Abstract
Mucus is a viscoelastic and adhesive gel that protects the lung airways, gastrointestinal (GI) tract, vagina, eye and other mucosal surfaces. Most foreign particulates, including conventional particle-based drug delivery systems, are efficiently trapped in human mucus layers by steric obstruction and/or adhesion. Trapped particles are typically removed from the mucosal tissue within seconds to a few hours depending on anatomical location, thereby strongly limiting the duration of sustained drug delivery locally. A number of debilitating diseases could be treated more effectively and with fewer side effects if drugs and genes could be more efficiently delivered to the underlying mucosal tissues in a controlled manner. This review first describes the tenacious mucus barrier properties that have precluded the efficient penetration of therapeutic particles. It then reviews the design and development of new mucus-penetrating particles that may avoid rapid mucus clearance mechanisms, and thereby provide targeted or sustained drug delivery for localized therapies in mucosal tissues.
1. Introduction
Delivery technologies that improve drug pharmacokinetics and facilitate localized delivery to target tissues strongly improve the efficacy of various therapies [1, 2]. In particular, an increasing number of nanoparticle-based drug delivery systems have been approved for human use or are currently being evaluated in clinical trials [3, 4]. Nanoparticle systems can be engineered to possess a number of desirable features for therapy, including: (i) sustained and controlled release of drugs locally [5, 6], (ii) deep tissue penetration due to the nano-metric size [7–9], (iii) cellular uptake and sub-cellular trafficking [10, 11], and (iv) protection of cargo therapeutics at both extracellular and intracellular levels [12, 13].
The development of controlled release systems for drug and gene delivery to mucosal surfaces, such as those of the lung airways, GI tract, female reproductive tract, nose and eye, is of widespread interest. However, the viscous, elastic and sticky mucus layer that lines all mucosal tissues has evolved to protect the body by rapidly trapping and removing foreign particles and hydrophobic molecules [14, 15]. The limited permeability of drug delivery particles and many hydrophobic drugs through the mucus barrier leads to their rapid clearance from the delivery site, often precluding effective drug therapies at non-toxic dosages.
In order to avoid rapid mucus clearance mechanism and/or reach the underlying epithelia, nanoparticles must quickly traverse at least the outermost layers of the mucus barrier (that is cleared most rapidly). Mucus layer thickness depends strongly on anatomical site, and can range from less than 1 micron up to several hundred microns [15, 16]. Until recently, nanoparticles were thought incapable of efficiently penetrating mucus layers[17]. The need for new strategies to increase particle transport rates is underscored by: (i) observations of the immobilization of conventional nanoparticles in mucus ex vivo [18, 19]; (ii) the very slow transport rate of 180 nm herpes simplex virus (diameter ~180 nm) in mucus ex vivo [19]; and (iii) animal studies showing that mucus immobilizes a range of particle types [20–23].
In order to penetrate mucus, synthetic nanoparticles must avoid adhesion to mucin fibers and be small enough to avoid significant steric inhibition by the dense fiber mesh. Recently, we demonstrated that nanoparticles as large as 500 nm, if sufficiently coated with a muco-inert polymer, can rapidly traverse physiological human mucus with diffusivities as high as only 4-fold reduced compared to their rates in pure water [17]. This finding suggests that it is possible to engineer nanoparticles that overcome the mucus barrier. Combined with a suitably tailored drug release profile, these “mucus-penetrating particle” (MPP) systems offer the prospect of sustained drug delivery at mucosal surfaces and, thus, provide hope for improved efficacy and reduced side effects for a wide range of therapeutics. The generation of MPP loaded with nucleic acids may also greatly enhance the efficacy of this critical family of therapeutic agents [24, 25].
This article reviews the mechanisms by which mucus hinders or prevents particle penetration, including a discussion of previous work on nanoparticle transport in mucus both ex vivo and in vivo. Subsequently, the recent development of mucus penetrating nanoparticles is described.
2. Mucus as a critical barrier to nanoparticle therapies
2.1 Composition of mucus, mucus thickness, and mucus clearance times
Mucus is a viscoelastic gel layer that protects tissues that would otherwise be exposed to the external environment. Mucus is composed primarily of crosslinked and entangled mucin fibers secreted by goblet cells and submucosal glands [26–28]. Mucins are large molecules, typically 0.5–40 MDa in size [15, 16] formed by the linking of numerous mucin monomers, each about 0.3–0.5 MDa [29, 30], and are coated with a complex and highly diverse array of proteoglycans[15, 31]. At least twenty mucin-type glycoproteins have been assigned to the MUC gene family [31, 32], with several mucin types expressed at each mucosal surface [32–35]. Mucins can be generally separated into two families: cell-associated mucins ranging between 100–500 nm in length that contain a transmembrane domain, and secreted mucins that are up to several microns long [31, 36, 37]. Individual mucin fibers are roughly 3–10 nm in diameter, as determined by biochemical and electron microscopy studies [38, 39]. They are highly flexible molecules, with a persistence length of roughly 15 nm [15]. With the exception of specific disease states (such as COPD and CF), the mucin content ranges between 2–5% by weight for cervical, nasal, and lung mucus [40–44], with glycosylated oligosaccharides representing 40–80% of the mucin mass [15]. The water content in most mucus types (i.e., lung, gastric, cervicovaginal) commonly falls within the 90–98% range [35, 43–46].
In addition to mucins, mucus gels are loaded with cells, bacteria, lipids, salts, proteins, macromolecules, and cellular debris [15, 17]. The various components work together to form a nanoscopically heterogeneous environment for particle transport [47], with a shear-dependent bulk viscosity that is typically 1,000–10,000 times more viscous than water at low shear rates [15, 17, 47]. Mucus viscoelasticity is tightly regulated in healthy subjects by controlling the mucin to water secretion ratio [48], as well as by varying lipid [49], protein [50], and ion content [51]. Readers are referred to a review on mucus rheology in this issue for further details [47].
Mucus pH can vary greatly depending on the mucosal surface, with highly acidic environments capable of aggregating mucin fibers and greatly increasing the mucus viscoelasticity[52, 53]. Lung and nasal mucus are in general pH neutral [54, 55], and eye mucus is slightly basic with pH ~7.8 [56]. In contrast, gastric mucus is exposed to a wide range of pH: a large pH gradient exists within the same mucus cross-section, with pH rising from the luminal pH of ~1–2 to ~7 at the epithelial surface [57]. Vaginal secretions typically exhibit pH in the range of 3.5 to 4.5 due to acidification from lactic acid produced by lactobacilli under anaerobic conditions [15, 58, 59].
Beyond biochemical differences, the thickness of the mucus blanket also varies for different mucosal surfaces. Estimates of human mucus layer thickness in different tissues are given in Table 1. In the lung, the thickness of the luminal mucus gel is generally thought to be ~5–10 μm [60, 61]. The underlying, less viscoelastic sol layer, also known as the periciliary liquid (PCL), is occupied by cilia and constitutes an additional 5–10 μm in thickness [60, 62, 63]. However, more recent studies based on confocal fluorescence microscopy suggest that airway mucus may range in thickness from 5 to 55 μm [64–67]. Under particular disease conditions, such as cystic fibrosis (CF), the average thickness of airway mucus can markedly increase, likely reflecting accumulation of the mucus resulting from impaired mucociliary clearance [67]. The nasal tract, which has a mucus layer of limited thickness, is readily accessible and considered highly permeable compared to other mucosal surfaces [1]. In the human GI tract, the mucus layer is thickest in the stomach and the colon, but exhibits significant variation [68–74]. The relative thickness of the luminal mucus gel and the cell-associated mucus layer in the human GI tract remains under-characterized. The thickness of GI mucus may also vary greatly depending on digestive activity. For instance, dietary fiber deficiency can lead to a significantly lower mucus thickness in rats [75]. In the female reproductive tract, the adherent mucus layer includes the glycocalyx of epithelial cells and is expected to be at least tens of microns thick in humans, although precise estimates are unavailable. In the eye, the secreted precorneal mucin gel covering the conjunctiva was previously thought to be ~5 μm [76, 77], but more recently suggested to be as thick as 30–40 μm [56, 78].
Table 1.
Thickness of various types of normal human mucus.
| Type of Mucus | Average Thickness (μm) | Reported Thicknesses (μm) |
|---|---|---|
| Respiratory | ||
| Airway | 15 | 7 [64, 66]; 30 [65] |
| Bronchial | 55 | 55 ± 5 [67] |
| Gastrointestinal* | ||
| Gastric | 170 | 144 ± 52 [208]; 192 ± 7 [209] |
| Ileal | 10 | 10 [74] |
| Cecal | 37 | 36.7 ± 7.2 [72] |
| Colonic† | 100 | 39.1 ± 9.9 (A), 57.5 ± 14.5 (T), and 69.6 ± 32.1 (D) [72]; 79 ± 40 [74]; 100–150 [68]; 107 ± 48 (A-T) and 134 ± 68 (T-D) [73]; 110–160 [69] |
| Rectal | 125 | 101.5 ± 80.3 [72]; 155 ± 54 [73] |
| Ocular | ||
| Mucus Layer (only) | 0.035 | 0.02–0.05 [77] |
| Tear Film | 5 | 3 [77]; 6–7 [76] |
| 40 | 34–45 [78] | |
Gastrointestinal mucus generally exists as two layers, a basal “unstirred” or “firmly adherent” layer and a luminal “stirred” or “sloppy” layer [210–212]; however, most of the cited references report only one value for mucus layer thickness. Matsuo et al. [72] report the thickness of both an “inner layer” and “outer layer” of mucus; in the cecum, the inner layer was measured to be 5.6 +/− 0.2 μm; in the colon, 4.7 +/− 1.4 μm for the ascending colon, 7.0 +/− 3.7 μm for the transverse colon, and 7.6 +/− 3.4 μm for the descending colon; and in the rectum, 12.7 +/− 6.0 μm.
A = ascending colon; T = transverse colon; D = descending colon.
Mucus is continuously secreted, then shed and discarded or digested and recycled. Its lifetime is short, often measured in minutes to hours (Table 2). The fastest turnover is typically observed at surfaces with the thinnest mucus layer, perhaps as an evolutionary response to improve the protective features of the mucosa. In the nasal tract, the ciliary motion transports mucus from the anterior towards the posterior region of the nasal cavity, moving entrapped particles and potentially toxic materials toward the nasopharynx. The mucus flow rate is about 5 mm per minute, and the mucus layer is renewed approximately every 20 minutes [32, 79, 80]. Likewise, the luminal gel layer of respiratory tract mucus is replaced every 10 to 20 minutes, leading to efficient clearance of inhaled particulates [32]. In contrast, the sol phase of respiratory mucus is thought to be cleared much less rapidly than the more solid-like luminal gel layer [55–58]. Continuous secretion and clearance by peristaltic forces leads to quick turnover times, on the order of 4–6 hrs, in the rat gastrointestinal tract [12, 81, 82] and likely similar values in humans. In the vagina, mucus is cleared (expelled through the introitus) by intra-abdominal pressure as well as abdominal motions, which squeeze the walls of the vagina together [83, 84]. The typical clearance time in the human CV tract remains unclear, but is likely on the order of a few hours. In the eye, the tear turnover rate under normal physiological conditions is in the range of 13–20% per minute, leading to nearly complete clearance of most molecules and particulates from the eye within minutes [56].
Table 2.
Clearance time and rate for various types of normal human mucus.
| Type of Mucus | Clearance Time (min) | Clearance Rate (mm/min) | Ref. |
|---|---|---|---|
| Respiratory | |||
| General | 10–20 | * | [32] |
| Maxillary Sinus | 20–30 | * | [32] |
| Nasal | 8.8 | * | [213] |
| * | 5–11 | [80] | |
| 20 | 5 | [79, 214, 215] | |
| Tracheal | * | 4.1±1.9 | [216] |
| * | 4.7 (range: 3.5–6) | [216–222] | |
| * | 15.5 (range: 4.5–30)# | [223–230] | |
| Bronchial | * | 2.4±0.5 | [217] |
| Small Airways | * | 1 | [231] |
| Ocular | 5–7.7 | * | [56] |
The understanding of mucus layer thickness and clearance times at various mucosal surfaces is important to the development of particles designed to overcome mucosal clearance mechanisms, since they must penetrate mucus at rates markedly faster than mucus renewal and clearance in order to overcome the barrier.
2.2 Mechanism of particulate transport in mucus: Channeling through low viscosity pores
The bulk viscosity of healthy human mucus is typically 1,000–10,000 times higher than the viscosity of water (at low shear rates). The Stokes-Einstein equation for diffusion in homogenous fluids predicts that neither viruses nor many hydrophilic macromolecules would be capable of penetrating a homogeneous fluid layer of this viscosity. Indeed, the diffusion of many macromolecules over extended distances in mucus, or at rates faster than mucociliary clearance, was long assumed to be an improbable event [85]. That view began to change with increasing evidence that a number of macromolecules rapidly diffuse through mucus. Important work by the Saltzman and Cone groups showed that the diffusion of various proteins, including antibodies, in human midcycle cervical mucus was largely unhindered relative to their rates in water [86]. The study also suggested that viruses as large as 30 nm should diffuse nearly unhindered in cervical mucus, which was subsequently proven by Cone and coworkers [19]. In particular, they found that Norwalk (38 nm) and human papilloma virus (HPV; 55 nm) penetrated mucus at rates roughly equivalent to that in water. These results firmly establish that particulates are capable of diffusing through low viscosity pores within the highly elastic mucin fiber matrix. In general, if the viscosity of the fluid that fills the pores in mucus is equivalent to that of water, the diffusion rates of particulates significantly smaller than the average mucus mesh pore size, assuming they do not adhere to mucus, are expected to be similar to their expected rates in water.
Cone and coworkers also showed that the diffusion of herpes simplex virus (HSV), a virus with a diameter ~180 nm, was nearly completely inhibited [19]. Even the very small fraction of virus that was mobile moved at rates 100- to 1000-fold slower than their expected rates in water. The slow transport of HSV agrees well with an obstruction scaling model [87, 88] that assumes the average pore size to be ~100 nm (Figure 1). This pore size estimate agreed well with the size of viruses capable of efficient infection of mucosal tissues, including polio (28 nm), hepatitis B (43 nm), adenoviruses (60–90 nm), and rotavirus (75 nm) [15]. Based on these lines of evidence, the development of mucus-penetrating particles appeared to be limited to the dimensions of small viruses, raising significant formulation and practical concerns.
Figure 1.

Transmission electron micrograph of human cervicovaginal mucus. The interfiber spacing ranges from 10 nm to 200 nm. Individual fibers can be observed with fiber diameters ~10 nm. Scale bar = 200 nm. Figure obtained from [19].
2.3 Mucus as a “sticky” net
Airborne particles typically adhere to respiratory mucus before reaching the alveoli. Filtered particles are removed from the airways by mucociliary clearance and become sterilized by gastric acid [14, 89]. Similarly, intestinal mucus prevents the transport of toxic contents from the lumen of the GI tract to the underlying interstitial and vascular fluids [15]. The primary mechanism by which mucus gels efficiently trap foreign particulates is the formation of polyvalent adhesive interactions [15, 90]. In addition to the negative charges imparted by the presence of carboxyl or sulfate groups on the mucin proteoglycans, there exist periodic hydrophobic “naked” globular regions along mucin strands, stabilized by multiple internal disulfide bonds [91]. The high density of hydrophobic domains, coupled with the flexible nature of mucin fibers, affords efficient formation of multiple low-affinity adhesive interactions with hydrophobic regions on the surfaces of foreign particulates. Although each low-affinity hydrophobic interaction can be readily disrupted by thermal energy, a large number of low-affinity adhesive interactions with the mucus mesh effectively immobilizes particles with permanent high viscidity [15].
