Abstract
Smoking is associated with poor symptom control and impaired therapeutic responses in asthma. A total of 843 patients with asthma were recruited. The patients received treatment for 1 yr according to the severity of their asthma. We compared the forced expiratory volume in 1 sec (FEV1), the ratio of FEV1 to forced vital capaity (FVC), atopy, total IgE, emphysema on high-resolution computed tomography (HRCT), the number of near-fatal asthma attacks, and physiological fixed airway obstruction between the smoking and nonsmoking groups. The study population consisted of 159 (18.8%) current smokers, 157 (18.7%) ex-smokers, and 525 (62.5%) nonsmokers. Although the prevalence of atopy was not different between the smoking and nonsmoking groups, the total IgE was higher among the smokers than the nonsmokers. Compared with the nonsmoking group, the smokers had a lower FEV1 % predicted and forced expiratory flow between 25 and 75% of FVC. A greater prevalence of emphysema and a significantly higher number of asthmatic patients with fixed airway obstruction were detected in the smoking versus nonsmoking group. The 37.5% of asthmatic patients who were former or current smokers showed decreased pulmonary function and increased IgE, emphysema on HRCT, and fixed airway obstruction, indicating that smoking can modulate the clinical and therapeutic responses in asthma.
Keywords: Smoking, Asthma, Atopy, Immunoglobulin E, Remodeling
INTRODUCTION
Cigarette smoking and asthma are associated with poor symptom control and impaired therapeutic responses to anti-asthma drugs (1). In the developed world, approximately 25% of the general population currently smokes cigarettes (2) and a further 25% are former smokers; the smoking rates are similar among adults with asthma (3-5). Higher levels of smoking are seen in patients with asthma who attend emergency departments with exacerbations (4). Compared with asthmatic nonsmokers, smokers with asthma have worse symptom control (3), an accelerated decline in lung function (6), and an increased mortality rate (7). Asthmatic smokers have more severe asthmatic symptoms (2, 3), greater need for rescue medications (8), and worse indices of health status in comparison with asthmatics who have never smoked (8).
The effect of smoking on the metabolism of drugs such as theophylline is well known, but recent study has reported that smokers with asthma had a poor responsiveness to corticosteroids (9). More studies are needed to elucidate the smoking-induced changes in lung function and airway inflammation that may result in changes in clinical variable outcomes. However, an analysis of the association between smoking status and asthma has not been fully performed in patients with asthma. In the present study, we evaluated the relationship between smoking status and clinical and therapeutic parameters in asthmatic patients.
MATERIALS AND METHODS
Subjects and study protocol
Subjects were recruited from the Asthma Genome Research Center of Soonchunhyang University Hospital, Bucheon, Korea. On the first day of the study, a clinical history was obtained from each patient, using a physician-administered questionnaire. Chest PA radiography, a Water's view, allergy skin prick tests, and spirometry, including bronchodilator responses after the inhalation of two puffs containing 100 µg of aerosolized albuterol, were performed. Blood and sputum were sampled for differential cell counts. On the second visit, airway hyperresponsiveness (AHR) was measured in cases with a forced expiratory volume in 1 sec (FEV1) % predicted of 70% or greater. All patients showed airway reversibility, as documented by an inhalant bronchodilator-induced improvement of more than 15% in FEV1, and/or airway hyperreactivity to less than 10 mg/mL of methacholine (10). The asthmatic patients (N=843) with mild to severe symptoms had comparable clinical symptoms and physical characteristics, according to the Global Initiative for Asthma (GINA) guidelines (11). Smoking status was assessed by the following questions: 1) have you ever smoked cigarettes, with yes or no response options. 2) do you smoke cigarettes now with responses yes, no; 3) if not a current cigarette smoker, did you smoke in the past 6 months; and From these questions a person was assigned to be a current, ex-, or never-smoker. Subjects were asked to record how many cigarettes they smoked. The exclusion criteria included FEV1/forced vital capacity (FVC) less than 70% and diffusing capacity less than 80%. All subjects provided informed consent to participate in the study, and the protocols were approved by the local ethics committee.
