Abstract
Purpose: Most health care organizations, including nursing homes, report having teams. However, little is known about everyday practice teams among staff providing direct resident care. We assess the prevalence of such teams in nursing homes as reported by direct care staff and administrators, and examine characteristics of facilities that foster these teams. Design and Methods: The analytical model is based on 149 nursing homes. Data sources include surveys of administrators (n = 292) and direct care staff (n = 6,867), and Online Survey Certification and Reporting System. Linear regression with robust standard errors and sampling probability weights is used to examine the relationship between daily practice teams and facility characteristics. Results: On average, 16% of workers per facility report practicing in formal multidisciplinary teams providing daily resident care. Team prevalence is 3.3% higher when managers view teams as very important for clinical care quality, 2.6% higher when the directors of nursing report formally organized teams, 2.5% higher for each 10% increase in workers' involvement in teams other than the daily practice teams, and 1.95% higher for each 1-hr increase in nursing hours. Implications: Our study shows that multidisciplinary daily practice teams can be found in most facilities in our large sample, but their penetration within nursing homes is far from pervasive; in 72% of facilities, staff report team prevalence of less than 25%. Given that the majority of managers report teamwork as very important to their facilities' operations, we discuss why only a relatively small proportion of daily care is provided in this fashion.
Keywords: Long-term care, Workforce, Teamwork
Assertions about the desirability, relevance, and effectiveness of health care teams have been common in the professional and popular literature for several decades (Halstead, 1976; Lawrence, 2002; Mickan & Roger, 2000). Among the benefits claimed for teams are reduced staff turnover and absenteeism, increased staff motivation, reduced staff conflict, increased quality of care, and improved financial outcomes (Firth-Cozens, 2001; Gittell et al., 2000; Mitchell, Shannon, Cain, & Hegyvary, 1996; Pearson et al. 2006). Good teamwork has been viewed as a prescription for improving patient outcomes (Gittell et al.; Shortell et al., 1994). Several studies have provided empirical evidence demonstrating that teamwork contributes to performance by reducing errors and improving the quality of patient care (Alexander et al., 2005; Edmondson, 1996; Proudfoot, Jayasinghe, Holton, Grimm, & Bubner, 2007; Rafferty, Ball, & Akien, 2001; Shortell et al.; West et al., 2002). Overall, however, there is no conclusive evidence that health care teams enhance patient or organizational outcomes in all health care settings (Lemieux-Charles & McGuire, 2006).
In long-term care where patients with multiple needs require much care coordination, interdisciplinary teams in particular have been lauded as a management practice resulting in better health care (Heinemann & Zeiss, 2002b; Wagner, 2004; Wagner et al., 2001). In nursing homes, teams have been identified as participating in assessing, planning, and delivering care (Forbes-Thompson, Gajewski, Scott-Cawiezell, & Duniton, 2006). Today, virtually all nursing homes have in place interdisciplinary care planning teams as mandated by the clinical guidelines for the Resident Assessment Instrument/Minimum Data Set process and by the long-term care accreditation requirements (Dellefield, 2006; Joint Commission on Accreditation of Healthcare Organizations, 2004). These teams develop residents’ care plans but do not provide ongoing daily care. Interdisciplinary care planning teams come together to perform specific tasks, and when these are accomplished, they disband until the need for these tasks arises again. How well these teams communicate and connect with staff providing direct care may be important in influencing resident outcomes (Colon-Emeric et al., 2006). Specialized multidisciplinary teams may also be present in nursing homes to develop quality improvement initiatives or to attend to specific clinical needs such as wound care or pressure ulcers. None of these teams, however, are specifically designated with the ongoing day-to-day provision of care to the residents. Although presence of interdisciplinary quality improvement and specialized care teams in nursing homes has been well documented, very little is known about the organization of the daily care practice in nursing homes, in particular the extent to which such care is provided by staff working in teams.
It has been argued that effective care coordination for the chronically ill requires strong leadership and good communication among members of different disciplines to develop and implement complex care plans (Keough, Field, & Gurwitz, 2002; Rantz et al., 2003). Empirical evidence to that effect has been provided by several studies focusing on community-based long-term care recipients and their health outcomes (Mukamel et al., 2006; Shortell et al., 2004; Sommers, Marton, Barbaccia, & Randolph, 2000; Wieland, Kramer, Waite, & Rubenstein, 1995). In nursing homes, however, the empirical evidence demonstrating either the presence of daily practice teams or the direct effect of teamwork on quality of care has been rare. Rantz and colleagues (2004) assessed 92 Missouri nursing homes and attributed better patient care outcomes to those facilities that used team and group processes in the provision of daily care. Based on a study of five nursing homes, Yeatts and colleagues offered both qualitative and quantitative data showing that work teams had modest positive effects on certified nursing assistants’ (CNAs) empowerment and performance and on residents’ care (Yeatts & Cready, 2007; Yeatts, Cready, Ray, Dewitt, & Queen, 2004). Scott-Cawiezell and colleagues (2005) investigated the relationship between organizational performance and attributes of teamwork in a purposeful sample of 32 nursing facilities. Key informants in better performing nursing homes were more likely to attribute “the morale and care of the residents” to “teamwork.” Berlowitz and colleagues (2003) demonstrated greater implementation of quality improvement efforts in nursing homes with an organizational culture that emphasizes innovation and teamwork. Several other studies have examined the association between organizational processes related to teamwork such as leadership, communication and interaction among staff, and better resident outcomes (Anderson, Issel, & McDaniel, 2003; Rantz et al., 2003; Scott-Cawiezell et al., 2003; Sheridan, White, & Fairchild, 1992).
Although much has been written about the desirability of management practices that foster teamwork among direct care staff, little is known about the prevalence of such teams in nursing homes or management's support for teamwork. According to one available survey of nursing home administrators (NHAs), conducted by the Iowa Better Jobs Better Care (BJBC) Coalition, 82% of respondents considered it very important to help staff organize their work in teams, but only 51% reported having the time to do so (Iowa BJBC Coalition, 2004). Although the belief in the efficacy of daily practice teams may be growing, empirical evidence for such teams is largely absent. In particular, there have been no large-scale surveys among direct care staff specifically addressing the organization of work environment and presence/absence of daily practice teams, that is, the extent to which workers who provide daily care to nursing home residents are formally organized in teams.
The objectives of this study were to examine the prevalence of daily practice teams in New York State (NYS) nursing homes, as reported by direct care staff and by top managers, and to assess the characteristics of the facilities that foster these teams. We define direct care staff as those who provide personal, clinical, or spiritual care to the residents on a daily basis. Top managers are defined as the facility administrator and the director of nursing (DON). We address the following questions:
What is the reported prevalence of daily practice teams in NYS nursing homes?
What are the characteristics of homes in which daily practice teams are reported?