The formation of polyvalent low-affinity interactions is critical for the removal of foreign particles smaller than the average mucus mesh pore size. An excellent example of this phenomenon is the strong immobilization of virus-sized carboxyl-modified polystyrene nanoparticles, including those as small as 59 nm, in human cervical mucus [18, 19]. Despite possessing a negative surface charge that might be expected to repel negatively charged mucins, polystyrene nanoparticles form multiple hydrophobic adhesive interactions with mucin fibers that are strong enough to bundle mucin strands into thick cables (Figure 2). Similar immobilization of albumin- or casein-coated particles underscores the efficiency of the hydrophobic adhesive interactions [15]. Hydrophobic interactions also represent an important mechanism by which mucus limits the transport of large entities such as bacteria. Potentially harmful pathogens, including Escherichia coli, Pseudomonas aeruginosa, and Yersinia enterocolitica, are all immobilized by mucus via hydrophobic interactions [92–94].
Figure 2.
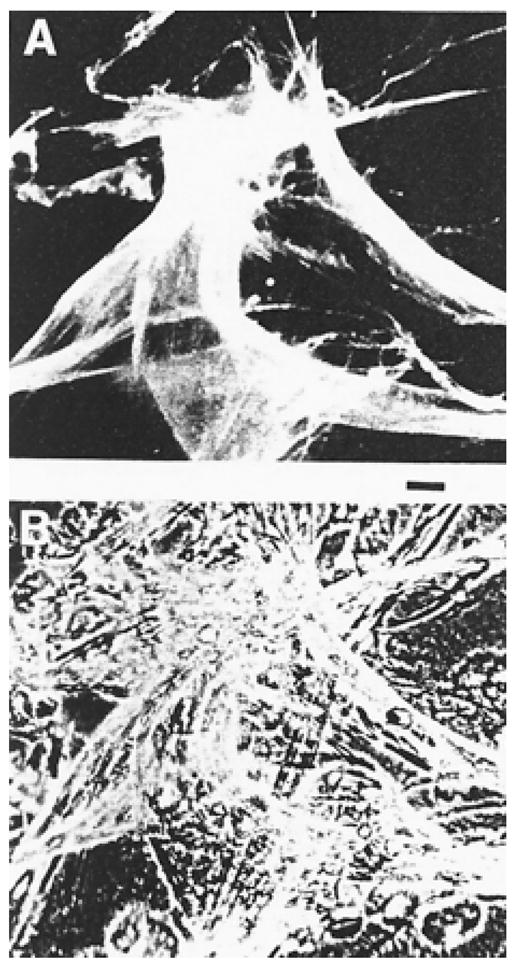
Fluorescently labeled 59 nm polystyrene particles formed thick cables with mucin fibers in human cervicovaginal mucus. (A) Fluorescent image. (B) Phase image. Scale bar = 500 μm. Figure obtained from [19].
Polyvalent adhesive interactions with mucus can be achieved via electrostatic interactions as well. Since the glycosylated regions of mucin fibers are densely coated with negative charges, mucus can also bind positively charged particles with high avidity. The dual capacity to form polyvalent adhesive interactions via both hydrophobic and anionic forces represents a particularly challenging problem for polymeric nanoparticles designed to deliver drugs and genes, since many commonly used biomaterials are either hydrophobic, such as poly(lactide-co-glycolide) and poly(anhydrides) [95, 96], or cationic, such as polyethylenimine, chitosan and polylysine [59, 97, 98]. However, despite the great avidity of these polyvalent adhesive interactions, the capacity for mucus to immobilize foreign particles may become saturated. This was demonstrated by the work of Durrer and colleagues, who found that small particles can be adsorbed to the mucin fibers only until the internal area available for adsorption is saturated [99–101].
The ubiquitous presence of hydrophobic domains in the mucus mesh also helps to explain why many therapeutic molecules diffuse more slowly through mucus than other molecules of similar or larger size. The diffusion of hydrophobic molecules is often significantly hindered in mucus compared to in water [102–104]. Diffusivity is typically reduced as nonpolar/polar partition coefficient increases, an expected consequence of adhesive interactions between hydrophobic molecules and the hydrophobic domains of mucus. Several investigators have also shown that mucus significantly decreases the diffusion of a number of both small and large molecules, including tertiary amines [105], bovine serum albumin [106], lysozyme [106], and others [104, 106–108], presumably due to hydrophobic interactions. Nonetheless, some hydrophobic molecules are capable of diffusing through mucus gels, perhaps because small molecules are not capable of forming polyvalent adhesive bonds with the mucus gel.
3. Conventional nanoparticles become trapped in mucus
3.1 Typical fate of nanoparticles in mucus-covered tissues & conventional strategies for enhancing residence time
When administered to various mucosal tissues, conventional nanoparticles are likely to be trapped by mucus via steric or adhesive forces and rapidly eliminated via mucociliary clearance. In the GI tract, for example, nanoparticles delivered orally may undergo: (1) association with chyme, causing direct transit through the GI tract and fecal elimination; (2) adhesion to mucin fibers, followed by mucus clearance and fecal elimination; or (3) transport across the mucus mesh for possible entry to the underlying epithelia or prolonged residence time in the unstirred layer of mucus gel [81, 109]. Typically, the majority of administered particles do not adhere or transport through the GI mucus, but rather undergo direct transit through the GI tract [81, 110]. The consequent short transit time in the GI tract can be inadequate for particles to release a significant fraction of encapsulated drugs, thereby precluding in many cases the realization of a high local drug concentration over extended periods of time, hence leading to low bioavailability and poor efficacy.
To overcome the short transit time, research has largely centered on minimizing the fraction of therapeutics undergoing direct transit and fecal elimination by improving their association to mucus. This phenomenon, known as mucoadhesion, is widely defined as the ability of polymeric systems to adhere to the mucus layer [81, 109, 111]. Mucoadhesion slows the particle transit time through the GI tract to the time scale of mucus renewal, thereby enhancing drug absorption. The design of mucoadhesive drug delivery systems is currently the predominant approach to improving mucosal delivery of therapeutics.
3.2 Ex vivo studies of conventional particle transport in mucus
That mucus slows the diffusion of macromolecules has long been inferred using indirect techniques, or by measuring rates of permeation through a thin layer of mucus in a diffusion chamber [104, 108]. The same experimental approach has been used extensively to study the diffusion of polymeric particles in mucus. Among the first reports to quantitatively measure the 1D diffusivity of particles in mucus, Sinko and coworkers studied the diffusion of variously sized polystyrene particles in a reconstituted porcine gastric mucin gel, sandwiched between the two chambers of a Transwell-Snapwell diffusion chamber (Figure 3), and observed a sharp decrease in translocation permeability when particle sizes approached 300 nm [90]. Sanders et al. reported that an extremely low percentage of carboxylated polystyrene nanospheres moved through a 220 μm-thick CF sputum layer after 150 minutes, with the largest nanospheres studied (560 nm) almost completely blocked by the sputum [112]. Interestingly, nanospheres diffused more efficiently through more viscoelastic sputum samples, which the authors attributed to a more macroporous structure as viscoelasticity increased. More recently, a similar diffusion-chamber method was used to investigate actin’s role in limiting the degree to which common mucolytics enhance the diffusion of particles in mucus [113]. Although the diffusion-chamber method is conceptually straightforward, it may be sensitive to parameters that are difficult to control, such as the precise thickness of the mucus layer, the uniformity of the mucus distribution across the face of the filters, blockage of the filter pores by mucus, and alterations in mucus properties during preparation [86]. As an example of the latter, a significant amount of mucin was found to have diffused through the membrane when the pore size of the diffusion chamber filter was greater than 5 μm, thereby reducing the barrier properties of mucus [90].
Figure 3.
Schematic drawing of a Transwell-Snapwell diffusion chamber (A). The donor and acceptor chambers are indicated by I and II, respectively. Mucus or mucin gel is sandwiched in between polycarbonate filters attached to the Snapwell ring (E) located between the two chambers. Figure obtained from [112].
To circumvent potential artifacts stemming from diffusion chamber studies, a number of studies measured the dynamic transport of nanoparticles using fluorescent microscopy techniques, including fluorescence recovery after photobleaching (FRAP), and more recently, high resolution multiple particle tracking (MPT). For example, pioneering work on protein and virus diffusion in human midcycle cervical mucus in two laboratories (Saltzman and Cone) relied on FRAP to elucidate rapid local diffusion in the low viscosity pores present in the mucus mesh [19, 86]. More recently, Saltzman and coworkers applied FRAP to investigate the diffusion of plasmid DNA, with and without association to liposomes, in reconstituted bovine cervical mucus [114]. They showed that bovine mucus hinders the diffusion of linear DNA, especially when the plasmid size exceeds 5 kb, compared to supercoiled DNA. Fluorescence recovery in 3D, via standard confocal scanning laser microscopes, was developed to test the diffusion of macromolecules in CF sputum by Demeester and coworkers in 2003 [18].
Although FRAP has contributed valuable insight to the diffusion of macromolecules and particulates in mucus, FRAP provides only ensemble-averaged diffusion rates and cannot be used to quantify the transport rates of individual particles. A lack of information at the individual particle level may limit insight into the complex phenomena that control nanoparticle transport in the heterogeneous mucus network, where the transport rates of identical particles can vary by several orders of magnitude in the same sample.[115]. To this end, Hanes and coworkers have pioneered the use of MPT as applied to drug and gene delivery applications [10, 115–117], including the transport of nanoparticles in mucus [17, 118, 119]. MPT allows for unparalleled insight into the fractions of particles that are adherent to mucus at any given time, and yields quantitative measures of the extent of particle hindrance to free diffusion at the individual particle or ensemble-average level, important feedback in the development of non-mucoadhesive particle surfaces. Coupled with Monte Carlo simulations of Brownian behavior, MPT can also be used to determine in a quantitative and high-throughput manner the transport mechanism (immobile, hindered-diffusion, diffusive, or active/convective transport) governing particle dynamics in mucus and in other complex biological fluids [17, 117, 120].
Dawson et al. first applied MPT to measure the transport rates of nanoparticles in mucus. Using a set up that achieved 5 nm and 33 ms spatiotemporal resolution, they studied the movements of carboxylate- and amine-modified polystyrene nanoparticles sized 100–500 nm in fresh human sputum obtained from patients with cystic fibrosis (CF) [118]. The diffusion of nanoparticles were more than an order of magnitude faster than the diffusivity predicted from the macrorheology of the mucus, but at least 300-fold slower than the same particles in water. Neutrally charged hydrophobic particles ~200 nm in diameter appeared to undergo more rapid transport in CF sputum than anionic but otherwise similar particles, suggesting surface charge may be an important parameter in governing transport rates of nanoparticles in mucus. In a separate work, Dawson et al. used MPT to study the diffusion of biodegradable hydrophobic PLGA nanoparticles surface coated with anionic DNA via the cationic surfactant dimethyl dioctadecyl ammonium bromide (DDAB). Coating with hydrophilic DNA improved the average nanoparticle transport rates by 10-fold in reconstituted pig gastric mucus compared to slightly smaller, hydrophobic polystyrene particles (Figure 4) [119]. In addition, a significant fraction of PLGA-DDAB/DNA particles appeared to undergo unrestricted diffusive transport, supported indirectly by the finding that a considerably higher percentage of PLGA-DDAB/DNA nanoparticles (8.5%) exhibited a MSD >5-fold higher than the ensemble average MSD, compared to corresponding polystyrene particles. More recently, Lai et al. applied MPT to quantify the transport of various sized particles in fresh undiluted human cervicovaginal mucus [17].
Figure 4.
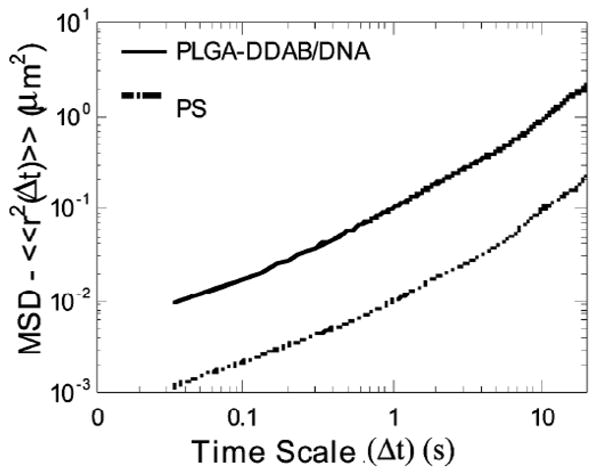
Ensemble-averaged mean square displacement (MSD) as a function of time scale for PLGA-DDAB/DNA and COOH-modified polystyrene nanoparticles in reconstituted pig gastric mucus. Figure obtained from [119].
3.3 In vivo studies of conventional particles in mucus
The fate of particulates in mucosal tissues of living systems has been studied for over a century, with much of the early work focusing on particle uptake into the intestinal epithelia following oral administration. As early as 1907, Basset and Carné suggested that the intestinal epithelium is impermeable to particles [121]. The lack of particle entry into mucosal epithelia has long been attributed to inefficient penetration through the mucus layer. Florey noted that intestinal mucus in cats surrounds particles of India Ink so that they do not come in direct contact with epithelial cells [122]. Arbos et al. observed that poly(methylvinylether-co-maleic anhydride) nanoparticles were not able to reach the enterocytes lining the small intestine and colon in rats and were largely localized within the mucus layer [20]. Gruber concluded that, irrespective of the size, density, or composition of particles, GI mucus in dogs formed them into mucus-covered ‘slugs’ [21]; such particle agglomeration is more recently highlighted by Rubinstein and coworkers in their studies of particles in rat intestines (Figure 5) [123]. Lamprecht et al., in an investigation of particles targeting inflamed colonic mucosa in rats, noted that a large number of the particles were associated to the thick mucus layer rather than attached to or internalized by intestinal cells [22]. O’Mullane et al. stated that “the transport of intact carriers across the gastro-intestinal tract is restricted to exceptional and unusual circumstances” [23]. Even the unusually thin mucus secreted in the tear film wraps particles in a mucus coat, as can be noticed on removing an irritating particle from the eyelid [15].
Figure 5.

Agglomerated non-adhesive particles coated with a mucus plug collected immediately following discharge from the proximal jejunum of the perfused rat (magnification: ×60). Figure obtained from [123].
Many researchers have sought to enhance the mucoadhesion of particles in order to improve their retention at mucosal surfaces. To maximize association with mucus, a variety of mucoadhesive drug delivery systems have been engineered, driven by various interaction forces between mucus and nanoparticles, including hydrogen bonding, van der Waals interactions, polymer chain interpenetration, hydrophobic forces, and electrostatic/ionic interactions [109, 111]. Electrostatic interaction is one of the most exploited forms of mucoadhesion, as exemplified by chitosan, a cationic polymer obtained from deacetylation of chitin, for a variety of oral and nasal drug delivery applications [124, 125]. Jubeh et al. similarly concluded that cationic liposomes adhered to healthy colonic rat mucosa at rates 3-fold greater than neutral or anionic liposomes [126]. Particles synthesized from common biomaterials, such as polyethylene glycol [127–129], polycarbophil and carbopol (derivatives of polyacrylic acid) [111, 130], poly(methacrylates) [131, 132], and poly(sebacic acid) [133, 134] may achieve mucoadhesion via hydrogen bonding, polymer entanglements with mucins, hydrophobic interactions, or a combination of these mechanisms.