Study intervention
Study patients received anti-asthma drugs according to their asthma severity for 1 yr, based on the GINA guidelines (11). The patients received long-term control medication consisting of inhaled glucocorticoids, inhaled glucocorticoids plus long-acting inhaled β2-agonists, sustained-release theophylline, a leukotriene modifier, or oral glucocorticoids, according to GINA guidelines (11). Patients also received rapid-relief medication consisting of two puffs of inhaled salbutamol (100 µg/dose) and two puffs of inhaled ipratropium bromide (20 µg/dose), as needed.
Fixed airway obstruction (11) as a functional marker of airway remodeling was defined as both FEV1/FVC and predicted FEV1 of less than 75% when patients with asthma had controlled status after anti asthma treatment for 1 yr according to GINA guidelines. We assessed the effects of emphysema by chest radiography or high-resolution computed tomography (HRCT) and recorded the number of near-fatal asthma attacks during the 1-yr anti-asthma treatment. Emphysema (12) was defined as a focal area of very low attenuation, usually without definable wall, that was surrounded by higher attenuation normal lung parenchyma. Near-fatal asthma was defined as the admission of a patient with asthma to ward or an intensive care unit due to acute respiratory failure matching the following criteria: the presence of hypercapnia (PaCO2, >45 mmHg) and signs of hypoxia (cyanosis or PaO2, <60 mmHg) with a duration of exacerbation of less than 7 days, according to GINA guidelines (13). During the initial 7 days of treatment for near-fatal asthma, steroids (prednisolone 2 mg/kg/day or an equivalent dose of methylprednosone) and aminophylline (5 mg/kg/day) were administered intravenously with concomitant inhalation of an aqueous β2-agonist (salbutamol) as needed. On the 7th day of treatment, the systemic steroid was replaced with an inhaled steroid.
Lung function tests
Baseline FVC and FEV1 measurements were obtained in the absence of recent bronchodilator use (within 8 hr) according to the American Thoracic Society criteria (14). Basal and post-bronchodilator FEV1, FVC, and forced expiratory flow between 25% and 75% FVC (FEF25-75%) were measured between 1:00 and 4:00 pm. AHR was measured using the methacholine challenge test and was expressed as the provocation concentration that caused a fall in the FEV1 of 20% (PC20), in non-cumulative units (15).
Sputum examination
Sputum was induced using isotonic saline that contained a short-acting bronchodilator, as described by Norzila et al. (16). The samples were treated within 2 hr of collection, according to the method of Pizzichini et al. (17) with a minor modification. Briefly, all visible portions with greater solidity were carefully selected and placed in a pre-weighed Eppendorf tube. The samples were treated by adding eight volumes of 0.05% dithiothreitol (Sputolysin; Calbiochem Corp., San Diego, CA, U.S.A.) in Dulbecco's phosphate-buffered saline (D-PBS). One volume of protease inhibitors (0.1 M EDTA and 2 mg/mL phenylmethylsulfonylfluoride) was added to 100 volumes of the homogenized sputum, and the total cell count was determined with a hemocytometer. The cells of the homogenized sputum were collected by cytocentrifugation, and 500 cells were examined on each sputum slide after staining with Diff-Quick (American Scientific Products, Chicago, IL, U.S.A.).
IgE measurements and allergy skin tests
Total IgE was measured using a UniCAP system (Pharmacia Diagnostics, Uppsala, Sweden). Allergy skin prick tests were performed using commercially available inhalant allergens, which included dust mites (Dermatophagoides farinae and D. pteronyssinus, Bencard Co., Devon, U.K.) and histamine (1 mg/mL). None of the subjects had received oral antihistamines during the 3 days preceding the study. All of the tests included positive (1 mg/mL histamine) and negative (diluent) controls. After 15 min, the mean diameter of the wheals formed by the allergens (A) was compared with that formed by histamine (H). If the former was the same or larger than the latter (A/H ratio, ≥1.0), the reaction was deemed positive. Atopy was determined by the presence of an immediate skin reaction to one or more aeroallergens, as previously described (18).
