Abstract
The dopamine hypothesis of schizophrenia has been one of the most enduring ideas in psychiatry. Initially, the emphasis was on a role of hyperdopaminergia in the etiology of schizophrenia (version I), but it was subsequently reconceptualized to specify subcortical hyperdopaminergia with prefrontal hypodopaminergia (version II). However, these hypotheses focused too narrowly on dopamine itself, conflated psychosis and schizophrenia, and predated advances in the genetics, molecular biology, and imaging research in schizophrenia. Since version II, there have been over 6700 articles about dopamine and schizophrenia. We selectively review these data to provide an overview of the 5 critical streams of new evidence: neurochemical imaging studies, genetic evidence, findings on environmental risk factors, research into the extended phenotype, and animal studies. We synthesize this evidence into a new dopamine hypothesis of schizophrenia—version III: the final common pathway. This hypothesis seeks to be comprehensive in providing a framework that links risk factors, including pregnancy and obstetric complications, stress and trauma, drug use, and genes, to increased presynaptic striatal dopaminergic function. It explains how a complex array of pathological, positron emission tomography, magnetic resonance imaging, and other findings, such as frontotemporal structural and functional abnormalities and cognitive impairments, may converge neurochemically to cause psychosis through aberrant salience and lead to a diagnosis of schizophrenia. The hypothesis has one major implication for treatment approaches. Current treatments are acting downstream of the critical neurotransmitter abnormality. Future drug development and research into etiopathogenesis should focus on identifying and manipulating the upstream factors that converge on the dopaminergic funnel point.
Keywords: psychosis; biology; etiology, cause; brain; imaging, pathophysiology; risk factors; treatment
Introduction
The hypothesis that dopamine and dopaminergic mechanisms are central to schizophrenia, and particularly psychosis, has been one of the most enduring ideas about the illness. Despite a relatively inauspicious start—dopamine was initially thought to be a precursor molecule of little functional significance—the idea has evolved and accommodated new evidence to provide an increasingly sophisticated account of the involvement of dopamine in schizophrenia. This review summarizes the evolution of the dopamine hypothesis, which we characterize as having 2 main prior incarnations (version I, the original incarnation, and version II, which was articulated in 1991 and has been the guiding framework since). The main effort in this article is to synthesize the evidence since version II and articulate what we call “The Dopamine Hypothesis of Schizophrenia: Version III,” which represents the most parsimonious account of the current state of knowledge. We call it version III—because we expect it to be revised. However, we highlight features of version III that we believe are sufficiently well established that they are likely to be constant in future revisions, as well as aspects that are still in evolution. Finally, we review the explanatory power of the hypothesis—indicating the known aspects of schizophrenia that it can and cannot explain.
The Dopamine Hypothesis: Version I
The first version of the dopamine hypothesis could be entitled the dopamine receptor hypothesis. It emerged from the discovery of antipsychotic drugs1 and the seminal work of Carlsson and Lindqvit who identified that these drugs increased the metabolism of dopamine when administered to animals.2 Further evidence came from observations that reserpine, which is effective for treating psychosis, was found to block the reuptake of dopamine and other monoamines, leading to their dissipation.3 Studies showing that amphetamine, which increases synaptic monoamine levels, can induce psychotic symptoms (reviewed in Lieberman et al4) provided additional evidence. It was not until the 1970s, however, that the dopamine hypothesis was finally crystallized with the finding that the clinical effectiveness of antipsychotic drugs was directly related to their affinity for dopamine receptors.5–7 The focus at the time was on excess transmission at dopamine receptors and blockade of these receptors to treat the psychosis (eg, Matthysse8 and Snyder9). While version I accounted for the data available then, it was seen as a hypothesis of schizophrenia as a whole without a clear articulation of its relationship to any particular dimension (eg, positive vs negative symptoms) and no link was made to genetics and neurodevelopmental deficits (understandably as little was then known about them), and there was little clear indication of where the abnormality was in the living brain—this would require the later application of in vivo imaging techniques. Additionally, dopamine was thought of in isolation, with little consideration of how it might relate to known risk factors for schizophrenia, and finally there was no framework for linking the dopaminergic abnormality to the expression of symptoms.
The Dopamine Hypothesis: Version II
In 1991, Davis et al10 published a landmark article describing what they called “a modified dopamine hypothesis of schizophrenia” that reconceptualized the dopamine hypothesis in the light of the findings available at the time. The main advance was the addition of regional specificity into the hypothesis to account for the available postmortem and metabolite findings, imaging data, and new insights from animal studies into cortical-subcortical interactions. It was clear by this stage that dopamine metabolites were not universally elevated in the cerebrospinal fluid (CSF) or serum of patients with schizophrenia. Also the focus on D2 receptors was brought into question by findings showing that clozapine had superior efficacy for patients who were refractory to other antipsychotic drugs despite having rather low affinity for and occupancy at D2 receptors. Furthermore, the postmortem studies of D2 receptors in schizophrenia could not exclude the confounds of previous antipsychotic treatment, and the early positron emission tomography (PET) studies of D2/3 receptors in drug-naive patients showed conflicting results.
Taken together, these findings were incompatible with the simple excess dopaminergic neurotransmission proposal of version I. Furthermore, there was the paradox that dopamine metabolite measures were reduced in some patients with schizophrenia while still correlating with symptom severity and response to antipsychotic drugs. Davis et al10 drew on these inconsistencies and the emerging evidence that dopamine receptors show different brain distributions—characterized as D1 predominantly cortical and D2 predominantly subcortical—to provide a basis for suggesting that the effects of abnormalities in dopamine function could vary by brain region. However, it was PET studies showing reduced cerebral blood flow in frontal cortex that provided the best evidence of regional brain dysfunction in schizophrenia. “Hypofrontality” in these studies was directly correlated with low CSF dopamine metabolite levels. Because CSF dopamine metabolite levels reflect cortical dopamine metabolism, they argued that the relationship between hypofrontality and low CSF dopamine metabolite levels indicates low frontal dopamine levels. Thus, the major innovation in version II was the move from a one-sided dopamine hypothesis explaining all facets of schizophrenia to a regionally specific prefrontal hypodopaminergia and a subcortical hyperdopaminergia. While the evidence for this in humans was indirect, animal studies provided direct evidence of a link between hypo- and hyperdopaminergia. Lesions of dopamine neurons in the prefrontal cortex result in increased levels of dopamine and its metabolites and D2 receptor density in the striatum,11 while the application of dopamine agonists to prefrontal areas reduced dopamine metabolite levels in the striatum.12 This provided a mechanism to propose that schizophrenia is characterized by frontal hypodopaminergia resulting in striatal hyperdopaminergia. Furthermore, Davis et al10 hypothesized that negative symptoms of schizophrenia resulted from frontal hypodopaminergia, based on the similarities between the behavior exhibited by animals and humans with frontal lobe lesions and the negative symptoms of schizophrenia. Positive symptoms were hypothesized to result from striatal hyperdopaminergia, based on the findings that higher dopamine metabolite levels are related to greater positive symptoms and response to antipsychotic drug treatment.
Although a substantial advance, there are a number of weaknesses in “version II” of the dopamine hypothesis, many of which the authors acknowledged at the time. Much of the evidence for the hypothesis relied on inferences from animal studies or other clinical conditions. There was no direct evidence for low dopamine levels in the frontal cortex and limited direct evidence for elevated striatal dopaminergic function. It was unclear how the dopaminergic abnormalities were linked to the clinical phenomena—there was no framework describing how striatal hyperdopaminergia translates into delusions or how frontal hypodopaminergia results into blunted affect, for example. Furthermore, it has subsequently become clear that the cortical abnormalities are more complicated that just the hypofrontality proposed at that time (eg, see reviews by Davidson and Heinrichs13 and McGuire et al14) and little clear evidence of frontal hypodopaminergia in schizophrenia has emerged (see below). But, more importantly, version II predated the studies into the neurodevelopment and prodromal aspects of schizophrenia, did not describe the etiological origins of the dopaminergic abnormality, and, beyond specifying “hyperdopaminergia” or “hypodopaminergia,” did not pinpoint which element of dopaminergic transmission was abnormal.
New Evidence and the Rationale for Version III
Much has changed since version II. There have been more than 6700 articles and 181 000 citations to the topic of “dopamine and schizophrenia” since 1991. It is not possible to provide a comprehensive review of all the new findings since then, much less try to weave them into a coherent hypothesis. So, the focus of our effort is to identify the 5 most critical streams of new evidence, briefly summarize what we see as the key findings from these, and use them to develop the most parsimonious understanding of the role of dopamine in schizophrenia—version III.
Advances in Neurochemical Imaging of Schizophrenia
Presynaptic Dopamine Function and Synaptic Dopamine
Although it is not possible to measure dopamine levels directly in humans, techniques have been developed that provide indirect indices of dopamine synthesis and release and putative synaptic dopamine levels. Presynaptic striatal dopaminergic function can be measured using radiolabelled L-dopa, which is converted to dopamine and trapped in striatal dopamine nerve terminals ready for release. This provides an index of the synthesis and storage of dopamine in the presynaptic terminals of striatal dopaminergic neurons (see review by Moore et al15). Seven out of 9 studies in patients with schizophrenia using this technique have reported elevated presynaptic striatal dopamine synthesis capacity in schizophrenia,16–22 with effect sizes in these studies ranging from 0.63 to 1.89.23 The other 2 studies, both in chronic patients, reported either a small but not significant elevation24 or a small reduction in levels.25 All the studies that investigated patients who were acutely psychotic at the time of PET scanning found elevated presynaptic striatal dopamine availability,18–21 with effect sizes from 0.63 to 1.25.23 This, then, is the single most widely replicated brain dopaminergic abnormality in schizophrenia, and the evidence indicates the effect size is moderate to large.