The association of the aforementioned biomaterials with mucus is typically considered non-specific, as they lack biological molecules that afford recognition and binding to particular target chemical structures on mucus or surfaces of mucosal epithelia [81, 109]. Alternatively, mucoadhesion can also be achieved via ligands that recognize particular mucin glycoproteins. For example, tomato lectins, which specifically recognize and bind to N-acetyl glucosamine-containing complexes on cell surfaces, were initially tested for specific interactions with intestinal tissues [111]. However, there was little improvement in intestinal transit time of tomato lectin compared to other mucoadhesive systems [135], an observation later justified by the strong association of lectins to mucus gel instead of epithelia [136–138]. Lectins with different sugar specificities have also been investigated, including those derived from Canavalia ensiformis [139] and Lotus tetragonolobus [140]. Readers are referred to excellent reviews for further information on non-specific and specific mucoadhesive materials [109, 111].
Mucoadhesive particles usually improve the pharmacokinetics of therapeutics in the GI tract compared to free drug alone. For example, mucoadhesive polyanhydride copolymers of fumaric and sebacic acids were used to encapsulate insulin and dicumarol (an anticoagulant drug with poor water solubility and erratic intestinal adsorption) and, in both cases, improved the bioavailability of both loaded drugs compared to their native form [133, 134]. Chitosan-based or chitosan-coated nanoparticles represent another common group of mucoadhesive systems [124, 125, 141], and several groups have studied nanoparticles made of these polymers to deliver proteins [142, 143], peptides [144], and DNA [145] to mucosal tissues. In addition to prolonged residence times, improved oral bioavailability of drugs observed in vivo may be partially attributed to improved drug stability in encapsulated form in the GI tract, which is rich in proteolytic enzymes such as pepsin, trypsin, and chymotrypsin [81]. For example, the stability of insulin and calcitonin exposed to protease degradation is significantly improved when loaded in polymeric nanoparticles [12, 146–148].
A range of reports have suggested that nanoparticles are capable of entry into intestinal epithelia via M cells on the domes of the Peyer’s patches in small animals. Not surprisingly, the Peyer’s patches are the intestinal surfaces least protected by mucus and most exposed to the chyme [15]. Since no mucus is secreted in the region surrounding these cells, which protrude relatively unprotected into the lumen, the mucus barrier is minimal [149]. Indeed, M cells are positioned as sensory outposts for cellular immune functions, transcytosing particles that impinge on their surface into the interior of the patch. The dominant opinion is that particulate uptake in GI tract of mammals is principally via the M cells of Peyer’s patches, and that uptake by enterocytes plays a minor role [81, 150]. Polystyrene nanopsheres and microspheres were found in the Peyer’s patches of the rat colon 12 hrs following oral administration [151]. Similarly, Jani et al. found microspheres up to a diameter of 3 μm in Peyer’s patches and in the gut associated lymphoid tissue 12 hrs after oral administration [152]. An ex vivo model using a diffusion chamber with pig intestinal tissue show that radiolabeled polyisobutyl cyanoacrylate nanoparticles (211 nm) cross pig Peyer’s patches, whereas tissue deprived of Peyer’s patches were impermeable to particles [153]. The extent of nanoparticle uptake in rabbits appeared at least an order of magnitude greater than that in mice, a finding attributed to the significantly greater abundance of M cells in rabbit Peyer’s patches [150, 154].
Although the above reports widely support the notion that M cells account for the bulk of particles crossing the intestinal epithelium, M cells occupy a relatively small portion of the total surface area of the GI tract. The potential of drug delivery to the systemic circulation via M cells instead of enterocytes has thus remained debatable. Furthermore, the prospects for using Peyer’s patches as a means of delivering peptides and proteins has been said to be “severely compromised” by: (a) the limited efficiency and capacity of the absorption pathway, (b) the time to onset of pharmacological response, due to both the kinetics of processing the particles and the flow rate of the lymph; and (c) the potential loss of drug to local lymphocytes and macrophages [155]. A number of studies have suggested that uptake of nanoparticles may occur through enterocytes as well as M cells [156–158]; however, as recently pointed out, no satisfying explanation has been advanced to elucidate conflicting reports [159].
A direct consequence of greater uptake into intestinal Peyer’s patches is the application of nanoparticles to enhance oral immunization [160], because the low intestinal permeability and high presystemic clearance of vaccines from the gastrointestinal tract requires the use of prohibitively large and repetitive doses to elicit even a modest immune response [161]. In general, antigens incorporated into particles are more effective for oral immunization than soluble antigens [81, 162]. For example, ovalbumin incorporated into PLGA particles induced potent serum and mucosal immune response, including both IgA and IgG antibodies [163, 164]. Similar results have been achieved with a variety of toxins, including staphylococcal enterotoxin B toxoid [165], tetanus toxoid [166], as well as DNA vaccines [134, 145]. For further details, readers are referred to several excellent reviews on the topic of nanoparticle-mediated oral vaccination [81, 156, 167].
3.4 Shortcomings of mucoadhesive nanoparticles
Although mucoadhesion is a promising approach to increase the bioavailability of drugs delivered via mucosal tissues, important fundamental limitations of this approach exist. Since mucoadhesive systems are bound to the mucus layer through interactions with mucin fibers, the transit time of these systems is determined by the physiological turnover time of the mucus layer [81, 168]. For oral delivery, considering the intestinal mucin turnover time is between 50–270 minutes [82], mucoadhesive particles are not expected to adhere to mucus for more than 4–5 hours. Furthermore, as mucoadhesive systems efficiently adhere to mucus, they are largely incapable of penetrating across the mucus layer and entering the underlying epithelia. Thus, mucoadhesive systems are especially unsuitable for delivery of drug and gene molecules that require intracellular delivery. To overcome these issues, various attempts have been made to engineer particles that adhere specifically to intestinal cells, as exemplified by the conjugation of tomato lectins to nanoparticles. However, these ligand-bound particles appear to have a limited capacity to diffuse through the mucus layer and, instead, undergo premature adsorption to mucus [136–138]. Thus, these systems reach the enterocyte surface inefficiently at best, and are instead bound to mucus, transported through the GI tract, and eliminated in the feces in a similar fashion to other mucoadhesive systems. To overcome this problem and achieve longer residence time of particles at mucosal surfaces, the foremost requirement is to engineer particles that can efficiently cross the mucus barrier (Figure 6).
Figure 6.
Summary schematic illustrating the fate of mucus-penetrating particles (MPP) and conventional mucoadhesive particles (CP) administered to a mucosal surface. MPP readily penetrate the luminal mucus layer (LML) and enter the underlying adherent mucus layer (AML). In contrast, CP are largely immobilized in the LML. Because MPP can enter the AML and thus are in closer proximity to the cells, cells will be exposed to a greater dose of drug released from MPP compared to drug released from CP. As the LML layer is cleared, CP are removed along with the LML whereas MPP in the AML are retained, leading to prolonged residence time for MPP at the mucosal surface. Thus, at long times, there is almost no drug dosing to cells with CP, whereas MPP, because they are retained longer, will continue to release drugs to cells. Since MPP can penetrate both the LML and AML, a fraction may reach and bind to the underlying epithelia and further improve drug delivery. While this schematic reflects the mucosal physiology of the gastrointestinal and cervicovaginal tracts, the same behavior is expected for the respiratory airways. In the respiratory airways, CP are mostly immobilized in the luminal stirred mucus gel layer, whereas MPP penetrate the mucus gel and enter the underlying periciliary layer. Upon mucociliary clearance, a significant fraction of MPP remains in the periciliary layer, resulting in prolonged retention. This schematic does not depict the glycocalyx adjacent to the epithelial surface, which may contribute an additional steric barrier to cellular entry of MPP.
4. Lessons from nature: transport of viruses in mucus
To gain mechanistic insight and rationally engineer particles to cross mucus, we took an alternative approach and looked to nature for guidance. Specifically, we focused on understanding the physicochemical properties (i.e. size and surface chemistry) that govern the rapid transport of specific viruses, which have evolved over thousands of years to infect mucosal tissues.
An indirect implication of the highly immobilized nature of virus-sized polystyrene beads in mucus is that viral particles possess a sufficiently large surface area to undergo polyvalent adhesive interactions with mucus [15]. Nevertheless, many viruses are capable of diffusing in mucus as fast as in water (Figure 7) [19]. This finding by Cone and coworkers motivated us to attempt to develop mucus-penetrating particles (MPP) by mimicking the essential surface properties of viruses that allow them to avoid mucoadhesion. A hypothesis first proposed by Cone and coworkers noted that many viruses, including poliovirus, Norwalk virus and human papilloma virus (HPV), are densely coated with both positively and negatively charged groups, leading to a densely charged yet net neutral surface [15]. Indeed, the average distance between charge groups on the surface of poliovirus is only 5Å. This feature is also found in many soluble proteins [169], including antibodies, such as IgG and IgA, which experience minimal hindrance to diffusion by mucus [19, 86]. We rationalized that the high density of surface charge creates a hydrophilic surface that minimizes hydrophobic entrapment to mucus. Furthermore, an equal density of positive and negative charges may facilitate efficient mucus transport by allowing the viruses to avoid electrostatic adhesive interactions. Some viruses thus appear well designed to penetrate mucus by simultaneously possessing a muco-inert surface to avoid mucoadhesion and a sufficiently small geometry to diffuse through the low viscosity pores in mucus without significant steric obstruction.
Figure 7.
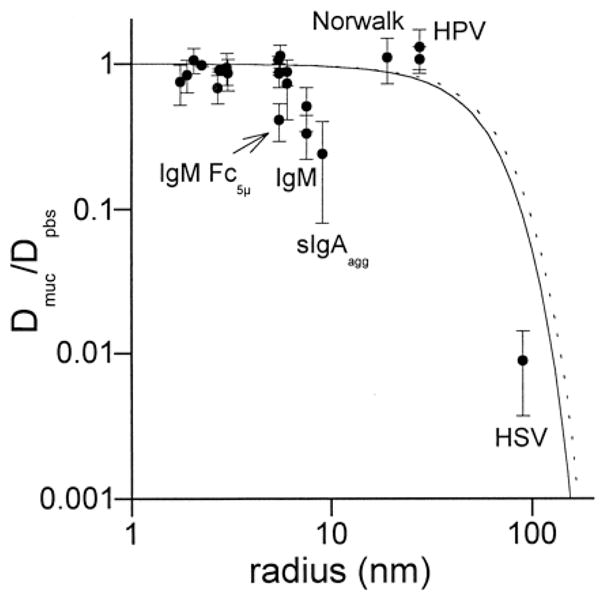
Normalized diffusion coefficients for proteins and viruses in mucus. If a particle diffuses in mucus as fast as it diffuses in saline, Dmuc/Dpbs = 1. The lines drawn on the graph are the ratios predicted by Amsden’s obstruction-scaling model using a mucin fiber radius of 3.5 nm and mesh fiber spacing of 100 nm (solid line) or 110 nm (dotted line), which accounts for a 10% increase in the mesh fiber spacing due to 20% dilution of the mucus sample. Figure obtained from [19].
5. Engineering particles to cross mucus barriers
5.1 Role of surface chemistry
Polystyrene nanoparticles as small as 59 nm, covalently modified with carboxyl groups on the surface, were found to be completely immobilized in human cervical mucus [19]. By reducing the concentrations, Dawson et al. found that some particles with surfaces modified with either carboxyl or amine groups were mobile in CF sputum, but the ensemble-averaged transport rates were still slowed at least 300-fold compared to the same particles in water [118]. Norris et al. similarly observed slow transport of nanoparticles surface-modified with carboxyl, sulfate, or amidine groups, although the fastest transport was found with the most hydrophilic (amidine) surface [90]. In contrast, Sakuma et al. studied the in vivo behavior of nanoparticles having surface poly(N-isopropyl acrylamide), poly(N-vinyl acetamide), poly(vinylamine), or poly(methacrylic acid) chains, and observed increased mucoadhesion for all chains except for poly(N-vinyl acetamide) [170, 171]. The increased mucoadhesion by the various hydrophilic chains was attributed to the presence of tertiary amines which may interact with anionic components of mucus. Thus, no clear correlation existed between the surface chemistry of synthetic nanoparticles and their transport rates in mucus.
5.2 Coating particles with low molecular weight polyethylene glycol
A faithful mimic of the muco-inert viruses would involve developing synthetic particles with a similarly high density of both cationic and anionic surface charge groups. However, although techniques have been advanced to generate multiple alternating layers of oppositely charged coatings with thicknesses on the order of angstroms [172, 173], the engineering of such densely charged yet neutral coatings onto the surfaces of synthetic particles remains exceedingly difficult. Furthermore, even if such chemistry is possible and scalable, densely charged synthetic particles may exhibit immunogenicity similar to viruses. To circumvent the difficult chemistry and immunological concerns, we abstracted the features of the highly charged yet net neutral surfaces of viruses to encompass high hydrophilicity and neutral charge. In particular, instead of a high density of charge groups, we hypothesized an uncharged surface may be as muco-inert as viral capsids, provided the surface is sufficiently hydrophilic and low H-bonding. We thus screened through GRAS (generally regarded as safe) polymers that may satisfy the dual requirements: (i) strong hydrophilicity and (ii) neutrally charged.
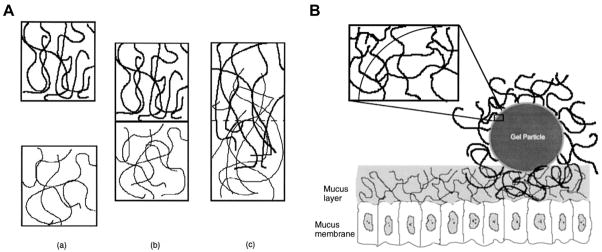
Polyethylene glycol (PEG) is an uncharged hydrophilic polymer routinely used in pharmaceutics to improve systemic circulation and minimize opsonization [4, 174]. However, it was not obvious, a priori, that PEG may reduce association of particles with mucus, since PEG was widely used as a mucoadhesive agent [175, 176]. Some authors have reported that PEG chains may establish adhesive interactions due to their ability to inter-diffuse with the mucus network [128, 175–178] and undergo hydrogen bonding [127]. It should be noted that a large fraction of the early work depicting PEG as mucoadhesive was based on PEG coating of hydrogel systems [179], where the characteristic size of the gel is far greater than the average mucus pore spacing. A number of reports over the past decade have further suggested PEG to enhance the mucoadhesive properties of nanoparticles [177, 180–182], although the density of the PEG coating was typically poorly characterized. In light of these findings, we hypothesized that coating particles with a high density of PEG may reduce particle-mucus adhesive interactions, provided: (i) the M.W. of PEG was too low to support adhesion via polymer interpenetration (Figure 8) and (ii) the PEG density is sufficient to effectively shield the hydrophobic core common to many biodegradable polymers.
Figure 8.
Schematic representation of (A) the interdiffusion of polymers upon contact and (B) the interpenetration between tethered chains on a particle surface and mucin fibers of the mucus gel layer. Figure obtained from [175].