Statistical analysis
Group differences were compared using a two-sample t-test, Wilcoxon rank-sum test, or Pearson's chi-square test for normally distributed, skewed, or categorical data, respectively. A p value of less than 0.05 was considered significant.
RESULTS
Demographic profiles of the study subjects
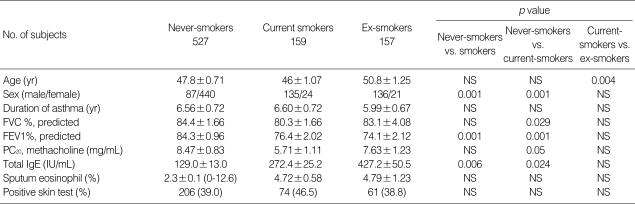
Descriptive statistics of the asthmatic patients by smoking status are shown in Table 1. The study population included 159 (18.8%) current smokers (cigarette smoking history, 23.9±4.0 pack-years), 157 (18.7%) ex-smokers (cigarette smoking history, 23.4±3.7 pack-years), and 525 (62.5%) nonsmokers (Table 1). The ratio of males to females was higher among smokers than nonsmokers (males/females; 171/45 vs. 87/440, p<0.001).
Table 1.
Clinical profiles of the study subjects
Plus-minus values are mean±S.E.
NS, not significant; NC, normal contols; PC20 methacholine, the concentration of methacholine required to decrease the FEV1 by 20%; FEV1, forced expiratory volume in one second; FVC, forced vital capacity.
Comparison of IgE and atopy by smoking status
Although the prevalence of atopy was not different between the smoking and nonsmoking groups, the total IgE was higher in the smoking group (272.2±25.4 vs. 129.0±13.0 U/L, p=0.006, Table 1).
Comparison of pulmonary function and severity of asthma by smoking status
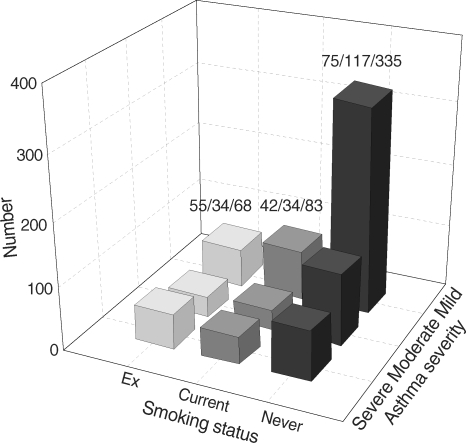
Compared with the nonsmoking group, the smoking group had lower FEV1 % predicted (Table 1) and FEF25-75% (34.2±2.2% vs. 72.9±1.6%, p<0.001). The proportion of asthmatic patients with severe symptoms was higher in the smoking than the nonsmoking group (exsmokers [mild/moderate/severe] vs. current smokers vs. nonsmokers: 42/34/83 vs. 55/34/68 vs. 75/117/335, p<0.01, Fig. 1).
Fig. 1.
Asthma severity according to smoking status.
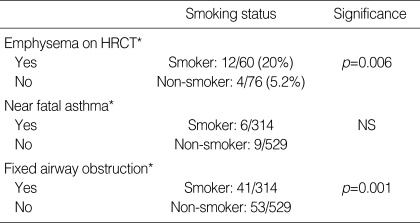
Comparison of emphysema on HRCT and fixed airway obstruction by smoking status
There was no difference in the proportion of near-fatal asthma attacks between the smokers and nonsmokers (Table 2). Emphysema was detected more often in the smoking than the nonsmoking group (12/60 vs. 4/76, p=0.001, Table 2). The proportion of asthmatic patients with fixed airway obstructions defined as the FEV1/FVC and FEV1 both of less than 75% following anti-asthma treatment were significantly higher in the smoking group than in the nonsmoking group (41/314 vs. 53/555, p=0.001, Table 2).
Table 2.
