Abstract
Objectives
To document the numbers and types of interorganizational partnerships within the national patient safety domain, changes over time in these networks, and their potential for disseminating patient safety knowledge and practices.
Data Sources
Self-reported information gathered from representatives of national-level organizations active in promoting patient safety.
Study Design
Social network analysis was used to examine the structure and composition of partnership networks and changes between 2004 and 2006.
Data Collection
Two rounds of structured telephone interviews (n=35 organizations in 2004 and 55 in 2006).
Principal Findings
Patient safety partnerships expanded between 2004 and 2006. The average number of partnerships per interviewed organization increased 40 percent and activities per reported partnership increased over 50 percent. Partnerships increased in all activity domains, particularly dissemination and tools development. Fragmentation of the overall partnership network decreased and potential for information flow increased. Yet network centralization increased, suggesting vulnerability to partnership failure if key participants disengage.
Conclusions
Growth in partnerships signifies growing strength in the capacity to disseminate and implement patient safety advancements in the U.S. health care system. The centrality of AHRQ in these networks of partnerships bodes well for its leadership role in disseminating information, tools, and practices generated by patient safety research projects.
Keywords: Patient safety, partnership, collaboration, dissemination, network analysis
Background
Since the publication of the Institute of Medicine's landmark report, To Err Is Human: Building a Safer Health System (Institute of Medicine 2000), national and local efforts have been mobilized to transform the U.S. health care industry into a safe and reliable system. Progress in these efforts has been slowed by inherent challenges in coordinating change across such a complex and fragmented health care system (Berwick 2003; Scalise 2004; Wachter 2004), as well as difficulties of implementing the breadth of changes in culture and procedure necessary to improve patient safety within health care organizations (Longo et al. 2005; Weiner et al. 2006).
With a Congressional mandate to improve patient safety beginning in 2000, the federal Agency for Healthcare Research and Quality (AHRQ) took a multifaceted approach to its patient safety initiative, including funding hundreds of research studies, directing specific projects on priority national needs, and contracting with RAND in 2002 to serve as its Patient Safety Evaluation Center (evaluation center) to monitor and support the progress of its patient safety programs. Given the scope of AHRQ's patient safety mandate and its relatively limited resources, the agency has recognized the need to work with and leverage the efforts of other private and public organizations in order to stimulate change within the U.S. health care system. Similarly, the evaluation center has recognized that AHRQ's activities are situated within a wider context that must be understood in order to assess the agency's impact and the ways in which it can effectively engage the wider domain of policy actors focused on improving patient safety across the country (Farley et al. 2008).
Consequently, as part of its evaluation of AHRQ's patient safety initiative, the evaluation center examined the extent to which organizational partnerships to support patient safety improvement were being formed at the national level, including a focus on AHRQ's involvement in those partnerships.
Roles of Collaborative Networks
Health services have increasingly embraced interorganizational partnerships as a strategy for leveraging complementary strengths and promoting system-wide change within communities of variegated stakeholder groups (Foster-Fishman et al. 2001; Lasker, Weiss, and Miller 2001; Provan et al. 2003). These forms of collaboration can enable comprehensive thinking and action across participating partners (Lasker, Weiss, and Miller 2001) and provide structures for facilitating interorganizational exchanges (Foster-Fishman et al. 2001).
The composition of networks comprised of such interorganizational relationships within health and other policy domains, and the patterns of communication and exchange among network participants, affect who participates in policy events and their outcomes over time (Laumann, Knoke, and Kim 1985; Laumann and Knoke 1988; Moore et al. 2006). Likewise, these kinds of networks can constitute “communities of practice” in which common understandings of best practices and collective learning take place, as well as form the structural basis of conduits along which information, practices, and innovations flow (Sisk 1993; Valente 1995; Strang and Soule 1998; Bate and Robert 2002; Greenhalgh et al. 2004; Luke and Harris 2007), especially in networks spanning the public and private sectors (O'Toole 1997; Mintrom and Vergari 1998; Brinkerhoff 1999).
Evaluation Questions
This paper presents the methods and findings of the examination of partnership networks for patient safety undertaken within the larger evaluation of AHRQ's patient safety initiative. As such, this study addressed the infrastructure component of the system framework developed by the wider evaluation (Farley and Battles 2008, in this issue). Our goal was to understand the evolution of the networks comprising this collaborative infrastructure across the United States, AHRQ's position within these networks, and their potential for developing and disseminating patient safety knowledge and practices. The study specifically focused on four evaluation questions:
To what extent is there an infrastructure of interorganizational partnerships on a national level that are pursuing collaborative approaches to improving patient safety practices?
What is the composition of these networks in terms of types of organizations involved, the patterns of relationships among them, and activities in which they are engaged?
To what extent is AHRQ involved in the partnerships?
How has the structure and composition of these collaborative networks changed over time?
Methods
This evaluation used social network analysis, a set of methods expressly designed to examine and visualize relationships among social actors, including individuals and organizations (Wasserman and Faust 1994; Scott 2000), and thus well-suited to the research questions for this study. Network approaches, which have been increasingly applied in health services research and other sciences (Luke and Harris 2007; Borgatti and Foster 2003), can offer a uniquely comprehensive perspective on the structure of policy domains and insights not typically identified through conventional analytical techniques (Brandes et al. 1999; Brandes, Raab, and Wagner 2001).