To test our hypothesis, we covalently modified the surfaces of polystyrene nanoparticles with a high density of low M.W. (2 kDa) PEG, and studied their diffusion in fresh undiluted human mucus [17]. Contrary to reports of PEG being mucoadhesive, a dense PEG coating, as characterized by a near-neutral surface charge and negligible protein adsorption, improved the transport of nanoparticles by up to 3 orders of magnitude for particles in the range of 100–500 nm in size (Figure 9). Large nanoparticles (200 and 500 nm in diameter) densely coated with PEG diffused through mucus with an effective diffusion coefficient (Deff) only 6- and 4-fold lower than that for the same particles in water. The greatly improved nanoparticle transport rates upon PEGylation correlated with a sharp decrease in the fraction of immobile particles for all sizes tested; less than 0.5% of 200 and 500 nm PEGylated particles were immobilized by mucus compared to 32 and 45% for uncoated 200 and 500 nm particles, respectively. To our knowledge, this is the first report to demonstrate that synthetically engineered nanoparticles can rapidly penetrate fresh undiluted human mucus barriers.
Figure 9.
Transport of COOH- and PEG-modified polystyrene particles in fresh, human cervicovaginal mucus (CVM). Ensemble-averaged geometric mean square displacements (<MSD>) as a function of time scale for (A) COOH- and (B) PEG-modified polystyrene particles in human CVM. Comparison of average Deff at a time scale of 1 s in water (W) vs. CVM of subfractions of (C) COOH- and (D) PEG-modified particles, from fastest to slowest. Theoretical Deff for same-sized particles in water is shown as W. The dashed black line at <Deff> = 1 × 10−4 signifies the microscope’s resolution. Data represent ensemble average of three experiments, with n ≥ 120 particles for each experiment. Figure obtained from [17].
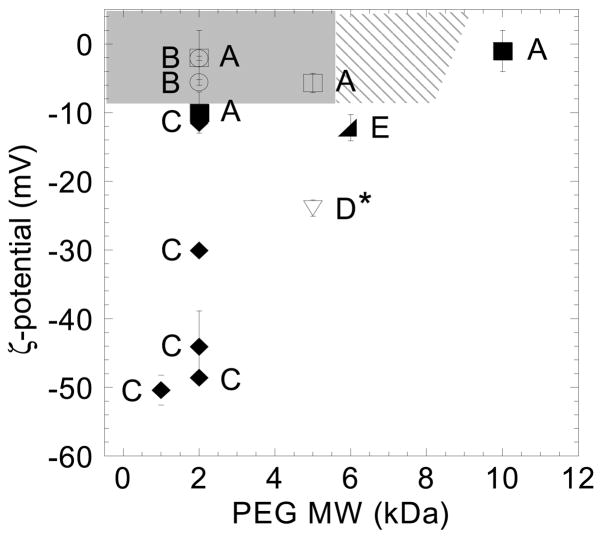
Despite the marked improvement of nanoparticle transport upon PEG modification, a significant fraction of 100 nm PEG-modified particles were found to be immobile or strongly hindered in mucus [17]. One possible explanation for the slower transport of 100 nm (vs. 200 and 500 nm) particles may be inadequate PEGylation of 100 nm particles. To better understand how the density of surface PEG coverage may affect particle transport, and to resolve the paradox between the mucoadhesive properties of PEG widely observed prior to our work and the muco-inert properties of PEG we observed, we recently tested the effect of coating density and PEG M.W. on the transport of PEG-coated particles in mucus [183]. We found that a 40% lower surface coverage of 2 kDa PEG, compared to particles well-coated with 2 kDa PEG, caused a 700-fold decrease in the average transport rate. Particles similarly well-coated with 5 kDa PEG diffused as rapidly through mucus as those with 2 kDa PEG, but a further increase of PEG M.W. to 10 kDa resulted in 1000-fold slower transport. These results suggest that both dense surface coverage and low M.W. PEG are required for PEG-coated particles to rapidly penetrate mucus. Using this design principle, we were able to engineer 100 nm particles that can rapidly penetrate mucus (unpublished observations). By comparing our results to previously published studies of the interaction of PEG-coated particles with mucus, we estimated the range of PEG M.W. and particle surface charge (an indirect measure of PEG surface coverage on non-neutral core particles) that likely provides muco-inert PEG coatings (Figure 10) [183].
Figure 10.
Phase diagram correlating muco-inert versus mucoadhesive particle behavior to surface charge and PEG MW for various PEG-coated nanoparticles (~200–500 nm in size) reported in literature. PEG-coated nanoparticles reported to be non-mucoadhesive compared to control (uncoated) particles are indicated by open symbols, and those reported to be mucoadhesive compared to control particles are indicated by filled symbols. The shaded region represents the confirmed range of PEG MW and particle ξ-potential (i.e., PEG surface coverage), and the hatched region an additional predicted range, that provides a muco-inert coating. Letters represent published results from various studies [17, 183, 232–235]. *Mucoadhesion was not observed based on adhesion to an in vitro mucin-secreting cell line, which is unlikely to produce mucus gels with the complex mesh structure and adhesivity of physiological mucus [234]. Figure obtained from [183].
In addition to improving transport, PEGylation of nanoparticles may also enhance their stability in mucus. Stability is particularly important when particles must diffuse through a thick mucus layer in order to reach underlying cells. Various studies have demonstrated that liposomes are not stable in the GI tract, particularly in the presence of bile salts [184, 185]. Low gene transfer to lung epithelia by lipoplexes administered via intratracheal or intranasal instillation has been attributed to the low stability and substantial aggregation of liposomes in mucus [186]. Upon PEGylation, Sanders et al. found that mucus components did not interact significantly with PEG-GL67 lipoplexes, and prior exposure to the mucus components did not reduce their gene transfer [187, 188]. Similarly, in vitro incubation of PEG-coated polylactide nanoparticles in simulated gastric fluid demonstrated 9-fold higher chemical stability than polylactide particles alone [129].
5.3 Implications of large “mucus penetrating” particles
Much to our surprise, we were able to engineer 200 and 500 nm particles to rapidly traverse fresh human cervicovaginal mucus. This directly implies that the average effective mesh spacing in human cervicovaginal secretions must be significantly larger than earlier reports [17] and must include a large number of pores with effective spacings substantially larger than 500 nm. It is unlikely that the rapid transport of PEGylated particles is due to alterations of the mucus structure, because they do not interact significantly with mucus. Instead, particles likely move in low-viscosity channels or pores within the mucus, as suggested in our earlier work on particle transport in cystic fibrosis mucus [118]. Furthermore, since our results are obtained with fresh, undiluted cervicovaginal mucus that is rheologically and compositionally comparable to mucus found in the airways of the lungs and gastrointestinal tract [15, 17], it is possible that large PEGylated nanoparticles may also transport quickly in mucus coating other entry sites into the body. In cases of less hydrated mucus, diffusion rates of nanoparticles may not differ markedly from those found in fresh cervicovaginal mucus, since the interfiber spacing does not strongly depend on hydration [86].
The rapid mucosal transport of large (200 and 500 nm) PEG-modified particles has important implications for the development of therapeutic and imaging applications in vivo. Larger nanoparticles afford substantially higher drug encapsulation as well as reduced aggregation upon freeze drying. In addition, as the size of drug-loaded particles increases, the drug-release kinetics are usually greatly improved as well, allowing sustained release of therapeutics over days and even months along with enhanced therapeutic efficacy [5, 189, 190]. In contrast, smaller nanoparticles suffer from large burst release typically within hours upon in vitro or in vivo application [191, 192]. These findings should strongly encourage the commercial development of new nanoparticle-based drug delivery systems for applications at mucosal surfaces.
Although large nanoparticles are preferred for improved drug loading and release kinetics, an optimal size likely exists for mucosal applications. Nanoparticles that are too large, even if they are well-coated so as to avoid mucoadhesion, may not diffuse at rates sufficient for overcoming mucociliary clearance due to the elevated friction forces predicted by the Stokes-Einstein equation. Since mucus layer thickness and mucus clearance time differ among the mucosal tissues, different nanoparticle diffusion rates may be required in order to overcome different mucus barriers. Furthermore, for cellular uptake into underlying epithelia, an increase in particle diameter is expected to reduce the rate of endocytosis [10, 193]. The size of MPP must be optimized with all of these considerations in mind, and will likely vary based on the requirements of different mucosal applications.
5.4. Disrupting the mucus barrier to enhance particle transport
Treatment of mucus with mucolytics agents [47] may improve the penetration rates of drug and gene carrier particles. The use of mucolytics as an adjuvant to particle transport may be particularly important for diseases where mucus is abnormally viscoelastic, such as cystic fibrosis and chronic obstruction pulmonary disease (COPD). For example, in CF sputum, water content is reduced and cellular debris is increased, leading to an increase in physical entanglements, a decrease in the average mesh pore spacing, and a pronounced increase in the viscoelastic nature of the sputum [194, 195]. Consequently, CF mucus is suggested to be a confounding barrier even to viruses [196], as well as a major cause for low gene transfer efficiencies in vivo [89, 197].
Pulmozyme®, a recombinant human DNase (rhDNase) also known as Dornase alfa, is the most commonly used mucolytic in CF and a potential candidate as an adjuvant to particle transport. Pulmozyme hydrolyzes the DNA that forms dense entanglements with mucin glycoproteins and other mucus constituents, thus reducing the number of crosslinks and the viscoelasticity of mucus [198, 199]. However, in a diffusion chamber study, Sanders et al. found only a moderate improvement in the transport of uncoated polystyrene nanospheres through CF sputum treated with rhDNase [112]. Dawson et al. observed that, while rhDNase treatment of undiluted CF sputum reduced its macroviscoelastic properties by up to 50%, it did not improve particle diffusion rates [118]. Multiple particle tracking analysis revealed that rhDNase treatment dramatically narrowed the distribution of individual particle diffusion rates in CF sputum, effectively removing the fast-moving “outlier” particle population. Dawson et al. suggested that soluble DNA fragments created by DNase treatment may increase the microviscosity within mucus pores, thereby eliminated fast-moving particles. This finding suggests that rhDNase may reduce, rather than enhance, the efficacy of nanoparticle therapeutics such as non-viral polymeric gene vectors, since the treatment eliminates the fast-moving fraction that may be critical for effective CF gene therapy [118].
Mucinex® (N-acetyl-L-cysteine; NAC) is another common mucolytic previously tested for its ability to improve the penetration of nanoparticles across CF sputum. NAC reduces the cross-linking of mucin fibers by cleaving disulfide bonds and thus the bulk mucus rheology [200, 201]. Alton and coworkers showed that the mucus barrier to non-viral gene vectors may be at least partially overcome by treatment with NAC in an ex vivo model of sheep tracheal epithelium [202]. NAC treatment has also been shown to increase reporter gene expression in the mouse lung; however, no correction of the nasal transepithelial potential difference was observed in CF-null mice, suggesting NAC alone may be inadequate to induce clinically relevant gene therapy via mucoadhesive cationic liposomes and polymers.
Although not widely investigated, other promising mucolytic agents are well established for reducing the bulk rheological properties of mucus and may potentially improve nanoparticle transport through mucus. These include Nacystelyn [203, 204], as well as Gelsolin [205] and thymosin β4 [206], agents that depolymerize F-actin. The varying effects of mucolytics, as in the cases of NAC and rhDNase, suggest that any potential adjuvant use of mucolytics must be carefully investigated for each agent. Furthermore, patients may respond differently to various mucolytics. A more thorough understanding of failures in mucolytic response in different patients may alleviate these concerns [207].
