Abstract
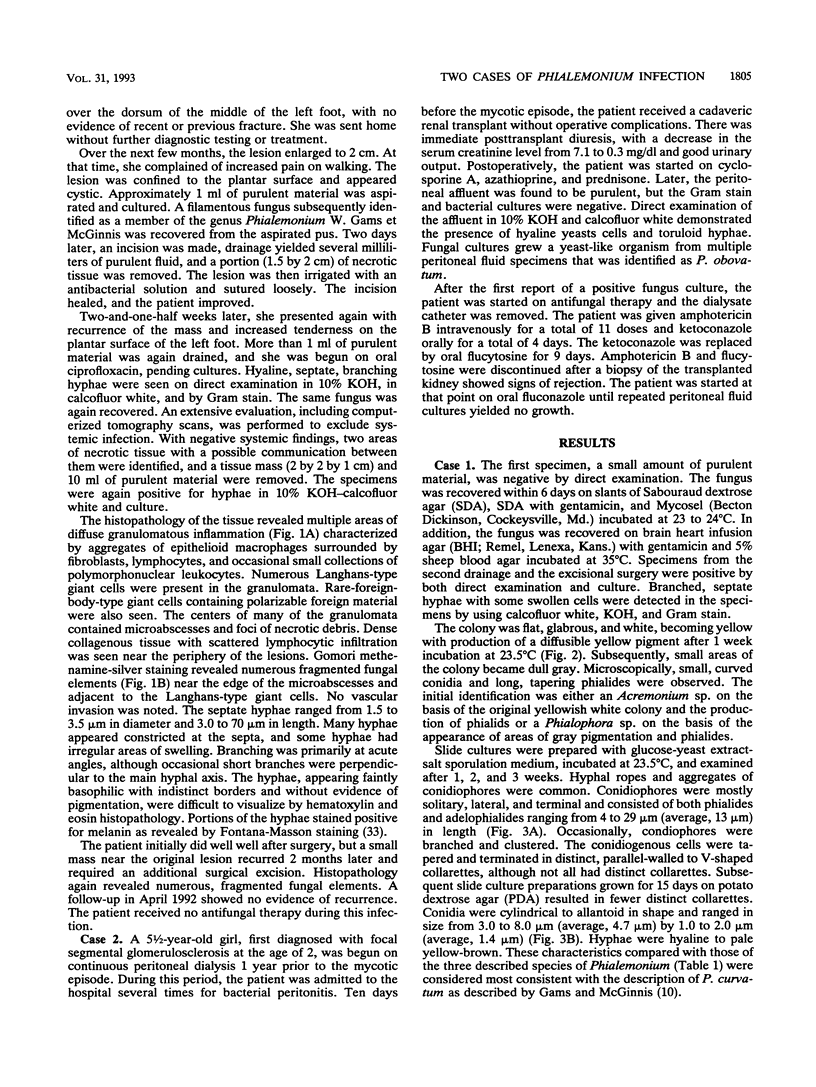
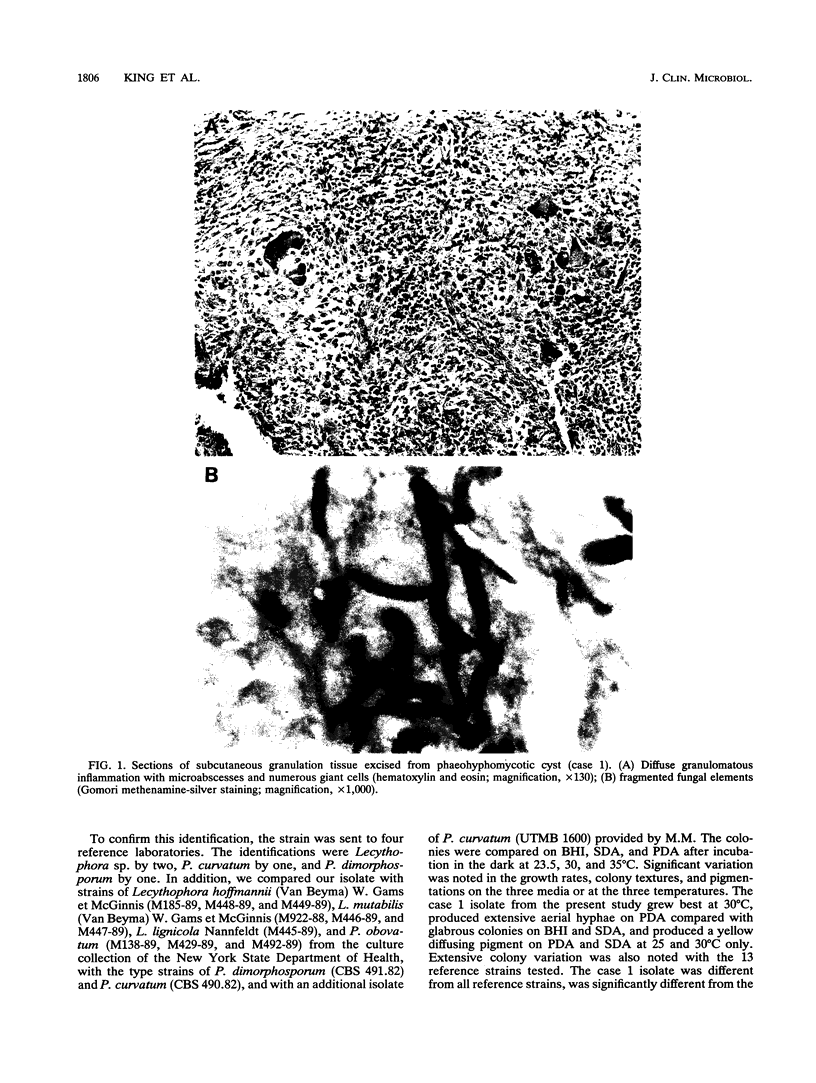
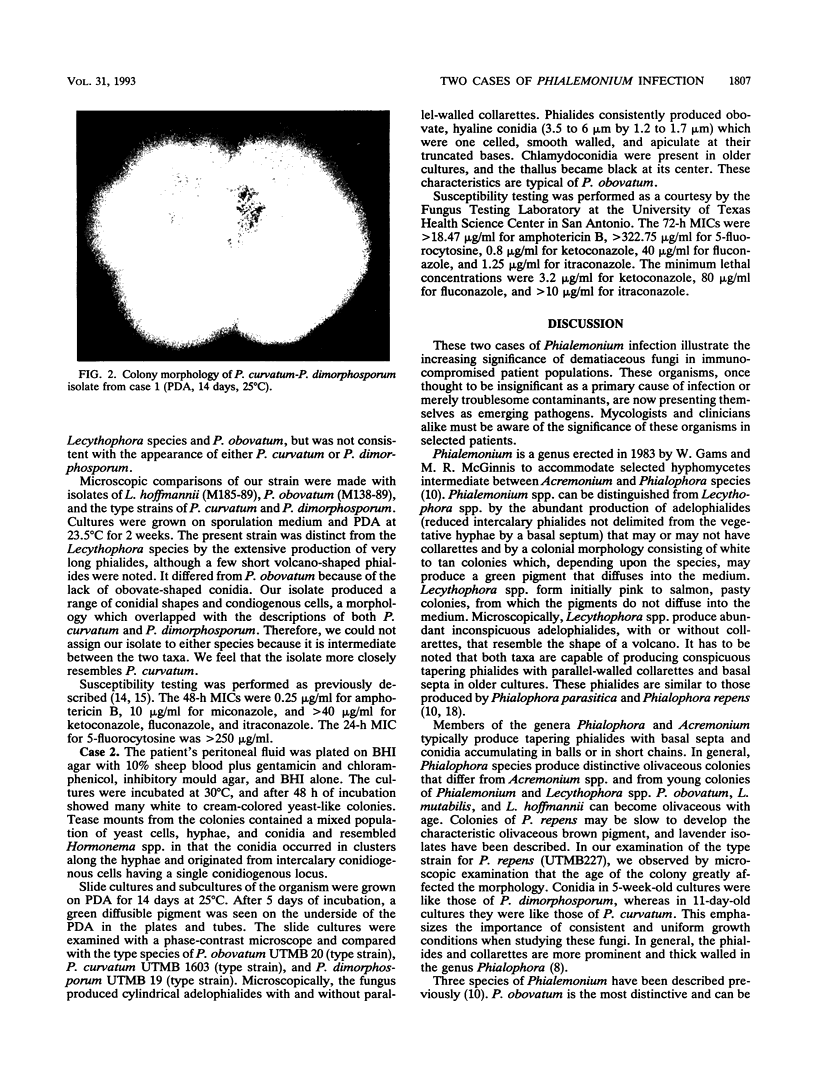
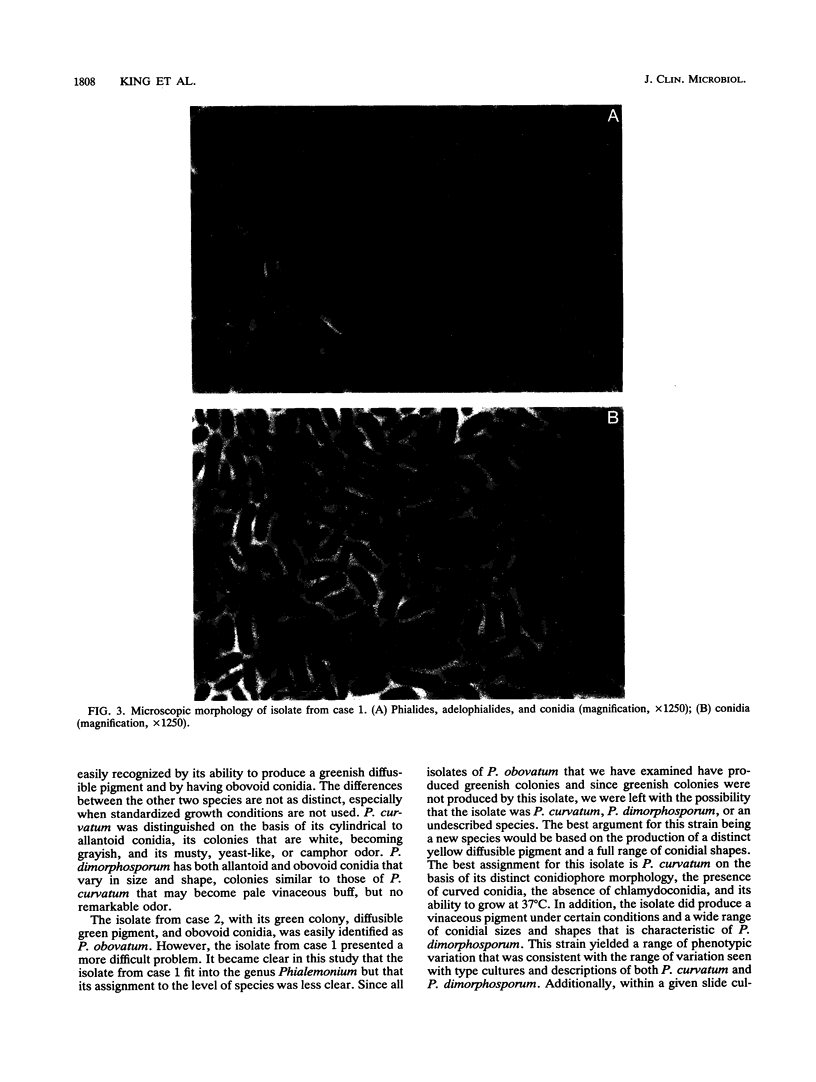
Two cases of human fungal infections caused by members of the genus Phialemonium, a genus proposed by Gams and McGinnis (1983) for fungi intermediate between the genera Acremonium and Phialophora, are presented. The first case was a phaeohyphomycotic cyst on the foot of a renal transplant recipient. The fungus was detected by direct examination and histopathology and was recovered by several procedures over 4 months. It was flat, glabrous, and white becoming yellow with the production of a diffusible yellow pigment; it had conidiophores that were mostly solitary and lateral and terminal phialides and adelophialides with distinct collarettes producing cylindrical to curved conidia. The isolate resembled both Phialemonium dimorphosporum and Phialemonium curvatum, although its characteristics were more consistent with those of the latter. The second case was peritonitis in a renal transplant recipient. The fungus was white-to-cream colored and yeast like, but later became black with a green diffusible pigment, and produced obovoid conidia; it was easily identified as Phialemonium obovatum. Difficulties encountered in the identification and taxonomy of members of this genus highlight the need for standardized conditions, e.g., potato dextrose agar culture incubated at 24 to 25 degrees C for morphologic comparisons, to control significant variations due to culture conditions.
