synapses (Hunt et al., 1996). PSD-95 binds to the NMDA receptor subunits NR2A and NR2B (Kornau et al., 1995) and also couples synaptic NMDA receptors to downstream signaling molecules such as nNOS (Brenman et al., 1996; Sattler et al., 1999) which serves as an intracellular mediator of NMDA receptor activation. MAGUKs appear to play fundamental role in the transport, anchoring, and signaling of glutamate NMDA receptors. In the present study, the increase in PSD-95 immunoreactivity in depressives was highly correlated with an increase in NR2A subunit immunoreactivity. Hence, the depression-associated elevation in levels of PSD-95 imply increased intracellular trafficking, synaptic delivery, and coupling of the NMDA receptors to intracellular signaling cascades in the amygdala. The lateral amygdala receives its major glutamatergic afferents from the cortical areas and from the thalamus (Mahanty and Sah, 1999). These inputs activate synapses containing both NMDA and non-NMDA receptors. Depression-associated perturbations in markers of glutamate transmission in cortical regions, as revealed by imaging and postmortem cell counting studies (Hasler et al., 2007; Rajkowska et al., 1999; Rajkowska et al., 2005; Sanacora et al., 2004; Si et al., 2004) could result in abnormalities of glutamatergic signaling in cortical projection areas, including the lateral amygdala. Recent imaging studies in depressed humans point to reduced prefrontal cortical function that is linked to increased amygdala activity (Drevets, 1999; Siegle et al., 2007). Elevated levels of NR2A/PSD-95 may reflect an adaptive response to altered cortical input to the amygdala and may contribute to altered amygdala activity in depression.
A shortcoming of the present study is that NMDA receptor subunits were measured as a total pool of proteins that included intracellular pools of unassembled proteins and assembled NMDA receptors expressed at the cell membrane, complicating the prediction of functional significance. However, it has been proposed that the NR1 subunit, which is synthesized in large excess (~10-fold), accounts for most of the intracellular pool (Huh and Wenthold, 1999). The excess production of NR1 increases the chance that NR2 subunits will find NR1 partners. In contrast to NR1, only a small percentage of NR2 subunit protein is intracellular (Huh and Wenthold, 1999); almost all NR2 subunits are expressed on the cell surface. Hence, the total number of functional NMDA receptors appears to be controlled by expression of the NR2 subunits (Prybylowski et al., 2002). Based on this, the elevation of NR2A immunoreactivity in homogenates of lateral amygdala from depressives is likely to reflect an increase of functional surface NMDA receptors. Of course, a depression-associated disruption in the normal cellular trafficking of NMDA receptor subunits cannot be ruled out with the present data.
Treatment of depression may contribute to the adaptive changes seen in the human postmortem brain. This study includes only two subjects with a reported history of medication with antidepressants at some point during their lifetime. In both cases, the selective serotonin reuptake inhibitor, sertraline, was prescribed. However, the presence of this drug was not revealed in the postmortem toxicology screening and both subjects died as a result of suicide (Table 1). One of these two subjects had PSD-95 and NR2A levels unchanged compared to their matched control, while the other subject had levels higher than that of the matched control subject and comparable to the average level of immunoreactivity of depressive subjects lacking the drug exposure. It can be inferred from these observations that the past antidepressant drug treatment is unlikely to contribute to the elevation of PSD-95 or NR2A levels observed in the depressed subjects.
In summary, a marked elevation of NR2A subunit and PSD-95 immunoreactivities in the lateral amygdala of depressed subjects as compared to control subjects were observed. A strong correlation between levels of NR2A subunit and PSD-95 immunoreactivities were observed in depressed subjects. Changes in NR2A and its anchoring protein in depression may reflect an adaptive response to a decreased excitatory input from cortical regions. Further studies of the glutamatergic signaling markers in depression involving non-NMDA ionotropic receptors, metabotropic receptors, and glutamate transporters will lead to a better understanding of the role of glutamate in the pathology of depression.
Acknowledgements
The authors thank John H. Kalbfleisch for assistance in statistical analysis. We gratefully acknowledge the work of Drs James C. Overholser, Herbert Y. Meltzer, Bryan L. Roth, George Jurjus, Ginny Dilley, Lisa Konick, Nicole Herbst and Lesa Dieter in the retrospective psychiatric diagnoses. The excellent assistance of the Cuyahoga County Coroner's Office, Cleveland, OH is greatly appreciated. This publication was supported by RR17701; AFSP (Young Investigator Award to BK); NARSAD (Young Investigator Award to BK), MH63187, MH46692, MH02031, and MH67996.