Conceptual Framework
Unlike assessment, quality improvement, and other functional teams, daily practice teams in nursing homes have been reported only anecdotally, and as occurring only in pockets—on some units, shifts, across departments—rather than in a pervasive facility-wide manner.
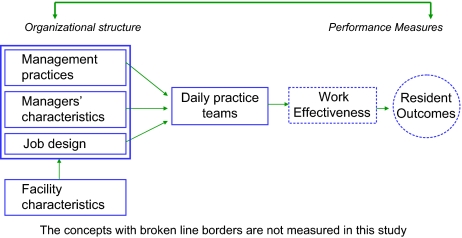
Figure 1 provides a schema of the study framework and the hypothesized relationships between managerial practices and characteristics, facility characteristics, and presence of daily practice teams. Based on current literature, we identified three dimensions of nursing home organizational structure to be particularly relevant to presence of daily practice teams (Anderson et al., 2003; Ashkenasy, Wilderon, & Peterson, 2000; Castle & Banaszak-Holl, 1997; Eaton, 2000; Shortell et al., 2004; Tyler et al., 2006): (a) management practices—the extent to which management values its employees, supports innovation, and encourages teamwork; (b) job design—the characteristics of the tasks that make up a job given to the direct care staff and their potential for producing motivated work behavior; and (c) characteristics of nursing home managers—top managements’ characteristics that may influence team presence. Furthermore, because facility characteristics, such as ownership status or nursing staffing, have been shown to affect these dimensions of nursing home structure (Unruh & Wan, 2004), we incorporate several such factors in the conceptual model.
Figure 1.
Expected relationships between organizational structure and prevalence of daily practice teams.
Hypotheses
Management Practices.—
Leadership characteristics and style have been noted to affect the presence of teams in nursing homes (Eaton, 2000; Reinhard & Stone, 2001). Similarly, organizational context, defined as atmosphere or environmental effect of the workplace, has been thought to promote or impede both the presence of teams and their work (Fagan, 2003; Heinemann & Zeiss, 2002a; Hollinger-Smith, 2003; Hollinger-Smith, Ortigara, & Linderman, 2001). Therefore, we propose to test the following hypothesis:
Hypothesis 1a: In nursing homes characterized by less autocratic management style, direct care staff report greater prevalence of daily practice teams.
The leaders of each facility—the NHA and the DON—are responsible for the development of communication, coordination, and teamwork, necessary for the delivery of care to frail and complex patients (Anderson et al., 2003). Consistent commitment of the senior leadership has been shown to be essential for developing and sustaining teamwork within organizations (Frankel, Leonard, & Denham, 2006). We therefore hypothesize the following:
Hypothesis 1b: Direct care staff is more likely to report daily care practice teams in nursing homes where management view such teams as very important to the operations of their facilities.
Although nursing home managers may routinely refer to groups of workers as a team, the workers are usually assigned individual tasks. For a group to function as a team, its mission, and members' roles and responsibilities, as well as rules and procedures for operating, need to be formally defined, developed, and implemented (Anderson et al., 2003; Heinemann & Zeiss, 2002a). We therefore hypothesize the following:
Hypothesis 1c: Direct care workers are more likely to report being part of daily practice teams in facilities where top managers report formally organized daily practice teams to be present.
Job Design.—
Job design theory suggests that job design is likely to affect work performance through such characteristics as skill variety, task significance, autonomy, and feedback (Hackman & Oldham, 1980). In nursing homes, job design has been shown to affect care quality, employee satisfaction, and turnover (Cotton & Tuttle, 1986; Eaton, 2000). For example, nurse aides’ participation in care planning teams has been shown to significantly lower turnover (Banaszak-Holl & Hines, 1996). Direct care workers’ participation on such teams may be associated with greater prevalence of daily practice teams. Therefore, we hypothesize the following:
Hypothesis 2a: Facilities that involve the direct care staff in specialized care teams (e.g., care planning, quality improvement) will have higher reported prevalence of daily practice teams.
Implementation of the daily practice teams in nursing homes involves changes in how the caregiving process is organized, for example, by placing more decision-making responsibility in the hands of the staff providing care to the residents. Especially salient in this regard is replacing the practice of rotating staff with “primary assignments,” in which staff work consistently with the same residents, a practice with documented benefits (Smyer, Brannon, & Cohn, 1992; Weiner & Ronch, 2003). We hypothesize the following:
Hypothesis 2b: Facilities with greater proportion of direct care staff reporting primary assignment will report higher prevalence of daily practice teams.
Managers’ Characteristics.—
Existing research has demonstrated a relationship between the adoption of innovations and the characteristics of top management in many organizations, including nursing homes (Lucas et al., 2005). Studies have suggested that longer tenure in the profession provides managers with the necessary legitimacy for the adoption of innovations (Castle & Banaszak-Holl, 1997). Studies have also shown that high administrative turnover may have a “destabilizing influence” (Singh & Schwab, 1998) on facility operations and may weaken employees’ commitment to the organization (Castle, 2005), both of which would be detrimental to the development and maintenance of teams. We therefore suggest the following hypotheses:
Hypothesis 3a: Facilities with greater turnover among top management will report lower prevalence of daily practice teams.
Hypothesis 3b: Facilities with longer tenure by top management will report higher prevalence of daily practice teams.
Facility Characteristics.—
Implementation of work improvement strategies such as teams is not likely to succeed in nursing home environments with inadequate staffing (Yeatts & Cready, 2007). We therefore suggest the following hypothesis:
Hypothesis 4a: Facilities with higher nursing staffing will report higher prevalence of daily practice teams.
For-profit nursing homes are often viewed as being driven primarily by the profit motive and thus as less likely to implement innovations in care delivery compared with the not-for-profit facilities (Banaszak-Holl, Zinn, & Mor, 1996; Mukamel & Spector, 2000; Spector & Takada, 1991). Because the development and implementation of teams is not without cost (Yeatts et al., 2004), we hypothesize the following:
Hypothesis 4b: Not-for-profit facilities will report higher prevalence of daily practice teams compared with for-profit homes.
Methods
Data used in this study come from primary and secondary sources. Primary data were collected via two surveys. First, a survey of nursing home managers—administrators and DONs—was conducted between March and September 2006. This survey focused on managers’ views on teams and teamwork and included information on the characteristics of respondents and their facilities. Second, a survey of nursing home workers—those providing direct care to the residents—was conducted from July 2006 through April 2007. This survey examined workers’ perception of daily practice teams in their facilities, job design, and their assessment of the management style prevalent in their facilities. Secondary data, containing information on facility characteristics, were obtained from the Online Survey Certification and Reporting System (OSCAR) uploaded in September 2006.
The study protocol was approved by the Institutional Review Board of the University of Rochester.
