Abstract
Objective
Recent public concern in response to states’ intended repeal of Medicaid bed-hold policies and report of their association with higher hospitalization rates prompts examination of these policies in ensuring continuity of care within the broader context of Medicaid policies.
Data Sources/Study Design
Minimum Data Set assessments of long-stay nursing home residents in April–June 2000 linked to Medicare claims enabled tracking residents’ hospitalizations during the ensuing 5 months and determining hospital discharge destination. Multinomial multilevel models estimated the effect of state policies on discharge destination controlling for resident, hospitalization, nursing home, and market characteristics.
Results
Among 77,955 hospitalizations, 5,797 (7.4 percent) were not discharged back to the baseline nursing home. Bed-hold policies were associated with lower odds of transfer to another nursing home (AOR=0.55, 95 percent CI 0.52–0.58) and higher odds of hospitalization (AOR=1.36), translating to 9.5 fewer nursing home transfers and 77.9 more hospitalizations per 1,000 residents annually, and costing Medicaid programs about $201,311. Higher Medicaid reimbursement rates were associated with lower odds of transfer.
Conclusions
Bed-hold policies were associated with greater continuity of NH care; however, their high cost compared with their small impact on transfer but large impact on increased hospitalizations suggests that they may not be effective.
Keywords: Medicare, multilevel models, hospitalizations, Minimum Data Set (MDS), relocation
The Omnibus Budget Reconciliation Act, or Nursing Home Reform Act of 1987, mandated that nursing homes adopt a bed-hold policy during acute hospitalization of residents. For a fee, nursing homes reserve the resident's bed during acute hospitalizations. The goals of this policy were twofold: to prevent facilities from discharging “difficult” or expensive patients, and to encourage continuity of residence for the nursing home client (Taylor 2004). Some state Medicaid programs assumed the responsibility for such payments for eligible nursing home residents in various ways, while other states did not.
Recent budget difficulties have led several states to decrease or eliminate bed-hold payments (Maryland 1999; Williams 2003; Correira 2004). Massachusetts has been in a flux regarding its bed-hold policies, changing the number of days and the rates paid several times, discontinuing payment for any bed-hold in 2003, and reinstating it 2 years later. The most attention to the flux in bed-hold policies was garnered in Florida, home to the second largest population of Americans older than 65, where the Medicaid program made $23 million in bed-hold payments annually in 2004 and 2005, roughly the equivalent of 4 days a year per Medicaid nursing home resident (Florida 2005). As statewide nursing home occupancy was under 90 percent, it was argued that bed-hold payments were superfluous, and could be eliminated (Freeman 2004; Nohlgren 2004). A similar argument was made recently in Pennsylvania where policy makers were considering the removal of bed-hold payments (Rotstein 2006).
Nursing home administrators counter that occupancy rates vary by region and by facility, and that elimination of bed-hold payments would increase hospital discharges to facilities other than the resident's original “home,” with potential consequences of relocation stress, including disorientation and dissatisfaction (Freeman 2004; Nohlgren 2004).
Historically, nursing home residents have taken legal action to prevent the closure of a substandard facility in order to avoid relocation, clearly implying social value to familiar surroundings (Cohen 1986). There is some literature suggesting that “relocation trauma” has a lasting negative effect on nursing home residents (Friedman et al. 1995; Capezuti et al. 2006; Laughlin et al. 2007). For example, change of venue alone has transiently increased fall rates (Friedman et al. 1995). Relocation may also lead to the duplication of tests and increased likelihood of medical errors (Boockvar et al. 2004; Coleman et al. 2004; Ma et al. 2004), both of which may be associated with morbidity and cost. A recent Presidential Council of Bioethics report emphasizes that hospitalizations at the end of life, a time at which more comfort and care are needed, are particularly traumatic to nursing home residents and families, exposing them to the possibility of relocation not only to a hospital, but to other nursing homes (Kass 2005).
Although the rationale for bed-hold policies was to facilitate residents’ return to their original nursing home, this effect has never been demonstrated. Hospital discharge destination is more complex than bed availability alone, and may be affected by other patients, nursing homes, market, and state factors, as has been shown for other transitions (Intrator et al. 2004, 2007). For specific diagnoses, and for sicker residents, discharge destinations other than nursing homes must be considered. Some patients or families may choose a different facility. For some patients, hospitalization may indicate that their condition is too severe to be managed in the originating nursing home, and indeed, possibly in any nursing home. Residents discharged with rehabilitation needs, such as following a hospitalization for hip fracture, stroke, or psychiatric diagnoses, may have limited facilities that can more appropriately serve them. Facilities with more available beds, advanced clinical capabilities, or higher staffing levels may be more likely to readmit their hospitalized residents. Within a given market, the availability of alternative nursing homes may affect discharge locale. Moreover, differences in the hospitalization rates of nursing home residents have been reported to vary with state policies (Intrator and Mor 2004; Nohlgren 2004). In particular, residents in states with any bed-hold payment policies were reported to have higher odds of being hospitalized (Intrator et al. 2007). Higher Medicaid reimbursement rates have been associated with fewer hospitalizations (Intrator et al. 2007) possibly because higher reimbursement allows facilities to invest in infrastructure and staffing that facilitate care within the nursing home environment as demonstrated in several papers (Intrator et al. 2005; Feng et al. 2008). The purpose of this paper was therefore to study the intended effect of bed-hold policies within the context of today's nursing home market, in light of the reported unintended consequences of associated increased hospitalization rates, while controlling for Medicaid reimbursement rates.
METHODS
Data Sources
We obtained resident characteristics from the Minimum Data Set (MDS), a federally mandated assessment for all nursing home residents that includes approximately 400 data elements, including demographics, diagnoses, treatments and measures of both physical and cognitive functions (Morris et al. 1990; Hawes et al. 1995). We used the Centers for Medicare and Medicaid Services’ (CMS's) Standard Analytic Files for part A claims for inpatient hospital, skilled nursing facility (SNF), hospice, home health, and outpatient services to determine other locations of care using the Residential History File methodology (Intrator et al. 2003). The CMS Online Survey Certification and Reporting (OSCAR) system provided nursing home data. We aggregated OSCAR data and used the Area Resource File to obtain market data (Stambler 1988). State Medicaid policies for the period of our study were available from a survey of the 48 contiguous states (Grabowski et al. 2004). We matched all data at the level of the resident, and performed our evaluation at the level of the hospitalization.
Subject Sample
We used MDS data from the second quarter of calendar year 2000 from free-standing urban nursing homes to identify a cohort of all long-stay (>90 days) residents. This established the nursing home of origin for each of 549,472 residents.
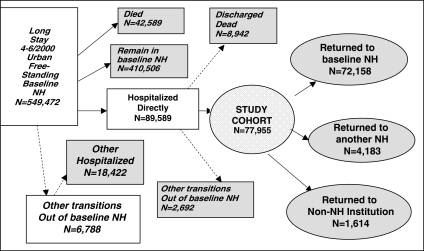
We matched residents to Medicare claims to identify the first acute hospitalization over the ensuing 5 months (N=97,141). We limited our analysis to 5 months to avoid hospitalizations that extended beyond the calendar year 2000. When hospitalization at one hospital was immediately followed by hospitalization at another, we considered this as a single hospitalization. We excluded hospitalizations in long-term hospitals or rehabilitation facilities (N=6,067), and hospitalizations not definitively originating from the baseline nursing home (N=1,485). Hospitalizations with discharges due to death were excluded as mortality was not relevant to the purpose of this study (N=8,942). Finally, hospitalizations with no matching resident, nursing home, or county information were excluded, and ambiguous discharge locations were censored (N=2,692). The final cohort included 77,955 residents served in 8,652 facilities in 812 counties in the 48 contiguous U.S. states. Figure 1 presents the framework for this paper in which the first hospitalization of long-stay residents was identified and followed for hospital discharge destination. Sample selection is denoted on the left part of the flow chart, and study outcomes on the right.
