Abstract
Background: Informed decision-making has been widely promoted in several medical settings, but little is known about the actual practice in orthopaedic surgery and there are no clear guidelines on how to improve the process in this setting. This study was designed to explore the quality of informed decision-making in orthopaedic practice and to identify excellent time-efficient examples with older patients.
Methods: We recruited orthopaedic surgeons, and patients sixty years of age or older, in a Midwestern metropolitan area for a descriptive study performed through the analysis of audiotaped physician-patient interviews. We used a valid and reliable measure to assess the elements of informed decision-making. These included discussions of the nature of the decision, the patient's role, alternatives, pros and cons, and uncertainties; assessment of the patient's understanding and his or her desire to receive input from others; and exploration of the patient's preferences and the impact on the patient's daily life. The audiotapes were scored with regard to whether there was a complete discussion of each informed-decision-making element (an IDM-18 score of 2) or a partial discussion of each element (an IDM-18 score of 1) as well as with a more pragmatic metric (the IDM-Min score), reflecting whether there was any discussion of the patient's role or preference and of the nature of the decision. The visit duration was studied in relation to the extent of the informed decision-making, and excellent time-efficient examples were sought.
Results: There were 141 informed-decision-making discussions about surgery, including knee and hip replacement as well as wrist/hand, shoulder, and arthroscopic surgery. Surgeons frequently discussed the nature of the decision (92% of the time), alternatives (62%), and risks and benefits (59%); they rarely discussed the patient's role (14%) or assessed the patient's understanding (12%). The IDM-18 scores of the 141 discussions averaged 5.9 (range, 0 to 15; 95% confidence interval, 5.4 to 6.5). Fifty-seven percent of the discussions met the IDM-Min criteria. The median duration of the visits was sixteen minutes; the extent of informed decision-making had only a modest relationship with the visit duration. Time-efficient strategies that were identified included use of scenarios to illustrate distinct choices, encouraging patient input, and addressing primary concerns rather than lengthy recitations of pros and cons.
Conclusions: In this study, which we believe is the first to focus on informed decision-making in orthopaedic surgical practice, we found opportunities for improvement but we also found that excellent informed decision-making is feasible and can be accomplished in a time-efficient manner.
Informed decision-making is the process by which physicians foster the informed participation of patients in clinical decision-making. The Institute of Medicine, in its landmark report “Crossing the Quality Chasm,” articulated the importance of the process to the provision of high-quality care1. It is particularly important for older adults to participate in informed decision-making since the decisions that they face are complex and often associated with a risk of death or major morbidity. Surgeons must routinely present these kinds of choices to patients, yet there is a striking paucity of literature about how informed decision-making is or should be conducted in the daily practice of surgery. Furthermore, there is little guidance for surgeons on “best practices” for accomplishing informed decision-making.
We previously developed an informed-decision-making model that can be used to assess the quality of informed-decision-making conversations. This model is related conceptually to the model of shared decision-making. Derived in the late 1970s by the President's Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research, shared decision-making describes a “process of mutual understanding” that accompanies clinical decision-making. Informed decision-making further emphasizes the importance of providing patients with adequate information with which they can effectively participate in shared decision-making2. The model, which is both ethically grounded and evidence-based, incorporates two key dimensions of informed decision-making: providing information and fostering patient involvement3,4. Specific elements of informed decision-making translate into the kinds of communication behaviors a surgeon can and should use to foster the patient's informed participation in a decision. Studies, particularly in the primary-care setting, indicate that effective communication in these dimensions can enhance patient satisfaction, improve adherence to treatment recommendations, and ultimately improve patient outcomes5-12.
One of the greatest challenges for surgeons is figuring out how to conduct effective informed-decision-making conversations within the constraints of a busy office practice. A concern often raised is that proposed models of excellent communication may not be feasible in the time-pressured work settings of practicing orthopaedic surgeons, although time pressure may be as much perceived as real13. We hypothesized that informed-decision-making discussions could be thorough without being unduly lengthy. To assess the feasibility of conducting time-efficient informed-decision-making discussions, we used our model to analyze discussions between practicing orthopaedic surgeons and their older patients who were considering a major procedure. Through this analysis, we identified examples of informed decision-making that were highly effective yet reasonably time-efficient to serve as a model for orthopaedic surgeons. Our overall goal was to use actually recorded encounters to locate instances of high-quality, time-efficient informed decision-making and offer them as exemplars of effective practice that others might emulate.