Nursing Home Management Surveys
This study utilizes data from a larger parent project designed to examine the impact of work performance on risk-adjusted outcomes of nursing home residents in NYS. For that study, a sample of 180 facilities was determined to be sufficient (to detect a 20% effect size in risk-adjusted outcomes), assuming a significance level of .05 and at least 80% power. Eligible facilities included 615 nursing homes that (a) were certified for Medicare or Medicaid; (b) had more than 50 beds, as measures of work performance in facilities with small staff size are subject to greater measurement error; (c) did not specifically focus on special-needs patients (e.g., pediatric facilities or those providing only rehabilitative care), as such facilities (including hospital-based facilities) have fundamentally different organizational structures and strategic aims; and (d) had at least 2 years of operational experience, as new facilities are more likely to be experiencing a learning curve.
To request participation in the study, all eligible nursing homes were contacted by mail and provided with a summary of the project and letters of support from the two state nursing home associations. Participation in the larger project required each facility to complete two management surveys, one by the NHA and another by the DON, and to distribute surveys aimed at the direct care staff. To increase participation in the study, several strategies were implemented: three follow-up reminders were mailed to each nonresponding facility; reminder emails and personal phone calls were made; three brief articles about the study appeared in the newsletters routinely distributed to all facilities by the two state nursing home associations.
In total, 190 facilities responded with at least one management survey. Overall, 372 management surveys were received.
Nursing Home Direct Care Staff Surveys
The administrators of each participating facility were provided with the number of survey packets corresponding to the estimated number of all direct care staff in their facility. We based our estimates on the staffing data provided in the management surveys. The administrators were asked to distribute the survey packets, which contained the survey, and letter from the research team and the facility administrator, as well as information on the participation in a prize raffle for those who complete the survey. Respondents mailed the surveys back directly to the research team using prepaid envelopes.
In total, direct care workers from 162 nursing homes completed 7,418 surveys representing response rates ranging from 3% to 91% per facility. Of the respondents, 50% were CNAs, 19% licensed practical nurses (LPNs), 13% registered nurses (RNs), 9% therapists, and 9% other (e.g., physicians, social workers, chaplains).
Analytical Sample
Data from the two surveys were merged at the facility level. Of the 162 nursing homes, which responded with the direct care staff surveys, 154 (81%) had completed both the DON and the administrator surveys. Five nursing homes were excluded from the final analytical sample because they had missing values for several independent variables. The analytical model is based on 149 nursing homes (78% of the 190 that agreed to participate) and includes data from 292 NHA and DON surveys (78% of the 372 management surveys received) and 6,867 direct worker surveys (93% of the 7,418 surveys received).
Measures
Development of the survey tools followed accepted questionnaire construction methods (Dillman, 1978). A review of the literature provided initial direction on item development. Interviews with key informants—nursing home managers and direct care staff—provided additional input. Content experts on nursing homes reviewed early drafts of the instruments and commented on content, relevance, face validity, and clarity. The management survey was then pilot tested with a group of individuals resembling the target population to identify any questions that were ambiguous or poorly written and to ascertain clarity of instructions and the time needed to complete the survey. As a result of the pilot, the questionnaire was slightly revised.
The survey instrument used with the direct care workers was modeled on a tool previously adapted from Shortell's organization and management survey (Shortell, Rousseau, Gilles, Devers, & Simons, 1991). Versions of this tool have been previously adapted for use in nursing homes (Scott-Cawiezell et al., 2003, 2005) and in other long-term care settings (Temkin-Greener, Mukamel, Gross, & Kunitz, 2004). The tool used in this study was modified specifically for the purposes of the study.
Outcome Variable.—
We defined the outcome of interest—prevalence of daily practice teams—as a continuous variable. In each facility, this variable measures the percent of direct care workers who report being a member of a formally organized team that exists to provide daily resident care.
Independent Variables.—
Independent variables, obtained from the two surveys and from OSCAR, have been grouped as follows:
Management practices.—
The direct care workers' survey included a scale for assessing the management style in each facility. Management style may be characterized as autocratic, custodial, supportive, or collegial, in order of increasing managerial receptivity for staff input, trust between management and workers, organizational capacity for change, and openness to new ideas, including teams. We used a pretested and validated scale from the Learn, Empower, Achieve, Produce (LEAP) Organizational Learning Readiness Survey (Hollinger-Smith, personal communication, December 20, 2005; Kiefer et al., 2005). This tool uses a 12-item scale (four subscales) with a 5-point Likert-type response format, ranging from almost never (1) to almost always (5). Average subscale scores were calculated for each facility based on all survey responses, and the highest total subscale score reflects the dominant management style in the facility. Only a few facilities were defined as autocratic, and they were combined together with the next category of homes, defined as custodial. This scale has been used in assessing nursing homes’ readiness for organizational change (Biles et al., 2005; Kiefer et al., 2005).
Within each facility, the DONs were asked if the direct care workers (e.g., RNs, LPNs, CNAs) were organized in teams to provide daily care to residents, and whether these teams were formally organized (with defined membership, structure, and processes) or were naturally occurring workgroups (staff working together as needed).
We also included questions about the importance the administrators and the DONs attributed to teamwork with regard to residents' quality of life, clinical quality of care, staff turnover and retention, and the relationship between staff and residents. The responses to each item, ranging from unimportant (score of 1) to very important (score of 4), were summed and averaged for each facility.
All management practice variables were coded as categorical variables.
Job design.—
Two job design variables associated with prevalence of daily practice teams were identified from the direct care workers' survey. These are as follows: specialized care teams and primary care assignment. Specialized care teams organized to accomplish specific tasks—for example, care planning, quality improvement, or special care (e.g., wound care, incontinence)—are known to exist in many nursing homes. We constructed a continuous variable defined as the percent of direct care workers participating on teams other than daily practice teams in each facility.
We defined primary assignment as the percent of direct care workers assigned to the same residents most of the time.
Characteristics of nursing home managers.—
Based on the management survey, we included measures of NHA and DON tenure and turnover. Turnover is defined by the number of times the manager changed in the past 3 years. Tenure is the overall professional experience, measured by the number of months in this position (in this or any other facility).
Facility characteristics.—
Two facility characteristics were included using the OSCAR database. These are as follows: ownership status and number of nursing hours per resident per day. We defined ownership as the profit status of the facility (dichotomous variable). Nursing hours (continuous variable) were defined as the sum of hours provided by RNs, LPNs, and CNAs per resident per day.
Statistical Analyses
To examine the relationship between daily practice teams and nursing home characteristics, we fit a weighted linear regression model with robust standard errors estimated using STATA version 9.2. For each facility, the dependent and the independent variables were weighted by the square root of the number of respondents in that facility to adjust for the variations across facilities. Furthermore, because the study sample includes disproportionately more nonprofit facilities than in the general population of NYS nursing homes, we included sampling weights to obtain the appropriately weighted estimations.
