Abstract
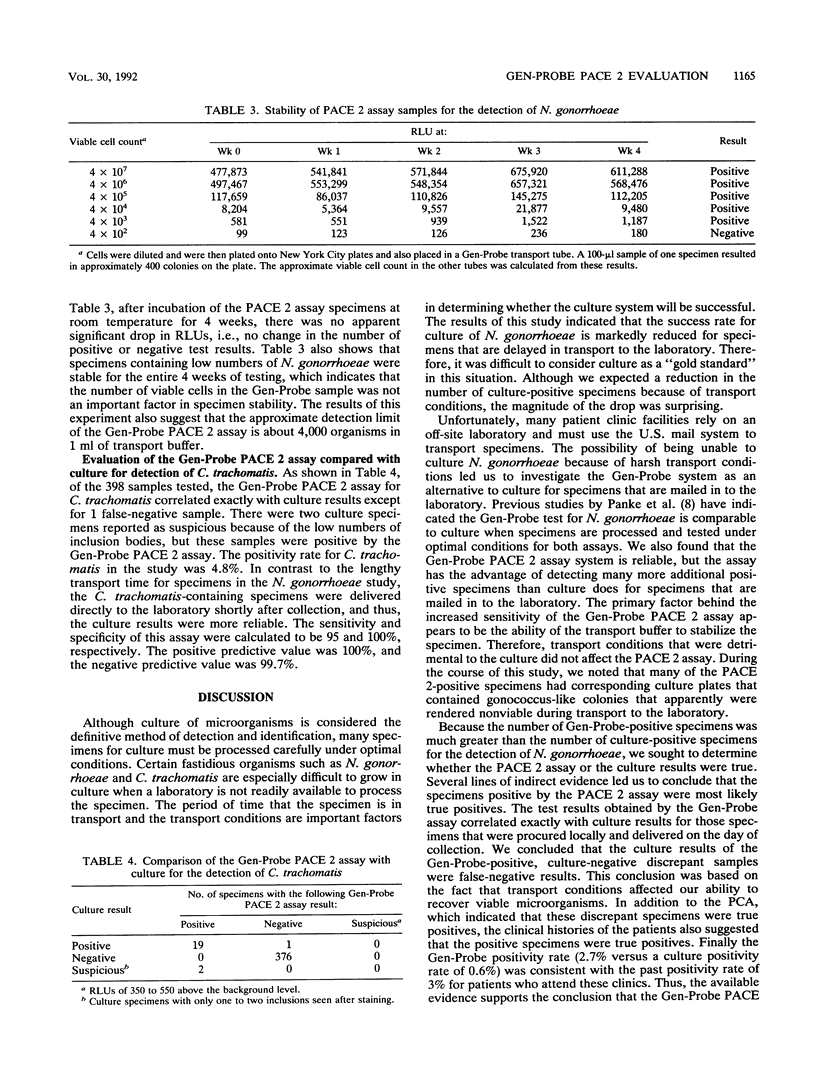
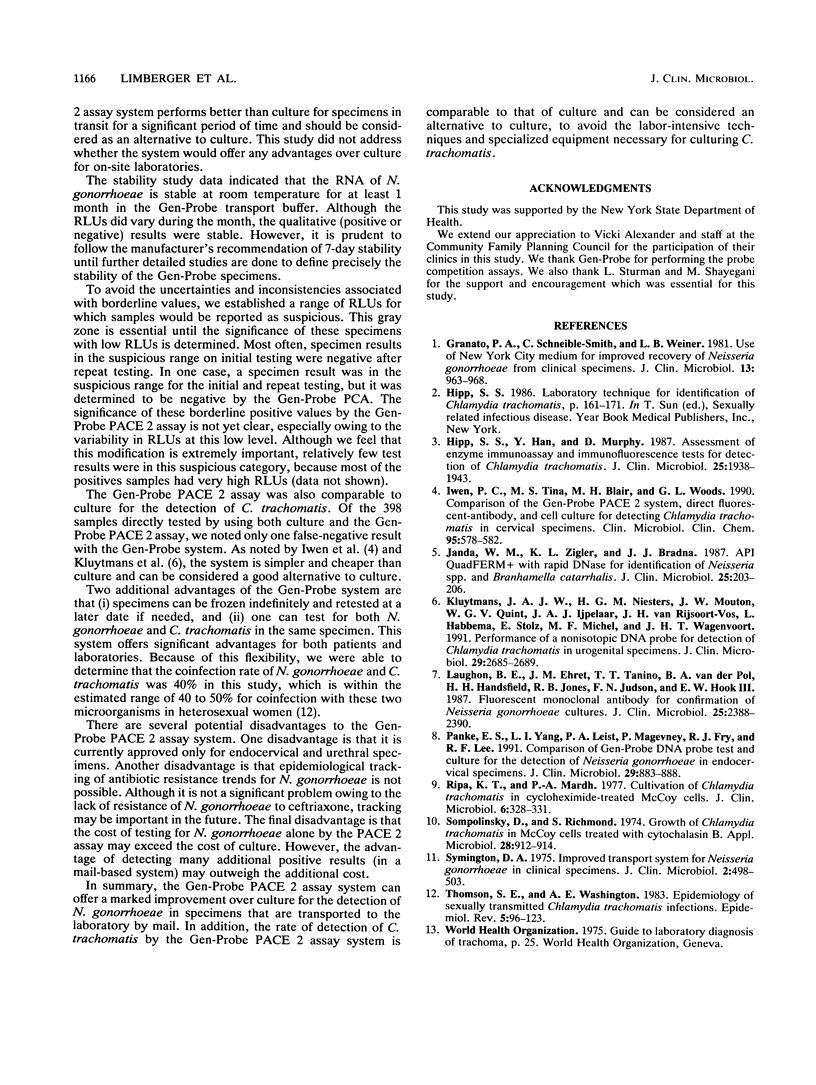
The Gen-Probe PACE 2 assay (Gen-Probe Inc., San Diego, Calif.) was compared with culture for the detection of Neisseria gonorrhoeae in endocervical specimens that were mailed to the laboratory. During mail transport, the specimens were exposed to extremes of hot and cold weather for several days before arriving in the laboratory. Specimens on culture plates deteriorated during transport, as evidenced by many dead gonococcus-like colonies. The manufacturer's recommendation for reporting PACE 2 assay-positive results was modified to create a suspicious category for samples with relative light units near the positive cutoff value. Of a total of 4,869 specimens tested, 30 were positive by both methods and 102 were positive only by the PACE 2 assay. These additional 102 positive specimens were likely to be true positives, as indicated by several lines of indirect evidence, including detailed probe competition analysis, patient history, and the lack of false-positive results in hand-delivered specimens. Although Gen-Probe Inc. indicates that specimens are stable for up to 7 days, N. gonorrhoeae was easily detectable by the PACE 2 assay after 1 month of incubation at room temperature in the PACE 2 transport buffer. We also compared the Gen-Probe PACE 2 assay for Chlamydia trachomatis with culture on endocervical specimens delivered by same-day courier. Of 398 endocervical specimens tested, the PACE 2 assay detected 19 of 20 culture-positive samples. Although the assay failed to detect one culture-positive sample, it was able to detect two very weak culture-suspicious samples. Finally, PACE 2 assays for N. gonorrhoeae and C. trachomatis performed on the same samples indicated that the coinfection rate was 40% for women attending five family planning clinics. We concluded that the Gen-Probe PACE 2 assay system should be considered for use in testing those specimens that are transported to the laboratory through the mail.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Granato P. A., Schneible-Smith C., Weiner L. B. Use of New York City medium for improved recovery of Neisseria gonorrhoeae from clinical specimens. J Clin Microbiol. 1981 May;13(5):963–968. doi: 10.1128/jcm.13.5.963-968.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hipp S. S., Han Y., Murphy D. Assessment of enzyme immunoassay and immunofluorescence tests for detection of Chlamydia trachomatis. J Clin Microbiol. 1987 Oct;25(10):1938–1943. doi: 10.1128/jcm.25.10.1938-1943.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwen P. C., Blair T. M., Woods G. L. Comparison of the Gen-Probe PACE 2 system, direct fluorescent-antibody, and cell culture for detecting Chlamydia trachomatis in cervical specimens. Am J Clin Pathol. 1991 Apr;95(4):578–582. doi: 10.1093/ajcp/95.4.578. [DOI] [PubMed] [Google Scholar]