Materials and Methods
We used a subset of data from a larger office-based study of communication between orthopaedic surgeons and patients sixty years of age or older. In the main study, routine visits were audiotaped in the offices of eighty-nine orthopaedic surgeons practicing in a Midwestern metropolitan area. Potential subjects were identified by approaching sequential eligible patients in the offices of participating surgeons. Patients who were sixty years of age or older provided informed consent to participate in the study, which included completing a questionnaire and allowing their visit with the surgeon to be recorded. Participating surgeons also completed questionnaires, which included items regarding their prior communication skills training and their beliefs about informed decision-making. Specifically, surgeons were asked to rate, on a scale of 1 (none) to 5 (substantial), (1) “How much training in communication skills did you have in medical school or residency?” and (2) “How much training in communication skills have you had since entering practice?” We assessed surgeons' beliefs about informed decision-making by asking them to rate their agreement (on a scale ranging from strongly agree to strongly disagree) to three statements: (1) “Patients prefer that doctors offer them choice and ask their opinion,” (2) “Patients prefer to leave decisions about their medical care up to their doctor,” and (3) “Patients prefer to rely on their doctor's knowledge and not try to find out about their condition on their own.” These items were adapted from the National Opinion Research Center's General Social Surveys, a well-established measure of national demographics and attitudes that has been in existence since 197214.
Visits were recorded during the time that the surgeon was in the room with the patient; additional conversations outside the examination room or during follow-up visits were not captured. In this way, we sought a consistent approach so as to reduce the variability in coding that could result from attempting to capture other incidental communication outside of the examination room. For this study, we focused on only those visits that included discussions about surgical procedures.
Informed consent was obtained from all subjects (both patients and surgeons) prior to their participation. Institutional review board approval was obtained from all five participating hospitals in a large Midwestern metropolitan area (University of Chicago, Evanston Northwestern Healthcare, Rush-Presbyterian-St. Luke's Medical Center, Northwestern University, and University of Illinois at Chicago), the University of Toronto, Stanford University, and National Opinion Research Center (NORC). All study data were deidentified to ensure confidentiality.
Physician Sample
Physicians were recruited from a list of surgeon members in this large Midwestern metropolitan area provided by the American Academy of Orthopaedic Surgeons. Eighty-nine (79%) of 112 surgeons agreed to participate. Reasons for refusal included concerns that the research would require additional surgeon time or make demands on busy office staff. The average age of the surgeons was forty-nine years (range, thirty-two to seventy-two years); all but one were men. Eighty-four percent were white, 8% were Asian, 4.5% were black, and 2% were Hispanic. Forty percent were in practice in an academic center, and 56% were in community practice. The distribution of the extent of the surgeons' prior communication skills training is shown in Figure 1. When queried about their beliefs about decision-making, 89% of the surgeons strongly or moderately agreed that patients wanted to make their own choices, 19% strongly or moderately agreed that the patient wanted the doctor to decide, and 12% believed that the patient preferred to rely on the physician's knowledge in making the decision.
Fig. 1.
Histogram showing the distribution of the surgeons' self-reported extent of prior training in communication skills, rated from “none” to “substantial.”
Patient Sample
In total, 1007 patients were asked to participate, 886 (88%) agreed, and surgery was discussed with 133. Of these 133 patients, 74% were female with an average age of 71.2 years (range, sixty to ninety-six years). Seventy-six percent were white, 21% were black, and 4% were Hispanic. We used the highest level of education attained as a proxy for socioeconomic status: 15% had some high-school education or less, 34% had completed high-school graduation requirements, and 51% had at least some college-level education. The use of education as a measure of socioeconomic status has been proposed by others because of its close association with many other social characteristics and the simplicity of collecting such data15. Twenty-six percent of the patients were making their first visit to the surgeon.
Informed-Decision-Making Coding
The audiorecordings themselves, not transcriptions, were coded. Three coders were trained until their rates of inter-rater reliability were acceptable (a kappa statistic of >0.65). A 15% sample of the recordings was double-coded to ensure accuracy and reliability. The overall inter-rater reliability in the study sample was excellent, with kappa statistics ranging from 0.62 to 1.0.