Statement of Interest
None
References
- Altamura CA, Mauri MC, Ferrara A, Moro AR, D'Andrea G, Zamberlan F. Plasma and platelet excitatory amino acids in psychiatric disorders. American Journal of Psychiatry. 1993;150:1731–1733. doi: 10.1176/ajp.150.11.1731. [DOI] [PubMed] [Google Scholar]
- Auer DP, Putz B, Kraft E, Lipinski B, Schill J, Holsboer F. Reduced glutamate in the anterior cingulate cortex in depression: an in vivo proton magnetic resonance spectroscopy study. Biological Psychiatry. 2000;47:305–313. doi: 10.1016/s0006-3223(99)00159-6. [DOI] [PubMed] [Google Scholar]
- Beneyto M, Kristiansen LV, Oni-Orisan A, McCullumsmith RE, Meador-Woodruff JH. Abnormal glutamate receptor expression in the medial temporal lobe in schizophrenia and mood disorders. Neuropsychopharmacology. 2007;32:1888–1902. doi: 10.1038/sj.npp.1301312. [DOI] [PubMed] [Google Scholar]
- Berman RM, Cappiello A, Anand A, Oren DA, Heninger GR, Charney DS, Krystal JH. Antidepressant effects of ketamine in depressed patients. Biological Psychiatry. 2000;47:351–354. doi: 10.1016/s0006-3223(99)00230-9. [DOI] [PubMed] [Google Scholar]
- Biegon A, Wolff M. Quantitative histochemistry of acetylcholinesterase in rat and human brain postmortem. Journal of Neuroscience Methods. 1986;16:39–45. doi: 10.1016/0165-0270(86)90006-3. [DOI] [PubMed] [Google Scholar]
- Bowley MP, Drevets WC, Ongur D, Price JL. Low glial numbers in the amygdala in major depressive disorder. Biological Psychiatry. 2002;52:404–412. doi: 10.1016/s0006-3223(02)01404-x. [DOI] [PubMed] [Google Scholar]
- Boyce-Rustay JM, Holmes A. Genetic inactivation of the NMDA receptor NR2A subunit has anxiolytic- and antidepressant-like effects in mice. Neuropsychopharmacology. 2006;31:2405–2414. doi: 10.1038/sj.npp.1301039. [DOI] [PubMed] [Google Scholar]
- Brenman JE, Chao DS, Gee SH, McGee AW, Craven SE, Santillano DR, Wu Z, Huang F, Xia H, Peters MF, Froehner SC, Bredt DS. Interaction of nitric oxide synthase with the postsynaptic density protein PSD-95 and alpha1-syntrophin mediated by PDZ domains. Cell. 1996;84:757–767. doi: 10.1016/s0092-8674(00)81053-3. [DOI] [PubMed] [Google Scholar]
- Bu DF, Erlander MG, Hitz BC, Tillakaratne NJ, Kaufman DL, Wagner-McPherson CB, Evans GA, Tobin AJ. Two human glutamate decarboxylases, 65-kDa GAD and 67-kDa GAD, are each encoded by a single gene. Proceedings of the National Academy of Sciences of the United States of America. 1992;89:2115–2119. doi: 10.1073/pnas.89.6.2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmichael ST, Price JL. Limbic connections of the orbital and medial prefrontal cortex in macaque monkeys. Journal of Comparative Neurology. 1995;363:615–641. doi: 10.1002/cne.903630408. [DOI] [PubMed] [Google Scholar]
- Cheetham SC, Crompton MR, Czudek C, Horton RW, Katona CL, Reynolds GP. Serotonin concentrations and turnover in brains of depressed suicides. Brain Research. 1989;502:332–340. doi: 10.1016/0006-8993(89)90629-x. [DOI] [PubMed] [Google Scholar]
- Choudary PV, Molnar M, Evans SJ, Tomita H, Li JZ, Vawter MP, Myers RM, Bunney WE, Jr., Akil H, Watson SJ, Jones EG. Altered cortical glutamatergic and GABAergic signal transmission with glial involvement in depression. Proceedings of the National Academy of Sciences of the United States of America. 2005;102:15653–15658. doi: 10.1073/pnas.0507901102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drevets WC. Prefrontal cortical amygdalar metabolism in major depression. Annals of the New York Academy of Sciences. 1999;877:614–637. doi: 10.1111/j.1749-6632.1999.tb09292.x. [DOI] [PubMed] [Google Scholar]
