Abstract
Despite 40 years of research demonstrating the efficacy of antihypertensive medications for lowering blood pressure and decreasing cardiovascular disease, hypertension control rates worldwide remain low. We explored here how both medication efficacy rates and patient/physician decision-making (discontinuation rates) affect overall hypertension control rates. To do this we introduced the use of Kaplan–Meier methodology to predict hypertension control rates separately within age strata. An important aspect of our analysis is the use of a “treatment intensity score,” including both the number of agent(s) and the percentage of maximal dose of agent(s). We investigated how blood pressure control rates vary with age, gender, and treatment intensity. Our analysis found that both efficacy and discontinuation rates at different treatment intensities vary with age and gender, so that for each increase in age by 1 decade, the log hazard of achieving controlled blood pressure at any given intensity decreases by 0.10 in men and 0.20 in women. Overall hypertension control rates ranged from 80.8% for persons age 15 to 39 years to only 42.1% for persons age ≥80 years. Our analysis more accurately represents achievable hypertension control rates, with differences by gender, than previous work, because we investigated the contributions of efficacy and treatment aggressiveness in the control of hypertension.
Keywords: hypertension, survival analysis, antihypertensive medication, aging, gender
Despite 40 years of studies demonstrating the impact of lowering blood pressure (BP) on decreasing cardiovascular disease,1–5 hypertension control rates worldwide remain disturbingly low.6–9 Impediments to achieving good BP control include both physician-related factors10–14 and patient-related factors, especially noncompliance.15–22 A question of great interest in hypertension research is the declining rate of control seen with increasing age of patients.23
There are, as yet, many unanswered questions. What is the maximum achievable hypertension control rate with our present BP treatment strategies? Are there age- and gender-specific differences in the ability to achieve BP control? No hypertension treatment trial has ever demonstrated 100% success in the control of even mild hypertension. With clinicians being graded more and more on outcomes,24 it is critical to know how successful they can expect to be in achieving BP control. In our study, we do not investigate the efficacy of individual antihypertensive compounds but rather we apply Kaplan–Meier (K-M) methods and Cox regression models25,26 in a unique way to estimate the efficacy of overall treatment strategy as a function of baseline characteristics.
Methods
Study Population
The study includes patients with BP measurements taken at the hypertension clinic in the Mayo Clinic Division of Hypertension from September 2001 to July 2003. The time interval chosen corresponded with a period where the composition of the physicians, nurses, and patient mix was constant. The details of this database have been described previously27 In brief, patient data were collected from the Mayo Clinic Hypertension Continuity Care Data-base, an electronic database that is a part of the care of hypertensive patients in the Mayo Clinic Division of Hypertension.
Two patient populations are present in this study. One group consists of patients who have long-standing hypertension, and hypertension specialists at Mayo Clinic provide their primary and hypertension care. Thus, this study includes a significant component of primary care patients. The second group consists of those referred for difficult-to-control hypertension and secondary forms of hypertension. The study population as a whole has a higher prevalence of secondary forms of hypertension (eg, renovascular disease) and more difficult-to-manage essential hypertension than typically would be seen in a primary care setting. Patients in both groups frequently have multiple comorbidities complicating their hypertension management, such as diabetes, coronary artery disease, or renal failure. All of the patients whose data were analyzed for this study had ≥1 visit with ≥2 standardized measurements of BP and gave consent to use their medical charts for research. The institutional review board of Mayo Clinic approved the protocol and methods of this study.
Definition of Treatment Intensity
Information on antihypertensive medications and dosages was gathered at the time of the visit and stored in a clinical database in the Mayo Clinic Division of Hypertension. Analyses were restricted to those patients with both antihypertensive medication information and BP information and to those patients who gave permission to use medical information for research. A total of 64 pill formulations were observed composed of 51 unique chemical compounds (some pills contained 2 chemical substances). All of the compounds were recorded with their dosage and daily frequency information at the time of clinical visit (for further information, see Appendix 1 in the online supplement for this article at http://hyper.ahajournals.org).
To allow for comparability of drug regimens across patients taking many different medications, we calculated a treatment intensity score at the time of visit using the January 2004 Monthly Prescribing Reference to determine the maximum recommended daily dose for each medication. The recorded daily dose taken by the patient was divided by the maximum recommended daily dose to obtain a proportional dose for that medication. For example, a patient taking a 40-mg daily dose of a drug for which 200 mg was the “maximum daily dose” was considered to be taking 0.2 “intensity” units. For completeness, dual-class drugs were separated into their components, and intensities were calculated separately for each of the chemical compounds. These proportional doses from individual medications were summed within person on a given visit to determine a patient’s “treatment intensity” at that visit.
Statistical Methods
We propose the use of survival analysis techniques to estimate not death, but 2 underlying events: the distribution of the treatment intensity at which efficacy is first achieved, ie, a hypertensive patient “just” becomes controlled, and the distribution of the treatment intensity at which a physician or patient “just” chooses to discontinue further increasing the intensity, despite not achieving control. We call the first distribution the “efficacy” distribution and the second distribution the “discontinuation” distribution. The discontinuation distribution is an indirect measure of the combined willingness of both physician and patient to not continue advancing treatment intensity.