Informed-decision-making coding measures the completeness of informed decision-making on the basis of the principle that surgeons should provide the patient with the relevant information necessary to make decisions and should foster the patient's active involvement in the process. The recordings were coded with use of a modification of the informed-decision-making scale, a previously developed and validated coding tool based on the informed-decision-making model3. The derivation of the nine elements of the coding has been described elsewhere; the informed-decision-making model represents a synthesis of recommendations from the literature regarding patient-physician communication, informed consent, and shared decision-making to determine what constitutes effective communication in the decision-making process1-3. The elements are: (1) discussion of the patient's role in decision-making (role), (2) exploration of the impact of the decision on the patient's daily life (context), (3) discussion of the nature of the clinical issue or decision (nature), (4) discussion of alternatives (alternatives), (5) discussion of pros and cons surrounding alternatives (pros and cons), (6) discussion of uncertainties with regard to alternatives (uncertainty), (7) the clinician's assessment of the patient's understanding (understanding), (8) the clinician's assessment of the patient's desire for input from trusted others (input), and (9) the clinician's solicitation and exploration of the patient's preference (preference). The informed-decision-making model was shown to be a valid and reliable measure in our previous study3. The elements are grouped into those that (1) provide information for patients and those that (2) foster patient involvement in decision-making (see Appendix).
Decisions were defined as a verbal commitment to a course of action. Discussion of a topic alone was not considered a decision unless the patient and physician expressed a commitment to a course of action. An example of such an expression of commitment would be a surgeon saying to a patient, “I would recommend that we give you a cortisone shot. Are you OK to go ahead with that?” and the patient responding, “That sounds fine to me.” For each decision, the coders identified the presence or absence of the nine elements of informed decision-making on a scale of 0 (absent), 1 (partially present), and 2 (fully present). An element was considered to be present even if it was only briefly mentioned, but it had to be mentioned by the physician. A brief mention of the element warrants a score of 1; in order to achieve a score of 2, the element must be discussed in depth and there must be some reciprocal interchange between the physician and patient. We created specific definitions of “in depth” for each of the informed-decision-making elements. Finally, the duration of the visit was calculated from the elapsed time of the recording of the patient-physician interaction.
Statistical Methods
We examined the frequency with which surgeons included each specific element of informed decision-making in their discussions about surgical procedures. We calculated two summary measures to characterize the overall degree of completeness of informed decision-making in each discussion. The derivation of these measures is described in our prior study3. The first summary measure involved simply summing all of the scores for the informed-decision-making elements present in the discussion of a given decision. The score for each element may be 0 (absent), 1 (partially present), or 2 (fully present). The result was an informed-decision-making score ranging from 0 to 18 (the IDM-18 score), with higher scores representing more extensive discussion of the clinical decision. The second summary measure, the IDM-Min, was designed to represent a “reasonable minimum” amount of informed decision-making. This measure was selected in order to acknowledge the concern that many clinicians express regarding the balance between the ideal of informed decision-making and the real or perceived time constraints and other barriers to extensive discussion of clinical decisions. The decision meets the criteria for IDM-Min when the physician has discussed the nature of the decision (element 3) and either the patient's role (element 1) or the patient's preference (element 9). The selection of these particular criteria for the IDM-Min reflected our judgment of the ethical minimum for allowing patients to be involved in decisions and ensuring that they are equipped with at least a modicum of information. Hence, IDM-Min sets a lower and more realistic metric for patient-physician discussions of important clinical decisions. IDM-Min is a dichotomous measure, scored as 0 or 1.
In an effort to identify the best practices of informed decision-making that were accomplished in relatively brief visits, we selected specific visits that had high IDM-18 scores and then extracted illustrative segments of best practices from office visits that were of average or below-average duration.
Results
Participants
We identified 141 decisions pertaining to surgery, including knee replacement (sixty-two decisions), hip replacement (eighteen), wrist/hand (eighteen), shoulder (twelve), ankle/foot (ten), arthroscopy (seven), neck/spine (two), and other (twelve).
Extent of Informed Decision-Making
The discussions about surgery most frequently included the nature of the decision, alternatives, and pros and cons. The proportion of discussions that included any mention of these topics was 92%, 62%, and 59%, respectively. The least frequent topics of these discussions were the patient's role in decision-making and the patient's understanding (14% and 12%). Table I shows the percentage of the discussions in which each specific element was talked about either partially or completely.
TABLE I.
Frequency of Each Element of the IDM-18 Score
| % of Cases with:
|
|||
|---|---|---|---|
| Element | Partial Discussion of Element (Score = 1) | Complete Discussion of Element (Score = 2) | Any Discussion of Element* |
| Discussion of patient's role | 14 | 0 | 14 |
| Exploration of context | 43 | 31 | 74 |
| Discussion of nature of decision | 43 | 49 | 92 |
| Description of alternatives | 51 | 11 | 62 |
| Discussion of pros and cons | 46 | 13 | 59 |
| Discussion of uncertainty | 33 | 14 | 47 |
| Assessment of patient's understanding | 12 | 0 | 12 |
| Assessment of patient's desire for others' input | 36 | 6 | 42 |
| Exploration of patient's preference | 48 | 11 | 59 |
The combined percentage of cases with partial or complete discussion of the element.