The next step in dopamine transmission is the release of dopamine. Striatal synaptic dopamine release can be assessed following a challenge that releases dopamine from the neuron using PET and single photon emission computerized tomography (SPECT). The released dopamine competes with the radioligand and leads to a reduction in radiotracer binding and is considered to be an indirect index of released dopamine.26,27 All the studies using this approach have found evidence of roughly doubled radiotracer displacement in patients with schizophrenia compared with controls—an elevation that is again equivalent to a moderate to large effect size.28–32 Finally, if dopamine synthesis is increased and is more sensitive to release in the face of challenges, one would expect heightened levels of endogenous synaptic dopamine when patients are psychotic. Evidence in line with this comes from a SPECT study using a dopamine depletion technique that found that baseline occupancy of D2 receptors by dopamine is also increased in schizophrenia.33
Dopamine Receptors
PET and SPECT studies have used various radiotracers to image dopamine D2/3 receptors in schizophrenia. As Davis et al10 noted, the findings of the initial studies were inconsistent, with some reporting increased D2/3 receptor binding in schizophrenia34–36 and others no difference from controls.37,38 There have now been at least 19 studies investigating striatal D2/3 receptors in patients with schizophrenia and 3 meta-analyses.30,39,40 These meta-analyses conclude that there is at most a modest (10%–20%) elevation in striatal D2/3 receptor density in schizophrenia independent of the effects of antipsychotic drugs. This appears to be specific to D2/3 receptors—striatal D1 receptor densities are unaltered,30,39,41,42 and this elevation may be regionally specific because these increases are not seen in the extrastriatal regions. If anything, there is a decrease in D2/D3 receptors in extrastriatal areas such as the thalamus and anterior cingulate.43–46 The D2 receptor exists in 2 states, and it remains to be determined if the balance between these 2 states is altered in schizophrenia.47 Also, because the current tracers bind to a mix of D2 and D3 receptors, it is difficult to be precise whether changes are in the D3 or the D2 subtype of the receptors—though preliminary data with a recently developed tracer, [11C]-(+)-4-propyl-9-hydroxynaphthoxazine, show that there is no abnormality in high states or in D3 receptors in schizophrenia.48
Dopaminergic transmission in the prefrontal cortex is mainly mediated by D1 receptors, and D1 dysfunction has been linked to cognitive impairment and negative symptom in schizophrenia (see reviews by Goldman-Rakic et al49 and Tamminga50 among others). Three studies have investigated D1 receptor levels in drug-free patients with schizophrenia and found associations with cognitive impairment and negative symptoms. One reported reduced D1 receptor density41 another no difference from controls,42 and a further study using a different radiotracer reported increased D1 levels.51 This variation may be explained by different properties of the radiotracers: the effect of dopamine depletion on binding by the tracer used in the first 2 studies may obscure D1 receptor density elevation that is detectable by the tracer used in the last study.52 The increased binding shown by the tracer used by Abi-Dargham and colleagues, which was directly correlated with cognitive impairment, is thus consistent with chronic low levels of dopamine in the prefrontal cortex underlying cognitive dysfunction in schizophrenia, assuming that there has been a compensatory D1 receptor density upregulation.51 Further studies in patients are required to clarify this, particularly because both tracers may also bind to serotonin receptors.53
Treatment and Dopamine Receptors
Over 120 neurochemical imaging studies have investigated the in vivo effects of antipsychotic treatments on dopamine receptors in schizophrenia (see, eg, review by Frankle and Laruelle54). These show that at clinical doses all currently licensed antipsychotic drugs block striatal D2 receptors. Furthermore, a threshold striatal D2 blockade is required for antipsychotic efficacy, but this is not sufficient—some patients show little improvement despite high D2 occupancy.55–57 A major stumbling block for the dopamine hypothesis used to be the notion that antipsychotic response was delayed for 2–3 weeks after the start of treatment (see review by Grace et al58). However, there is now convincing evidence that there is no delayed response: the onset of antipsychotic action is early,59,60 this response is related to striatal D2 receptor occupancy,61 and D2 occupancy at as early as 48 hours predicts the nature of response that follows over the next 2 weeks.62 Thus, the original tenet of version I still stands—dopamine D2 receptors continue to dominate and remain necessary for antipsychotic treatment and the imaging data has further strengthened the quantitative and temporal aspects of this relationship.
In summary, the molecular imaging studies show that presynaptic striatal dopaminergic function is elevated in patients with schizophrenia and correlates most closely with the symptom dimension of psychosis and blockade of this heightened transmission, either by decreasing dopamine levels or blocking dopamine transmission, leads to a resolution of symptoms for most patients.
Advances in Understanding the Genetic Etiology of Schizophrenia
The dopamine hypothesis ‘version II’ was published before the Human Genome Project and the huge advances in genetic research in schizophrenia. After over 1200 studies, it seems clear that no one gene “encodes” for schizophrenia.63 Rather, in common with many other complex diseases, there are a number of genes each of small effect size associated with schizophrenia.63 The gene database on the Schizophrenia Research Forum (http://www.schizophreniaforum.org) provides a systematic and regularly updated meta-analysis of genetic association studies. As of autumn 2008, 4 of the top 10 gene variants most strongly associated with schizophrenia are directly involved in dopaminergic pathways. The strongest association is with a gene variant affecting the vesicular monoamine transporter protein (rs2270641, odds ratio 1.63). This protein acts to accumulate dopamine and other monoamines into vesicles, which fits with the PET studies that show elevated radiolabeled dopamine accumulation into striatal vesicles in schizophrenia. Additionally, other gene variants in the list of the strongest associations, such as in the genes for methylenetetrahydrofolate reductase and V-akt murine thymoma viral oncogene homolog 1, indirectly affect the dopaminergic system among other effects.64 Many of the other gene variants in the top list are involved in brain development, such as the gene for dysbindin, or influence more ubiquitous brain transmitters such as glutamate or γ-aminobutyric acid (GABA).63,64 While recent findings have breathed great interest in the copy number variations in schizophrenia—the early evidence there also suggests that they are rare, tend to be unique to families, and are unlikely to account for more than a few percent of schizophrenia.63,65–67 It would be premature to try and synthesize these genes into a pathway leading to dopamine abnormality because the precise number, nature, function, and association of these genes to schizophrenia is evolving. The most parsimonious statement that can be made today is that while a number of genetic associations have been identified, none of them accounts for the majority of schizophrenia and most of them are likely to be susceptibilities. Of the ones that have been identified, some have already been tied to altered dopamine transmission.68 However, the functional relevance of most of them to dopamine function is not known.68 This view of schizophrenia genetics then reemphasizes a critical role for other interacting factors—particularly the environmental risk factors for schizophrenia.
Environmental Risk Factors for Schizophrenia
A large number of disparate environmental factors clearly contribute to the risk for schizophrenia, yet many hypotheses of schizophrenia, including previous versions of the dopamine hypothesis, make no allowance for them. Markers of social adversity such as migration, unemployment, urban upbringing, lack of close friends, and childhood abuse are all associated with a well-established increased risk for schizophrenia that cannot readily be explained by genetic factors alone.69 These factors either directly index social isolation/subordination or are linked to these experiences.70 Studies in animals of social isolations71–73 and subordination73,74 find that these factors lead to dopaminergic overactivity.
Other environmental factors, such as pregnancy/obstetric complications, act in early life to increase the subsequent risk of schizophrenia (reviewed by Cannon et al,75 Geddes and Lawrie,76 and Kunugi et al77). There is now substantial evidence from animal models that pre- and perinatal factors can lead to long-term overactivity in mesostriatal dopaminergic function (reviewed by Boksa and El-Khodor78 and Boksa79). For example, neonatal lesions affecting the hippocampus80,81 or frontal cortex82 increase dopamine-mediated behavioral responses in rats, as does prenatal stress, whether induced by corticosterone administration83 or maternal handling.84 Neonatal exposure to toxins also leads to increased dopamine-mediated behavioral responses85 and elevated striatal dopamine release.86 Prenatal and neonatal stress, such as maternal separation, also increases striatal dopamine metabolism83 and release.87,88 The latter findings parallel the increased presynaptic dopaminergic function found in schizophrenia.
A number of psychoactive substances also increase the risk of schizophrenia. The relationship between stimulants, psychosis, and their effects on dopaminergic function has already been considered (eg, Lieberman et al,4 Angrist and Gershon,89 and Yui et al90). However, recent PET imaging work has shown that even a few doses of a stimulant may sensitize the striatal dopamine system and can lead to enduring increases in dopamine release to amphetamine even after many months of abstinence.91 Since earlier versions of the dopamine hypothesis, cannabis use has emerged as a risk factor for schizophrenia.92,93 The main psychoactive component of cannabis primarily acts at cannabinoid receptors,94 and this as well as other cannabinoid agonists have been shown in animals to increase striatal dopamine release.95,96 Initial findings indicate this is the case in man as well,97 a result supported by observations that dopamine metabolite levels are increased in patients admitted during a first episode of psychosis associated with cannabis use.98 Psychoactive drugs acting on other systems may also indirectly act on the dopaminergic system by potentiating dopamine release caused by other effects. This has been shown for the N-methyl-D-aspartic acid (NMDA) blocker ketamine, which has been found to increase amphetamine-induced dopamine release in healthy humans to the levels seen in schizophrenia.99 These new data therefore indicate that even psychoactive drugs that do not directly act on the dopamine system can impact on dopamine release through indirect effects.
Multiple Routes to Dopamine Dysfunction: Interacting Environmental and Genetic Factors
Genes and environmental factors do not exist in isolation. Many add to each other, and some show synergistic effects on the risk of schizophrenia or brain abnormalities associated with schizophrenia (see, eg, Cannon et al100 and Nicodemus et al101 and reviews by Mittal et al102 and van Os et al103). Furthermore, animal studies indicate that at least some of these factors interact in their effects on the dopamine system: social isolation rearing potentiates the later effects of stimulants104,105 or of stress106 on the dopamine system.105 Similar effects have also been found in humans, where striatal dopamine release in response to stress was increased in people who reported low maternal care during their early childhood.107 Additionally, there are interactions with other neurotransmitter systems: dopamine release is not seen under the influence of ketamine alone108 but enhances the action of amphetamine, suggesting the effects of NMDA blockade, or by extension other putative causes of glutamatergic dysfunction, such as neonatal insults, are modulatory. GABA interneurons are also involved in the regulation of subcortical dopamine function and have been implicated in schizophrenia.109
Interactions between gene variants, including those influencing dopaminergic function, and environmental risk factors are another possible route to dopaminergic dysfunction. This is illustrated by findings that variants of the catechol-O-methyltransferase gene (involved in dopamine catabolism) interact with early cannabis exposure to increase the subsequent risk of psychosis110 and, in other studies, to increase stress reactivity and paranoid reactions to stress (see review by van et al70). Family history of psychosis also interacts with environmental factors such as urbanicity to increase the risk of schizophrenia.111,112 Additionally, genetic risk for schizophrenia appears to interact with obstetric complications: some “schizophrenia” genetic factors make the individual more susceptible to the effects of obstetric complications, such as frontal and temporal structural abnormalities (see review by Mittal et al102). As reviewed above, animal studies indicate that frontal and temporal dysfunction can lead to increased striatal dopamine release and suggest that this is another route to dopamine dysregulation.
While further work is clearly needed to investigate the nature and extent of all these possible interactions, the evidence indicates that many disparate, direct and indirect environmental and genetic, factors may lead to dopamine dysfunction and that some occur independently while others interact. The striking empirical fact is this: the relative risks for developing schizophrenia that are accorded to migration (about 2.9113), obstetric complications (about 2.0, see meta-analyses75,76), and frequent cannabis or amphetamine use (2.09 for cannabis93 and about 10 for amphetamine use114) are considerably higher than those for any single gene variant. Thus, as the dopamine hypothesis evolves, the scientific challenge will be not just to find predisposing genes but to articulate how genes and environment interact to lead to dopamine dysfunction.