Figure 1.
Flow chart of study sample selection and outcomes. Rectangular nodes relate to sample selection, among which those with a darker background represent cases omitted from analyses. Oval nodes represent outcomes. The circular node in the middle represents the final cohort. Of 549,472 long-stay residents of free-standing urban nursing homes, in the second quarter of 2000, 77,955 were hospitalized directly from their original nursing home and entered the study. Of cohort members, 72,158 were discharged back to the original nursing home from the hospital; 4,183 were discharged to another nursing home; and 1,614 were discharged to another institution.
Outcomes
We used the MDS assessment dates, Medicare claims, and discharge location information to determine each resident's first location within 7 days after hospital discharge using the Residential History File methodology (Intrator et al. 2003). We considered three possibilities for discharge destination: the original nursing home, a different nursing home, and a nonnursing home institutional provider (including long-term hospitals, rehabilitation facilities or home hospice-care). Figure 1 presents these outcomes.
Variable Definitions
The main research question in this study was to examine the effect of two state policies on the post-hospital discharge location of long-stay nursing home residents. Any bed-hold policy was measured by a state-specific indicator. Medicaid per-diem reimbursement was measured as a continuous variable of the average Medicaid per-diem rate (total Medicaid payments to nursing homes divided by total bed-days paid for), standardized at its mean among the 48 states ($103.30), and in steps of $10 (1/2 SD). We note that bed-hold policies included maximum number of days paid within a prespecified period of time, the proportion of the regular per-diem paid, and whether there were occupancy standards that facilities were to meet in order to be paid for bed-hold. Table 1 lists the three state-bed-hold parameters: specific maximal days, the period during which those days were counted, and the proportion of the Medicaid per-diem rate paid. There was no correlation among any of these parameters and the per-diem reimbursement rate. Equivalent Reimbursement Days (ERD), a product of the maximum annual days for bed-hold and proportion of rate paid, incorporating the three parameters of bed-hold policies to a standardized measure, was also not correlated with Medicaid per-diem.
Table 1.
States’ Medicaid Policies and Distribution of Hospital Discharge Destination
| State Policies |
Hospital Discharge Destination per Resident |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bed-Hold Policies |
Total |
Baseline NH |
Other NH |
Non NH |
|||||||||
| Per-Diem ($) | % Per-Diem | Max Days | Time Frame | Occupancy Requirement | ERD | N | N | % | N | % | N | % | |
| 103.30 | 64.8 | 16.6 | N/A | N/A | 16.0 | All States | 77,955 | 72,158 | 92.5 | 4,183 | 5.4 | 1,614 | 2.1 |
| 112.54 | 75 | 4 | Hosp | No | 3.6 | Alabama | 1,322 | 1,280 | 96.8 | 31 | 2.3 | 11 | 0.8 |
| 99.57 | 100 | 9 | Cal | No | 9.0 | Arizona | 265 | 238 | 89.8 | ||||
| 69.36 | 100 | 5 | Hosp | Yes | 6.0 | Arkansas | 566 | 506 | 89.4 | 49 | 8.7 | 11 | 1.9 |
| 110.27 | 100 | 7 | Hosp | No | 8.4 | California | 5,556 | 4,683 | 84.3 | 655 | 11.8 | 218 | 3.9 |
| 111.62 | 0 | 0 | NA | NA | 0.0 | Colorado | 432 | 398 | 92.1 | 22 | 5.1 | 12 | 2.8 |
| 151.59 | 100 | 15 | Hosp | Yes | 18.0 | Connecticut | 1,533 | 1,451 | 94.7 | 61 | 4 | 21 | 1.4 |
| 117.66 | 100 | 14 | Cal | No | 14.0 | Delaware | 202 | 198 | 98 | ||||
| 113.45 | 100 | 8 | Hosp | Yes | 9.6 | Florida | 5,188 | 4,704 | 90.7 | 297 | 5.7 | 187 | 3.6 |
| 83.64 | 100 | 7 | Hosp | No | 8.4 | Georgia | 1,547 | 1,483 | 95.9 | 45 | 2.9 | 19 | 1.2 |
| 116.37 | 0 | 0 | NA | NA | 0.0 | Idaho | 64 | 52 | 81.3 | ||||
| 90.06 | 75 | 10 | Hosp | Yes | 9.0 | Illinois | 5,038 | 4,705 | 93.4 | 274 | 5.4 | 59 | 1.2 |
| 92.83 | 50 | 15 | Hosp | No | 9.0 | Indiana | 2,617 | 2,481 | 94.8 | 99 | 3.8 | 37 | 1.4 |
| 85.90 | 42 | 10 | Hosp | No | 5.0 | Iowa | 671 | 612 | 91.2 | ||||
| 83.53 | 67 | 10 | Hosp | Yes | 8.0 | Kansas | 592 | 506 | 85.5 | 71 | 12 | 15 | 2.5 |
| 100.35 | 100 | 14 | Mixed | No | 16.8 | Kentucky | 1,031 | 988 | 95.8 | 29 | 2.8 | 14 | 1.4 |
| 68.97 | 75 | 7 | Hosp | No | 6.3 | Louisiana | 2,120 | 1,742 | 82.2 | 236 | 11.1 | 142 | 6.7 |
| 115.77 | 100 | 10 | Cal | No | 10.0 | Maine | 123 | 119 | 96.7 | ||||
| 122.15 | 48 | 15 | Hosp | No | 8.6 | Maryland | 1,201 | 1,144 | 95.3 | 46 | 3.8 | 11 | 0.9 |
| 124.47 | Hosp | No | 24.0 | Massachusetts | 3,659 | 3,469 | 94.8 | 126 | 3.4 | 64 | 1.7 | ||
| 98.87 | 0 | 0 | NA | No | 0 | Michigan | 2,696 | 2,513 | 93.2 | 97 | 3.6 | 86 | 3.2 |
| 116.84 | 79 | 18 | Hosp | Yes | 17.1 | Minnesota | 854 | 798 | 93.4 | 41 | 4.8 | 15 | 1.8 |
| 90.38 | 100 | 15 | Hosp | No | 18.0 | Mississippi | 397 | 375 | 94.5 | ||||
| 91.65 | 100 | 12 | Mixed | Yes | 3.6 | Missouri | 1,711 | 1,525 | 89.1 | 169 | 9.9 | 17 | 1 |
| 94.04 | 100 | 365 | Hosp | Yes | 365.0 | Montana | 64 | 63 | 98.4 | ||||
| 81.42 | 100 | 15 | Hosp | Yes | 18.0 | Nebraska | 277 | 256 | 92.4 | ||||
| 101.00 | 0 | 0 | NA | NA | 0.0 | Nevada | 140 | 117 | 83.6 | ||||
| 118.91 | 0 | 0 | NA | NA | 0.0 | New Hampshire | 178 | 170 | 95.5 | ||||
| 127.63 | 90 | 10 | Hosp | No | 10.8 | New Jersey | 4,618 | 4,516 | 97.8 | 85 | 1.8 | 17 | 0.4 |
| 92.96 | 50 | 12 | Cal | Yes | 6.0 | New Mexico | 82 | 75 | 91.5 | ||||
| 160.66 | 100 | 20 | Hosp | Yes | 24.0 | New York | 7,026 | 6,763 | 96.3 | 212 | 3 | 51 | 0.7 |
| 122.14 | 0 | 0 | NA | NA | 0.0 | North Carolina | 1,467 | 1,362 | 92.8 | 89 | 6.1 | 16 | 1.1 |
| 104.94 | 100 | 15 | Hosp | Yes | 18.0 | North Dakota | 115 | 108 | 93.9 | ||||
| 121.76 | 50 | 30 | Cal | No | 15.0 | Ohio | 5,956 | 5,657 | 95 | 225 | 3.8 | 74 | 1.2 |