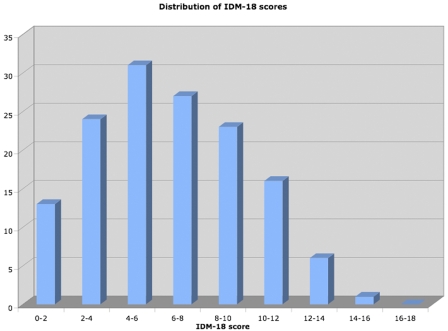
Overall, complete informed decision-making was not common; there were no cases in which the IDM-18 score identified a fully comprehensive discussion. The mean IDM-18 score was 5.9 (range, 0 to 15; 95% confidence interval, 5.4 to 6.5). The distribution of IDM-18 scores is shown in Figure 2.
Fig. 2.
Histogram showing the distribution of the total extent of the informed decision-making (the IDM-18 scores). The x-axis shows the ranges of IDM-18 scores (see text), and the y-axis shows the percentage of discussions in each range of IDM-18 scores.
Fifty-seven percent of the surgical decisions met the IDM-Min criteria. In general, decisions regarding knee and hip replacement tended to be based on more extensive discussions than were wrist, shoulder, or other surgical procedures. Table II shows the extent of the informed-decision-making discussions about hip, knee, wrist, and shoulder surgery as well as other orthopaedic procedures as measured by the mean and median IDM-18 scores and the percentage of cases meeting the IDM-Min criteria.
TABLE II.
Overall Extent of Informed Decision-Making About Common Surgical Procedures
| IDM-18 Score
|
% of Cases Meeting IDM-Min | ||
|---|---|---|---|
| Surgical Procedure | Mean (Range) | Median | |
| Knee replacement | 6.6 (1-15) | 6.7 | 57 |
| Hip replacement | 6.8 (1-13) | 7.0 | 67 |
| Shoulder, wrist, other | 5.4 (0-12) | 4.9 | 55 |
| All surgery | 5.9 (0-15) | 5.7 | 57 |
Efficiency of Informed Decision-Making
The median duration of the visits was 16.1 minutes (range, three to seventy-six minutes). More complete informed decision-making had only a modest impact on the duration of these office visits. Visits that met the IDM-Min criteria were longer (median duration, 17.8 minutes) than visits that did not (median duration, 15.4 minutes); however, this difference was not significant (p = 0.12). There was a modest trend for the discussion of more elements of informed decision-making increasing the duration of the visit (p = 0.0001), as shown in Table III.
TABLE III.
Relationship Between Extent of Informed Decision-Making and Duration of Visit*
| IDM-18 Score | Median Duration of Visit (min) |
|---|---|
| 0-3 | 10.6 |
| 4-5 | 17.2 |
| 6-7 | 13.9 |
| 8-9 | 19.9 |
| ≥10 | 21.3 |
The discussions with the lowest informed-decision-making scores (0 to 3) were shorter than those with the highest scores (≥10), a trend that was significant (p = 0.0001).
Best Practice of Informed Decision-Making: Illustrative Cases
In this section, we present two illustrative cases in which informed decision-making was of high quality, including one example of high-quality informed decision-making accomplished in a relatively short discussion. The purpose of these examples is to illustrate the differences between visits involving high and low-quality informed decision-making. Such examples can provide insight into specific strategies and techniques to achieve excellent informed decision-making in practice. To obtain these examples, we selected several cases for which the IDM-18 scores were high and transcribed them verbatim. We then selected phrases or passages that exemplified the principles and elements of informed decision-making. In each example, we indicated in brackets those elements of informed decision-making exemplified in the physician's comments.
Example 1: Knee Replacement Surgery
A surgeon discussed possible knee replacement surgery with a seventy-eight-year-old woman who had a history of coronary artery disease. Overall, this surgeon discussed eight of the nine elements of informed decision-making. While this visit lasted fourteen and one-half minutes, shorter than the average for our sample, almost nine minutes were devoted to discussing the possibility of total knee replacement. The patient had expressed concerns about the risks of surgery, but she was also bothered by substantial symptoms. In the discussion, the surgeon began by explicitly stating what was being decided (the nature of the decision), explored the context by inviting the patient's perspective on the impact of her symptoms on her daily life, and discussed the potential risks and benefits (pros and cons) of continued medical management or a possible knee replacement:
Surgeon: The choice to have knee replacement depends on how bad your pain is [nature]. Your knee is pretty bad and certainly could potentially benefit from that type of surgery, where it would go out straight again and you could walk without pain [pros and cons]. That would be sort of our end point of the surgery, you know, basically allowing you to walk better [context].
