Abstract
Inhibition of heat shock protein 90 (HSP90) leads to inappropriate processing of proteins involved in cell survival pathways. We found that HSP90 inhibitor, 17-(dimethylaminoethylamino)-17-demethoxygeldanamycin (DMAG), is synergistic with radiation for non-small cell lung cancer cell lines, NCI-H460 and A549. To establish the optimal schedule for this combination, cells were radiated before, after, or simultaneously with DMAG, and survival was scored by clonogenic assay. The sequence of DMAG administration was critical for synergy with radiation, and pretreatment for 16 h led to maximal synergy. Similar radiosensitization was observed in isogenic cells in which expression of wild-type p53 was silenced by RNA interference, although p53 loss rendered cells overall less radiosensitive. The mechanistic basis for synergy was studied by Western blotting, cell cycle analysis, alkaline comet assay, and direct measurement of the activities of key base excision repair enzymes. Regardless of schedule of administration, DMAG led to degradation of proteins involved in activation of cell survival pathways after radiation, which did not explain the differences in the schedule of administration observed in clonogenic assays. In addition to previously reported decrease in activation of ATM, pretreatment with DMAG blocked activation of base excision repair machinery and activity of key enzymes, apurinic/apyrimidinic endonuclease, and DNA polymerase-β. Similarly, pretreatment with specific apurinic/apyrimidinic endonuclease inhibitor, CRT0044876, reproduced the effects of DMAG. Thus, administration of HSP90 inhibitors before radiation is critical for optimizing their use as radiosensitizers.
Introduction
Heat shock protein 90 (HSP90) is a molecular chaperone required for conformational folding of many proteins. HSP90 is important for stabilization and trafficking of tyrosine and serine/threonine kinases that are activated in response to genotoxic stress, including those that are essential for survival of cancer cells (1). The naturally occurring ansamycin antibiotic geldanamycin (GA; NSC 122750) has been known to have anticancer properties since the 1980s (2). Although originally believed to function as a kinase inhibitor, it was subsequently discovered that GA blocks the ATP-binding pocket of HSP90 protein in active conformation (1). Several inhibitors of HSP90 have been developed recently, including related benzoquinone ansamycin agents, and some are undergoing clinical trials. The recently developed GA analogue 17-(dimethylaminoethylamino)-17-demethoxygeldanamycin (DMAG; NSC 707545) is a hydrophilic GA derivative that can be administered orally with good bioavailability and better activity in vitro and in vivo than its predecessor, 17-allylamino-17-demethoxygeldanamycin (3, 4). DMAG is currently in phase I/II clinical trials but has yet to be tested in patients in combination with radiation or other chemotherapeutic agents.
Radiotherapy following surgical resection and chemotherapy are done with curative intent for patients with limited stage non-small cell lung cancer (NSCLC), but radiotherapy provides only marginal improvement in survival (5). The development of novel radiosensitizers is an active area of research, and many agents, effective in preclinical testing, are currently in clinical trials. The molecular determinants and optimal schedules for combination of HSP90 inhibitors with radiation have not been rigorously addressed.
We recently described that treatment schedule is critical for combination of DMAG with doxorubicin, as an example of DNA-damaging agent, in lymphoma cells (6). DMAG added 24 h after treatment with doxorubicin led to mitotic catastrophe and cell death with significant synergy regardless of p53 status, whereas loss of synergy, and even antagonism, was observed when DMAG was administered simultaneously with or before doxorubicin. The synergy required destabilization of a critical component of cell cycle progression, the checkpoint kinase CHK1 (6).
Here, we show that radiosensitization of NSCLC cells requires pretreatment with DMAG. In addition to previously noted inhibition of ATM in prostate cell lines (7), we established that DMAG impairs DNA repair in NSCLC lines at multiple levels, including inhibition of ATM and base excision repair (BER) machinery. Optimal scheduling of DMAG before radiation was only partially dependent on functional p53.
Materials and Methods
Reagents and Cells
NSCLC cell lines, NCI-H460 and A549, were obtained from the American Type Culture Collection and cultured in RPMI 1640 supplemented with 10% fetal bovine sera, penicillin/streptomycin, and glutamine at 37°C in 5% CO2. HSP90 inhibitor, DMAG, was obtained from the Cancer Therapy Evaluation Program, National Cancer Institute, stored in aliquots at −20°C as 10 mmol/L solution in DMSO, and diluted in media immediately before use. ATM inhibitor, KU55933, and apurinic/apyrimidinic endonuclease (APE1) inhibitor, CRT0044876, were obtained from Calbiochem.
Stable p53 knockdown (p53KD) isogenic cell line pairs from wild-type p53 (wtp53) expressing H460 and A549 cells were generated using pSUPER.retro.puro (Oligoengine) retroviral construct with short-hairpin shRNA sequence against human p53 (p53KD) or a scrambled (SC) sequence (8). Plasmids were introduced into Amphopack 293 cells using LipofectAMINE 2000 (Invitrogen). Fresh viral supernatants were collected, filtered, and applied to the target cells in the presence of 1 μg/mL polybrene. After 48 h, cells were selected by incubation with 0.5 μg/mL (H460) or 1 μg/mL (A549) puromycin (Sigma). Silencing of p53 was verified by Western blot showing p53 accumulation in response to doxorubicin.
Clonogenic Survival Assay
Preliminary studies were conducted to optimize the number of cells plated in clonogenic assays, aiming for 100 colonies per well. Cells were plated by triplicate on 6-well or 100-mm tissue culture plates and treated within 24 h. Cells were irradiated using a cesium-137 chamber at 1.7 Gy/min at indicated times simultaneously, before, or after exposure to DMAG, APE1, or ATM inhibitors. Colonies were fixed and stained with 0.5% crystal violet, and the number of colonies containing at least 50 cells, as examined by microscopy, was recorded 12 to 14 days later. Plating efficiency was calculated as the number of colonies divided by number of cells plated and normalized to the average plating efficiency of untreated samples, which was between 0.6 and 0.8. The average of these values was reported as “surviving fraction.” SD of the normalized values were calculated accordingly.