| 66.57 | 50 | 5 | Cal | No | 2.5 | Oklahoma | 883 | 694 | 78.6 | 143 | 16.2 | 46 | 5.2 |
| 95.43 | 0 | 0 | NA | NA | 0.0 | Oregon | 114 | 108 | 94.7 | ||||
| 122.91 | 33 | 15 | Hosp | No | 6.0 | Pennsylvania | 6,058 | 5,872 | 96.9 | 111 | 1.8 | 75 | 1.2 |
| 116.03 | 0 | 0 | NA | NA | 0.0 | Rhode Island | 626 | 577 | 92.2 | ||||
| 94.36 | 100 | 10 | Hosp | No | 12.0 | South Carolina | 727 | 699 | 96.1 | ||||
| 79.60 | 100 | 5 | Hosp | No | 6.0 | South Dakota | 153 | 143 | 93.5 | ||||
| 81.76 | 100 | 15 | Hosp | Yes | 18.0 | Tennessee | 1,666 | 1,556 | 93.4 | 89 | 5.3 | 21 | 1.3 |
| 83.53 | 0 | 0 | NA | NA | 0.0 | Texas | 4,533 | 3,806 | 84 | 454 | 10 | 273 | 6 |
| 90.19 | 0 | 0 | NA | NA | 0.0 | Utah | 107 | 90 | 84.1 | ||||
| 112.56 | 80 | 6 | Hosp | Yes | 5.8 | Vermont | 44 | 43 | 97.7 | ||||
| 99.99 | 0 | 0 | NA | NA | 0.0 | Virginia | 1,264 | 1,190 | 94.1 | 58 | 4.6 | 16 | 1.3 |
| 121.79 | 0 | 0 | NA | NA | 0.0 | Washington | 654 | 603 | 92.2 | ||||
| 113.68 | 100 | 12 | Cal | Yes | 12.0 | West Virginia | 411 | 403 | 98.1 | ||||
| 98.77 | 85 | 15 | Hosp | Yes | 15.3 | Wisconsin | 1,364 | 1,276 | 93.5 | 70 | 5.1 | 18 | 1.3 |
| 97.89 | 100 | 14 | Cal | No | 14.0 | Wyoming | 43 | 41 | 95.3 | ||||
Some cells have been suppressed to meet the Centers for Medicare and Medicaid Services privacy guidelines.
ERD, Equivalent Reimbursement Days is calculated as the product of proportion of daily coverage and maximum number of days covered (converted to annual when necessary and multiplied by the average number of annual hospitalizations, 1.2).
Confounders to the investigated relationship between bed-hold policies and discharge destination are described in Table 2. These included measures of inpatient acuity from the inpatient claims: inpatient length of stay, several categories of primary diagnoses, Elixhauser comorbidity index (Elixhauser et al. 1998), and an indicator of intensive care unit (ICU) use. Resident level controls relating to resident condition or potential preferences were obtained from the MDS. Characteristics of the discharging nursing home obtained from the OSCAR data included measures of structure, markers of facility revenue, low occupancy (<85 percent) as an indicator of ready bed supply for a return the availability of a dementia unit and a rehabilitation unit (which may potentially offer opportunities for returning to the baseline facility), and two measures of nursing home casemix acuity of the admitted and long-stay residents1 (Fries et al. 1994; Feng et al. 2006). Finally, we controlled for nurse and medical staffing levels, at the county level, we controlled for nursing home competition (Nyman 1989), assuming that return to the baseline nursing home would be more likely in competitive markets(Grabowski 2002; Mukamel et al. 2005; Castle et al. 2007), and average hospital occupancy rate in the county, indicating a pressure to discharge residents quicker, potentially leading to more transitions. Local wage index was used to control for geographical differences in the cost of living.
Table 2.
Description of Cohort
| N | % | Mean | SD | |
|---|---|---|---|---|
| State policies (N=48) | ||||
| Any bed-hold policy | 36 | 0.75 | ||
| Average per-diem Medicaid rate | 103.29 | 19.62 | ||
| County (N=812) | ||||
| Area wage index adjuster to geographic variation in $ | 0.96 | 0.12 | ||
| Average number of empty beds | 14.62 | 9.32 | ||
| Average hospital occupancy | 52.62 | 23.01 | ||
| Baseline nursing home (NH) (N=8,652) | ||||
| Total beds | 123.72 | 69.48 | ||
| For profit | 6,364 | 73.56 | ||
| Chain ownership | 5,151 | 59.54 | ||
| Average nursing case-mix index on admission assessments | 0.96 | 0.11 | ||
| Average nursing case-mix index on annual assessments | 0.72 | 0.06 | ||
| Occupancy <85% | 2,754 | 31.83 | ||
| Dementia unit available | 1,681 | 19.43 | ||
| Rehabilitation unit available | 298 | 3.44 | ||
| >35% Residents nongovernment paid | 1,991 | 23.01 | ||
| >15% Medicare paid | 1,338 | 15.46 | ||
| >1/2 FTE MD | 921 | 10.64 | ||
| Any NP/PA | 1,914 | 22.12 | ||
| Ratio RNs to (RNs+LPNs) | 0.34 | 0.20 | ||
| Hospitalization event (N=77,955) | ||||
| Event length of stay (LOS) | 7.04 | 6.59 | ||
| LOS <3 days | 11,334 | 14.53 | ||
| LOS 3–7 days | 32,752 | 42.00 | ||
| LOS 8–14 days | 27,225 | 34.90 | ||
| LOS >14 days | 6,684 | 8.57 | ||
| Primary diagnosis is ambulatory care sensitive | 23,859 | 30.61 | ||
| Primary diagnosis is stroke | 3,496 | 4.48 | ||
| Primary diagnosis is chronic obstructive pulmonary disease | 1,944 | 2.49 | ||
| Primary diagnosis is congestive heart failure | 4,218 | 5.41 | ||
| Hip fracture | 4,197 | 5.38 | ||
| Has a psychiatric diagnosis | 3,649 | 4.68 | ||
| Elixhauser comorbidity score | 2.54 | 1.38 | ||
| Any ICU during hospitalization event | 16,286 | 20.89 | ||
| Resident baseline Minimum Data Set (MDS) (N=77,955) | ||||
| Age | 83.07 | 7.82 | ||
| Married | 13,775 | 17.67 | ||
| African American | 10,888 | 13.97 | ||
| Male | 21,464 | 27.53 | ||
| Do-not-resuscitate order | 35,813 | 45.94 | ||
| Moderate cognitive impairment (CPS=3, 4) | 30,691 | 39.37 | ||
| Severe cognitive impairment (CPS=5, 6) | 16,396 | 21.03 | ||
| ADL <8 | 16,373 | 21.00 | ||
| ADL 8–16 | 19,148 | 24.56 | ||
| Weight loss | 9,800 | 12.57 | ||
| Flacker score | 4.36 | 2.15 | ||
| Diagnosis of diabetes affecting functioning | 22,203 | 28.48 | ||
| Diagnosis of CHF affecting functioning | 15,936 | 20.44 | ||
| Bipolar/schizophrenia without treatment | 994 | 1.28 | ||
| Bipolar/schizophrenia with treatment | 2,783 | 3.57 | ||
| More than nine medications in past 7 days | 31,601 | 40.54 | ||
| Obese (BMI>30) | 11,250 | 14.43 | ||
| Low weight (BMI<18) | 7,024 | 9.01 | ||
FTE, full-time-equivalent (% time employed); NP/PA, nurse practitioner/physician assistant; ICU, intensive care unit; CPS, cognitive performance scale; ADL, activity of daily living scale; BMI, body mass index.