The surgeon then acknowledged the patient's worry about the risks and offered to talk with her primary care physician to help them decide on the level of risk associated with surgery (input of trusted others). He also checked on her level of understanding. Also, by offering two examples of what a patient might reasonably think in her situation, he allowed her to feel comfortable taking either position, thereby reinforcing the legitimacy of her role in the decision.
Surgeon: So part of this, you know, part of it depends on your own desires of whether or not you even want to consider surgery, OK? Because if you say, you know, “I don't even want to think about it,” then we don't need to do anything [alternative]. If you say, you know, “I'd really like to consider that though I know it's a risk,” I can talk with [your primary care doctor] doctor-to-doctor and see if he really thinks that you just can't even get close to the operating room or whether or not he just thinks, you know, that there's some moderate risk or something like that [input of trusted other]. Frequently, if we … you know, you're not too old to have a knee replacement if you're in reasonable health. But, uh, you understand? [understanding].
In the next passage, the surgeon clearly articulates the alternatives and appropriately refers to the patient's own experience of the symptom severity as a main factor that should influence her thinking (context).
Patient: But there's nothing else we can do besides replacing the knee …
Surgeon: No, that's right. When it's as bad as this one, you're kind of … you're really not … I mean the Vioxx is helping you some, you're starting to lose motion cause you can't get it straight and you're walking with it bent [context; alternative].
Patient: What about exercise?
Surgeon: Exercise is good [alternative]; it won't damage it. It's already kind of worn out.
Patient: A bicycle?
Surgeon: Sure, as much as you can. I mean exercising and maintaining the motion you have is good.
Later in the same discussion, the physician responded to the patient's query about another approach, involving more intense physical therapy. In so doing, the patient's understanding was enhanced.
Patient: So there's really not anything else I can do. Rehab's no good?
Surgeon: It's just not going to make a difference. We have to be realistic about what really is going to help you and what isn't [understanding].
Finally, the surgeon elicited the patient's concurrence with a plan of action: to talk with her primary care physician and, on the basis of that input and her own deliberations, decide how to proceed:
Surgeon: Right. Well I tell you what, why don't I at least call him and talk to him and see what he thinks with me asking him more specific questions. How's that sound? [preference].
Patient: Hmm-hmm.
Example 2: Lumbar Disc Surgery
In this second example, a surgeon conducted an equally substantive discussion, but in a shorter time. This visit, regarding possible lumbar disc surgery, lasted a total of fourteen and one-half minutes, with the discussion of surgery lasting only three and one-half minutes. Despite its brevity, this discussion also had a high IDM-18 score. In beginning this discussion, the surgeon first reviewed the nature of the decision and alternatives, discussing the pros and cons of each. He also used a spine model to promote understanding:
Surgeon: OK, number one—there's two techniques. Here, let's look at this model [understanding]. Your problem level is L5-S1. The disc is worn out. When the disc is worn out, the disc causes back pain, the bones settle down, and it actually can go down the leg. A pinched nerve [nature]. There's two techniques—one is to go in through the back, remove the osseous arch to free up nerves, then put a little metal cage from the back into here, and little rods and screws in the back with bone. That is the fusion part. The other alternative is to go in through a small incision below the belly button, going through the front, and in so doing you can put two little titanium metal cages in the disc and fill it with a bone growth protein [alternative]. The advantage of this is that you don't have all of the big muscle in the back that you have to deal with, which hurts more than anything, and you use the bone growth protein as opposed to taking bone from the hip [pros and cons].
After the patient raised a concern about the duration of postoperative recovery and its impact on her ability to return to work, the surgeon responded with specific comparisons regarding how rapidly she might return to work with either alternative:
Patient: My mother had similar surgery. She was laid up for a couple of weeks, and then she had a long recovery period [input of trusted others; context].
Surgeon: Which kind of procedure did she have?
Patient: It sounds like the first one.
Surgeon: From the back side; those types can leave you sore. Because you have to get to the spine, you have to go through layers of muscle [pros and cons].
