Abstract
The inability to propagate obligate intracellular pathogens under axenic (host cell-free) culture conditions imposes severe experimental constraints that have negatively impacted progress in understanding pathogen virulence and disease mechanisms. Coxiella burnetii, the causative agent of human Q (Query) fever, is an obligate intracellular bacterial pathogen that replicates exclusively in an acidified, lysosome-like vacuole. To define conditions that support C. burnetii growth, we systematically evaluated the organism's metabolic requirements using expression microarrays, genomic reconstruction, and metabolite typing. This led to development of a complex nutrient medium that supported substantial growth (approximately 3 log10) of C. burnetii in a 2.5% oxygen environment. Importantly, axenically grown C. burnetii were highly infectious for Vero cells and exhibited developmental forms characteristic of in vivo grown organisms. Axenic cultivation of C. burnetii will facilitate studies of the organism's pathogenesis and genetics and aid development of Q fever preventatives such as an effective subunit vaccine. Furthermore, the systematic approach used here may be broadly applicable to development of axenic media that support growth of other medically important obligate intracellular pathogens.
Keywords: axenic growth, metabolism, microaerophile, obligate intracellular pathogen
Coxiella burnetii is the causative agent of human Q fever, a disease that typically manifests as a debilitating influenzae-like illness (1). Shortly after the discovery of Q fever as a clinical entity in 1937 (2) attempts were made to culture C. burnetii under axenic (host cell-free) conditions (3). However, despite over 6 decades of ensuing research, growth of the organism still remains limited to colonization of a viable eukaryotic host cell.
Early studies showed minimal C. burnetii metabolic capacity in buffers adjusted to neutral pH (4). The organism's intracellular growth compartment was subsequently described as “phagolysosomal-like” (5) which led to the discovery by Hackstadt and Williams (6) that significant metabolic activity by C. burnetii only occurs in buffers that mimic the moderately acidic (approximately pH 4–5) conditions of this vacuole. Building on this work, we recently developed a nutrient medium termed Complex Coxiella Medium (CCM) that supports axenic metabolic activity by C. burnetii for at least 24 h (7). Critical components of CCM include 3 complex nutrient sources (neopeptone, FBS, and RPMI cell culture medium), a high concentration of chloride (140 mM), and citrate buffer (pH approximately 4.75) (7).
The obligate intracellular nature of C. burnetii imposes considerable experimental limitations that impede progress in understanding the organism's physiology and virulence. Indeed, systems to genetically manipulate Coxiella are lacking and lipopolysaccharide is the only defined virulence factor of the organism (8). While obvious growth of C. burnetii is not observed in CCM (unpublished data), the pathogen's sustained axenic metabolic activity in this medium suggested a modified formulation might support replication. To this end, we evaluated the organism's transcriptome during metabolism in CCM and identified a potential nutritional deficiency of this medium. Moreover, using genomic reconstruction and metabolite typing, we defined C. burnetii as a microaerophile. These data allowed development of a medium that supports axenic growth of infectious C. burnetii under microaerobic conditions.
Results
C. burnetii Exhibits Reduced Ribosomal Gene Expression in CCM.
As an initial step to identify nutritional deficiencies of CCM that could preclude C. burnetii cell division, a comparison of genome wide transcript profiles between organisms replicating in Vero cells and incubated in CCM for 24 h was conducted. This analysis showed substantially reduced expression of ribosomal genes during incubation in CCM (supporting information (SI) Table S1), suggesting that protein synthesis was insufficient to support C. burnetii replication in this axenic medium. Supplementation of CCM with pyruvate, succinate, or glutamate, efficiently oxidized energy sources of C. burnetii (9), did not improve C. burnetii de novo protein synthesis in CCM (7), suggesting energy starvation was not the reason for reduced ribosomal gene expression.
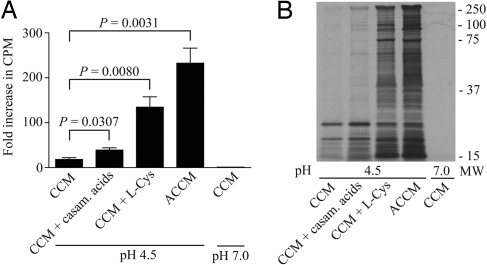
Supplementation of CCM with Protein Precursors Improves C. burnetii Catabolic Activity.
Amino acid deficiencies in CCM could also explain reduced ribosomal gene expression. C. burnetii has multiple amino acid auxotrophies that appear compensated for by amino acid and peptide transporters (10). Moreover, intracellular bacteria frequently use amino acids as carbon sources (11), with an exceptionally high concentration of L-cysteine required for axenic growth by some (12). To evaluate whether supplementation of CCM with amino acids and peptides improves C. burnetii metabolic activity, casamino acids (a mixture of amino acids and peptides) and/or L-cysteine were added to the medium (Table 1). Following 24 h preincubations in media, C. burnetii was subjected to a 3 h [35S]Cys/Met pulse and the fold increase in radiolabel incorporation over the negative control (i.e., organisms labeled in labeling buffer at pH 7) used to assess the catabolic capacity (7) of the organism. CCM supplemented with casamino acids or L-cysteine supported statistically significant increases in C. burnetii radiolabel incorporation of (39.1 ± 5.1)-fold and (134.5 ± 23.4)-fold, respectively (Fig. 1A). The effect of supplementing CCM with both casamino acids and L-cysteine was additive, resulting in a (232.7 ± 33.5)-fold increase in incorporation (Fig. 1A). Overall, this medium termed Acidified Citrate Cysteine Medium (ACCM) (Table 1) supported an approximately 13-fold increase in protein synthesis compared to CCM. SDS/PAGE and autoradiography confirmed that radiolabel was incorporated into C. burnetii de novo synthesized protein (Fig. 1B).
