Abstract
Cervical spine instability in children is rare but not exceptional and may be due to many factors. Although it mostly occurs at the upper cervical spine, all vertebrae from the occiput to T1 may be involved. It may be acute or chronic, occurring secondary to trauma or due to congenital anomaly, skeletal or metabolic dystrophy or rheumatoid arthritis. It can be isolated or associated with other musculoskeletal or visceral anomalies. A thorough knowledge of embryology, anatomy, physiology and physiopathology of the cervical spine in children is essential to avoid pitfalls, recognize normal variants and identify children at risk of developing cervical spine instability and undertake the appropriate treatment.
Keywords: Pediatric cervical spine instability, Cervical spine subluxation, Atlantoaxial subluxation, Atlantoaxial rotatory dislocation, Atlantooccipital instability
Introduction
The cervical spine represents the most mobile spinal segment and is therefore more exposed to accidents which can sometimes lead to irreversible neurological complications. Anatomical and biomechanical differences between the developing child and the adult account for the different patterns of injury in these two groups.
A thorough knowledge of the anatomy, embryology and normal development of the pediatric cervical spine is essential to understand its specific problems and avoid pitfalls. Diseases are classified according to whether they involve the upper (occiput, C1, C2) or lower (C3–C7) cervical spine segments.
Anatomy and development
The cervical spine is made up of two anatomically and functionally distinct segments: the upper cervical spine (C1 and C2), which possesses the most rotational mobility with some degrees of frontal and sagittal plane mobility, and the lower cervical spine, which allows for two types of movements—flexion-extension and inclination–rotation [1].
The pediatric cervical spine has the distinguishing feature of being able to adapt to an abnormal situation of one or the other of the two segments. Thus, a decrease in upper cervical spine mobility results in an adaptive increase in the rotatory mobility of the lower segment. Range of motion of both of these segments decreases as the child gets older, being limited by osteoligamentous structures ensuring mechanical stability during growth.
Stabilizing features of cervical spine anatomy [2–5]
Cervical instability concerns mainly the upper cervical spine, particularly between C1 and C2.
Upper cervical bones and joints are intrinsically unstable. Articular facets would have little inherent stability if it were not for their capsuloligamentous attachments. The osseous anatomy of the lower cervical vertebrae resembles that of the thoracic or lumbar vertebrae, and the orientation of the unco-vertebral and zygoapophyseal joints between C3 and C7 contributes to some stability.
Ligaments are the main providers of upper cervical spine stability (Fig. 1).
Fig. 1.

Craniocervical ligaments of clinical relevance. a The most dorsal layer anterior to the spinal cord is the tectorial membrane (1), a continuation of the posterior longitudinal ligament. b Just anterior to the former lies the cruciate ligament. This important stabilizer of C1–2 anterior translation is composed of the transverse ligament (2), and triangular vertical bands extending cranially to the basion and caudally to C-2 (3). c The most anterior layer consists of the occipitoodontoid ligaments. These are the rudimentary apical ligament and the essential alar ligaments. The alar ligaments extend from the lateral aspect of the dens tip to the medial aspect of the occipital condyles. A lower portion of the alar ligament attaches to the medial aspect of the atlas lateral masses
Embryology
Certain aspects of embryology are important in order to fully understand cervical instability in children. Each vertebra develops from three primary ossification centers and later from secondary centers [6].
The first two cervical vertebrae are unique in their development, and the remaining five all develop similarly, from the caudal sclerotome half of one segment and the cranial sclerotome half of the succeeding segment [7]. The cranial half of the first cervical sclerotome, known as the proatlas contributes to the formation of the tip of the odontoid process and to the occipital condyles [8]. The vertebral arch of the atlas separates from its centrum and becomes the ring of C1; the separated centrum fuses with the proatlas above and the centrum of C2 below and becomes the odontoid process and body of C2. In summary, the atlas is made up of three main components—the anterior arch and the two lateral masses. The axis is made of four—the body, the two neural arches and the dens (or five components if the proatlas rudiment is considered).
The lower cervical vertebrae follow the normal formation scheme of the thoracic and lumbar vertebrae [9] with two lateral ossification centers and a third one for the body.
Growth and development (Fig. 2)
Fig. 2.
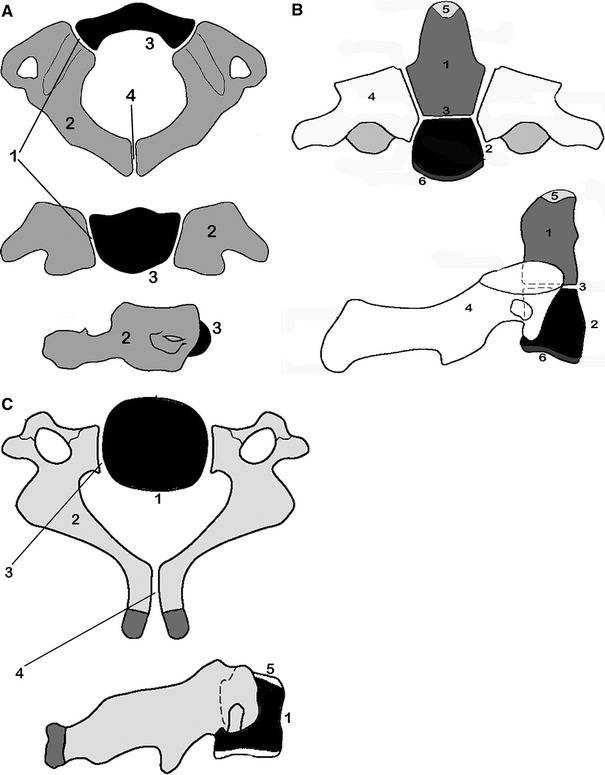
Development of the cervical vertebrae. a Atlas: the neurocentral synchondrosis (1) unites the neural arch (2) to the anterior arch (3) of the atlas. The ossification center of the anterior arch (3) appears between 6 months and 2 years of life. The posterior synchondrosis of the spinous processes (4) unites by 4–6 years of age, followed by the neurocentral synchondrosis (1), which fuses by about the seventh year. b Axis: the odontoid process (1) develops from two primary ossification centers that usually coalesce within the first 3 months of life; the C2 centrum (2) appears by the fifth fetal month and is separated from the dens (2) by the dentocentral synchondrosis (3). Neural arches (4) appear bilaterally by the seventh fetal month. Neural arches fuse posteriorly by the third year. The dentocentral synchondrosis (3) fuses at 3–6 years. Thus, both the posterior and the anterior synchondroses of C2 are closed by 6 years of age. The ossiculum terminale (5) at the tip of the dens appears between 5 and 8 years of age and fuses to the dens between 10 and 13 years of age. The inferior epiphyseal ring (6) appears at puberty and fuses at about 25 years of age. c Lower cervical vertebrae: the body (1) appears by the fifth fetal month. Neural arches (2) appear by the seventh to ninth fetal week. These are separated from the body by the neurocentral synchondroses (3), which close between 3 and 6 years of age. The posterior synchondrosis between the spinous processes usually unites by 2–4 years of age. Superior and inferior epiphyseal rings (5) appear at puberty, are involved in the vertical growth of the body and unite with the body at about 25 years
The developing spine is characterized by the presence of ossific centers joined by synchondroses. These can be confused with fractures and occasionally can be the site of injury.
Constitutional variants
Certain variations occur during embryogenesis and ossification of the cervical vertebrae and may be of interest in certain cases of cervical instability.
The posterior arch of C1 is sometimes in contact with, articulated with, or even coalesced with the posterior aspect of the foramen magnum, in which case the atlas is said to be occipitalized.
The tip of the odontoid process may develop enough to articulate with the anterior rim of the foramen magnum, producing a “basilar impression”. This variant is important in cases of “acute” cervical instability because of the greater risk of neurological insult. There may be compression of the brain stem and occurrence of neurological lesions by mechanical compression, vascular compromise or by changes in the cerebrospinal fluid circulation [10].
Terminology
From a clinical orthopedic point of view, joint instability occurs each time the anatomical relationships between the articular components are altered or have the propensity of becoming abnormal under the influence of certain solicitations (usually due to insufficiency or rupture of the stabilizing structures around the joint) [11, 12]. Vertebral instability has the distinguishing feature of associating a risk of neurological involvement with this architectural problem. This risk is greater because the problem occurs higher in the spine, and may lead to death in upper cervical spine instability.