The data that we observed are treatment intensities at a given visit and the corresponding BPs, which we will simply categorize as “in control” or “not in control.” We define control as a systolic BP measurement <140 mm Hg and a diastolic BP measurement <90 mm Hg. We must assume that these data represent the steady state of a long-term process of trying to achieve BP control in each patient (ie, that patients are sufficiently far along in their treatment process). Furthermore, we assume that treatment intensity is progressively increased until either the patient is in control or the patient and/or physician decide to discontinue further increases in treatment (and accept the present level of BP). It is assumed that accepted norms for BP control are in place and represent universal minimal goals for all patients.
The crucial idea for the application of survival analysis methodology is to consider treatment intensity, although observed in a cross-sectional manner, as the time variable. That is, for each patient and at each visit we observe 2 pieces of information, both the treatment intensity and the corresponding BP control status. Furthermore, we make the following assumptions, as described below.
First, if the patient is in control, we assume that the patient is on the minimum treatment intensity at which control can be achieved. Thus, we have observed an “efficacy event” at that observed treatment intensity. Second, if the patient is not in control, then all we know about the true minimum intensity for “achieving control” is that it would be larger than the observed value of intensity (ie, it is a right-censored efficacy event). Third, if the patient is not in control, then we assume that we have observed the maximum intensity to which the physician and patient are willing to increase treatment. That is, we have observed a “discontinuation event” at that intensity, whereby no further increases would be attempted. Fourth, if the patient is in control, then we know only that the patient and physician did not discontinue further treatment increases before that observed intensity. Because control (defined as BP <140/90 mm Hg) was achieved, we do not know how much higher of an intensity would have been considered to lower BP or required to sustain the BP <140/90 mm Hg over time (ie, this is a right-censored discontinuation event).
Readers familiar with survival analysis or failure-time analysis will recognize the above set of assumptions as those of 2 complementary events. However, the time concept in this case is a progressively increased treatment intensity instead of the classical “time-to-event” data.
By properly defining the censoring and event variables, we can use K-M methodology to estimate the cumulative efficacy by calculating 1 minus the K-M estimate with “in control” as the event indicator. Similarly, we estimate the cumulative rate of discontinuation (of further increases in intensity) by calculating 1 minus the K-M estimate with “not in control” as the event indicator. This method can then be used to predict the probability that any given individual will get into control (before they give up) as simply the probability that treatment intensity to just achieve control is less than the intensity where the patient-physician team discontinues further attempts at increasing intensity of therapy. In addition, we can model each of these distributions in terms of baseline covariates, such as age and sex, using familiar techniques, such as Cox regression.26
For simplicity and to maintain independence of measurements, the last sequential observation for each individual was used. This measured BP can be thought of as the observation making the steady-state assumption as likely as possible. In addition, we performed sensitivity analyses including only the last observation of those patients with ≥5 visits to the clinic during our follow-up in the definition of the discontinuation curve. The analyses were repeated considering only the observed visit with the highest intensity for each patient; this differs slightly from the last observation method, because the last observation may not necessarily be the highest intensity observed. In general, one would want to use the highest treatment intensity tried such that control is not achieved, and, conversely, one would want to use the lowest intensity at which control is achieved. Allowing for multiple measurements (and their possible inconsistency) is beyond the scope of this article. For an in-depth description of the statistical methods of this study, please see the online data supplement.
Results
The population under study was composed of 2587 unique patients with 8527 BP measurements (median number of visits per person was 2; first quartile: 1; third quartile: 4; range: 1 to 31 visits). Table 1 shows the numeric descriptive statistics on a per-visit and per-patient basis across age strata. Patients included in the study ranged in age from 15 to 98 years, with median age of 67 years (first quartile: 56 years; third quartile: 75 years). Of the 2587 unique individuals, 1392 were women (53.8%). At last visit there were 1025 patients (39.6%) with elevated BP measurements (out of control). A total of 1588 patients (61.4%) had ≥1 clinic visit with an elevated BP, most because of isolated elevation of systolic pressure measurements (≥140 mm Hg; 1273 patients; 80.2%). Only 39 patients (2.4%) had isolated elevation of diastolic pressure (≥90 mm Hg), whereas the remaining 276 (17.4%) had both elevated systolic and diastolic pressures. The number of medications at time of visit varied greatly from 1 to as many as 7, with a median of 2. The median treatment intensity was 0.5, with a first quartile of 0.25 and a third quartile of 1.0. Thus the “typical patient” was taking 2 medications at one fourth of the maximum dose of each.
Table 1.