Table 1.
Components of Acidified Citrate Cysteine Medium (ACCM)
| Ions | Final concentration a, b | Nutrients | Final concentration |
|---|---|---|---|
| Na+ | 190 | Neopeptone | 0.1 mg/ml |
| SO4− | 0.06 | FBS | 1% |
| Fe2+ | 0.01 | RPMI 1640 | 1/8X |
| Cl− | 140 | Citrate | 29 |
| Ca+ | 0.15 | Casamino acidsc | 2.5 mg/ml |
| Mg2+ | 1.0 | L-cysteinec | 1.5 |
| K+ | 4.3 | ||
| PO4− | 4.5 | ||
| NO3− | 0.1 | ||
| HCO3− | 3.0 |
aConcentrations are in mM unless otherwise specified.
bExcluding contribution from neopeptone and FBS.
cAbsent in CCM.
Fig. 1.
Supplemented CCM supports enhanced C. burnetii metabolic activity. Effects of casamino acids and L-cysteine on C. burnetii catabolic capacity were determined by incubating organisms in CCM or CCM supplemented with 2.5 mg/ml casamino acids, 1.5 mM L-cysteine or both (ACCM). Bacteria were preincubated in the respective media for 24 h, then labeled with [35S]Cys/Met in labeling buffer (pH 4.5) for 3 h. (A) De novo protein synthesis by C. burnetii was measured by quantification of radiolabel incorporation by scintillation counting. Results are expressed as fold increase in incorporation when compared with incorporation of bacteria preincubated in CCM, then labeled in labeling buffer (pH 7.0) (negative control). Casamino acids and L-cysteine significantly improved C. burnetii metabolic activity. (B) SDS/PAGE and autoradiography confirmed incorporation of radiolabel into bacterial proteins. Values are mean ± SEM (n = 3). The level of radiolabel incorporation in CCM (pH 7.0) is normalized to 1.
C. burnetii Substrate Oxidation Increases Under Microaerobic Conditions.
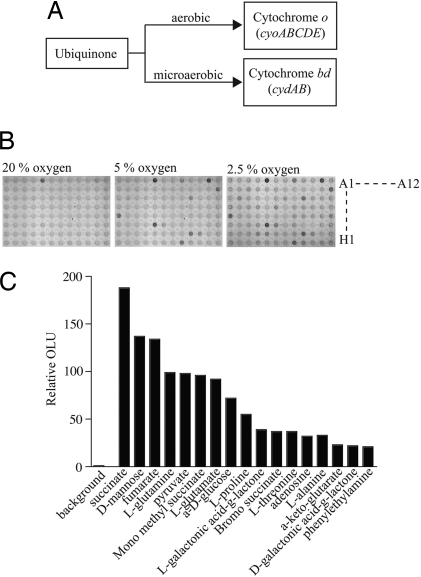
Terminal oxidases containing either cytochrome o or cytochrome bd (associated with aerobic and microaerobic respiration, respectively) are encoded by the C. burnetii genome (Fig. 2A). This observation suggested that C. burnetii responds to alterations in oxygen tension during intracellular growth. Therefore, we assessed the effect of oxygen tension on C. burnetii metabolism of a wide variety of metabolites, including amino acids and carbohydrates, using Phenotype Microarrays (PM). C. burnetii oxidation of 95 substrates in PM-1 arrays was tested under oxygen tensions of 20%, 5%, and 2.5%. Incubation in 20% oxygen resulted in efficient oxidation of only succinate (Fig. 2B). However, incubations in 5% or 2.5% oxygen showed oxidation of 10 and 17 substrates, respectively (Fig. 2B). Intermediates of major metabolic pathways including the tricarboxylic acid cycle and glycolysis were most efficiently oxidized (Fig. 2C). Several substrates efficiently oxidized by C. burnetii in PMs have also been identified as substrates for the organism in independent studies (e.g., succinate, glutamate, and proline) (9, 13).
Fig. 2.
The number of substrates oxidized by C. burnetii increases with decreasing oxygen availability. The ability of C. burnetii to oxidize substrates in different oxygen environments was assessed using PM. (A) C. burnetii genes encoding terminal oxidases associated with aerobic (cytochrome o) and microaerobic (cytochrome bd) metabolism suggested C. burnetii can respire under microaerophilic conditions. (B) Purified C. burnetii was added to PM-1 plates and incubated for 24 h in 20%, 5%, and 2.5% oxygen. The number of metabolites oxidized increased with decreasing oxygen tension, consistent with microaerophilic metabolism. Representative PM plate images are shown. (C) Seventeen substrates were efficiently oxidized by C. burnetii in 2.5% oxygen. Signal intensities were measured using an OmniLog detection system and expressed as relative OmniLog units (OLU). Quantitative analysis is representative of at least 3 independent experiments. Substrate key (rows A-H, columns 1–12): A1, no substrate control; A5, succinate; A8, L-proline; A11, D-mannose; B12, L-glutamate; C2, D-galactonic acid-γ-lactone; C9, α-D-glucose; D6, α-ketoglutarate; E1, L-glutamine; E12, adenosine; F5, fumarate; F6, bromo succinate; G4, L-threonine; G5, L-alanine; G9, mono methyl succinate; H8, pyruvate; H9, L-galactonic acid-γ-lactone; H11, phenylethylamine.