Findings From the Prodrome and “Extended Phenotype” of Schizophrenia
Another area of significant neurobiological research over recent years has focused on the early signs, or “prodrome,” of the illness and the subtler manifestations of symptoms within family members and the population at large. These groups are at increased risk of schizophrenia but have not yet developed the illness. Evidence from studying these groups therefore has the potential to provide information about the causal chain of events leading to the development of schizophrenia. Individuals meeting clinical criteria for a high risk of psychosis, eg, have an approximate 400-fold increased risk of developing of psychotic illnesses, predominantly schizophrenia, within the following few years.115,116 They show elevated striatal [18F]-dopa accumulation, which is positively associated with greater symptom severity and approaches the levels seen in patients with schizophrenia.20 Elevated presynaptic striatal dopaminergic function is also seen in other groups with an increased risk of developing psychosis, such as schizotypy,117,118 and the relatives of people with schizophrenia.119 The latter also show a greater change in dopamine metabolite levels in response to a given stressor than healthy controls120 and an association between greater change in dopamine metabolite levels with higher levels of psychotic-like symptoms following stress.121 These dopaminergic abnormalities appear intermediate to those seen in patients with schizophrenia,20,117,120 although this needs to be tested in adequately powered studies. Overall, these findings indicate that dopaminergic abnormalities are not just seen in people who are frankly psychotic but are also seen in people with risk factors for psychosis, who often have symptoms, albeit at a less severe level. Furthermore, stress in these individuals has been linked to both an increase in these symptoms and an increase in dopaminergic indices (see review by van et al70). This suggests that the dopaminergic abnormalities might underlie “psychosis proneness” and shows how the environment might further impact on this to lead to frank psychosis.
A further development since version II of the dopamine hypothesis is the evidence regarding structural differences prior to the onset of schizophrenia. Individuals with prodromal signs also show brain structural deficits, quite like those in patients, although to a lesser degree (see review by Wood et al122), as do the relatives of people with schizophrenia and people with schizotypal features123 (see review by Dickey et al124). These brain abnormalities are in frontotemporal regions—the same areas where lesions in animals result in striatal dopaminergic abnormalities.80,82,125 There is also evidence of longitudinal brain structural changes in schizophrenia (eg, DeLisi126 and van Haren et al127) and people at risk of schizophrenia.122,128 However, the contribution of factors such as medication129,130 and cannabis use131 to the longitudinal brain changes has yet to be fully resolved—as such these changes are not addressed in the proposed dopamine hypothesis: version III. It is not just brain structure that is altered in these individuals at risk of schizophrenia—there are functional differences as well that are generally in similar brain regions to those seen in schizophrenia (see reviews by Fusar-Poli et al132 and Lawrie et al133) and a similar pattern of neurocognitive impairments to those seen in schizophrenia, although again to a lesser degree (see review and subsequent studies by Brewer et al,134 Eastvold et al,135 and Simon et al136).
Parsimoniously, one can conclude that striatal dopaminergic elevation is present in a compromised brain in schizophrenia and that the same appears true in the “extended phenotype.” Furthermore, there is some evidence that the 2 are connected in the prodrome as well as in schizophrenia: greater striatal dopaminergic elevation in “prodromal individuals” is directly associated with poorer neurocognitive function and altered activation in frontal cortical areas during the task.20 There are also indications that there may be a gradation in the degree of dopaminergic elevation, although direct comparisons are required to substantiate this. Finally, recent studies in schizophrenia and its prodrome have begun to further localize the presynaptic dopamine elevation in the striatum to the parts functionally linked to associative cortical areas.20,137
Schizophrenia or Psychosis
The diagnosis of schizophrenia encapsulates patients with markedly different clinical features and courses (see reviews by Dutta et al138 and Peralta and Cuesta139). Classification systems have attempted to deal with this categorically by proposing subtypes and intermediate syndromes.138,139 On the other hand, factor analyses have identified a number of symptom dimensions: positive, negative, disorganized, affective, and cognitive, eg, Dutta et al138 and Peralta and Cuesta.139 The dominance and mix of the dimensions may fluctuate during the natural history of the illness.138,139 Additionally, many patients meet Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition) (DSM-IV) criteria for other psychiatric disorders as well.140 Despite this variability, it remains the fact that the vast majority of patients with schizophrenia come to clinical attention due to their psychosis. However, psychosis itself is not unique to schizophrenia. About 8% of the general population also report psychotic experiences, and in some 4% or so this is associated with impairment and distress (see review by van Os et al141). Thus, the distinction between clinical and subclinical psychosis may reflect interacting personal and sociocultural factors as much as it does biology.141
The paragraph above underlines that it would be highly implausible that any one biological factor could deterministically “explain” a diagnosis of schizophrenia. A much more likely scenario is that a biological dysfunction may contribute to one of the major dimensions of the illness. The evidence certainly suggests that striatal dopamine function appears most elevated in people who are acutely psychotic whether in the context of schizophrenia or psychosis seen in another condition. The dopamine dysfunction is present even in subjects reflecting the extended phenotype—family members, people with schizotypy, and symptomatic individuals at high risk of psychosis.20,117,119 Thus, the current evidence is consistent with dopamine hyperfunction being most closely linked to the dimension of psychosis. Insofar because psychosis is a hallmark of schizophrenia, dopamine abnormality is routinely seen in schizophrenia. However, we would predict that if nonpsychotic forms of schizophrenia were studied (and such a category is allowable under the DSM-IV), they would not show similar dopamine abnormalities—thus dissociating psychosis from schizophrenia.
Specificity of Presynaptic Striatal Dopamine Elevation to Schizophrenia or Psychosis
Striatal dopamine elevation is not seen in mania, depression, or other psychiatric disorders without psychosis142–147 and not related to measures of anxiety or depression in people with psychotic symptoms.20,148 Thus, it is not a nonspecific indicator of psychiatric morbidity. However, striatal dopamine elevation is seen in psychosis associated with psychosis in at least one disorder other than schizophrenia.22 Furthermore, dopamine blockade with antipsychotic drugs does not respect diagnostic boundaries either—it is effective for psychosis related to mania, depression, or Parkinson disease149,150 as well as for psychosis in schizophrenia. While further studies and direct comparisons are required, dopamine elevation appears specifically related more generally to psychosis proneness and not just to psychosis in schizophrenia.
Linking Dopamine Abnormalities to Clinical Expression of Schizophrenia
If a neurochemical hypothesis (based on dopamine or any other neurotransmitter) is to explain a psychiatric illness defined by its clinical expression, it has to link the 2. A major shortcoming of the first 2 versions of the dopamine hypothesis was the total silence on the issues of how dopaminergic abnormalities led to the clinical expression of the disease. Since version II of the dopamine hypothesis, developments in neuroscience have provided increasing evidence of dopamine's role in motivational incentive salience. The experiments and syntheses of data by Berridge and Robinson,151 Robbins and Everitt,152,153 and Schultz and others154–158 have implicated a distinct role for subcortical dopamine systems in incentive or motivational salience and reward prediction, respectively. These conceptualizations provided a framework to link neurochemical dysfunction to clinical expression using concepts of salience and reward. According to one such extension of the dopamine hypothesis,159,160 the abnormal firing of dopamine neurons and the abnormal release of dopamine leads to an aberrant assignment of salience to innocuous stimuli. It is argued that psychotic symptoms, especially delusions and hallucinations, emerge over time as the individual's own explanation of the experience of aberrant salience. Psychosis is, therefore, aberrant salience driven by dopamine and filtered through the individual's existing cognitive and sociocultural schemas—thus allowing the same chemical (dopamine) to have different clinical manifestations in different cultures and different individuals.159,160 Incentive salience models also provide a plausible explanation for negative symptoms: dopamine dysregulation may increase the noise in the system, “drowning out” dopaminergic signals linked to stimuli indicating reward, eg, Roiser et al161 and Seamans and Yang.162 The net result would be reduced motivational drive that would lead over time to negative symptoms, such as social withdrawal, and neglect of interests. As an explanation, this has face validity, and there is some evidence that schizophrenia is associated with reduced ventral striatal activation to reward, and greater reduction is related to higher levels of negative symptoms.163 However, this proposal and the hypothesis linking low frontal dopamine levels to the cognitive impairments in schizophrenia both need to be tested by further in vivo studies of neurochemical function in patients.
The Dopamine Hypothesis of Schizophrenia: Version III
We propose a revised “third version” of the dopamine hypothesis to account for the new evidence, drawing on the work of many previous reviews (eg, Laruelle and Abi-Dargham,32 van et al,70 Cannon et al,164 and Howes et al165). The hypothesis has 4 distinctive components.
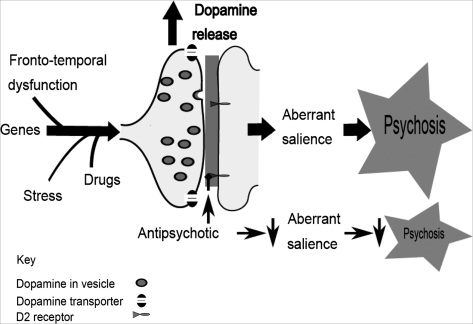
Firstly, we hypothesize that multiple “hits” interact to result in dopamine dysregulation—the final common pathway to psychosis in schizophrenia. This is illustrated schematically in figure 1. Second, the locus of dopamine dysregulation moves from being primarily at the D2 receptor level to being at the presynaptic dopaminergic control level. Third, dopamine dysregulation is linked to “psychosis” rather than schizophrenia, and perhaps in the fullness of time it will be about “psychosis proneness.” The exact diagnosis, however, reflects the nature of the hits coupled with sociocultural factors and not the dopamine dysfunction per se. And finally, the dopamine dysregulation is hypothesized to alter the appraisal of stimuli, perhaps through a process of aberrant salience.
Fig. 1.
Multiple hits interact to result in striatal dopamine dysregulation to alter the appraisal of stimuli and resulting in psychosis, whilst current antipsychotic drugs act downstream of the primary dopaminergic dysregulation.