In 2004 and again in 2006, the evaluation center conducted structured interviews with representatives of organizations prominent in the arena of national patient safety policy and initiatives. For each organization, we identified representatives considered most knowledgeable about the organization's patient safety activities and collaborative relationships with other entities.1 The interviews were approximately an hour in length and designed to document current and recent patient safety partnership activities, the types and extent of collaborative activities that they entailed, and the organization's experiences with these partnerships. Other interview topics included the organization's priorities and general activities with respect to patient safety, the organization's constituency and its perceived needs related to patient safety issues, as well as the organization's interest in future collaborations involving the dissemination of patient safety knowledge and practices.
Definition of Partnership
We defined a partnership based on the literature (cf. Foster-Fishman et al. 2001; Lasker, Weiss, and Miller 2001) as: “A formal relationship, either ongoing or limited in time, between individuals or groups that is characterized by mutual cooperation and responsibility for the achievement of a specified goal.”
This relatively narrow definition of partnership was not intended to capture all interactions between organizations on the topic of patient safety. In order to emphasize the mutual responsibility explicit in our definition, we specifically excluded relationships solely based on membership on another organization's board, grants or other contractual relationships, and such passive activities as attending a patient safety conference, receiving a patient safety newsletter, or using an existing patient safety curriculum.
Sampling Design
To characterize the structure of national patient safety partnership networks, we sought to generate an interview sample that encompassed what could be considered the “core” actors in this domain (Laumann, Marsden, and Prensky 1983; Laumann, Knoke, and Kim 1985). For the first round of interviews in 2004, we began with organizations identified through the various studies conducted by the evaluation center as major players in patient safety on the national scene (Farley et al. 2005). We then utilized “snowball” sampling by including organizations mentioned by more than two of our initial interview respondents as either partners or other key players in the realm of patient safety.2 This produced a sample frame of 38 nationally visible organizations active in patient safety that reflected a wide array of stakeholders.
For the second round of interviews in 2006, we started with the 35 organizations in the 2004 sample that completed interviews. We then reviewed the data from the 2004 interviews for organizations meeting our criteria3 that also participated in two or more “group partnerships,” which we defined as collaborative efforts reported by respondents involving more than two individual organizations (e.g., the Surgical Care Improvement Project [SCIP]).4 In addition, to ensure our sample did not overlook patient safety partnerships involving health information technology (health IT), a newly expanding area since our first round of interviews, we identified key health IT-related organizations drawing on data collected by the evaluation center of organizations that participated in national patient safety conferences and on polling of health IT experts within AHRQ. These two procedures generated 24 additional organizations, resulting in a total sample for the 2006 interviews of 59 organizations. The snowball sampling procedures did not yield any additional organizations for the sample in the second round of interviews.
Analysis of Partnership Patterns
We compared the partnership networks in 2004 and 2006 utilizing both descriptive statistics and social network analysis. In particular, network measures and visual graphs derived with generally available network analytic software (Borgatti 2002; Borgatti, Everett, and Freeman 2002)5 were used to systematically examine the structure and patterns of interorganizational partnerships related to patient safety as reported in the interviews,6 as well as their evolution over the 2-year period.
We relied on two common network measures to characterize the centrality of individual organizations within the partnership networks—degree centrality and betweeness centrality. Degree centrality is simply the sheer number of ties that an organization has with other organizations in the network. Betweeness centrality assesses the extent to which an organization serves as a link or bridge across different parts of the network that would otherwise not be connected.
We used three other network measures to characterize the structure of the networks as a whole—density, transitivity, and network centralization. Density measures the general degree of interconnectedness of a network based on the ratio of observed links among nodes to the total number that could possibly exist. Higher density is an indicator of cohesion and interaction within a network, which is often associated with greater awareness of others and faster rates of diffusion within a community.
Transitivity is a more specialized measure of how well information flows within a network, based on the proportion of times a connection from one node to two others is accompanied (or “closed”) by a connection between the other two nodes (akin to a “friend of a friend” scenario). Higher transitivity in a network indicates a higher degree of cross-linking paths across which information can flow.
Network centralization is a measure of the extent to which a network is dominated by one or a few very central hubs (i.e., nodes with high degree and betweeness centrality). In a highly centralized network, these central hubs represent single points of failure, which, if removed or damaged, quickly fragment the network into unconnected subnetworks. A less centralized network has fewer points of failure and exhibits greater resilience. At the same time, network centralization, like density, is associated with faster diffusion of innovations. Thus, although a centralized network is more efficient, it may be more prone to failure and less empowering to average members (Valente 1995; Valente, Chou, and Pentz 2007).
Results
In 2004, we interviewed representatives from 35 of the 38 organizations invited to participate in the study, yielding a response rate of 92 percent.7 In 2006, we interviewed 55 of the 59 organizations invited to participate for a response rate of 93 percent. Patient safety was reported as a primary or major focus for the vast majority of our respondents (78 percent in 2004 and 76 percent in 2006). All the interviewees indicated that their constituents had an interest in patient safety, although the extent varied from broad interest to specific interest in particular issues. Those who defined patient safety more broadly often included quality of care in their definition, identifying patient safety as one component of health care quality.
