Abstract
Objective
To illustrate how the Analytic Hierarchy Process (AHP) can be used to promote shared decision-making and enhance clinician-patient communication.
Methods
Tutorial review.
Results
The AHP promotes shared decision making by creating a framework that is used to define the decision, summarize the information available, prioritize information needs, elicit preferences and values, and foster meaningful communication among decision stakeholders.
Conclusions
The AHP and related multi-criteria methods have the potential for improving the quality of clinical decisions and overcoming current barriers to implementing shared decision making in busy clinical settings. Further research is needed to determine the best way to implement these tools and to determine their effectiveness.
Practice Implications
Many clinical decisions involve preference-based trade-offs between competing risks and benefits. The AHP is a well-developed method that provides a practical approach for improving patient-provider communication, clinical decision-making, and the quality of patient care in these situations.
Keywords: shared decision-making, decision making, doctor-patient communication, analytic hierarchy process, multi-criteria decision making
1. Introduction
To do good work, one must first have good tools
Confucius
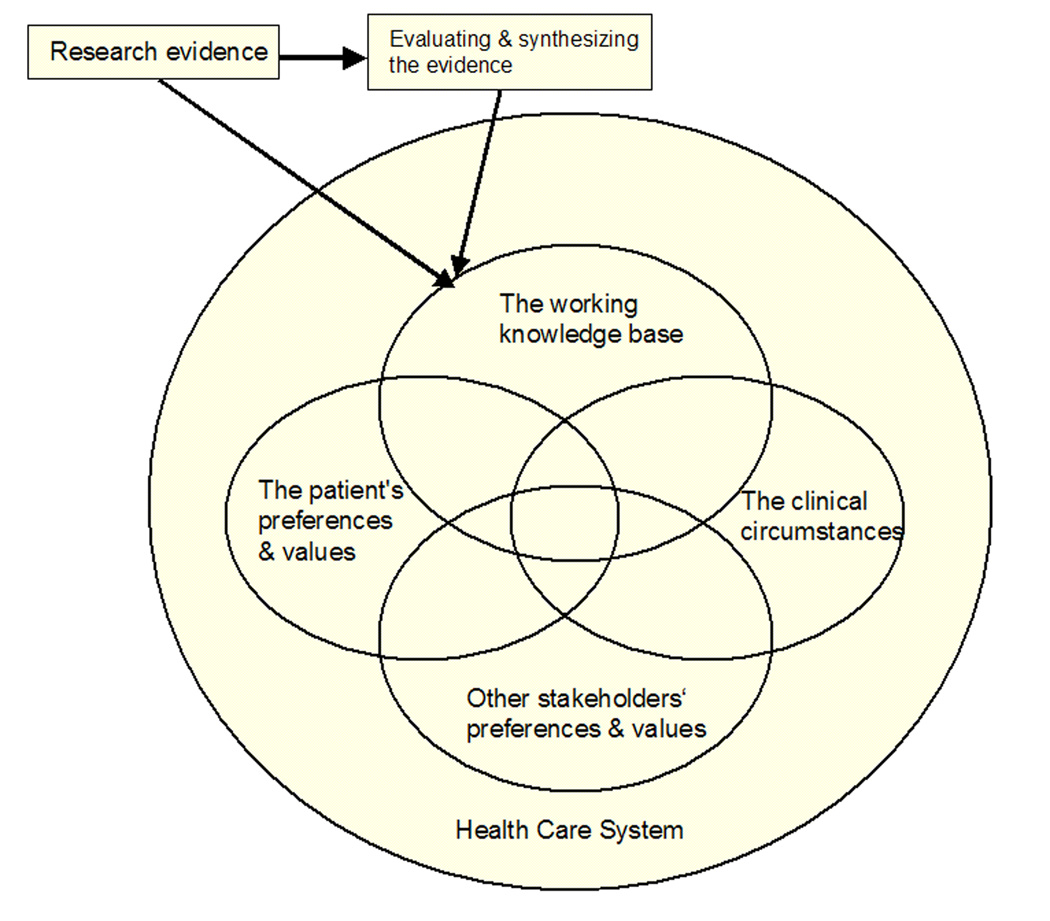
In most current health systems patient management decisions are extremely complex. As illustrated by the diagram in Figure 1, within the constraints imposed by the local health care system, the clinical circumstances, the working knowledge base, the patient’s preferences and values, and the preferences and values of other stakeholders all influence patient care decisions.
Figure 1. A model of clinical decision-making.
Footnote: Adapted from Haynes and Devereaux. 60 Other stakeholders may include: other health care providers, family members, friends, health care system administrators, and health care policy makers. See text for details.
The clinical circumstances include the nature of the problem, its severity and acuity, and the health care setting where the decision is being made. The working knowledge base includes what the patient and the clinician know about the problem and any additional information obtained from other sources. The patient’s preferences and values are most important in situations where there is no clearly preferred course of action (clinical equipoise) 1, but a good argument can be made that they play an important role in every patient management decision. 2–5 Finally, the preferences and values of other involved parties also affect patient management decisions. This group of additional stakeholders always includes the current health care provider and frequently also includes family members and friends.
2. Quality of care
The quality of care delivered within a health system depends on how well individual patients are managed. In the complex environment of modern health care, the best way to promote high quality patient care is to adopt patient-centered approach.
Patient-centered care is consistent with the respect for human dignity and the uniqueness of every individual that underlie contemporary ethical and moral standards of health care. 6–8 There is evidence to suggest that patient-centered care, especially if patients are empowered to take an active part in their care, results in better decisions, improved patient outcomes, enhanced patient and provider satisfaction, and more efficient and effective use of health care resources. 9–14
The five characteristics of patient-centered care defined by Mead and Bower are shown in Table 1. 15, 16 An important component of this model is the sharing of power and responsibility between doctor and patient or, in other words, shared decision-making. 15–17
Table 1.
| The biopsychosocial perspective |
| Understanding the patient as a person in his or her own right |
| Sharing power and responsibility between doctor and patient |
| Building a therapeutic alliance (relationship) |
| Understanding the doctor as a person, not merely a skilled technician |
3. Shared decision-making
Shared decision making has been defined as “…a collaborative endeavor in which patient and physician share not only information and intuitions but the making of decisions.” 5 Essential elements of a shared decision making process are summarized in Table 2. 18 The clinical decision makers need to arrive at a joint understanding of the goal, the available options, and how to identify which option is best. They also need to assess and compare their preferences regarding any necessary tradeoffs and to integrate all of these considerations into a mutually agreeable decision that can then be carried out. Clearly, effective communication among all those involved is crucial for the clinical implementation of the shared decision-making process.