Implications of the Dopamine Hypothesis of Schizophrenia: Version III
The hypothesis that the final common pathway is presynaptic dopamine dysregulation has some important clinical implications. Firstly, it implies that current antipsychotic drugs are not treating the primary abnormality and are acting downstream. While antipsychotic drugs block the effect of inappropriate dopamine release, they may paradoxically worsen the primary abnormality by blocking presynaptic D2 autoreceptors, resulting in a compensatory increase in dopamine synthesis. There is some evidence from healthy volunteers that acute antipsychotic treatment does increase presynaptic dopamine synthesis capacity,166 and while successful subacute treatment can reduce this,167 it is nevertheless elevated in patients who have received antipsychotic treatment for many years.17 This may explain why patients relapse rapidly on stopping their medication, and if the drugs may even worsen the primary abnormality, it also accounts for more severe relapse after discontinuing treatment. This suggests that drug development needs to focus on modulating presynaptic striatal dopamine function, either directly or through upstream effects.
What About the Other Dimensions of Schizophrenia in Version III?
An attractive feature of version II was that it proposed a dysfunction in the dopamine system as a complete explanation for schizophrenia: a prefrontal hypodopaminergia leading to a subcortical hyperdopaminergia. We depart from this parsimony in version III mainly because in the last 2 decades there has been little convincing evidence for this sequence of dopamine dysfunction. On the other hand, the last 2 decades have provided substantially more evidence about the multiple routes (genetic, neurodevelopmental, environmental, social) that lead to the striatal hyperdopaminergia, as discussed earlier. Furthermore, the appreciation of the dimensional nature of symptoms of schizophrenia also speaks for partial independence of the different features (cognitive, negative) from psychosis.139 There is of course correlational evidence that striatal dopamine abnormalities are associated with poor performance on cognitive tasks17,20,168 and suggestion that higher striatal dopamine synthesis capacity is linked to functional abnormalities in the cortical regions engaged by these tasks.168,169 However, it should be noted that recent data suggest that these frontal/cognitive changes need not necessarily be primary but instead may arise as a consequence of striatal dysfunction.170 Thus, in contrast to version II, which proposed a single pathway, we propose that changes in multiple transmitter/neural systems underlie the cognitive dysfunction and negative symptoms of schizophrenia, and in many cases these dysfunctions precede the onset of psychosis. It is when these pathways, in convergence with other biological or environmental influences, lead to striatal dopamine hyperfunction that psychosis becomes evident and the label of schizophrenia is assigned. Thus, rather than being a hypothesis of schizophrenia—version III is more accurately a “dopamine hypothesis of psychosis-in-schizophrenia.” It remains to be tested whether this is specific to psychosis of schizophrenia or is seen with psychosis in other disorders too.
What Would Lead to a Rejection of the Hypothesis?
Because so much is unknown, it is given that the hypothesis will be revised as more data become available. The more intriguing question is whether one can envisage evidence that would lead to a wholesale rejection of the hypothesis. The 2 central claims of version III are the primacy of the presynaptic abnormality and the claim that dopamine is the “final common pathway.” Two different kinds of evidence could lead to a complete rejection of the hypothesis. PET studies directly implicating presynaptic dopamine dysfunction are a major foundation of this new version of the hypothesis. PET data require to be modeled to provide estimates of L-dopa uptake or synaptic dopamine levels—and the results are inferred rather than direct measurements. Thus, if it turns out that the body of evidence based on PET imaging is a confound or an artifact of modeling and technical approaches, this would be a serious blow for version III, though the data behind versions I and II would still stand strong. While possible, we think this to be highly unlikely. What is perhaps more likely is that a new drug is found that treats psychosis without a direct effect on the dopamine system. In other words, the dopamine abnormalities continue unimpeded, and psychosis improves despite them. A good example of such a new drug might be LY2140023, an mGlu 2/3 agonist.171 If this were to be an effective antipsychotic and it could be shown that the new pathways do not show any interaction with the dopamine system, then the fundamental claim of version III, that it is the final common pathway, would be demolished. A similar situation would arise if a pathophysiological mechanism that does not impact on the dopamine system is found to be universal to schizophrenia. Much more likely is the possibility that the hypothesis will be revised but with a stronger version IV. The next decade will provide more information on the role of dopamine, particularly how genetic and environmental factors combine to influence the common pathway, and better drugs will be developed that directly influence presynaptic dopaminergic function—both logical successors to the idea of a final common pathway.
Conclusions
A considerable body of new evidence has amassed in the last 2 decades that is not compatible with reconceptualization of Davis and colleagues of the dopamine hypothesis of schizophrenia. To account for these developments, we have elaborated the dopamine hypothesis of schizophrenia: version III—the final common pathway. This hypothesis accounts for the multiple environmental and genetic risk factors for schizophrenia and proposes that these interact to funnel through one final common pathway of presynaptic striatal hyperdopaminergia. Furthermore, it provides a framework linking the abnormal neurochemistry to symptoms and explains both why many disparate risk factors and functional and structural abnormalities are associated with schizophrenia but are not specific to schizophrenia. It provides an explanation for overlapping findings in people with risk factors for schizophrenia and explains eventual diagnosis not in neurochemical terms but as the result of individual factors interacting with the sociocultural milieu. In addition to funneling through dopamine dysregulation, the multiple environmental and genetic risk factors influence diagnosis by affecting other aspects of brain function that underlie negative and cognitive symptoms. Schizophrenia is thus dopamine dysregulation in the context of a compromised brain. It follows from this that future drug development should focus on the systems acting on the funnel points leading to the final common pathway.
Acknowledgments
Howes has received investigator-led charitable research funds or speaking engagements from AstraZeneca, Eli Lilly, and Janssen. Kapur has received grant support or has been a consultant/scientific advisor or had speaking engagements with AstraZeneca, Bristol Meyers Squibb, Eli Lilly, EMD—Darmstadt, Glaxo Smith Kline, Janssen (Johnson and Johnson), Neuromolecular Inc, Pfizer, Otsuka, Organon, Sanofi-Synthelabo, Servier, and Solvay Wyeth.
References
- 1.Delay J, Deniker P, Harl JM. Therapeutic use in psychiatry of phenothiazine of central elective action (4560 RP) Ann Med Psychol (Paris) 1952;110:112–117. [PubMed] [Google Scholar]
- 2.Carlsson A, Lindqvist M. Effect of chlorpromazine or haloperidol on the formation of 3-methoxytyramine and normetanephrine in mouse brain. Acta Pharmacol Toxicol (Copenh) 1963;20:140–144. doi: 10.1111/j.1600-0773.1963.tb01730.x. [DOI] [PubMed] [Google Scholar]
- 3.Carlsson A, Lindqvist M, Magnusson T. 3,4-Dihydroxyphenylalanine and 5-hydroxytryptophan as reserpine antagonists. Nature. 1957;180:1200. doi: 10.1038/1801200a0. [DOI] [PubMed] [Google Scholar]
- 4.Lieberman JA, Kane JM, Alvir J. Provocative tests with psychostimulant drugs in schizophrenia. Psychopharmacology (Berl) 1987;91:415–433. doi: 10.1007/BF00216006. [DOI] [PubMed] [Google Scholar]
- 5.Seeman P, Lee T. Antipsychotic drugs: direct correlation between clinical potency and presynaptic action on dopamine neurons. Science. 1975;188:1217–1219. doi: 10.1126/science.1145194. [DOI] [PubMed] [Google Scholar]
- 6.Creese I, Burt DR, Snyder SH. Dopamine receptor binding predicts clinical and pharmacological potencies of antischizophrenic drugs. Science. 1976;192:481–483. doi: 10.1126/science.3854. [DOI] [PubMed] [Google Scholar]
- 7.Seeman P, Lee T, Chau-Wong M, Wong K. Antipsychotic drug doses and neuroleptic/dopamine receptors. Nature. 1976;261:717–719. doi: 10.1038/261717a0. [DOI] [PubMed] [Google Scholar]
- 8.Matthysse S. Antipsychotic drug actions: a clue to the neuropathology of schizophrenia? Fed Proc. 1973;32:200–205. [PubMed] [Google Scholar]
- 9.Snyder SH. The dopamine hypothesis of schizophrenia: focus on the dopamine receptor. Am J Psychiatry. 1976;133:197–202. doi: 10.1176/ajp.133.2.197. [DOI] [PubMed] [Google Scholar]
- 10.Davis KL, Kahn RS, Ko G, Davidson M. Dopamine in schizophrenia: a review and reconceptualization. Am J Psychiatry. 1991;148:1474–1486. doi: 10.1176/ajp.148.11.1474. [DOI] [PubMed] [Google Scholar]
- 11.Pycock CJ, Kerwin RW, Carter CJ. Effect of lesion of cortical dopamine terminals on subcortical dopamine receptors in rats. Nature. 1980;286:74–76. doi: 10.1038/286074a0. [DOI] [PubMed] [Google Scholar]