Comparison of emphysema on HRCT, airway remodeling, and near fatal asthma attack by smoking status (χ2 test)
*Emphysema was defined as a focal area of very low attenuation, usually without definable wall, that was surrounded by higher attenuation normal lung parenchyma. Near-fatal asthma* was defined as the admission of a patient with asthma to ward or an intensive care unit due to acute respiratory failure matching the following criteria: the presence of hypercapnia (PaCO2, >45 mmHg) and signs of hypoxia (cyanosis or PaO2, <60 mmHg) with a duration of exacerbation of less than 7 days, according to GINA guidelines. Fixed airway obstruction* as a functional marker of airway remodeling was defined as both FEV1/FVC and predicted FEV1 of less than 75% when patients with asthma had controlled status after anti asthma treatment for 1 yr according to GINA guidelines.
DISCUSSION
In this study, we observed that smoking was associated with asthma severity, decreased pulmonary function, and increased total IgE, emphysema on HRCT, and fixed airway obstruction.
The rate of smoking has been reported to be similar between adults with and without asthma, and the smoking rate in our study (18.8%) was similar to these previously reported rates (3, 5). The smoking rate was higher among males than females in our study population.
The morbidity and mortality from asthma are both increased in patients who smoke cigarettes compared with patients who have never smoked (2).
Asthmatic smokers have more severe asthmatic symptoms (2, 3), a greater need for rescue medication (8), and worse indices of health status compared with subjects who have never smoked (8). Smoking a cigarette can cause acute bronchoconstriction, although tobacco smoke does not act as an acute irritant in all patients (19). The baseline FEV1 is directly related to the immediate response to inhaling cigarette smoke (20), suggesting that asthmatic smokers with poorer lung function may be particularly susceptible to the acute effect of tobacco smoke. In our study, asthmatic patients who smoked had a lower FEV1 than those who did not smoke, suggesting that smokers with asthma have poorer lung function.
Visits to an emergency department as a result of exacerbations of asthma occur more frequently among heavy cigarette smokers with asthma following days with high levels of ambient ozone pollution (21). Hospital admission rates for asthma and hospital-based care are increased in smokers (22), although possibly not in younger adults (23). There is conflicting evidence as to whether current smoking is a risk factor for near-fatal or fatal asthma episodes (24). Nevertheless, the 6-yr mortality rate is higher for smokers than nonsmokers following a near-fatal asthma attack, with an age-adjusted odds ratio (95% confidence interval [CI]) of 3.6 (2-6.2) (25). In the present study there was no difference in the proportion of near-fatal asthma attacks between the smokers and nonsmokers, suggesting that smoking is not the only risk factor for near-fatal asthma. A further long-term study in a large population is necessary to clarify this effect of smoking.
The combination of cigarette smoking and asthma accelerates the decline in lung function that occurs with either factor alone (26). In one study, the combination of asthma and smoking had a synergistic effect on the decline in lung function, resulting in a 17.8% decline in FEV1 over 10 yr (26). In our study, lung function, measured as the FEV1 predicted, FEF 25-75%, and FEV1/FVC, was lower in the smoking group than those in the nonsmoking group, indicating that smoking is an important factor for decreased lung function.
International guidelines on asthma management emphasize inhaled corticosteroids as the most effective anti-inflammatory therapy for chronic asthma (13). The evidence for this recommendation is based on clinical studies conducted largely in asthmatic patients who have never smoked or were former smokers. Smokers with asthma can be resistant to the beneficial therapeutic effects of corticosteroids (9). Several clinical factors might influence the response to corticosteroids in asthmatic smokers (27, 28). The asthmatic smokers in these studies had several clinical features that were distinct from subjects with chronic obstructive pulmonary disease (COPD) (27, 28). They were younger than subjects typically associated with symptomatic COPD (27, 28) and had a long history of asthma. In addition, the patients had evidence of bronchial hyperreactivity to methacholine (27) or reversibility following salbutamol of 15% (28). Among patients with atopic asthma, smokers were less responsive to inhaled adenosine than nonsmokers, which may indicate differences in airway inflammation (29). In the present study, the prevalence of emphysema and functional airway remodeling was higher in the smoking group than in the nonsmoking group, suggesting that emphysema and fixed airway obstruction can influence the response to anti-asthmatic drugs, including corticosteroids, in asthmatic smokers. The potential mechanisms of corticosteroid resistance in asthmatic smokers are largely unstudied but may include one or more of the pathways implicated in nonsmokers with asthma or other inflammatory diseases. Alternative treatments or treatments in addition to inhaled corticosteroids may be required for asthmatic patients who are unable to stop smoking or who have persistent symptoms following smoking cessation (30).