Cell CycleAnalysis
Cells at 60% to 80% confluency were exposed to radiation or DMAG as described above, fixed in 70% ethanol, stained with 50 μg/mL propidium iodide (Sigma) in the presence of 50 μg/mL RNase (Roche), and analyzed by flow cytometry using FACSCalibur (Becton Dickinson). Data were collected with Cell Quest Pro software (Becton Dickinson) from no fewer than 10,000 cells and analyzed with FlowJo.
BER Enzymatic Assay
The activities of each of the following BER enzymes, alkyl adenine DNA glycosylase, APE1, and DNA polymerase-β (Pol-β), were examined in whole-cell lysates using oligonucleotide-based assays (9–11). Enzymatic activities were expressed as femtomoles of oligonucleotide per microgram of protein per minute based on 100 femtomoles uncut product added to each reaction (10).
Alkaline Comet Assay
The comet assay was done essentially as described (12). Cells exposed to DMAG for 16 h were irradiated and the drug was removed immediately after. Three thousand cells were scraped into ice-cold PBS at indicated times and suspended in 150 μL NuSieve GTG at 42°C and 50 μL cell mixture was distributed in triplicate circles of a Comet slide (Trevigen). Agarose was allow to solidify for 20 min at 4°C, and cells were lysed for 1 h in 2.5 mol/L NaCl, 100 mmol/L EDTA, and 10 mmol/L Tris (pH 10.0–10.5) with freshly added 1% (v/v) Triton X-100 and 10% (v/v) DMSO. The slides were incubated in alkaline buffer [300 mmol/L NaOH and 1 mmol/L EDTA (pH >13)] for 30 min, and DNA was electrophoresed for 23 min at 25 V (0.90 V/cm) and 300 mA. The buffer was neutralized with 0.4 mmol/L Tris (pH 7.5), slides were fixed for 10 min in 100% ethanol, and DNA was stained with ethidium bromide (20 μg/mL). Images of 50 randomly selected cells were analyzed using High Capacity Slide Analysis System Software version 2.2.2 (Loats Associates) for percent DNA damage and tail moment.
Immunoblot
Cells at 60% to 80% confluency were exposed to radiation or DMAG as described above and processed for Western blot analysis as published (6) using the following primary antibodies: p53 (Ab-6) from Calbiochem; HSP70, AKT, and CHK1 from Cell Signaling Technology; ATM and phosphospecific ATM(S1981) from Rockland Immunochemicals; Pol-β from Biomeda; and APE1/REF-1 from Trevigen. Antibodies were visualized after horseradish peroxidase–labeled secondary antibodies (Amersham) by enhanced chemiluminescence reagent (Amersham).
Results
NSCLC Cells Are Relatively Resistant to DMAG Alone
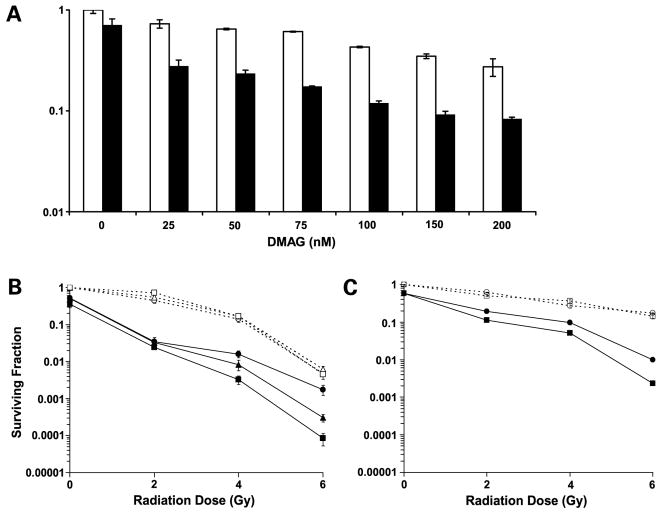
Studies of the pharmacokinetics of DMAG in patients have shown a peak plasma concentration of 36 ng/mL (55 nmol/L) DMAG with a half-life of 19 h after a single i.v. injection of 1.0 mg/m2 (13). Two-fold higher oral and i.v. doses are currently used in clinical trials. To find the dose of DMAG to be used in clonogenic studies, we examined the effect of an overnight exposure to increasing concentrations of DMAG alone or in combination with radiation (Fig. 1A). In spite of previously reported sensitivity of leukemia and melanoma cell lines (3), the NSCLC cell lines were relatively resistant to DMAG alone, with IC50 = 83 nmol/L, but showed decreased survival when exposed to DMAG before low-dose (2 Gy) radiation. Taking into consideration pharmacokinetics of DMAG in humans and rodents (13, 14) and the results from our assays, we selected 100 nmol/L DMAG as the dose for further studies.
Figure 1.
DMAG sensitizes lung cancer cell lines to radiation. A, dose-finding assay. Colony formation assay of H460 cells treated with increasing concentrations of DMAG for 16 h before radiation. Surviving fractions were calculated as plating efficiency-treated divided by plating efficiency-control in triplicate. Average ±SD. Cells treated with DMAG alone (white columns) or in combination with 2 Gy radiation (black columns). B, surviving fraction as measured by clonogenic assay of H460 cells exposed to 0, 2, 4, or 6 Gy radiation alone (dashed lines) or in the presence of 100 nmol/L DMAG (solid lines). Cells were radiated simultaneously (circles), after 8 h (triangles), or after 16 h (squares) treatment with DMAG. C, surviving fraction of A549 cells exposed to radiation alone (dashed line) or combination therapy (solid line) using simultaneous (circles) or 16-h pretreatment (squares) with DMAG. Results are normalized to untreated cells and presented as ±SD of triplicate samples. Results for one of three or more independent experiments.