The interviews in 2004 yielded 135 partnerships while those done in 2006 yielded 244 partnerships. In each year, over 90 percent of partnerships were in existence at the time of the interviews. Because information obtained on ceased partnerships was not uniform between the two rounds of interviews, the analyses include only partnerships that existed at the time of the interviews each year (117 in 2004 and 220 in 2006).
Characteristics of Partnering Organizations
As shown in Table 1, the ongoing partnerships identified in the two rounds of interviews involved a total of 92 and 147 organizations in 2004 and 2006, respectively (i.e., including the organizations of the respondents interviewed plus the additional partners they mentioned). The most common types of organizations involved in these patient safety partnerships in both years were health industry and professional associations (15 in 2004 and 33 in 2006), followed by government departments and agencies (12 and 18, respectively). Other types of organizations less frequently involved in these partnerships included accrediting and standards-setting bodies, foundations, health policy and improvement organizations, health IT policy and development organizations, health care consumer or purchaser groups, consulting firms, and academic or research institutions. In both years, there were also a large number of “group partnerships,” which represent bundles of relationships through which multiple organizations are connected, even if each organization is not denoted separately in our analysis.
Table 1.
All Organizations Engaged in Patient Safety Partnerships,* 2004 and 2006
| Number of Organizations | |||
|---|---|---|---|
| Type of Organization | 2004 | 2006 | Change from 2004 |
| Accrediting or standards-setting entity | 4 | 5 | +1 |
| Foundation | 3 | 3 | 0 |
| Government department or agency | 12 | 18 | +6 |
| Health industry or professional association | 15 | 33 | +18 |
| Health policy/improvement organization | 4 | 12 | +8 |
| HIT policy/development organization | 2 | 7 | +5 |
| Health care consumer or purchaser group | 4 | 9 | +5 |
| Consulting firm | 0 | 1 | +1 |
| Academic or research institution | 5 | 10 | +5 |
| Group partnership | 43 | 49 | +6 |
| Total | 92 | 147 | +55 |
Includes both interviewed organizations and their reported partner organizations.
HIT, health information technology.
Characteristics of Partnerships
The majority of current partnerships reported in both rounds of interviews had been in existence for >1 year (61 percent in 2004 and 79 percent in 2006), indicating some sustainability of these partnerships over time. Fewer respondents reported that the partnerships were too new to determine success in 2006 (13 percent) compared with 2004 (40 percent). However, similar to the results from 2004, when respondents did feel able to judge the success of a partnership, over 80 percent were deemed successful, with only two described as not successful.8 Also similar to results from 2004, over half of the partnerships in 2006 were supported solely through in-kind time and effort by staff from participating agencies. Approximately a third received dedicated funding from either of the partner organizations, and 12 percent received dedicated funding from external sources (the later an increase from 6 percent in 2004).
Table 2 provides data on the average number of partnerships and partnership activities for the sample of interviewed organizations, as well as the percentage of partnerships involving specific types of activities.9 To ensure comparable figures between 2004 and 2006, the table includes comparisons based on a consistent sample limited to the 35 organizations that were interviewed in both years. These comparisons indicate an overall expansion in partnership activity around patient safety issues, with a 40 percent increase in the mean number of partnerships per interviewed organization (from 4.29 in 2004 to 6.00 in 2006), and an over 50 percent increase in the mean number of activities per reported partnership (from 1.55 in 2004 to 2.34 in 2006).
Table 2.
Numbers and Types of Patient Safety Partnerships, 2004 and 2006
| Consistent Sample* | ||||
|---|---|---|---|---|
| 2006 | 2004 | 2006 | Change from 2004 | |
| Mean number of | ||||
| Partnerships per interviewed organization | 5.25 | 4.29 | 6.00 | +1.7 |
| Activities per reported partnership | 2.39 | 1.55 | 2.34 | +0.8 |
| Type of activity† (as percent of partnerships) | (n=220) | (n=117) | (n=161) | |
| Research-related (percentage) | 16.4 | 16.2 | 18.6 | +2.4 |
| Dissemination (percentage) | 50.5 | 27.4 | 51.6 | +24.2 |
| Intellectual exchange (percentage) | 40.5 | 25.6 | 39.8 | +14.2 |
| Standards and guidelines development (percentage) | 33.2 | 31.6 | 29.8 | −1.8 |
| Tools development (percentage) | 32.3 | 14.5 | 35.4 | +20.9 |
| Education and training (percentage) | 24.1 | 17.9 | 26.7 | +8.8 |
| Policy change and advocacy (percentage) | 20.9 | 10.3 | 18.6 | +8.3 |
Based on the 35 organizations interviewed in both 2004 and 2006.
Categories are not mutually exclusive.
n represents the total number of partnerships ongoing as of the time of the interviews.
This expansion is also reflected in a relative increase in virtually all domains of partnership activity, which also is shown in Table 2. The most notable growth has occurred in dissemination (including organizing conferences, providing information to constituency groups, etc.) and development of patient safety tools (e.g., medication error and decision support checklists, electronic physician order systems, data repositories of adverse events and other patient safety indicators, etc.), with increases of 24 and 21 percentage points, respectively. Intellectual exchange (representing discussions and regular exchange of information between organizations that may or may not result in products) also experienced a substantial increase. These trends suggest that the dissemination and translation of patient safety knowledge and usable tools have become a greater focus of collaborative activities.