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ahlmén J., Edebo L., Eriksson C., Carlsson L., Torgersen A. K. Fluconazole therapy for fungal peritonitis in continuous ambulatory peritoneal dialysis (CAPD): a case report. Perit Dial Int. 1989;9(1):79–80. [PubMed] [Google Scholar]
- Ahmad S., Johnson R. J., Hillier S., Shelton W. R., Rinaldi M. G. Fungal peritonitis caused by Lecythophora mutabilis. J Clin Microbiol. 1985 Aug;22(2):182–186. doi: 10.1128/jcm.22.2.182-186.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ampel N. M., White J. D., Varanasi U. R., Larwood T. R., Van Wyck D. B., Galgiani J. N. Coccidioidal peritonitis associated with continuous ambulatory peritoneal dialysis. Am J Kidney Dis. 1988 Jun;11(6):512–514. doi: 10.1016/s0272-6386(88)80088-x. [DOI] [PubMed] [Google Scholar]
- Branton M. H., Johnson S. C., Brooke J. D., Hasbargen J. A. Peritonitis due to Rhizopus in a patient undergoing continuous ambulatory peritoneal dialysis. Rev Infect Dis. 1991 Jan-Feb;13(1):19–21. doi: 10.1093/clinids/12.5.19. [DOI] [PubMed] [Google Scholar]
- Castaldo P., Stratta R. J., Wood R. P., Markin R. S., Patil K. D., Shaefer M. S., Langnas A. N., Reed E. C., Li S. J., Pillen T. J. Clinical spectrum of fungal infections after orthotopic liver transplantation. Arch Surg. 1991 Feb;126(2):149–156. doi: 10.1001/archsurg.1991.01410260033005. [DOI] [PubMed] [Google Scholar]
- Cheng I. K., Fang G. X., Chan T. M., Chan P. C., Chan M. K. Fungal peritonitis complicating peritoneal dialysis: report of 27 cases and review of treatment. Q J Med. 1989 May;71(265):407–416. [PubMed] [Google Scholar]
- Chiaradia V., Schinella D., Pascoli L., Tesio F., Santini G. F. Fusarium peritonitis in peritoneal dialysis: report of two cases. Microbiologica. 1990 Jan;13(1):77–78. [PubMed] [Google Scholar]
- Dixon D. M., Polak-Wyss A. The medically important dematiaceous fungi and their identification. Mycoses. 1991 Jan-Feb;34(1-2):1–18. doi: 10.1111/j.1439-0507.1991.tb00613.x. [DOI] [PubMed] [Google Scholar]
- Dressler R., Peters A. T., Lynn R. I. Pseudomonal and candidal peritonitis as a complication of continuous ambulatory peritoneal dialysis in human immunodeficiency virus-infected patients. Am J Med. 1989 Jun;86(6 Pt 2):787–790. doi: 10.1016/0002-9343(89)90474-9. [DOI] [PubMed] [Google Scholar]
- García-Martos P., Díaz Portillo J., Pérez Ruilópez M. A., Castaño López M. A., Fernández Gutiérrez del Alamo C. Peritonitis fúngica en diálisis peritoneal continua ambulatoria (DPCA). Enferm Infecc Microbiol Clin. 1991 Jan;9(1):30–32. [PubMed] [Google Scholar]
- Gibb A. P., Aggarwal R., Swainson C. P. Successful treatment of Prototheca peritonitis complicating continuous ambulatory peritoneal dialysis. J Infect. 1991 Mar;22(2):183–185. doi: 10.1016/0163-4453(91)91679-r. [DOI] [PubMed] [Google Scholar]
- Gidding H., Hawes L., Dwyer B. The isolation of Malassezia furfur from an episode of peritonitis. Med J Aust. 1989 Nov 20;151(10):603–603. doi: 10.5694/j.1326-5377.1989.tb101300.x. [DOI] [PubMed] [Google Scholar]
- Gordon M. A., Lapa E. W., Passero P. G. Improved method for azole antifungal susceptibility testing. J Clin Microbiol. 1988 Sep;26(9):1874–1877. doi: 10.1128/jcm.26.9.1874-1877.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guarner J., Del Rio C., Williams P., McGowan J. E., Jr Fungal peritonitis caused by Curvularia lunata in a patient undergoing peritoneal dialysis. Am J Med Sci. 1989 Nov;298(5):320–323. doi: 10.1097/00000441-198911000-00008. [DOI] [PubMed] [Google Scholar]
- Hida M. Autopsy findings in 68 fatal renal transplant recipients, collected from the annuals of pathological autopsy cases in Japan. Tokai J Exp Clin Med. 1988 Feb;13(1):23–29. [PubMed] [Google Scholar]