- Drevets WC, Price JL, Bardgett ME, Reich T, Todd RD, Raichle ME. Glucose metabolism in the amygdala in depression: relationship to diagnostic subtype and plasma cortisol levels. Pharmacology Biochemistry and Behavior. 2002;71:431–447. doi: 10.1016/s0091-3057(01)00687-6. [DOI] [PubMed] [Google Scholar]
- Fatemi SH, Stary JM, Earle JA, raghi-Niknam M, Eagan E. GABAergic dysfunction in schizophrenia and mood disorders as reflected by decreased levels of glutamic acid decarboxylase 65 and 67 kDa and Reelin proteins in cerebellum. Schizophrenia Research. 2005;72:109–122. doi: 10.1016/j.schres.2004.02.017. [DOI] [PubMed] [Google Scholar]
- Gerlach M, Blum-Degen D, Ransmayr G, Leblhuber F, Pedersen V, Riederer P. Expression, but not activity, of neuronal nitric oxide synthase is regionally increased in the alcoholic brain. Alcohol and alcoholism. 2001;36:65–69. doi: 10.1093/alcalc/36.1.65. [DOI] [PubMed] [Google Scholar]
- Hamidi M, Drevets WC, Price JL. Glial reduction in amygdala in major depressive disorder is due to oligodendrocytes. Biological Psychiatry. 2004;55:563–569. doi: 10.1016/j.biopsych.2003.11.006. [DOI] [PubMed] [Google Scholar]
- Hasler G, van der Veen JW, Tumonis T, Meyers N, Shen J, Drevets WC. Reduced prefrontal glutamate/glutamine and gamma-aminobutyric acid levels in major depression determined using proton magnetic resonance spectroscopy. Archives of General Psychiatry. 2007;64:193–200. doi: 10.1001/archpsyc.64.2.193. [DOI] [PubMed] [Google Scholar]
- Huh KH, Wenthold RJ. Turnover analysis of glutamate receptors identifies a rapidly degraded pool of the N-methyl-D-aspartate receptor subunit, NR1, in cultured cerebellar granule cells. Journal of Biological Chemistry. 1999;274:151–157. doi: 10.1074/jbc.274.1.151. [DOI] [PubMed] [Google Scholar]
- Hunt CA, Schenker LJ, Kennedy MB. PSD-95 is associated with the postsynaptic density and not with the presynaptic membrane at forebrain synapses. Journal of Neuroscience. 1996;16:1380–1388. doi: 10.1523/JNEUROSCI.16-04-01380.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karolewicz B, Johnson L, Szebeni K, Stockmeier CA, Ordway GA. Glutamate signaling proteins and tyrosine hydroxylase in the locus coeruleus of alcoholics. Journal of Psychiatric Research. 2008;42:348–355. doi: 10.1016/j.jpsychires.2007.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karolewicz B, Klimek V, Zhu H, Szebeni K, Nail E, Stockmeier CA, Johnson L, Ordway GA. Effects of depression, cigarette smoking, and age on monoamine oxidase B in amygdaloid nuclei. Brain Research. 2005a;1043:57–64. doi: 10.1016/j.brainres.2005.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karolewicz B, Stockmeier CA, Ordway GA. Elevated Levels of the NR2C Subunit of the NMDA receptor in the locus coeruleus in depression. Neuropsychopharmacology. 2005b;30:1557–1567. doi: 10.1038/sj.npp.1300781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karolewicz B, Szebeni K, Stockmeier CA, Konick L, Overholser JC, Jurjus G, Roth BL, Ordway GA. Low nNOS protein in the locus coeruleus in major depression. Journal of Neurochemistry. 2004;91:1057–1066. doi: 10.1111/j.1471-4159.2004.02792.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JS, Schmid-Burgk W, Claus D, Kornhuber HH. Increased serum glutamate in depressed patients. Archiv für Psychiatrie und Nervenkrankheiten. 1982;232:299–304. doi: 10.1007/BF00345492. [DOI] [PubMed] [Google Scholar]
- Klimek V, Schenck JE, Han H, Stockmeier CA, Ordway GA. Dopaminergic abnormalities in amygdaloid nuclei in major depression: a postmortem study. Biological Psychiatry. 2002;52:740–748. doi: 10.1016/s0006-3223(02)01383-5. [DOI] [PubMed] [Google Scholar]