The Partnership Networks Identified
Most of the organizations were linked in an overall infrastructure around patient safety, as evidenced by the first three network statistics presented in Table 3 (see also graphs of the full partnership networks in Appendix Figure S1). In both 2004 and 2006, only a small number of organizations that we interviewed did not report any patient safety partnerships that met our definition (which show up as “isolates” in the network analysis), although they were all involved in various other patient safety activities. In 2004, the 92 organizations with partnerships were distributed across five separate, disconnected clusters. In the comparable sample for 2006, the 110 organizations with partnerships were connected into one large component.
Table 3.
Characteristics of the National Patient Safety Partnership Network: Comparative Statistics 2004 and 2006
| Consistent Sample* | |||
|---|---|---|---|
| Network Statistic | 2006 | 2004 | 2006 |
| Total number of organizations reported in the network† | 147 | 92 | 110 |
| Number of isolates | 5 | 4 | 3 |
| Number of components | 1 | 5 | 1 |
| Density‡ | 0.053 | 0.067 | 0.092 |
| Transitivity (percentage)‡ | 17.39 | 11.36 | 24.44 |
| Network centralization (percentage)‡ | 30.99 | 20.94 | 24.51 |
Based on the 35 organizations interviewed in both 2004 and 2006.
Includes both interviewed organizations and their reported partner organizations.
Calculated only on partnerships among interviewed organizations.
In both years, AHRQ was the most central and interconnected organization in the full set of partnerships identified both in terms of “degree” and “betweeness” centrality. In addition, AHRQ substantially expanded the number of its direct partners between the two rounds of interviews from 21 to 38, including relationships to other individual organizations as well as group partnerships.
Other analyses (not shown) indicate that government agencies in general and accrediting and standard-setting bodies as a group tend to be the most central types of organizations in the overall network on both measures of centrality.10 Government agencies in both years also tend to be generally interconnected, having most of their partnerships with one another.11 Similarly, consumer and purchaser groups tended to have most of their partnerships with other organizations of the same type. The health IT organizations in 2006 had an equal emphasis on health industry or professional associations and other health IT-related organizations. In contrast, accrediting and standards organizations, health industry and professional associations, and academic and research institutions tended to have most of their patient safety partnerships with organizations outside of their categories, typically with government agencies (see Appendix Table S1).
The remaining three network analytic measures in Table 3 suggest that the rate at which information could diffuse through the patient safety partnerships increased between 2004 and 2006. For the overall patient safety partnership network, density increased over 37 percent (from 0.067 to 0.092), transitivity increased 115 percent (from 11.4 to 24.4 percent), and network centralization increased 17 percent (from 20.9 to 24.5 percent).12 As noted previously, however, higher centralization is also associated with greater vulnerability of networks to failure and lower levels of empowerment among average participants.
Partnership Networks by Type of Activity
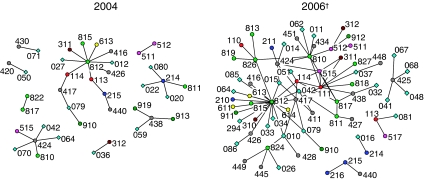
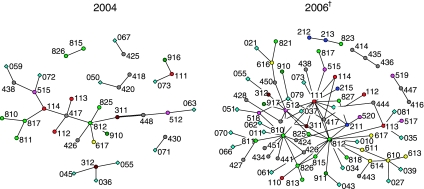
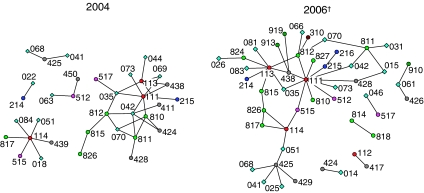
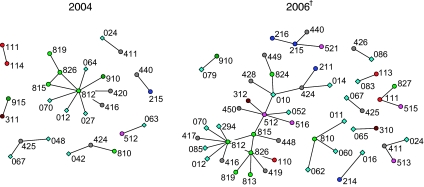
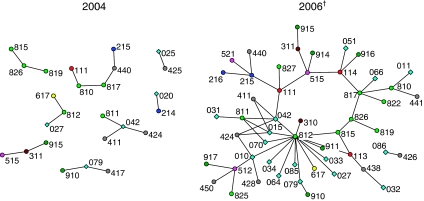
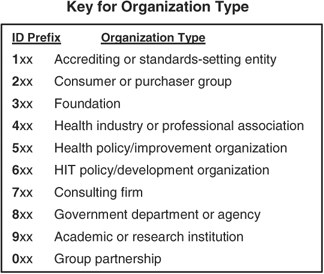
Figures 1–5 display graphs based on the consistent sample of organizations in both years (n=35) for the networks related to the five largest domains of partnership activity listed in Table 2: disseminating patient safety information, developing patient safety standards or guidelines, providing education or training, developing tools to improve patient safety, and exchanging intellectual expertise and patient safety know-how. Each line in the graphs represents a partnership relationship between two entities. Circles represent individual organizations, and diamonds are the “group partnerships.” Organization type is indicated by the first digit of the ID code for each node, as given in the ID prefix key. In these figures, AHRQ is organization 812.
Figure 1.
Dissemination Partnerships, 2004 and 2006
†Consistent sample based on the 35 organizations interviewed in both 2004 and 2006.
Figure 5.