We performed diagnostic tests for collinearity, using a variance inflation factor among the independent variables, and detected no evidence of significant effects that may inflate standard errors. Furthermore, based on the Breusch–Pagan and White tests, we found no evidence of heteroscedasticity.
Results
Response Bias and Generalizability
Because the survey was open to all eligible NYS nursing homes rather than based on a randomly selected sample of facilities, the possibility of a response bias must be considered. To assess this, we compared the 149 nursing homes included in the analytical sample with all eligible NYS facilities on several characteristics that could affect presence of daily practice teams (Table 1). The participating homes appear to be statistically significantly different (p = .03) in terms of occupancy rates (94.2% vs. 93.1%) from all NYS facilities eligible for the study, but this difference does not seem to be operationally or organizationally meaningful. However, the participating homes are significantly (p < .0001) less likely to represent for-profit facilities in New York (31.5% vs. 49.1%). We correct for this potential bias in the multivariate analysis with the use of sampling probability weights. We find no other statistically significant (p < .05) differences between the study sample and all eligible nursing homes on the remaining facility characteristics or with regard to quality of care and staffing measures.
Table 1.
Characteristics of Sample Facilities Compared With All Eligible NYS Nursing Homes
| Participating nursing homes (N = 149) | All NYS nursing homes (N = 615) | p Value | |
| Quality measuresa | |||
| No. of health-related citations | 13.14 | 13.18 | .96 |
| No. of non-health-related citations | 3.70 | 4.18 | .12 |
| Staffing characteristicsa | |||
| RN hours per resident per day | 0.61 | 0.58 | .23 |
| LPN + CNA hours per resident per day | 3.10 | 3.02 | .07 |
| Facility characteristicsb | |||
| Bed size | 216.16 | 192.83 | .06 |
| Occupancy rate (%) | 94.22 | 93.09 | .03 |
| Church related (%) | 8.72 | 6.58 | .29 |
| Chain membership (%) | 10.07 | 12.50 | .37 |
| For profit (%) | 31.54 | 49.11 | <.00 |
Notes: NYS = New York State; CNA = certified nurse assistant; LPN = licensed practical nurse; RN = registered nurse.
Data source: CMS Nursing Home Compare.
Data source: Online Survey Certification and Reporting System.
Description of Daily Practice Teams
Descriptive statistics consisting of the percent and sample size (categorical variables) and the mean, standard deviation, and range (continuous variables) are presented for the dependent and the independent variables in Table 2.
Table 2.
Variables Included in the Analysis of Daily Care Teams Prevalence: Descriptive Statisticsa
| Variable | Categorical variables | Continuous variables |
||
| % (n) | M (SD) | Range |
||
| Minimum | Maximum | |||
| Dependent variable | ||||
| % direct care staff who report working in formal daily practice teams | 15.95 (7.8) | 0.00 | 44.44 | |
| Predictor variables | ||||
| Management practice | ||||
| % facilities with NHAs reporting formal daily practice teamsb | 71.81 (107) | |||
| % facilities with DONs reporting formal daily practice teamsb | 77.18 (115) | |||
| Managers view teamwork as very important with regard tob | ||||
| Residents’ quality of life | 89.61 (134) | |||
| Clinical quality of care | 90.26 (134) | |||
| Staff turnover and retention | 68.18 (102) | |||
| Staff–residents relationship | 79.22 (118) | |||
| Management style | ||||
| Collegial | 47.65 (71) | |||
| Supportive | 30.87 (46) | |||
| Custodial/autocratic | 21.48 (32) | |||
| Job design | ||||
| % direct care workers with primary assignment | 40.20 (15.9) | 0.00 | 100.00 | |
| % direct care workers participating in other than daily practice teams | 33.20 (12.2) | 8.77 | 83.33 | |
| Characteristics of nursing home managers | ||||
| Turnover—DONb | 0.8523 (1.003) | 0.00 | 5.000 | |
| Tenure—DON (months)b | 81.42 (73.602) | 1.000 | 336.000 | |
| Turnover—NHAb | 0.557 (0.825) | 0.000 | 3.000 | |
| Tenure—NHA (months)b | 169.85 (113.86) | 1.000 | 441.000 | |
| Facility characteristics | ||||
| Not-for-profit facilityc | 68.46 (102) | |||
| Total nursing hours per resident per dayc | 3.71 (0.626) | 1.540 | 5.630 | |
Notes: NHA = nursing home administrator; DON = director of nursing.
Facility level data from 149 New York State nursing homes.
Variables from the management surveys.
Variables from Online Survey Certification and Reporting System database. All other variables are from surveys of nursing home workers.
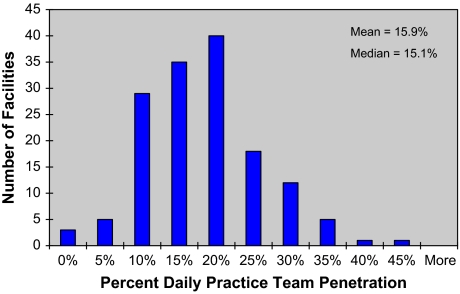
In an average facility, 15.9% of the direct care workers view themselves as working in formally organized daily practice teams. The distribution of daily practice team penetration in the study nursing homes is shown in Figure 2. In half of the facilities, daily practice team penetration is lower than 15%, but only a few (n = 3) report no daily practice teams at all. Similarly, almost half of the facilities report team prevalence greater than 20%, but none report penetrations above 44%. It is important to point out that these daily practice teams are reported to be formally organized and to be multidisciplinary (Figure 3). Overall, the CNAs report 84% of their daily practice teams to include other disciplines, whereas the LPNs and the RNs report, respectively, 94% and 98% of their teams to be multidisciplinary. These workers report roughly similar participation of their own professions in the daily practice teams but show more variation with regard to team participation of physicians, social workers, and therapists (Figure 3). For example, whereas 46% of the CNAs report physicians to be on their teams, 66% and 69% of the LPNs and the RNs, respectively, report physicians on daily practice teams.
Figure 2.
Prevalence of daily practice teams in nursing homes (N = 149).
Figure 3.
Daily practice team composition reported by CNAs, RNs, and LPNs. CNA = certified nurse assistant; LPN = licensed practical nurse; RN = registered nurse; SW = social worker; PT/OT = therapist; MD = physician; Or = other.
The respondents were also asked about specific activities such as team meetings with other members to discuss residents’ care. Almost half (47.2%) report these meetings to occur daily, whereas an additional 25.0% and 16.2% report meeting at least once per week or once per month, respectively.