- Kornau HC, Schenker LT, Kennedy MB, Seeburg PH. Domain interaction between NMDA receptor subunits and the postsynaptic density protein PSD-95. Science. 1995;269:1737–1740. doi: 10.1126/science.7569905. [DOI] [PubMed] [Google Scholar]
- Kristiansen LV, Beneyto M, Haroutunian V, Meador-Woodruff JH. Changes in NMDA receptor subunits and interacting PSD proteins in dorsolateral prefrontal and anterior cingulate cortex indicate abnormal regional expression in schizophrenia. Molecular Psychiatry. 2006;11:737–747. doi: 10.1038/sj.mp.4001844. [DOI] [PubMed] [Google Scholar]
- Kristiansen LV, Meador-Woodruff JH. Abnormal striatal expression of transcripts encoding NMDA interacting PSD proteins in schizophrenia, bipolar disorder and major depression. Schizophrenia Research. 2005;78:87–93. doi: 10.1016/j.schres.2005.06.012. [DOI] [PubMed] [Google Scholar]
- Kronfeld I, Kazimirsky G, Lorenzo PS, Garfield SH, Blumberg PM, Brodie C. Phosphorylation of protein kinase Cdelta on distinct tyrosine residues regulates specific cellular functions. Journal of Biological Chemistry. 2000;275:35491–35498. doi: 10.1074/jbc.M005991200. [DOI] [PubMed] [Google Scholar]
- Kugaya A, Sanacora G. Beyond monoamines: glutamatergic function in mood disorders. CNS Spectrums. 2005;10:808–819. doi: 10.1017/s1092852900010403. [DOI] [PubMed] [Google Scholar]
- Ling LL, Hughes LF, Caspary DM. Age-related loss of the GABA synthetic enzyme glutamic acid decarboxylase in rat primary auditory cortex. Neuroscience. 2005;132:1103–1113. doi: 10.1016/j.neuroscience.2004.12.043. [DOI] [PubMed] [Google Scholar]
- Lopez de Armentia M, Sah P. Development and subunit composition of synaptic NMDA receptors in the amygdala: NR2B synapses in the adult central amygdala. Journal of Neuroscience. 2003;23:6876–6883. doi: 10.1523/JNEUROSCI.23-17-06876.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeng S, Zarate CA, Jr., Du J, Schloesser RJ, McCammon J, Chen G, Manji HK. Cellular mechanisms underlying the antidepressant effects of ketamine: role of alpha-amino-3-hydroxy-5-methylisoxazole-4-propionic acid receptors. Biological Psychiatry. Published Online: 20 Jul 2007. DOI:10.1016/j.biopsych.2007.05.028. [DOI] [PubMed]
- Mahanty NK, Sah P. Excitatory synaptic inputs to pyramidal neurons of the lateral amygdala. European Journal of Neuroscience. 1999;11:1217–1222. doi: 10.1046/j.1460-9568.1999.00528.x. [DOI] [PubMed] [Google Scholar]
- Mauri MC, Ferrara A, Boscati L, Bravin S, Zamberlan F, Alecci M, Invernizzi G. Plasma and platelet amino acid concentrations in patients affected by major depression and under fluvoxamine treatment. Neuropsychobiology. 1998;37:124–129. doi: 10.1159/000026491. [DOI] [PubMed] [Google Scholar]
- McDonald AJ. Cortical pathways to the mammalian amygdala. Progress in Neurobiology. 1998;55:257–332. doi: 10.1016/s0301-0082(98)00003-3. [DOI] [PubMed] [Google Scholar]
- Michael N, Erfurth A, Ohrmann P, Arolt V, Heindel W, Pfleiderer B. Metabolic changes within the left dorsolateral prefrontal cortex occurring with electroconvulsive therapy in patients with treatment resistant unipolar depression. Psychological Medicine. 2003a;33:1277–1284. doi: 10.1017/s0033291703007931. [DOI] [PubMed] [Google Scholar]
- Michael N, Erfurth A, Ohrmann P, Arolt V, Heindel W, Pfleiderer B. Neurotrophic effects of electroconvulsive therapy: a proton magnetic resonance study of the left amygdalar region in patients with treatment-resistant depression. Neuropsychopharmacology. 2003b;28:720–725. doi: 10.1038/sj.npp.1300085. [DOI] [PubMed] [Google Scholar]