Multilevel Model
We constructed a hierarchical, four-level multinomial model using MLwiN (Centre for Multilevel Modeling, Institute of Education, London, U.K.). In this model, the unit of analysis is a resident who was hospitalized from the original nursing home, and who was discharged from the hospital alive to an institution.
The model postulates that residents in the same nursing home would have unmeasured errors that are more similar than residents in other nursing homes, and likewise nursing homes in the same county, and counties in the same state. Thus, this method partitions the overall model error variance to components, accounting for the variance at each level of nesting. Denoted by Yijkr, the location of hospital discharge for resident i in nursing home j in county k in state r, where discharge location is denoted 0 for return to original nursing home, 1 to another nursing home, and 2 for an institution other than a nursing home, we model the logit of the probability of hospital discharge to another nursing home or to a nonnursing home institution compared with discharge to original nursing home, i.e.
where  is the facility-specific intercept and βy are the regression parameters associated with each outcome y, in particular, they contain the regression parameters associated with any bed-hold policy,
is the facility-specific intercept and βy are the regression parameters associated with each outcome y, in particular, they contain the regression parameters associated with any bed-hold policy,  for which we test the null hypotheses that bed-hold is not related to discharge locations, i.e. that the parameters are zero, versus the alternative hypotheses that each is different from zero. The intercept is composed of a constant
for which we test the null hypotheses that bed-hold is not related to discharge locations, i.e. that the parameters are zero, versus the alternative hypotheses that each is different from zero. The intercept is composed of a constant  and three random error terms
and three random error terms 
 and
and  each from a normal distribution with zero mean and specific variances,
each from a normal distribution with zero mean and specific variances, 
 and
and  which along with the overall model error's variance
which along with the overall model error's variance  comprise the four-model variance parameters for each outcome y=1, 2.
comprise the four-model variance parameters for each outcome y=1, 2.
To simplify the estimation of the multinomial outcome, we estimated two multilevel logistic regression models comparing discharges to the baseline nursing home with discharges to a different nursing home and with discharges to nonnursing home settings. This method provides unbiased estimates with potentially inflated standard errors (Begg and Gray 1984).
Sensitivity Analyses
We conducted several exploratory analyses to examine the robustness of the results. We first removed the restriction of studying a single hospitalization. Next, we allowed transitions from other nursing homes including hospital-based nursing homes and studied whether the residents returned to the discharging nursing home, as well as whether they returned to the baseline nursing home.
Nursing home residents in states with a bed-hold policy were more likely to be hospitalized (Intrator et al. 2007) raising a concern that residents admitted to hospital in those states were less sick and more likely to be readmitted back to the baseline nursing home. Another sensitivity analysis was conducted by estimating the models only on residents who were in the upper quartile of the posterior predicted probability of hospitalization (>.2) providing a perspective on the association of bed-hold and discharge destination on a more homogeneous sample of hospitalized residents who were sicker. The hospitalization model included only resident characteristics and controlled for the competing event of death, adjusting for clustering of residents in nursing homes (following Intrator et al. 2007).
RESULTS
Sample Description
The final cohort of 77,955 hospitalized nursing home residents had 100,269 hospitalizations over the 5-month window of which the first was used in the analyses. Overall, 92.5 percent of residents returned to their baseline nursing home. This varied from less than 82 percent in Oklahoma, Louisiana, and Nebraska to over 98 percent in Delaware, West-Virginia, and Montana (Table 1). The proportion of residents discharged to another nursing home averaged 5.4 percent, and the proportion of residents returning to an institution other than nursing home averaged 2.1 percent. Twelve states offered no bed-hold payment. Among the 36 states with bed-hold, most allowed bed-hold days per hospitalization (25 states), with an average ERD of 11.5 days (SD=5.7 days). Average state-level Medicaid per-diem rates ranged between $66.57 and $160.66, with an average of $103.30, (SD=$19.60).
Table 2 presents the characteristics of the 8,652 urban free-standing nursing homes (NHs) with any hospitalized residents in this cohort. These characteristics do not differ from the characteristics of all urban free-standing NHs (Intrator et al. 2007). Of note, 19.4 percent of NHs had a dementia unit, and 3.4 percent had a rehabilitation unit. Almost 32 percent of NHs had less than 85 percent occupancy suggesting that there were plenty of beds available for returning hospitalized nursing home residents.
The average length of inpatient stay was 7 days indicating that almost 15 percent of the hospitalizations were less than the minimum stay required for Medicare SNF benefits (3 days). Another 8.6 percent of hospitalizations were longer than 2 weeks.
Multilevel Model
Table 3 presents the results of the multilevel model. Nursing home residents from states with a bed-hold policy were more likely to return to their baseline nursing home. When compared with returning to the baseline nursing home, the adjusted odds ratio (AOR) of discharge to another nursing home was 0.55 (95 percent confidence interval [CI] 0.52–0.58). Being discharged to an institution other than a nursing home was also less likely (AOR=0.76; CI 0.44–1.31), although not statistically significant. Nursing home residents from states with higher Medicaid per-diem rates were more likely to return to their baseline nursing home. When compared with return to baseline, the AOR of returning to another nursing home with a $10 higher Medicaid per-diem rate was 0.85 and 0.88 for discharge to another institution, both statistically significant at the 5 percent level.
Table 3.