Intellectual Exchange Partnerships, 2004 and 2006
†Consistent sample based on the 35 organizations interviewed in both 2004 and 2006.
These graphs omit organizations that did not participate in partnerships for a specific patient safety activity (the isolates described above), which would be represented by unconnected circles. Graphs for the two smallest domains of collaborative activity—research-related and policy change and advocacy partnerships—are provided in Appendix S1.
Dissemination Partnerships
In 2004, the largest cluster of dissemination partnerships draws together over a third of the organizations involved in this collaborative activity in the form of a centralized “star” or “wheel” (i.e., hub and spoke pattern) (Figure 1). The overall shape of a graph affects the flow of interaction and the ability of the network as a whole to perform certain tasks or functions (Bavelas 1950; Guetzkow and Simon, 1955; Burt 1980). Star-shaped structures tend to perform simple tasks more quickly and accurately, but they do less well with more complex tasks. This type of structure also places a relatively heavy burden on the central partner, which in this network is AHRQ, to coordinate information flows, requiring a high degree of internal cross-sharing of information and coordination of partnering activities. There also were a number of clusters of other organizations in the 2004 graph to which the main star-shaped cluster was not connected.
The graph for 2006 exhibits both an increase in the number of partnerships involved in dissemination, and additional links connecting various hubs into one large, interconnected component. Consequently, although the main cluster from the 2004 network roughly maintained its star-shaped form, the overall network became substantially less fragmented over the 2-year period and more conducive to broad-scale sharing of information and resources related to dissemination of safe practices. AHRQ maintained a central role in the 2006 network.
Standards and Guidelines Development Partnerships
Accreditation and standard-setting organizations are the most central to partnerships around this activity (i.e., ID nos 111, 113, and 114) (Figure 2). Two positive changes occurred in these partnerships between 2004 and 2006—the sharp increase in the number of partnerships and the linking in 2006 of the two main clusters of collaborative standards and guidelines activity observed in 2004. As a consequence, the 2006 network reflects a stronger bridge between efforts focused on medication safety guidelines and clinical performance standards.
Figure 2.
Standards and Guidelines Development Partnerships, 2004 and 2006
†Consistent sample based on the 35 organizations interviewed in both 2004 and 2006.
Education and Training Partnerships
A salient feature of the network graph for this activity is the “triangle” of collaboration among AHRQ and two other central government agencies (ID nos 815 and 826) in both years (Figure 3). In 2006, this cluster was substantially extended, largely through bridges created by the collaborative activities of a particular health policy and improvement organization (ID no. 512) and a new group partnership (ID no. 010). However, there remain a number of disconnected clusters of collaborative activity that could be used to build on what has already been established in this area.
Figure 3.
Education and Training Partnerships, 2004 and 2006
†Consistent sample based on the 35 organizations interviewed in both 2004 and 2006.
Tools Development Partnerships
Tools development was a relatively sparse domain of activity in 2004, but it progressed into one of the most extensive areas of collaboration by 2006, as evidenced by a five-fold increase in numbers of partnerships (Figure 4). In 2006, 11 percent of the partnerships in this area specifically focused on development of new technologies (such as computerized physician order and entry systems, electronic health records, electronic decision support systems), and 34 percent specifically focused on development of data repositories. Similar to the changes in other areas, the growth in this area has been accompanied by a substantial decrease in fragmentation. AHRQ's involvement in these partnerships increased substantially from 2004 to 2006, making it one of the central organizations in the 2006 network.
Figure 4.
Tools Development Partnerships, 2004 and 2006
†Consistent sample based on the 35 organizations interviewed in both 2004 and 2006.
The most noticeable feature of the 2006 graph is the “ring” structure around which the central organizations are connected. “Ring” structures, like long “chain” network structures, tend toward information flows that are slow and susceptible to distortion. Cross-links across this ring would improve collective awareness and knowledge of tools development activities in other parts to the network. However, this is probably less an issue in this context given the extent of group partnerships in which tools development activities are occurring and the multiplicity of partnerships in other activity domains that the organizations around this ring already share.13
Intellectual Exchange Partnerships
Intellectual exchange activities often represent the first step in building more focused and committed partnerships. These activities expanded substantially from 2004 to 2006 (Figure 5). In 2004, we found a predominantly “chain”-like structure within the network of intellectual exchange partnerships, which is particularly problematic for this type of activity for the reasons noted above. Since then, this structure has morphed into a highly interconnected web of relations with much greater potential for rapid and widespread flows of knowledge and expertise. AHRQ sits in a central location in this web, along with other government (e.g., ID no. 810), accrediting and standards-setting (ID no. 111), health professional (ID no. 417), and health policy and improvement (ID no. 512) organizations—which suggests a diversity of interests shaping the collective dialogue for sharing knowledge and strategies to improve patient safety.
Discussion
This evaluation analysis shows that interorganizational partnerships for patient safety activities have been forged by key organizations across the United States and that the size of these networks and interactions among participating organizations increased substantially from 2004 to 2006. There was also an increase in virtually all domains of partnership activity, with the greatest growth in activities such as dissemination and tools development that reflect a stronger emphasis on the translation of patient safety knowledge into practice. Intellectual exchange partnerships also experienced notable growth, suggesting the importance of this activity in building and sustaining various types of collaborative efforts over time.