- Miguel-Hidalgo JJ, Baucom C, Dilley G, Overholser JC, Meltzer HY, Stockmeier CA, Rajkowska G. Glial fibrillary acidic protein immunoreactivity in the prefrontal cortex distinguishes younger from older adults in major depressive disorder. Biological Psychiatry. 2000;48:861–873. doi: 10.1016/s0006-3223(00)00999-9. [DOI] [PubMed] [Google Scholar]
- Mirza Y, Tang J, Russell A, Banerjee SP, Bhandari R, Ivey J, Rose M, Moore GJ, Rosenberg DR. Reduced anterior cingulate cortex glutamatergic concentrations in childhood major depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:341–348. doi: 10.1097/00004583-200403000-00017. [DOI] [PubMed] [Google Scholar]
- Nowak G, Ordway GA, Paul IA. Alterations in the N-methyl-D-aspartate (NMDA) receptor complex in the frontal cortex of suicide victims. Brain Research. 1995;675:157–164. doi: 10.1016/0006-8993(95)00057-w. [DOI] [PubMed] [Google Scholar]
- Nowak G, Siwek M, Dudek D, Zieba A, Pilc A. Effect of zinc supplementation on antidepressant therapy in unipolar depression: a preliminary placebo-controlled study. Polish Journal of Pharmacology. 2003;55:1143–1147. [PubMed] [Google Scholar]
- Nudmamud-Thanoi S, Reynolds GP. The NR1 subunit of the glutamate/NMDA receptor in the superior temporal cortex in schizophrenia and affective disorders. Neuroscience Letters. 2004;372:173–177l. doi: 10.1016/j.neulet.2004.09.035. [DOI] [PubMed] [Google Scholar]
- Ongur D, Drevets WC, Price JL. Glial reduction in the subgenual prefrontal cortex in mood disorders. Proceedings of the National Academy of Sciences of the United States of America. 1998;95:13290–13295. doi: 10.1073/pnas.95.22.13290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul IA. Antidepressant activity and calcium signaling cascades. Human Psychopharmacology. 2001;16:71–80. doi: 10.1002/hup.186. [DOI] [PubMed] [Google Scholar]
- Paul IA, Skolnick P. Glutamate and depression: clinical and preclinical studies. Annals of the New York Academy of Sciences. 2003;1003:250–272. doi: 10.1196/annals.1300.016. [DOI] [PubMed] [Google Scholar]
- Pfleiderer B, Michael N, Erfurth A, Ohrmann P, Hohmann U, Wolgast M, Fiebich M, Arolt V, Heindel W. Effective electroconvulsive therapy reverses glutamate/glutamine deficit in the left anterior cingulum of unipolar depressed patients. Psychiatry Research. 2003;122:185–192. doi: 10.1016/s0925-4927(03)00003-9. [DOI] [PubMed] [Google Scholar]
- Pittenger C, Sanacora G, Krystal JH. The NMDA receptor as a therapeutic target in major depressive disorder. CNS & Neurological Disorders - Drug Targets. 2007;6:101–115. doi: 10.2174/187152707780363267. [DOI] [PubMed] [Google Scholar]
- Prybylowski K, Fu Z, Losi G, Hawkins LM, Luo J, Chang K, Wenthold RJ, Vicini S. Relationship between availability of NMDA receptor subunits and their expression at the synapse. Journal of Neuroscience. 2002;22:8902–8910. doi: 10.1523/JNEUROSCI.22-20-08902.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radley JJ, Farb CR, He Y, Janssen WG, Rodrigues SM, Johnson LR, Hof PR, LeDoux JE, Morrison JH. Distribution of NMDA and AMPA receptor subunits at thalamo-amygdaloid dendritic spines. Brain Research. 2007;1134:87–94. doi: 10.1016/j.brainres.2006.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkowska G, Miguel-Hidalgo JJ, Dubey P, Stockmeier CA, Krishnan KR. Prominent reduction in pyramidal neurons density in the orbitofrontal cortex of elderly depressed patients. Biological Psychiatry. 2005;58:297–306. doi: 10.1016/j.biopsych.2005.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkowska G, Miguel-Hidalgo JJ, Wei J, Dilley G, Pittman SD, Meltzer HY, Overholser JC, Roth BL, Stockmeier CA. Morphometric evidence for neuronal and glial prefrontal cell pathology in major depression. Biological Psychiatry. 1999;45:1085–1098. doi: 10.1016/s0006-3223(99)00041-4. [DOI] [PubMed] [Google Scholar]