Thus, a thorough knowledge of the terminology used in certain conditions is necessary to recognize some normal variants that may be mistaken for real instability situations. For example, it is necessary to differentiate “laxity”, “hypermobility” (its corollary), “fixed articular displacement”, “subluxation” and “dislocation”.
Clinical presentation
Cervical spine instability is frequently discovered accidently in an asymptomatic patient, especially in connective tissue disorders associated with ligamentous laxity, and in congenital anomalies. The second clinical picture is that of torticollis associated with variable trauma. Rarely is a neurological deficit the revealing clinical sign.
Imaging
Some of the radiographic parameters that indicate pathology of the cervical spine in adults represent normal developmental processes in children. As in adults, standard radiographs remain the main diagnostic tool of pediatric cervical instability [13]. Studies such as MRI and/or computed tomography scanning are reserved for complex cases in which a more detailed analysis of a congenital anomaly or a neurological impairment is warranted. Certain rules must be kept in mind to obtain good quality radiographs to minimize the risk of diagnostic errors:
Radiographs should be taken when possible on an awake patient, either sitting or standing, in order to see the patient’s true cervical lordosis, which tends to diminish in the supine position. If the radiograph must be taken supine, the child’s shoulders should be lifted from the table by bolsters [14, 15] because of the relatively larger head of the child.
The X-ray beam must be strictly perpendicular to the anatomical region to be examined.
The X-ray source should be at the farthest possible distance from the region examined (if a minimal distance of 2.75 m cannot be respected, a graduated scale should be radiographed next to the neck to account for radiographic magnification) [16, 17].
The lateral and open mouth odontoid views, although of little value in children younger than 5 years because of difficulty in interpretation [18, 19] are of extreme importance in the diagnosis of cervical instability in older children and adolescents. Oblique projections may be useful in some situations but are not part of the standard trauma series.
Atlantodens interval and space available for the cord (Fig. 3)
Fig. 3.

a, b The atlantodens interval (ADI) and the space available for cord (SAC) are used in determining atlantoaxial instability. The ADI increases as the SAC decreases. A SAC less than 13 mm is significant
The Atlantodens interval (ADI) is the space between the anterior aspect of the dens and the posterior aspect of the anterior ring of the atlas. An ADI of more than 5 mm on lateral radiographs indicates instability [1, 20]. This is more than the 3-mm adult value because of the increased cartilage content of the odontoid and ring of the atlas in children, as well as the increased ligamentous laxity in children. In extension, overriding of the anterior arch of the atlas on top of the odontoid also can be seen in up to 20% of children [21].
A mild increase in the ADI may indicate a subtle disruption of the transverse atlantal ligament. In adults, an ADI of 5 mm or more suggests such a disruption [22]. In chronic atlantoaxial conditions (e.g., rheumatoid arthritis, Down syndrome, congenital anomalies), the ADI is less useful. In children with these disorders, the ADI is frequently increased beyond the 3- to 5-mm range without disruption of the transverse atlantal ligaments. The complement of the ADI, the space available for the cord (SAC), is a more useful measure in this situation. This space is the distance between the posterior aspect of the dens and the anterior aspect of the posterior ring of the atlas or the foramen magnum. A SAC of less than 13 mm may be associated with neurological problems [23]. In doubtful cases, a flexion-extension MRI is extremely useful in evaluating the SAC and repercussions on the brain stem or the spinal cord [24, 25].
In patients in whom there is an attenuation of the transverse atlantal ligament without rupture, the alar ligament provides some stability. It acts like a checkrein [26], first tightening up in rotation, then becoming completely taut as the odontoid process continues to rotate and move posteriorly for a distance equivalent to its full transverse diameter. This safety zone between the anterior wall of the spinal canal of the atlas, the axis, and the neural structures is an anatomic constant equal to the transverse diameter of the odontoid. This constant defines Steel’s rule of thirds: one-third cord, one-third odontoid and one-third space (safe zone) (Fig. 4) [26]. This rule remains constant throughout the growth of the cervical spine [27]. It is here that the alar ligament becomes taut, acting as a checkrein and secondary restraint, preventing further movement of the odontoid into the cord. In the chronic situation, it is important to recognize when this safe zone has been exceeded and the child enters the region of impending spinal cord compression. In the case of trauma, the alar ligament is insufficient to prevent a fatal cord injury in the event of another neck injury similar to the one that caused the initial interruption of the transverse atlantal ligament.
Fig. 4.
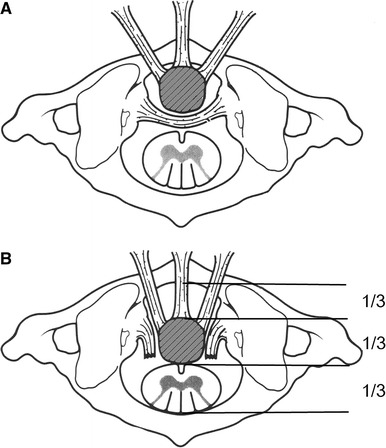
a, b Drawing showing the free space according to Steel’s rule of thirds
Atlantooccipital motion
Normal ranges of motion at the atlantooccipital joint are not well defined. In a series of 40 normal college freshmen, the tip of the odontoid remained directly below the basion of the skull in both flexion and extension [28]. Thus, the joint should not allow any horizontal translation during flexion and extension. Tredwell and colleagues [29] believe that a posterior displacement at the atlantooccipital joint of more than 4 mm in extension indicates instability. This can be measured as the distance between the anterior margin of the condyles at the base of the skull and the sharp contour of the anterior aspect of the concave joint of the atlas anteriorly, or as the distance between the occipital protuberance and the superior arch of the atlas posteriorly. The Powers ratio is used to assess the position of the skull base relative to the atlas and is another way of evaluating the atlantooccipital region (Fig. 5a). The value should be between 0.7 and 1; a higher value indicates anterior subluxation of the atlantooccipital joint and a lower value indicates a posterior subluxation. Another method to measure posterior subluxation of the atlantooccipital joint is that of Wiesel and Rothman [30] (Fig. 5b).
Fig. 5.

aThe powers ratio is determined by drawing a line from the basion (b) to the posterior arch of the atlas (c) and a second line from the opisthion (O) to the anterior arch of the atlas (a). The length of the line BC is divided by the length of the line OA, producing the Powers ratio. The problem lies in the fact that the basion is not always visible on plain X-rays. A value less than 0.7 and 1 suggests a posterior subluxation, whereas a value greater than 1 indicates an anterior subluxation. b The Wiesel and Rothman method consists of drawing a line that connects the anterior and posterior arches of the atlas. Two lines perpendicular to this one are then drawn, one through the basion and one through the posterior margin of the anterior arch of the atlas. The distance (x) between these two lines should not change by more than 1 mm in flexion and extension
Intervertebral relationships of the lower cervical spine
The C2–C3 interspace and, to a lesser extent, the C3–C4 interspace in children have a normal physiological displacement. In a study of 161 normal children [21], marked anterior displacement of C2 on C3 was observed in 9% of children between 1 and 7 years of age. In some children, the anterior physiological displacement of C2 on C3 is so pronounced that it appears pathological (pseudosubluxation). To differentiate this from pathological subluxation, Swischuk [31] has used the posterior cervical line drawn from the anterior cortex of the posterior arch of C1 to the anterior cortex of the posterior arch of C3 (Fig. 6). In physiological displacement of C2 on C3, the posterior cervical line may pass through the cortex of the posterior arch of C2, touch the anterior aspect of the cortex of the posterior arch of C2, or come within 1 mm of the anterior cortex of the posterior arch of C2. A Swischuk line passing 2 mm or more behind the anterior cortex of the posterior arch of C2 indicates a pathological anterior displacement of C2 over C3.
Fig. 6.

The posterior line of Swischuk, showing the normal limits. a Passing through or just behind the anterior cortex of C-2. b Coming within 1 mm of the anterior aspect of the cortex of C-2. c Touching the anterior aspect of the cortex of C-2
The planes of the articular facets change with growth. The horizontal orientation of the facet joints along with the relative ligamentous laxity and relatively larger skull than in the trunk in young children contribute to this common finding of pseudosubluxation. No treatment is needed for this normal “physiological subluxation” [32, 33].
Variations in the curvature and growth of the cervical spine
In the transversal radiographic study of Catell and Filtzer [21], 16% of normal children showed marked angulation at a single interspace, suggestive of injury to the interspinous or posterior longitudinal ligament, and 14% showed absence of the normal lordosis in neutral position. All of these signs could be erroneously interpreted as changes secondary to injury [34].