Table 2.
Steps in a shared decision making process & the AHP
| Shared decision making * | Analytic Hierarchy Process |
|---|---|
| Definition of the problem & options available | Create a decision model that contains the decision goal, the options being considered, and the criteria used to determine how well the options are likely to meet the goal |
| Review of options’ pros and cons | Pairwise comparisons regarding how well the options satisfy the criteria |
| Elicitation of patient values and preferences | Pairwise comparisons to prioritize factors affecting the decision (the decision criteria) |
| Clinician recommendations | Review results using the clinician’s perspective |
| Review of patient’s ability to implement plan | Include feasibility as a decision criterion |
| Check for clarity and understanding | Detailed review of model results, sensitivity analyses if indicated |
| Make a decision or defer until later | Use results to inform the decision making process |
Adapted from [18]
4. Implementing patient-centered care and shared decision-making
Both patient-centered care and shared decision-making are relatively new concepts that are not fully integrated into the organizational culture of many health care settings. There are several well-known barriers to implementing shared decision-making including the complexity of the task, lack of time 19, and missing information. 1, 20
The standard approach to promoting clinical shared decision-making has been the development and use of patient decision aids. Patient decision aids have been shown to improve patient knowledge, satisfaction, and participation in the decision making process. 21 However they are not well suited for actively facilitating communication between the clinician, the patient, and other involved stakeholders about all essential elements of a decision. To effectively implement clinical shared decision-making, it is especially important to identify and discuss differences in values and preferences and their effect on medical decisions because we know that in many cases the decision priorities of doctors and patients differ. 22–24 The development of methods that will promote efficient and effective communication among all involved stakeholders is, therefore, a high priority topic for shared decision-making research.
5. Multi-criteria decision making
There is good evidence that people have difficulty making consistently good decisions when faced with unfamiliar problems involving value-based trade-offs between the advantages and disadvantages of two or more options. 25, 26 Many medical decisions meet this description. To help people make better decisions in these circumstances, a number of multi-criteria decision-making methods have been developed. These techniques are specifically designed to help people make better choices that are consistent with their preferences and values. They are especially useful in situations that involve two or more decision makers, a mixture of tangible and intangible considerations, or both. 27, 28 As shown in Table 2, the steps involved in using a multi-criteria method are analogous to the essential elements of a shared decision making process. This similarity suggests that multi-criteria methods can be used as the basis for a new generation of clinical decision support systems that will facilitate the clinical implementation of high quality shared decision-making.
6. The Analytic Hierarchy Process
The Analytic Hierarchy Process (AHP) is perhaps the most well known and widely used multi-criteria method. It has firm theoretical underpinnings and has been used successfully to help people make better decisions in a wide variety of complex circumstances. 29–32 A main strength of the AHP is that it is both methodologically sound and user-friendly. Its ease of use is due to a unique combination of design characteristics. The AHP frames a decision as a hierarchy, an organizational framework many people are already familiar with and easy to explain to those who are not. All inputs consist of comparisons between just two decision elements at a time; pairwise comparisons like these are generally considered to be one of the best ways to elicit judgments from people. 33 The output is easy to understand because it is based on simple scales derived from the pairwise comparisons. Finally, there is a built-in measure of the consistency of the judgments being made which both checks the reliability of the analysis and reduces the chance of making a procedural mistake.
7. Performing an AHP analysis
An AHP analysis consists of the six steps listed in Table 3.
Table 3.
Steps in the Analytic Hierarchy Process
| 1. | Define the decision elements: |
| • goal of the decision, | |
| • the options, and | |
| • the criteria for determining how well the options meet the goal. | |
| 2. | Construct decision model |
| 3. | Decompose the decision into smaller parts |
| • Compare importance of criteria in achieving goal | |
| • Compare alternatives’ abilities to meet the criteria | |
| 4. | Synthesis: How well can alternatives be expected to meet goal? |
| 5. | Sensitivity analysis |
| 6. | Make decision or refine the analysis |
To illustrate the process, imagine that a decision needs to be made about which of three drugs – Drug A, Drug B, or Drug C – is the best option for initial treatment of a chronic medical condition. The information you have available is summarized in Table 4.
Table 4.
Drug comparison information
| Drug | Risk of side effects |
Ease of administration |
Effectiveness | Monthly price |
|---|---|---|---|---|
| A | 1% | 1 tablet twice a day | 85% | $5 * |
| B | 5% | 1 tablet daily * | 90% * | $50 |
| C | 0.5% * | 1 tablet daily * | 75% | $25 |
Preferred option for each criterion.
7.1. Define the decision elements and the working knowledge base
The first step consists of two parts. The first is to define the elements of the decision: the goal, the options to be considered, and the criteria that will be used to determine how well the options meet the goal. The second part consists of examining the working knowledge base to see if there is a dominant option that is clearly better than the others across all of the decision criteria.
Let’s assume that the decision makers agree that the goal is to pick the best initial treatment, the four criteria contained in the table will be used to compare the options, and the only options to be considered at this time are Drugs A, B, and C. A review of the working knowledge base contained in the table reveals that in this case there is no dominant option: Drug A is best in terms of cost, Drug B is best in terms of effectiveness, and Drug C is best in terms of safety. Thus, choosing a drug will involve making tradeoffs between decision criteria and a full multi-criteria analysis needs to be performed.