6. Conclusions
The possibility of using polymer nanoparticles for controlled drug or gene delivery at mucosal sites over many hours to days is expected to lead to effective new therapeutics. However, no such product currently exists since conventional therapeutic particles cannot penetrate the human mucosal barrier, which rapidly clears trapped pathogens and particulates. The development of mucus-penetrating particles (MPP), by rendering the surfaces of particles non-mucoadhesive via lessons learned from viruses, provides a powerful strategy for overcoming the mucus barrier. In particular, the efficient transport of large MPP (200 to 500 nm) through human mucus should strongly encourage the commercial development of new nanoparticle-based drug delivery systems for use in various mucosal surfaces, since drug delivery kinetics and loading efficiency are vastly improved as particle diameter increases. As such, MPP offers the prospect of sustained delivery of a variety of potentially important drugs to treat diseases at mucosal tissues.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rosen H, Abribat T. The rise and rise of drug delivery. Nat Rev Drug Discov. 2005;4:381–5. doi: 10.1038/nrd1721. [DOI] [PubMed] [Google Scholar]
- 2.Shmulewitz A, Langer R, Patton J. Convergence in biomedical technology. Nat Biotech. 2006;24:277–277. [Google Scholar]
- 3.Duncan R. The dawning era of polymer therapeutics. Nat Rev Drug Discov. 2003;2:347–60. doi: 10.1038/nrd1088. [DOI] [PubMed] [Google Scholar]
- 4.Allen TM, Cullis PR. Drug delivery systems: entering the mainstream. Science. 2004;303:1818–22. doi: 10.1126/science.1095833. [DOI] [PubMed] [Google Scholar]
- 5.Langer R. Drug delivery and targeting. Nature. 1998;392:5–10. [PubMed] [Google Scholar]
- 6.Farokhzad OC, Langer R. Nanomedicine: Developing smarter therapeutic and diagnostic modalities. Adv Drug Deliv Rev. 2006;58:1456–1459. doi: 10.1016/j.addr.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 7.Prego C, Garcia M, Torres D, Alonso MJ. Transmucosal macromolecular drug delivery. J Control Release. 2005;101:151–62. doi: 10.1016/j.jconrel.2004.07.030. [DOI] [PubMed] [Google Scholar]
- 8.Yuan F, Leunig M, Huang SK, Berk DA, Papahadjopoulos D, Jain RK. Mirovascular Permeability and Interstitial Penetration of Sterically Stabilized (Stealth) Liposomes in a Human Tumor Xenograft. Cancer Res. 1994;54:3352–3356. [PubMed] [Google Scholar]
- 9.MacKay JA, Deen DF, Szoka JFC. Distribution in brain of liposomes after convection enhanced delivery; modulation by particle charge, particle diameter, and presence of steric coating. Brain Res. 2005;1035:139–153. doi: 10.1016/j.brainres.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 10.Lai SK, Hida K, Man ST, Chen C, Machamer C, Schroer TA, Hanes J. Privileged delivery of polymer nanoparticles to the perinuclear region of live cells via a non-clathrin, non-degradative pathway. Biomaterials. 2007 doi: 10.1016/j.biomaterials.2007.02.021. [DOI] [PubMed] [Google Scholar]
- 11.Medina-Kauwe LK, Xie J, Hamm-Alvarez S. Intracellular trafficking of nonviral vectors. Gene Ther. 2005;12:1734–1751. doi: 10.1038/sj.gt.3302592. [DOI] [PubMed] [Google Scholar]
- 12.Allemann E, Leroux JC, Gurny R. Polymeric nano- and microparticles for the oral delivery of peptides and peptidomimetics. Adv Drug Deliv Rev. 1998;34:171–189. doi: 10.1016/s0169-409x(98)00039-8. [DOI] [PubMed] [Google Scholar]
- 13.Panyam J, Labhasetwar V. Biodegradable nanoparticles for drug and gene delivery to cells and tissue. Adv Drug Deliv Rev. 2003;55:329–47. doi: 10.1016/s0169-409x(02)00228-4. [DOI] [PubMed] [Google Scholar]
- 14.Knowles MR, Boucher RC. Mucus clearance as a primary innate defense mechanism for mammalian airways. J Clin Invest. 2002;109:571–7. doi: 10.1172/JCI15217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cone R. Mucus. In: Michael WS, Lamm E, McGhee Jerry R, Mayer Lloyd, Mestecky Jiri, Bienenstock John, editors. Mucosal Immunlogy. Academic Press; San Diego: 1999. pp. 43–64. [Google Scholar]
- 16.Cone R. Barrier Properties of Mucus. Adv Drug Deliv Rev. 2008 doi: 10.1016/j.addr.2008.09.008. Accepted. [DOI] [PubMed] [Google Scholar]
- 17.Lai SK, O’Hanlon DE, Harrold S, Man ST, Wang YY, Cone R, Hanes J. Rapid transport of large polymeric nanoparticles in fresh undiluted human mucus. Proc Natl Acad Sci U S A. 2007;104:1482–7. doi: 10.1073/pnas.0608611104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Braeckmans K, Peeters L, Sanders NN, De Smedt SC, Demeester J. Three-dimensional fluorescence recovery after photobleaching with the confocal scanning laser microscope. Biophys J. 2003;85:2240–52. doi: 10.1016/s0006-3495(03)74649-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Olmsted SS, Padgett JL, Yudin AI, Whaley KJ, Moench TR, Cone RA. Diffusion of macromolecules and virus-like particles in human cervical mucus. Biophys J. 2001;81:1930–1937. doi: 10.1016/S0006-3495(01)75844-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arbos P, Campanero MA, Arangoa MA, Renedo MJ, Irache JM. Influence of the surface characteristics of PVM/MA nanoparticles on their bioadhesive properties. J Controlled Release. 2003;89:19–30. doi: 10.1016/s0168-3659(03)00066-x. [DOI] [PubMed] [Google Scholar]
- 21.Gruber P, Longer MA, Robinson JR. Some biological issues in oral, controlled drug delivery. Adv Drug Deliv Rev. 1987;1:1–18. [Google Scholar]
- 22.Lamprecht A, Schafer U, Lehr CM. Size-dependent bioadhesion of micro- and nanoparticulate carriers to the inflamed colonic mucosa. Pharm Res. 2001;18:788–93. doi: 10.1023/a:1011032328064. [DOI] [PubMed] [Google Scholar]
- 23.O’Mullane JE, Artursson P, Tomlinson E. Biopharmaceutics of microparticulate drug carriers. Ann N Y Acad Sci. 1987;507:120–40. doi: 10.1111/j.1749-6632.1987.tb45796.x. [DOI] [PubMed] [Google Scholar]
- 24.Griesenbach U, Alton E. Gene Transfer to the Lung: Lessons Learned from More Than Two Decades of CF Gene Therapy. Adv Drug Deliv Rev. 2008 doi: 10.1016/j.addr.2008.09.010. Accepted. [DOI] [PubMed] [Google Scholar]
- 25.Sanders N, Rudolph C, Braeckmans K, De Smedt S, Demeester J. Extracellular Barriers in Respiratory Gene Therapy. Adv Drug Deliv Rev. 2008 doi: 10.1016/j.addr.2008.09.011. Accepted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carlstedt I, Sheehan JK. Structure and macromolecular properties of cervical mucus glycoproteins. Symp Soc Exp Biol. 1989;43:289–316. [PubMed] [Google Scholar]
- 27.Thornton DJ, Sheehan JK. From mucins to mucus: toward a more coherent understanding of this essential barrier. Proc Am Thorac Soc. 2004;1:54–61. doi: 10.1513/pats.2306016. [DOI] [PubMed] [Google Scholar]
- 28.Wickstrom C, Davies JR, Eriksen GV, Veerman EC, Carlstedt I. MUC5B is a major gel-forming, oligomeric mucin from human salivary gland, respiratory tract and endocervix: identification of glycoforms and C-terminal cleavage. Biochem J. 1998;334(Pt 3):685–93. doi: 10.1042/bj3340685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sheehan JK, Carlstedt I. Hydrodynamic properties of human cervical-mucus glycoproteins in 6M-guanidinium chloride. Biochem J. 1984;217:93–101. doi: 10.1042/bj2170093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thornton DJ, Holmes DF, Sheehan JK, Carlstedt I. Quantitation of mucus glycoproteins blotted onto nitrocellulose membranes. Anal Biochem. 1989;182:160–4. doi: 10.1016/0003-2697(89)90735-5. [DOI] [PubMed] [Google Scholar]
- 31.Dekker J, Rossen JWA, Buller HA, Einerhand AWC. The MUC family: an obituary. Trends Biochem Sci. 2002;27:126–131. doi: 10.1016/s0968-0004(01)02052-7. [DOI] [PubMed] [Google Scholar]
- 32.Ali MS, Pearson JP. Upper airway mucin gene expression: a review. Laryngoscope. 2007;117:932–8. doi: 10.1097/MLG.0b013e3180383651. [DOI] [PubMed] [Google Scholar]
- 33.Rubin BK. Physiology of airway mucus clearance. Respir Care. 2002;47:761–8. [PubMed] [Google Scholar]
- 34.Corfield AP, Carroll D, Myerscough N, Probert CS. Mucins in the gastrointestinal tract in health and disease. Front Biosci. 2001;6:D1321–57. doi: 10.2741/corfield. [DOI] [PubMed] [Google Scholar]
- 35.Gipson IK. Mucins of the human endocervix. Front Biosci. 2001;6:D1245–55. doi: 10.2741/gipson. [DOI] [PubMed] [Google Scholar]
- 36.Thornton DJ, Carlstedt I, Howard M, Devine PL, Price MR, Sheehan JK. Respiratory mucins: identification of core proteins and glycoforms. Biochem J. 1996;316(Pt 3):967–75. doi: 10.1042/bj3160967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Van Klinken BJ, Dekker J, Buller HA, Einerhand AW. Mucin gene structure and expression: protection vs. adhesion. Am J Physiol. 1995;269:G613–27. doi: 10.1152/ajpgi.1995.269.5.G613. [DOI] [PubMed] [Google Scholar]
- 38.Slayter HS, Wold JK, Midtvedt T. Intestinal mucin of germ-free rats. Biochemical and electron-microscopic characterization. Carbohydr Res. 1991;222:1–9. doi: 10.1016/0008-6215(91)89001-v. [DOI] [PubMed] [Google Scholar]
- 39.Yurewicz EC, Matsuura F, Moghissi KS. Structural studies of sialylated oligosaccharides of human midcycle cervical mucin. J Biol Chem. 1987;262:4733–9. [PubMed] [Google Scholar]
- 40.Allen A, Flemstrom G, Garner A, Kivilaakso E. Gastroduodenal mucosal protection. Physiol Rev. 1993;73:823–857. doi: 10.1152/physrev.1993.73.4.823. [DOI] [PubMed] [Google Scholar]
- 41.Carlstedt I, Lindgren H, Sheehan JK, Ulmsten U, Wingerup L. Isolation and characterization of human cervical-mucus glycoproteins. Biochem J. 1983;211:13–22. doi: 10.1042/bj2110013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chao CCW, Butala SM, Herp A. Studies on the isolation and composition of human ocular mucin. Exp Eye Res. 1988;47:185–196. doi: 10.1016/0014-4835(88)90002-4. [DOI] [PubMed] [Google Scholar]
- 43.Quraishi MS, Jones NS, Mason J. The rheology of nasal mucus: a review. Clin Otolaryngol. 1998;23:403–413. doi: 10.1046/j.1365-2273.1998.00172.x. [DOI] [PubMed] [Google Scholar]
- 44.Samet JM, Cheng PW. The Role of Airway Mucus in Pulmonary Toxicology. Environ Health Perspect. 1994;102:89–103. doi: 10.1289/ehp.9410289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chao CCW, Vergnes JP, Brown SI. Fractionation and partial characterization of macromolecular components from human ocular mucus. Exp Eye Res. 1983;36:139–150. doi: 10.1016/0014-4835(83)90097-0. [DOI] [PubMed] [Google Scholar]
- 46.Engel E, Guth PH, Nishizaki Y, Kaunitz JD. Barrier function of the gastric mucus gel. Am J Physiol Gastrointest Liver Physiol. 1995;269:G994–999. doi: 10.1152/ajpgi.1995.269.6.G994. [DOI] [PubMed] [Google Scholar]
- 47.Lai SK, Wang YY, Wirtz D, Hanes J. Microrheology and Macrorheology of Mucus: Implications for Drug and Gene Delivery to Mucosal Tissues. Adv Drug Deliv Rev. 2008 Accepted. [Google Scholar]
- 48.Wolf DP, Blasco L, Khan MA, Litt M. Human cervical mucus. I. Rheologic characteristics. Fertil Steril. 1977;28:41–46. [PubMed] [Google Scholar]
- 49.Galabert C, Jacquot J, Zahm JM, Puchelle E. Relationships between the lipid content and the rheological properties of airway secretions in cystic fibrosis. Clin Chim Acta. 1987;164:139–149. doi: 10.1016/0009-8981(87)90065-9. [DOI] [PubMed] [Google Scholar]
- 50.Girod S, Zahm JM, Plotkowski C, Beck G, Puchelle E. Role of the physiochemical properties of mucus in the protection of the respiratory epithelium. Eur Res J. 1992;5:477–487. [PubMed] [Google Scholar]
- 51.Raynal BD, Hardingham TE, Sheehan JK, Thornton DJ. Calcium-dependent protein interactions in MUC5B provide reversible cross-links in salivary mucus. J Biol Chem. 2003;278:28703–28710. doi: 10.1074/jbc.M304632200. [DOI] [PubMed] [Google Scholar]
- 52.Bhaskar KR, Garik P, Turner BS, Bradley JD, Bansil R, Stanley HE, LaMont JT. Viscous fingering of HCI through gastric mucin. Nature. 1992;360:458–461. doi: 10.1038/360458a0. [DOI] [PubMed] [Google Scholar]
- 53.Celli JP, Turner BS, Afdhal NH, Ewoldt RH, McKinley GH, Bansil R, Erramilli S. Rheology of gastric mucin exhibits a pH-dependent sol-gel transition. Biomacromolecules. 2007;8:1580–6. doi: 10.1021/bm0609691. [DOI] [PubMed] [Google Scholar]
- 54.Hehar SS, Mason JD, Stephen AB, Washington N, Jones NS, Jackson SJ, Bush D. Twenty-four hour ambulatory nasal pH monitoring. Clin Otolaryngol Allied Sci. 1999;24:24–5. doi: 10.1046/j.1365-2273.1999.00190.x. [DOI] [PubMed] [Google Scholar]
- 55.Jayaraman S, Joo NS, Reitz B, Wine JJ, Verkman AS. Submucosal gland secretions in airways from cystic fibrosis patients have normal [Na(+)] and pH but elevated viscosity. Proc Natl Acad Sci U S A. 2001;98:8119–23. doi: 10.1073/pnas.131087598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Greaves JL, Wilson CG. Treatment of diseases of the eye with mucoadhesive delivery systems. Adv Drug Deliv Rev. 1993;11:349–383. [Google Scholar]
- 57.Schreiber S, Scheid P. Gastric mucus of the guinea pig: proton carrier and diffusion barrier. Am J Physiol. 1997;272:G63–70. doi: 10.1152/ajpgi.1997.272.1.G63. [DOI] [PubMed] [Google Scholar]
- 58.Boskey ER, Cone RA, Whaley KJ, Moench TR. Origins of vaginal acidity: high D/L lactate ratio is consistent with bacteria being the primary source. Hum Reprod. 2001;16:1809–13. doi: 10.1093/humrep/16.9.1809. [DOI] [PubMed] [Google Scholar]
- 59.Valenta C. The use of mucoadhesive polymers in vaginal delivery. Adv Drug Deliv Rev. 2005;57:1692–1712. doi: 10.1016/j.addr.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 60.Sleigh MA, Blake JR, Liron N. The propulsion of mucus by cilia. Am Rev Respir Dis. 1988;137:726–41. doi: 10.1164/ajrccm/137.3.726. [DOI] [PubMed] [Google Scholar]