The dentocentral synchondrosis may be visible in vestigial forms up to 11 years of age [21], and may be erroneously interpreted as an undisplaced fracture or even a non-union of an old fracture. Similarly, the ossiculum terminale may appear by 5 years of age, although it most typically appears around 8 years of age. This also can be misinterpreted as an odontoid tip fracture.
Wedging of the C3 vertebral body is a normal radiographic finding in 7% of younger children [35]. A MRI or a CT scan will demonstrate fracture lines through the body if one is present and help distinguish it from a normal variation.
Clinical instability disorders and their treatment
Instabilities of malformative origin
Instabilities of malformative origin are the result of congenital anomalies, mainly in the upper cervical spine [36].
Atlantooccipital anomalies
C1–C2 instability is present in up to 50% of congenital atlantooccipital anomalies. Flexion-extension MRI is often necessary to fully evaluate the pathology [25]. Anterior compression of the brainstem or cervical cord occurs from posterior displacement of the odontoid process. This results in a wide range of manifestations, depending on the site and severity of compression. Pyramidal tract signs and symptoms are most common, although signs of lower cranial nerve involvement can be seen. Compression from the posterior lip of the foramen magnum or dural constricting band can disturb the posterior columns, with a loss of proprioception, vibration and tactile senses. Nystagmus may occur as a result of posterior cerebellar compression. Vascular disturbances from vertebral artery involvement can result in brainstem ischemia, manifested by syncope, seizures, vertigo and unsteady gait. Cerebellar tonsil herniation can occur. The altered mechanics of the cervical spine may result in a dull, aching pain in the posterior neck, with intermittent stiffness and torticollis. Irritation of the greater occipital nerve may cause tenderness in the posterior scalp [37].
The natural history of atlantooccipital anomalies is unknown. The neurological symptoms may develop very late, and show slow progression, because the associated C1–C2 instability progresses with age, and the increased strain placed on the C1–C2 interval produces gradual spinal cord or vertebral artery compromise.
Treatment is difficult. Surgery for atlantooccipital anomalies is more risky than for isolated anomalies of the odontoid [38, 39]. For this reason, nonoperative methods should be attempted initially. Cervical collars, braces, and traction often help for persistent complaints of head and neck pain, especially after minor trauma or infection. Immobilization may achieve only temporary relief if neurological deficits are present. Patients with evidence of a compromised upper cervical area should take precautions not to expose themselves to undue trauma.
When symptoms and signs of C1–C2 instability are associated with atlantooccipital anomalies, a posterior occiput-C2 fusion is indicated. Preliminary traction to attempt reduction is used if necessary. If reduction is possible and there are no neurological signs, surgery has a better outcome [38–40]. In posterior instability, there is an increased risk of pseudarthrosis and graft resorption after isolated posterior fusion. An anterior transoral fusion can be offered, but its results are variable due to the relatively thin anterior border of the occiput. Posterior signs and symptoms may be an indication of posterior decompression, depending on the evidence of dural or osseous compression. Results vary from complete resolution to increased deficits and death [38, 41]. In the instance of no instability but only compressive pathology, the role of concomitant posterior fusion has not yet been determined. However, if decompression destabilizes the spine, concomitant posterior fusion should be considered.
Unilateral absence of C1
Unilateral absence of C1 ranges from hypoplasia of a lateral mass to complete agenesis of a hemiatlas with rotatory instability and basilar impression [42, 43]. Two-thirds of the children present with symptoms at birth; the others develop torticollis and are noticed later. Neck flexibility is variable and decreases with age. The condition is not painful. Neurological signs are present in about a quarter of the patients. The natural history is unknown.
Standard anteroposterior and lateral radiographs rarely give the diagnosis, although the open-mouth odontoid view may suggest it. Tomograms or CT scans usually are needed to visualize the anomaly. Occasionally, the atlas is occipitalized.
The deformity should be observed to document the presence or absence of progression. This observation is primarily clinical (e.g., photographic), because radiographic measurements are difficult if not impossible to obtain. Bracing does not halt the progression of the deformity. Surgical intervention is recommended in those patients with severe deformities. A posterior fusion from the occiput-C2 or occiput-C3 with or without decompression is performed. The ideal age for posterior fusion is between 5 and 8 years, corresponding to the age at which the canal size reaches adult proportions.
Aplasia of the odontoid
Aplasia of the odontoid ranges from mild hypoplasia to complete aplasia. It may be isolated or be part of a complex of syndromes, and is often an incidental finding. Its clinical relevance lies in the associated atlantoaxial instability which may be in flexion, extension or multidirectional.
Treatment is only surgical because of the high risk of neurological complications following the mildest trauma. In some instances, it is discovered in adults seeking treatment for cervical pain or repetitive torticollis. The resulting hypermobility may produce a pannus similar to that seen in rheumatoid arthritis.
Os odontoideum
Os odontoideum is a rare anomaly characterized by a transverse gap dividing the odontoid process separating the apical segment from the basilar segment [44, 45]. Some advocate a congenital cause, whereas others incriminate a mechanical and vascular compromise leading to segmental necrosis of the odontoid process. The exact etiology, however, remains unknown [46].
Neck pain is the usual presentation. Presentations attributable to vertebral artery compression from instability are less common. Sudden death rarely occurs.
Radiographs show an oval or round ossicle with a smooth border located in the position of the odontoid tip. It is sometimes difficult to differentiate this entity from non-union following a fracture. Flexion-extension lateral radiographs are useful to assess instability, and MRI and CT scan are useful to analyze bony anatomy and any possible impact on the nervous system.
Hypermobility at the C1–C2 level may cause transient occlusion of the vertebral artery. Patients with pain or transient myelopathies often recover with immobilization. Strenuous activities should be avoided. The long-term natural history is unknown.
Surgery is indicated for those with an ADI of 10 mm or more, a SAC of 13 mm or less on flexion radiographs [23], neurological involvement, progressive instability and persistent neck pain. A posterior C1–C2 fusion, or rarely occiput-C2, is the procedure of choice. Internal fixation using sublaminar wires must be avoided because the os odontoidum may be pulled back into the canal with disastrous consequences. Halo cast is a preferred method of fixation.
Fixed atlantoaxial rotatory displacement
Atlantoaxial rotatory displacement is a common cause of childhood torticollis and has many etiologies.
Interpretation of radiographs is difficult [47]. On open mouth views, the lateral mass of C1 that has rotated anteriorly appears wider and closer to the midline (medial offset), whereas the opposite lateral mass is narrower and away from the midline (lateral offset) (Fig. 7). The facet joints may be obscured because of apparent overlapping. The lateral view shows the wedge-shaped lateral mass of the atlas lying anteriorly where the oval arch of the atlas normally lies, and the posterior arches fail to superimpose because of the head tilt. The normal relationship between the occiput and C1 is preserved.
Fig. 7.
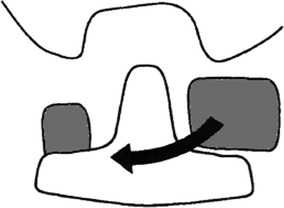
Schematic anteroposterior view revealing the relationship of the lateral masses of C1 to the odontoid with fixed atlantoaxial displacement. The lateral mass rotating anteriorly appears broader, more cephalad and closer to the midline odontoid process (medial offset) than the lateral mass rotating posteriorly, which appears narrower and further from the odontoid (lateral offset)
The C1–C2 “rotatory dislocation”, as defined initially by Fielding and Hawkins, is classified into four types [48] (Fig. 8).
Type 1 is a simple rotatory displacement without an anterior shift.
Type 2 is rotatory displacement with an anterior shift of 5 mm or less.
Type 3 is rotatory displacement with an anterior shift greater than 5 mm.
Type 4 is rotatory displacement with a posterior shift.
When considering anatomic variations of the cervical spine, and physiological limits of the ADI, types 1 and 2 may correspond to a normal atlantoaxial articulation fixed in a vicious rotatory position. This was confirmed by our unpublished study on 20 children without any cervical problems [49]. A CT scan was performed in the position of extreme torticollis to the right then to the left (40 positions). Four independent radiologists interpreted the results independently and classified only 24 cases as normal; 14 were classified type 1 and two as type 2. Types 3 and 4 are very rare and may produce neurological complications.
Fig. 8.