- 12.Scatton B, Worms P, Lloyd KG, Bartholini G. Cortical modulation of striatal function. Brain Res. 1982;232:331–343. doi: 10.1016/0006-8993(82)90277-3. [DOI] [PubMed] [Google Scholar]
- 13.Davidson LL, Heinrichs RW. Quantification of frontal and temporal lobe brain-imaging findings in schizophrenia: a meta-analysis. Psychiatry Res. 2003;122:69–87. doi: 10.1016/s0925-4927(02)00118-x. [DOI] [PubMed] [Google Scholar]
- 14.McGuire P, Howes OD, Stone J, Fusar-Poli P. Functional neuroimaging in schizophrenia: diagnosis and drug discovery. Trends Pharmacol Sci. 2008;29:91–98. doi: 10.1016/j.tips.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 15.Moore RY, Whone AL, McGowan S, Brooks DJ. Monoamine neuron innervation of the normal human brain: an 18F-DOPA PET study. Brain Res. 2003;982:137–145. doi: 10.1016/s0006-8993(03)02721-5. [DOI] [PubMed] [Google Scholar]
- 16.Meyer-Lindenberg A, Miletich RS, Kohn PD, et al. Reduced prefrontal activity predicts exaggerated striatal dopaminergic function in schizophrenia. Nat Neurosci. 2002;5:267–271. doi: 10.1038/nn804. [DOI] [PubMed] [Google Scholar]
- 17.McGowan S, Lawrence AD, Sales T, Quested D, Grasby P. Presynaptic dopaminergic dysfunction in schizophrenia: a positron emission tomographic [18F]fluorodopa study. Arch Gen Psychiatry. 2004;61:134–142. doi: 10.1001/archpsyc.61.2.134. [DOI] [PubMed] [Google Scholar]
- 18.Hietala J, Syvalahti E, Vuorio K, et al. Presynaptic dopamine function in striatum of neuroleptic-naive schizophrenic patients. Lancet. 1995;346:1130–1131. doi: 10.1016/s0140-6736(95)91801-9. [DOI] [PubMed] [Google Scholar]
- 19.Hietala J, Syvalahti E, Vilkman H, et al. Depressive symptoms and presynaptic dopamine function in neuroleptic-naive schizophrenia. Schizophr Res. 1999;35:41–50. doi: 10.1016/s0920-9964(98)00113-3. [DOI] [PubMed] [Google Scholar]
- 20.Howes OD, Montgomery AJ, Asselin MC, et al. Elevated striatal dopamine function linked to prodromal signs of schizophrenia. Arch Gen Psychiatry. 2008 doi: 10.1001/archgenpsychiatry.2008.514. [DOI] [PubMed] [Google Scholar]
- 21.Lindstrom LH, Gefvert O, Hagberg G, et al. Increased dopamine synthesis rate in medial prefrontal cortex and striatum in schizophrenia indicated by L-(beta-11C) DOPA and PET. Biol Psychiatry. 1999;46:681–688. doi: 10.1016/s0006-3223(99)00109-2. [DOI] [PubMed] [Google Scholar]
- 22.Reith J, Benkelfat C, Sherwin A, et al. Elevated dopa decarboxylase activity in living brain of patients with psychosis. Proc Natl Acad Sci U S A. 1994;91:11651–11654. doi: 10.1073/pnas.91.24.11651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Howes OD, Montgomery AJ, Asselin MC, Murray RM, Grasby PM, McGuire PK. Molecular imaging studies of the striatal dopaminergic system in psychosis and predictions for the prodromal phase of psychosis. Br J Psychiatry Suppl. 2007;51:s13–s18. doi: 10.1192/bjp.191.51.s13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dao-Castellana MH, Paillere-Martinot ML, Hantraye P, et al. Presynaptic dopaminergic function in the striatum of schizophrenic patients. Schizophr Res. 1997;23:167–174. doi: 10.1016/S0920-9964(96)00102-8. [DOI] [PubMed] [Google Scholar]
- 25.Elkashef AM, Doudet D, Bryant T, Cohen RM, Li SH, Wyatt RJ. 6-(18)F-DOPA PET study in patients with schizophrenia. Positron emission tomography. Psychiatry Res. 2000;100:1–11. doi: 10.1016/s0925-4927(00)00064-0. [DOI] [PubMed] [Google Scholar]
- 26.Laruelle M, Iyer RN, al-Tikriti MS, et al. Microdialysis and SPECT measurements of amphetamine-induced dopamine release in nonhuman primates. Synapse. 1997;25:1–14. doi: 10.1002/(SICI)1098-2396(199701)25:1<1::AID-SYN1>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 27.Laruelle M. Imaging synaptic neurotransmission with in vivo binding competition techniques: a critical review. J Cereb Blood Flow Metab. 2000;20:423–451. doi: 10.1097/00004647-200003000-00001. [DOI] [PubMed] [Google Scholar]
- 28.Abi-Dargham A, Gil R, Krystal J, et al. Increased striatal dopamine transmission in schizophrenia: confirmation in a second cohort. Am J Psychiatry. 1998;155:761–767. doi: 10.1176/ajp.155.6.761. [DOI] [PubMed] [Google Scholar]
- 29.Breier A, Su TP, Saunders R, et al. Schizophrenia is associated with elevated amphetamine-induced synaptic dopamine concentrations: evidence from a novel positron emission tomography method. Proc Natl Acad Sci U S A. 1997;94:2569–2574. doi: 10.1073/pnas.94.6.2569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kestler LP, Walker E, Vega EM. Dopamine receptors in the brains of schizophrenia patients: a meta-analysis of the findings. Behav Pharmacol. 2001;12:355–371. doi: 10.1097/00008877-200109000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Laruelle M, Abi-Dargham A, van Dyck CH, et al. Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic subjects. Proc Natl Acad Sci U S A. 1996;93:9235–9240. doi: 10.1073/pnas.93.17.9235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laruelle M, Abi-Dargham A. Dopamine as the wind of the psychotic fire: new evidence from brain imaging studies. J Psychopharmacol. 1999;13:358–371. doi: 10.1177/026988119901300405. [DOI] [PubMed] [Google Scholar]
- 33.Abi-Dargham A, Rodenhiser J, Printz D, et al. Increased baseline occupancy of D2 receptors by dopamine in schizophrenia. Proc Natl Acad Sci U S A. 2000;97:8104–8109. doi: 10.1073/pnas.97.14.8104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crawley JC, Crow TJ, Johnstone EC, et al. Uptake of 77Br-spiperone in the striata of schizophrenic patients and controls. Nucl Med Commun. 1986;7:599–607. doi: 10.1097/00006231-198608000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Gjedde A, Wong DF. Positron tomographic quantitation of neuroreceptors in human brain in vivo–with special reference to the D2 dopamine receptors in caudate nucleus. Neurosurg Rev. 1987;10:9–18. doi: 10.1007/BF01780587. [DOI] [PubMed] [Google Scholar]
- 36.Wong DF, Wagner HN, Jr, Tune LE, et al. Positron emission tomography reveals elevated D2 dopamine receptors in drug-naive schizophrenics. Science. 1986 19;234:1558–1563. doi: 10.1126/science.2878495. [DOI] [PubMed] [Google Scholar]
- 37.Farde L, Wiesel FA, Stone-Elander S, et al. D2 dopamine receptors in neuroleptic-naive schizophrenic patients. A positron emission tomography study with [11C]raclopride. Arch Gen Psychiatry. 1990;47:213–219. doi: 10.1001/archpsyc.1990.01810150013003. [DOI] [PubMed] [Google Scholar]
- 38.Martinot JL, Peron-Magnan P, Huret JD, et al. Striatal D2 dopaminergic receptors assessed with positron emission tomography and [76Br]bromospiperone in untreated schizophrenic patients. Am J Psychiatry. 1990;147:44–50. doi: 10.1176/ajp.147.1.44. [DOI] [PubMed] [Google Scholar]
- 39.Laruelle M. Imaging dopamine transmission in schizophrenia. A review and meta-analysis. Q J Nucl Med. 1998;42:211–221. [PubMed] [Google Scholar]
- 40.Zakzanis KK, Hansen KT. Dopamine D2 densities and the schizophrenic brain. Schizophr Res. 1998;32:201–206. doi: 10.1016/s0920-9964(98)00041-3. [DOI] [PubMed] [Google Scholar]
- 41.Okubo Y, Suhara T, Suzuki K, et al. Decreased prefrontal dopamine D1 receptors in schizophrenia revealed by PET. Nature. 1997;385:634–636. doi: 10.1038/385634a0. [DOI] [PubMed] [Google Scholar]
- 42.Karlsson P, Farde L, Halldin C, Sedvall G. PET study of D(1) dopamine receptor binding in neuroleptic-naive patients with schizophrenia. Am J Psychiatry. 2002;159:761–767. doi: 10.1176/appi.ajp.159.5.761. [DOI] [PubMed] [Google Scholar]
- 43.Talvik M, Nordstrom AL, Okubo Y, et al. Dopamine D2 receptor binding in drug-naive patients with schizophrenia examined with raclopride-C11 and positron emission tomography. Psychiatry Res. 2006;148:165–173. doi: 10.1016/j.pscychresns.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 44.Buchsbaum MS, Christian BT, Lehrer DS, et al. D2/D3 dopamine receptor binding with [F-18]fallypride in thalamus and cortex of patients with schizophrenia. Schizophr Res. 2006;85:232–244. doi: 10.1016/j.schres.2006.03.042. [DOI] [PubMed] [Google Scholar]
- 45.Suhara T, Okubo Y, Yasuno F, et al. Decreased dopamine D2 receptor binding in the anterior cingulate cortex in schizophrenia. Arch Gen Psychiatry. 2002;59:25–30. doi: 10.1001/archpsyc.59.1.25. [DOI] [PubMed] [Google Scholar]
- 46.Takahashi H, Higuchi M, Suhara T. The role of extrastriatal dopamine D2 receptors in schizophrenia. Biol Psychiatry. 2006;59:919–928. doi: 10.1016/j.biopsych.2006.01.022. [DOI] [PubMed] [Google Scholar]
- 47.Seeman P, Schwarz J, Chen JF, et al. Psychosis pathways converge via D2high dopamine receptors. Synapse. 2006;60:319–346. doi: 10.1002/syn.20303. [DOI] [PubMed] [Google Scholar]
- 48.Graf-Guerrero A, Romina M, Agid O, et al. The dopamine D2 receptors in high-affinity state and D3 receptors in schizophrenia: a clinical [11C]-(+)-PHNO PET study. Neuropsychopharmacology. 2009;34:1078–1086. doi: 10.1038/npp.2008.199. [DOI] [PubMed] [Google Scholar]
- 49.Goldman-Rakic PS, Castner SA, Svensson TH, Siever LJ, Williams GV. Targeting the dopamine D1 receptor in schizophrenia: insights for cognitive dysfunction. Psychopharmacology (Berl) 2004;174:3–16. doi: 10.1007/s00213-004-1793-y. [DOI] [PubMed] [Google Scholar]
- 50.Tamminga CA. The neurobiology of cognition in schizophrenia. J Clin Psychiatry. 2006;67:e11. [PubMed] [Google Scholar]
- 51.Abi-Dargham A, Mawlawi O, Lombardo I, et al. Prefrontal dopamine D1 receptors and working memory in schizophrenia. J Neurosci. 2002;22:3708–3719. doi: 10.1523/JNEUROSCI.22-09-03708.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Guo N, Hwang DR, Lo ES, Huang YY, Laruelle M, bi-Dargham A. Dopamine depletion and in vivo binding of PET D1 receptor radioligands: implications for imaging studies in schizophrenia. Neuropsychopharmacology. 2003;28:1703–1711. doi: 10.1038/sj.npp.1300224. [DOI] [PubMed] [Google Scholar]