- 61.Widdicombe J. Airway surface liquid: concepts and measurements. In: Lethem DRaM., editor. Airway mucus: basic mechanisms and clinical perspectives. Birkhauser; 1997. pp. 1–18. [Google Scholar]
- 62.Ally J, Ally J, Amirfazli A, Roa W. Model studies of magnetic particle retention in the conducting airways. Proceedings of the 2005 International Conference on MEMS, NANO and Smart Systems; 2005. [Google Scholar]
- 63.Overton J, Miller F. Dosimetry Modeling of Inhaled Toxic Reactive Gases. In: Watson RBA, Kennedy D, editors. Air Pollution, the Automobile, and Public Health. The National Academies Press; 1988. [PubMed] [Google Scholar]
- 64.Clunes MT, Boucher RC. Cystic Fibrosis: The Mechanisms of Pathogenesis of an Inherited Lung Disorder. Drug Discov Today Dis Mech. 2007;4:63–72. doi: 10.1016/j.ddmec.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Matsui H, Grubb BR, Tarran R, Randell SH, Gatzy JT, Davis CW, Boucher RC. Evidence for periciliary liquid layer depletion, not abnormal ion composition, in the pathogenesis of cystic fibrosis airways disease. Cell. 1998;95:1005–15. doi: 10.1016/s0092-8674(00)81724-9. [DOI] [PubMed] [Google Scholar]
- 66.Tarran R, Grubb BR, Gatzy JT, Davis CW, Boucher RC. The relative roles of passive surface forces and active ion transport in the modulation of airway surface liquid volume and composition. J Gen Physiol. 2001;118:223–36. doi: 10.1085/jgp.118.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Verkman AS, Song Y, Thiagarajah JR. Role of airway surface liquid and submucosal glands in cystic fibrosis lung disease. Am J Physiol Cell Physiol. 2003;284:C2–15. doi: 10.1152/ajpcell.00417.2002. [DOI] [PubMed] [Google Scholar]
- 68.Behrens I, Stenberg P, Artursson P, Kissel T. Transport of lipophilic drug molecules in a new mucus-secreting cell culture model based on HT29-MTX cells. Pharm Res. 2001;18:1138–45. doi: 10.1023/a:1010974909998. [DOI] [PubMed] [Google Scholar]
- 69.Copeman M, Matuz J, Leonard AJ, Pearson JP, Dettmar PW, Allen A. The gastroduodenal mucus barrier and its role in protection against luminal pepsins: the effect of 16,16 dimethyl prostaglandin E2, carbopol-polyacrylate, sucralfate and bismuth subsalicylate. J Gastroenterol Hepatol. 1994;9(Suppl 1):S55–9. doi: 10.1111/j.1440-1746.1994.tb01303.x. [DOI] [PubMed] [Google Scholar]
- 70.Jordan N, Newton J, Pearson J, Allen A. A novel method for the visualization of the in situ mucus layer in rat and man. Clin Sci. 1998;95:97–106. [PubMed] [Google Scholar]
- 71.Kerss S, Allen A, Garner A. A simple method for measuring thickness of the mucus gel layer adherent to rat, frog and human gastric mucosa: influence of feeding, prostaglandin, N-acetylcysteine and other agents. Clin Sci. 1982;63:187–95. doi: 10.1042/cs0630187. [DOI] [PubMed] [Google Scholar]
- 72.Matsuo K, Ota H, Akamatsu T, Sugiyama A, Katsuyama T. Histochemistry of the surface mucous gel layer of the human colon. Gut. 1997;40:782–9. doi: 10.1136/gut.40.6.782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pullan RD, Thomas GA, Rhodes M, Newcombe RG, Williams GT, Allen A, Rhodes J. Thickness of adherent mucus gel on colonic mucosa in humans and its relevance to colitis. Gut. 1994;35:353–9. doi: 10.1136/gut.35.3.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.van der Waaij LA, Harmsen HJ, Madjipour M, Kroese FG, Zwiers M, van Dullemen HM, de Boer NK, Welling GW, Jansen PL. Bacterial population analysis of human colon and terminal ileum biopsies with 16S rRNA-based fluorescent probes: commensal bacteria live in suspension and have no direct contact with epithelial cells. Inflamm Bowel Dis. 2005;11:865–71. doi: 10.1097/01.mib.0000179212.80778.d3. [DOI] [PubMed] [Google Scholar]
- 75.Brownlee IA, Havler ME, Dettmar PW, Allen A, Pearson JP. Colonic mucus: secretion and turnover in relation to dietary fibre intake. Proc Nutr Soc. 2003;62:245–9. doi: 10.1079/pns2003206. [DOI] [PubMed] [Google Scholar]
- 76.Holly FJ, Lemp MA. Tear physiology and dry eyes. Surv Ophthalmol. 1977;22:69–87. doi: 10.1016/0039-6257(77)90087-x. [DOI] [PubMed] [Google Scholar]
- 77.King-Smith PE, Fink BA, Hill RM, Koelling KW, Tiffany JM. The thickness of the tear film. Curr Eye Res. 2004;29:357–68. doi: 10.1080/02713680490516099. [DOI] [PubMed] [Google Scholar]
- 78.Prydal JI, Artal P, Woon H, Campbell FW. Study of human precorneal tear film thickness and structure using laser interferometry. Invest Ophthalmol Vis Sci. 1992;33:2006–11. [PubMed] [Google Scholar]
- 79.Mainardes RM, Urban MC, Cinto PO, Chaud MV, Evangelista RC, Gremiao MP. Liposomes and micro/nanoparticles as colloidal carriers for nasal drug delivery. Curr Drug Deliv. 2006;3:275–85. doi: 10.2174/156720106777731019. [DOI] [PubMed] [Google Scholar]
- 80.Saketkhoo K, Januszkiewicz A, Sackner MA. Effects of drinking hot water, cold water, and chicken soup on nasal mucus velocity and nasal airflow resistance. Chest. 1978;74:408–10. doi: 10.1378/chest.74.4.408. [DOI] [PubMed] [Google Scholar]
- 81.Galindo-Rodriguez SA, Allemann E, Fessi H, Doelker E. Polymeric nanoparticles for oral delivery of drugs and vaccines: a critical evaluation of in vivo studies. Crit Rev Ther Drug Carrier Syst. 2005;22:419–64. doi: 10.1615/critrevtherdrugcarriersyst.v22.i5.10. [DOI] [PubMed] [Google Scholar]
- 82.Lehr CM, Poelma FGJ, Junginger HE, Tukker JJ. An Estimate of Turnover Time of Intestinal Mucus Gel Layer in the Rat Insitu Loop. Int J Pharm. 1991;70:235–240. [Google Scholar]
- 83.Kieweg SL, Geonnotti AR, Katz DF. Gravity-induced coating flows of vaginal gel formulations: in vitro experimental analysis. J Pharm Sci. 2004;93:2941–52. doi: 10.1002/jps.20194. [DOI] [PubMed] [Google Scholar]
- 84.Kieweg SL, Katz DF. Squeezing flows of vaginal gel formulations relevant to microbicide drug delivery. J Biomech Eng. 2006;128:540–53. doi: 10.1115/1.2206198. [DOI] [PubMed] [Google Scholar]
- 85.Lamont JT. Mucus: the front line of intestinal mucosal defense. Ann N Y Acad Sci. 1992;664:190–201. doi: 10.1111/j.1749-6632.1992.tb39760.x. [DOI] [PubMed] [Google Scholar]
- 86.Saltzman WM, Radomsky ML, Whaley KJ, Cone RA. Antibody Diffusion in Human Cervical-Mucus. Biophys J. 1994;66:508–515. doi: 10.1016/s0006-3495(94)80802-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Amsden B. Solute diffusion within hydrogels. Mechanisms and models. Macromolecules. 1998;31:8382–8395. [Google Scholar]
- 88.Amsden B. An obstruction-scaling model for diffusion in homogeneous hydrogels. Macromolecules. 1999;32:874–879. [Google Scholar]
- 89.Hanes J, Dawson M, Har-el Y, Suh J, Fiegel J. In: Gene Delivery to the Lung, Pharmaceutical Inhalation Aerosol Technology. Hickey AJ, editor. Marcel Dekker Inc.; New York: 2003. pp. 489–539. [Google Scholar]
- 90.Norris DA, Sinko PJ. Effect of size, surface charge, and hydrophobicity on the translocation of polystyrene microspheres through gastrointestinal mucin. J App Polym Sci. 1997;63:1481–1492. [Google Scholar]
- 91.Sheehan JK, Oates K, Carlstedt I. Electron microscopy of cervical, gastric and bronchial mucus glycoproteins. Biochem J. 1986;239:147–53. doi: 10.1042/bj2390147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Drumm B, Neumann AW, Policova Z, Sherman PM. Bacterial cell surface hydrophobicity properties in the mediation of in vitro adhesion by the rabbit enteric pathogen Escherichia coli strain RDEC-1. J Clin Invest. 1989;84:1588–94. doi: 10.1172/JCI114336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sajjan U, Reisman J, Doig P, Irvin RT, Forstner G, Forstner J. Binding of nonmucoid Pseudomonas aeruginosa to normal human intestinal mucin and respiratory mucin from patients with cystic fibrosis. J Clin Invest. 1992;89:657–65. doi: 10.1172/JCI115632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mantle M, Basaraba L, Peacock SC, Gall DG. Binding of Yersinia enterocolitica to rabbit intestinal brush border membranes, mucus, and mucin. Infect Immun. 1989;57:3292–9. doi: 10.1128/iai.57.11.3292-3299.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bala I, Hariharan S, Kumar MN. PLGA nanoparticles in drug delivery: the state of the art. Crit Rev Ther Drug Carrier Syst. 2004;21:387–422. doi: 10.1615/critrevtherdrugcarriersyst.v21.i5.20. [DOI] [PubMed] [Google Scholar]
- 96.Kumar N, Langer RS, Domb AJ. Polyanhydrides: an overview. Adv Drug Deliv Rev. 2002;54:889–910. doi: 10.1016/s0169-409x(02)00050-9. [DOI] [PubMed] [Google Scholar]
- 97.Pack DW, Hoffman AS, Pun S, Stayton PS. Design and development of polymers for gene delivery. Nat Rev Drug Discov. 2005;4:581–93. doi: 10.1038/nrd1775. [DOI] [PubMed] [Google Scholar]
- 98.Kircheis RLW, Wagner E. Design and gene delivery activity of modified polyethylenimines. Adv Drug Deliv Rev. 2001;53:341–58. doi: 10.1016/s0169-409x(01)00202-2. [DOI] [PubMed] [Google Scholar]
- 99.Durrer C, Irache JM, Puisieux F, Duchene D, Ponchel G. Mucoadhesion of latexes. II. Adsorption isotherms and desorption studies. Pharm Res. 1994;11:680–3. doi: 10.1023/a:1018920128007. [DOI] [PubMed] [Google Scholar]
- 100.Durrer C, Irache JM, Puisieux F, Duchene D, Ponchel G. Mucoadhesion of latexes. I. Analytical methods and kinetic studies. Pharm Res. 1994;11:674–9. doi: 10.1023/a:1018968011169. [DOI] [PubMed] [Google Scholar]
- 101.Ponchel G, Montisci MJ, Dembri A, Durrer C, Duchene D. Mucoadhesion of colloidal particulate systems in the gastro-intestinal tract. Eur J Pharmaceut Biopharmaceut. 1997;44:25–31. [Google Scholar]
- 102.Larhed AW, Artursson P, Grasjo J, Bjork E. Diffusion of drugs in native and purified gastrointestinal mucus. J Pharm Sci. 1997;86:660–5. doi: 10.1021/js960503w. [DOI] [PubMed] [Google Scholar]
- 103.Matthes I, Nimmerfall F, Vonderscher J, Sucker H. Mucus models for investigation of intestinal absorption mechanisms. 4. Comparison of mucus models with absorption models in vivo and in situ for prediction of intestinal drug absorption. Pharmazie. 1992;47:787–91. [PubMed] [Google Scholar]
- 104.Khanvilkar K, Donovan MD, Flanagan DR. Drug transfer through mucus. Adv Drug Deliv Rev. 2001;48:173–93. doi: 10.1016/s0169-409x(01)00115-6. [DOI] [PubMed] [Google Scholar]
- 105.Saitoh H, Hasegawa N, Kawai S, Miyazaki K, Arita T. Interaction of tertiary amines and quaternary ammonium compounds with gastrointestinal mucin. J Pharmacobiodyn. 1986;9:1008–14. doi: 10.1248/bpb1978.9.1008. [DOI] [PubMed] [Google Scholar]
- 106.Desai MA, Mutlu M, Vadgama P. A study of macromolecular diffusion through native porcine mucus. Experientia. 1992;48:22–6. doi: 10.1007/BF01923598. [DOI] [PubMed] [Google Scholar]
- 107.Bhat PG, Flanagan DR, Donovan MD. The limiting role of mucus in drug absorption: Drug permeation through mucus solution. Int J Pharm. 1995;126:179–187. [Google Scholar]
- 108.Bhat PG, Flanagan DR, Donovan MD. Drug diffusion through cystic fibrotic mucus: steady-state permeation, rheologic properties, and glycoprotein morphology. J Pharm Sci. 1996;85:624–30. doi: 10.1021/js950381s. [DOI] [PubMed] [Google Scholar]
- 109.Ponchel G, Irache J. Specific and non-specific bioadhesive particulate systems for oral delivery to the gastrointestinal tract. Adv Drug Deliv Rev. 1998;34:191–219. doi: 10.1016/s0169-409x(98)00040-4. [DOI] [PubMed] [Google Scholar]
- 110.Kreuter J, Muller U, Munz K. Quantitative and microautoradiographic study on mouse intestinal distribution of polycyanoacrylate nanoparticles. Int J Pharm. 1989;55:39–45. [Google Scholar]
- 111.Woodley J. Bioadhesion: new possibilities for drug administration? Clin Pharmacokinet. 2001;40:77–84. doi: 10.2165/00003088-200140020-00001. [DOI] [PubMed] [Google Scholar]
- 112.Sanders NN, De Smedt SC, Van Rompaey E, Simoens P, De Baets F, Demeester J. Cystic fibrosis sputum: a barrier to the transport of nanospheres. Am J Respir Crit Care Med. 2000;162:1905–11. doi: 10.1164/ajrccm.162.5.9909009. [DOI] [PubMed] [Google Scholar]
- 113.Broughton-Head VJ, Smith JR, Shur J, Shute JK. Actin limits enhancement of nanoparticle diffusion through cystic fibrosis sputum by mucolytics. Pulm Pharmacol Ther. 2006 doi: 10.1016/j.pupt.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 114.Shen H, Hu Y, Saltzman WM. DNA diffusion in mucus: effect of size, topology of DNAs, and transfection reagents. Biophys J. 2006;91:639–44. doi: 10.1529/biophysj.105.077404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Suh J, Dawson M, Hanes J. Real-time multiple-particle tracking: applications to drug and gene delivery. Adv Drug Deliv Rev. 2005;57:63–78. doi: 10.1016/j.addr.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 116.Suh J, Wirtz D, Hanes J. Efficient active transport of gene nanocarriers to the cell nucleus. Proc Natl Acad Sci U S A. 2003;100:3878–3882. doi: 10.1073/pnas.0636277100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Suk JS, Suh J, Lai SK, Hanes J. Quantifying the intracellular transport of viral and nonviral gene vectors in primary neurons. Exp Biol Med. 2007;232:461–9. [PubMed] [Google Scholar]
- 118.Dawson M, Wirtz D, Hanes J. Enhanced viscoelasticity of human cystic fibrotic sputum correlates with increasing microheterogeneity in particle transport. J Biol Chem. 2003;278:50393–50401. doi: 10.1074/jbc.M309026200. [DOI] [PubMed] [Google Scholar]
- 119.Dawson M, Krauland E, Wirtz D, Hanes J. Transport of polymeric nanoparticle gene carriers in gastric mucus. Biotechnol Progress. 2004;20:851–857. doi: 10.1021/bp0342553. [DOI] [PubMed] [Google Scholar]
- 120.Lai SK, Hida K, Chen C, Hanes J. Characterization of the intracellular dynamics of a non-degradative pathway accessed by polymer nanoparticles. J Controlled Release. 2008;125:107–11. doi: 10.1016/j.jconrel.2007.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Florence AT. The oral absorption of micro- and nanoparticulates: neither exceptional nor unusual. Pharm Res. 1997;14:259–66. doi: 10.1023/a:1012029517394. [DOI] [PubMed] [Google Scholar]