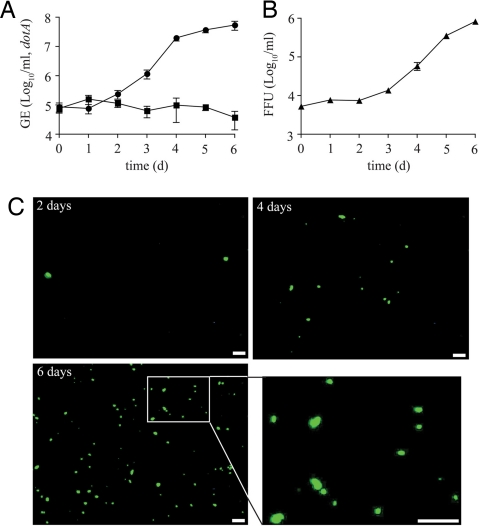
ACCM Supports C. burnetii Replication in a Microaerobic Environment.
The characterization of C. burnetii as a potential microaerophile suggested that incubation in ACCM in an optimal oxygen environment might support growth. Therefore, ACCM was inoculated with C. burnetii and the cultures incubated in a 20% or 2.5% oxygen environment. Cultures were monitored for C. burnetii replication by measuring bacterial genome equivalents (GE) by quantitative Taqman PCR (QPCR) every 24 h over 6 days. Incubation of C. burnetii in ACCM in 20% oxygen did not result in an increase in C. burnetii GE (Fig. 3A). However, substantial replication of C. burnetii occurred in 2.5% oxygen (8.71 × 104 to 5.49 × 107 GE/ml) (Fig. 3A). C. burnetii replication in ACCM in 1% or 5% oxygen was similar to that observed in 2.5% while no replication was observed in 10% oxygen (data not shown). The growth cycle of organisms incubated in ACCM in 2.5% oxygen consisted of a lag phase of approximately 1 day, followed by 3 days of exponential growth and the onset of stationary phase thereafter. The generation time of C. burnetii during exponential growth in ACCM was 9.1 h which is 1–2 h less than the generation time in Vero cells (14). C. burnetii also formed colonies (approximately 0.05–0.1 mm in diameter) after a 14 day incubation in an ACCM-based solid agarose medium (Fig. S1).
Fig. 3.
ACCM supports axenic cell division of infectious C. burnetii under microaerobic conditions. (A) C. burnetii GE were assessed by QPCR daily for 6 days. Incubation in 20% (■) oxygen did not support C. burnetii replication while incubation in 2.5% (•) oxygen resulted in considerable C. burnetii replication. (B) Increases in C. burnetii GE during incubation in ACCM correlated with production of infectious bacteria as determined by a quantitative FFU assay. Values are mean ± SEM (n = 3). (C) Representative staining of FFUs contained in equal aliquots of ACCM harvested at 2, 4, and 6 days post inoculation. A magnified view of the inset in the 6 days post inoculation panel in also shown. (Scale bars, 30 μm.)
To confirm that the increase in C. burnetii genome equivalents corresponded to an increase in C. burnetii infective units, organisms incubated in ACCM in 2.5% oxygen were assayed for Vero cell infectivity using a fluorescent infectious focus-forming unit (FFU) assay that employs a Coxiella-specific antibody. ACCM culture aliquots taken every 24 h for 6 days postinoculation showed an increase in FFUs of 2.19 logs (Fig. 3 B-C) with the kinetics of FFU development directly corresponding to increases in GE (Fig. 3A). Coxiella containing vacuoles showed typical staining for the lysosomal marker CD63 (data not shown). Ten to fifteen genomes were required for development of each vacuole, equivalent to published GE/FFU ratios (14). Collectively, these data show that ACCM supports robust cell division of infectious C. burnetii that are antigenically similar to cell culture-cultivated organisms.