DMAG Sensitizes NSCLC Cells to Radiation
Clonogenic survival assays were done to examine whether DMAG is a radiosensitizing agent for NSCLC and whether the schedule of administration modulates efficacy of DMAG. H460 cells were irradiated simultaneously or after 8 or 16 h of pretreatment with DMAG (Fig. 1B and C). The schedule of administration had substantial effect on radiosensitization, especially at ≥4 Gy. Maximal efficacy was observed in cells pretreated with DMAG for 16 h before radiation, whereas simultaneous exposure was less effective. Pretreatment with DMAG for 8 h or radiation before addition of DMAG were substantially less effective (Fig. 1B; data not shown). Similar observations were obtained using A549 cells, although these cells are more resistant to radiation and, consequently, to the combination therapy. Differential radiation sensitivity of A549 and H460 cells has been noted previously (15). The maximal radiosensitizing effect of DMAG was also achieved when A549 cells were irradiated after 16-h exposure to DMAG (Fig. 1C).
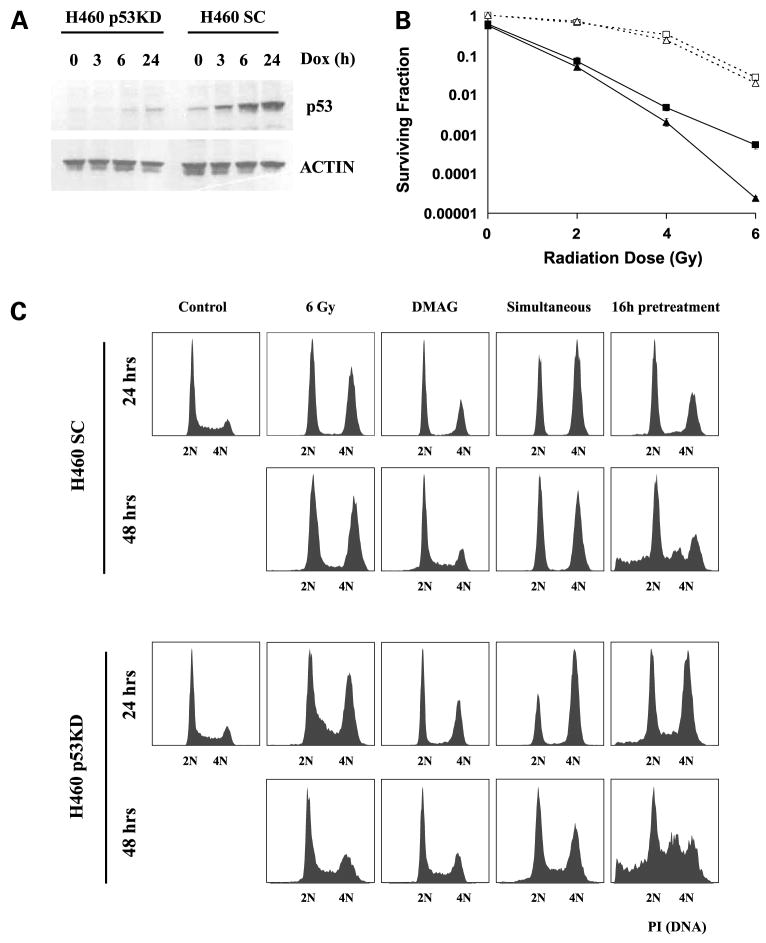
Radiosensitization by DMAG Is Only Partially Dependent on Functional p53
Deletion and mutations of the p53 tumor suppressor gene are associated with resistance to radiation and other therapies. Both cell lines used in this study express wtp53. To test the effect of p53 loss on DMAG-mediated radiosensitization, we generated isogenic cell lines in which wtp53 expression was silenced by RNA interference. The p53 protein has a short half-life; however, it is stabilized through post-translational modifications on DNA damage. Efficient suppression of p53 stabilization after exposure to doxorubicin was apparent in H460 cells transformed with p53 shRNA (H460 p53KD) compared with cells expressing scrambled shRNA sequence (H460 SC; Fig. 2A). Loss of p53 was associated with reproducible, albeit modest, radio-resistance compared with cells expressing scrambled shRNA (Fig. 2B). Radiation, administered after a 16-h exposure to DMAG, decreased clonogenic survival of isogenic cell types in response to low doses of radiation, although p53KD cells were more resistant to higher doses of radiation (Fig. 2B). Similar results were obtained using A549 SC and A549 p53KD cells (data not shown). Thus, although cells with wtp53 are more responsive to combination therapy, radiosensitization by DMAG does not require functional p53.
Figure 2.
Radiosensitization by DMAG does not require functional p53. A, expression of p53 in H460 cells that express shRNA-containing scrambled sequence (H460 SC) or p53 knockdown (H460 p53KD). Cells were plated to 60% to 80% confluence and exposed to 0.5 μg/mL doxorubicin to induce functional p53 for indicated times. Cell extracts were subjected to Western blot and probed with anti-p53 antibody. Actin was used as a loading control. B, surviving fraction of H460 SC (triangles) and H460 p53KD (squares) cells exposed to radiation alone (dashed lines) or irradiated at the end of 16-h exposure to 100 nmol/L DMAG (solid lines). Results are normalized to untreated cells. Mean ±SD of triplicate samples in one of three independent experiments. C, effect of radiation alone or in the presence of DMAG on cell cycle progression and apoptosis of H460 SC and H460 p53KD cells. Cells were examined at 24 and 48 h as indicated. Simultaneous treatment is compared with pretreatment with DMAG for 16 h. Note the appearance of a fraction of cells with sub-G1 DNA content in both H460 SC and p53KD cells preexposed to 12% and 19% DMAG, respectively. Results from one of three independent experiments.