7.2. Construct the decision model
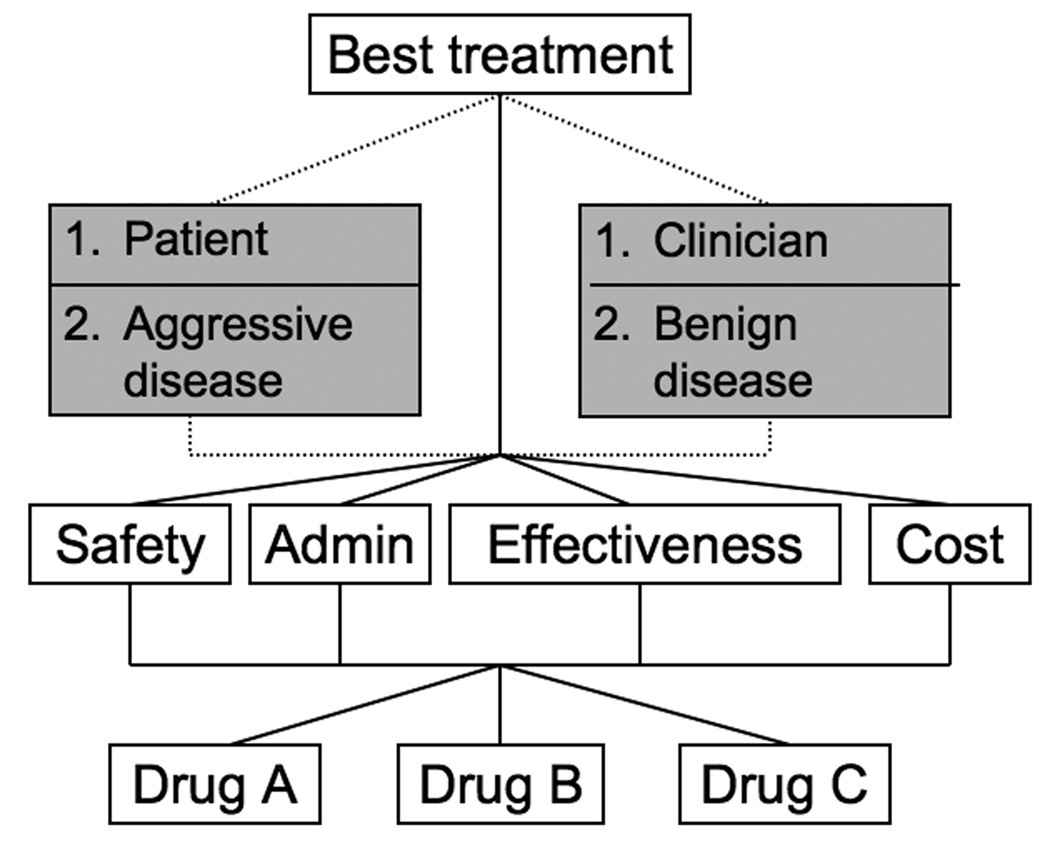
The next step is to arrange the decision elements into a hierarchy. The model for the example is shown in the unshaded parts of Figure 2. The goal is at the top, the options at the bottom, and the criteria in between. (The shaded level will be used later to illustrate variations in how the model can be used to explore different scenarios.)
Figure 2. AHP decision model with optional variations showing different perspectives and how to explore the effects of uncertainty.
Footnote: The basic AHP model is shown in the clear boxes on levels 1, 3 and 4. The model can be enlarged to explore the effects of different perspectives by performing separate analyses from different points of view. This is illustrated by adding the upper part of the shaded boxes on level two. In this model separate analyses would be performed from the perspective of both the patient and the clinician. Similarly the model can be enlarged to explore the effects of future uncertainty. This is illustrated using the lower part of the shaded boxes on level 2. This model would compare the options under two different scenarios: benign disease and aggressive disease. See text for further details. Abbreviations: Admin = Ease of Administration.
7.3. Decompose and make pairwise comparisons to determine local priorities
The decision is analyzed by dividing it into smaller parts and making comparisons between the decision elements on lower levels of the hierarchy relative to each of the elements on the next higher level. Every possible pair of lower-level elements is compared; each set requires n(n-1) comparisons.
All comparisons are made using the procedure summarized in Table 5. The decision maker is first asked if the two elements being compared are equally important, likely, or preferred relative to the referent element on the next higher level of the hierarchy. (The specific wording of the question is chosen so it is appropriate for the comparison being made.) If they are equal, no further input is needed. If one is better, the decision maker indicates how much more important, likely, or preferable they think it is. These relative judgments can be done numerically, verbally, or graphically. Examples of each format are included in the table. After the judgments are completed, they are converted to a 1–9 scale and entered into a comparison matrix.
Table 5.
The AHP pairwise comparison process
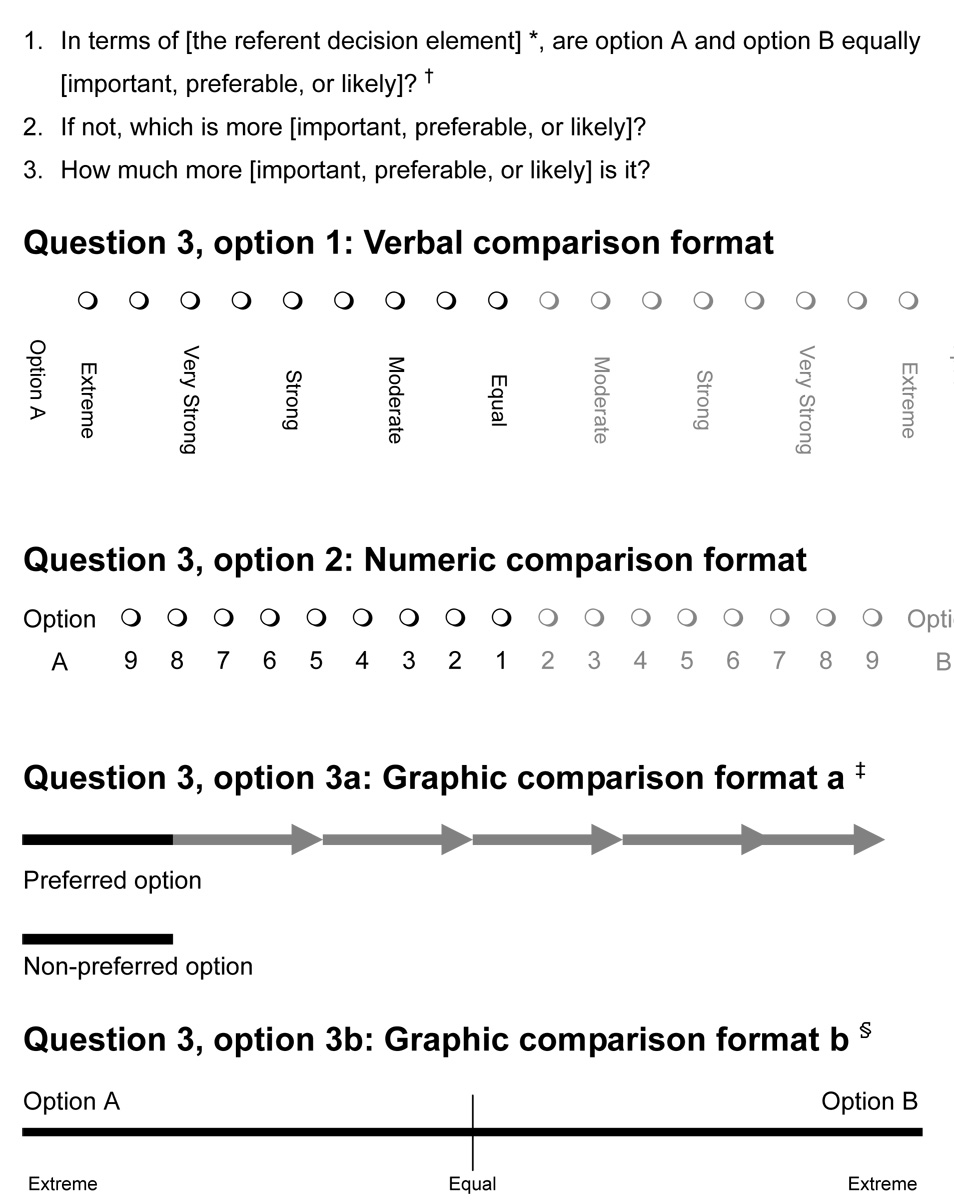 |
 |
The referent decision element refers to the element on the next higher level of the hierarchy that is serving as the basis for the comparisons.