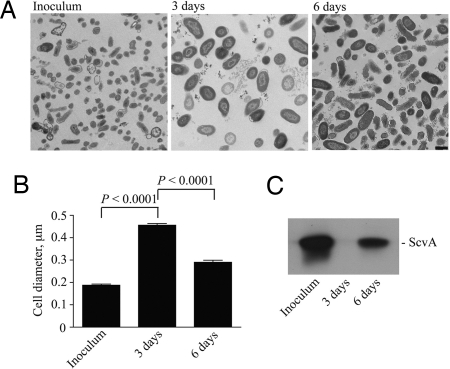
C. burnetii Developmental Transitions Occur in ACCM.
During infection of eucaryotic host cells, C. burnetii undergoes a biphasic developmental cycle characterized by transition of metabolically dormant, nonreplicative small cell variants (SCV) to metabolically active, replicative large cell variants (LCV) (14). To determine whether this developmental program occurs during replication in ACCM, medium was inoculated with purified SCVs and morphological differentiation assessed by transmission electron microscopy (TEM). Ultrastructural features of the inoculum were characteristic of the SCV, most notably small cell size (< 0.2 μm) and electron-dense chromatin (Fig. 4A-B) (14). Organisms incubated in ACCM for 3 days and in exponential phase displayed ultrastructural characteristics of the LCV including increased cell size (> 0.2 μm) and dispersed chromatin (Fig. 4 A-B) (14). Organisms incubated in ACCM for 6 days and in early stationary phase were a mixture of SCVs and LCVs (Fig. 4 A-B). ACCM cultures initiated with purified SCVs also showed approximately 3 logs of growth after 6 days of incubation (Fig. S2). Developmental transitions were confirmed by immunoblotting for ScvA, a DNA-binding protein specific to the SCV (14, 15). ScvA was detected only in the SCV inoculum and the LCV/SCV mixture present at early stationary phase (Fig. 4C). Thus, C. burnetii undergoes a developmental program in ACCM that is similar to in vivo propagated organisms.
Fig. 4.
C. burnetii SCV to LCV development occurs in ACCM. To determine whether C. burnetii transitions between nonreplicative SCV and replicative LCV developmental forms during incubation in ACCM, medium was inoculated with purified SCVs and TEM used to assess developmental transitions. (A and B) TEM showed the inoculum had ultrastructural characteristics of the SCV including small cell size (average diameter: 0.188 ± 0.0044 μm) and condensed chromatin. Organisms incubated in ACCM for 3 days exhibited ultrastructural characteristics of the LCV including increased cell size (average diameter: 0.456 ± 0.0078 μm) and dispersed chromatin. Following 6 days of incubation, a mixed population of SCVs and LCVs was observed, resulting in an overall reduction in cell size (average diameter: 0.290 ± 0.0087 μm). Values are mean ± SEM (n = 60 cells). (Scale bar, 0.5 μm.) (C) Immunoblot demonstrating the presence of ScvA (3.5 kDa), a SCV-specific DNA-binding protein, only in the SCV inoculum and the LCV/SCV mixture present in stationary phase.
Discussion
The systematic approach described herein allowed identification of nutritional and biophysical conditions that support C. burnetii host cell-free growth. Based on a 2.5–3 log increase in C. burnetii GE after 6 days of culture in ACCM in 2.5% oxygen, we estimate that 100 ml of ACCM can yield the same number of organisms as 7 × 108 infected Vero cells. Growth of C. burnetii in ACCM was also established with an inoculum as low as 100 GE/ml (data not shown), suggesting ACCM can be used to isolate C. burnetii from the small number of organisms typically contained in clinical samples. Axenic culture of C. burnetii in ACCM will improve our ability to define factors required for intracellular growth and pathogenesis. Moreover, growth of C. burnetii on solid ACCM medium will facilitate clonal isolation and development of genetic tools for this organism.
The substantial increase in C. burnetii metabolic activity in ACCM compared to CCM is largely an effect of L-cysteine. An elevated level of L-cysteine is also required for in vitro culture of Legionella pneumophila (16, 17) where the amino acid may serve as an antioxidant in scavenging hydrogen peroxide (18). While L-cysteine is bio-accessible to L. pneumophila, the oxidized form L-cystine is not, making it necessary to supplement nutrient media with L-cysteine in great excess of what is consumed by the organism (12). ACCM containing the alternative antioxidant L-glutathione instead of L-cysteine did not support C. burnetii growth (data not shown), suggesting that C. burnetii's requirement for L-cysteine in ACCM is nutritional. In addition to serving as a precursor in protein synthesis, L-cysteine may also be a source of sulfur.
C. burnetii replication in ACCM is optimal in a 2.5% oxygen environment and the presence of genes encoding cytochrome bd (i.e., cydAB) with high affinity for oxygen provides a biochemical/physiological explanation for the observed growth phenotype. Interestingly, the intracellular bacteria Mycobacterium tuberculosis (19), Chlamydia trachomatis (20), and Rickettsia rickettsii all encode cydAB, suggesting adaptation to microaerobic metabolism in intracellular bacteria may be underappreciated. Indeed, transcriptional analysis of M. tuberculosis during infection of macrophages indicates the organism adapts to a reduced oxygen environment (21), and improved growth of Chlamydia pneumoniae is observed under low oxygen conditions (22). Like M. tuberculosis, C. burnetii can occupy tissue granulomas (23), a defined low oxygen environment (24). Mammalian cell intracellular oxygen tension can be significantly lower than the extracellular oxygen tension (25). Moreover, the membrane of the C. burnetii replicative vacuole is enriched in cholesterol (26), and cholesterol-rich membranes are known to impede oxygen diffusion (27). Collectively, these observations suggest the vacuolar compartment of C. burnetii is a low oxygen environment. In addition to potentially serving as a terminal oxidase in low oxygen conditions, CydAB may also protect C. burnetii against oxidative agents of the phagolysosome. In support of this hypothesis, cydB mutants of Brucella abortus and Escherichia coli are hypersensitive to hydrogen peroxide (28, 29).