- 53.Ekelund J, Slifstein M, Narendran R, et al. In vivo DA D(1) receptor selectivity of NNC 112 and SCH 23390. Mol Imaging Biol. 2007;9:117–125. doi: 10.1007/s11307-007-0077-4. [DOI] [PubMed] [Google Scholar]
- 54.Frankle WG, Laruelle M. Neuroreceptor imaging in psychiatric disorders. Ann Nucl Med. 2002;16:437–446. doi: 10.1007/BF02988639. [DOI] [PubMed] [Google Scholar]
- 55.Kapur S, Zipursky R, Jones C, Remington G, Houle S. Relationship between dopamine D(2) occupancy, clinical response, and side effects: a double-blind PET study of first-episode schizophrenia. Am J Psychiatry. 2000;157:514–520. doi: 10.1176/appi.ajp.157.4.514. [DOI] [PubMed] [Google Scholar]
- 56.Nordstrom AL, Farde L, Wiesel FA, et al. Central D2-dopamine receptor occupancy in relation to antipsychotic drug effects: a double-blind PET study of schizophrenic patients. Biol Psychiatry. 1993;33:227–235. doi: 10.1016/0006-3223(93)90288-o. [DOI] [PubMed] [Google Scholar]
- 57.Wolkin A, Barouche F, Wolf AP, et al. Dopamine blockade and clinical response: evidence for two biological subgroups of schizophrenia. Am J Psychiatry. 1989;146:905–908. doi: 10.1176/ajp.146.7.905. [DOI] [PubMed] [Google Scholar]
- 58.Grace AA, Bunney BS, Moore H, Todd CL. Dopamine-cell depolarization block as a model for the therapeutic actions of antipsychotic drugs. Trends Neurosci. 1997;20:31–37. doi: 10.1016/S0166-2236(96)10064-3. [DOI] [PubMed] [Google Scholar]
- 59.Kapur S, Arenovich T, Agid O, Zipursky R, Lindborg S, Jones B. Evidence for onset of antipsychotic effects within the first 24 hours of treatment. Am J Psychiatry. 2005;162:939–946. doi: 10.1176/appi.ajp.162.5.939. [DOI] [PubMed] [Google Scholar]
- 60.Leucht S, Busch R, Hamann J, Kissling W, Kane JM. Early-onset hypothesis of antipsychotic drug action: a hypothesis tested, confirmed and extended. Biol Psychiatry. 2005;57:1543–1549. doi: 10.1016/j.biopsych.2005.02.023. [DOI] [PubMed] [Google Scholar]
- 61.Agid O, Mamo D, Ginovart N, et al. Striatal vs extrastriatal dopamine D2 receptors in antipsychotic response–a double-blind PET study in schizophrenia. Neuropsychopharmacology. 2007;32:1209–1215. doi: 10.1038/sj.npp.1301242. [DOI] [PubMed] [Google Scholar]
- 62.Catafau AM, Corripio I, Perez V, et al. Dopamine D2 receptor occupancy by risperidone: implications for the timing and magnitude of clinical response. Psychiatry Res. 2006;148:175–183. doi: 10.1016/j.pscychresns.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 63.Allen NC, Bagade S, McQueen MB, et al. Systematic meta-analyses and field synopsis of genetic association studies in schizophrenia: the SzGene database. Nat Genet. 2008;40:827–834. doi: 10.1038/ng.171. [DOI] [PubMed] [Google Scholar]
- 64.Shi J, Gershon ES, Liu C. Genetic associations with schizophrenia: meta-analyses of 12 candidate genes. Schizophr Res. 2008;104:96–107. doi: 10.1016/j.schres.2008.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Stefansson H, Rujescu D, Cichon S, et al. Large recurrent microdeletions associated with schizophrenia. Nature. 2008;455:232–236. doi: 10.1038/nature07229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rare chromosomal deletions and duplications increase risk of schizophrenia. Nature. 2008;455:237–241. doi: 10.1038/nature07239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.O'Donovan MC, Craddock N, Norton N, et al. Identification of loci associated with schizophrenia by genome-wide association and follow-up. Nat Genet. 2008 doi: 10.1038/ng.201. [DOI] [PubMed] [Google Scholar]
- 68.Talkowski ME, Kirov G, Bamne M, et al. A network of dopaminergic gene variations implicated as risk factors for schizophrenia. Hum Mol Genet. 2008;17:747–758. doi: 10.1093/hmg/ddm347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cantor-Graae E. The contribution of social factors to the development of schizophrenia: a review of recent findings. Can J Psychiatry. 2007;52:277–286. doi: 10.1177/070674370705200502. [DOI] [PubMed] [Google Scholar]
- 70.van WR, Stefanis NC, Myin-Germeys I. Psychosocial stress and psychosis. A review of the neurobiological mechanisms and the evidence for gene-stress interaction. Schizophr Bull. 2008 doi: 10.1093/schbul/sbn101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hall FS, Wilkinson LS, Humby T, et al. Isolation rearing in rats: pre- and postsynaptic changes in striatal dopaminergic systems. Pharmacol Biochem Behav. 1998;59:859–872. doi: 10.1016/s0091-3057(97)00510-8. [DOI] [PubMed] [Google Scholar]
- 72.Hall FS, Wilkinson LS, Humby T, Robbins TW. Maternal deprivation of neonatal rats produces enduring changes in dopamine function. Synapse. 1999;32:37–43. doi: 10.1002/(SICI)1098-2396(199904)32:1<37::AID-SYN5>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 73.Morgan D, Grant KA, Gage HD, et al. Social dominance in monkeys: dopamine D2 receptors and cocaine self-administration. Nat Neurosci. 2002;5:169–174. doi: 10.1038/nn798. [DOI] [PubMed] [Google Scholar]
- 74.Tidey JW, Miczek KA. Social defeat stress selectively alters mesocorticolimbic dopamine release: an in vivo microdialysis study. Brain Res. 1996;721:140–149. doi: 10.1016/0006-8993(96)00159-x. [DOI] [PubMed] [Google Scholar]
- 75.Cannon M, Jones PB, Murray RM. Obstetric complications and schizophrenia: historical and meta-analytic review. Am J Psychiatry. 2002;159:1080–1092. doi: 10.1176/appi.ajp.159.7.1080. [DOI] [PubMed] [Google Scholar]
- 76.Geddes JR, Lawrie SM. Obstetric complications and schizophrenia: a meta-analysis. Br J Psychiatry. 1995;167:786–793. doi: 10.1192/bjp.167.6.786. [DOI] [PubMed] [Google Scholar]
- 77.Kunugi H, Nanko S, Murray RM. Obstetric complications and schizophrenia: prenatal underdevelopment and subsequent neurodevelopmental impairment. Br J Psychiatry Suppl. 2001;40:s25–s29. doi: 10.1192/bjp.178.40.s25. [DOI] [PubMed] [Google Scholar]
- 78.Boksa P, El-Khodor BF. Birth insult interacts with stress at adulthood to alter dopaminergic function in animal models: possible implications for schizophrenia and other disorders. Neurosci Biobehav Rev. 2003;27:91–101. doi: 10.1016/s0149-7634(03)00012-5. [DOI] [PubMed] [Google Scholar]
- 79.Boksa P. Animal models of obstetric complications in relation to schizophrenia. Brain Res Brain Res Rev. 2004;45:1–17. doi: 10.1016/j.brainresrev.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 80.Lipska BK, Jaskiw GE, Weinberger DR. Postpubertal emergence of hyperresponsiveness to stress and to amphetamine after neonatal excitotoxic hippocampal damage: a potential animal model of schizophrenia. Neuropsychopharmacology. 1993;9:67–75. doi: 10.1038/npp.1993.44. [DOI] [PubMed] [Google Scholar]
- 81.Lipska BK, Halim ND, Segal PN, Weinberger DR. Effects of reversible inactivation of the neonatal ventral hippocampus on behavior in the adult rat. J Neurosci. 2002;22:2835–2842. doi: 10.1523/JNEUROSCI.22-07-02835.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Flores G, Wood GK, Liang JJ, Quirion R, Srivastava LK. Enhanced amphetamine sensitivity and increased expression of dopamine D2 receptors in postpubertal rats after neonatal excitotoxic lesions of the medial prefrontal cortex. J Neurosci. 1996;16:7366–7375. doi: 10.1523/JNEUROSCI.16-22-07366.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Diaz R, Ogren SO, Blum M, Fuxe K. Prenatal corticosterone increases spontaneous and d-amphetamine induced locomotor activity and brain dopamine metabolism in prepubertal male and female rats. Neuroscience. 1995;66:467–473. doi: 10.1016/0306-4522(94)00605-5. [DOI] [PubMed] [Google Scholar]
- 84.Henry C, Guegant G, Cador M, et al. Prenatal stress in rats facilitates amphetamine-induced sensitization and induces long-lasting changes in dopamine receptors in the nucleus accumbens. Brain Res. 1995;685:179–186. doi: 10.1016/0006-8993(95)00430-x. [DOI] [PubMed] [Google Scholar]
- 85.Fortier ME, Joober R, Luheshi GN, Boksa P. Maternal exposure to bacterial endotoxin during pregnancy enhances amphetamine-induced locomotion and startle responses in adult rat offspring. J Psychiatr Res. 2004;38:335–345. doi: 10.1016/j.jpsychires.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 86.Watanabe M, Nonaka R, Hagino Y, Kodama Y. Effects of prenatal methylazoxymethanol treatment on striatal dopaminergic systems in rat brain. Neurosci Res. 1998;30:135–144. doi: 10.1016/s0168-0102(97)00123-5. [DOI] [PubMed] [Google Scholar]
- 87.Kehoe P, Shoemaker WJ, Triano L, Hoffman J, Arons C. Repeated isolation in the neonatal rat produces alterations in behavior and ventral striatal dopamine release in the juvenile after amphetamine challenge. Behav Neurosci. 1996;110:1435–1444. doi: 10.1037//0735-7044.110.6.1435. [DOI] [PubMed] [Google Scholar]
- 88.Kehoe P, Clash K, Skipsey K, Shoemaker WJ. Brain dopamine response in isolated 10-day-old rats: assessment using D2 binding and dopamine turnover. Pharmacol Biochem Behav. 1996;53:41–49. doi: 10.1016/0091-3057(95)00196-4. [DOI] [PubMed] [Google Scholar]
- 89.Angrist BM, Gershon S. The phenomenology of experimentally induced amphetamine psychosis–preliminary observations. Biol Psychiatry. 1970;2:95–107. [PubMed] [Google Scholar]
- 90.Yui K, Ikemoto S, Ishiguro T, Goto K. Studies of amphetamine or methamphetamine psychosis in Japan: relation of methamphetamine psychosis to schizophrenia. Ann N Y Acad Sci. 2000;914:1–12. doi: 10.1111/j.1749-6632.2000.tb05178.x. [DOI] [PubMed] [Google Scholar]
- 91.Boileau I, Dagher A, Leyton M, et al. Modeling sensitization to stimulants in humans: an [11C]raclopride/positron emission tomography study in healthy men. Arch Gen Psychiatry. 2006;63:1386–1395. doi: 10.1001/archpsyc.63.12.1386. [DOI] [PubMed] [Google Scholar]