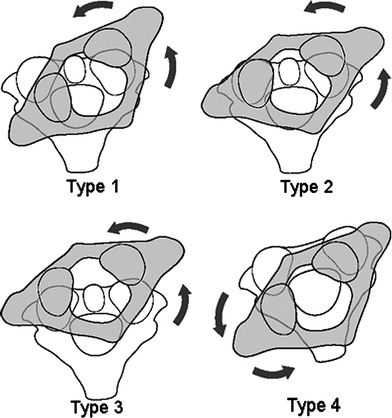
Fielding classification of rotary displacement in atlantoaxial rotatory displacement (refer to text)
The child with rotatory displacement presents with a torticollis and resists any attempt to move the head because of pain. The associated muscle spasm is noted on the side of the long sternocleidomastoid muscle because the muscle is attempting to correct the deformity, unlike congenital muscular torticollis, in which the muscle causes the torticollis. If the deformity becomes fixed, the pain subsides but the torticollis persists, along with decreased neck motion. In long-standing cases, plagiocephaly and facial flattening may develop on the side of the tilt.
Etiology and pathology are not well known [50]. The atlantoaxial rotatory displacement occurs predominantly after a minor trauma, a surgery of the head and neck or following an infection of the upper respiratory tract.
Spontaneous atlantoaxial subluxation with inflammation of adjacent neck tissues, also known as Grisel’s syndrome, is commonly seen in children after upper respiratory tract infections. A direct connection exists between the pharyngovertebral veins, the periodontal venous plexus and suboccipital epidural sinuses [51]. This anatomic feature facilitates the translocation of pharyngovertebral inflammatory products to the upper cervical spine, which causes spastic contracture of cervical muscles with subsequent rotatory C1–C2 displacement.
Most atlantoaxial rotatory displacements resolve spontaneously. Treatment depends on the duration of symptoms and the severity of neck deformity [52].
Patients with symptoms of less than 1 week duration should be treated by means of immobilization in a soft cervical collar and rest for about 1 week. If spontaneous reduction does not occur after this initial treatment, hospitalization and the use of halo traction, muscle relaxants (e.g., diazepam) and analgesics are recommended.
Patients with rotatory subluxation of more than 1 week but less than 1 month should be hospitalized for cervical traction, muscle relaxants and analgesics. A halo cast is occasionally needed to achieve reduction.
In patients with rotatory subluxation of more than 1 month, cervical traction may be tried for up to 3 weeks, but the chances of achieving closed reduction are minimal.
Indications for surgical management are: deformity for more than 3 months, impossibility of reaching or maintaining the correction, recurrence of the deformity following nonsurgical treatment, presence of neurological signs and persistence of abnormal anterior displacement.
Before surgery, halo traction for several days is used to obtain as much straightening of the head and neck as possible; this may not translate into a full anatomical reduction of C1–C2 dislocation. Forceful or manipulative reduction should not be attempted [53]. Following traction, halo-cast is installed in the most physiological position of the head and neck. In situ posterior C1–C2 fusion is then performed with the halo-cast in place. The latter is kept for a minimum period of 3 months. A fusion in a position of incomplete reduction will be compensated for by a progressive adaptation of the lower cervical spine [54].
Traumatic instability
Children younger than 11 years of age are more likely to sustain ligamentous injuries and fractures to the upper cervical spine. Adolescents, however, more frequently sustain fractures and injuries to the lower cervical spine [55, 56].
If after a trauma, a child is comatose, unconscious or complaining of neck pain, cervical spine radiographs should be done [57]. The views recommended are the anteroposterior, the cross-table lateral and the open-mouth views. A unique lateral view can be made if the child is critically ill.
Attention must be made when a baby is positioned on a standard backboard because the relatively large head will lead to a flexed posture of the neck; this can eventually lead to further anterior displacement of an unstable cervical spine. To avoid this problem, the chest may be raised by a double mattress or bolster.
If instability is suspected, dynamic radiographs (flexion-extension) should be performed. Ligamentous injury may not be seen immediately and dynamic views 10–15 days later may document instability [58, 59].
Indirect signs raising the suspicion of fracture or subluxation are malalignment of spinous processes on the anteroposterior view, highly suspicious of a jumped facet or an increased interspinous distance [60], suspicious of a posterior ligamentous injury.
CT scan is useful to assess an abnormal radiograph of the cervical spine or for planning treatment. MRI will help in assessing the spinal cord and discs and is of premium importance when evaluating a “Spinal Cord Injury Without Radiographic Abnormality” (SCIWORA).
Fractures and ligamentous injuries of the upper cervical spine
Atlantooccipital dislocation
Atlantooccipital dislocation is rare in childhood [61, 62]. Deployment of air bags has been associated with this injury in children [63]. Most cases present with complete tetraplegia and survive only by ventilator support. Some present with hypotension, tachycardia or a cardiac arrest [64].
The diagnosis is sometimes difficult. A distance of more than 12.5 mm between the dens and the basion suggest the possibility of atlantooccipital dislocation [61]. CT scan or MRI may be useful to ascertain the diagnosis. Immobilization with a rigid collar and cardiorespiratory support constitute the first approach to treatment, and immobilization with halo-cast associated in severe cases with a posterior occiput-C1 or occiput-C2 fusion with or without instrumentation are the essentials of treatment [65, 66]. Traction has to be avoided as it causes articular distraction with additional neurological compromise.
Fractures of the atlas
The Jefferson fracture is rare in children [67, 68]. It is caused by an axial load from the head into the lateral masses. CT scans are useful in both the diagnosis of this injury and the assessment of healing. This injury is usually not visible on radiographs. Treatment is usually simple immobilization with a Minerva or halo-cast. Surgery is rarely indicated unless there is a rupture of the transverse alar ligament, which renders the spine unstable [69].
Transverse ligament ruptures
Isolated ruptures of the transverse ligament may occur from either mild or severe trauma [43]. The ADI is increased more than 5 mm. Adequate ligamentous healing is difficult to obtain by simple immobilization. The recommended treatment is a C1–C2 posterior fusion with instrumentation [70] or an immobilization with halo-cast.
Odontoid fractures
Odontoid fractures are a common pediatric cervical spine injury [71]. They are usually physeal fractures of the dentocentral synchondrosis. Neurological problems are rare. These fractures are usually displaced anteriorly with posterior angulation of the odontoid and are best seen on lateral radiographs.
The fractures with anterior displacement are easily reduced by mild extension and posterior translation, and immobilized with a rigid collar or halo-cast. Healing is rapid and immobilization can usually be stopped after 6–10 weeks. These injuries have a low rate of non-union and do not require a C1–C2 fusion [72].
Spondylolisthesis of C2
Also known as “hangman fractures” in adults, this injury is rare in children. It occurs following a trauma in hyperextension. These fractures heal with immobilization (rigid collar or halo-cast) after gentle reduction. A posterior C1–C3 fusion is reserved for rare cases of non-union or instability [73].
Fractures and ligamentous injuries of the lower cervical spine
Only injuries with potential instability are discussed here. These lesions are more common in older children and adolescents [56, 74]. The typical patterns of these fractures are compression fractures of the vertebral body, or facet fractures and dislocation caused by hyperflexion. These injuries are like those of adults and the same treatment patterns apply. Physeal fractures are frequently missed in severely injured children [75], and instability may occur with subsequent neurological injuries. Simple installation in cervical extension is all that is needed to achieve reduction. Immobilization is done with a rigid collar or a halo-cast. Healing is fast, as for all physeal injuries.
Post-traumatic ligamentous instability may occur [59]. The upper cervical spine offers little resistance to traumatic shear forces, which often result in ligamentous injuries. The problem is to differentiate between this entity and pseudosubluxation using the posterior cervical line (Fig. 9). In one study, 7 of 11 ligamentous pediatric cervical spine injuries occurred at the C2–C3 level [76]. Treatment of mild sprains is immobilization for comfort followed by dynamic radiographs 10–15 days later to ensure that late instability does not occur. Posterior cervical fusion with external fixation using halo-cast is indicated for persistent instability.
Fig. 9.

Case of a 10-year-old boy with persistent neck pain 3 months following a cervical spine trauma. a Lateral radiographic view of the cervical spine. b Flexion view: subluxation of C2 over C3 with local kyphosis of 20°. c MRI showing no abnormalities. d CT scan in flexion: anterior displacement is within the normal physiological range (Swischuk line)
Developmental or dystrophic instability
Down syndrome
Because of collagen abnormalities, children with Down syndrome have articular laxity with potential instability. The latter is more common at the upper cervical spine. The incidence of atlantooccipital hypermobility may be as high as 60% [29] in children and 69% in adults [77]. Most cases are asymptomatic [78, 79]. No guidelines exist regarding the frequency of periodic screening or surgical indications, except for symptomatic children in whom atlantooccipital fusion is indicated [80, 81]. Tredwell and colleagues [29] believe that treatment plans should depend on the amount of space available for the cord rather than on absolute values of displacement.