- 122.Florey HW. The secretion and function of intestinal mucus. Gastroenterology. 1962;43:326–9. [PubMed] [Google Scholar]
- 123.Tirosh B, Rubinstein A. Migration of adhesive and nonadhesive particles in the rat intestine under altered mucus secretion conditions. J Pharm Sci. 1998;87:453–6. doi: 10.1021/js9703380. [DOI] [PubMed] [Google Scholar]
- 124.Bernkop-Schnurch A. Thiomers: A new generation of mucoadhesive polymers. Adv Drug Delivery Rev. 2005;57:1569–1582. doi: 10.1016/j.addr.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 125.Prego C, Torres D, Alonso MJ. The potential of chitosan for the oral administration of peptides. Expert Opin Drug Deliv. 2005;2:843–54. doi: 10.1517/17425247.2.5.843. [DOI] [PubMed] [Google Scholar]
- 126.Jubeh TT, Barenholz Y, Rubinstein A. Differential adhesion of normal and inflamed rat colonic mucosa by charged liposomes. Pharm Res. 2004;21:447–53. doi: 10.1023/B:PHAM.0000019298.29561.cd. [DOI] [PubMed] [Google Scholar]
- 127.Lele BS, Hoffman AS. Mucoadhesive drug carriers based on complexes of poly(acrylic acid) and PEGylated drugs having hydrolysable PEG-anhydride-drug linkages. J Controlled Release. 2000;69:237–48. doi: 10.1016/s0168-3659(00)00303-5. [DOI] [PubMed] [Google Scholar]
- 128.Peppas NA, Keys KB, Torres-Lugo M, Lowman AM. Poly(ethylene glycol)-containing hydrogels in drug delivery. J Controlled Release. 1999;62:81–7. doi: 10.1016/s0168-3659(99)00027-9. [DOI] [PubMed] [Google Scholar]
- 129.Yoncheva K, Gomez S, Campanero MA, Gamazo C, Irache JM. Bioadhesive properties of pegylated nanoparticles. Expert Opin Drug Deliv. 2005;2:205–18. doi: 10.1517/17425247.2.2.205. [DOI] [PubMed] [Google Scholar]
- 130.Takeuchi H, Yamamoto H, Kawashima Y. Mucoadhesive nanoparticulate systems for peptide drug delivery. Adv Drug Deliv Rev. 2001;47:39–54. doi: 10.1016/s0169-409x(00)00120-4. [DOI] [PubMed] [Google Scholar]
- 131.Keely S, Rullay A, Wilson C, Carmichael A, Carrington S, Corfield A, Haddleton DM, Brayden DJ. In vitro and ex vivo intestinal tissue models to measure mucoadhesion of poly (methacrylate) and N-trimethylated chitosan polymers. Pharm Res. 2005;22:38–49. doi: 10.1007/s11095-004-9007-1. [DOI] [PubMed] [Google Scholar]
- 132.Quintanar-Guerrero D, Villalobos-Garcia R, Alvarez-Colin E, Cornejo-Bravo JM. In vitro evaluation of the bioadhesive properties of hydrophobic polybasic gels containing N,N-dimethylaminoethyl methacrylate-co-methyl methacrylate. Biomaterials. 2001;22:957–61. doi: 10.1016/s0142-9612(00)00260-x. [DOI] [PubMed] [Google Scholar]
- 133.Chickering D, Jacob J, Mathiowitz E. Poly(fumaric-co-sebacic) microspheres as oral drug delivery systems. Biotechnol Bioeng. 1996;52:96–101. doi: 10.1002/(SICI)1097-0290(19961005)52:1<96::AID-BIT9>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 134.Mathiowitz E, Jacob JS, Jong YS, Carino GP, Chickering DE, Chaturvedi P, Santos CA, Vijayaraghavan K, Montgomery S, Bassett M, Morrell C. Biologically erodable microsphere as potential oral drug delivery system. Nature. 1997;386:410–414. doi: 10.1038/386410a0. [DOI] [PubMed] [Google Scholar]
- 135.Naisbett B, Woodley J. The Potential Use of Tomato Lectin for Oral-Drug Delivery. 3. Bioadhesion in-Vivo. Int J Pharm. 1995;114:227–236. [Google Scholar]
- 136.Lehr CM, Bouwstra JA, Kok W, Noach AB, de Boer AG, Junginger HE. Bioadhesion by means of specific binding of tomato lectin. Pharm Res. 1992;9:547–53. doi: 10.1023/a:1015804816582. [DOI] [PubMed] [Google Scholar]
- 137.Irache JM, Durrer C, Duchene D, Ponchel G. Bioadhesion of lectin-latex conjugates to rat intestinal mucosa. Pharm Res. 1996;13:1716–9. doi: 10.1023/a:1016405126656. [DOI] [PubMed] [Google Scholar]
- 138.Montisci MJ, Dembri A, Giovannuci G, Chacun H, Duchene D, Ponchel G. Gastrointestinal transit and mucoadhesion of colloidal suspensions of Lycopersicon esculentum L. and Lotus tetragonolobus lectin-PLA microsphere conjugates in rats. Pharm Res. 2001;18:829–37. doi: 10.1023/a:1011044730790. [DOI] [PubMed] [Google Scholar]
- 139.Haltner E, Easson JH, Russel-Jones G, Lehr CM. A rapid assay for bioadhesion of lectin-functionalized nano-particles to Caco-2 cell monolayers. J Controlled Release. 1996;41:S3. [Google Scholar]
- 140.Irache JM, Durrer C, Duchene D, Ponchel G. Preparation and characterization of lectin-latex conjugates for specific bioadhesion. Biomaterials. 1994;15:899–904. doi: 10.1016/0142-9612(94)90114-7. [DOI] [PubMed] [Google Scholar]
- 141.Janes KA, Calvo P, Alonso MJ. Polysaccharide colloidal particles as delivery systems for macromolecules. Adv Drug Deliv Rev. 2001;47:83–97. doi: 10.1016/s0169-409x(00)00123-x. [DOI] [PubMed] [Google Scholar]
- 142.Fernandez-Urrusuno R, Calvo P, Remunan-Lopez C, Vila-Jato JL, Alonso MJ. Enhancement of nasal absorption of insulin using chitosan nanoparticles. Pharm Res. 1999;16:1576–81. doi: 10.1023/a:1018908705446. [DOI] [PubMed] [Google Scholar]
- 143.Pan Y, Li YJ, Zhao HY, Zheng JM, Xu H, Wei G, Hao JS, Cui FD. Bioadhesive polysaccharide in protein delivery system: chitosan nanoparticles improve the intestinal absorption of insulin in vivo. Int J Pharm. 2002;249:139–47. doi: 10.1016/s0378-5173(02)00486-6. [DOI] [PubMed] [Google Scholar]
- 144.Prego C, Torres D, Alonso MJ. Chitosan nanocapsules as carriers for oral peptide delivery: effect of chitosan molecular weight and type of salt on the in vitro behaviour and in vivo effectiveness. J Nanosci Nanotechnol. 2006;6:2921–8. doi: 10.1166/jnn.2006.429. [DOI] [PubMed] [Google Scholar]
- 145.Roy K, Mao HQ, Huang SK, Leong KW. Oral gene delivery with chitosan--DNA nanoparticles generates immunologic protection in a murine model of peanut allergy. Nat Med. 1999;5:387–91. doi: 10.1038/7385. [DOI] [PubMed] [Google Scholar]
- 146.Damge C, Vranckx H, Balschmidt P, Couvreur P. Poly(alkyl cyanoacrylate) nanospheres for oral administration of insulin. J Pharm Sci. 1997;86:1403–9. doi: 10.1021/js970124i. [DOI] [PubMed] [Google Scholar]
- 147.Lowe PJ, Temple CS. Calcitonin and insulin in isobutylcyanoacrylate nanocapsules: protection against proteases and effect on intestinal absorption in rats. J Pharm Pharmacol. 1994;46:547–52. doi: 10.1111/j.2042-7158.1994.tb03854.x. [DOI] [PubMed] [Google Scholar]
- 148.Sarmento B, Ribeiro A, Veiga F, Sampaio P, Neufeld R, Ferreira D. Alginate/chitosan nanoparticles are effective for oral insulin delivery. Pharm Res. 2007;24:2198–206. doi: 10.1007/s11095-007-9367-4. [DOI] [PubMed] [Google Scholar]
- 149.Neutra MR, Forstner JF. Gastrointestinal mucus: synthesis, secretion and function. In: Johnson LR, editor. Physiology of the Gastrointestinal Tract. Raven; New York: 1987. pp. 975–1009. [Google Scholar]
- 150.Lavelle EC, Sharif S, Thomas NW, Holland J, Davis SS. The importance of gastrointestinal uptake of particles in the design of oral delivery systems. Adv Drug Deliv Rev. 1995;18:5–22. [Google Scholar]
- 151.Jani PU, Mccarthy DE, Florence AT. Nanosphere and Microsphere Uptake Via Peyer Patches - Observation of the Rate of Uptake in the Rat after a Single Oral Dose. Int J Pharm. 1992;86:239–246. [Google Scholar]
- 152.Jani PU, Halbert GW, Langridge J, Florence AT. The uptake and translocation of latex nanospheres and microspheres after oral administration to rats. J Pharm Pharmacol. 1989;41:809–12. doi: 10.1111/j.2042-7158.1989.tb06377.x. [DOI] [PubMed] [Google Scholar]
- 153.Scherer D, Mooren FC, Kinne RK, Kreuter J. In vitro permeability of PBCA nanoparticles through porcine small intestine. J Drug Target. 1993;1:21–7. doi: 10.3109/10611869308998761. [DOI] [PubMed] [Google Scholar]
- 154.O’Hagan DT. The intestinal uptake of particles and the implications for drug and antigen delivery. J Anat. 1996;189(Pt 3):477–82. [PMC free article] [PubMed] [Google Scholar]
- 155.Sternson LA. Obstacles to polypeptide delivery. Ann N Y Acad Sci. 1987;507:19–21. doi: 10.1111/j.1749-6632.1987.tb45788.x. [DOI] [PubMed] [Google Scholar]
- 156.des Rieux A, Fievez V, Garinot M, Schneider Y-J, Preat V. Nanoparticles as potential oral delivery systems of proteins and vaccines: A mechanistic approach. J Controlled Release. 2006;116:1–27. doi: 10.1016/j.jconrel.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 157.Florence AT, Sakthivel T, Tooth I. Oral uptake and translocation of a polylysine dendrimer with a lipid surface. J Controlled Release. 2000;65:253–9. doi: 10.1016/s0168-3659(99)00237-0. [DOI] [PubMed] [Google Scholar]
- 158.Hillyer JF, Albrecht RM. Gastrointestinal persorption and tissue distribution of differently sized colloidal gold nanoparticles. J Pharm Sci. 2001;90:1927–36. doi: 10.1002/jps.1143. [DOI] [PubMed] [Google Scholar]
- 159.Delie F. Evaluation of nano- and microparticle uptake by the gastrointestinal tract. Adv Drug Deliv Rev. 1998;34:221–233. doi: 10.1016/s0169-409x(98)00041-6. [DOI] [PubMed] [Google Scholar]
- 160.Clark MA, Jepson MA, Hirst BH. Exploiting M cells for drug and vaccine delivery. Adv Drug Deliv Rev. 2001;50:81–106. doi: 10.1016/s0169-409x(01)00149-1. [DOI] [PubMed] [Google Scholar]
- 161.Czerkinsky C, Svennerholm AM, Holmgren J. Induction and assessment of immunity at enteromucosal surfaces in humans: implications for vaccine development. Clin Infect Dis. 1993;16(Suppl 2):S106–16. doi: 10.1093/clinids/16.supplement_2.s106. [DOI] [PubMed] [Google Scholar]
- 162.Langer R, Cleland JL, Hanes J. New advances in microsphere-based single-dose vaccines. Adv Drug Deliv Rev. 1997;28:97–119. doi: 10.1016/s0169-409x(97)00053-7. [DOI] [PubMed] [Google Scholar]
- 163.Challacombe SJ, Rahman D, Jeffery H, Davis SS, O’Hagan DT. Enhanced secretory IgA and systemic IgG antibody responses after oral immunization with biodegradable microparticles containing antigen. Immunology. 1992;76:164–8. [PMC free article] [PubMed] [Google Scholar]
- 164.O’Hagan DT, McGee JP, Holmgren J, Mowat AM, Donachie AM, Mills KH, Gaisford W, Rahman D, Challacombe SJ. Biodegradable microparticles for oral immunization. Vaccine. 1993;11:149–54. doi: 10.1016/0264-410x(93)90011-l. [DOI] [PubMed] [Google Scholar]
- 165.Eldridge JH, Hammond CJ, Meulbroek JA, Staas JK, Gilley RM, Tice TR. Controlled Vaccine Release in the Gut-Associated Lymphoid-Tissues.1. Orally-Administered Biodegradable Microspheres Target the Peyers Patches. J Controlled Release. 1990;11:205–214. [Google Scholar]
- 166.Jung T, Kamm W, Breitenbach A, Hungerer KD, Hundt E, Kissel T. Tetanus toxoid loaded nanoparticles from sulfobutylated poly(vinyl alcohol)-graft-poly(lactide-co-glycolide): evaluation of antibody response after oral and nasal application in mice. Pharm Res. 2001;18:352–60. doi: 10.1023/a:1011063232257. [DOI] [PubMed] [Google Scholar]
- 167.Bhavsar MD, Amiji MM. Polymeric nano- and microparticle technologies for oral gene delivery. Expert Opin Drug Deliv. 2007;4:197–213. doi: 10.1517/17425247.4.3.197. [DOI] [PubMed] [Google Scholar]
- 168.Bernkop-Schnurch A. Mucoadhesive systems in oral drug delivery. Drug Discovery Today: Technologies. 2005;2:83–87. doi: 10.1016/j.ddtec.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 169.Wada A, Nakamura H. Nature of the charge distribution in proteins. Nature. 1981;293:757–8. doi: 10.1038/293757a0. [DOI] [PubMed] [Google Scholar]
- 170.Sakuma S, Sudo R, Suzuki N, Kikuchi H, Akashi M, Hayashi M. Mucoadhesion of polystyrene nanoparticles having surface hydrophilic polymeric chains in the gastrointestinal tract. Int J Pharm. 1999;177:161–72. doi: 10.1016/s0378-5173(98)00346-9. [DOI] [PubMed] [Google Scholar]
- 171.Sakuma S, Sudo R, Suzuki N, Kikuchi H, Akashi M, Ishida Y, Hayashi M. Behavior of mucoadhesive nanoparticles having hydrophilic polymeric chains in the intestine. J Controlled Release. 2002;81:281–90. doi: 10.1016/s0168-3659(02)00072-x. [DOI] [PubMed] [Google Scholar]
- 172.Ai H, Jones SA, Lvov YM. Biomedical applications of electrostatic layer-by-layer nano-assembly of polymers, enzymes, and nanoparticles. Cell Biochem Biophys. 2003;39:23–43. doi: 10.1385/CBB:39:1:23. [DOI] [PubMed] [Google Scholar]
- 173.Bertrand P, Jonas A, Laschewsky A, Legras R. Ultrathin polymer coatings by complexation of polyelectrolytes at interfaces: suitable materials, structure and properties. Macromol Rapid Commun. 2000;21:319–348. [Google Scholar]
- 174.Harris JM, Chess RB. Effect of pegylation on pharmaceuticals. Nat Rev Drug Discov. 2003;2:214–21. doi: 10.1038/nrd1033. [DOI] [PubMed] [Google Scholar]
- 175.Huang Y, Leobandung W, Foss A, Peppas NA. Molecular aspects of muco- and bioadhesion: tethered structures and site-specific surfaces. J Controlled Release. 2000;65:63–71. doi: 10.1016/s0168-3659(99)00233-3. [DOI] [PubMed] [Google Scholar]
- 176.Bures P, Huang Y, Oral E, Peppas NA. Surface modifications and molecular imprinting of polymers in medical and pharmaceutical applications. J Controlled Release. 2001;72:25–33. doi: 10.1016/s0168-3659(01)00259-0. [DOI] [PubMed] [Google Scholar]
- 177.Fresta M, Fontana G, Bucolo C, Cavallaro G, Giammona G, Puglisi G. Ocular tolerability and in vivo bioavailability of poly(ethylene glycol) (PEG)-coated polyethyl-2-cyanoacrylate nanosphere-encapsulated acyclovir. J Pharm Sci. 2001;90:288–97. doi: 10.1002/1520-6017(200103)90:3<288::aid-jps4>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 178.Serra L, Domenech J, Peppas NA. Design of poly(ethylene glycol)-tethered copolymers as novel mucoadhesive drug delivery systems. Eur J Pharmaceut Biopharmaceut. 2006;63:11–18. doi: 10.1016/j.ejpb.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 179.Sahlin JJ, Peppas NA. Enhanced hydrogel adhesion by polymer interdiffusion: use of linear poly(ethylene glycol) as an adhesion promoter. J Biomater Sci Polym Ed. 1997;8:421–36. doi: 10.1163/156856297x00362. [DOI] [PubMed] [Google Scholar]