The debilitating nature of acute Q fever, along with C. burnetii's environmental stability and aerosol route of transmission, have raised concerns over potential illegitimate use of this microorganism (30). In this regard, axenic cultivation of C. burnetii will aid molecular characterization of the organism to enable development of protective measures against Q fever, including improved diagnostic tools and efficacious vaccines. Moreover, the strategy used here to establish culture conditions for C. burnetii may be broadly applicable to identifying media formulations and biophysical conditions that support growth of other currently obligate intracellular bacterial pathogens of humans within the genera Anaplasma, Ehrlichia, Treponema, Chlamydia and Rickettsia.
Materials and Methods
Cultivation and Purification of C. burnetii from Vero Cells.
C. burnetii Nine Mile phase II (RSA439, clone 4) was propagated in African green monkey kidney (Vero) fibroblasts (CCL-81; American Type Culture Collection) grown in RPMI medium (Invitrogen Corp.) supplemented with 2% FBS. At 7 days post infection, host cells were disrupted by sonication and C. burnetii purified by differential centrifugation as described (31, 32). At this time point postinfection, infected Vero cells contain roughly equal numbers of SCV and LCV morphological forms (14). C. burnetii SCVs were generated by prolonged culture in Vero cells as previously reported (14) and purified as described above. Purified bacteria were resuspended in K-36 buffer (0.05 M K2HPO4 and KH2PO4, 0.1 M KCl, 0.15 M NaCl, pH 7.0) (33) and stored at −80 °C until further use. With the exception of experiments examining C. burnetii biphasic development (Figs. 4 and S2), all experiments used C. burnetii purified from Vero cells at 7 days post infection.
Transcription Microarray Analysis.
For analysis of C. burnetii transcript profiles during intracellular growth, Vero cells at 90–95% confluence in T-75 cell culture flasks were infected with C. burnetii at a multiplicity of infection of 100 for 2 h at room temperature. The inoculum was removed, cell cultures washed to remove noninternalized bacteria, then 10 ml RPMI supplemented with 2% FBS added to the culture flasks. At 5 days postinfection, host cell cultures were washed with 10 ml of Hank's buffered salt solution, then lysed with 3 ml of TRIzol reagent (Invitrogen). For analysis of C. burnetii transcript profiles in CCM, 2.5 × 109 GE of C. burnetii were incubated in triplicate in 0.5 ml CCM in 24-well plates for 24 h. Bacteria were transferred to a 1.5 ml Microfuge tube, pelleted by centrifugation, then TRIzol reagent (1.0 ml) added to each tube. Total RNA in TRIzol samples was purified and processed as previously described (34).
A MicrobEnrich kit (Applied Biosystems) was used to increase the relative level of C. burnetii RNA derived from Vero cell-propagated organisms. Enriched RNA (approximately 1 μg) was amplified using a MessageAmp II Bacteria kit (Applied Biosystem). Briefly, double stranded (ds) cDNA was synthesized, product was purified using a QiaQuick 96-well system, and biotin-labeled cRNA was in vitro transcribed using ds cDNA as a template. RNA samples from C. burnetii cultured in CCM were treated identically to facilitate comparisons with RNA samples derived from Vero cell-propagated C. burnetii.
All cRNA originating from Vero cell-propagated C. burnetii and 3 μg cRNA from CCM-cultivated organisms were hybridized to a custom Affymetrix GeneChip designed as previously described (35). Microarray data were analyzed using Partek Genomics Suite software (Partek Inc.) essentially as described (36).
Radiolabeling with [35S] Cysteine/Methionine.
Radiolabeling of C. burnetii proteins was conducted using 2.5 × 109 GE of freshly thawed organisms. Following preincubations in 6-well plates containing 2.0 ml medium per well, bacteria were pelleted (20,000 × g for 5 min) and washed in 200 μl citrate salts buffer (7) supplemented with 1.0 mM glutamate (labeling buffer) to remove excess nutrients. Bacteria were then resuspended in 500 μl labeling buffer containing 25–50 μCi [35S]Cys/Met protein labeling mix (Perkin-Elmer) and incubated for 3 h in a screw-cap tube to allow incorporation of the radionuclide. Following radiolabeling of bacterial proteins, bacteria were pelleted for 5 min at 20,000 × g and washed in 100 μl of PBS (PBS; 10 mM Na2HPO4, 10 mM NaH2PO4, 150 mM NaCl, pH 7.8) to remove unincorporated [35S]Cys/Met. Bacterial pellets were lysed in equal volumes of a SDS polyacrylamide gel electrophoresis (SDS/PAGE) sample buffer and boiled for 10 min. Equal volumes of each sample were analyzed by scintillation counting to determine cpm. Twelve percent SDS/PAGE followed by autoradiography using CL-Xposure (Pierce) film was used to visualize radiolabeled proteins (3 h exposure). Precision Plus Protein Dual Color Standards (Bio-Rad) were used as molecular mass markers.
Phenotype Microarrays.