To understand the molecular mechanisms of schedule-dependent radiosensitization by DMAG and their relation to p53 status, we examined early and late changes in cell cycle in cells that express wtp53 (H460 SC) and in H460 p53KD cells. Cells that express wtp53 usually undergo G1-S and G2-M arrest after DNA damage, whereas p53-deficient cells bypass G1-S arrest and accumulate in G2-M which is transient, and cells eventually reenter the cell cycle. Consistent with previously reported 20-h doubling time (16), radiation led to G2-M arrest within 24 h of wtp53 H460 cells, which was maintained for 48 h. In contrast, there was a transient accumulation in G2-M of p53KD cells, and cell cycle recovered by 48 h. Exposure to DMAG alone led to a loss of S phase and accumulation of cells with G2-M followed by recovery at 48 h in both cell types (Fig. 2C). It is important to note that DMAG is not a DNA-damaging agent, and its effects are fully reversible once the agent has been removed. For experiments shown in Fig. 2, cells were exposed to DMAG for 16 h, culture medium was replaced, and samples were analyzed 24 h after the beginning of the experiment (that is, 8 h after removal of DMAG). There was no significant increase in sub-G1 DNA content, a marker of apoptotic cell death, with single agent, or after simultaneous treatment of radiation with DMAG. In contrast, pretreatment with DMAG induced a sustained G2-M arrest and the appearance of a fraction of cells with sub-G1 DNA content in wtp53 and p53KD cell types. The sub-G1 fraction was in the range of 12% to 20% in independent experiments without significant differences between H460 SC and p53KD cells. The difference between the amount of sub-G1 fraction and clonogenic survival data is because clonogenic assays measure the combined ability of single cells to repair DNA, survive, and form colonies, whereas sub-G1 fraction shows only the immediate response to DNA damage.
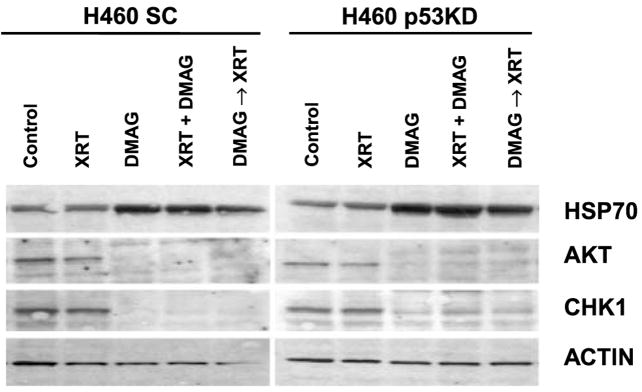
Effects of HSP90 Inhibition on Cell Survival Pathways Activated by Radiation
To determine the molecular mechanisms of enhanced cell death after pretreatment with DMAG, we examined changes in protein levels of AKT and CHK1, two key regulators of survival and cell cycle control. Both proteins require active HSP90 for proper folding and stability (17, 18), and their inhibition has been associated with decreased cell survival after radiation (19, 20). We compared these changes between cells that express wtp53 (H460 SC) and p53KD. Expression of AKT and CHK1 was decreased in cells exposed to DMAG regardless of schedule of administration in relation to radiation (Fig. 3). No substantial differences were observed between cells isogenic for p53 expression. As expected, both cell types had compensatory induction of HSP70, a functional indicator of HSP90 inhibition (21). Thus, in spite of significant schedule-dependent differences in cell survival, there were no differences in the short-term effects of DMAG on expression of key proteins involved in survival after radiation.
Figure 3.
DMAG induces down-regulation of cell survival proteins regardless of the schedule of administration. Analysis of protein expression in H460 SC and p53KD cells 24 h after radiation with or without 100 nmol/L DMAG administered simultaneously with radiation or before radiation for 16 h. Top, single treatment or combination therapy.
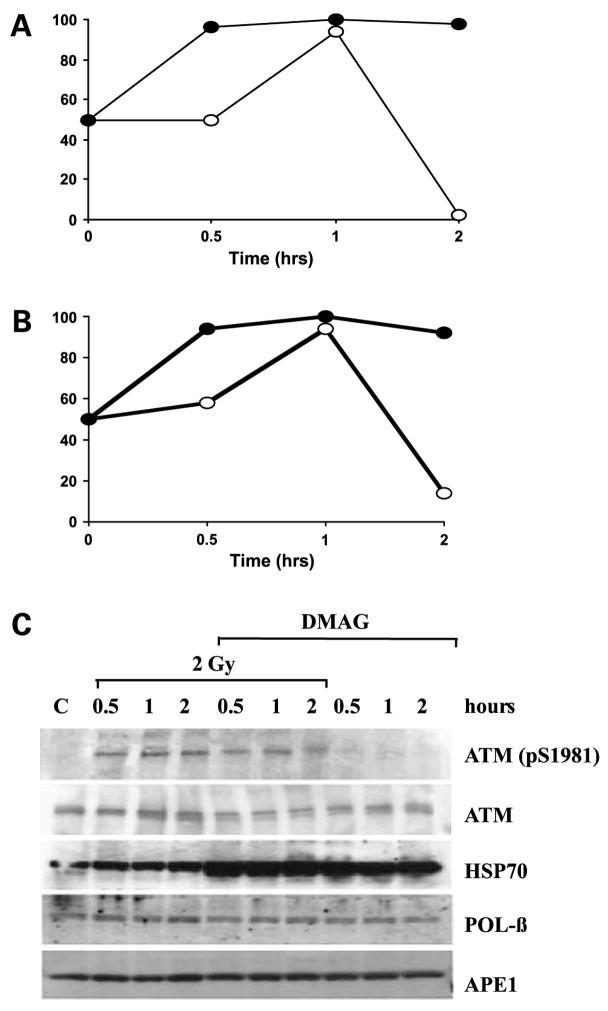
Pretreatment with DMAG Impairs Radiation-Induced DNA Repair
Because depletion of key HSP90-regulated cell survival can cell cycle progression proteins did not explain the difference in radiosensitization observed by changing the schedule of exposure to DMAG, we examined whether DMAG interferes with the kinetics of radiation-induced DNA repair. We did an alkaline comet assay, a sensitive method for quantifying both single-strand and double-strand DNA breaks (22, 23). Consistent with a published report (7), radiation induced a transient surge in DNA repair in H460 cells with subsequent decline in percent total DNA damage below baseline. Pretreatment with DMAG significantly enhanced this effect with persistent DNA damage over 2 h (Fig. 4A). Tail moment, a measure that takes into account the amount of DNA damage per cell, was also increased in DMAG-treated cells and maintained for up to 2 h above the level induced by radiation alone (Fig. 4B). In a separate set of experiments, we found that percent DNA damage and tail moment returned to baseline levels by 4 h (data not shown). There was no difference in DNA damage compared with radiation alone when cells were treated simultaneously with DMAG and radiation or in cells that received DMAG 24 h after radiation (data not shown).