Cigarette smoking may change the airway inflammation associated with asthma. Cigarette smoking has been shown to induce airway inflammation in non-asthmatic smokers without airflow obstruction, compared with nonsmokers (31, 32). Normal smokers have shown increased T-lymphocytes, mainly CD8 cells (30) and macrophages, within the airway wall; higher neutrophil numbers within bronchial secretions; and infiltration of peripheral airways with mononuclear cells and macrophages (31). Sputum interleukin (IL)-8 levels were increased in asthmatic smokers; the concentrations were positively related to the neutrophil proportions in sputum and smoking history in pack-years and were negatively correlated with the FEV1 % predicted (30). In the present study, there were no differences in the numbers of sputum eosinophils and neutrophils between smoking and nonsmoking asthmatic patients. Cell and tissue sampling of lung using bronchoalveolar lavage, and lung biopsy in addition to noninvasive studies including exhaled nitric oxides for evaluation of the role of airway inflammatory cells is needed.
Smoking was found to alter the IgE response and increase the sensitization to allergens in an animal model (32). In the present study, although the prevalence of atopy was not different between the smoking and nonsmoking groups, the total IgE was higher in the smoking than the nonsmoking group, suggesting that smoking may influence IgE secretion from B cells. The underlying mechanism of this effect has not been clarified.
In conclusion, the 37.5% of asthmatic patients in this study who were ex or current smokers showed decreased pulmonary function and increased IgE levels, emphysema on HRCT, and fixed airway obstruction, indicating that smoking can modulate the clinical and therapeutic responses in asthma. Future studies of adult asthma should consider the effects of smoking on the clinical state and efficacy of therapy and investigate the related mechanisms.
Footnotes
This work was supported by a grant of Korea Healthcare technology R&D Project, Ministry for Health, Welfare and Family Affaris, Republic of Korea (01-PJ3-PG6-01GN04-003 and A040153).
References
- 1.Thomson NC, Spears M. The influence of smoking on the treatment response in patients with asthma. Curr Opin Allergy Clin Immunol. 2005;5:57–63. doi: 10.1097/00130832-200502000-00011. [DOI] [PubMed] [Google Scholar]
- 2.UK Gov. Office for National Statistics; 2004. [Accessed 20 August 2004]. Living in Britain: results from the 2002 General Household Survey. Available at http://www.statistics.gov.uk/lib. [Google Scholar]
- 3.Althuis M, Sexton M, Prybylski D. Cigarette smoking and asthma symptom severity among adult asthmatics. J Asthma. 1999;36:257–264. doi: 10.3109/02770909909075409. [DOI] [PubMed] [Google Scholar]
- 4.Silverman RA, Boudreaux ED, Woodruff PG, Clark S, Camargo CA., Jr Cigarette smoking among asthmatic adults presenting to 64 emergency departments. Chest. 2003;123:1472–1479. doi: 10.1378/chest.123.5.1472. [DOI] [PubMed] [Google Scholar]
- 5.Turner MO, Noertjojo K, Vedal S, Bai T, Crump S, Fitzgerald JM. Risk factors for near fatal asthma: a case-control study in hospitalized patients with asthma. Am J Respir Crit Care Med. 1998;157:1804–1809. doi: 10.1164/ajrccm.157.6.9708092. [DOI] [PubMed] [Google Scholar]
- 6.Lange P, Parner J, Vestbo J, Schnohr P, Jensen G. A 15 year follow-up study of ventilatory function in adults with asthma. N Engl J Med. 1998;339:1194–1200. doi: 10.1056/NEJM199810223391703. [DOI] [PubMed] [Google Scholar]