C. burnetii oxidation of substrates under different oxygen concentrations was tested using Phenotype Microarrays (PM-1) (Biolog Inc.) containing 95 substrates including amino acids and carbohydrates. Purified C. burnetii were suspended in CCM (7) (5 × 109 GE/ml) supplemented with 0.65 mM of the reporter dye tetrazolium violet (Sigma–Aldrich) (37). CCM (7) was used as the inoculation fluid rather than more nutritionally rich ACCM to promote oxidation of individual PM substrates. Bacterial suspension (100 μl) was added to each well of the 96-well PM plate and plates incubated for 24 h in an Innova CO-48 incubator (New Brunswick Scientific) at 37 °C adjusted to 5% CO2 and 20%, 5%, or 2.5% O2. Atmospheric oxygen was displaced by nitrogen gas. At the end of the incubation period, reduction of reporter dye was quantified using an OmniLog detection system (Biolog Inc.) and expressed as OmniLog Units (OLU).
Preparation of ACCM Medium and Incubation Conditions.
The ingredients of ACCM are listed in Table 1. Casamino acids were prepared fresh at the time of medium preparation while other components were kept as refrigerated (citrate buffer, salt solution, RPMI cell culture medium) or frozen (neopeptone, FBS, L-cysteine, FeSO4) stocks. The pH of ACCM was adjusted to 4.75 using 6 N NaOH and the medium filtered through a 0.22 μm filter to sterilize. C. burnetii cultures were established in T-25 and T-75 polystyrene cell culture flasks containing 7 ml and 20 ml of ACCM, respectively. Flasks were inoculated with C. burnetii (1.0 × 106 GE/ml) purified from Vero host cells. Cultures were incubated in an Innova CO-48 incubator as described for PM analysis. Growth of C. burnetii on solid medium was conducted using a soft agarose overlay method. A 2× solution of ACCM nutrients was adjusted to pH 4.75, sterilized by filtration and 7.5 ml added to an equal volume of 2% (wt/vol in water) molten UltraPure Agarose (Invitrogen). The 1% ACCM-agarose was poured into 100 × 20 mm Petri dishes to create a solid medium base. Purified C. burnetii was spread on the ACCM-agarose base and 10 ml 0.25% ACCM-agarose added as top agarose. Plates were incubated for 14 days in an Innova CO-48 incubator adjusted to 5% CO2 and 2.5% O2. Colonies were imaged using a Axiovert 40 C microscope (Carl Zeiss MicroImaging, Inc.) equipped with an AxioCam ICc 1 digital camera (Carl Zeiss).
Quantification of C. burnetii Cell Division and Infectivity.
C. burnetii replication during incubation in ACCM was quantified by QPCR of C. burnetii GE using a primer and probe set specific to dotA of C. burnetii (14). ACCM culture aliquots (50 μl) were diluted in 150 μl sterile PBS, diluted 5-fold further with sterile water, then mechanically disrupted to release bacterial DNA using a FastPrep homogenizer (Q-Biogene Inc., CA) and 0.1 mm zerconia/silica beads (Biospec Products Inc., Bartlesville, OK) as lysing matrix. Samples were centrifuged for 1 min at 20,000 × g to pellet the lysing matrix, and equal volumes of supernatant containing chromosomal DNA were used as template DNA for PCR reactions. QPCRs were performed using TaqMan Universal PCR Master Mix and a Prism 7000 sequence detection system (Applied Biosystems).
Infectivity of C. burnetii cultivated in ACCM was determined by a fluorescent focus forming unit (FFU) assay (14). Ten microliter aliquots of C. burnetii ACCM cultures were collected at the indicated times and added to 240 μl RPMI cell culture medium which was then frozen at −80 °C until needed. Equal volumes of thawed culture aliquots were used to infect confluent Vero cell cultures in 24-well plates. Following a 1 h incubation at room temperature with rocking, 1 ml of fresh RPMI medium supplemented with 2% FBS was added to each well. After a 5 day incubation, infected cells were fixed with 100% cold methanol and FFUs stained by indirect immunofluorescence employing polyclonal guinea pig antiserum generated against formalin-killed C. burnetii and Alexa Fluor 448-conjugated goat anti-guinea pig IgG serum (Molecular Probes). FFUs were enumerated by fluorescence microscopy using a Ziess Axiovert 25 inverted microscope. Color saturation was adjusted equally for all images using Adobe PhotoShop.
Transmission Electron Microscopy.
Specimens were fixed as previously described (14). Thin sections were cut with an RMC MT-7000 ultramicrotome (Ventana), stained with 1% uranyl acetate and Reynold's lead citrate before viewing at 80 kV on a Philips CM-10 transmission electron microscope (FEI). Digital images were acquired with a Hammamatsu XR-100 bottom mount CCD system (Advanced Microscopy Techniques). Cross section diameters were measured with the AMT software measuring tool and data analyzed using Prism software (GraphPad Software Inc.). Final images were processed with Adobe PhotoShop (Adobe Systems, Inc.).
Immunoblotting.
C. burnetii was pelleted by centrifugation and lysed by boiling in a solution of 1% SDS. The protein concentration of each sample was determined using a DC Protein Assay kit (Bio-Rad). Samples were diluted in SDS/PAGE sample buffer and 10 μg total protein separated by SDS/PAGE on a 10–20% Tris-HCl Ready Gel (Bio-Rad). Proteins were transferred to an Immobilon-P membrane (Millipore) that was blocked overnight at 4 °C in PBS containing 0.1% Tween-20 and 3% nonfat milk (PBST). Membranes were then incubated for 1 h at room temperature in PBST containing anti-ScvA rabbit polyclonal antibody (15). Membranes were washed, then incubated for 1 h at room temperature in PBST containing anti-mouse IgG secondary antibody conjugated to horseradish peroxidase (Pierce). Reacting proteins were detected via enhanced chemiluminescence using ECL Pico reagent (Pierce) and CL-XPosure film (Pierce).