Description of Patients and Visits Included in Analyses
| Variable | Age of Patient, y |
Total | |||||
|---|---|---|---|---|---|---|---|
| 15 to 3 | 40 to 49 | 50 to 59 | 60 to 69 | 70 to 79 | ≥80 | ||
| Per patient description | |||||||
| Women, n (%) | 76 (57.1) | 123 (48.1) | 217 (48.4) | 337 (52.0) | 451 (55.7) | 188 (64.4) | 1392 (53.8) |
| No. of visits* | 2 (1, 3) | 2 (1, 3) | 2 (1, 3) | 2 (1, 4) | 3 (2, 4) | 3 (2, 4) | 2 (1, 4) |
| ≥2 visits, n (%) | 77 (57.9) | 155 (60.6) | 283 (63.2) | 442 (68.2) | 640 (79.0) | 223 (76.4) | 1820 (70.4) |
| Days between visit* | 16 (5, 67) | 15 (2, 57) | 18 (2, 70) | 12 (2, 61) | 7 (1, 51) | 14 (2, 62) | 12 (2, 58) |
| High SBP at ≥1 visit, n (%)† | 34 (25.6) | 97 (37.9) | 204 (45.5) | 396 (61.1) | 582 (71.9) | 236 (80.8) | 1549 (59.9) |
| High DBP at ≥1 visit, n (%)† | 30 (22.6) | 72 (28.1) | 75 (16.7) | 64 (9.9) | 57 (7.0) | 17 (5.8) | 315 (12.2) |
| High SBP or DBP at ≥1 visit, n (%) | 44 (33.1) | 112 (43.8) | 213 (47.5) | 398 (61.4) | 585 (72.2) | 236 (80.8) | 1588 (61.4) |
| High SBP or DBP at last visit, n (%) | 25 (18.8) | 66 (25.8) | 134 (29.9) | 259 (40.0) | 376 (46.4) | 165 (56.5) | 1025 (39.6) |
| Total, n (%) | 133 (5.1) | 256 (9.9) | 448 (17.3) | 648 (25.1) | 810 (31.3) | 292 (11.3) | 2587 (100.0) |
| Per visit description, mean (SD) | |||||||
| No. of medications | 1.41 (0.65) | 1.83 (1.30) | 1.79 (1.01) | 1.90 (1.12) | 1.93 (1.06) | 1.82 (0.90) | 1.86 (1.06) |
| Total intensity | 0.55 (0.49) | 0.81 (0.89) | 0.76 (0.67) | 0.79 (0.66) | 0.77 (0.62) | 0.68 (0.56) | 0.76 (0.66) |
| SBP, mm Hg | 122.8 (17.0) | 132.2 (20.1) | 134.4 (20.0) | 139.5 (20.0) | 142.9 (20.8) | 149.2 (23.0) | 139.7 (21.5) |
| DBP, mm Hg | 77.8 (11.8) | 81.0 (12.8) | 75.9 (10.8) | 71.9 (10.6) | 68.0 (11.0) | 64.7 (10.7) | 71.3 (12.1) |
| Total, n (%) | 364 (4.3) | 775 (9.1) | 1362 (16.0) | 2012 (23.6) | 2869 (33.6) | 1145 (13.4) | 8527 (100.0) |
SBP indicates systolic BP; DBP, diastolic BP.
These values are reported as the median (25th percentile, 75th percentile).
High SBP is defined as ≥140 mm Hg; high DBP is defined as ≥90 mm Hg.
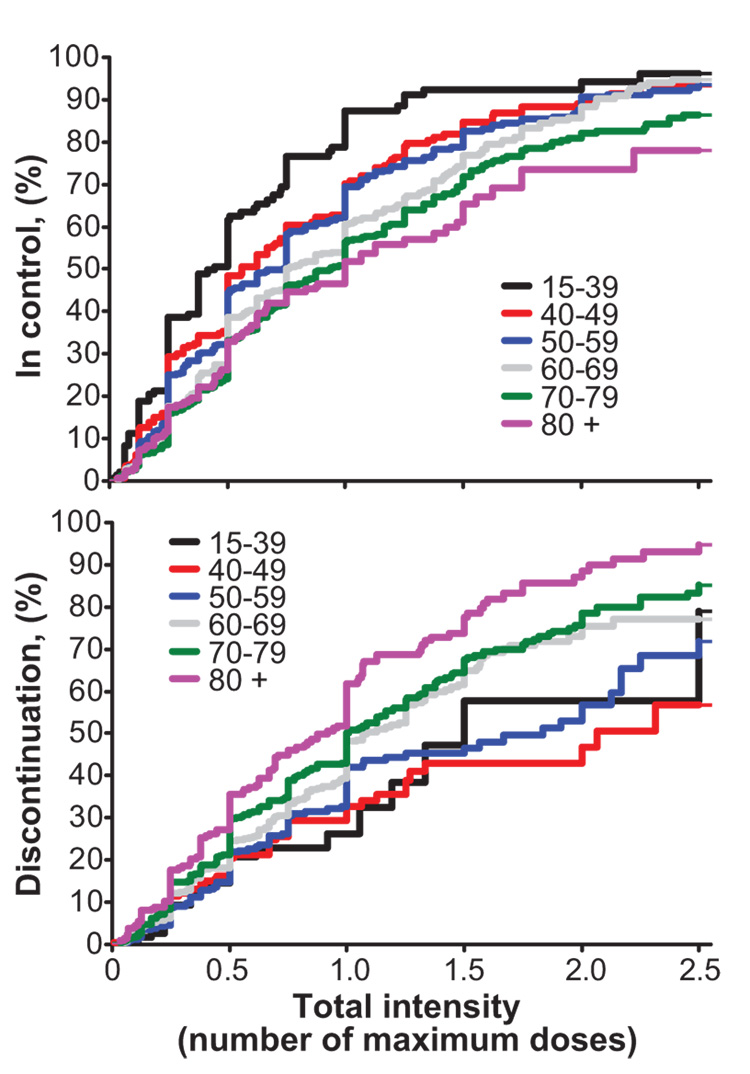
The cumulative efficacy distribution for the treatment intensity by age strata is shown in Figure 1 (top panel). This curve shows the cumulative probability of attaining control as treatment intensity increases. With older age we observed a marked decrease in control rates at any given intensity. For example, the K-M estimated curve predicts that 61.5% (51.6% to 68.3%) of those in the age 15- to 39-year stratum would be in control at an intensity of ≤0.5, whereas only 33.0% (26.7% to 38.7%) of those in the age ≥80-year stratum would have controlled BP at this or a lower intensity. Note that these are not the answers we get if we naively consider the proportion of individuals treated at this intensity or less who are in control (80.9% and 47.9%, respectively). Such naive estimates ignore the information in those individuals who are treated at higher intensities (presumably because they were not controlled at lower intensities). This parameter (the cumulative percentage of the population controlled at a given intensity or less) is only available in an unbiased way using our framework.