In at least 70% of the facilities, NHAs (71.8%) and DONs (77.2) report presence of formal daily practice teams. The NHAs and the DONs are very enthusiastic about the importance of teamwork in the operations of their facilities. Almost all view teams as very important in promoting residents' quality of life (89.6%) and clinical quality of care (90.3%). Furthermore, 79.2% report teams as very important in maintaining good staff–resident relationships, and 68.2% think teams are very important with regard to staff turnover and retention (Table 2).
Description of other independent variables is also provided in Table 2. Nursing home staff assessed close to 80% of the facilities as having collegial (47.65%) or supportive (30.87%) management styles, that is, not hierarchical and open to employee input, whereas an additional 21.48% reported homes with more traditional and authoritarian management style (i.e., custodial/autocratic).
There appears to be substantial variability across nursing homes with regard to the job design indicators. In an average facility, 40% of the direct care workers report having primary assignment (SD = 15.9%), ranging from none to 100% across all facilities. In the average facility, 33.2% of direct care workers report participating on teams other than the daily practice teams (SD = 12%), with a range from 8.7% to 83.3%.
There is also substantial variability across these facilities in both tenure and turnover of the top administrators. For example, the average tenure is 81 months (SD = 73) for the DONs and 169 months (SD = 113) for the NHAs.
Characteristics of Nursing Homes With Daily Practice Teams
We estimated a linear regression model with robust standard errors and sampling weights, correcting for response bias, to examine the characteristics of nursing homes associated with daily practice teams' prevalence. (The model was also estimated without the probability weights, and the results, not shown here, were virtually unchanged.) The results are summarized in Table 3.
Table 3.
Characteristics Predicting Prevalence of Daily Care Teams in Nursing Homes: Linear Regression Model With Robust Standard Errors and Probability Weightsa
| Predictor variables | Parameter coefficient | Standardized coefficientb | p Valuec |
| Intercept | 2.677 | — | .796 |
| Management practices (H1a–b) | |||
| Management style (custodial/autocratic = reference category) | |||
| Collegial | −1.715 | −0.111 | .157 |
| Supportive | −1.795 | −0.102 | .245 |
| Managers view teamwork as very important with regard to | |||
| Residents’ quality of life | −1.488 | −0.076 | .459 |
| Clinical quality of care | 3.302 | 0.166 | .080 |
| Staff turnover and retention | 1.027 | 0.065 | .402 |
| Staff–residents relationship | −1.420 | −0.085 | .389 |
| NHAs reporting formal daily care teams | −0.188 | −0.012 | .892 |
| DONs reporting formal daily care teams | 2.601 | 0.159 | .072 |
| Job design (H2a–b) | |||
| % direct care staff with primary assignment | −8.276 | −0.200 | .100 |
| % direct care staff on other than daily teams | 25.014 | 0.412 | <.001 |
| Characteristics of nursing home managers (H3a–b) | |||
| Turnover—DON | 0.034 | 0.004 | .952 |
| Tenure—DON (months) | 0.008 | 0.083 | .171 |
| Turnover—NHA | 0.859 | 0.082 | .280 |
| Tenure—NHA (months) | 0.004 | 0.060 | .422 |
| Facility characteristics (H4a–b) | |||
| Not-for-profit facility (profit = reference category) | 0.095 | 0.006 | .930 |
| Total nursing hours per resident per day | 1.946 | 0.317 | .012 |
Notes: NHA = nursing home administrator; DON = director of nursing. Model: N = 149, R2 = .4703.
Probability weights corrected for sampling response bias.
Parameter coefficients were standardized by subtracting the mean and dividing by standard deviation.
p values <.1 are bolded.
The importance of several management practices in predicting prevalence of daily practice teams supports several posited hypotheses. In facilities where nursing home leaders consider teams very important with regard to clinical quality of care, team prevalence is significantly higher by 3.3% (Hypothesis 1b). However, administrators’ perceptions of the importance of teams with regard to other aspects of care (e.g., residents’ quality of life), reported as equally important, are not significantly associated with the presence of daily practice teams. Furthermore, team prevalence as reported by the direct care staff is 2.6% higher in facilities in which the DON reports presence of formal daily practice teams (Hypothesis 1c).
Of the two job design variables—primary assignment and participation on other teams—only the latter is statistically significant (p < .001). A 10% increase in direct care staff involvement in other than daily teams is associated with a 2.5% increase in prevalence of daily practice teams (Hypothesis 2a). This is the strongest predictor (standardized coefficient = 41.20) of daily practice team prevalence in the study facilities.
One of the facility characteristics is also shown to be significantly associated with daily practice team prevalence, providing support for Hypothesis 4a. A 1-hr increase in nursing hours per resident per day is associated with a 1.95% increase in daily team prevalence.
We find no statistically significant association between managers’ characteristics or management practices and team prevalence.
Discussion
A number of largely qualitative studies have suggested that presence of teams may be an important organizational feature related to a variety of nursing home performance measures, including better resident care (Anderson et al., 2003; Berlowitz et al., 2003; Scott-Cawiezell et al., 2005). Although 97% of U.S. health care organizations report the use of teams in some form (Shortell et al., 2004), little is known about the presence of daily practice teams in nursing facilities. The findings from this study provide, for the first time, empirical evidence regarding the prevalence of daily practice teams as reported by both the managers and, more importantly, a large sample of the direct care staff employed in nursing homes in NYS, one of the largest states in the country.
Our findings are to some extent consistent with the apparently widespread reporting of teams in health care organizations but are at the same time surprising. On the one hand our study shows that daily practice teams can be found in most nursing homes in our large sample. Based on reports from NHAs and DONs, more than 70% of facilities have formally organized daily practice teams. Based on employee surveys, all but 10% of the facilities had at least 5% of the direct care staff work in daily practice teams. So, daily practice teams seem to be present in the vast majority of facilities. On the other hand, their penetration within the nursing home is far from pervasive. On average, the prevalence is only 16%, and in 72% of the facilities, direct care workers report a prevalence of less than 25%.
These findings, considered together with the fact that between 80% and 90% of the managers state that teamwork is “very important” to various aspects of their facilities’ operations, indicate that most nursing home managers recognize the importance of teams, yet at the same time raising the question of why penetration of teams is so limited. If teams are indeed a beneficial way of providing daily care in nursing homes, why is only a relatively small proportion of the care provided in this fashion?