Figure 4.
Radiation-induced DNA damage repair is impaired in cells pretreated with DMAG. A, DNA damage as quantified by alkaline comet assay. Percent of cells with DNA damage above the average for control untreated cells. B, tail moments above the mean values of untreated cells. Cells were treated with radiation alone (open circles) or radiation after exposure to DMAG for 16 h (closed circles). Results are means from counts of 50 random cells done in triplicate samples. C, Western blot analysis of ATM, HSP70, APE1, and Pol-β. Cell extracts were harvested at indicated times relative to sham-treated control cells. Results from one of two independent experiments.
A previous report showed reduced phosphorylation of ATM in response to 4 Gy radiation in prostate cells preexposed to another HSP90 inhibitor, 17-allylamino-17-demethoxygeldanamycin (7), which indicated inhibition of double-strand break DNA repair. Although we used lower doses of radiation (2 Gy) that lead mainly to oxidative damage with only few DNA breaks, we detected an increase in ATM phosphorylation within 30 min (Fig. 4C). Cells pretreated with DMAG had a decrease in phospho-ATM following radiation. A compensatory accumulation of HSP70 is included for comparison (21). These data support that DMAG interferes with activation of ATM-mediated DNA double-strand break repair in response to radiation.
DMAGBlocks Radiation-Induced Activation of BER
To determine the mechanism of synergy between DMAG and lower doses of radiation that induce predominantly oxidative stress and DNA repair by activation of BER, we measured the activity of three key enzymes involved in BER: alkyl adenine DNA glycosylase, APE1, and Pol-β. The enzymatic activities of APE1 and Pol-β were increased within 1 h after radiation (Fig. 5A and B), whereas activity of alkyl adenine DNA glycosylase was not changed (data not shown). All enzymatic activities returned to baseline within 4 h of radiation. Peak activation of APE1 was observed after 2 Gy (Fig. 5A), whereas activation of Pol-β was higher after 1 Gy (Fig. 5B). Exposure to DMAG before radiation suppressed activation of both enzymes. Under these experimental conditions, Pol-β and APE1 protein levels were unchanged (Fig. 4C). These data indicate that their stability is not regulated by HSP90.
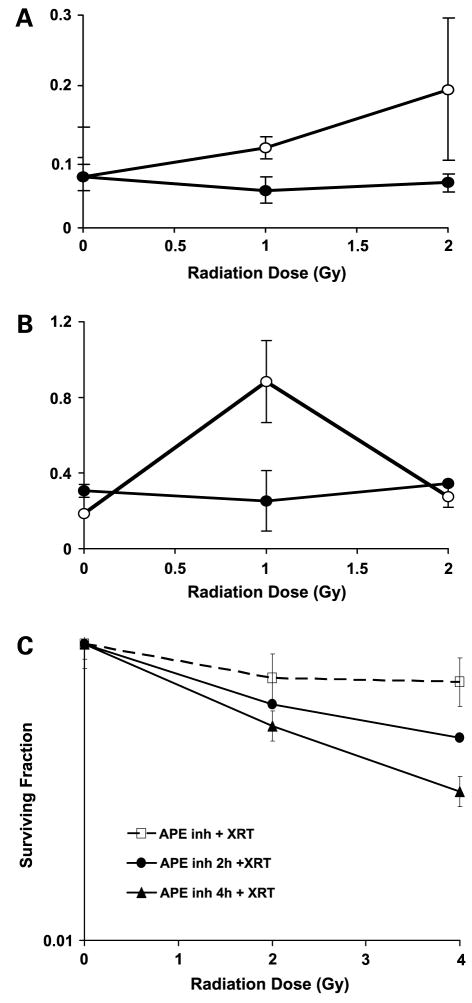
Figure 5.
Inhibition of BER by DMAG enhances the effect of radiation. APE1 (A) and Pol-β (B) enzymatic activities were measured in whole-cell extracts from cells treated with 2 Gy radiation alone (open circles) or at the end of pretreatment with DMAG (closed circles). Activities were normalized to the average activity of control in the absence of radiation. Mean ±SD. C, effect of APE1 inhibitor, CRT0044876, on clonogenic survival of cells exposed to 2 and 4 Gy radiation. Cells were exposed to CRT0044876 simultaneously with radiation (dashed line, squares), 2 h before (solid line, circles), or 4 h before (solid line, triangles) radiation. Results are normalized to cells exposed to CRT0044876 alone. Mean ±SD of triplicate samples from two independent experiments.