Figure 1.
Efficacy and discontinuation curves separate by age category. Top, The efficacy curves show the probability of attaining blood pressure control at various treatment intensity units and separately across age categories. Bottom, The discontinuation curves show the probability of either the physician or the patient choosing to discontinue further medication increases to attain BP control. Curves in both panels are calculated using the K-M method.
The discontinuation distributions for intensity stratified by age are shown in Figure 1 (bottom panel). Again, we can see that the probability of discontinuation (ie, the likelihood of no further increases in treatment intensity) steadily increases as intensity increases. Indeed, very few patients and/or physicians are willing to increase treatment intensity beyond 3.0 U. As was the case for the efficacy curves, there is a marked trend across age strata, with the elderly having a higher probability of discontinuation of further increases in treatment intensity at lower intensities than the younger patients. As an example, the K-M method predicts that 20.7% (11.3% to 29.2%) of the age 15- to 39-year population would discontinue further medication increases at an intensity of 0.5, whereas 35.6% (29.3% to 41.5%) of the age ≥80-year populations would discontinue further intensity increases. Again, we note that this parameter cannot be accurately estimated by naively considering the proportion of the population actually treated at such intensity. The naive estimate ignores the fact that those who achieve BP control at lower intensities have not been challenged in terms of their willingness to try higher treatment intensities.
We were reassured by our calculations when we compared our method with a more naive method. In particular, if only patients who achieved control are included and the distribution of control intensities is described, the proportion of subjects with an intensity of ≤1.0 U is estimated at 82.5% (80.6% to 84.4%) in control. However, when using our method and taking into account those subjects who never achieved control, the cumulative control rate of 62.6% (61.3% to 64.8%) is attained. The naive method overestimates control rates. Naive estimates of discontinuation are plagued by the same overestimation, because no concept of censoring is used (ie, patients may persist to higher intensities if given the chance).
The standard K-M estimates of the overall distributions of treatment intensity in control and when discontinuation occurs have limitations in that they likely vary considerably as a function of age and sex and other baseline variables. Therefore, to further exploit our alternative analysis methodology, Cox regression models for treatment intensity when control is just achieved as a function of age and sex are reported in Table 2 (top). The Cox regression model posits a constant “hazard ratio” associated with gender, or with a specific age difference, for the “hazard” of becoming controlled at any given intensity. The interaction test indicates whether the effect of age on BP control differs between men and women. This analysis shows that control rates are highly affected by age and, furthermore, that the way they are affected by age differs in men and women. The β coefficients from the sex-specific models show that, with each decade of age increase, the logarithm of the hazard of getting into control drops by 0.10 in men and by 0.20 in women. This is interpreted as showing that, for each increase in age by 10 years, the percentage of patients achieving control (at all treatment intensities) is reduced by 10% in men and by 20% in women.
Table 2.
Efficacy and Discontinuation Cox Regression Models
| Variable | Beta±SE | P | Hazard Ratio | 95% CI |
|---|---|---|---|---|
| Efficacy models | ||||
| Full model with interaction | ||||
| Age, decades | −0.20±0.02 | <0.0001 | 0.82 | 0.78 to 0.86 |
| Sex, male | −0.68±0.24 | 0.005 | 0.51 | 0.32 to 0.81 |
| Interaction | 0.10±0.04 | 0.006 | 1.11 | 1.03 to 1.19 |
| Men only analysis | ||||
| Age, decades | −0.09±0.03 | 0.0007 | 0.91 | 0.86 to 0.96 |
| Women only analysis | ||||
| Age, decades | −0.20±0.02 | <0.0001 | 0.82 | 0.78 to 0.86 |
| Discontinuation models | ||||
| Full model with interaction | ||||
| Age, decades | 0.22±0.04 | <0.0001 | 1.25 | 1.17 to 1.34 |
| Sex, male | 0.07±0.37 | 0.84 | 1.08 | 0.52 to 2.23 |
| Interaction | −0.04±0.05 | 0.47 | 0.96 | 0.87 to 1.07 |
| Men only analysis | ||||
| Age, decades | 0.19±0.04 | <0.0001 | 1.21 | 1.11 to 1.30 |
| Women only analysis | ||||
| Age, decades | 0.22±0.04 | <0.0001 | 1.25 | 1.16 to 1.34 |
The corresponding Cox regression models for discontinuation are shown in Table 2 (bottom). We see that, at each treatment intensity, the hazard of discontinuation increases with age but is not different in men and women. This analysis enables us to quantify the extent to which the observed decline with age in control rates is because of a decline in efficacy versus an unwillingness to intensify a medication regimen. This suggests that physicians in this study had no gender bias about increasing treatment intensity to try to obtain BP control.