The importance of AHRQ's role in many of the types of partnerships is shown in its central positions in the various partnership network graphs, reflecting AHRQ's leadership involvement in partnership strategies and activities. In particular, the growth in its direct linkages with other organizations between 2004 and 2006 suggests that AHRQ has expanded and consolidated relationships through which organizations can collaborate to provide needed infrastructure for the adoption and diffusion of patient safety practices in the health care community.
Statistics characterizing the overall network of partnerships showed that, from 2004 to 2006, fragmentation of the partnership networks decreased (as indicated by the number of disconnected components) and potential for information flow increased (as assessed by measures of density and transitivity). At the same time, measures of network centralization increased, with greater dominance by central hubs in the network, in which AHRQ tended to be centrally placed. AHRQ's central location in the network highlights its critical role, but it also suggests that timely dissemination of information and practices may be highly dependent on its actions. In general, the centralization measures and graphs of specific partnership activities suggest that attention be paid to further improving the structure and resiliency of these collaborative networks.
One limitation of our data is that an unknown number of partnerships were not captured in the sample frame or interview protocol. This stems from a range of factors, including respondents not being familiar with all activities occurring within their organizations, time constraints of a 1-hour interview leading to only partial identification of an organization's activities, or respondents restricting the description of a partnership to that portion of activities in which their organization was involved. We also do not have data on all the partnerships for the many organizations that respondents identified as a partner but were not interviewed. However, because >80 percent of such organizations (in both rounds) were only identified by one responding organization, we are confident that the data provide a reasonable representation of the main national-level infrastructure of patient safety partnerships.
Conclusion
Partnerships among organizations represent a means for widespread diffusion of information, technologies, and practices and the collective improvement of patient safety. The growth in reported partnerships of all types is an encouraging sign that the capacity to spread and implement advancements in patient safety within the U.S. health care system has become stronger over the past few years. The centrality of AHRQ in these networks of partnerships bodes well for its ability to facilitate the packaging and dissemination of information, tools, and practices generated by the projects funded through its patient safety initiative. The research also identifies opportunities to enhance the configuration and performance of this infrastructure for collaborative improvement.
As shown in this application to patient safety networks, social network analysis offers one set of tools that can be useful for systematically documenting the structure of relationships among organizations working collaboratively to promote health care quality and safety improvement, and also for informing policies and strategies to guide the development of these partnerships. In particular, network analysis results can help AHRQ and other involved organizations to better “manage” and cultivate partnership networks through such actions as bringing in new actors, reconfiguring their positions, encouraging particular types of connections, and reframing goals and tasks of collaborative efforts (Klijn 1996; Provan et al. 2004)—strategies which can be used not only to develop their own partnership networks but also to build the capacity of the overall collaborative infrastructure for improvement.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The research described in this manuscript was undertaken as one part of a larger evaluation project funded by AHRQ under contract no. 290-02-0010. Pursuant to that contract, AHRQ had the right to review and comment on this manuscript before its publication.
This manuscript was developed with data collected and/or analyzed under contract with AHRQ. The information and opinions expressed herein reflect solely the position of the authors. Nothing herein should be construed to indicate AHRQ support or endorsement of its contents.
We would like to thank Lily Bradley, Allison DeCristofaro, Jake Dembosky, Rachel Kaganoff Stern, and Rebecca Shaw for their assistance in conducting the data collection interviews for this study, as well as express our gratitude to Donna Keyser at RAND and the two anonymous HESR reviewers for their helpful comments on this manuscript.
Disclosures: None.
Notes
These representatives typically included the executive director or director of patient safety, quality, and related initiatives. For a few organizations with large portfolios of partnerships or differentiated units engaged in separate collaborative activities, we conducted interviews with multiple representatives at different times.
In order not to condition the sample based on the links possessed by organizations (Laumann, Marsden, and Prensky 1983), we asked respondents to tell us the organizations that they considered active and influential in the area of patient safety and whether they partnered with those organizations. We then only included in the sample domestic organizations whose patient safety activities spanned more than one state.
That is, domestic organizations nationally active in patient safety (see also footnote 2).
The information on participants in the “group partnerships” was only compiled after the 2004 interviews were completed.
Ucinet 6 for Windows (Borgatti, Everett, and Freeman 2002) was used to transform the data for network analysis and provide statistics on network characteristics. The network data were graphed visually in NetDraw 1.0 (Borgatti 2002), with the layout of nodes and lines derived using a “spring embedding” algorithm.
Our analysis assumes that a partnership existed between two organizations if one was reported by a respondent in either organization. We adopt this procedure because the most likely reason for partnerships not being reported reciprocally is the incomplete familiarity of even knowledgeable respondents of all activities in which their organization is engaged, and the fact that the type of interorganization relationships under study are by definition nondirectional (i.e., if one organization is involved in a partnership, so is its partner). Although analyses of relationships in which social desirability is likely to be high (e.g., personal friendship networks) typically are limited to “confirmed” ties in which both parties report the relationship (Marsden 1990), this bias is relatively small in these data given the nature of these collaborative relationships and the extensive set of additional questions respondents were asked about each partnership.
Only one organization mentioned by more than two respondents in 2004 was not able to be included in the final sample due to time constraints. Another organization was dropped from the sample frame after completion of the interview because it did not meet our criteria of being involved in patient safety activities, whether collaborative or otherwise.