The comparison term is chosen to fit the context.
In option 3a, as illustrated by the sequential arrows, the length of the top line representing the preferred option is extended until its length, relative to the line representing the less-preferred option.
In option 3b, a vertical line is made to the left or right of the midline to indicate which option is preferred and the degree of preference.
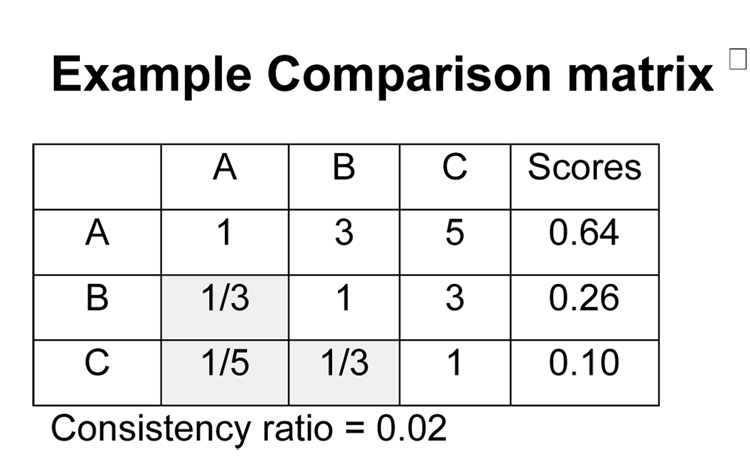
This matrix shows the results of comparing decision elements A, B, and C. The cells indicate the comparison of the row element versus the column element. Direct comparisons are entered in the upper right triangle. Reciprocals are used to fill the corresponding cells in the shaded left lower triangle.
The comparison matrix is used to determine the relative abilities of the compared elements to satisfy the referent criterion or goal. The standard method is to calculate the normalized right principal eigenvector of the matrix. This matrix algebra procedure is conceptually equivalent to taking the mean of the direct and indirect relationships among the comparisons contained within the matrix. The eigenvector is calculated by raising the matrix to successive powers and is then normalized. Detailed descriptions of how to perform this calculation and several approximate methods have been published previously and are available from the author on request. 34 The result is a ratio scale that indicates how well each compared element satisfies the referent criterion or goal. Because the scale is normalized, all scores add to 1 or 100%.
When all the pairwise comparisons are completed, scales have been created that indicate the relative priorities of the criteria in meeting the goal, the priorities of any sub-criteria in satisfying parent criteria, and how well the options satisfy the criteria. These results are illustrated in Table 6, which shows the results of comparisons made among the alternatives and criteria of our example.
Table 6.
Results of example pairwise comparison process. *
| Risk of side effects (0.31) |
Ease of admin (0.16) |
Effectiveness (0.36) |
Price (0.20) |
Score Distrib synthesis |
Score Ideal synthesis |
|
|---|---|---|---|---|---|---|
| Drug A | 0.31 | 0.25 | 0.37 | 0.60 | 39.5% | 38.0% |
| Drug B | 0.19 | 0.375 | 0.41 | 0.12 | 29.2% | 30.6% |
| Drug C | 0.50 | 0.375 | 0.24 | 0.28 | 31.3% | 31.4% |
| CR | 0.02 | 0.00 | 0.00 | 0.04 | 0.01 | 0.01 |
The numbers in parentheses under the criteria indicate their priorities relative to the goal. The numbers in the columns indicate the judged relative abilities of the three options to meet the criteria. Abbreviations: Ease of admin = ease of administration; CR = consistency ratio; distrib = distributive
In addition to creating the scale, the comparison matrix is used to calculate a measure of the consistency of the judgments it contains called the consistency ratio. Consistency refers to the property that if X is judged two times more important than Y, and Y is judged two times more important than Z, then, X should be judged four times more important than Z. The AHP does not require perfectly consistent judgments but, to ensure the reliability of the analysis, they should be close. The consistency ratio compares the consistency of the judgments within the matrix with those of a completely random matrix. Consistency ratios range between 0 and 1, with 0 indicating perfect consistency. The standard definition of acceptable consistency is a consistency ratios ≤ 0.10. In certain applied settings, a ratio ≤ 0.20 is acceptable. 35 The consistency ratios for the example comparisons are listed in Table 6.
7.4. Synthesis
The next step is to combine the scales created through the pairwise comparisons to determine how well the options can be expected to meet the goal. There are two methods for doing this: distributive synthesis and ideal synthesis.
If the objective of the analysis is to rank order the options, the distributive method is used. Data regarding the options and criteria are combined using a weighted additive model that is analogous to the formula for calculating a weighted average.
If the objective is to identify a single best option, the ideal method is used. In this case, the best option for each criterion is given the full weight of the criterion and the other options are weighted proportionally. The resulting ideal weights are then combined with the criteria priorities using a weighted additive model identical to the one used in the distributive synthesis mode. Examples of both synthesis modes are shown in Table 6.