Probability of Achieving Control
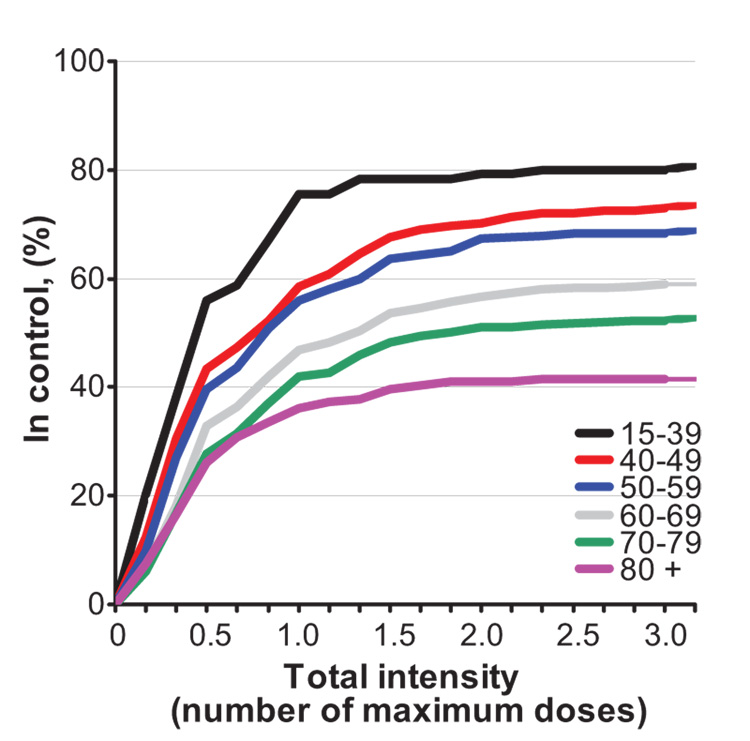
The age-stratified efficacy (Figure 1, top) and discontinuation (Figure 1, bottom) curves are shown visually based on K-M estimates for different age groups. Using these same age strata, Figure 2 shows the predicted cumulative probability of control up to any intensity in each age group, based on combining the 2 K-M distributions. This model allows us to estimate, eg, what impact it would have if the rate of discontinuation were equalized between age groups or if the efficacy were equalized between age groups (Table 3). We see from the figure and from the Cox regression models that both efficacy patterns and discontinuation patterns (of either the patient or physician) vary across age strata. Interestingly, we note that even if patients ≥80 years of age were treated in an aggressive manner similar to patients much younger (ages 15 to 39 years), our analysis estimates that the cumulative control rate would still only be 61.5%.
Figure 2.
The combination of efficacy and discontinuation information to estimate the overall control rates separate by age categories. Note that beyond a treatment intensity of 2 intensity units, the incremental improvement in BP control is minimal.
Table 3.
Projected Control Rates (%) Across Age-Specific Efficacy Patterns and Discontinuation Patterns
| Efficacy Pattern, Age Group |
Discontinuation Pattern, Age Group |
|||||
|---|---|---|---|---|---|---|
| 15 to 39 y | 40 to 49 y | 50 to 59 y | 60 to 69 y | 70 to 79 y | ≥80 y | |
| 15 to 39 y | 80.8 | 79.2 | 77.9 | 73.9 | 71.1 | 65.3 |
| 40 to 49 y | 73.1 | 73.6 | 71.1 | 65.2 | 62.3 | 55.4 |
| 50 to 59 y | 70.6 | 71.6 | 69.2 | 63.2 | 60.1 | 53.1 |
| 60 to 69 y | 68.1 | 70.2 | 66.9 | 59.0 | 56.1 | 48.4 |
| 70 to 79 y | 63.8 | 66.4 | 63.0 | 55.7 | 52.5 | 44.8 |
| ≥80 y | 61.5 | 65.9 | 60.3 | 52.7 | 50.0 | 42.1 |
Discussion
We have introduced the use of an alternative and unique analysis methodology to examine a cross-sectional BP data-base in the Mayo Clinic Division of Hypertension. This method assumes an embedded process of cumulative increases of treatment intensity until either BP control is just achieved or until discontinuation occurs (acceptance of uncontrolled BP by the patient-physician team). Despite the passage of >40 years since the first hypertension treatment trials1,2 and with the more recent clinical trials, such as the Antihypertensive and Lipid-Lowering Trial to Prevent Heart Attack Study,3 Heart Outcomes Prevention Evaluation Study,4 and the Systolic Hypertension in Europe Study,5 rates of control of hypertension have remained low. In fact, rates of hypertension control vary from 29.2% in the United States6 and 22% in England7 to as low as 11.2% in Portugal8 and 8.1% in China.9 Many attempts have been made to analyze factors that may be responsible for this lack of success in hypertension treatment. Factors evaluated have been divided into 2 main types. First, physician-related factors have been implicated, including physician bias, therapeutic inertia, impact of comorbidities, treatment thresholds, physician specialty, and physician acceptance and incorporation into their practice of guideline information about hypertension management.10–14 Second, patient-related factors, such as age, gender, persistence of therapy, and especially noncompliance with antihypertensive therapy,15–22 have been investigated.