Model of Discharge Location Following Hospitalization, Compared with Returning to Baseline Nursing Home
| Other Nursing Home |
Institution Other Than Nursing Home |
|||||
|---|---|---|---|---|---|---|
| Characteristics/Factors | AOR | LCI | UCI | AOR | LCI | UCI |
| State policies | ||||||
| Any bed-hold policy | 0.55** | 0.52 | 0.58 | 0.76 | 0.44 | 1.31 |
| Average per-diem Medicaid rate (std to [x−$103.3]/$10) | 0.85** | 0.82 | 0.87 | 0.88* | 0.78 | 0.99 |
| County market | ||||||
| Area wage index adjusted to geographic variation (std to [x−0.96]/0.12) | 0.93** | 0.90 | 0.96 | 0.95 | 0.84 | 1.08 |
| Average number of empty beds (std to [x−14 beds]/10 beds) | 1.05 | 0.96 | 1.14 | 1.26** | 1.06 | 1.50 |
| Average hospital occupancy (std to [x−52.6%]/20%) | 1.11* | 1.02 | 1.21 | 1.04 | 0.91 | 1.19 |
| Baseline nursing home | ||||||
| Total beds (std to [x−100 beds]/70 beds) | 0.87** | 0.83 | 0.92 | 1.06+ | 1.00 | 1.13 |
| For-profit | 1.22** | 1.14 | 1.30 | 1.09 | 0.93 | 1.29 |
| Chain ownership | 1.03 | 0.99 | 1.08 | 1.05 | 0.92 | 1.21 |
| Average nursing case-mix index on admission assessments (std to [x−0.96]/0.125) | 0.84** | 0.79 | 0.89 | 1.00 | 0.92 | 1.10 |
| Average nursing case-mix index on annual assessments (std to [x−0.719]/0.066) | 0.89** | 0.84 | 0.95 | 0.92+ | 0.84 | 1.01 |
| Occupancy <85% | 1.08** | 1.03 | 1.14 | 0.98 | 0.85 | 1.12 |
| Dementia unit available | 0.93+ | 0.85 | 1.01 | 1.11 | 0.95 | 1.30 |
| Rehabilitation unit available | 1.13 | 0.90 | 1.41 | 1.09 | 0.79 | 1.52 |
| >35% Residents nongovernment paid | 1.10+ | 0.98 | 1.22 | 1.05 | 0.88 | 1.25 |
| >15% Medicare paid | 1.01 | 0.93 | 1.09 | 1.08 | 0.90 | 1.29 |
| >1/2 FTE MD | 1.01 | 0.87 | 1.16 | 0.95 | 0.77 | 1.16 |
| Any NP/PA | 1.04 | 0.98 | 1.10 | 1.18* | 1.02 | 1.36 |
| Ratio RNs/(RNs+LPNs) (std to [x−0.3]/0.2) | 0.98 | 0.94 | 1.01 | 1.02 | 0.94 | 1.11 |
| Hospitalization event | ||||||
| Event length of stay (LOS) (std to [x−7.3 days]/7.3 days) | 1.41** | 1.35 | 1.46 | 1.28** | 1.20 | 1.37 |
| LOS <3 days | 0.20** | 0.17 | 0.25 | 0.99 | 1.04 | 0.94 |
| LOS 3–7 days | 0.73** | 0.69 | 0.76 | 0.61** | 0.53 | 0.70 |
| LOS >14 days | 1.33** | 1.21 | 1.45 | 1.37** | 1.12 | 1.68 |
| Primary diagnosis is ambulatory care sensitive | 1.07+ | 1.00 | 1.15 | 0.67** | 0.58 | 0.77 |
| Primary diagnosis is stroke | 1.23+ | 1.03 | 1.49 | 2.59** | 2.13 | 3.16 |
| Primary diagnosis is chronic obstructive pulmonary disease | 0.71** | 0.55 | 0.92 | 1.01 | 0.67 | 1.54 |
| Primary diagnosis is congestive heart failure | 0.70** | 0.61 | 0.80 | 0.87 | 0.63 | 1.20 |
| Hip fracture | 1.97** | 1.73 | 2.24 | 1.72** | 1.36 | 2.16 |
| Has a psychiatric diagnosis | 1.29** | 1.17 | 1.42 | 0.31** | 0.22 | 0.45 |
| Elixhauser comorbidity score | 1.00 | 0.97 | 1.04 | 1.13** | 1.07 | 1.19 |
| Any ICU during hospitalization event | 0.93+ | 0.86 | 1.00 | 1.59** | 1.41 | 1.80 |
| Resident | ||||||
| Age (std to [x−83 years]/8 years) | 1.00 | 0.94 | 1.06 | 0.93* | 0.88 | 0.99 |
| Married | 1.00 | 0.94 | 1.06 | 1.15* | 1.00 | 1.33 |
| African American | 0.86+ | 0.72 | 1.02 | 0.99 | 0.84 | 1.17 |
| Male | 1.12** | 1.06 | 1.19 | 1.07 | 0.95 | 1.21 |
| Do-not-resuscitate order | 0.86** | 0.79 | 0.92 | 0.97 | 0.86 | 1.09 |
| Moderate cognitive impairment (CPS=3, 4) | 0.93 | 0.84 | 1.03 | 0.80** | 0.71 | 0.91 |
| Severe cognitive impairment (CPS=5, 6) | 0.87* | 0.77 | 0.98 | 1.05 | 0.90 | 1.22 |
| ADL <8 | 0.72** | 0.63 | 0.81 | 0.77** | 0.64 | 0.92 |
| ADL 8–15 | 0.91** | 0.85 | 0.97 | 0.73** | 0.63 | 0.83 |
| Weight loss | 1.03 | 0.93 | 1.14 | 0.85+ | 0.70 | 1.02 |
| Flacker score (std) | 0.98 | 0.94 | 1.02 | 1.23** | 1.13 | 1.34 |
| Diagnosis of diabetes affecting functioning | 0.93+ | 0.85 | 1.01 | 0.87* | 0.77 | 0.98 |
| Diagnosis of CHF affecting functioning | 1.09* | 1.02 | 1.18 | 0.90 | 0.77 | 1.04 |
| Bipolar/schizophrenia without treatment | 0.63** | 0.47 | 0.83 | 0.87 | 0.54 | 1.41 |
| Bipolar/schizophrenia with treatment | 0.70** | 0.55 | 0.89 | 0.93 | 0.68 | 1.27 |
| More than nine medications in past 7 days | 1.01 | 0.93 | 1.09 | 1.05 | 0.94 | 1.18 |
| Obese (BMI>30) | 0.93+ | 0.86 | 1.01 | 1.07 | 0.91 | 1.26 |
| Low weight (BMI<18) | 1.11* | 1.02 | 1.21 | 0.98 | 0.82 | 1.17 |
| Variance components | var | SE | ICC (%) | var | SE | ICC (%) |
| State | 0.199 | 0.052 | 4.72 | 0.418 | 0.143 | 8.66 |
| County | 0.216 | 0.014 | 5.13 | 0.6 | 0.099 | 12.45 |
| Facility | 0.514 | 0.011 | 12.19 | 0.516 | 0.09 | 10.70 |
Std, standardized; AOR, adjusted odds ratio; LCI, lower confidence interval; UCI, upper confidence interval; ICC, intra-class correlation; FTE, full-time-equivalent (% time employed); NP/PA, nurse practitioner/physician assistant; ICU, intensive care unit; CPS, cognitive performance scale; ADL, activity of daily living scale; BMI, body mass index; Var, variance; SE, standard error.
p-value <.01.
p-value <.05.
p-value <.1.
Higher hospital occupancy in the local market was associated with increased odds of being discharged to another nursing home (AOR=1.11). Higher competition for nursing home residents as measured by excess capacity (empty beds) in the market was associated with higher odds of being discharged to an institution other than a nursing home (AOR=1.26).
Residents of for-profit nursing homes were more likely to be discharged to other nursing homes (AOR=1.22), but chain membership was not associated with discharge location. Residents hospitalized from larger nursing homes were less likely to be discharged to another nursing home (AOR=0.87 for every 70 beds more than 100), but more likely to be discharged to another institution (AOR=1.06 for every 70 beds more than 100).
Discharge location was not affected by payer mix at the baseline nursing home. On the other hand, residents from nursing homes with low occupancy (<85 percent) had higher odds of being discharged to another nursing home (AOR=1.08). The availability of a rehabilitation unit in the baseline nursing home was not associated with discharge location in this cohort, and the availability of a dementia unit was only marginally associated with lower odds of discharge to another nursing home (AOR=0.93). Finally, neither nursing home staffing level nor skill mix was related to the hospital discharge location.
The length of patients’ hospitalization was a major determinant of discharge location. Overall, longer length of stay (LOS) was associated with higher odds of being discharged to locations other than the baseline nursing home. Residents hospitalized for very brief stays (<3 days) were much less likely to be discharged to another NH (AOR=0.20), and those hospitalized for 3–7 days were also less likely to be discharged to another nursing home (AOR=0.73). Other hospitalization characteristics such as diagnosis and use of the ICU were also associated with the discharge location.