The determination of whether a partnership was successful was left to the respondent's own criteria, as we were interested in general perceptions of success and could not accommodate the many possible dimensions of effective collaboration (Lasker, Weiss, and Miller 2001) within the constraints of our interview protocol.
The seven types of activities listed in Table 2 were derived based on patient safety activities of various organizations identified in the series of studies conducted during the evaluation center's first year (Farley et al. 2005). Although respondents were asked open-ended questions on this topic, all responses were able to be fitted into the initial typology.
The average degree centrality score for both of these groups in 2006 was 5.8 and 7.4, respectively (compared with a mean of 2.8 across all organizations, p<.01), and the average betweeness centrality score was 72.0 and 45.7, respectively (compared with a mean of 15.2 across all organizations, p<.01), with substantively similar results in 2004.
Only including direct partnerships with other organizations, and not connections to any of the “group partnerships.” See Appendix Table S1 for cross-tabulations of partnership linkages across organization types for the full 2006 sample.
Because these three indicators are “sociometric” measures of the overall structure of a network (Scott 2000) and sensitive to incomplete linkage data on nodes, the calculations presented here are based only on partnerships among interviewed organizations (i.e., excluding ties with reported partner organizations that we did not interview). Results using the full sample of reported partnerships yielded substantively similar results.
A condition known in network analysis as “multiplexity,” i.e., having multiple types of relationships with others.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Appendix S1: Supplemental Results
Figure S1. Overall Patient Safety Partnership Network, 2004 and 2006.
Figure S2. Research-Related Partnerships, 2004 and 2006.
Figure S3. Policy Change & Advocacy Partnerships, 2004 and 2006.
Table S1. Cross-Tabulation of Partnerships by Organization Type, 2006 (full sample).
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Bate SP, Robert G. Knowledge Management and Communities of Practice in the Private Sector: Lessons for Modernizing the National Health Service in England and Wales. Public Administration. 2002;80(4):643–63. [Google Scholar]
- Bavelas A. Communication Patterns in Task-Oriented Groups. Journal of the Acoustical Society of America. 1950;22:725–30. [Google Scholar]
- Berwick DM. Disseminating Innovations in Health Care. Journal of the American Medical Association. 2003;289:1969–75. doi: 10.1001/jama.289.15.1969. [DOI] [PubMed] [Google Scholar]
- Borgatti SP. NetDraw: Network Visualization Software (Version 1.0.0.21) Harvard, PA: Analytic Technologies; 2002. [Google Scholar]
- Borgatti SP, Everett MG, Freeman LC. Ucinet 6 for Windows: Software for Social Network Analysis (Version 6.29) Harvard, PA: Analytic Technologies; 2002. [Google Scholar]
- Borgatti SP, Foster PC. The Network Paradigm in Organizational Research: A Review and Typology. Journal of Management. 2003;29(6):991–1013. [Google Scholar]
- Brandes U, Kenis P, Raab J, Schneider V, Wagner D. Explorations in to the Visualization of Policy Networks. Journal of Theoretical Politics. 1999;11(1):75–106. [Google Scholar]
- Brandes U, Raab J, Wagner D. Exploratory Network Visualization: Simultaneous Display of Actor Status and Connections. Journal of Social Structure. 2001;2(4):1–28. [Google Scholar]
- Brinkerhoff DW. State-Civil Society Networks for Policy Implementation in Developing Countries. Policy Studies Review. 1999;16(1):123–47. [Google Scholar]
- Burt RS. Models of Network Structure. Annual Review of Sociology. 1980;6:79–141. [Google Scholar]
- Farley DO, Battles JB. Evaluation of the AHRQ Patient Safety Initiative: Framework and Approach. Health Services Research. 2008 doi: 10.1111/j.1475-6773.2008.00931.x. DOI 10.1111/j.1475-6773.2008.00931.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farley DO, Damberg CL, Ridgely MS, Sorbero MES, Greenberg MD, Haviland AM, Teleki SS, Mendel P, Bradley LA, Dembosky JW, Fremont A, Nuckols TK, Shaw RN, Straus S, Taylor SL, Yu H, Tharp-Taylor S. Assessment of the National Patient Safety Initiative: Focus on Implementation and Dissemination: Final Report, Evaluation Report IV. 2008. RAND Technical Report TR-563-AHRQ. Santa Monica, CA: RAND Corporation.
- Farley DO, Morton SC, Damberg CL, Fremont A, Berry SH, Greenberg MD, Sorbero MES, Teleki SS, Ricci KA, Pollock N. Assessment of the National Patient Safety Initiative: Context and Baseline Evaluation Report I. 2005. RAND Technical Report TR-203-AHRQ. Santa Monica, CA: RAND Corporation.