Patient: So something like that would kill me as far as my work is concerned.
Surgeon: Yeah, you'd be out about four to six weeks. The rehab would be quicker with the other. Once you're comfortable, you can go back to work [context].
The surgeon then went on to address uncertainties about the likely outcome, offering some quantitative estimates of success. The next question clearly signaled to the patient her role in the decision-making, centered around her own judgment about the severity of her pain:
Surgeon: We generally tell people we can improve you 90%; no one's going to make you twenty-two, but you can be improved [uncertainty]. But as I prefaced all this conversation today, you're the one living with the pain, and, in your mind, which is the real problematic pain? [role].
Much like in the first example, this surgeon then introduced two versions of what the patient might plausibly say, thereby opening the door for the patient to express preferences:
Surgeon: Because if you said, “Look Dr. __ I can live with this back pain,” then we'd do that. But if you said, “Look it's 50-50, or a lot of this back stuff is limiting,” then we'd give more consideration to the surgery [preference].
Discussion
In the face of increasing calls to involve patients in clinical decision-making, there are few guidelines to shape the practice of informed decision-making, especially regarding surgery. Our results illustrate how surgeons approach this process, and we provided examples of ethically sound and clinically feasible best practices of informed decision-making regarding surgery. While many physicians rightfully worry about their ability to be simultaneously effective at fostering informed decision-making and efficient in time management, our findings show how surgeons can do so and how some can do it well. Surgeons who did well with fostering informed decision-making did not have substantially longer visits than their colleagues, an observation that is of critical importance given the real and perceived time pressures of clinical practice. The dialogue examples that we presented suggest ways in which a surgeon can effectively foster informed decision-making while recognizing the realities and constraints of everyday practice. Such examples may prove useful to those developing educational programs to enhance informed decision-making in orthopaedic surgical practice.
One such strategy for fostering time-efficient informed decision-making involved the surgeon stating two different and reasonable patient perspectives for making a decision. The surgeon used actual words that a patient might say about either choice to clearly frame the decision. This strategy may make the decision understandable and reinforce the patient's role in decision-making. Another communication strategy was eliciting and focusing on the patient's most dominant symptom or concern. This strategy enabled the surgeon to explore the context of the decision as well as to quickly identify the information that would be most salient to the patient. Given the volumes of information that the surgeon could discuss with a patient, this strategy allowed the surgeon to focus his or her energy on the concerns that were most germane to the patient. This communication approach is consistent with reports in the literature demonstrating the importance of attention to subtle patient clues about their worries and concerns16.
This study provides an assessment of the quality of the present practice of informed decision-making about orthopaedic procedures. Our findings reveal both the areas in which informed decision-making is acceptable and the specific areas that represent opportunities for improvement. Identifying these gaps may help to target improvements that will bring informed decision-making in orthopaedic surgical practice closer to the ideal.
Discussion of the nature of the decision, its alternatives, and its pros and cons tends to be performed at an acceptable level by surgeons. This may reflect the long-standing influence on medical practice of the legal model of informed consent, which traditionally encourages the provision of extensive information prior to the patient signing a consent form17. The main opportunities for enhancing informed decision-making regarding surgery lie with those elements that relate to fostering the patient's involvement in making the decision. For example, surgeons less frequently explored the patient's understanding of the surgical decision. This is of particular concern because of the importance of assessing understanding in order to ensure that the patient is truly an informed participant. Our study was not designed to assess a patient's actual understanding, but the low level of the physicians' assessments implies that they did not know how much their patients understood either. Exploration by the physician of patient understanding is a necessary, although not sufficient, condition for ascertainment of actual patient understanding. This finding underscores the importance of introducing specific strategies to help surgeons explore their patients' understanding and that training in such strategies is an important topic in medical education. Similarly, the patient's role in decision-making was infrequently discussed. It is possible that these elements of informed decision-making seem less important to busy surgeons than providing information. The ethical framework of informed decision-making, however, requires that physicians provide information as well as invite patients to participate in, or include patients in, decision-making, regardless of time pressure. Time pressure simply creates the need to find effective but time-efficient strategies to meet the ethical obligations of informed decision-making13.
There is growing interest in alternative strategies to provide the core information to patients in a complete yet time-efficient manner. One such strategy is the use of decision aids, tools ranging from pamphlets to interactive computer programs that enhance the patient's knowledge before he or she enters into the discussion with the physician18,19. Another strategy involves incorporating other members of the health-care team in patient education and preparation, such as a “hip school” to prepare patients for total hip replacement. Further use of these strategies may allow more of the limited time in the office visit to be devoted to promoting patient involvement, by directing the conversation to the patient's questions or concerns rather than reciting large amounts of information. In addition to freeing up time for such discussion, these strategies may help patients to better understand the core information critical to their informed participation.