7.5. Sensitivity analysis
If desired, it is then possible to do a range of sensitivity analyses to determine how different judgments or assumptions affect the analysis.
7.6. Make a decision
The last step is to either make a decision or go back and refine the analysis until everyone is satisfied that a decision can be made.
8. Variations
The explicit approach provided by the AHP makes it possible to examine how different viewpoints affect the results. For example, when there are multiple decision makers involved, it is possible to create separate analyses for each person and compare the results. Adding the upper shaded part of Figure 2 to the basic model shows how the medical treatment model could be structured to show the priorities and preferences of the patient and the clinician separately. This approach can identify areas where patients and clinicians disagree and determine how the differences impact the results of the decision. In this way, important areas for further exploration and dialog can be identified.
Future uncertainties can be addressed by comparing the results of scenarios that vary the likelihoods of different outcomes. An example of this type of decision model is shown in the lower shaded part of Figure 2.
Many additional variations are possible. Interested readers are directed to collections of AHP models published by Saaty and others for additional information. 36 More specific examples of how the AHP can be used to discuss treatment options with a patient and to create and disseminate practice guidelines within a health system have been published previously. 37, 38
9. The AHP and Medical Decision Making
The AHP has been successfully applied to a variety of clinical decisions. Figure 3 shows the model used in our first study that involved asking patients and physicians to complete an AHP analysis. In the days before therapeutic endoscopy, we interviewed patients who were hospitalized for upper gastrointestinal bleeding and a group of primary care physicians. Both groups completed a full AHP analysis using a laptop computer. We found that the doctors and the patients disagreed about the decision priorities. While both groups indicated that avoiding a poor outcome was the most important consideration, the patients thought that identifying the cause of bleeding was next most important whereas the doctors thought avoiding test complications was. A second major finding was that it was not hard for ordinary patients and physicians to complete successfully a moderately complex AHP analysis. 23
Figure 3. AHP gastrointestinal bleeding diagnosis model. 23.
The next study tested the hypothesis that patients can successfully use the AHP to analyze a realistically complex clinical decision. We asked a group of patients recruited from a medical clinic population to complete an AHP analysis regarding colorectal cancer screening for patients with a family history of colorectal cancer. Once again, we found that the majority of patients were able to complete the analysis with little difficulty and were overwhelmingly positive about the experience. 39
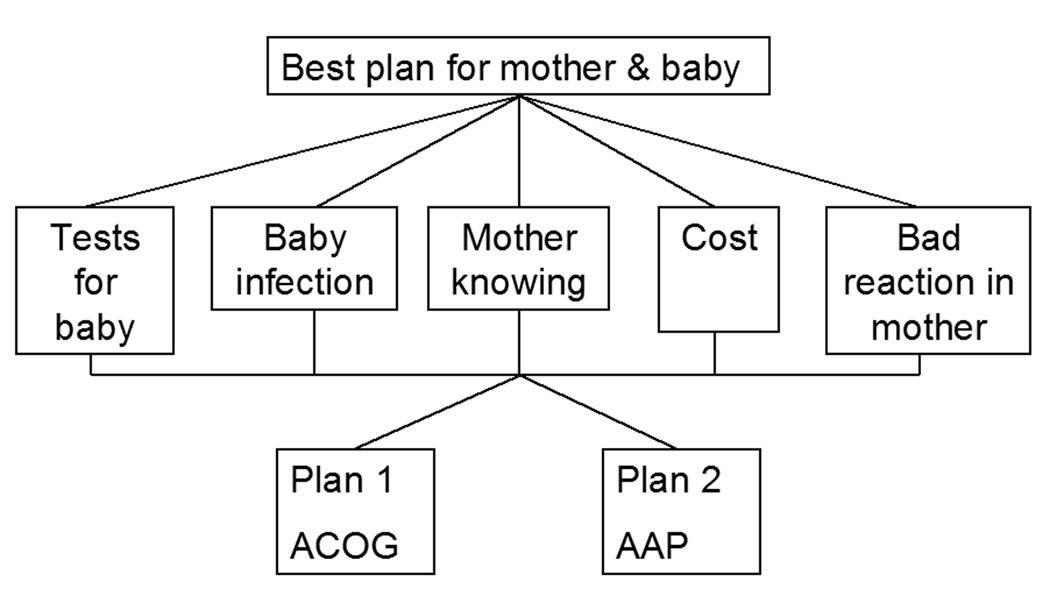
The findings of these two early studies were then confirmed in a study that compared the opinions of obstetricians, pediatricians, and pregnant women regarding two different guidelines for the prevention of neonatal group B streptococcal infections – one issued by the American College of Obstetrics and Gynecology and the other by the American Academy of Pediatrics. The model used for this study is shown in Figure 4. The priorities of all three groups differed. The obstetricians favored the obstetric guideline and the mothers and pediatricians favored the pediatric guidelines, but for different reasons. Once again, both the mothers, who were from a high-risk obstetric clinic population, and the doctors were able to complete the analysis with little trouble and were very positive about the experience. 24
Figure 4. AHP Management of neonatal group B streptococcal sepsis model. 24.