The incidence of C1–C2 instability in children with Down syndrome ranges from 7.6 to 22% [29, 82–84]. The incidence of symptomatic atlantoaxial instability is much less and varies between 0 and 2.6% [84]. In a yet-to-be-published study on 442 patients with Down syndrome [85], we found mild neurological symptoms in 42% of the cases. None of the patients had major neurological problems.
Rarely does sudden death occur. Most patients have had weeks or years of mild neurological symptoms prior to the catastrophic injury.
Identification of children at risk for dangerous C1–C2 instability is difficult. The systematic radiographic screening for instability is of unproven value [79, 86]. A regular clinical assessment is much more helpful. Parental education regarding the early signs of myelopathy is extremely important (e.g., frequent falls, deterioration of upper limb function). Radiographs should include anteroposterior and lateral views of the cervical spine and of C1–C2 (open mouth and lateral views). Flexion-extension radiographs should also be done.
Treatment of C1–C2 instability ranges from simple avoidance of accidents to surgical fusion. Surgery is indicated for cases with recent or progressive neurological deficit. Posterior cervical fusion of the pathological levels with prolonged immobilization (3–6 months) using halo-cast is the procedure of choice. The incidence of non-union following surgery is not negligible.
Postoperative neurological improvement is indirectly proportional to the duration of neurological symptoms before intervention [87].
Neurofibromatosis
Radiographic features of neurofibromatosis in the cervical spine are vertebral body deficiencies and dysplasia. Although instability is rare, lateral flexion-extension radiographs are recommended before general anesthesia or surgery [88].
Clinical follow-up is the rule in the absence of neurological signs. If symptomatic, surgery is indicated. The strategy is similar to that for those with Down syndrome’s. Non-unions are frequent after isolated posterior fusion. A circumferential fusion is recommended because of vertebral dystrophy.
Neurological instabilities (cerebral palsy)
Angular and listhetic instabilities are more frequent in athetoid cerebral palsy [89]. Disc degeneration develops early and involves multiple levels. The combination of disc degeneration and listhetic instability predisposes these patients to progressive neurological deficit. Symptoms range from mild brachialgia to tetraparesia [90–92]. Treatment is mainly surgical with posterior fusion with or without instrumentation.
Post-laminectomy instability
Laminectomy is a cause of gradual instability in children, with a progressive kyphosis rather than an acute intervertebral displacement. This problem is more common in the immature growing child [14, 93–99]. If not treated, cuneiformisation of the vertebral body with anterior translation may occur, leading ultimately to swan-neck deformity [98].
Laminoplasty was described by Raimondi as a surgical modification to avoid post-laminectomy kyphosis [100, 101]. Severe and progressive deformities are managed by circumferential fusion [95].
Rheumatismal instability (juvenile rheumatoid arthritis)
Juvenile rheumatoid arthritis is a chronic synovitis that can affect the joints of the cervical spine. The subtypes that usually involve the cervical spine are the polyarticular and systemic onset types; only rarely does the pauciarticular type affect the cervical spine [102]. Cervical spine involvement usually occurs in the first 1–2 years from the disease onset and presents with stiffness. Subluxation of C1–C2 or inferior cervical spine is possible [102].
Treatment is essentially non-surgical. Patients rarely develop flexion deformity; a cervical collar may prevent this [103]. Fusion is rarely indicated except for children with certified instability or progressive neurological deterioration.
Other syndromes
Mucopolysaccharidoses [104–107]
Morquio disease is characterized by C1–C2 instability and cervical stenosis due to incarceration of the posterior arch of C1 and the high incidence of associated pannus. Particular attention should be paid when intubating these patients.
Surgical treatment is indicated whenever there is instability, or recent or progressive neurological deficit. Cautious excision of the posterior arch of C1 with posterior occiput-C2 or C3 fusion is the treatment of choice.
Skeletal dysplasias
The problem usually seen in skeletal dysplasias is cervical stenosis [108]. However, instability is not exceptional. Treatment plans follow the same rules as for congenital and developmental instabilities.
Larsen syndrome [109–112]
Instability is frequent at the C1–C2 level. Another feature is lysis of the pedicles of C2, leading to displacement of C2 over C3. When general anesthesia has to be done, careful intubation under fibroscopic guidance is mandatory. Posterior occiput-C2 or C3 fusion is performed whenever neurological complications are of concern. Anterior fusion is associated in the presence of vertebral body hypoplasia with angular kyphosis.
Conclusion
Instability of the cervical spine is a relatively frequent problem in pediatric orthopedics. Good diagnostic and therapeutic plans cannot be achieved without a thorough knowledge and understanding of the anatomical and physiological characteristics of the child’s cervical spine.
References
- 1.Pennecot GF, Gouraud D, Hardy JR, Pouliquen JC. Roentgenographical study of the stability of the cervical spine in children. J Pediatr Orthop. 1984;4:346–352. doi: 10.1097/01241398-198405000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Dvorak J, Panjabi MM. Functional anatomy of the alar ligaments. Spine. 1987;12:183–189. doi: 10.1097/00007632-198703000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Dvorak J, Schneider E, Saldinger P, Rahn B. Biomechanics of the craniocervical region: the alar and transverse ligaments. J Orthop Res. 1988;6:452–461. doi: 10.1002/jor.1100060317. [DOI] [PubMed] [Google Scholar]
- 4.Ebraheim NA, Yang H, Lu J, Biyani A, Yeasting RA. Cartilage and synovium of the human atlanto-odontoid joint. An anatomic and histological study. Acta Anat. 1997;159:48–56. doi: 10.1159/000147964. [DOI] [PubMed] [Google Scholar]
- 5.Panjabi M, Dvorak J, Crisco J, Oda T, Hilibrand A, Grob D. Flexion, extension, and lateral bending of the upper cervical spine in response to alar ligament transections. J Spinal Disord. 1991;4:157–167. doi: 10.1097/00002517-199106000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Clavert JM (1989) Embryologie du rachis. In: Bollini G, Bouyala JM (eds) Chirurgie et orthopédie du rachis. Sauramps médical, Montpellier, pp 21–28
- 7.O’Rahilly R, Meyer DB. The timing and sequence of events in the development of the human vertebral column during the embryonic period proper. Anat Embryol. 1979;157:167–176. doi: 10.1007/BF00305157. [DOI] [PubMed] [Google Scholar]
- 8.Sensenig EC. The development of the occipital and cervical segments and their associated structures in human embryos. Contrib Embryol Carnegie Inst. 1957;36:141–151. [Google Scholar]