There are also communication strategies, including the posing of questions at the start of the decision-making discussion, that allow the physician to assess the patient's baseline level of understanding of his or her condition and the proposed treatment and potentially avoid a long, redundant monologue by the physician. One such approach, promoted by the U.S. Preventive Services Task Force, is the “5-A Model”: Ask, Advise, Assess, Assist, Arrange. Each step in this model is intended to help the physician guide the patient through the decision-making process while providing sufficient information and eliciting the patient's preferences and concerns along the way20,21. Tools such as this warrant increased attention as a guide to informed decision-making in clinical practice. Finally, efforts to enhance the surgeon's overall effectiveness in interpersonal communication could substantially enhance communication around decision-making.
Our analysis has limitations. First, this is a cross-sectional study of communication and decision-making and as such may not capture the full extent of discussions held over several visits or the patient-physician communication patterns embedded in a longitudinal relationship. Also, many clinics have processes in place to foster informed decision-making, such as informational pamphlets and videotapes or allied health-care staff performing education and counseling functions. However, not all clinics have these adjunctive resources, nor do we fully know their impact on informed decision-making. These issues warrant future study. In addition, many patients in this sample had not seen the surgeon before or had had only one prior visit, hence making it less likely that a substantive relationship or extensive communication had previously occurred. Second, we studied orthopaedic surgeons rather than examining informed decision-making in a broader range of specialties. We think that this sample of orthopaedic surgeons from practices in both community and academic settings is likely to be similar in their informed-decision-making practices to other surgical specialties given the nature of decision-making. Third, the validity of the informed-decision-making model itself could be criticized by questioning whether it represents what patients want. We believe that the informed-decision-making model represents a balance between an unrealistic ideal and the suboptimal norm of clinical practice. Furthermore, there is a growing body of literature that supports the view that the majority of patients—although not all—prefer to be involved in clinical decisions affecting their health22-24. Finally, although we offer examples of time-efficient strategies for informed decision-making, we acknowledge that our study was not designed to measure the incremental effectiveness of informed decision-making in relationship to time. In fact, our analysis of time versus excellent informed decision-making did not demonstrate time-savings; the important observation is that, done well, the introduction of informed decision-making does not add a substantial amount of time.
While acknowledging these barriers, we believe that efforts to improve surgeon-patient communication and enhance decision-making through the application of the informed-decision-making model should continue. Given the complex and increasingly frequent decisions that orthopaedic surgeons and older patients face, such guidance may prove vital. Educational efforts to provide clinicians with knowledge about the informed-decision-making model could have a huge impact on the quality of decision-making. Enhancing informed decision-making in this way may reap the benefits of increasing patient satisfaction and improving quality of care. The translation of ethical theory into real-world practice that we have explored in this study can be a model for exploration of best practices in other realms of patient-physician interaction, in surgery and beyond.
Supplementary Material
Appendix
A table showing details of the informed-decision-making model is available with the electronic versions of this article, on our web site at jbjs.org (go to the article citation and click on “Supplementary Material”) and on our quarterly CD/DVD (call our subscription department, at 781-449-9780, to order the CD or DVD). 
Disclosure: In support of their research for or preparation of this work, one or more of the authors received, in any one year, outside funding or grants in excess of $10,000 from the National Institute on Aging, National Institutes of Health (R01 AG018781-05). Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, division, center, clinical practice, or other charitable or nonprofit organization with which the authors, or a member of their immediate families, are affiliated or associated.
A commentary is available with the electronic versions of this article, on our web site (www.jbjs.org) and on our quarterly CD-ROM/DVD (call our subscription department, at 781-449-9780, to order the CD-ROM or DVD).
Investigation performed at Stanford University School of Medicine, Stanford, California, and University of Toronto, Toronto, Ontario, Canada
References
- 1.Committee on Quality of Health Care in America; Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academy Press; 2001.
- 2.President's Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Making health care decisions: a report on the ethical and legal implications of informed consent in the patient-practitioner relationship. Washington, DC: US Government Printing Office; 1982.