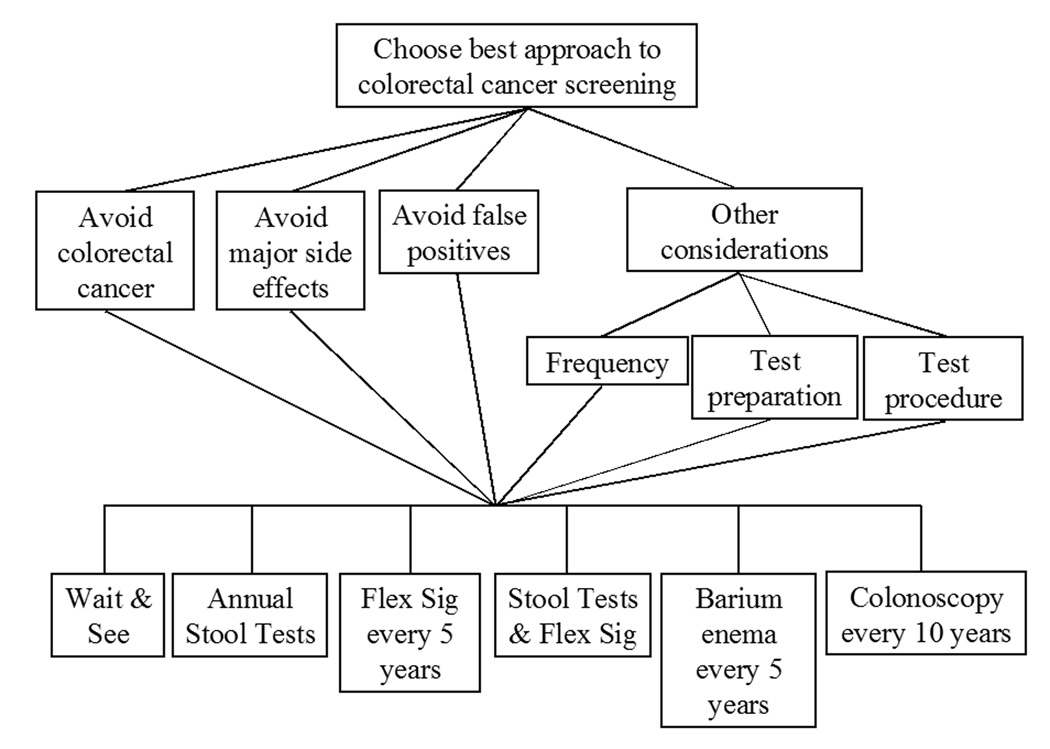
Our next study compared an AHP-based patient decision aid for colorectal cancer screening with a simple educational intervention in a randomized controlled trial. 40 The model used in this study is shown in Figure 5. Patients in the AHP group had lower decisional conflict scores, implying a better decision-making process. The majority of patients in the AHP group was able to complete the analysis without difficulty and indicated that they liked the experience and thought it should be used routinely. There were no differences, however, in subsequent screening-related outcomes. Because physicians’ recommendations have a strong influence on colorectal cancer screening41–44, this finding may have been due to the lack of decision support given to the physicians of the patients who were in the study.
Figure 5. AHP model used in colorectal cancer screening decision aid study. 40.
Other patient-based applications of the AHP that are currently being developed include a decision aid to help women who have had a caesarian section decide whether to attempt a vaginal birth for a subsequent delivery and AHP-based surveys of patient preferences for rehabilitative treatments. 45–48 The AHP has also been used to address a variety of health care planning and administrative issues. 49, 50 A comprehensive review of the AHP in medical and health care decision making has been published recently. 51
10. Current Research Issues
10.1 AHP theory
Over the past 20 years numerous studies have addressed various aspects of AHP theory. Earlier questions about the validity of the technique have been largely resolved. 31 Currently, the most important practical questions relevant to the use of the AHP to support medical decision-making are whether it is possible to speed up the process without compromising the results and if the assumptions that justify the use a hierarchical model are appropriate.
In addition to the Analytic Hierarchy Process there is a more general application of the theory called the Analytic Network Process (ANP). Instead of a hierarchy, the ANP uses a network model structure. This change makes it possible to make fewer assumptions in the analysis but requires even more pairwise comparisons. 52, 53 It is currently unknown whether the benefits of the ANP approach outweigh the additional effort required.
10.2. Can the AHP help patients and other clinical decision makers manage the emotional aspects of medical decisions?
Many medical decision making situations provoke powerful emotional responses. Recent research has shown that emotions can influence decision-making and sometimes cause decision makers to make choices that are inconsistent with their values and preferences. 54
The use of the AHP may help people mitigate the deleterious effects of emotions on decision making. Because the AHP can readily incorporate intangible considerations into the decision making model, emotional factors can be defined and explicitly incorporated into the decision making process. It is also possible that simply making the decision making process more explicit, transparent, and deliberate will reduce the negative influence of emotions on clinical decisions. Investigation of the interplay between decision aiding interventions and the emotional aspects of medical decision-making is a high priority area for future research.
10.3. The role of other multi-criteria methods
In addition to the AHP and the ANP, there are a number of other multi-criteria methods that use different strategies to accomplish the same goals. They vary in complexity, format, and theoretical basis. 27, 28 Little is known about the comparative effectiveness of these methods for supporting shared medical decision-making.
10.4. Implementation
Another issue is how to implement multi-criteria-based decision aids. One question is how to best integrate them into the clinical flow of events. Another is whether the results of single decision support method are reliable enough to adequately inform decision-making for high-stakes decisions. Some authors have argued that, for truly important decisions, multiple methods should be used to make sure they all yield the same results – a process called plural analysis. 55, 56 Whether this is needed for important medical decisions is currently unknown.
10.5. Do the benefits justify the costs?
Finally, it is not known how much value is gained by using sophisticated multi-criteria methods instead of less complicated decision aids. 57 A related issue is whether every decision requires an expensive customized decision aid or if a more generic decision aid that can be easily adapted for a range of similar problems will work just as well. Because most currently used evaluation tools primarily address the outcome of the decision making process but not the process itself 58, 59, resolution of these issues will require the development of better methods for comparing the effects of different decision support methods on the clinical decision making process.
11. Discussion and Conclusion
11.1 Discussion
Shared medical decision making is an essential element of high quality patient care. Effectively implementing shared decision making in clinical settings will require the use of tools that enable patients, clinicians, and other involved decision makers to communicate effectively about the nature of the decision, the information available, the considerations that should be incorporated into the decision making process, values, preferences, and trade-offs. There is a close match between these tasks and the capabilities of the AHP and other multi-criteria methods.
11.2 Conclusion
The promising results obtained so far in applying the AHP to clinical problems suggest that the AHP and similar methods can be used to create decision aids that will simplify and expedite the shared decision making process, supply the information medical decision makers need in a format they can use, and help persuade reluctant doctors, patients and health care systems that shared decision making is an effective, efficient, and feasible approach to providing patients with care of the highest quality.
11.3 Practice implications
Many clinical decisions involve preference-based trade-offs between competing risks and benefits. The AHP and other multi-criteria decision-making methods are well-developed tools that provide a practical approach for improving the quality of clinician-patient communication, clinical decision-making, and the patient care in these situations.