- 9.O’Rahilly R, Muller F, Meyer DB. The human vertebral column at the end of the embryonic period proper. 1. The column as a whole. J Anat. 1980;131:565–575. [PMC free article] [PubMed] [Google Scholar]
- 10.Taylor AR, Chakravorty BC. Clinical syndromes associated with basilar impression. Arch Neurol. 1964;10:475–484. doi: 10.1001/archneur.1964.00460170045008. [DOI] [PubMed] [Google Scholar]
- 11.Nuckley DJ, Hertsted SM, Eck MP, Ching RP. Effect of displacement rate on the tensile mechanics of pediatric cervical functional spinal units. J Biomech. 2005;38:2266–2275. doi: 10.1016/j.jbiomech.2004.09.021. [DOI] [PubMed] [Google Scholar]
- 12.Ouyang J, Zhu Q, Zhao W, Xu Y, Chen W, Zhong S. Biomechanical assessment of the pediatric cervical spine under bending and tensile loading. Spine. 2005;30:716–723. doi: 10.1097/01.brs.0000192280.53831.70. [DOI] [PubMed] [Google Scholar]
- 13.Lustrin ES, Karakas SP, Ortiz AO, Cinnamon J, Castillo M, Vaheesan K, Brown JH, Diamond AS, Black K, Singh S. Pediatric cervical spine: normal anatomy, variants, and trauma. Radiographics. 2003;23:539–560. doi: 10.1148/rg.233025121. [DOI] [PubMed] [Google Scholar]
- 14.Curran C, Dietrich AM, Bowman MJ, Ginn-Pease ME, King DR, Kosnik E. Pediatric cervical-spine immobilization: achieving neutral position. J Trauma. 1995;39:729–732. doi: 10.1097/00005373-199510000-00022. [DOI] [PubMed] [Google Scholar]
- 15.Treloar D. Neutral cervical spine positioning in children. Ann Emerg Med. 1994;23:208–211. doi: 10.1016/s0196-0644(94)70032-x. [DOI] [PubMed] [Google Scholar]
- 16.Bell DF, Walker JL, O’Connor G, Tibshirani R. Spinal deformity after multiple-level cervical laminectomy in children. Spine. 1994;19:406–411. doi: 10.1097/00007632-199402001-00005. [DOI] [PubMed] [Google Scholar]
- 17.Ghanem I. Le rachis cervical instable de l’enfant. In: Duparc J, editor. Cahiers d’enseignement de la SOFCOT. Paris: Expansion Scientifique Française; 2006. pp. 289–321. [Google Scholar]
- 18.Buhs C, Cullen M, Klein M, Farmer D. The pediatric trauma C-spine: is the ‘odontoid’ view necessary? J Pediatr Surg. 2000;35:994–997. doi: 10.1053/jpsu.2000.6951. [DOI] [PubMed] [Google Scholar]
- 19.Swischuk LE, John SD, Hendrick EP. Is the open-mouth odontoid view necessary in children under 5 years? Pediatr Radiol. 2000;30:186–189. doi: 10.1007/s002470050043. [DOI] [PubMed] [Google Scholar]
- 20.Locke GR, Gardner JI, van Epps EF. Atlas-dens interval (ADI) in children: a survey based on 200 normal cervical spines. Am J Roentgenol. 1966;97:135–140. doi: 10.2214/ajr.97.1.135. [DOI] [PubMed] [Google Scholar]
- 21.Catell HS, Filtzer DL. Pseudosubluxation and other normal variations in the cervical spine in children. J Bone Joint Surg Am. 1965;47:1295–1309. [PubMed] [Google Scholar]
- 22.Fielding JW, Cochran GVB, Lawsing JF, III, Hohl M. Tears of the transverse ligament of the atlas: a clinical and biomechanical study. J Bone Joint Surg Am. 1974;56:1683–1691. [PubMed] [Google Scholar]
- 23.Spierings ELH, Braakman R. The management of os odontoideum. J Bone Joint Surg Br. 1982;64:422–428. doi: 10.1302/0301-620X.64B4.7096415. [DOI] [PubMed] [Google Scholar]
- 24.Volle E. Functional magnetic resonance imaging—video diagnosis of soft-tissue trauma to the craniocervical joints and ligaments. Int Tinnitus J. 2000;6:134–139. [PubMed] [Google Scholar]
- 25.Weng MS, Haynes RJ. Flexion and extension cervical MRI in a pediatric population. J Pediatr Orthop. 1996;16:359–363. doi: 10.1097/00004694-199605000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Steel HH. Anatomical and mechanical considerations of the atlanto-axial articulations. J Bone Joint Surg Am. 1968;50:1481–1482. [Google Scholar]
- 27.Jauregui N, Lincoln T, Mubarak S, Garfin S. Surgically related upper cervical spine canal anatomy in children. Spine. 1993;18:1939–1944. doi: 10.1097/00007632-199310001-00002. [DOI] [PubMed] [Google Scholar]
- 28.El-Khoury GY, Clark CR, Dietz FR, Harre RG, Tozzi JE, Kathol MH. Posterior atlantooccipital subluxation in Down syndrome. Radiology. 1986;159:507–509. doi: 10.1148/radiology.159.2.2938213. [DOI] [PubMed] [Google Scholar]
- 29.Tredwell SJ, Newman DE, Lockitch G. Instability of the upper cervical spine in Down syndrome. J Pediatr Orthop. 1990;10:602–606. doi: 10.1097/01241398-199009000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Wiesel SW, Rothman RH. Occipitoatlantal hypermobility. Spine. 1979;4:187–191. doi: 10.1097/00007632-197905000-00001. [DOI] [PubMed] [Google Scholar]
- 31.Swischuk LE. Anterior displacement of C2 in children: physiologic or pathologic. A helpful differentiating line. Radiology. 1977;122:759–763. doi: 10.1148/122.3.759. [DOI] [PubMed] [Google Scholar]
- 32.Ralston ME. Physiologic anterior subluxation: case report of occurrence at C5 to C6 and C6 to C7 spinal levels. Ann Emerg Med. 2004;44:472–475. doi: 10.1016/j.annemergmed.2004.05.024. [DOI] [PubMed] [Google Scholar]
- 33.Goni Orayen C, Perez Martinez A, Martin Martinez C, Asensio Llorente M, Peiro Ibanez JL, de Diego Suarez M. Pseudosubluxation of C2-C3 in childhood: a frequent clinico-radiological diagnostic error. Esp Pediatr. 1992;36:390–392. [PubMed] [Google Scholar]
- 34.Penning L. Normal movements of the cervical spine. Am J Roent. 1978;130:317–326. doi: 10.2214/ajr.130.2.317. [DOI] [PubMed] [Google Scholar]
- 35.Swischuk LE, Swischuk PN, John SD. Wedging of C-3 in infants and children: usually a normal finding and not a fracture. Radiology. 1993;188:523–526. doi: 10.1148/radiology.188.2.8327708. [DOI] [PubMed] [Google Scholar]
- 36.Dubousset JF (1993) Approche clinique diagnostique et thérapeutique des malformations congénitales du rachis cervical chez l’enfant. In Mallet JF, Lechevallier J. Chirurgie et orthopédie du rachis cervical de l’enfant. Sauramps médical, Montpellier, pp 115–124
- 37.Dubousset JF, Queneau P. Les malformations de la charniere cranio-rachidienne chez l’enfant: formes anatomo-cliniques et indications therapeutiques. Rev Chir Orthop. 1981;67:383–394. [PubMed] [Google Scholar]
- 38.Bharucha EP, Dastur HM. Craniovertebral anomalies (a report on 40 cases) Brain. 1964;87:469–480. doi: 10.1093/brain/87.3.469. [DOI] [PubMed] [Google Scholar]
- 39.Wadia NH. Myelopathy complicating congenital atlantoaxial dislocation (a study of 28 cases) Brain. 1967;90:449–472. doi: 10.1093/brain/90.2.449. [DOI] [PubMed] [Google Scholar]
- 40.Greenberg AD. Atlantoaxial dislocation. Brain. 1968;91:655–684. doi: 10.1093/brain/91.4.655. [DOI] [PubMed] [Google Scholar]
- 41.Nicholson JT, Sherk HH. Anomalies of the occipitocervical articulation. J Bone Joint Surg Am. 1968;50:295–304. doi: 10.2106/00004623-196850020-00008. [DOI] [PubMed] [Google Scholar]
- 42.Dubousset J. Torticollis in children caused by congenital anomalies of the axis. J Bone Joint Surg Am. 1986;68:178–188. [PubMed] [Google Scholar]
- 43.Hosalkar HS, Gerardi JA, Shaw BA. Combined asymptomatic congenital anterior and posterior deficiency of the atlas. Pediatr Radiol. 2001;31:810–813. doi: 10.1007/s002470100542. [DOI] [PubMed] [Google Scholar]
- 44.Choit RL, Jamieson DH, Reilly CW. Os odontoideum: a significant radiographic finding. Pediatr Radiol. 2005;35:803–807. doi: 10.1007/s00247-005-1448-0. [DOI] [PubMed] [Google Scholar]