To examine whether inhibition of BER and ATM-mediated DNA repair mimic the effects of DMAG on H460 cells, we used two recently developed specific inhibitors: APE1 inhibitor, CRT0044876 (24), and ATM inhibitor, KU55933 (25). Because APE1 activation is essential for removal of damaged bases generated by oxidative stress and it regulates the activity of Pol-β, which fills the gap, inhibition of APE1 is a key for activity of both enzymes (26). As shown in Fig. 5C, CRT0044876 significantly enhanced the effect of 2 and 4 Gy radiation. In addition, pretreatment for 4 h was better than 2 h, and simultaneous treatment was virtually ineffective. Addition of APE1 inhibitor after radiation had no effect (data not shown). Interestingly, ATM inhibitor KU55933 was more effective when added 2 h rather than 4 h before radiation, which may reflect rapid turnover of activated ATM in response to DNA damage (data not shown).
Discussion
Several distinct lines of evidence indicate that the effects of radiation are significantly enhanced by HSP90 inhibitors if these agents are added before radiation. We established that DMAG blocks two independent DNA repair mechanisms, BER and double-strand DNA repair mediated by ATM. Although HSP90 inhibitors block multiple survival pathways, we propose that the schedule-dependent effect on radiosensitization is due to inhibition of DNA repair pathways, and it is only partially dependent on functional p53.
Depletion of several components of survival pathways, known to be regulated by HSP90 inhibitors, were previously proposed to mediate radiosensitization by these agents (27). We found that depletion of AKT and other survival and cell cycle checkpoint components were evident within 24 h regardless of schedule of DMAG administration. Nevertheless, the maximal effect on overall long-term survival was observed only when DMAG was administered overnight before radiation. Thus, inhibition of survival pathways is likely to contribute to, but cannot solely be responsible for, the significant differences in radiosensitization observed with different treatment schedules.
Chemotherapeutic agents and radiation activate several overlapping and unique signal transduction pathways that lead to cell cycle checkpoints, DNA repair, and apoptosis. The advantage of using HSP90 inhibitors as radiosensitizers is that these agents impair multiple intracellular survival pathways activated in response to radiation, such as abrogation of G2 arrest (28) and delay DNA repair after high doses of radiation. The multiple types of DNA damage induced by radiation are reviewed elsewhere (29–31). Most DNA damage induced by low, clinically achievable, doses of γ irradiation, such as 2 to 4 Gy in vitro, are secondary to oxidative stress and formation of free radicals leading to a rapid activation of BER machinery. Oxidative stress leads to release of free bases from DNA generating strand breaks with various sugar modifications and abasic sites. It has been estimated that endogenous reactive oxygen species result in ~2 × 105 base lesions per cell per day (31) Recent data indicate that removal of damaged bases by DNA glycosylases is followed by formation of a single-strand break by APE1. APE1 regulates the recruitment and activity of Pol-β, which subsequently fills the gap (26). Recent information indicates that the next step is formation of an active complex at replication forks in cycling cells that contain other components of BER, DNA protein kinase, and cyclin A (32). Cells pretreated with DMAG were unable to activate APE1 and, subsequently, Pol-β, critical components of BER. The decrease in cell survival and the delay in removal of AP sites were reproduced by pretreatment with APE1 inhibitor, CRT0044876, before radiation. These findings are novel and indicate that DMAG impairs BER in response to ionizing radiation. Because activation of BER does not involve p53, these findings may explain why the effect of DMAG was similar in H460 SC and p53KD cells following lower doses of radiation.
The mechanisms of BER activation in response to ionizing radiation and other injuries are not well defined. Increase in APE1 and Pol-β protein levels was observed in some, but not other, studies (9, 33). We found no change in APE1 or Pol-β protein levels in cells exposed to radiation and no destabilization of these proteins in response to DMAG. Post-translational modifications or intracellular trafficking have been proposed to regulate radiation-induced activation of BER, but there are no reports supporting these hypotheses. Further studies are needed to establish whether inhibition of BER is an additional target for cancer therapies.
In contrast to the effects of ionizing radiation, higher doses of radiation lead to double-strand DNA breaks, and this type of DNA repair is predominantly mediated by ATM pathway (31). We found that ATM phosphorylation was evident even after 2 Gy of radiation, and this response was blunted by pretreatment with DMAG. These data are consistent with a previous report that ATM phosphorylation after 4 Gy of pancreatic cancer cells is decreased by pretreatment with another HSP90 inhibitor, 17-allylamino-17-demethoxygeldanamycin (7). We found no change in total ATM protein that indicates no protein degradation. Thus, similar to the regulation of APE1 and Pol-β, DMAG may interfere with ATM intracellular trafficking or activation of upstream signal transduction pathways.
Inactivation of p53 is known to contribute to radiation resistance because p53 is critical for activation of ATM and cell cycle arrest. We found that functional p53 is not required for radiosensitization induced by DMAG. The discrepancy of our data with a recent report indicating that a HSP90 inhibitor, 17-allylamino-17-demethoxygeldanamycin, is more effective in cells with wtp53 compared with cells with mutant p53 (21) may be because higher doses of radiation were used in that study as well as a less effective treatment schedule. In that study, cells were irradiated 30 min after addition of 17-allylamino-17-demethoxygeldanamycin, which may be comparable with our simultaneous or postradiation schedule. Our findings that p53 depletion only partially contributes to cell survival are consistent with the critical role of BER, which, in contrast to ATM-mediated DNA repair, is not dependent on functional p53.