Acknowledgements
Support for this project was provided by grant 1R01CA112366-01A1 from the National Cancer Institute. The National Cancer Institute had no other involvement in this study. The author is indebted to the anonymous reviewer of this manuscript for their helpful comments and suggestions and to the organizers of the Freiburg 4th International Shared Decision Making Conference for the invitation to give this talk. The author has no conflicts of interest regarding this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Elwyn G, Edwards A, Kinnersley P, Grol R. Shared decision making and the concept of equipoise: the competences of involving patients in healthcare choices. Brit J Gen Pract. 2000;50:892–899. [PMC free article] [PubMed] [Google Scholar]
- 2.Street R. Aiding medical decision making: A communication perspective. Med Decis Making. 2007;27:550–553. doi: 10.1177/0272989X07307581. [DOI] [PubMed] [Google Scholar]
- 3.Forrow L, Wartman S, Brock D. Science, ethics, and the making of clinical decisions. Implications for risk factor intervention. J Amer Med Assoc. 1988;259:3161–3167. [PubMed] [Google Scholar]
- 4.Berwick D. A user's manual for the IOM's "Quality Chasm" report. Health Aff. 2002;21 doi: 10.1377/hlthaff.21.3.80. [DOI] [PubMed] [Google Scholar]
- 5.Whitney SN, McGuire AL, McCullough LB. A Typology of Shared Decision Making, Informed Consent, and Simple Consent. Ann Intern Med. 2004;140:54. doi: 10.7326/0003-4819-140-1-200401060-00012. [DOI] [PubMed] [Google Scholar]
- 6.Snyder L, Leffler C. Ethics Manual. Ann Intern Med. 2005;142:560–582. doi: 10.7326/0003-4819-142-7-200504050-00014. [DOI] [PubMed] [Google Scholar]
- 7.American Medical Association. [Accessed December 19, 2007];Principles of Medical Ethics. at http://www.ama-assn.org/ama/pub/category/2498.html.
- 8.Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National academy of sciences; 2001. [Google Scholar]
- 9.Kaplan S, Greenfield S, Ware J. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27:S110–S127. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 10.Bodenheimer T, Wagner E, Grumbach K. Improving primary care for patients with chronic illness. The chronic care model ,part 2. J Amer Med Assoc. 2002;288:1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 11.Little P, Everitt H, Williamson I, et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. Brit Med J. 2001;323:908–911. doi: 10.1136/bmj.323.7318.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O'Connor AM, Wennberg JE, Legare F, et al. Toward The 'Tipping Point': Decision Aids And Informed Patient Choice. Health Aff. 2007;26:716–725. doi: 10.1377/hlthaff.26.3.716. [DOI] [PubMed] [Google Scholar]
- 13.Michie S, Miles J, Weinman J. Patient-centredness in chronic illness: what is it and does it matter? Patient Educ Couns. 2003;51:197–206. doi: 10.1016/s0738-3991(02)00194-5. [DOI] [PubMed] [Google Scholar]
- 14.Epstein R, Street R. Bethesda, MD: National Cancer Institute; Patient-centered communication in cancer care: Promoting healing and reducing suffering. NIH publication No. 07-6225. 2007
- 15.Duggan PS, Geller G, Cooper LA, Beach MC. The moral nature of patient-centeredness: is it "just the right thing to do"? Patient Educ Couns. 2006;62:271–276. doi: 10.1016/j.pec.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 16.Mead N, Bower P. Patient-centred consultations and outcomes in primary care: a review of the literature. Patient Educ Couns. 2002;48:51–61. doi: 10.1016/s0738-3991(02)00099-x. [DOI] [PubMed] [Google Scholar]
- 17.Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196:129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 18.Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006;60:301–312. doi: 10.1016/j.pec.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 19.Gravel K, Legare F, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: a systematic review of health professionals' perceptions. Implement Sci. 2006;1:16. doi: 10.1186/1748-5908-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elwyn G, Edwards A, Gwyn R, Grol R, Fretheim A. Towards a feasible model for shared decision making: focus group study with general practice registrars. Brit Med J. 1999;319:753–756. doi: 10.1136/bmj.319.7212.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.O'Connor A, Fiset V, Rostom A, et al. Decision aids for people facing health treatment or screening decisions. The Cochrane Library. 2006;(Issue 4) doi: 10.1002/14651858.CD001431. [DOI] [PubMed] [Google Scholar]
- 22.Montgomery A, Fahey T. How do patients' treatment preferences compare with those of clinicians? Qual Saf Health Care. 2001;10:i39–i43. doi: 10.1136/qhc.0100039... [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dolan JG, Bordley DR, Miller H. Diagnostic strategies in the management of acute upper gastrointestinal bleeding: patient and physician preferences. J Gen Intern Med. 1993;8:525–529. doi: 10.1007/BF02599632. [DOI] [PubMed] [Google Scholar]
- 24.Peralta-Carcelen M, Fargason CA, Jr., Coston D, Dolan JG. Preferences of pregnant women and physicians for 2 strategies for prevention of early-onset group B streptococcal sepsis in neonates. Arch Pediatr Adolesc Med. 1997;151:712–718. doi: 10.1001/archpedi.1997.02170440074013. [DOI] [PubMed] [Google Scholar]
- 25.Redelmeier D, Shafir E. Medical decision making in situations that offer multiple alternatives. J Amer Med Assoc. 1995;273:302–305. doi: 10.1001/jama.1995.03520280048038. [DOI] [PubMed] [Google Scholar]
- 26.Russo J, Schoemaker P. Decision Traps. 1st ed. New York: Doubleday; 1989. [Google Scholar]
- 27.Belton V, Stewart T. Multiple Criteria Decision Analysis. Boston/Dordrecht/London: Kluwer Academic Publishers; 2002. [Google Scholar]
- 28.Figueira J, Greco S, Ehrgott M, editors. State of the art surveys. New York: Springer; 2005. Multiple Criteria Decision Analysis. [Google Scholar]
- 29.Golden B, Wasil E, Harker P. Applications and studies. Berlin: Springer-Verlag; 1989. The Analytic Hierarchy Process. [Google Scholar]