- 45.Fielding JW, Hensinger RN, Hawkins RJ. Os odontoideum. J Bone Joint Surg Am. 1980;62:376–383. [PubMed] [Google Scholar]
- 46.Kuhns LR, Loder RT, Farley FA, Hensinger RN. Nuchal cord changes in children with os odontoideum: evidence for associated trauma. J Pediatr Orthop. 1998;18:815–819. [PubMed] [Google Scholar]
- 47.Fielding JW. Normal and selected abnormal motion of the cervical spine from the second cervical vertebra to the seventh cervical vertebra based on cineroentgenography. J Bone Joint Surg Am. 1964;46:1779–1781. [PubMed] [Google Scholar]
- 48.Fielding JW, Hawkins RJ (1977) Atlanto-axial rotatory fixation. J Bone Joint Surg Am 59:37–44 [PubMed]
- 49.Ghanem I, Kreichaty G, Kharrat K. Atlantoaxial rotatory dislocation: pitfalls and controversies. Personal communication. Pediatric Orthopaedic Society of North America (POSNA) Florida: Lake Buena Vista; 1999. [Google Scholar]
- 50.Mathern GW, Batzdorf U. Grisel’s syndrome: cervical spine clinical, pathologic and neurologic manifestations. Clin Orthop. 1989;244:131–146. [PubMed] [Google Scholar]
- 51.Parke WW, Rothman RH, Brown MD. The pharyngovertebral veins: an anatomical rationale for Grisel’s syndrome. J Bone Joint Surg Am. 1984;66:568–574. [PubMed] [Google Scholar]
- 52.Phillips WA, Hensinger RN. The management of rotatory atlanto-axial subluxation in children. J Bone Joint Surg Am. 1989;71:664–668. [PubMed] [Google Scholar]
- 53.Subach BR, McLaughlin MR, Albright AL, Pollack IF. Current management of pediatric atlantoaxial rotatory subluxation. Spine. 1998;23:2174–2179. doi: 10.1097/00007632-199810150-00006. [DOI] [PubMed] [Google Scholar]
- 54.Ghanem IB, London C, Delalande O, Dubousset JF. Chiari I malformation associated with syringomyelia and scoliosis. Spine. 1997;22:1313–1317. doi: 10.1097/00007632-199706150-00006. [DOI] [PubMed] [Google Scholar]
- 55.Caird MS, Reddy S, Ganley TJ, Drummond DS. Cervical spine fracture-dislocation birth injury: prevention, recognition, and implications for the orthopaedic surgeon. J Pediatr Orthop. 2005;25:484–486. doi: 10.1097/01.bpo.0000158006.61294.ff. [DOI] [PubMed] [Google Scholar]
- 56.McGrory BJ, Klassen RA, Chao EYS, Staeheli JW, Weaver AL. Acute fractures and dislocations of the cervical spine in children and adolescents. J Bone Joint Surg Am. 1993;75:988–995. doi: 10.2106/00004623-199307000-00004. [DOI] [PubMed] [Google Scholar]
- 57.Hardy J, Pouliquen JC, Liverneaux P. Luxation traumatique C1-C2 chez l’enfant. Etude pronostique et indications thérapeutiques a propos de 13 cas. Rev Chir Orthop. 1990;76:17–22. [PubMed] [Google Scholar]
- 58.Filipe G, Berges O, Lebard JP, Carlioz H. Instabilités post-traumatiques entre l’atlas et l’axis chez l’enfant. A propos de 5 observations. Rev Chir Orthop. 1982;68:461–469. [PubMed] [Google Scholar]
- 59.Pennecot GF, Leonard P, Peyrot Des Gachons S, Hardy JR, Pouliquen JC. Traumatic ligamentous instability of the cervical spine in children. J Pediatr Orthop. 1984;4:339–345. doi: 10.1097/01241398-198405000-00010. [DOI] [PubMed] [Google Scholar]
- 60.Naidisch JB, Naidisch JP, Liebeskind AL, Hyman RA. The widened inter-spinal distance: a useful sign of anterior cervical dislocation in the supine frontal projection. Radiology. 1977;123:113–116. doi: 10.1148/123.1.113. [DOI] [PubMed] [Google Scholar]
- 61.Bulas DI, Fitz CR, Johnson DL. Traumatic atlanto-occipital dislocation in children. Radiology. 1993;188:155–158. doi: 10.1148/radiology.188.1.8511290. [DOI] [PubMed] [Google Scholar]
- 62.Kenter K, Worley G, Griffin T, Fitch RD. Pediatric traumatic atlanto-occipital dislocation: five cases and a review. J Pediatr Orthop. 2001;21:585–589. [PubMed] [Google Scholar]
- 63.Giguere JF, St-Vil D, Turmel A, Di Lorenzo M, Pothel C, Manseau S, Mercier C. Airbags and children: a spectrum of C-spine injuries. J Pediatr Surg. 1998;33:811–816. doi: 10.1016/s0022-3468(98)90648-0. [DOI] [PubMed] [Google Scholar]
- 64.Shamoun JM, Riddick L, Powell RW. Atlanto-occipital subluxation/dislocation: a “survivable” injury in children. Am Surg. 1999;65:317–320. [PubMed] [Google Scholar]
- 65.Przybylski GJ, Clyde BL, Fitz CR. Craniocervical junction subarachnoid hemorrhage associated with atlanto-occipital dislocation. Spine. 1996;21:1761–1768. doi: 10.1097/00007632-199608010-00009. [DOI] [PubMed] [Google Scholar]
- 66.Sponseller PD, Cass JR. Atlanto-occipital fusion for dislocation in children with neurologic preservation. Spine. 1997;22:344–347. doi: 10.1097/00007632-199702010-00020. [DOI] [PubMed] [Google Scholar]
- 67.Marlin AE, Williams GR, Lee JF. Jefferson fractures in children. J Neurosurg. 1983;58:277–279. doi: 10.3171/jns.1983.58.2.0277. [DOI] [PubMed] [Google Scholar]
- 68.Mikawa Y, Watanabe R, Yamano Y, Ishii K. Fracture through a synchondrosis of the anterior arch of the atlas. J Bone Joint Surg Br. 1987;69:483. doi: 10.1302/0301-620X.69B3.3584210. [DOI] [PubMed] [Google Scholar]
- 69.Razif M, Lim HH. Delayed decompression of chronic C1C2 subluxation in a pediatric patient with tetraplegia—is recovery possible? Med J Malaysia. 2001;56(Suppl C):76–79. [PubMed] [Google Scholar]
- 70.Wang J, Vokshoor A, Kim S, Elton S, Kosnik E, Bartkowski H. Pediatric atlantoaxial instability: management with screw fixation. Pediatr Neurosurg. 1999;30:70–78. doi: 10.1159/000028766. [DOI] [PubMed] [Google Scholar]
- 71.Sherk HH, Nicholson JT, Chung SMK. Fractures of the odontoid process in young children. J Bone Joint Surg Am. 1978;60:921–924. [PubMed] [Google Scholar]
- 72.Odent T, Langlais J, Glorion C, Kassis B, Bataille J, Pouliquen JC. Fractures of the odontoid process: a report of 15 cases in children younger than 6 years. J Pediatr Orthop. 1999;19:51–54. [PubMed] [Google Scholar]
- 73.Hardy J, Pouliquen JC, Pennecot GF. Les arthrodèses postérieures du rachis cervical supérieur chez l’enfant et l’adolescent a propos de 19 observations. Rev Chir Orthop. 1985;71:153–166. [PubMed] [Google Scholar]
- 74.McGrory BJ, Klassen RA, Chao EYS, Staeheli JW, Weaver AL. Acute fractures and dislocations of the cervical spine in children and adolescents. J Bone Joint Surg Am. 1993;75:988–995. doi: 10.2106/00004623-199307000-00004. [DOI] [PubMed] [Google Scholar]
- 75.Lawson JP, Ogden JA, Bucholz RW, Hughes SA. Physeal injuries of the cervical spine. J Pediatr Orthop. 1987;7:428–435. doi: 10.1097/01241398-198707000-00010. [DOI] [PubMed] [Google Scholar]
- 76.Lundy DW, Murray HH. Neurological deterioration after posterior wiring of the cervical spine. J Bone Joint Surg Br. 1997;79:948–951. doi: 10.1302/0301-620x.79b6.7923. [DOI] [PubMed] [Google Scholar]
- 77.Spitzer R, Rabinowitch JY, Wybor KC. A study of the abnormalities of the skull, teeth, and lenses in mongolism. Can Med Assoc J. 1961;84:567–572. [PMC free article] [PubMed] [Google Scholar]
- 78.Matsuda Y, Sano N, Watanabe S, Oki S, Shibata T. Atlanto-occipital hypermobility in subjects with Down’s syndrome. Spine. 1995;20:2283–2286. doi: 10.1097/00007632-199511000-00004. [DOI] [PubMed] [Google Scholar]