Statistical Analysis.
Statistical analyses were performed by unpaired Student's t test using Prism software (GraphPad Software Inc.). Differences between data sets where P < 0.05 were considered statistically significant.
Supplementary Material
Acknowledgments.
We thank Ted Hackstadt, Harlan Caldwell, Shelly Robertson, and Frank Gherardini for critical review of this manuscript; Gary Hettrick for graphic illustrations; and Kent Barbian for initial help with the OmniLog detection system. This work was supported by the Intramural Research Program of the National Institutes of Health, National Institute of Allergy and Infectious Diseases.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
Data deposition: The data reported in this paper have been deposited in the Gene Expression Omnibus (GEO) database, www.ncbi.nlm.nih.gov/geo (accession no. GSE13338).
This article contains supporting information online at www.pnas.org/cgi/content/full/0812074106/DCSupplemental.
References
- 1.Maurin M, Raoult D. Q fever. Clin Microbiol Rev. 1999;12:518–553. doi: 10.1128/cmr.12.4.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Derrick EH. “Q” fever, a new fever entity: Clinical features, diagnosis and laboratory investigation. Med J Aust. 1937;2:281–298. doi: 10.1093/clinids/5.4.790. [DOI] [PubMed] [Google Scholar]
- 3.Cox HR. A filter-passing infectious agent isolated from ticks. Description of organism and cultivation experiments. Public Health Rep. 1938;53:2270–2276. [Google Scholar]
- 4.Ormsbee RA, Peacock MG. Metabolic activity in Coxiella burnetii. J Bacteriol. 1964;88:1205–1210. doi: 10.1128/jb.88.5.1205-1210.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burton PR, Stueckemann J, Welsh RM, Paretsky D. Some ultrastructural effects of persistent infections by the rickettsia Coxiella burnetii in mouse L cells and green monkey kidney (Vero) cells. Infect Immun. 1978;21:556–566. doi: 10.1128/iai.21.2.556-566.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hackstadt T, Williams JC. Biochemical stratagem for obligate parasitism of eukaryotic cells by Coxiella burnetii. Proc Natl Acad Sci USA. 1981;78:3240–3244. doi: 10.1073/pnas.78.5.3240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Omsland A, Cockrell DC, Fischer ER, Heinzen RA. Sustained axenic metabolic activity by the obligate intracellular bacterium Coxiella burnetii. J Bacteriol. 2008;190:3203–3212. doi: 10.1128/JB.01911-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moos A, Hackstadt T. Comparative virulence of intra- and interstrain lipopolysaccharide variants of Coxiella burnetii in the guinea pig model. Infect Immun. 1987;55:1144–1150. doi: 10.1128/iai.55.5.1144-1150.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hackstadt T, Williams JC. Stability of the adenosine 5′-triphosphate pool in Coxiella burnetii: Influence of pH and substrate. J Bacteriol. 1981;148:419–425. doi: 10.1128/jb.148.2.419-425.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seshadri R, et al. Complete genome sequence of the Q-fever pathogen Coxiella burnetii. Proc Natl Acad Sci USA. 2003;100:5455–5460. doi: 10.1073/pnas.0931379100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Appelberg R. Macrophage nutriprive antimicrobial mechanisms. J Leukocyte Biol. 2006;79:1117–1128. doi: 10.1189/jlb.0206079. [DOI] [PubMed] [Google Scholar]
- 12.Ewann F, Hoffman PS. Cysteine metabolism in Legionella pneumophila: characterization of an L-cystine-utilizing mutant. Appl Environ Microbiol. 2006;72:3993–4000. doi: 10.1128/AEM.00684-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hendrix L, Mallavia LP. Active transport of proline by Coxiella burnetii. J Gen Microbiol. 1984;130:2857–2863. doi: 10.1099/00221287-130-11-2857. [DOI] [PubMed] [Google Scholar]
- 14.Coleman SA, Fischer ER, Howe D, Mead DJ, Heinzen RA. Temporal analysis of Coxiella burnetii morphological differentiation. J Bacteriol. 2004;186:7344–7352. doi: 10.1128/JB.186.21.7344-7352.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heinzen RA, Howe D, Mallavia LP, Rockey DD, Hackstadt T. Developmentally regulated synthesis of an unusually small, basic peptide by Coxiella burnetii. Mol Microbiol. 1996;22:9–19. doi: 10.1111/j.1365-2958.1996.tb02651.x. [DOI] [PubMed] [Google Scholar]
- 16.George JR, Pine L, Reeves MW, Harrell WK. Amino acid requirements of Legionella pneumophila. J Clin Microbiol. 1980;11:286–291. doi: 10.1128/jcm.11.3.286-291.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barker J, Farrell ID, Hutchison JG. Factors affecting growth of Legionella pneumophila in liquid media. J Med Microbiol. 1986;22:97–100. doi: 10.1099/00222615-22-2-97. [DOI] [PubMed] [Google Scholar]