Some insights into this apparent paradox may be gleaned from the multivariate analysis that tests the hypotheses we delineated about the influence of management practices, job design, and facility characteristics on the prevalence of daily practice teams in nursing homes. We find that higher team penetration is associated with three factors: (a) management perceptions of teams’ importance with respect to quality of care, (b) staff participation in other functional teams (i.e., care planning or specialized care), and (c) higher staffing ratios. The first is self-explanatory. Obviously, a management team that believes in the importance of team practice as contributing to quality of care is more likely to foster the creation of teams. However, given that most managers already recognize the importance of teams, the magnitude of the association with team prevalence that we observe is rather small. The second factor can be understood as the effect of a team learning curve. Nursing homes that gain positive experience with task-specific teams might be more comfortable applying these work structures more broadly to daily care activities, which affect wider areas of their operations. It has been suggested that the development of teams in an organization is evolutionary and moves through sequential stages (Abbott, Boyd, & Miles, 2006; Heinemann, 2002). The use of teams in performing the primary work of the organization occurs in the last stage of this process, and it requires the greatest organizational commitment (VanAken, Monetta, & Sink, 1994). In a prior stage, employees’ involvement may include participation in problem-solving teams that are task specific, such as for care planning, quality improvement, or wound care, but which do not extend to the provision of ongoing daily care. Greater prevalence of daily practice teams may be possible in only those facilities that have already invested in other task-specific team-based job designs. The third factor, higher nursing staffing level, may be related to the fact that teamwork may not be feasible or efficient at low staffing levels. However, the association with staffing revealed by the multivariate analysis, suggesting a small increase (1.95%) in team prevalence for 1 additional nursing hour per resident per day, may not be conducive to greater team development given the current nursing home reimbursement rates. In the absence of specific payment incentives to increase staffing levels, nursing homes are not likely to volunteer on their own. Early results from the recently implemented nursing home payment incentive programs in Florida and California have shown that additional payments to nursing homes did increase staff wages and resulted in some increases in staffing (Hyer, Johnson, Harman, & Mehra, 2007; Schnelle, Mukamel, Sato, & Chang, 2008).
Limitations
Several caveats are noteworthy and may be instructive of further research needed. First, our assessment of daily practice team prevalence is based on a single point-in-time estimate. In facilities with significant staff turnover, such point-in-time estimates may not be stable. Similarly, as nursing homes undertake organizational and/or cultural changes that include team building, they may experience increased prevalence in daily practice teams. Second, our study is limited to facilities in NYS. To the extent that nursing homes in other states may be affected by different regulatory requirements, such as those related to staffing, they may have substantially different prevalence of daily practice teams. Finally, although we include what we considered the most important and most likely potential predictors of team prevalence in this study, given that many of them have not proven to be predictive, it is possible that other omitted factors may be more important in explaining this phenomenon. For example, although we considered the stability of management as a predictor of team prevalence, characteristics relating to the stability of staff were not included in this analysis, and yet, they might be more important. Additional analyses with regard to staff retention and turnover and their relationship to team prevalence may be warranted. Team development and teamwork may also be functions of certain attributes of the work environment such as leadership and communication (Forbes-Thompson et al., 2006). Future studies should explore these relationships.
Conclusions
Although this analysis identifies some of the factors that are associated with higher penetration of teams, it does not answer the question of why the overall penetration of daily practice teams in nursing homes is so low. Further research into factors that facilitate the organization and functioning of teams in nursing homes may help administrators make daily practice teams more common by lowering the barriers to their implementation.
Perhaps the apparent inconsistency we observe with regard to daily practice teams’ pervasiveness may be, at least partially, traced to the lack of clear empirical evidence about their effectiveness. Although, as discussed in the introduction, there is extensive literature about the effectiveness of teams in acute and chronic care settings, most studies do not include nursing homes. The empirical evidence from nursing homes is limited, based on small samples, and for the most part does not relate to daily practice teams. Therefore, it may not be surprising that although the managers appear enthusiastic about such teams’ potential, they are also hesitant and embrace them only cautiously. Further research is needed to provide empirical evidence about the effectiveness of daily practice teams in nursing homes in terms of their impact both on costs and quality, in particular the impact on resident health outcomes. Such evidence would be useful in informing management’s decisions as to how best to organize their workforce.
Funding
We gratefully acknowledge funding from the National Institute on Aging, grant R01 AG23077.
Acknowledgments
Thanks go to the participating nursing homes and their staff and to the New York Association of Homes and Services for the Aging and the NYS Health Facilities Association. We also thank Ms. Pluma (Scottie) Kluess for her assistance.
References
- Abbott J, Boyd N, Miles G. Does type of team matter? An investigation of the relationship between job characteristics and outcomes within a team-based environment. Journal of Social Psychology. 2006;146:485–507. doi: 10.3200/SOCP.146.4.485-507. [DOI] [PubMed] [Google Scholar]
- Alexander J, Lichtenstein R, Jinnettt K, Wells R, Zazzali J, Liu D. Cross-functional team processes and patient functional improvement. Health Services Research. 2005;40:1335–1355. doi: 10.1111/j.1475-6773.2005.00418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson R, Issel L, McDaniel R., Jr Nursing homes as complex adaptive systems: Relationship between management practice and resident outcomes. Nursing Research. 2003;52:12–21. doi: 10.1097/00006199-200301000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashkenasy N, Wilderon C, Peterson M. Handbook of organizational culture and climate. Thousand Oaks, CA: Sage; 2000. [Google Scholar]