Model Robustness
An examination of all hospitalizations, including those not emanating from the baseline nursing home, controlling for discharging nursing home characteristics, resulted in similar estimates that were somewhat tempered (particular results available upon request). Residents hospitalized from a hospital-based nursing home had 3.24 higher odds of being discharged to another nursing home (CI=1.90–5.52).
Among residents more likely to be hospitalized (N=27,524), 1,678 (6.1 percent) were discharged to another nursing home and 661 (2.4 percent) were discharged to an institution other than a nursing home. Model results revealed that Medicaid per-diem rate was associated with lower odds of discharge to another nursing home (AOR=0.88; 95 percent CI 0.82–0.95); however, the effect of bed-hold policy was much smaller and not statistically significant (AOR=0.81; 95 percent CI 0.58–1.12).
DISCUSSION
Previously reported nursing home to nursing home transfer was 2–3 percent annually (Mor et al. 1997; Hirth et al. 2000), lower than the rate observed in this cohort of long-stay residents following hospitalization (5.4 percent). Whereas the cohorts and unit of analysis were different in those earlier studies, this suggests that the majority of nursing home to nursing home transfers occur via an intervening hospitalization. Moreover, residents who stayed longer in the hospital were more likely to be transferred to other nursing homes. These results suggest that a hospitalization is a catharsis for re-evaluation of a relative's goals of care and needs.
The study confirmed the hypothesis that bed-hold policies were associated with a lower rate of transfer to other nursing homes. Interestingly, this result did not vary by the generosity of the bed-hold policy. Moreover, higher Medicaid reimbursement was associated with a greater likelihood of return to the original nursing home, continuing a line of research that suggests that higher Medicaid payments for nursing home resident care are associated with better nursing home quality and resident outcomes, possibly due to financial stability allowing investment in infrastructure and staffing (Grabowski 2001, 2004; Grabowski et al. 2004; Intrator and Mor 2004; Intrator et al. 2005, 2007; Feng et al. 2008). These findings indicate the need for a comprehensive analysis of the relative merits of bed-hold policies compared to their price and to other policies that might achieve comparable merits.
Nursing home transfer may be a consequence of potential quality differences between the baseline and new nursing home. A previous study showed that nursing home to nursing home transfer, though infrequent, was more common from lower quality facilities (Hirth et al. 2000). However, the relative quality of the new facility was not investigated. Among residents transferred to another nursing home in this study, 48.8 percent subsequently returned to their baseline nursing home within 92 days, indicating that quality might not have been the reason for those transitions. Moreover, lower occupancy rate at the baseline nursing home did not appear to guarantee a return to that nursing home. Indeed, contrary to our expectations, lower occupancy was associated with more transfers to another nursing home, suggesting that occupancy per se might be a surrogate measure of nursing home quality with lower occupancy serving as a marker of poorer quality. Other literature suggests the relationship between lower occupancy and poor nursing home quality (Mor et al. 2004; Smith et al. 2007).
Medicare policies allow SNF care following a hospitalization of 3 days or more. Thus, it was hypothesized that one reason for hospitalization would be to establish resident eligibility for Medicare SNF-level care, which is generally compensated at higher rates than Medicaid (MEDPAC 2005). Among residents returning to their baseline nursing home, only 20,387 (29.1 percent) returned with Medicare SNF level of care, while among residents transferred to another nursing home, 53.7 percent received Medicare SNF level of care from their new nursing home. Even though most nursing homes in the country were dually certified to provide Medicaid and Medicare covered services, it is likely that the type of SNF care required following a hospitalization was not available in residents’ baseline nursing home requiring the temporary transition.
There has been a growing concern regarding unnecessary hospitalizations (Saliba et al. 2000; Miller et al. 2003; Intrator et al. 2004; Porell and Carter 2005), another indicator of poor quality of care in nursing homes. Indeed, among the hospitalizations in this cohort, 30.6 percent were for an Ambulatory Care Sensitive condition, indicating the hospitalization could potentially have been avoided (Intrator et al. 2004). Moreover, the fact that many hospitalizations did not result in SNF care increases doubts regarding the circumstances of the hospitalizations. As bed-hold policies have been associated with increased hospitalizations (albeit not more potentially preventable than otherwise), the number of potentially preventable hospitalizations would necessarily have been higher than without the policy.
Our cross-sectional analysis has several limitations. We identified associations between policy and discharge destination, but could not ascertain causality. Whereas we have controlled for occupancy with annually updated OSCAR data, we were unable to consider the day-to-day variations in occupancy that could disallow bed-hold payments. Therefore, some hospitalizations in states, which require minimum nursing home occupancy (e.g., 90 percent) in order to activate a bed-hold policy, may not have resulted in bed-hold payments. Furthermore, our cohort includes nongovernment paid nursing home residents for whom Medicaid bed-hold payments would not apply. However, both limitations serve to bias our results towards the null hypothesis of no bed-hold policy effect on discharge destination.
We conducted a rough cost estimate based on the model presented in Table 3 and assuming 17.4 percent hospitalization rate without bed-hold and 22.3 percent with bed-hold (assuming AOR=1.36, based on prior literature). Using these figures, we estimated that bed-hold policies were associated with 9.5 fewer annual relocations for every 1,000 residents, with an associated 77.9 more hospitalizations. It is therefore instructive to examine the associated budgetary implications, especially in light of arguments made by the nursing home industry that bed-hold payments were integral to the financial viability of nursing homes (Florida 1999; Massachusetts 2003; Rotstein 2006). A simple calculation shows that with a generous bed-hold policy such as in Massachusetts and New York, and other states that pay for bed-hold at 100 percent for 12 calendar days or more, the average Medicaid payment for the bed-hold would be $201.31 per resident per year.2 With a less generous bed-hold policy such as in Oklahoma, with a maximum of 5 days reimbursed annually at 50 percent, the extra revenue to nursing homes from the bed-hold policy would be $1.18 per resident year.3 A simple calculation shows that by increasing Medicaid daily reimbursement rate by 55 cents, the most generous bed-hold policies would be offset. Assuming that the causal effect of increased Medicaid rate on limiting hospitalizations and increasing return to baseline nursing home is unchanged, this substitution would encourage better quality care, and ultimately cost Medicare less by saving payments for the additional hospitalizations. These rough calculations, coupled with the lower levels of nursing home occupancy in today's markets, appear to indicate that bed-hold policies may have reached the end of their life.
In making this estimation, we acknowledge that we do not have all the inputs to conduct a full cost–benefit analysis regarding bed-hold policy. Specifically, any benefit or harm associated with relocation has yet to be quantified. For example, when a state has no bed-hold policy, some residents may refuse hospitalization to avoid loss of their bed (Nohlgren 2004). In particular, if ill patients refuse hospitalization, mortality may increase. Providing care to more acutely ill patients in nursing homes ill-prepared to do so may take time away from other residents, increasing the potential for adverse events and litigation (Stevenson and Studdert 2003). Absence of a bed-hold policy may prolong hospitalization due to difficulty in determining a locale for hospital discharge (Nohlgren 2004). Verification of these potential effects will require further research.
A full-scale cost analysis examining all cost implications of removing or adding a bed-hold policy should be considered to further elucidate the issues of financial viability. A cost–benefit study could be designed to examine the costs relative to the social and personal benefits of such policies.
Acknowledgments
Joint Acknowledgement/Disclosure Statement: We would like to thank the editors and the reviewers for their valuable comments that helped to greatly improve this manuscript. We gratefully acknowledge the contribution of Nancy Grossman who conducted the survey of states’ policies; the programming expertise of Christian Brostup-Jensen and Jeffrey Hiris; and the thoughtful input of Pedro Gozalo, David Gifford, Zhanlian Feng, and Susan Miller. We would also like to thank Ning Wu and Yuwei Wang for conducting some of the earlier analyses.