- 7.Marquette CH, Saulnier F, Leroy O, Wallaert B, Chopin C, Demarcq JM, Durocher A, Tonnel AB. Long-term prognosis of near-fatal asthma. A 6-year follow-up study of 145 asthmatic patients who underwent mechanical ventilation for a near-fatal attack of asthma. Am Rev Respir Dis. 1992;146:76–81. doi: 10.1164/ajrccm/146.1.76. [DOI] [PubMed] [Google Scholar]
- 8.Gallefoss F, Bakke PS. Does smoking affect the outcome of patient education and self management in asthmatics? Patient Educ Couns. 2003;49:91–97. doi: 10.1016/s0738-3991(02)00051-4. [DOI] [PubMed] [Google Scholar]
- 9.Chalmers GW, Macleod KJ, Little SA, Thomson LJ, McSharry CP, Thomson NC. Influence of cigarette smoking on inhaled corticosteroid treatment in mild asthma. Thorax. 2002;57:226–230. doi: 10.1136/thorax.57.3.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Thoracic Society. Standards for the diagnosis and treatment of patients with chronic obstructive pulmonary disease (COPD) and asthma. Am Rev Respir Dis. 1987;136:225–244. doi: 10.1164/ajrccm/136.1.225. [DOI] [PubMed] [Google Scholar]
- 11.Park SW, Park JS, Lee YM, Lee JH, Jang AS, Kim DJ, Hwangbo Y, Uh ST, Kim YH, Park CS. Differences in radiological/HRCT findings in eosinophilic bronchitis and asthma: implication for bronchial responsiveness. Thorax. 2006;61:41–47. doi: 10.1136/thx.2005.044420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jang AS, Lee JH, Park SW, Park JS, Kim DJ, Park CS. Risk factors related to fixed airway obstruction in patients with asthma after anti-asthma treatment. Ann Allergy Asthma Immunol. 2007;99:408–412. doi: 10.1016/S1081-1206(10)60564-9. [DOI] [PubMed] [Google Scholar]
- 13.National Asthma Education and Prevention Program. Expert panel report: guidelines for the diagnosis and management of asthma update on selected topics--2002. J Allergy Clin Immunol. 2002;110(5 Suppl):S141–S219. [PubMed] [Google Scholar]
- 14.American Thoracic Society. Lung function testing: selection of reference values and interpretative strategies. Am Rev Respir Dis. 1991;144:1202–1218. doi: 10.1164/ajrccm/144.5.1202. [DOI] [PubMed] [Google Scholar]
- 15.Juniper EF, Frith PA, Dunnett C, Cockcroft DW, Hargreave FE. Reproducibility and comparison of responses to inhaled histamine and methacholine. Thorax. 1978;33:705–710. doi: 10.1136/thx.33.6.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Norzila MZ, Fakes K, Henry RL, Simpson J, Gibson PG. Interleukin-8 secretion and neutrophil recruitment accompanies induced sputum eosinophil activation in children with acute asthma. Am J Respir Crit Care Med. 2000;161:769–774. doi: 10.1164/ajrccm.161.3.9809071. [DOI] [PubMed] [Google Scholar]
- 17.Pizzichini MM, Pizzichini E, Clelland L, Efthimiadis A, Mahony J, Dolovich J, Hargreave FE. Sputum in severe exacerbations of asthma: kinetics of inflammatory indices after prednisone treatment. Am J Respir Crit Care Med. 1997;155:1501–1508. doi: 10.1164/ajrccm.155.5.9154849. [DOI] [PubMed] [Google Scholar]
- 18.Park CS, Kim YY, Kang SY. Collection between RAST and skin test for inhalant offending allergens. J Korean Soc Allergol. 1983;3:1–9. [Google Scholar]
- 19.Higenbottam T, Feyeraband C, Clark T. Cigarette smoking in asthma. Br J Dis Chest. 1980;74:279–284. doi: 10.1016/0007-0971(80)90056-x. [DOI] [PubMed] [Google Scholar]