- 18.Hoffman PS, Pine L, Bell S. Production of superoxide and hydrogen peroxide in medium used to culture Legionella pneumophila: Catalytic decomposition by charcoal. Appl Environ Microbiol. 1983;45:784–791. doi: 10.1128/aem.45.3.784-791.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kana BD, et al. Characterization of the cydAB-encoded cytochrome bd oxidase from Mycobacterium smegmatis. J Bacteriol. 2001;183:7076–7086. doi: 10.1128/JB.183.24.7076-7086.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stephens RS, et al. Genome sequence of an obligate intracellular pathogen of humans: Chlamydia trachomatis. Science. 1998;282:754–759. doi: 10.1126/science.282.5389.754. [DOI] [PubMed] [Google Scholar]
- 21.Schnappinger D, et al. Transcriptional adaptation of Mycobacterium tuberculosis within macrophages: Insights into the phagosomal environment. J Exp Med. 2003;198:693–704. doi: 10.1084/jem.20030846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Juul N, Jensen H, Hvid M, Christiansen G, Birkelund S. Characterization of in vitro chlamydial cultures in low-oxygen atmospheres. J Bacteriol. 2007;189:6723–6726. doi: 10.1128/JB.00279-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.La Scola B, Lepidi H, Raoult D. Pathologic changes during acute Q fever: Influence of the route of infection and inoculum size in infected guinea pigs. Infect Immun. 1997;65:2443–2447. doi: 10.1128/iai.65.6.2443-2447.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Via LE, et al. Tuberculous granulomas are hypoxic in guinea pigs, rabbits, and nonhuman primates. Infect Immun. 2008;76:2333–2340. doi: 10.1128/IAI.01515-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hu H, Sosnovsky G, Swartz HM. Simultaneous measurements of the intra- and extra-cellular oxygen concentration in viable cells. Biochim Biophys Acta. 1992;1112:161–166. doi: 10.1016/0005-2736(92)90387-2. [DOI] [PubMed] [Google Scholar]
- 26.Howe D, Heinzen RA. Coxiella burnetii inhabits a cholesterol-rich vacuole and influences cellular cholesterol metabolism. Cell Microbiol. 2006;8:496–507. doi: 10.1111/j.1462-5822.2005.00641.x. [DOI] [PubMed] [Google Scholar]
- 27.Khan N, et al. Plasma membrane cholesterol: A possible barrier to intracellular oxygen in normal and mutant CHO cells defective in cholesterol metabolism. Biochemistry. 2003;42:23–29. doi: 10.1021/bi026039t. [DOI] [PubMed] [Google Scholar]
- 28.Endley S, McMurray D, Ficht TA. Interruption of the cydB locus in Brucella abortus attenuates intracellular survival and virulence in the mouse model of infection. J Bacteriol. 2001;183:2454–2462. doi: 10.1128/JB.183.8.2454-2462.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldman BS, Gabbert KK, Kranz RG. The temperature-sensitive growth and survival phenotypes of Escherichia coli cydDC and cydAB strains are due to deficiencies in cytochrome bd and are corrected by exogenous catalase and reducing agents. J Bacteriol. 1996;178:6348–6351. doi: 10.1128/jb.178.21.6348-6351.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Madariaga MG, Rezai K, Trenholme GM, Weinstein RA. Q fever: A biological weapon in your backyard. Lancet Infect Dis. 2003;3:709–721. doi: 10.1016/s1473-3099(03)00804-1. [DOI] [PubMed] [Google Scholar]
- 31.Shannon JG, Heinzen RA. Infection of human monocyte-derived macrophages with Coxiella burnetii. Methods Mol Biol. 2008;431:189–200. doi: 10.1007/978-1-60327-032-8_15. [DOI] [PubMed] [Google Scholar]
- 32.Cockrell DC, Beare PA, Fischer ER, Howe D, Heinzen RA. A method for purifying obligate intracellular Coxiella burnetii that employs digitonin lysis of host cells. J Microbiol Methods. 2008;72:321–325. doi: 10.1016/j.mimet.2007.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weiss E. Adenosine triphosphate and other requirements for the utilization of glucose by agents of the psittacosis-trachoma group. J Bacteriol. 1965;90:243–253. doi: 10.1128/jb.90.1.243-253.1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Virtaneva K, et al. Longitudinal analysis of the group A Streptococcus transcriptome in experimental pharyngitis in cynomolgus macaques. Proc Natl Acad Sci USA. 2005;102:9014–9019. doi: 10.1073/pnas.0503671102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beare PA, et al. Genetic diversity of the Q fever agent, Coxiella burnetii, assessed by microarray-based whole-genome comparisons. J Bacteriol. 2006;188:2309–2324. doi: 10.1128/JB.188.7.2309-2324.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li M, et al. Gram-positive three-component antimicrobial peptide-sensing system. Proc Natl Acad Sci USA. 2007;104:9469–9474. doi: 10.1073/pnas.0702159104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bochner BR, Gadzinski P, Panomitros E. Phenotype microarrays for high-throughput phenotypic testing and assay of gene function. Genome Res. 2001;11:1246–1255. doi: 10.1101/gr.186501. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.