- 30.Zahedi F. The analytic hierarchy process - A survey of the method and its applications. Interfaces. 1986;16:96–108. [Google Scholar]
- 31.Forman E, Gass S. The Analytic Hierarchy Process - An Exposition. Operations Research. 2001;49:469–486. [Google Scholar]
- 32.Vaidya OS, Kumar S. Analytic hierarchy process: An overview of applications. European Journal of Operational Research. 2006;169(1):1–29. [Google Scholar]
- 33.Reynolds T, Jolly J. Measuring personal values: An evaluation of alternative methods. Journal of Marketing Science. 1980;17:531–536. [Google Scholar]
- 34.Dolan JG, Isselhardt BJ, Jr., Cappuccio JD. The analytic hierarchy process in medical decision making: a tutorial. Med Decis Making. 1989;9:40–50. doi: 10.1177/0272989X8900900108. [DOI] [PubMed] [Google Scholar]
- 35.Forman E, Selly M. Decision by objectives. Hackensack, NJ: World Scientific; 2001. [Google Scholar]
- 36.Saaty T, Forman E. The hierarchon: A dictionary of hierarchies. Pittsburgh: RWS Publications; 1992. [Google Scholar]
- 37.Dolan JG, Bordley DR. Involving patients in complex decisions about their care: an approach using the analytic hierarchy process. J Gen Intern Med. 1993;8:204–209. doi: 10.1007/BF02599268. [DOI] [PubMed] [Google Scholar]
- 38.Dolan JG, Bordley DR. Using the analytic hierarchy process (AHP) to develop and disseminate guidelines. QRB Qual Rev Bull. 1992;18:440–447. doi: 10.1016/s0097-5990(16)30570-x. [DOI] [PubMed] [Google Scholar]
- 39.Dolan JG. Are patients capable of using the analytic hierarchy process and willing to use it to help make clinical decisions? Med Decis Making. 1995;15:76–80. doi: 10.1177/0272989X9501500111. [DOI] [PubMed] [Google Scholar]
- 40.Dolan J, Frisina S. Randomized controlled trial of a patient decision aid for colorectal cancer screening. Med Decis Making. 2002;22:125–139. doi: 10.1177/0272989X0202200210. [DOI] [PubMed] [Google Scholar]
- 41.Kelly KM, Dickinson SL, Degraffinreid CR, Tatum CM, Paskett ED. Colorectal cancer screening in 3 racial groups. Am J Health Behav. 2007;31:502–513. doi: 10.5555/ajhb.2007.31.5.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Teng EJ, Friedman LC, Green CE. Determinants of colorectal cancer screening behavior among Chinese Americans. Psycho-Oncology. 2006;15:374–381. doi: 10.1002/pon.958. [DOI] [PubMed] [Google Scholar]
- 43.Klabunde CN, Schenck AP, Davis WW. Barriers to colorectal cancer screening among Medicare consumers. Am J Prev Med. 2006;30:313–319. doi: 10.1016/j.amepre.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 44.Seeff LC, Nadel MR, Klabunde CN, et al. Patterns and predictors of colorectal cancer test use in the adult U.S. population. Cancer. 2004;100:2093–2103. doi: 10.1002/cncr.20276. [DOI] [PubMed] [Google Scholar]
- 45.Eden K, Perrin N, Dolan J, Rosenberg D, Sharma P, Guise J. Use of a childbirth decision aid encourages women to reconsider decisions; Abstract presented at Annual Meeting Society for Medical Decision Making; Pittsburgh, PA. 2007. [Google Scholar]
- 46.Sharma P, Eden K, Dolan J, Jimison H, Guise J. Multi-criteria decision analyses for a childbirth after cesarean decision; Abstract presented at Annual Meeting Society for Medical Decision Making; Pittsburgh, PA. 2007. [Google Scholar]
- 47.Hummel JM, Snoek GJ, van Til JA, van Rossum W, Ijzerman MJ. A multicriteria decision analysis of augmentative treatment of upper limbs in persons with tetraplegia. J Rehabil Res Dev. 2005;42:635–644. doi: 10.1682/jrrd.2004.07.0088. [DOI] [PubMed] [Google Scholar]
- 48.van Til JA, Renzenbrink GJ, Dolan JG, Ijzerman MJ. The use of the analytic hierarchy process to aid decision making in acquired equinovarus deformity. Arch Phys Med Rehabil. 2008;89:457–462. doi: 10.1016/j.apmr.2007.09.030. [DOI] [PubMed] [Google Scholar]
- 49.Sloane E, Liberatore M, Nydick R. Medical decision support using the analytic hiearchy process. Journal of Healthcare Information Management. 2002;16:38–43. [PubMed] [Google Scholar]
- 50.Hariharan S, Dey P, Chen DHM, Kumar A. Application of the analytic hierarchy process for measuring and comparing the global performance of intensive care units. J Crit Care. 2005;20:117–124. doi: 10.1016/j.jcrc.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 51.Libertore M, Nydick R. The analytic hierarchy process in medical and health care decision making: A literature review. European Journal of Operational Research. 2008;189:194–207. [Google Scholar]
- 52.Saaty T. The Analytic Network Process: Decision Making With Dependence and Feedback. Pittsburgh: RWS Publications; 2001. [Google Scholar]
- 53.Saaty T. The Analytic Hierarchy and Analytic Network Processes for the Measurement of Intangible Criteria and for Decision Making. In: Figueira J, Greco S, Ehrgott M, editors. Multiple Criteria Decision Analysis State of the Art Surveys. New York: Springer Science+Business Media, Inc.; 2005. [Google Scholar]
- 54.Shafir E, LeBoeuf R. Rationality. Annu Rev Psychol. 2003;53:491–517. doi: 10.1146/annurev.psych.53.100901.135213. [DOI] [PubMed] [Google Scholar]
- 55.Phillips L. A theory of requisite decision models. Acta Psychologica. 1984;56:29–48. [Google Scholar]
- 56.Brown R. Rational choice and judgment. Hoboken, NJ: J Wiley & Sons; 2005. [Google Scholar]
- 57.Williams M, Dennis A, Stam A, Aronson J. The impact of DSS use and information load on errors and decision quality. European Journal of Operational Research. 2007;176:468–481. [Google Scholar]
- 58. [Accessed 9/25/07];Evaluation measures, Ottawa Decision Support Framework. at http://decisionaid.ohri.ca/eval.html#ChoicePredisposition. [Google Scholar]
- 59.Nelson WL, Han PK, Fagerlin A, Stefanek M, Ubel PA. Rethinking the objectives of decision aids: a call for conceptual clarity. Med Decis Making. 2007;27:609–618. doi: 10.1177/0272989X07306780. [DOI] [PubMed] [Google Scholar]
- 60.Haynes R, Devereaux P. Pysicians' and patients' choices in evidence based practice. Brit Med J. 2002;324:1350. doi: 10.1136/bmj.324.7350.1350. [DOI] [PMC free article] [PubMed] [Google Scholar]