- Janda W. M., Zigler K. L., Bradna J. J. API QuadFERM+ with rapid DNase for identification of Neisseria spp. and Branhamella catarrhalis. J Clin Microbiol. 1987 Feb;25(2):203–206. doi: 10.1128/jcm.25.2.203-206.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kluytmans J. A., Niesters H. G., Mouton J. W., Quint W. G., Ijpelaar J. A., Van Rijsoort-Vos J. H., Habbema L., Stolz E., Michel M. F., Wagenvoort J. H. Performance of a nonisotopic DNA probe for detection of Chlamydia trachomatis in urogenital specimens. J Clin Microbiol. 1991 Dec;29(12):2685–2689. doi: 10.1128/jcm.29.12.2685-2689.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laughon B. E., Ehret J. M., Tanino T. T., Van der Pol B., Handsfield H. H., Jones R. B., Judson F. N., Hook E. W., 3rd Fluorescent monoclonal antibody for confirmation of Neisseria gonorrhoeae cultures. J Clin Microbiol. 1987 Dec;25(12):2388–2390. doi: 10.1128/jcm.25.12.2388-2390.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panke E. S., Yang L. I., Leist P. A., Magevney P., Fry R. J., Lee R. F. Comparison of Gen-Probe DNA probe test and culture for the detection of Neisseria gonorrhoeae in endocervical specimens. J Clin Microbiol. 1991 May;29(5):883–888. doi: 10.1128/jcm.29.5.883-888.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ripa K. T., Mårdh P. A. Cultivation of Chlamydia trachomatis in cycloheximide-treated mccoy cells. J Clin Microbiol. 1977 Oct;6(4):328–331. doi: 10.1128/jcm.6.4.328-331.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sompolinsky D., Richmond S. Growth of Chlamydia trachomatis in McCoy cells treated with cytochalasin B. Appl Microbiol. 1974 Dec;28(6):912–914. doi: 10.1128/am.28.6.912-914.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Symington D. A. Improved transport system for Neisseria gonorrhoeae in clinical specimens. J Clin Microbiol. 1975 Dec;2(6):498–503. doi: 10.1128/jcm.2.6.498-503.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson S. E., Washington A. E. Epidemiology of sexually transmitted Chlamydia trachomatis infections. Epidemiol Rev. 1983;5:96–123. doi: 10.1093/oxfordjournals.epirev.a036266. [DOI] [PubMed] [Google Scholar]