“Oncogene addiction,” a term that describes tumor cells that are more sensitive to inhibition of constitutively active growth-promoting pathways than are normal cells, is well documented for several oncogenes and tumor types. More recently, it has become apparent that tumor cells are protected by multiple pathways that communicate through “cross-talk.” Therapies that focus on an individual molecule or pathway are often less effective than those which simultaneously target multiple pathways. Multiple prosurvival and DNA repair pathways must be inhibited to improve the outcome and maximize the benefit from each agent. Current strategies for enhancing tumor radiosensitivity are focused on combining radiation, which induces activation of prosurvival and DNA damage repair pathways, with molecularly targeted therapies that interfere with both processes. Although inhibition of cell survival pathways contribute to overall efficacy of HSP90 inhibitors, DMAG is most effective as radiosensitizer when administered before radiation because of its suppression of DNA repair at multiple levels, including BER and ATM-regulated pathways. Combining radiation with HSP90 inhibitors is an attractive option for future clinical trials.
Acknowledgments
We thank Dr. Curtis C. Harris for scientific advice and support, Karen MacPherson and Dorothea Dudek for editorial assistance, and Mohamed Khan and Judith Welsh for technical support.
Grant support: Supported in part by the Intramural Research Program of the NIH, Center for Cancer Research, NCI.
Footnotes
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- 1.McDonald E, Jones K, Brough PA, Drysdale MJ, Workman P. Discovery and development of pyrazole-scaffold Hsp90 inhibitors. Curr Top Med Chem. 2006;6:1193–203. doi: 10.2174/156802606777812086. [DOI] [PubMed] [Google Scholar]
- 2.Uehara Y, Hori M, Takeuchi T, Umezawa H. Phenotypic change from transformed to normal induced by benzoquinonoid ansamycins accompanies inactivation of p60src in rat kidney cells infected with Rous sarcoma virus. Mol Cell Biol. 1986;6:2198–206. doi: 10.1128/mcb.6.6.2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hollingshead M, Alley M, Burger AM, et al. In vivo antitumor efficacy of 17-DMAG (17-dimethylaminoethylamino-17-demethoxygeldanamycin hydrochloride), a water-soluble geldanamycin derivative. Cancer Chemother Pharmacol. 2005;56:115–25. doi: 10.1007/s00280-004-0939-2. [DOI] [PubMed] [Google Scholar]
- 4.Gossett DR, Bradley MS, Jin X, Lin J. 17-Allyamino-17-demethoxygeldanamycin and 17-N,N-dimethyl ethylene diamine-geldanamycin have cytotoxic activity against multiple gynecologic cancer cell types. Gynecol Oncol. 2005;96:381–8. doi: 10.1016/j.ygyno.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 5.Pijls-Johannesma M, De Ruysscher D, Vansteenkiste J, Kester A, Rutten I, Lambin P. Timing of chest radiotherapy in patients with limited stage small cell lung cancer: a systematic review and meta-analysis of randomised controlled trials. Cancer Treat Rev. 2007;33:461–73. doi: 10.1016/j.ctrv.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Robles AI, Wright MH, Gandhi B, et al. Schedule-dependent synergy between the heat shock protein 90 inhibitor 17-(dimethylaminoethylamino)-17-demethoxygeldanamycin and doxorubicin restores apoptosis to p53-mutant lymphoma cell lines. Clin Cancer Res. 2006;12:6547–56. doi: 10.1158/1078-0432.CCR-06-1178. [DOI] [PubMed] [Google Scholar]
- 7.Dote H, Burgan WE, Camphausen K, Tofilon PJ. Inhibition of hsp90 compromises the DNA damage response to radiation. Cancer Res. 2006;66:9211–20. doi: 10.1158/0008-5472.CAN-06-2181. [DOI] [PubMed] [Google Scholar]
- 8.Brummelkamp TR, Bernards R, Agami R. A system for stable expression of short interfering RNAs in mammalian cells. Science. 2002;296:550–3. doi: 10.1126/science.1068999. [DOI] [PubMed] [Google Scholar]
- 9.Zurer I, Hofseth LJ, Cohen Y, et al. The role of p53 in base excision repair following genotoxic stress. Carcinogenesis. 2004;25:11–9. doi: 10.1093/carcin/bgg186. [DOI] [PubMed] [Google Scholar]
- 10.Hofseth LJ, Khan MA, Ambrose M, et al. The adaptive imbalance in base excision-repair enzymes generates microsatellite instability in chronic inflammation. J Clin Invest. 2003;112:1887–94. doi: 10.1172/JCI19757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sukhanova MV, Khodyreva SN, Lebedeva NA, Prasad R, Wilson SH, Lavrik OI. Human base excision repair enzymes apurinic/apyrimidinic endonuclease 1 (APE1), DNA polymerase β and poly(ADP-ribose) polymerase 1: interplay between strand-displacement DNA synthesis and proofreading exonuclease activity. Nucleic Acids Res. 2005;33:1222–9. doi: 10.1093/nar/gki266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singh NP, McCoy MT, Tice RR, Schneider EL. A simple technique for quantitation of low levels of DNA damage in individual cells. Exp Cell Res. 1988;175:184–91. doi: 10.1016/0014-4827(88)90265-0. [DOI] [PubMed] [Google Scholar]