- Foster-Fishman PG, Berkowitz SL, Lounsbury DW, Jacobson S, Allen NA. Building Collaborative Capacity in Community Coalitions: A Review and Integrative Framework. American Journal of Community Psychology. 2001;29(2):241–61. doi: 10.1023/A:1010378613583. [DOI] [PubMed] [Google Scholar]
- Foster-Fishman PG, Salem DA, Allen NA, Fahrback K. Facilitating Interorganizational Collaboration: The Contributions of Interorganizational Alliances. American Journal of Community Psychology. 2001;29(6):875–905. doi: 10.1023/A:1012915631956. [DOI] [PubMed] [Google Scholar]
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of Innovations in Service Organizations: Systematic Review and Recommendations. Milbank Quarterly. 2004;82(4):581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guetzkow H, Simon HA. The Impact of Certain Communication Nets upon Organization and Performance in Task-Oriented Groups. Management Science. 1955;1:233–50. [Google Scholar]
- Kohn LT, Corrigan JM, Donaldson MS, editors. Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- Klijn EH. Analyzing and Managing Policy Processes in Complex Networks: A Theoretical Examination of the Concept Policy Network and Its Problems. Administration and Society. 1996;28(1):90–119. [Google Scholar]
- Lasker RD, Weiss ES, Miller R. Partnership Synergy: A Practical Framework for Studying and Strengthening the Collaborative Advantage. Milbank Quarterly. 2001;79(2):179–205. doi: 10.1111/1468-0009.00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laumann EO, Knoke D. The Increasingly Organizational State. Society. 1988;25(2):21–8. [Google Scholar]
- Laumann EO, Knoke D, Kim YH. An Organizational Approach to State Policy Formation: A Comparative Study of Energy and Health Domains. American Sociological Review. 1985;50(1):1–19. [Google Scholar]
- Laumann EO, Marsden PV, Prensky D. The Boundary Specification Problem in Network Analysis. In: Burt RS, Minor MJ, editors. Applied Network Analysis: Structural Methodology for Empirical Social Research. Beverly Hills, CA: Sage; 1983. pp. 18–34. [Google Scholar]
- Longo DR, Hewett JE, Ge B, Schubert S. The Long Road to Patient Safety: A Status Report on Patient Safety Systems. Journal of American Medical Association. 2005;294(22):2858–65. doi: 10.1001/jama.294.22.2858. [DOI] [PubMed] [Google Scholar]
- Luke DA, Harris JK. Network Analysis in Public Health: History, Methods, and Applications. Annual Review of Public Health. 2007;28:16.1–25. doi: 10.1146/annurev.publhealth.28.021406.144132. [DOI] [PubMed] [Google Scholar]
- Marsden PV. Network Data and Measurement. In: Scott WR, editor. Annual Review of Sociology. Vol. 16. Palo Alto, CA: Annual Reviews; 1990. pp. 435–63. [Google Scholar]
- Mintrom M, Vergari S. Policy Network and Innovation Diffusion: The Case of State Education Reforms. The Journal of Politics. 1998;60(1):126–48. [Google Scholar]
- Moore, Smith SC, Simpson T, Minke SW. The Influence of Partnership Centrality on Organizational Perceptions of Support: A Case Study of the AHLN Structure. BMC Health Services Research. 2006;6:141. doi: 10.1186/1472-6963-6-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Toole LJ. Implementing Public Innovations in Network Settings. Administration and Society. 1997;29(2):115–38. [Google Scholar]
- Provan KG, Nakama L, Veazie MA, Teufel-Shone NI, Huddleston C. Building Community Capacity Around Chronic Disease Services through a Collaborative Interorganizational Network. Health Education and Behavior. 2003;30(6):646–62. doi: 10.1177/1090198103255366. [DOI] [PubMed] [Google Scholar]
- Provan KG, Veazie MA, Teufel-Shone NE, Huddleston C. Network Analysis as a Tool for Assessing and Building Community Capacity for Provision of Chronic Disease Services. Health Promotion Practice. 2004;5(2):174–81. doi: 10.1177/1524839903259303. [DOI] [PubMed] [Google Scholar]
- Scalise D. 5 Years after IOM … The Evolving State of Patient Safety. Hospital and Health Networks. 2004;78(10):59–62. [PubMed] [Google Scholar]
- Scott J. Social Network Analysis. A Handbook. 2d edition. London: Sage; 2000. [Google Scholar]
- Sisk JE. Improving the Use of Research-Based Evidence in Policy-Making: Effective Care in Pregnancy and Childbirth in the United States. Milbank Quarterly. 1993;71(3):477–96. [PubMed] [Google Scholar]
- Strang D, Soule SA. Diffusion in Organisations and Social Movements: From Hybrid Corn to Poison Pills. Annual Review of Sociology. 1998;24:265–90. [Google Scholar]
- Valente TW. Network Models of the Diffusion of Innovations. Cresskill, NJ: Hampton; 1995. [Google Scholar]
- Valente TW, Chou CP, Pentz MA. Community Coalitions as a System: Effects of Network Change on Adoption of Evidence-Based Substance Abuse Prevention. American Journal of Public Health. 2007;97(5):880–6. doi: 10.2105/AJPH.2005.063644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wachter RM. The End of the Beginning: Patient Safety Five Years after ‘To Err Is Human.’. Health Affairs. 2004;30:W4-534–44. doi: 10.1377/hlthaff.w4.534. web exclusive. [DOI] [PubMed] [Google Scholar]
- Wasserman S, Faust K. Social Network Analysis. Methods and Applications. Cambridge: Cambridge University Press; 1994. [Google Scholar]
- Weiner BJ, Alexander JA, Baker LC, Shortell SM, Becker M. Quality Improvement Implementation and Hospital Performance on Patient Safety Indicators. Medical Care Research and Review. 2006;63(1):29–57. doi: 10.1177/1077558705283122. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.