- 79.Selby KA, Newton RW, Gupta S, Hunt L. Clinical predictors and radiological reliability in atlantoaxial subluxation in Down’s syndrome. Arch Dis Child. 1991;66:876–878. doi: 10.1136/adc.66.7.876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Brockmeyer D. Down syndrome and craniovertebral instability. Topic review and treatment recommendations. Pediatr Neurosurg. 1999;31:71–77. doi: 10.1159/000028837. [DOI] [PubMed] [Google Scholar]
- 81.White KS, Ball WS, Prenger EC, Patterson BJ, Kirks DR. Evaluation of the craniocervical junction in Down syndrome: correlation of measurements obtained with radiography and MR imaging. Radiology. 1993;186:377–382. doi: 10.1148/radiology.186.2.8421738. [DOI] [PubMed] [Google Scholar]
- 82.Burke SW, French HG, Roberts JM, Johnston CE, Whitecloud TS, Edmunds JO., Jr Chronic atlanto-axial instability in Down syndrome. J Bone Joint Surg Am. 1985;67:1356–1360. [PubMed] [Google Scholar]
- 83.Committee on Sports Medicine and Fitness of the American Academy of Pediatrics Atlantoaxial instability in Down syndrome: subject review. Pediatrics. 1995;96:151–154. [PubMed] [Google Scholar]
- 84.Pueschel SM, Herndon JH, Gelch MM, Senft KE, Scola FH, Goldberg MJ. Symptomatic atlantoaxial subluxation in persons with Down syndrome. J Pediatr Orthop. 1984;4:682–688. doi: 10.1097/01241398-198411000-00005. [DOI] [PubMed] [Google Scholar]
- 85.Ghanem I, Chalouhi J, Kalouche I, Kharrat K, Dagher F. Atlantoaxial instability in Down syndrome. Personal communication. San Diego: Pediatric Orthopaedic Society of North America (POSNA); 2006. [Google Scholar]
- 86.Karol LA, Sheffield EG, Crawford K, Moody MK, Browne RH. Reproducibility in the measurement of atlanto-occipital instability in children with Down syndrome. Spine. 1996;21:2463–2467. doi: 10.1097/00007632-199611010-00010. [DOI] [PubMed] [Google Scholar]
- 87.Pueschel SM, Findley TW, Furia J, Gallagher PL, Scola FH, Pezzullo JC. Atlantoaxial instability in Down syndrome: roentgenographic, neurologic, and somatosensory evoked potential studies. J Pediatr. 1987;110:515–521. doi: 10.1016/s0022-3476(87)80541-3. [DOI] [PubMed] [Google Scholar]
- 88.Yong-Hing K, Kalamchi A, MacEwen GD. Cervical spine abnormalities in neurofibromatosis. J Bone Joint Surg Am. 1979;61:695–699. [PubMed] [Google Scholar]
- 89.Harada T, Ebara S, Anwar MM, Okawa A, Kajiura I, Hiroshima K, Ono K. The cervical spine in athetoid cerebral palsy. J Bone Joint Surg Br. 1996;78:613–619. [PubMed] [Google Scholar]
- 90.Fuji T, Yonenobu K, Fujiwara K, Yamashita K, Ebara S, Ono K, Okada K. Cervical radiculopathy or myelopathy secondary to athetoid cerebral palsy. J Bone Joint Surg Am. 1987;69:815–821. [PubMed] [Google Scholar]
- 91.Nishihara N, Tanabe G, Nakahara S, Imai T, Murakawa H. Surgical treatment of cervical spondylotic myelopathy complicating athetoid cerebral palsy. J Bone Joint Surg Br. 1984;66:504–508. doi: 10.1302/0301-620X.66B4.6746682. [DOI] [PubMed] [Google Scholar]
- 92.Reese ME, Msall ME, Owen S, Pictor SP, Paroski MW. Acquired cervical impairment in young adults with cerebral palsy. Dev Med Child Neurol. 1991;33:153–158. doi: 10.1111/j.1469-8749.1991.tb05094.x. [DOI] [PubMed] [Google Scholar]
- 93.Aronson DD, Kahn RH, Canady A, Bollinger RO, Towbin R. Instability of the cervical spine after decompression in patients who have Arnold-Chiari malformation. J Bone Joint Surg Am. 1991;73:898–906. [PubMed] [Google Scholar]
- 94.Cattell HS, Clark GL., Jr Cervical kyphosis and instability following multiple laminectomies in children. J Bone Joint Surg Am. 1967;49:713–720. [PubMed] [Google Scholar]
- 95.Francis WR, Jr, Noble DP. Treatment of cervical kyphosis in children. Spine. 1988;13:883–887. doi: 10.1097/00007632-198808000-00001. [DOI] [PubMed] [Google Scholar]
- 96.Ghanem I, Zeller R, Dubousset J. Tumeurs extra-osseuses du rachis chez l’enfant et l’adolescent. Complications rachidiennes. Rev Chir Orthop. 1996;82:313–320. [PubMed] [Google Scholar]
- 97.McLaughlin MR, Wahlig JB, Pollack IF. Incidence of postlaminectomy kyphosis after Chiari decompression. Spine. 1997;22:613–617. doi: 10.1097/00007632-199703150-00007. [DOI] [PubMed] [Google Scholar]
- 98.Sim FH, Svien HJ, Bickel WH, Janes JN. Swan-neck deformity following extensive cervical laminectomy. J Bone Joint Surg Am. 1974;56:564–580. [PubMed] [Google Scholar]
- 99.Yasuoka S, Peterson H, Laws ER, Jr, MacCarty CS. Pathogenesis and prophylaxis of postlaminectomy deformity of the spine after multiple level laminectomy: difference between children and adults. Neurosurgery. 1981;9:145–152. doi: 10.1227/00006123-198108000-00006. [DOI] [PubMed] [Google Scholar]
- 100.Meyer NJ, Flatley TJ, Dunn DD. Superiorly based laminoplasty in children: average 6.8-year follow-up of 21 patients. J Spinal Disord Tech. 2003;16:156–162. doi: 10.1097/00024720-200304000-00007. [DOI] [PubMed] [Google Scholar]
- 101.Raimondi AJ, Guiterrez FA, DiRocco C. Laminectomy and total reconstruction of posterior spinal arch for spinal canal surgery in childhood. J Neurosurgery. 1976;45:555–560. doi: 10.3171/jns.1976.45.5.0555. [DOI] [PubMed] [Google Scholar]
- 102.Hensinger RN, DeVito PD, Ragsdale CG. Changes in the cervical spine in juvenile rheumatoid arthritis. J Bone Joint Surg Am. 1986;68:189–198. [PubMed] [Google Scholar]
- 103.Fried JA, Athreya B, Gregg JR, Das M, Doughty R. The cervical spine in juvenile rheumatoid arthritis. Clin Orthop. 1983;179:102–106. [PubMed] [Google Scholar]
- 104.Dickerman RD, Colle KO, Bruno CA, Jr, Schneider SJ. Craniovertebral instability with spinal cord compression in a 17-month-old boy with Sly syndrome (mucopolysaccharidosis type VII): a surgical dilemma. Spine. 2004;29:92–94. doi: 10.1097/01.brs.0000112074.48566.fa. [DOI] [PubMed] [Google Scholar]
- 105.Dullenkopf A, Holzmann D, Feurer R, Gerber A, Weiss M. Tracheal intubation in children with Morquio syndrome using the angulated video-intubation laryngoscope. Can J Anaesth. 2002;49:198–202. doi: 10.1007/BF03020496. [DOI] [PubMed] [Google Scholar]
- 106.Morell RC, Colonna DM, Mathes DD, Wilson JA. Fluoroscopy-assisted intubation of a child with an unstable subluxation of C1/C2. J Neurosurg Anesthesiol. 1997;9:25–28. doi: 10.1097/00008506-199701000-00008. [DOI] [PubMed] [Google Scholar]
- 107.Pouliquen JC, Pennecot GF, Guyonvongh G. Charnière crânio-rachidienne et maladie de Morquio. Rev Chir Orthop. 1980;66(suppl 1):107–108. [PubMed] [Google Scholar]
- 108.Glorion C, Langlais J, Finidori G (2004) Monographie du GEOP. Sauramps
- 109.Banks JT, Wellons JC, III, Tubbs RS, Blount JP, Oakes WJ, Grabb PA. Cervical spine involvement in Larsen’s syndrome: a case illustration. Pediatrics. 2003;111:199–201. doi: 10.1542/peds.111.1.199. [DOI] [PubMed] [Google Scholar]
- 110.Bellon JM, Filipe G. Problemes rachidiens rencontres au cours du syndrome de Larsen. A propos de 3 cas. Rev Chir Orthop. 1987;73:57–62. [PubMed] [Google Scholar]
- 111.Lefort G, Mourad H, Deniscault G, Daoud S. Dislocation du rachis cervical supérieur dans le syndrome de Larsen. Chir Ped. 1983;24:211–212. [PubMed] [Google Scholar]
- 112.Tobias JD. Anesthetic implications of Larsen syndrome. J Clin Anesth. 1996;8:255–257. doi: 10.1016/0952-8180(96)00021-9. [DOI] [PubMed] [Google Scholar]