- Banaszak-Holl J, Hines M. Factors associated with nursing home staff turnover. Gerontologist. 1996;36:512–517. doi: 10.1093/geront/36.4.512. [DOI] [PubMed] [Google Scholar]
- Banaszak-Holl J, Zinn J, Mor V. The impact of market and organizational characteristics on nursing facility service innovation: A resource dependency perspective. Health Services Research. 1996;31:97. [PMC free article] [PubMed] [Google Scholar]
- Berlowitz D, Young G, Hickey E, Saliba B, Mittman BS, Czamowski E, et al. Quality Improvement Implementation in the Nursing Home. Health Services Research. 2003;38:65–83. doi: 10.1111/1475-6773.00105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biles B, Burke R, Stone R, Wing R, McCloskey K, Henderson TM, et al. Act now for your tomorrow: Final report of the National Commission on Nursing Workforce for Long-Term Care. 2005. [Google Scholar]
- Castle N. Turnover begets turnover. Gerontologist. 2005;45:186–195. doi: 10.1093/geront/45.2.186. http://www.ahca.org/research/workforce_rpt_050519. [DOI] [PubMed] [Google Scholar]
- Castle N, Banaszak-Holl J. Top management team characteristics and innovation in nursing homes. Gerontologist. 1997;37:572–580. doi: 10.1093/geront/37.5.572. [DOI] [PubMed] [Google Scholar]
- Colon-Emeric C, Lekan-Rutledge D, Utley-Smith Q, Ammarell N, Bailey D, Piven ML, et al. Connection, regulation, and care plan innovation: A case study of four nursing homes. Health Care Management Review. 2006;31:337–346. doi: 10.1097/00004010-200610000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotton J, Tuttle J. Employee turnover: A meta-analysis and review with implications for research. Academy of Management Review. 1986;11:55–70. [Google Scholar]
- Dellefield M. Interdisciplinary care planning and the written care plan in nursing homes: A critical review. Gerontologist. 2006;46:128–133. doi: 10.1093/geront/46.1.128. [DOI] [PubMed] [Google Scholar]
- Dillman D. Mail and telephone surveys: The total design method. New York: Wiley; 1978. [Google Scholar]
- Eaton S. Beyond unloving care: Linking human resource management and patient care quality in nursing homes. International Journal of Human Resource Management. 2000;11:591–616. [Google Scholar]
- Edmondson A. Learning from mistakes is easier said than done: Group and organizational influences on the detection and correction of human error. Journal of Applied Behavioral Science. 1996;32:5–28. [Google Scholar]
- Fagan R. Culture change in long-term care. In: Weiner A, Ronch J, editors. Pioneer network. New York: Hawthorn Press; 2003. pp. 125–149. [Google Scholar]
- Firth-Cozens J. Multidisciplinary teamwork: The good, bad, and everything in between. Quality in Health Care. 2001;10:65–66. doi: 10.1136/qhc.10.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes-Thompson S, Gajewski B, Scott-Cawiezell J, Dunton N. An exploration of nursing home organizational processes. Western Journal of Nursing Research. 2006;28:935–954. doi: 10.1177/0193945906287053. [DOI] [PubMed] [Google Scholar]
- Frankel A, Leonard M, Denham C. Fair and just culture, team behavior, and leadership engagement: The tools to achieve high reliability. Health Services Research. 2006;41:1690–1709. doi: 10.1111/j.1475-6773.2006.00572.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittell J, Fairfield K, Bierbaum B, Head W, Jackson R, Kelly M, et al. Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: A nine-hospital study of surgical patients. Medical Care. 2000;38:807–819. doi: 10.1097/00005650-200008000-00005. [DOI] [PubMed] [Google Scholar]
- Hackman J, Oldham G. Work redesign. Reading, MA: Addison-Wesley; 1980. [Google Scholar]
- Halstead L. Team in chronic illness: A review of the literature of the past 25 years. Archives of Physical Medicine and Rehabilitation. 1976;57:507–511. [PubMed] [Google Scholar]
- Heinemann GD. Teams in health care settings. In: Heinemann GD, Zeiss AM, editors. Team performance in health care: Assessment and development. New York: Kluwer Academic/Plenum; 2002. pp. 3–28. [Google Scholar]
- Heinemann GD, Zeiss AM. A model of team performance. In: Heinemann GD, Zeiss AM, editors. Team performance in health care: Assessment and development. New York: Kluwer Academic/Plenum; 2002a. pp. 29–42. [Google Scholar]
- Heinemann GD, Zeiss AM. Team performance in health care: Assessment and development. New York: Kluwer Academic/Plenum; 2002b. [Google Scholar]
- Hollinger-Smith L. It takes a village to retain quality nursing staff: The Mather LifeWays LEAP training program uses the three Rs of retention to prevent staff turnover. Nursing Home Magazine. 2003;52:52–54. [Google Scholar]
- Hollinger-Smith L, Ortigara A, Lindeman D. Developing a comprehensive long term care workforce initiative. Alzheimer's Care Quarterly. 2001;2:33–40. [Google Scholar]
- Hyer K, Johnson C, Harman J, Mehra S. Staffing mandates matter: Florida nursing home provider response to financial incentives to increase nurse staffing. 2007, June Paper presented at the annual meeting of Academy Health, Orlando, FL. [Google Scholar]
- Iowa BJBC Coalition. Nursing home administrator survey. Report of findings. Des Moines, IA: Iowa Caregivers Association; 2004. [Google Scholar]
- Joint Commission on Accreditation of Healthcare Organizations. Comprehensive accreditation manual for long-term care. Oakbrook Terrace, IL: Joint Commission Resources; 2004. [Google Scholar]
- Keough M, Field T, Gurwitz J. A model of community-based interdisciplinary team training in the care of the frail elderly. Academic Medicine. 2002;77:936. doi: 10.1097/00001888-200209000-00041. [DOI] [PubMed] [Google Scholar]
- Kiefer K, Harris-Kojetin L, Brannon D, Barry T, Vasey J, Lepore M. Measuring long-term care work: A guide to selected instruments to examine direct care worker experience and outcomes. (Rep. No. HHS-100-01-0025) Washington, DC: Office of the Assistant Secretary for Policy, U.S. Department of Labor; 2005. [Google Scholar]
- Lawrence D. From chaos to care: The promise of team-based medicine. Cambridge, MA: Perseus; 2002. [Google Scholar]
- Lemieux-Charles L, McGuire W. What do we know about health care team effectiveness? Medical Care Research and Review. 2006;63:263–300. doi: 10.1177/1077558706287003. [DOI] [PubMed] [Google Scholar]
- Lucas JA, Avi-Itzhak T, Robinson J, et al. Continuous quality improvement as an innovation: Which nursing facilities adopt it? Gerontologist. 2005;45:68–77. doi: 10.1093/geront/45.1.68. [DOI] [PubMed] [Google Scholar]
- Lucas JA, Avi-Itzhak T, Robinson J, Morris CG, Koren MJ, Reinhard SC. Characteristics of effective teams: A literature review. Australian Health Review. 2000;23:201–208. doi: 10.1071/ah000201. [DOI] [PubMed] [Google Scholar]