This study is supported in part by National Institute on Aging Grants R01 AG02557 and R01 AG023622. Data made available by CMS under Data Use Agreement #12432. Mark Schleinitz was supported by a Building Interdisciplinary Research Careers in Women's Health grant K12 HD43447 administered through Women and Infants’ Hospital, Providence, RI. David Grabowski was supported in part by a NIA career development award (K01 AG024403).
Disclosures: A prior version of this paper was presented at the Annual Meeting of the Gerontological Society of America in Washington, DC, in November 2004.
Disclaimers: No funding source played a role in the design or conduct of the study, the collection, analysis or interpretation of data, or the preparation, review or approval of this manuscript.
NOTES
Case-mix measures were aggregated from all admission MDS assessments and separately for all annual MDS assessments in 2000 using the nursing case-mix index, an index of the ratio of the average number of nursing staff minutes required to care for residents at each of 44 Resource Utilization Groups to the overall average of staff minutes.
This calculation is based on the average number of hospitalization days, 11.2 days, multiplied by 100 percent bed-hold rate, and per-diem of $103.30, applied to 17.4 percent residents estimated to be hospitalized. The additional hospitalized resident days due to the increased hospitalization rates would not incur additional cost since they would have been paid for had the resident not been hospitalized. Under this scenario, the total cost to Medicaid would be $201.31 per resident year. In making the calculations, we assumed that the effect of bed-hold policy on the hospitalization rate does not vary by the generosity of the policy.
Given bed-hold payment at 50 percent of rate for a maximum of 5 days would reimburse NHs $44.97 for hospitalizations that would have occurred if the hospitalization rate had remained at 17.4 percent. However, Medicaid would save $43.71 for the extra residents hospitalized due to the higher hospitalization rate by paying the partial bed-hold rate on days that the resident would have otherwise been in the nursing home. This brings the total extra payment due to bed-hold policy to $1.18 per resident year.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Begg C B, Gray R. Calculation of Polychotomous Logistic Regression Parameters Using Individualized Regressions. Biometrika. 1984;71:11–8. [Google Scholar]
- Boockvar K S, Litke A, et al. Patient Relocation in the 6 Months after Hip Fracture: Risk Factors for Fragmented Care. Journal of the American Geriatrics Society. 2004;52(11):1826–31. doi: 10.1111/j.1532-5415.2004.52512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capezuti E, Boltz M, Ranz S, Hoffman D, Norman R G. Nursing Home Involuntary Relocation: Clinical Outcomes and Perceptions of Residents and Families. Journal of the American Medical Directors Association. 2006;7(8):486–92. doi: 10.1016/j.jamda.2006.02.011. [DOI] [PubMed] [Google Scholar]
- Castle N G, Engberg J, Liu D. Have Nursing Home Compare Quality Measure Scores Changed over Time in Response to Competition? Quality and Safety in Health Care. 2007;16(3):185–91. doi: 10.1136/qshc.2005.016923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen E S. Legislative and Educational Alternatives to a Judicial Remedy for the Transfer Trauma Dilemma. American Journal of Law and Medicine. 1986;11(4):405–32. [PubMed] [Google Scholar]
- Coleman E A, Min S J, Chomiak A, Kramer A M. Posthospital Care Transitions: Patterns, Complications, and Risk Identification. Health Services Research. 2004;39(5):1449–65. doi: 10.1111/j.1475-6773.2004.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correira D J. “Massachusetts Medicaid Alert. Holland and Knight Law Firm. March 29, 2004.”. 2004. [accessed on October 8, 2007]. Available at http://www.hklaw.com/Publications/OtherPublication.asp?Article=2192&Print=Yes.
- Elixhauser A, Steiner C, Harns D R, Coffey R M. Comorbidity Measures for Use with Administrative Data. Medical Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- Feng Z, Grabowski D C, Intrator O, Mor V. The Effect of State Medicaid Case-Mix Payment on Nursing Home Resident Acuity. Health Services Research. 2006;41(4, pt 1):1317–36. doi: 10.1111/j.1475-6773.2006.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Z, Grabowski D C, Intrator O, Zinn J, Mor V. Medicaid Payment Rates, Case-Mix Reimbursement, and Nursing Home Staffing–1996–2004. Medical Care. 2008;46(1):33–40. doi: 10.1097/MLR.0b013e3181484197. [DOI] [PubMed] [Google Scholar]
- Florida. “Nursing Home Reimbursement: Florida Association of Homes for the Aging and Florida Health Care Association.” Presentation to the Senate Appropriations Committee on Health and Human Services, March 4, 2004. 1999. [accessed on May 17, 2004]. Available at http://www.fhca.org/fhca/news/hhsappr.ppt.
- Florida. “Florida's E-Budget: 2004–2005”. 2005. [accessed on May 17, 2004]. Available at http://www.ebudget.state.fl.us/BDIssueDetail.asp?IssRecNum=12&policyid=&PolicyLevel=&ServiceID=68501500.
- Freeman L. “Budget Proposal Would Ax Medicaid ‘Bed-Hold’ Policy.”Naples Daily News, March 14, 2004. 2004. [accessed on October 8, 2007]. Available at http://www.protectelders.org/news/press/03_14_04.htm.