- Rajkowska G, O'Dwyer G, Teleki Z, Stockmeier CA, Miguel-Hidalgo JJ. GABAergic neurons immunoreactive for calcium binding proteins are reduced in the prefrontal cortex in major depression. Neuropsychopharmacology. 2007;32:471–482. doi: 10.1038/sj.npp.1301234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanacora G, Gueorguieva R, Epperson CN, Wu YT, Appel M, Rothman DL, Krystal JH, Mason GF. Subtype-specific alterations of gammaaminobutyric acid and glutamate in patients with major depression. Archives of General Psychiatry. 2004;61:705–713. doi: 10.1001/archpsyc.61.7.705. [DOI] [PubMed] [Google Scholar]
- Sanacora G, Mason GF, Rothman DL, Behar KL, Hyder F, Petroff OA, Berman RM, Charney DS, Krystal JH. Reduced cortical gamma-aminobutyric acid levels in depressed patients determined by proton magnetic resonance spectroscopy. Archives of General Psychiatry. 1999;56:1043–1047. doi: 10.1001/archpsyc.56.11.1043. [DOI] [PubMed] [Google Scholar]
- Sattler R, Xiong Z, Lu WY, Hafner M, MacDonald JF, Tymianski M. Specific coupling of NMDA receptor activation to nitric oxide neurotoxicity by PSD-95 protein. Science. 1999;284:1845–1848. doi: 10.1126/science.284.5421.1845. [DOI] [PubMed] [Google Scholar]
- Sheline YI, Gado MH, Price JL. Amygdala core nuclei volumes are decreased in recurrent major depression. Neuroreport. 1998;9:2023–2028. doi: 10.1097/00001756-199806220-00021. [DOI] [PubMed] [Google Scholar]
- Sheng M, Kim MJ. Postsynaptic signaling and plasticity mechanisms. Science. 2002;298:776–780. doi: 10.1126/science.1075333. [DOI] [PubMed] [Google Scholar]
- Si X, Miguel-Hidalgo JJ, O'Dwyer G, Stockmeier CA, Rajkowska G. Agedependent reductions in the level of glial fibrillary acidic protein in the prefrontal cortex in major depression. Neuropsychopharmacology. 2004;29:2088–2096. doi: 10.1038/sj.npp.1300525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegle GJ, Thompson W, Carter CS, Steinhauer SR, Thase ME. Increased amygdala and decreased dorsolateral prefrontal BOLD responses in unipolar depression: related and independent features. Biological Psychiatry. 2007;61:198–209. doi: 10.1016/j.biopsych.2006.05.048. [DOI] [PubMed] [Google Scholar]
- Toro C, Deakin JF. NMDA receptor subunit NRI and postsynaptic protein PSD-95 in hippocampus and orbitofrontal cortex in schizophrenia and mood disorder. Schizophrenia Research. 2005;80:323–330. doi: 10.1016/j.schres.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Toro CT, Hallak JE, Dunham JS, Deakin JF. Glial fibrillary acidic protein and glutamine synthetase in subregions of prefrontal cortex in schizophrenia and mood disorder. Neuroscience Letters. 2006;404:276–281. doi: 10.1016/j.neulet.2006.05.067. [DOI] [PubMed] [Google Scholar]
- Witkin JM, Marek GJ, Johnson BG, Schoepp DD. Metabotropic glutamate receptors in the control of mood disorders. CNS & Neurological Disorders -- Drug Targets. 2007;6:87–100. doi: 10.2174/187152707780363302. [DOI] [PubMed] [Google Scholar]
- Zarate CA, Jr., Singh JB, Carlson PJ, Brutsche NE, Ameli R, Luckenbaugh DA, Charney DS, Manji HK. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Archives of General Psychiatry. 2006;63:856–864. doi: 10.1001/archpsyc.63.8.856. [DOI] [PubMed] [Google Scholar]