- 20.Jensen EJ, Dahl R, Steffensen F. Bronchial reactivity to cigarette smoke; relation to lung function, respiratory symptoms, serum-immunoglobulin E and blood eosinophil and leukocyte counts. Respir Med. 2000;94:119–127. doi: 10.1053/rmed.1999.0664. [DOI] [PubMed] [Google Scholar]
- 21.Cassino C, Ito K, Bader I, Ciotoli G, Thurston G, Reibman J. Cigarette smoking and ozone-associated emergency department use for asthma by adults in New York City. Am J Respir Crit Care Med. 1999;159:1773–1779. doi: 10.1164/ajrccm.159.6.9809042. [DOI] [PubMed] [Google Scholar]
- 22.Prescott E, Lange P, Vestbo J. Effect of gender on hospital admissions for asthma and prevalence of self-reported asthma: a prospective study based on a sample of the general population. Thorax. 1997;52:287–289. doi: 10.1136/thx.52.3.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rasmussen F, Taylor DR, Flannery EM, Cowan JO, Greene JM, Herbison GP, Sears MR. Risk factors for hospital admissions for asthma from children to young adulthood: a longitudinal population study. J Allergy Clin Immunol. 2002;110:220–227. doi: 10.1067/mai.2002.125295. [DOI] [PubMed] [Google Scholar]
- 24.Mitchell I, Tough SC, Semple LK, Green FH, Hessel PA. Near-fatal asthma: a population-based study of risk factors. Chest. 2002;121:1407–1413. doi: 10.1378/chest.121.5.1407. [DOI] [PubMed] [Google Scholar]
- 25.Marquette CH, Saulnier F, Leroy O, Wallaert B, Chopin C, Demarcq JM, Durocher A, Tonnel AB. Long-term prognosis of near-fatal asthma. A 6-year follow-up study of 145 asthmatic patients who underwent mechanical ventilation for a near-fatal attack of asthma. Am Rev Respir Dis. 1992;146:76–81. doi: 10.1164/ajrccm/146.1.76. [DOI] [PubMed] [Google Scholar]
- 26.Apostol G, Jacobs DR, Jr, Tsai AW, Crow RS, Williams OD, Townsend MC, Beckett WS. Early life factors contribute to the decrease in lung function between ages 18 and 40: the Coronary Artery Risk Development in Young Adults study. Am J Respir Crit Care Med. 2002;166:166–172. doi: 10.1164/rccm.2007035. [DOI] [PubMed] [Google Scholar]
- 27.Chalmers GW, Macleod KJ, Little SA, Thomson LJ, McSharry CP, Thomson NC. Influence of cigarette smoking on inhaled corticosteroid treatment in mild asthma. Thorax. 2002;57:226–230. doi: 10.1136/thorax.57.3.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chaudhuri R, Livingston E, McMahon AD, Thomson L, Borland W, Thomson NC. Cigarette smoking impairs the therapeutic response to oral corticosteroids in chronic asthma. Am J Respir Crit Care Med. 2003;168:1308–1311. doi: 10.1164/rccm.200304-503OC. [DOI] [PubMed] [Google Scholar]
- 29.Oosterhoff Y, Jansen MA, Postma D, Koeter GH. Airway responsiveness to adenosine 59-monophoshate in smokers and nonsmokers with atopic asthma. J Allergy Clin Immunol. 1993;92:773–776. doi: 10.1016/0091-6749(93)90023-9. [DOI] [PubMed] [Google Scholar]
- 30.Chalmers GW, MacLeod KJ, Thomson L, Little SA, McSharry C, Thomson NC. Smoking and airway inflammation in patients with mild asthma. Chest. 2001;120:1917–1922. doi: 10.1378/chest.120.6.1917. [DOI] [PubMed] [Google Scholar]
- 31.Saetta M, Turato G, Maestrelli P, Mapp CE, Fabbri LM. Cellular and structural bases of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;163:1304–1309. doi: 10.1164/ajrccm.163.6.2009116. [DOI] [PubMed] [Google Scholar]
- 32.Moerloose KB, Pauwels RA, Joos GF. Short-term cigarette smoke exposure enhances allergic airway inflammation in mice. Am J Respir Crit Care Med. 2005;172:168–172. doi: 10.1164/rccm.200409-1174OC. [DOI] [PubMed] [Google Scholar]