The Antihypertensive and Lipid-Lowering Trial to Prevent Heart Attack Study3 had the highest rate of hypertension control achieved in a large clinical trial, at 63%. These subjects were similar to the patients in our study regarding both age and gender distribution and a higher-than-average burden of comorbid conditions. Validation of our estimates comes from inspection of Table 3, which shows that our prediction of achievable control for the patients of the mean age in the Antihypertensive and Lipid-Lowering Trial to Prevent Heart Attack Study is almost identical (ages 50 to 59 years: 69.2%; ages 60 to 69 years: 59.0%) to what was achieved. Perhaps the most important study of physician factors affecting BP control is that by Okonofua et al.11 They investigated therapeutic inertia (the failure of a clinician to increase therapy when BP was elevated) in a retrospective study of 7253 hypertensive patients. They found that therapeutic inertia accounted for 19% of the lack of BP control. Furthermore, they argued that if therapeutic inertia scores were improved by 50% (ie, if on 30% of the visits medications were advanced), control rates would have improved from the observed 45.1% to 65.9% in only 1 year. This observation is similar to what we have observed (Figure 1) regarding the role of increased treatment intensities on achieving BP control. Unfortunately, Okonofua et al11 did not stratify by age; however, they did find a significant correlation of age with therapeutic inertia in their multivariate analyses. Our unique modeling, which investigates the overall medical strategy of both physician and patient, supports their finding that physician behavior has a major impact on achieving BP control. We demonstrate not only an age effect on hypertension control but that the age effect is expressed differently in men and women. Thus, at any level of treatment intensity, we found that the likelihood of achieving control was reduced by 10% in men and 20% in women (P<0.001). Lloyd-Jones et al15 also reported on the impact of age on control rates separately for women and men; however, no information regarding therapy intensity was provided. Borzecki et al16 found that increasing age was associated with increased use of medications until reaching age 80 years, after which medication usage decreased. However, their analysis was limited only to the number of medications used, which may not be a true reflection of intensity of treatment. In our analyses, we used medication intensity and, thus, created a powerful argument that there are gender and age differences in the treatment of hypertension, even after accounting for possible differences in dosing and the use of dual drugs across age groups.
Factors that may explain this were described previously by Van Wijk et al18 in a 10-year historical cohort study of antihypertensive medication adherence in 2325 patients in the Netherlands. Using a national pharmacy database of filled prescriptions (PHARMO Medical Record Linking System), they examined the likelihood of persistence of antihypertensive therapy and found that women were less likely than men to persist with their BP therapy. Because we are only able to analyze the impact of prescribed medications rather than filled prescriptions, we cannot rule out that the lower rates of control in women may be because of nonadherence to therapy. Another theory for the age and gender difference comes from Winickhoff and Murphy.21 They identified the impact of the number of medications on BP control. In particular, they found that the more pills the person is required to take the less likely they were to adhere to therapy and, thus, less likely to achieve BP control. This phenomenon may explain results in Figure 1, which demonstrates that discontinuation rates are age dependent and that they increase with higher intensity of therapy. Thus, there may be a point at which further increases in medication intensity cannot lead to better control if the increase in intensity requires ingestion of more pills rather than an increase in dose strength of an existing pill.
Limitations
We recognize that this method of analysis is an oversimplification in several ways. First, by reducing a time series to a single observation and further reducing this observation to “in control” versus “not in control,” we miss the possible additional information of multiple observations. For example, in our study, a patient may have had 9 previous visits while in control, and at the 10th visit (the 1 used for our analysis) the BP may have been ≥140/90 mm Hg (not in control). This patient would be analyzed the same as a patient who had 10 previous visits not in control. We are comforted by previous clinical trials that have reported that little change in BP occurs after 6 months of attempts at therapy alterations4,5 and the fact that our results from our sensitivity analysis of only patients with ≥5 visits did not change the outcome.
Second, by reducing a complex medication regimen to a single “treatment intensity,” we ignore differences between medications. Specific medications were not of primary interest, because we felt that overall treatment intensity is better at representing the aggressiveness of a treatment regimen and better reflects physician practice patterns, as well as patient acceptance (more likely to use increase in strength of a medication before adding second drug). We acknowledged that this intensity measure, although intended to equalize the different medications, may not completely achieve this goal. For example, dual medications may be used more in the elderly than in the young, whereas intensities may be similar.