- 180.Giannavola C, Bucolo C, Maltese A, Paolino D, Vandelli MA, Puglisi G, Lee VH, Fresta M. Influence of preparation conditions on acyclovir-loaded poly-d, l-lactic acid nanospheres and effect of PEG coating on ocular drug bioavailability. Pharm Res. 2003;20:584–90. doi: 10.1023/a:1023290514575. [DOI] [PubMed] [Google Scholar]
- 181.Sezgin Z, Yuksel N, Baykara T. Investigation of pluronic and PEG-PE micelles as carriers of meso-tetraphenyl porphine for oral administration. Int J Pharm. 2007;332:161–7. doi: 10.1016/j.ijpharm.2006.09.030. [DOI] [PubMed] [Google Scholar]
- 182.Yoncheva K, Guembe L, Campanero MA, Irache JM. Evaluation of bioadhesive potential and intestinal transport of pegylated poly(anhydride) nanoparticles. Int J Pharm. 2007;334:156–65. doi: 10.1016/j.ijpharm.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 183.Wang YY, Lai SK, Suk JS, Pace A, Cone R, Hanes J. Addressing the PEG Mucoadhesivity Paradox to Engineer Nanoparticles that “Slip” through the Human Mucus Barrier. Angew Chem Int Ed Engl. 2008 doi: 10.1002/anie.200803526. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Chia-Ming C, Weiner N. Gastrointestinal uptake of liposomes. I. In vitro and in situ studies. Int J Pharm. 1987;37:75–85. [Google Scholar]
- 185.Rowland RN, Woodley JF. The stability of liposomes in vitro to pH, bile salts and pancreatic lipase. Biochim Biophys Acta. 1980;620:400–9. doi: 10.1016/0005-2760(80)90131-9. [DOI] [PubMed] [Google Scholar]
- 186.Sanders NN, Van Rompaey E, De Smedt SC, Demeester J. Structural alterations of gene complexes by cystic fibrosis sputum. Am J Respir Crit Care Med. 2001;164:486–93. doi: 10.1164/ajrccm.164.3.2011041. [DOI] [PubMed] [Google Scholar]
- 187.Sanders NN, De Smedt SC, Demeester J. Mobility and stability of gene complexes in biogels. J Controlled Release. 2003;87:117–29. doi: 10.1016/s0168-3659(02)00355-3. [DOI] [PubMed] [Google Scholar]
- 188.Sanders NN, De Smedt SC, Cheng SH, Demeester J. Pegylated GL67 lipoplexes retain their gene transfection activity after exposure to components of CF mucus. Gene Ther. 2002;9:363–71. doi: 10.1038/sj.gt.3301663. [DOI] [PubMed] [Google Scholar]
- 189.Kim DH, Martin DC. Sustained release of dexamethasone from hydrophilic matrices using PLGA nanoparticles for neural drug delivery. Biomaterials. 2006;27:3031–7. doi: 10.1016/j.biomaterials.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 190.Yoo HS, Oh JE, Lee KH, Park TG. Biodegradable nanoparticles containing doxorubicin-PLGA conjugate for sustained release. Pharm Res. 1999;16:1114–8. doi: 10.1023/a:1018908421434. [DOI] [PubMed] [Google Scholar]
- 191.Fu K, Harrell R, Zinski K, Um C, Jaklenec A, Frazier J, Lotan N, Burke P, Klibanov AM, Langer R. A potential approach for decreasing the burst effect of protein from PLGA microspheres. J Pharm Sci. 2003;92:1582–91. doi: 10.1002/jps.10414. [DOI] [PubMed] [Google Scholar]
- 192.Gref R, Minamitake Y, Peracchia MT, Trubetskoy V, Torchilin V, Langer R. Biodegradable long-circulating polymeric nanospheres. Science. 1994;263:1600–3. doi: 10.1126/science.8128245. [DOI] [PubMed] [Google Scholar]
- 193.Rejman J, Oberle V, Zuhorn IS, Hoekstra D. Size-dependent internalization of particles via the pathways of clathrin- and caveolae-mediated endocytosis. Biochem J. 2004;377:159–69. doi: 10.1042/BJ20031253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Rubin BK. Mucus structure and properties in cystic fibrosis. Paediatr Respir Rev. 2007;8:4–7. doi: 10.1016/j.prrv.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 195.Boucher RC. An overview of the pathogenesis of cystic fibrosis lung disease. Adv Drug Deliv Rev. 2002;54:1359–71. doi: 10.1016/s0169-409x(02)00144-8. [DOI] [PubMed] [Google Scholar]
- 196.Pediatr Pulmonol Suppl; Summary Conclusion of the 17th annual North American Cystic Fibrosis Conference; Anaheim, California, USA. October 16–19, 2003; 2003. pp. 92–394. [PubMed] [Google Scholar]
- 197.Kitson C, Angel B, Judd D, Rothery S, Severs NJ, Dewar A, Huang L, Wadsworth SC, Cheng SH, Geddes DM, Alton EW. The extra- and intracellular barriers to lipid and adenovirus-mediated pulmonary gene transfer in native sheep airway epithelium. Gene Ther. 1999;6:534–46. doi: 10.1038/sj.gt.3300840. [DOI] [PubMed] [Google Scholar]
- 198.Shak S, Capon DJ, Hellmiss R, Marsters SA, Baker CL. Recombinant human DNase I reduces the viscosity of cystic fibrosis sputum. Proc Natl Acad Sci U S A. 1990;87:9188–92. doi: 10.1073/pnas.87.23.9188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Shah PL, Scott SF, Knight RA, Marriott C, Ranasinha C, Hodson ME. In vivo effects of recombinant human DNase I on sputum in patients with cystic fibrosis. Thorax. 1996;51:119–25. doi: 10.1136/thx.51.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Sheffner AL, Medler EM, Jacobs LW, Sarett HP. The in Vitro Reduction in Viscosity of Human Tracheobronchial Secretions by Acetylcysteine. Am Rev Respir Dis. 1964;90:721–9. doi: 10.1164/arrd.1964.90.5.721. [DOI] [PubMed] [Google Scholar]
- 201.Henke MO, Ratjen F. Mucolytics in cystic fibrosis. Paediatr Respir Rev. 2007;8:24–9. doi: 10.1016/j.prrv.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 202.Ferrari S, Kitson C, Farley R, Steel R, Marriott C, Parkins DA, Scarpa M, Wainwright B, Evans MJ, Colledge WH, Geddes DM, Alton EW. Mucus altering agents as adjuncts for nonviral gene transfer to airway epithelium. Gene Ther. 2001;8:1380–6. doi: 10.1038/sj.gt.3301525. [DOI] [PubMed] [Google Scholar]
- 203.App EM, Baran D, Dab I, Malfroot A, Coffiner M, Vanderbist F, King M. Dose-finding and 24-h monitoring for efficacy and safety of aerosolized Nacystelyn in cystic fibrosis. Eur Respir J. 2002;19:294–302. doi: 10.1183/09031936.02.00025802. [DOI] [PubMed] [Google Scholar]
- 204.Tomkiewicz RP, App EM, De Sanctis GT, Coffiner M, Maes P, Rubin BK, King M. A comparison of a new mucolytic N-acetylcysteine L-lysinate with N-acetylcysteine: airway epithelial function and mucus changes in dog. Pulm Pharmacol. 1995;8:259–65. doi: 10.1006/pulp.1995.1035. [DOI] [PubMed] [Google Scholar]
- 205.Vasconcellos CA, Allen PG, Wohl ME, Drazen JM, Janmey PA, Stossel TP. Reduction in viscosity of cystic fibrosis sputum in vitro by gelsolin. Science. 1994;263:969–71. doi: 10.1126/science.8310295. [DOI] [PubMed] [Google Scholar]
- 206.Rubin BK, Kater AP, Goldstein AL. Thymosin beta4 sequesters actin in cystic fibrosis sputum and decreases sputum cohesivity in vitro. Chest. 2006;130:1433–40. doi: 10.1378/chest.130.5.1433. [DOI] [PubMed] [Google Scholar]
- 207.Sanders NN, Franckx H, De Boeck K, Haustraete J, De Smedt SC, Demeester J. Role of magnesium in the failure of rhDNase therapy in patients with cystic fibrosis. Thorax. 2006;61:962–8. doi: 10.1136/thx.2006.060814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Jordan N, Newton J, Pearson J, Allen A. A novel method for the visualization of the in situ mucus layer in rat and man. Clin Sci (Lond) 1998;95:97–106. [PubMed] [Google Scholar]
- 209.Kerss S, Allen A, Garner A. A simple method for measuring thickness of the mucus gel layer adherent to rat, frog and human gastric mucosa: influence of feeding, prostaglandin, N-acetylcysteine and other agents. Clin Sci (Lond) 1982;63:187–95. doi: 10.1042/cs0630187. [DOI] [PubMed] [Google Scholar]
- 210.Atuma C, Strugala V, Allen A, Holm L. The adherent gastrointestinal mucus gel layer: thickness and physical state in vivo. Am J Physiol Gastrointest Liver Physiol. 2001;280:G922–9. doi: 10.1152/ajpgi.2001.280.5.G922. [DOI] [PubMed] [Google Scholar]
- 211.Strugala V, Allen A, Dettmar PW, Pearson JP. Colonic mucin: methods of measuring mucus thickness. Proc Nutr Soc. 2003;62:237–43. doi: 10.1079/pns2002205. [DOI] [PubMed] [Google Scholar]
- 212.Szentkuti L, Lorenz K. The thickness of the mucus layer in different segments of the rat intestine. Histochem J. 1995;27:466–72. [PubMed] [Google Scholar]
- 213.Schuhl JF. Nasal mucociliary clearance in perennial rhinitis. J Investig Allergol Clin Immunol. 1995;5:333–6. [PubMed] [Google Scholar]
- 214.Illum L. Nasal drug delivery--possibilities, problems and solutions. J Control Release. 2003;87:187–98. doi: 10.1016/s0168-3659(02)00363-2. [DOI] [PubMed] [Google Scholar]
- 215.Mitra AK, Krishnamoorthy R. Prodrugs for nasal drug delivery. Adv Drug Deliv Rev. 1998;29:135–146. doi: 10.1016/s0169-409x(97)00065-3. [DOI] [PubMed] [Google Scholar]
- 216.Wong JW, Keens TG, Wannamaker EM, Crozier DN, Levison H, Aspin N. Effects of gravity on tracheal mucus transport rates in normal subjects and in patients with cystic fibrosis. Pediatrics. 1977;60:146–52. [PubMed] [Google Scholar]
- 217.Foster WM, Langenback E, Bergofsky EH. Measurement of tracheal and bronchial mucus velocities in man: relation to lung clearance. J Appl Physiol. 1980;48:965–71. doi: 10.1152/jappl.1980.48.6.965. [DOI] [PubMed] [Google Scholar]
- 218.Hofmann W, Asgharian B. The effect of lung structure on mucociliary clearance and particle retention in human and rat lungs. Toxicol Sci. 2003;73:448–56. doi: 10.1093/toxsci/kfg075. [DOI] [PubMed] [Google Scholar]
- 219.Leikauf G, Yeates DB, Wales KA, Spektor D, Albert RE, Lippmann M. Effects of sulfuric acid aerosol on respiratory mechanics and mucociliary particle clearance in healthy nonsmoking adults. Am Ind Hyg Assoc J. 1981;42:273–82. doi: 10.1080/15298668191419721. [DOI] [PubMed] [Google Scholar]
- 220.Yeates DB, Aspin N, Levison H, Jones MT, Bryan AC. Mucociliary tracheal transport rates in man. J Appl Physiol. 1975;39:487–95. doi: 10.1152/jappl.1975.39.3.487. [DOI] [PubMed] [Google Scholar]
- 221.Yeates DB, Gerrity TR, Garrard CS. Characteristics of tracheobronchial deposition and clearance in man. Ann Occup Hyg. 1982;26:245–57. [PubMed] [Google Scholar]
- 222.Yeates DB, Pitt BR, Spektor DM, Karron GA, Albert RE. Coordination of mucociliary transport in human trachea and intrapulmonary airways. J Appl Physiol. 1981;51:1057–64. doi: 10.1152/jappl.1981.51.5.1057. [DOI] [PubMed] [Google Scholar]
- 223.Denton R. The rheology of human lung mucus. Ann N Y Acad Sci. 1963;106:746–54. doi: 10.1111/j.1749-6632.1963.tb16681.x. [DOI] [PubMed] [Google Scholar]
- 224.Friedman M, Dougherty R, Nelson SR, White RP, Sackner MA, Wanner A. Acute effects of an aerosol hair spray on tracheal mucociliary transport. Am Rev Respir Dis. 1977;116:281–6. doi: 10.1164/arrd.1977.116.2.281. [DOI] [PubMed] [Google Scholar]
- 225.Goodman RM, Yergin BM, Landa JF, Golivanux MH, Sackner MA. Relationship of smoking history and pulmonary function tests to tracheal mucous velocity in nonsmokers, young smokers, ex-smokers, and patients with chronic bronchitis. Am Rev Respir Dis. 1978;117:205–14. doi: 10.1164/arrd.1978.117.2.205. [DOI] [PubMed] [Google Scholar]
- 226.Sackner MA, Landa J, Hirsch J, Zapata A. Pulmonary effects of oxygen breathing. A 6-hour study in normal men. Ann Intern Med. 1975;82:40–3. doi: 10.7326/0003-4819-82-1-40. [DOI] [PubMed] [Google Scholar]
- 227.Santa Cruz R, Landa J, Hirsch J, Sackner MA. Tracheal mucous velocity in normal man and patients with obstructive lung disease: effects of terbutaline. Am Rev Respir Dis. 1974;109:458–63. doi: 10.1164/arrd.1974.109.4.458. [DOI] [PubMed] [Google Scholar]
- 228.Toomes H, Vogt-Moykopf I, Heller WD, Ostertag H. Measurement of mucociliary clearance in smokers and nonsmokers using a bronchoscopic video-technical method. Lung. 1981;159:27–34. doi: 10.1007/BF02713894. [DOI] [PubMed] [Google Scholar]
- 229.Wanner A, Salathe M, O’Riordan TG. Mucociliary clearance in the airways. Am J Respir Crit Care Med. 1996;154:1868–902. doi: 10.1164/ajrccm.154.6.8970383. [DOI] [PubMed] [Google Scholar]
- 230.Yeates DB, Gerrity TR, Garrard CS. Particle deposition and clearance in the bronchial tree. Ann Biomed Eng. 1981;9:577–92. doi: 10.1007/BF02364772. [DOI] [PubMed] [Google Scholar]
- 231.Donaldson SH, Corcoran TE, Laube BL, Bennett WD. Mucociliary clearance as an outcome measure for cystic fibrosis clinical research. Proc Am Thorac Soc. 2007;4:399–405. doi: 10.1513/pats.200703-042BR. [DOI] [PubMed] [Google Scholar]
- 232.Yoncheva K, Guembe L, Campanero MA, Irache JM. Evaluation of bioadhesive potential and intestinal transport of pegylated poly(anhydride) nanoparticles. Int J Pharm. 2007;334:156–65. doi: 10.1016/j.ijpharm.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 233.Yoncheva K, Lizarraga E, Irache JM. Pegylated nanoparticles based on poly(methyl vinyl ether-co-maleic anhydride): preparation and evaluation of their bioadhesive properties. Eur J Pharm Sci. 2005;24:411–9. doi: 10.1016/j.ejps.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 234.Behrens I, Pena AI, Alonso MJ, Kissel T. Comparative uptake studies of bioadhesive and non-bioadhesive nanoparticles in human intestinal cell lines and rats: the effect of mucus on particle adsorption and transport. Pharm Res. 2002;19:1185–93. doi: 10.1023/a:1019854327540. [DOI] [PubMed] [Google Scholar]
- 235.Fresta M, Fontana G, Bucolo C, Cavallaro G, Giammona G, Puglisi G. Ocular tolerability and in vivo bioavailability of poly(ethylene glycol) (PEG)-coated polyethyl-2-cyanoacrylate nanosphere-encapsulated acyclovir. J Pharm Sci. 2001;90:288–97. doi: 10.1002/1520-6017(200103)90:3<288::aid-jps4>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]