- Hironaga M., Nakano K., Yokoyama I., Kitajima J. Phialophora repens, an emerging agent of subcutaneous phaeohyphomycosis in humans. J Clin Microbiol. 1989 Mar;27(3):394–399. doi: 10.1128/jcm.27.3.394-399.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim W., Chau S. P., Chan P. C., Cheng I. K. Histoplasma capsulatum infection associated with continuous ambulatory peritoneal dialysis. J Infect. 1991 Mar;22(2):179–182. doi: 10.1016/0163-4453(91)91657-j. [DOI] [PubMed] [Google Scholar]
- Lomax L. G., Cole J. R., Padhye A. A., Ajello L., Chandler F. W., Smith B. R. Osteolytic phaeohyphomycosis in a German shepherd dog caused by Phialemonium obovatum. J Clin Microbiol. 1986 May;23(5):987–991. doi: 10.1128/jcm.23.5.987-991.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinnis M. R., Gams W., Goodwin M. N., Jr Phialemonium obovatum infection in a burned child. J Med Vet Mycol. 1986 Feb;24(1):51–55. [PubMed] [Google Scholar]
- Mocan H., Murphy A. V., Beattie T. J., McAllister T. A. Fungal peritonitis in children on continuous ambulatory peritoneal dialysis. Scott Med J. 1989 Aug;34(4):494–496. doi: 10.1177/003693308903400404. [DOI] [PubMed] [Google Scholar]
- Moses A., Maayan S., Shvil Y., Dudin A., Ariel I., Thalji A., Polacheck I. Hansenula anomala infections in children: from asymptomatic colonization to tissue invasion. Pediatr Infect Dis J. 1991 May;10(5):400–402. doi: 10.1097/00006454-199105000-00010. [DOI] [PubMed] [Google Scholar]
- Murugasu B., Conley S. B., Lemire J. M., Portman R. J. Fungal peritonitis in children treated with peritoneal dialysis and gastrostomy feeding. Pediatr Nephrol. 1991 Sep;5(5):620–621. doi: 10.1007/BF00856656. [DOI] [PubMed] [Google Scholar]
- Nakamura M., Weil W. B., Jr, Kaufman D. B. Fatal fungal peritonitis in an adolescent on continuous ambulatory peritoneal dialysis: association with deferoxamine. Pediatr Nephrol. 1989 Jan;3(1):80–82. doi: 10.1007/BF00859631. [DOI] [PubMed] [Google Scholar]
- Perez-Lasala G., Nolan R. L., Chapman S. W., Achord J. L. Peritoneal blastomycosis. Am J Gastroenterol. 1991 Mar;86(3):357–359. [PubMed] [Google Scholar]
- Prewitt K., Lockard J., Rodgers D., Hasbargen J. Successful treatment of Aspergillus peritonitis complicating peritoneal dialysis. Am J Kidney Dis. 1989 Jun;13(6):501–503. doi: 10.1016/s0272-6386(89)80009-5. [DOI] [PubMed] [Google Scholar]
- Pritchard R. C., Muir D. B. Black fungi: a survey of dematiaceous hyphomycetes from clinical specimens identified over a five year period in a reference laboratory. Pathology. 1987 Jul;19(3):281–284. doi: 10.3109/00313028709066564. [DOI] [PubMed] [Google Scholar]
- Rubin J., Kirchner K., Walsh D., Green M., Bower J. Fungal peritonitis during continuous ambulatory peritoneal dialysis: a report of 17 cases. Am J Kidney Dis. 1987 Nov;10(5):361–368. doi: 10.1016/s0272-6386(87)80102-6. [DOI] [PubMed] [Google Scholar]
- Scroggs M. W., Wolfe J. A., Bollinger R. R., Sanfilippo F. Causes of death in renal transplant recipients. A review of autopsy findings from 1966 through 1985. Arch Pathol Lab Med. 1987 Oct;111(10):983–987. [PubMed] [Google Scholar]
- Ujhelyi M. R., Raasch R. H., van der Horst C. M., Mattern W. D. Treatment of peritonitis due to Curvularia and Trichosporon with amphotericin B. Rev Infect Dis. 1990 Jul-Aug;12(4):621–627. doi: 10.1093/clinids/12.4.621. [DOI] [PubMed] [Google Scholar]
- Vogelgesang S. A., Lockard J. W., Quinn M. J., Hasbargen J. A. Alternaria peritonitis in a patient undergoing continuous ambulatory peritoneal dialysis. Perit Dial Int. 1990;10(4):313–313. [PubMed] [Google Scholar]
- Wood C., Russel-Bell B. Characterization of pigmented fungi by melanin staining. Am J Dermatopathol. 1983 Feb;5(1):77–81. doi: 10.1097/00000372-198302000-00015. [DOI] [PubMed] [Google Scholar]
- Záruba K., Peters J., Jungbluth H. Successful prophylaxis for fungal peritonitis in patients on continuous ambulatory peritoneal dialysis: six years' experience. Am J Kidney Dis. 1991 Jan;17(1):43–46. doi: 10.1016/s0272-6386(12)80249-6. [DOI] [PubMed] [Google Scholar]