Third, we know that in real life there is an “up and down” titration and testing process that occurs within individual patients. Thus, although we considered our patients to have reached a steady state, ≈40% of patients had BP measurements considered out of control at last visit. Our database analysis did not allow us to know the therapeutic intent of the last visit, thus, we do not know if that visit engendered an increase in treatment intensity in patients not in control.
Fourth, our method makes the unverifiable assumptions made in all K-M and Cox regression analyses. Namely, we assume that the conditional distribution of “future” efficacy (at higher intensities) is the same in uncontrolled individuals who give up as it is in those who do go on to higher intensities. The method also assumes that the conditional distribution of discontinuation (to higher intensities) is the same in those who are uncontrolled and controlled at a particular intensity.
Lastly, we assume that we have observed the exact value of the “discontinuation intensity” for each patient who is not in control. Of course, the farther out we are in the course of treatment for a given patient, the closer we are to the truth of this assumption.4,5 Table 1 shows that there was a significant treatment effect on control rates as evidenced by comparing the percentage of patients with an elevated systolic or diastolic BP anytime during follow-up (61.4%) and those with elevated measures at last visit (39.6%). This observation supports that many patients were indeed well progressed in a successful treatment program. In addition, our results did not change in a sensitivity analysis when we restricted to patients with ≥5 observed visits (data not shown). Because a large proportion of the patients included in our study were primary care patients, we feel that application of our alternative methods to hypertension control in a strictly primary care database will be robust. Nonetheless, we encourage others to apply these methods and report their findings, because it is ever more important to gauge the target rate of maximal achievable BP control for clinical practice and quality evaluation.
Perspectives
The ability to control BP is important to the individual and to society. Although many studies have reported control rates for hypertension, these studies have not given information regarding how these rates compare with what can feasibly be expected. In fact, though no study or medication has ever achieved 100% hypertension control, it continues to be suggested that the target is that all patients attain BP control. This study is the first to attempt to predict the maximum ability to control BP with our present systems, medications, and approach to disease management. Our analysis is compatible with clinical observations in that the efficacy of treatments decrease with age and that the patient-physician team is less likely to further increase treatment in older patients. Our estimates strongly suggest that elderly patients are unlikely to reach the target of <140/90 mm Hg, even if patients and physicians attempted to do so with increasing pharmacotherapy. We also find that women, controlling for age, have a reduction in apparent efficacy of antihypertensive therapy compared with men, whereas discontinuation of therapy (patient-physician team decision) is not gender dependent. Our study suggests that targets for hypertension control rates should be gender specific and that the assumption that 1 target fits both genders may be erroneous. Further validation of our predictions in a strictly primary care setting is needed.
Supplementary Material
Acknowledgments
Source of Funding
Research was funded by National Institutes of Health grant R03 HL68259 from the National Heart, Blood, and Lung Institute.
Footnotes
The online version of this article, along with updated information and services, is located on the World Wide Web at: http://hyper.ahajournals.org/cgi/content/full/51/4/841
Data Supplement (unedited) at: http://hyper.ahajournals.org/cgi/content/full/HYPERTENSIONAHA.107.101659/DC1
Reprints: Information about reprints can be found online at http://www.lww.com/reprints
Disclosures
None.
References
- 1.Hamilton M, Thompson EN, Wisniewski TKM. The role of blood-pressure control in preventing complications of hypertension. Lancet. 1964;1:235–238. doi: 10.1016/s0140-6736(64)92344-x. [DOI] [PubMed] [Google Scholar]
- 2.Veterans Administration Cooperative Study Group on Antihypertensive Agents. Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg. JAMA. 1967;202:1028–1034. [PubMed] [Google Scholar]
- 3.The ALLHAT offices and Coordinators of the ALLHAT Collaborative Research Group. Major cardiovascular events in hypertensive patients randomized to doxazosin vs chlorthalidone. JAMA. 2000;283:1967–1975. [PubMed] [Google Scholar]
- 4.Heart Outcomes Prevention Evaluation (HOPE) Study Investigators. Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Lancet. 2000;355:253–259. [PubMed] [Google Scholar]
- 5.Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhager WH, Bulpitt CJ, de Leeuw PW, Dollery CT, Fletcher AE, Forette F, Leonetti G, Nachev C, O’Brien ET, Rosenfeld J, Rodicio JL, Tuomilehto J, Zanchetti A for the Syst-Eur Trial Investigators. Randomized double-blind placebo and active treatment for older patients with isolated systolic hypertension. Lancet. 1997;360:757–764. doi: 10.1016/s0140-6736(97)05381-6. [DOI] [PubMed] [Google Scholar]
- 6.Ong KL, Cheung BYM, Man YB, Lau CP, Lam KSL. Prevalence, awareness, treatment and control of hypertension among Untied States Adults 1999–2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 7.Primatesta P, Poulter NR. Improvement in hypertension management in England results from the Health Survey for England 2003. J Hypertens. 2006;24:1193–1200. doi: 10.1097/01.hjh.0000226210.95936.bc. [DOI] [PubMed] [Google Scholar]
- 8.Macedo ME, Lima MJ, Silva AO, Alcantara P, Ramalhinho V, Carmona J. Prevalence, awareness, treatment and control of hypertension in Portugal: the PAP study. J Hypertens. 2005;23:1661–1666. doi: 10.1097/01.hjh.0000179908.51187.de. [DOI] [PubMed] [Google Scholar]
- 9.Gu D, Reynolds K, Wu X, Chen J, Duan X, Muntner P, Huang G, Reynolds RF, Su S, Whelton PK, He J for the InterASIA Collaborative Group. The International Collaborative Study of Cardiovascular Disease in ASIA. Prevalence, awareness, treatment and control of hypertension in China. Hypertension. 2002;40:920–927. doi: 10.1161/01.hyp.0000040263.94619.d5. [DOI] [PubMed] [Google Scholar]
- 10. [Accessed July 26, 2000];Shield National Faculty Press Release Doctor’s Guide. Available at: www.docguide.com.