- Mitchell P, Shannon S, Cain K, Hegyvary S. Critical care outcomes: Linking structures, processes, and organizational and clinical outcomes. American Journal of Critical Care. 1996;5:353–363. [PubMed] [Google Scholar]
- Mukamel DB, Spector WD. Nursing home costs and risk-adjusted outcome measures of quality. Medical Care. 2000;38:78–89. doi: 10.1097/00005650-200001000-00009. [DOI] [PubMed] [Google Scholar]
- Mukamel D, Temkin-Greener H, Delavan R, Petterson D, Gross D, Kunitz S, et al. Team performance and risk-adjusted health outcomes in the Program of All-Inclusive Care for the Elderly (PACE) Gerontologist. 2006;46:227–237. doi: 10.1093/geront/46.2.227. [DOI] [PubMed] [Google Scholar]
- Pearson A, Porritt K, Doran D, Vincent L, Craig D, Tucker D, et al. A comprehensive systematic review of evidence on the structure, process, characteristics and composition of a nursing team that fosters healthy work environment. International Journal of Evidence-Based Healthcare. 2006;4:118–159. doi: 10.1111/j.1479-6988.2006.00039.x. [DOI] [PubMed] [Google Scholar]
- Proudfoot J, Jayasinghe U, Holton C, Grimm J, Bubner TEA. Team climate for innovation: What difference does it make in general practice? International Journal for Quality in Health Care. 2007;19:164–169. doi: 10.1093/intqhc/mzm005. [DOI] [PubMed] [Google Scholar]
- Rafferty A, Ball J, Aiken L. Are teamwork and professional autonomy compatible, and do they result in improved hospital care? Quality in Health Care. 2001;10:32–37. doi: 10.1136/qhc.0100032... [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rantz M, Grando V, Conn V, Zwygart-Staffacher M, Hicks L, Flesner M, et al. Getting the basics right. Care delivery in nursing home. Journal of Gerontological Nursing. 2003;29:15–25. doi: 10.3928/0098-9134-20031101-07. [DOI] [PubMed] [Google Scholar]
- Rantz M, Hicks L, Grando V, Petroski G, Madsen R, Mehr D, et al. Nursing home quality, cost, staffing, and staff mix. Gerontologist. 2004;44:24–38. doi: 10.1093/geront/44.1.24. [DOI] [PubMed] [Google Scholar]
- Reinhard S, Stone R. Promoting quality in nursing homes: The Wellspring Model. New York: The Commonwealth Fund; 2001. [Google Scholar]
- Schnelle J, Mukamel DB, Sato H, Chang J. Study of California's New Medi-Cal Reimbursement System for nursing homes. 2008. (Rep. No. California Alliance For Nursing Home Reform). Unpublished report. [Google Scholar]
- Scott-Cawiezell J, Main D, Vojir C, Jones K, Moore L, Nutting PA, et al. Linking nursing home working conditions to organizational performance. Health Care Management Review. 2005;30:372–380. doi: 10.1097/00004010-200510000-00011. [DOI] [PubMed] [Google Scholar]
- Scott-Cawiezell J, Schenkman M, Moore L, Vojir C, Connolly R, Pratt M, et al. Exploring nursing home staff's perceptions of communication and leadership to facilitate quality improvement. Journal of Nursing Care Quality. 2004;19:242–252. doi: 10.1097/00001786-200407000-00011. [DOI] [PubMed] [Google Scholar]
- Sheridan JE, White J, Fairchild TJ. Ineffective staff, ineffective supervision, or ineffective administration? Why some nursing homes fail to provide adequate care. Gerontologist. 1992;32:334–341. doi: 10.1093/geront/32.3.334. [DOI] [PubMed] [Google Scholar]
- Shortell S, Marsteller J, Lin M, Pearson ML, Wu S, Mendel P, et al. The role of perceived team effectiveness in improving chronic illness care. Medical Care. 2004;42:1040–1048. doi: 10.1097/00005650-200411000-00002. [DOI] [PubMed] [Google Scholar]
- Shortell SM, Rousseau DM, Gillies RR, Devers K, Simons TL. Organizational assessment in intensive care units (ICUs): Construct development, reliability, and validity of the ICU Nurse-Physician Questionnaire. Medical Care. 1991;29:709–727. doi: 10.1097/00005650-199108000-00004. [DOI] [PubMed] [Google Scholar]
- Shortell SM, Zimmerman JE, Rousseau DM, Gillies RR, Wagner DP, Draper EA, et al. The performance of intensive care units: Does good management make a difference? Medical Care. 1994;32:508–525. doi: 10.1097/00005650-199405000-00009. [DOI] [PubMed] [Google Scholar]
- Singh D, Schwab R. Retention of administrators in nursing homes. What can management do? Gerontologist. 1998;38:362–369. doi: 10.1093/geront/38.3.362. [DOI] [PubMed] [Google Scholar]
- Smyer M, Brannon D, Cohn M. Improving nursing home care through training and job redesign. Gerontologist. 1992;32:327–333. doi: 10.1093/geront/32.3.327. [DOI] [PubMed] [Google Scholar]
- Sommers L, Marton K, Barbaccia J, Randolph J. Physician, nurse, and social worker collaboration in primary care for chronically ill seniors. Archives of Internal Medicine. 2000;160:1825–1833. doi: 10.1001/archinte.160.12.1825. [DOI] [PubMed] [Google Scholar]
- Spector WD, Takada HA. Characteristics of nursing homes that affect resident outcomes. Journal of Aging Health. 1991;3:427–454. doi: 10.1177/089826439100300401. [DOI] [PubMed] [Google Scholar]
- Temkin-Greener H, Mukamel D, Gross D, Kunitz S. Measuring interdisciplinary team performance in a long-term care setting. Medical Care. 2004;42:472–481. doi: 10.1097/01.mlr.0000124306.28397.e2. [DOI] [PubMed] [Google Scholar]
- Tyeler D, Parkers V, Engle R, et al. An exploration of job design in long-term care facilities and its effect on nursing employee satisfaction. Health Care Management Review. 2006;31:137–144. doi: 10.1097/00004010-200604000-00007. [DOI] [PubMed] [Google Scholar]
- Unruh L, Wan T. A systems framework for evaluating nursing care quality in nursing homes. Journal of Medical Systems. 2004;28:197–214. doi: 10.1023/b:joms.0000023302.80118.74. [DOI] [PubMed] [Google Scholar]
- VanAken E, Monetta D, Sink D. Affinity groups: The missing link in employee involvement. Organizational Dynamics. 1994;22:38–54. [Google Scholar]
- Wagner EH. Effective teamwork and quality of care. Medical Care. 2004;42:1037–1039. doi: 10.1097/01.mlr.0000145875.60036.ed. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Glasgow RE, Davis C, Bonomi AE, Provost L, McCulloch D, et al. Quality improvement in chronic illness care: A collaborative approach. Joint Commission Journal on Quality Improvement. 2001;27:63–80. doi: 10.1016/s1070-3241(01)27007-2. [DOI] [PubMed] [Google Scholar]
- Weiner A, Ronch J. Culture change in long-term care. New York: Haworth Press; 2003. [Google Scholar]
- West M, Borrill C, Dawson J, Scully J, Carter M, Anelay S, et al. The link between the management of employees and patient mortality in acute hospitals. International Journal of Human Resource Management. 2002;13:1299–1310. [Google Scholar]
- Wieland D, Kramer BJ, Waite M, Rubenstein L. The interdisciplinary team in geriatric care. American Behavioral Scientist. 1995;39:655–664. [Google Scholar]
- Yeatts D, Cready C. Consequences of empowered CNA teams in nursing home settings: A longitudinal assessment. Gerontologist. 2007;47:323–339. doi: 10.1093/geront/47.3.323. [DOI] [PubMed] [Google Scholar]
- Yeatts D, Cready C, Ray B, DeWitt A, Queen C. Self-managed work teams in nursing homes: Implementing and empowering nurse aide teams. Gerontologist. 2004;44:256–261. doi: 10.1093/geront/44.2.256. [DOI] [PubMed] [Google Scholar]