- 3.Braddock CH 3rd, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed decision making in outpatient practice: time to get back to basics. JAMA. 1999;282:2313-20. [DOI] [PubMed] [Google Scholar]
- 4.Braddock CH 3rd, Fihn SD, Levinson W, Jonsen AR, Pearlman RA. How doctors and patients discuss routine clinical decisions. Informed decision making in the outpatient setting. J Gen Intern Med. 1997;12:339-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adams RJ, Appleton S, Wilson DH, Ruffin RE. Participatory decision making, asthma action plans, and use of asthma medication: a population survey. J Asthma. 2005;42:673-8. [DOI] [PubMed] [Google Scholar]
- 6.Bieber C, Müller KG, Blumenstiel K, Schneider A, Richter A, Wilke S, Hartmann M, Eich W. Long-term effects of a shared decision-making intervention on physician-patient interaction and outcome in fibromyalgia. A qualitative and quantitative 1 year follow-up of a randomized controlled trial. Patient Educ Couns. 2006;63:357-66. [DOI] [PubMed] [Google Scholar]
- 7.Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17:243-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jahng KH, Martin LR, Golin CE, DiMatteo MR. Preferences for medical collaboration: patient-physician congruence and patient outcomes. Patient Educ Couns. 2005;57:308-14. [DOI] [PubMed] [Google Scholar]
- 9.Mandelblatt J, Kreling B, Figeuriedo M, Feng S. What is the impact of shared decision making on treatment and outcomes for older women with breast cancer? J Clin Oncol. 2006;24:4908-13. [DOI] [PubMed] [Google Scholar]
- 10.Mead N, Bower P, Hann M. The impact of general practitioners' patient-centredness on patients' post-consultation satisfaction and enablement. Soc Sci Med. 2002;55:283-99. [DOI] [PubMed] [Google Scholar]
- 11.Parhiscar A, Rosenfeld RM. Can patient satisfaction with decisions predict compliance with surgery? Otolaryngol Head Neck Surg. 2002;126:365-70. [DOI] [PubMed] [Google Scholar]
- 12.Rosenberger PH, Jokl P, Cameron A, Ickovics JR. Shared decision making, preoperative expectations, and postoperative reality: differences in physician and patient predictions and ratings of knee surgery outcomes. Arthroscopy. 2005;21:562-9. [DOI] [PubMed] [Google Scholar]
- 13.Braddock CH 3rd, Snyder L. The doctor will see you shortly. The ethical significance of time for the patient-physician relationship. J Gen Intern Med. 2005;20:1057-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith TW, Davis JA, Marsden PV. General social surveys, 1972-2006: cumulative codebook. Chicago: National Opinion Research Center; 2007.
- 15.Liberatos P, Link BG, Kelsey JL. The measurement of social class in epidemiology. Epidemiol Rev. 1988;10:87-121. [DOI] [PubMed] [Google Scholar]
- 16.Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and physician responses in primary care and surgical settings. JAMA. 2000;284:1021-7. [DOI] [PubMed] [Google Scholar]
- 17.Lidz CW, Appelbaum PS, Meisel A. Two models of implementing informed consent. Arch Intern Med. 1988;148:1385-9. [PubMed] [Google Scholar]
- 18.Barry MJ. Health decision aids to facilitate shared decision making in office practice. Ann Intern Med. 2002;136:127-35. [DOI] [PubMed] [Google Scholar]
- 19.O'Connor AM, Stacey D, Entwistle V, Llewellyn-Thomas H, Rovner D, Holmes-Rovner M, Tait V, Tetroe J, Fiset V, Barry M, Jones J. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2003;2:CD001431. [DOI] [PubMed] [Google Scholar]
- 20.Sheridan SL, Harris RP, Woolf SH; Shared Decision-Making Workgroup of the U.S. Preventive Services Task Force. Shared decision making about screening and chemoprevention. A suggested approach from the U.S. Preventive Services Task Force. Am J Prev Med. 2004;26:56-66. [DOI] [PubMed] [Google Scholar]
- 21.Whitlock EP, Orleans CT, Pender N, Allan J. Evaluating primary care behavioral counseling interventions: an evidence-based approach. Am J Prev Med. 2002;22:267-84. [DOI] [PubMed] [Google Scholar]
- 22.Deber RB, Kraetschmer N, Irvine J. What role do patients wish to play in treatment decision making? Arch Intern Med. 1996;156:1414-20. [PubMed] [Google Scholar]
- 23.Frosch DL, Kaplan RM. Shared decision making in clinical medicine: past research and future directions. Am J Prev Med. 1999;17:285-94. [DOI] [PubMed] [Google Scholar]
- 24.Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med. 2005;20:531-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.