- 92.Arseneault L, Cannon M, Witton J, Murray RM. Causal association between cannabis and psychosis: examination of the evidence. Br J Psychiatry. 2004;184:110–117. doi: 10.1192/bjp.184.2.110. [DOI] [PubMed] [Google Scholar]
- 93.Moore TH, Zammit S, Lingford-Hughes A, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370:319–328. doi: 10.1016/S0140-6736(07)61162-3. [DOI] [PubMed] [Google Scholar]
- 94.Freund TF, Katona I, Piomelli D. Role of endogenous cannabinoids in synaptic signaling. Physiol Rev. 2003;83:1017–1066. doi: 10.1152/physrev.00004.2003. [DOI] [PubMed] [Google Scholar]
- 95.Cheer JF, Wassum KM, Heien ML, Phillips PE, Wightman RM. Cannabinoids enhance subsecond dopamine release in the nucleus accumbens of awake rats. J Neurosci. 2004;24:4393–4400. doi: 10.1523/JNEUROSCI.0529-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tanda G, Pontieri FE, Di CG. Cannabinoid and heroin activation of mesolimbic dopamine transmission by a common mu1 opioid receptor mechanism. Science. 1997;276:2048–2050. doi: 10.1126/science.276.5321.2048. [DOI] [PubMed] [Google Scholar]
- 97.Bossong MG, van Berckel BN, Boellaard R, et al. Delta9-tetrahydrocannabinol induces dopamine release in the human striatum. Neuropsychopharmacology. 2008 doi: 10.1038/npp.2008.138. [DOI] [PubMed] [Google Scholar]
- 98.Bowers MB, Kantrowitz JT. Elevated plasma dopamine metabolites in cannabis psychosis. Am J Psychiatry. 2007;164:1615–1616. doi: 10.1176/appi.ajp.2007.07010217. [DOI] [PubMed] [Google Scholar]
- 99.Kegeles LS, Abi-Dargham A, Zea-Ponce Y, et al. Modulation of amphetamine-induced striatal dopamine release by ketamine in humans: implications for schizophrenia. Biol Psychiatry. 2000;48:627–640. doi: 10.1016/s0006-3223(00)00976-8. [DOI] [PubMed] [Google Scholar]
- 100.Cannon TD, van Erp TG, Rosso IM, et al. Fetal hypoxia and structural brain abnormalities in schizophrenic patients, their siblings, and controls. Arch Gen Psychiatry. 2002;59:35–41. doi: 10.1001/archpsyc.59.1.35. [DOI] [PubMed] [Google Scholar]
- 101.Nicodemus KK, Marenco S, Batten AJ, et al. Serious obstetric complications interact with hypoxia-regulated/vascular-expression genes to influence schizophrenia risk. Mol Psychiatry. 2008;13:873–877. doi: 10.1038/sj.mp.4002153. [DOI] [PubMed] [Google Scholar]
- 102.Mittal VA, Ellman LM, Cannon TD. Gene-environment interaction and covariation in schizophrenia: the role of obstetric complications. Schizophr Bull. 2008 doi: 10.1093/schbul/sbn080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.van Os J, Rutten BP, Poulton R. Gene-environment interactions in schizophrenia: review of epidemiological findings and future directions. Schizophr Bull. 2008;34:1066–1082. doi: 10.1093/schbul/sbn117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Howes SR, Dalley JW, Morrison CH, Robbins TW, Everitt BJ. Leftward shift in the acquisition of cocaine self-administration in isolation-reared rats: relationship to extracellular levels of dopamine, serotonin and glutamate in the nucleus accumbens and amygdala-striatal FOS expression. Psychopharmacology (Berl) 2000;151:55–63. doi: 10.1007/s002130000451. [DOI] [PubMed] [Google Scholar]
- 105.Jones GH. Social isolation and individual differences: behavioural and dopaminergic responses to psychomotor stimulants. Clin Neuropharmacol. 1992;15(suppl 1, pt A):253A–254A. doi: 10.1097/00002826-199201001-00132. [DOI] [PubMed] [Google Scholar]
- 106.Fulford AJ, Marsden CA. Effect of isolation-rearing on conditioned dopamine release in vivo in the nucleus accumbens of the rat. J Neurochem. 1998;70:384–390. doi: 10.1046/j.1471-4159.1998.70010384.x. [DOI] [PubMed] [Google Scholar]
- 107.Pruessner JC, Champagne F, Meaney MJ, Dagher A. Dopamine release in response to a psychological stress in humans and its relationship to early life maternal care: a positron emission tomography study using [11C]raclopride. J Neurosci. 2004;24:2825–2831. doi: 10.1523/JNEUROSCI.3422-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kegeles LS, Martinez D, Kochan LD, et al. NMDA antagonist effects on striatal dopamine release: positron emission tomography studies in humans. Synapse. 2002;43:19–29. doi: 10.1002/syn.10010. [DOI] [PubMed] [Google Scholar]
- 109.Wassef A, Baker J, Kochan LD. GABA and schizophrenia: a review of basic science and clinical studies. J Clin Psychopharmacol. 2003;23:601–640. doi: 10.1097/01.jcp.0000095349.32154.a5. [DOI] [PubMed] [Google Scholar]
- 110.Caspi A, Moffitt TE, Cannon M, et al. Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene X environment interaction. Biol Psychiatry. 2005;57:1117–1127. doi: 10.1016/j.biopsych.2005.01.026. [DOI] [PubMed] [Google Scholar]
- 111.van Os J, Pedersen CB, Mortensen PB. Confirmation of synergy between urbanicity and familial liability in the causation of psychosis. Am J Psychiatry. 2004;161:2312–2314. doi: 10.1176/appi.ajp.161.12.2312. [DOI] [PubMed] [Google Scholar]
- 112.van Os J, Hanssen M, Bak M, Bijl RV, Vollebergh W. Do urbanicity and familial liability coparticipate in causing psychosis? Am J Psychiatry. 2003;160:477–482. doi: 10.1176/appi.ajp.160.3.477. [DOI] [PubMed] [Google Scholar]
- 113.Cantor-Graae E, Selten JP. Schizophrenia and migration: a meta-analysis and review. Am J Psychiatry. 2005;162:12–24. doi: 10.1176/appi.ajp.162.1.12. [DOI] [PubMed] [Google Scholar]
- 114.McKetin R, McLaren J, Lubman DI, Hides L. The prevalence of psychotic symptoms among methamphetamine users. Addiction. 2006;101:1473–1478. doi: 10.1111/j.1360-0443.2006.01496.x. [DOI] [PubMed] [Google Scholar]
- 115.Cannon TD, Cadenhead K, Cornblatt B, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65:28–37. doi: 10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Yung AR. Psychosis prediction: 12-month follow up of a high-risk (“prodromal”) group. 2003 doi: 10.1016/s0920-9964(02)00167-6. [DOI] [PubMed] [Google Scholar]
- 117.Abi-Dargham A, Kegeles LS, Zea-Ponce Y, et al. Striatal amphetamine-induced dopamine release in patients with schizotypal personality disorder studied with single photon emission computed tomography and [123I]iodobenzamide. Biol Psychiatry. 2004;55:1001–1006. doi: 10.1016/j.biopsych.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 118.Soliman A, O'Driscoll GA, Pruessner J, et al. Stress-induced dopamine release in humans at risk of psychosis: a [(11)C]raclopride PET study. Neuropsychopharmacology. 2008;33:2033–2041. doi: 10.1038/sj.npp.1301597. [DOI] [PubMed] [Google Scholar]
- 119.Huttunen J, Heinimaa M, Svirskis T, et al. Striatal dopamine synthesis in first-degree relatives of patients with schizophrenia. Biol Psychiatry. 2007 doi: 10.1016/j.biopsych.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 120.Brunelin J, d'Amato T, van Os J, Cochet A, Suaud-Chagny MF, Saoud M. Effects of acute metabolic stress on the dopaminergic and pituitary-adrenal axis activity in patients with schizophrenia, their unaffected siblings and controls. Schizophr Res. 2008;100:206–211. doi: 10.1016/j.schres.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 121.Myin-Germeys I, Marcelis M, Krabbendam L, Delespaul P, van Os J. Subtle fluctuations in psychotic phenomena as functional states of abnormal dopamine reactivity in individuals at risk. Biol Psychiatry. 2005;58:105–110. doi: 10.1016/j.biopsych.2005.02.012. [DOI] [PubMed] [Google Scholar]
- 122.Wood SJ, Pantelis C, Velakoulis D, Yucel M, Fornito A, McGorry PD. Progressive changes in the development toward schizophrenia: studies in subjects at increased symptomatic risk. Schizophr Bull. 2008;34:322–329. doi: 10.1093/schbul/sbm149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Boos HB, Aleman A, Cahn W, Pol HH, Kahn RS. Brain volumes in relatives of patients with schizophrenia: a meta-analysis. Arch Gen Psychiatry. 2007;64:297–304. doi: 10.1001/archpsyc.64.3.297. [DOI] [PubMed] [Google Scholar]
- 124.Dickey CC, McCarley RW, Shenton ME. The brain in schizotypal personality disorder: a review of structural MRI and CT findings. Harv Rev Psychiatry. 2002;10:1–15. doi: 10.1080/10673220216201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lodge DJ, Grace AA. Aberrant hippocampal activity underlies the dopamine dysregulation in an animal model of schizophrenia. J Neurosci. 2007;27:11424–11430. doi: 10.1523/JNEUROSCI.2847-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.DeLisi LE. The concept of progressive brain change in schizophrenia: implications for understanding schizophrenia. Schizophr Bull. 2008;34:312–321. doi: 10.1093/schbul/sbm164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.van Haren NE, Hulshoff Pol HE, Schnack HG, et al. Focal gray matter changes in schizophrenia across the course of the illness: a 5-year follow-up study. Neuropsychopharmacology. 2007;32:2057–2066. doi: 10.1038/sj.npp.1301347. [DOI] [PubMed] [Google Scholar]
- 128.Brans RG, van Haren NE, van Baal GC, Schnack HG, Kahn RS, Hulshoff Pol HE. Heritability of changes in brain volume over time in twin pairs discordant for schizophrenia. Arch Gen Psychiatry. 2008;65:1259–1268. doi: 10.1001/archpsyc.65.11.1259. [DOI] [PubMed] [Google Scholar]
- 129.Lieberman JA, Tollefson GD, Charles C, et al. Antipsychotic drug effects on brain morphology in first-episode psychosis. Arch Gen Psychiatry. 2005;62:361–370. doi: 10.1001/archpsyc.62.4.361. [DOI] [PubMed] [Google Scholar]
- 130.Konopaske GT, Dorph-Petersen KA, Pierri JN, Wu Q, Sampson AR, Lewis DA. Effect of chronic exposure to antipsychotic medication on cell numbers in the parietal cortex of macaque monkeys. Neuropsychopharmacology. 2007;32:1216–1223. doi: 10.1038/sj.npp.1301233. [DOI] [PubMed] [Google Scholar]