- 11.Okonofua EC, Simpson KN, Jesri A, Rehman SU, Durkalski VL, Egan BM. Therapeutic Inertia is an impediment to achieving the healthy people 2010 blood pressure control goals. Hypertension. 2006;47:345–351. doi: 10.1161/01.HYP.0000200702.76436.4b. [DOI] [PubMed] [Google Scholar]
- 12.Brokensha G, Marley JE. An observational study of the medical events associated with clinician initiated changes in treatment for essential hypertension. J Hum Hypertens. 2001;15:381–385. doi: 10.1038/sj.jhh.1001195. [DOI] [PubMed] [Google Scholar]
- 13.Wang YR, Alexander C, Stafford RS. Outpatient hypertension treatment, treatment intensification and control in Western Europe and the United States. Arch Intern Med. 2007;167:141–147. doi: 10.1001/archinte.167.2.141. [DOI] [PubMed] [Google Scholar]
- 14.Olvieria SA, Lapuerta P, McCarthy BD, L’Italien GJ, Berlowitz DR, Asch SM. Physician related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162:413–420. doi: 10.1001/archinte.162.4.413. [DOI] [PubMed] [Google Scholar]
- 15.Lloyd-Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA. 2005;294:466–472. doi: 10.1001/jama.294.4.466. [DOI] [PubMed] [Google Scholar]
- 16.Borzecki AM, Glickman ME, Kader B, Berlowitz DR. The effect of age on hypertension control and management. Am J Hypertens. 2006;19:520–527. doi: 10.1016/j.amjhyper.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 17.Jokisalo E, Kumpusalo E, Enlund H, Halonen P, Tkala J. Factors related to non-compliance with antihypertensive drug therapy. J Hum Hypertens. 2002;16:577–583. doi: 10.1038/sj.jhh.1001448. [DOI] [PubMed] [Google Scholar]
- 18.Van Wijk BLG, Klungel OH, Heerdink ER, de Boer A. Rate and determinants of 10-year persistence with antihypertensive drugs. J Hypertens. 2005;23:2101–2107. doi: 10.1097/01.hjh.0000187261.40190.2e. [DOI] [PubMed] [Google Scholar]
- 19.Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326:1427–1434. doi: 10.1136/bmj.326.7404.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hasford J, Mimran A, Simons WR. A population based European cohort study of persistence in newly diagnosed hypertensive patients. J Hum Hypertens. 2002;16:569–575. doi: 10.1038/sj.jhh.1001451. [DOI] [PubMed] [Google Scholar]
- 21.Winickhoff RN, Murphy PK. The persistent problem of poor blood pressure control. Arch Intern Med. 1987;147:1393–1396. [PubMed] [Google Scholar]
- 22.Wetzels GEC, Nelemans P, Schouten JS, Prins MH. Facts and fiction of poor compliance as a cause of inadequate blood pressure control: a systematic review. J Hypertens. 2004;22:1849–1855. doi: 10.1097/00004872-200410000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Beilin LJ. Hypertension research in the 21st century: where is the gold? J Hypertens. 2004;22:2243–2251. doi: 10.1097/00004872-200412000-00002. [DOI] [PubMed] [Google Scholar]
- 24. [Accessed September 1, 2007];The National Committee for Quality Assurance. State of health care quality 2007. Available at: http://www.ncqa.org/tabid/543/Default.aspx.
- 25.Kaplan EL, Meier P. Non-parametric estimation from incomplete observations. J Am Statist Assoc. 1958;53:457–481. [Google Scholar]
- 26.Cox DR. Regression models and life-tables. J Roy Statist Soc B. 1972;34:187–220. [Google Scholar]
- 27.Graves JW, Bailey KR, Grossardt BR, Gullerud RE, Meverden RA, Grill DE, Sheps SG. The impact of observer and patient factors on the occurrence of digit preference for zero in blood pressure measurement in a hypertension specialty clinic: evidence for the need of continued observation. Am J Hypertens. 2006;19:567–572. doi: 10.1016/j.amjhyper.2005.04.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.