- Friedman S M, Williamson J D, Lee B H, Ankrom M A, Ryan S D, Denman S J. Increased Fall Rates in Nursing Home Residents after Relocation to a New Facility. Journal of the American Geriatrics Society. 1995;43(11):1237–42. doi: 10.1111/j.1532-5415.1995.tb07399.x. [DOI] [PubMed] [Google Scholar]
- Fries B E, Schneider D P, Foley W J, Gavazzi M, Burke R, Cornelius E. Refining a Case-Mix Measure for Nursing Homes: Resource Utilization Groups (RUG-III) Medical Care. 1994;32(7):668–85. doi: 10.1097/00005650-199407000-00002. [DOI] [PubMed] [Google Scholar]
- Grabowski D C. Medicaid Reimbursement and the Quality of Nursing Home Care. Journal of Health Economics. 2001;20(4):549–69. doi: 10.1016/s0167-6296(01)00083-2. [DOI] [PubMed] [Google Scholar]
- Grabowski D C. The Economic Implications of Case-Mix Medicaid Reimbursement for Nursing Home Care. Inquiry. 2002;39(3):258–78. doi: 10.5034/inquiryjrnl_39.3.258. [DOI] [PubMed] [Google Scholar]
- Grabowski D C. A Longitudinal Study of Medicaid Payment, Private-Pay Price and Nursing Home Quality. International Journal of Health Care Finance and Economics. 2004;4(1):5–26. doi: 10.1023/b:ihfe.0000019258.29496.03. [DOI] [PubMed] [Google Scholar]
- Grabowski D C, Angelelli J J, Mor V. Medicaid Payment and Risk-Adjusted Nursing Home Quality Measures. Health Affairs (Millwood) 2004;23(5):243–52. doi: 10.1377/hlthaff.23.5.243. [DOI] [PubMed] [Google Scholar]
- Grabowski D C, Feng Z, Intrator O, Mor V. Recent Trends in State Nursing Home Payment Policies. Health Affairs (Millwood) 2004 doi: 10.1377/hlthaff.w4.363. Suppl Web Exclusives: W4-363-73. [DOI] [PubMed] [Google Scholar]
- Hawes C, Morris J N, Phillips C D, Mor V, Fries B E, Nonemaker S. Reliability Estimates for the Minimum Data Set for Nursing Home Resident Assessment and Care Screening (MDS) Gerontologist. 1995;35(2):172–8. doi: 10.1093/geront/35.2.172. [DOI] [PubMed] [Google Scholar]
- Hirth R A, Banaszak-Holl J C, McCarthy J F. Nursing Home-to-Nursing Home Transfers: Prevalence, Time Pattern, and Resident Correlates. Medical Care. 2000;38(6):660–9. doi: 10.1097/00005650-200006000-00007. [DOI] [PubMed] [Google Scholar]
- Intrator O, Berg K, Hiris J, Mor V, Miller S C. Development and Validation of the Medicare-MDS Residential History File. Gerontologist. 2003;43:30–1. [Google Scholar]
- Intrator O, Feng Z, Mor V, Gifford D, Bourbonniere M, Zinn J. The Employment of Nurse Practitioners and Physician Assistants in U.S. Nursing Homes. Gerontologist. 2005;45(4):486–95. doi: 10.1093/geront/45.4.486. [DOI] [PubMed] [Google Scholar]
- Intrator O, Grabowski D C, Zinn J, Schleinitz M, Feng Z, Miller S C, Mor V. Hospitalization of Nursing Home Residents: The Effects of States’ Medicaid Payment and Bed-Hold Policies. Health Services Research. 2007;42(4):1651–71. doi: 10.1111/j.1475-6773.2006.00670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intrator O, Mor V. Effect of State Medicaid Reimbursement Rates on Hospitalizations from Nursing Homes. Journal of the American Geriatrics Society. 2004;52(3):393–8. doi: 10.1111/j.1532-5415.2004.52111.x. [DOI] [PubMed] [Google Scholar]
- Intrator O, Zinn J, Mor V. Nursing Home Characteristics and Potentially Preventable Hospitalizations of Long-Stay Residents. Journal of the American Geriatrics Society. 2004;52(10):1730–6. doi: 10.1111/j.1532-5415.2004.52469.x. [DOI] [PubMed] [Google Scholar]
- Kass L R. Taking Care: Ethical Caregiving in Our Aging Society. Washington, DC: The Presidential Council on Bioethics; 2005. Available at http://www.bioethics.gov/reports/taking_care/index.html. [Google Scholar]
- Laughlin A, Parsons M, Kosloki K D, Evans-Bergnan B. Predictors of Mortality Following Involuntary Interinstitutional Relocation. Journal of Gerontological Nursing. 2007;33(9):20–6. doi: 10.3928/00989134-20070901-04. quiz 28–9. [DOI] [PubMed] [Google Scholar]
- Ma E, Coleman E A, Fish R, Lin M, Kramer A M. Quantifying Posthospital Care Transitions in Older Patients. Journal of the American Medical Directors Association. 2004;5(2):71–4. doi: 10.1097/01.JAM.0000110658.01514.F7. [DOI] [PubMed] [Google Scholar]
- Maryland. “State of Maryland Department of Legislative Services. HB791 Fiscal Note (revised)”. 1999. [accessed on October 8, 2007]. Available at http://mlis.state.md.us/1999rs/fnotes/bil_0001/hb0791.rtf.
- Massachusetts. “Crisis at Home: the Impact of Massachusetts’ Nursing Home Closures. Policy Brief.” Massachusetts Senate Post Audit and Oversight Committee. 2003. [accessed on October 30, 2007]. Available at http://www.state.ma.us/legis/senate/nhomes_brief.htm.
- MEDPAC. Report to the Congress: Medicare Payment Policy. Washington, DC: Medicare Payment Advisory Commission; 2005. [Google Scholar]
- Miller S C, Mor V, Intrator O, Gozalo P, Roy J, Barber J, Wu N. 2003. “Nursing Home Care at the End of Life: Costs and Quality.” Final Report to AHRQ: Grant Number R01 HS10549.
- Morris J N, Hawes C, Fries B E, Phillips C D, Mor V, Katz S, Murphy K, Drugovich M L, Friedlob A S. Designing the National Resident Assessment Instrument for Nursing Homes. Gerontologist. 1990;30(3):293–307. doi: 10.1093/geront/30.3.293. [DOI] [PubMed] [Google Scholar]
- Mor V, Intrator O, Fries B E, Phillips C, Teno J, Hiris S, Hawes C, Morris J. Changes in Hospitalization Associated with Introducing the Resident Assessment Instrument. Journal of the American Geriatrics Society. 1997;45(8):1002–10. doi: 10.1111/j.1532-5415.1997.tb02973.x. [DOI] [PubMed] [Google Scholar]
- Mor V, Zinn J, Angelelli J, Teno J M, Miller S C. Driven to Tiers: Socioeconomic and Racial Disparities in the Quality of Nursing Home Care. Milbank Quarterly. 2004;82(2):227–56. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukamel D B, Spector W D, Bajorska A. Nursing Home Spending Patterns in the 1990s: The Role of Nursing Home Competition and Excess Demand. Health Services Research. 2005;40(4):1040–55. doi: 10.1111/j.1475-6773.2005.00394.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nohlgren S. Patients May Lose Cherished Bed: A Bush Medicaid Cut Could Leave Nursing Home Patients Who Have to Be Hospitalized. 2004. St. Petersburg Times, March 1, 2004.
- Nyman J A. Excess Demand, Consumer Rationality, and the Quality of Care in Regulated Nursing Homes. Health Services Research. 1989;24(1):105–27. [PMC free article] [PubMed] [Google Scholar]
- Porell F W, Carter M. Discretionary Hospitalization of Nursing Home Residents with and without Alzheimer's Disease: A Multilevel Analysis. Journal of Aging and Health. 2005;17(2):207–38. doi: 10.1177/0898264304274302. [DOI] [PubMed] [Google Scholar]
- Rotstein G. “Nursing Homes, Rendell Duel over Funds; State Wants to Change Medicaid Payments.”. 2006. Pittspurgh Post-Gazette. Pittsburgh: B-1.
- Saliba D, Kington R, Buchanan J, Bell R, Wang M, Lee M, Herbst M, Lee D, Sur D, Rubenstein L. Appropriateness of the Decision to Transfer Nursing Facility Residents to the Hospital. Journal of the American Geriatrics Society. 2000;48(2):154–63. doi: 10.1111/j.1532-5415.2000.tb03906.x. [DOI] [PubMed] [Google Scholar]
- Smith D B, Feng Z, Fennell M L, Zinn J, Mor V. Separate and Unequal: Racial Segregation and Disparities in Quality across U.S. Nursing Homes. Health Affairs (Millwood) 2007;26(5):1448–58. doi: 10.1377/hlthaff.26.5.1448. [DOI] [PubMed] [Google Scholar]
- Stambler H V. The Area Resource File–A Brief Look. Public Health Report. 1988;103(2):184–8. [PMC free article] [PubMed] [Google Scholar]
- Stevenson D G, Studdert D M. The Rise of Nursing Home Litigation: Findings from a National Survey of Attorneys. Health Affairs (Millwood) 2003;22(2):219–29. doi: 10.1377/hlthaff.22.2.219. [DOI] [PubMed] [Google Scholar]
- Taylor J A. “Legal Counsel for the Elderly.” University of Alabama Law School. 2004. [accessed on October 8, 2007]. Available at http://www.uaelderlaw.org/nursing.html.
- Williams C. “An Overview of Recent State HCBS Budget Cuts. Policy Brief.” Center for Home Care Policy and Research, New York, NY. 2003. [accessed on October 30, 2007]. Available at http://www.vnsny.org/research/publications/pdf/No16_Williams.pdf. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.