- 131.Rais M, Cahn W, Van HN, et al. Excessive brain volume loss over time in cannabis-using first-episode schizophrenia patients. Am J Psychiatry. 2008;165:490–496. doi: 10.1176/appi.ajp.2007.07071110. [DOI] [PubMed] [Google Scholar]
- 132.Fusar-Poli P, Perez J, Broome M, et al. Neurofunctional correlates of vulnerability to psychosis: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2007;31:465–484. doi: 10.1016/j.neubiorev.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 133.Lawrie SM, McIntosh AM, Hall J, Owens DG, Johnstone EC. Brain structure and function changes during the development of schizophrenia: the evidence from studies of subjects at increased genetic risk. Schizophr Bull. 2008;34:330–340. doi: 10.1093/schbul/sbm158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Brewer WJ, Wood SJ, Phillips LJ, et al. Generalized and specific cognitive performance in clinical high-risk cohorts: a review highlighting potential vulnerability markers for psychosis. Schizophr Bull. 2006;32:538–555. doi: 10.1093/schbul/sbj077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Eastvold AD, Heaton RK, Cadenhead KS. Neurocognitive deficits in the (putative) prodrome and first episode of psychosis. Schizophr Res. 2007;93:266–277. doi: 10.1016/j.schres.2007.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Simon AE, Cattapan-Ludewig K, Zmilacher S, et al. Cognitive functioning in the schizophrenia prodrome. Schizophr Bull. 2007;33:761–771. doi: 10.1093/schbul/sbm018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Laruelle M. Schizophrenia is associated with increased synaptic dopamine in associative rather than limbic regions of the striatum: implications for the mechanisms of actions of antipsychotic drugs. Schizophr Res. 2006;81:16. [Google Scholar]
- 138.Dutta R, Greene T, Addington J, McKenzie K, Phillips M, Murray RM. Biological, life course, and cross-cultural studies all point toward the value of dimensional and developmental ratings in the classification of psychosis. Schizophr Bull. 2007;33:868–876. doi: 10.1093/schbul/sbm059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Peralta V, Cuesta MJ. How many and which are the psychopathological dimensions in schizophrenia? Issues influencing their ascertainment. Schizophr Res. 2001;49:269–285. doi: 10.1016/s0920-9964(00)00071-2. [DOI] [PubMed] [Google Scholar]
- 140.Kessler RC, Birnbaum H, Demler O, et al. The prevalence and correlates of nonaffective psychosis in the National Comorbidity Survey Replication (NCS-R) Biol Psychiatry. 2005;58:668–676. doi: 10.1016/j.biopsych.2005.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2008:1–17. doi: 10.1017/S0033291708003814. [DOI] [PubMed] [Google Scholar]
- 142.Yatham LN, Liddle PF, Shiah IS, et al. PET study of [(18)F]6-fluoro-L-dopa uptake in neuroleptic- and mood-stabilizer-naive first-episode nonpsychotic mania: effects of treatment with divalproex sodium. Am J Psychiatry. 2002;159:768–774. doi: 10.1176/appi.ajp.159.5.768. [DOI] [PubMed] [Google Scholar]
- 143.Martinot M, Bragulat V, Artiges E, et al. Decreased presynaptic dopamine function in the left caudate of depressed patients with affective flattening and psychomotor retardation. Am J Psychiatry. 2001;158:314–316. doi: 10.1176/appi.ajp.158.2.314. [DOI] [PubMed] [Google Scholar]
- 144.Parsey RV, Oquendo MA, Zea-Ponce Y, et al. Dopamine D(2) receptor availability and amphetamine-induced dopamine release in unipolar depression. Biol Psychiatry. 2001;50:313–322. doi: 10.1016/s0006-3223(01)01089-7. [DOI] [PubMed] [Google Scholar]
- 145.Reith J, Benkelfat C, Sherwin A, et al. Elevated dopa decarboxylase activity in living brain of patients with psychosis. Proc Natl Acad Sci U S A. 1994;91:11651–11654. doi: 10.1073/pnas.91.24.11651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Turjanski N, Sawle GV, Playford ED, et al. PET studies of the presynaptic and postsynaptic dopaminergic system in Tourette's syndrome. J Neurol Neurosurg Psychiatry. 1994;57:688–692. doi: 10.1136/jnnp.57.6.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Ernst M, Zametkin AJ, Matochik JA, Pascualvaca D, Cohen RM. Low medial prefrontal dopaminergic activity in autistic children. Lancet. 1997;350:638. doi: 10.1016/s0140-6736(05)63326-0. [DOI] [PubMed] [Google Scholar]
- 148.Laruelle M, Abi-Dargham A, Gil R, Kegeles L, Innis R. Increased dopamine transmission in schizophrenia: relationship to illness phases. Biol Psychiatry. 1999;46:56–72. doi: 10.1016/s0006-3223(99)00067-0. [DOI] [PubMed] [Google Scholar]
- 149.Dannon PN, Lowengrub K, Gonopolski Y, Kotler M. Current and emerging somatic treatment strategies in psychotic major depression. Expert Rev Neurother. 2006;6:73–80. doi: 10.1586/14737175.6.1.73. [DOI] [PubMed] [Google Scholar]
- 150.Zahodne LB, Fernandez HH. Pathophysiology and treatment of psychosis in Parkinson's disease: a review. Drugs Aging. 2008;25:665–682. doi: 10.2165/00002512-200825080-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Berridge KC, Robinson TE. What is the role of dopamine in reward: hedonic impact, reward learning, or incentive salience? Brain Res Brain Res Rev. 1998;28:309–69. doi: 10.1016/s0165-0173(98)00019-8. [DOI] [PubMed] [Google Scholar]
- 152.Robbins TW, Everitt BJ. Functional studies of the central catecholamines. Int Rev Neurobiol. 1982;23:303–365. doi: 10.1016/s0074-7742(08)60628-5. [DOI] [PubMed] [Google Scholar]
- 153.Robbins TW, Everitt BJ. Neurobehavioural mechanisms of reward and motivation. Curr Opin Neurobiol. 1996;6:228–236. doi: 10.1016/s0959-4388(96)80077-8. [DOI] [PubMed] [Google Scholar]
- 154.Heinz A. Anhedonia–a general nosology surmounting correlate of a dysfunctional dopaminergic reward system? Nervenarzt. 1999;70:391–398. doi: 10.1007/s001150050454. [DOI] [PubMed] [Google Scholar]
- 155.Martin-Soelch C, Leenders KL, Chevalley AF, et al. Reward mechanisms in the brain and their role in dependence: evidence from neurophysiological and neuroimaging studies. Brain Res Brain Res Rev. 2001;36:139–149. doi: 10.1016/s0165-0173(01)00089-3. [DOI] [PubMed] [Google Scholar]
- 156.Schultz W, Dayan P, Montague PR. A neural substrate of prediction and reward. Science. 1997;275:1593–1599. doi: 10.1126/science.275.5306.1593. [DOI] [PubMed] [Google Scholar]
- 157.Schultz W. Getting formal with dopamine and reward. Neuron. 2002;36:241–263. doi: 10.1016/s0896-6273(02)00967-4. [DOI] [PubMed] [Google Scholar]
- 158.Wise RA. Dopamine, learning and motivation. Nat Rev Neurosci. 2004;5:483–494. doi: 10.1038/nrn1406. [DOI] [PubMed] [Google Scholar]
- 159.Kapur S. Psychosis as a state of aberrant salience: a framework linking biology, phenomenology, and pharmacology in schizophrenia. Am J Psychiatry. 2003;160:13–23. doi: 10.1176/appi.ajp.160.1.13. [DOI] [PubMed] [Google Scholar]
- 160.Kapur S, Mizrahi R, Li M. From dopamine to salience to psychosis–linking biology, pharmacology and phenomenology of psychosis. Schizophr Res. 2005;79:59–68. doi: 10.1016/j.schres.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 161.Roiser JP, Stephan KE, Ouden HE, Barnes TR, Friston KJ, Joyce EM. Do patients with schizophrenia exhibit aberrant salience? Psychol Med. 2008:1–11. doi: 10.1017/S0033291708003863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Seamans JK, Yang CR. The principal features and mechanisms of dopamine modulation in the prefrontal cortex. Prog Neurobiol. 2004;74:1–58. doi: 10.1016/j.pneurobio.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 163.Juckel G, Schlagenhauf F, Koslowski M, et al. Dysfunction of ventral striatal reward prediction in schizophrenia. Neuroimage. 2006;29:409–416. doi: 10.1016/j.neuroimage.2005.07.051. [DOI] [PubMed] [Google Scholar]
- 164.Cannon TD, van Erp TG, Bearden CE, et al. Early and late neurodevelopmental influences in the prodrome to schizophrenia: contributions of genes, environment, and their interactions. Schizophr Bull. 2003;29:653–669. doi: 10.1093/oxfordjournals.schbul.a007037. [DOI] [PubMed] [Google Scholar]
- 165.Howes OD, McDonald C, Cannon M, Arseneault L, Boydell J, Murray RM. Pathways to schizophrenia: the impact of environmental factors. Int J Neuropsychopharmacol. 2004;7(suppl 1):S7–S13. doi: 10.1017/S1461145704004122. [DOI] [PubMed] [Google Scholar]
- 166.Vernaleken I, Kumakura Y, Cumming P, et al. Modulation of [18F]fluorodopa (FDOPA) kinetics in the brain of healthy volunteers after acute haloperidol challenge. Neuroimage. 2006;30:1332–1339. doi: 10.1016/j.neuroimage.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 167.Grunder G, Vernaleken I, Muller MJ, et al. Subchronic haloperidol downregulates dopamine synthesis capacity in the brain of schizophrenic patients in vivo. Neuropsychopharmacology. 2003;28:787–794. doi: 10.1038/sj.npp.1300103. [DOI] [PubMed] [Google Scholar]
- 168.Meyer-Lindenberg A, Miletich RS, Kohn PD, et al. Reduced prefrontal activity predicts exaggerated striatal dopaminergic function in schizophrenia. Nat Neurosci. 2002;5:267–271. doi: 10.1038/nn804. [DOI] [PubMed] [Google Scholar]
- 169.Fusar-Poli P, Howes OD, Allen P, et al. Altered prefrontal activation directly related to striatal dopamine dysfunction in people with prodromal symptoms of schizophrenia. 2008;102 S30. [Google Scholar]
- 170.Kellendonk C, Simpson EH, Polan HJ, et al. Transient and selective overexpression of dopamine D2 receptors in the striatum causes persistent abnormalities in prefrontal cortex functioning. Neuron. 2006;49:603–615. doi: 10.1016/j.neuron.2006.01.023. [DOI] [PubMed] [Google Scholar]
- 171.Patil ST, Zhang L, Martenyi F, et al. Activation of mGlu2/3 receptors as a new approach to treat schizophrenia: a randomized Phase 2 clinical trial. Nat Med. 2007;13:1102–1107. doi: 10.1038/nm1632. [DOI] [PubMed] [Google Scholar]