- 13.Hwang K, Scripture CD, Gutierrez M, Kummar S, Figg WD, Sparreboom A. Determination of the heat shock protein 90 inhibitor 17-dimethylaminoethylamino-17-demethoxygeldanamycin in plasma by liquid chromatography-electrospray mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci. 2006;830:35–40. doi: 10.1016/j.jchromb.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 14.Glaze ER, Lambert AL, Smith AC, et al. Preclinical toxicity of a geldanamycin analog, 17-(dimethylaminoethylamino)-17-demethoxygeldanamycin (17-DMAG), in rats and dogs: potential clinical relevance. Cancer Chemother Pharmacol. 2005;56:637–47. doi: 10.1007/s00280-005-1000-9. [DOI] [PubMed] [Google Scholar]
- 15.Shareef MM, Cui N, Burikhanov R, et al. Role of tumor necrosis factor-alpha and TRAIL in high-dose radiation-induced bystander signaling in lung adenocarcinoma. Cancer Res. 2007;67:11811–20. doi: 10.1158/0008-5472.CAN-07-0722. [DOI] [PubMed] [Google Scholar]
- 16.Carmichael J, DeGraff WG, Gazdar AF, Minna JD, Mitchell JB. Evaluation of a tetrazolium-based semiautomated colorimetric assay: assessment of radiosensitivity. Cancer Res. 1987;47:943–6. [PubMed] [Google Scholar]
- 17.Sato S, Fujita N, Tsuruo T. Modulation of Akt kinase activity by binding to Hsp90. Proc Natl Acad Sci U S A. 2000;97:10832–7. doi: 10.1073/pnas.170276797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arlander SJ, Eapen AK, Vroman BT, McDonald RJ, Toft DO, Karnitz LM. Hsp90 inhibition depletes Chk1 and sensitizes tumor cells to replication stress. J Biol Chem. 2003;278:52572–7. doi: 10.1074/jbc.M309054200. [DOI] [PubMed] [Google Scholar]
- 19.Albert JM, Kim KW, Cao C, Lu B. Targeting the Akt/mammalian target of rapamycin pathway for radiosensitization of breast cancer. Mol Cancer Ther. 2006;5:1183–9. doi: 10.1158/1535-7163.MCT-05-0400. [DOI] [PubMed] [Google Scholar]
- 20.Carrassa L, Broggini M, Erba E, Damia G. Chk1, but not Chk2, is involved in the cellular response to DNA damaging agents: differential activity in cells expressing or not p53. Cell Cycle. 2004;3:1177–81. [PubMed] [Google Scholar]
- 21.Shintani S, Zhang T, Aslam A, Sebastian K, Yoshimura T, Hamakawa H. p53-dependent radiosensitizing effects of Hsp90 inhibitor 17-allylamino-17-demethoxygeldanamycin on human oral squamous cell carcinoma cell lines. Int J Oncol. 2006;29:1111–7. doi: 10.3892/ijo.29.5.1111. [DOI] [PubMed] [Google Scholar]
- 22.Collins AR. The comet assay for DNA damage and repair: principles, applications, and limitations. Mol Biotechnol. 2004;26:249–61. doi: 10.1385/MB:26:3:249. [DOI] [PubMed] [Google Scholar]
- 23.Hartmann A, Agurell E, Beevers C, et al. Recommendations for conducting the in vivo alkaline Comet assay. 4th International Comet Assay Workshop Mutagenesis. 2003;18:45–51. doi: 10.1093/mutage/18.1.45. [DOI] [PubMed] [Google Scholar]
- 24.Madhusudan S, Smart F, Shrimpton P, et al. Isolation of a small molecule inhibitor of DNA base excision repair. Nucleic Acids Res. 2005;33:4711–24. doi: 10.1093/nar/gki781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hickson I, Zhao Y, Richardson CJ, et al. Identification and characterization of a novel and specific inhibitor of the ataxia-telangiectasia mutated kinase ATM. Cancer Res. 2004;64:9152–9. doi: 10.1158/0008-5472.CAN-04-2727. [DOI] [PubMed] [Google Scholar]
- 26.Hegde ML, Hazra TK, Mitra S. Early steps in the DNA base excision/single-strand interruption repair pathway in mammalian cells. Cell Res. 2008;18:27–47. doi: 10.1038/cr.2008.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Matsumoto Y, Machida H, Kubota N. Preferential sensitization of tumor cells to radiation by heat shock protein 90 inhibitor geldanamycin. J Radiat Res (Tokyo) 2005;46:215–21. doi: 10.1269/jrr.46.215. [DOI] [PubMed] [Google Scholar]
- 28.Bull EE, Dote H, Brady KJ, et al. Enhanced tumor cell radiosensitivity and abrogation of G2 and S phase arrest by the Hsp90 inhibitor 17-(dimethylaminoethylamino)-17-demethoxygeldanamycin. Clin Cancer Res. 2004;10:8077–84. doi: 10.1158/1078-0432.CCR-04-1212. [DOI] [PubMed] [Google Scholar]
- 29.Ward JF. The yield of DNA double-strand breaks produced intracellularly by ionizing radiation: a review. Int J Radiat Biol. 1990;57:1141–50. doi: 10.1080/09553009014551251. [DOI] [PubMed] [Google Scholar]
- 30.Iliakis G, Wang Y, Guan J, Wang H. DNA damage checkpoint control in cells exposed to ionizing radiation. Oncogene. 2003;22:5834–47. doi: 10.1038/sj.onc.1206682. [DOI] [PubMed] [Google Scholar]
- 31.Rouse J, Jackson SP. Interfaces between the detection, signaling, and repair of DNA damage. Science. 2002;297:547–51. doi: 10.1126/science.1074740. [DOI] [PubMed] [Google Scholar]
- 32.Parlanti E, Locatelli G, Maga G, Dogliotti E. Human base excision repair complex is physically associated to DNA replication and cell cycle regulatory proteins. Nucleic Acids Res. 2007;35:1569–77. doi: 10.1093/nar/gkl1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Inoue M, Shen GP, Chaudhry MA, Galick H, Blaisdell JO, Wallace SS. Expression of the oxidative base excision repair enzymes is not induced in TK6 human lymphoblastoid cells after low doses of ionizing radiation. Radiat Res. 2004;161:409–17. doi: 10.1667/3163. [DOI] [PubMed] [Google Scholar]