Abstract
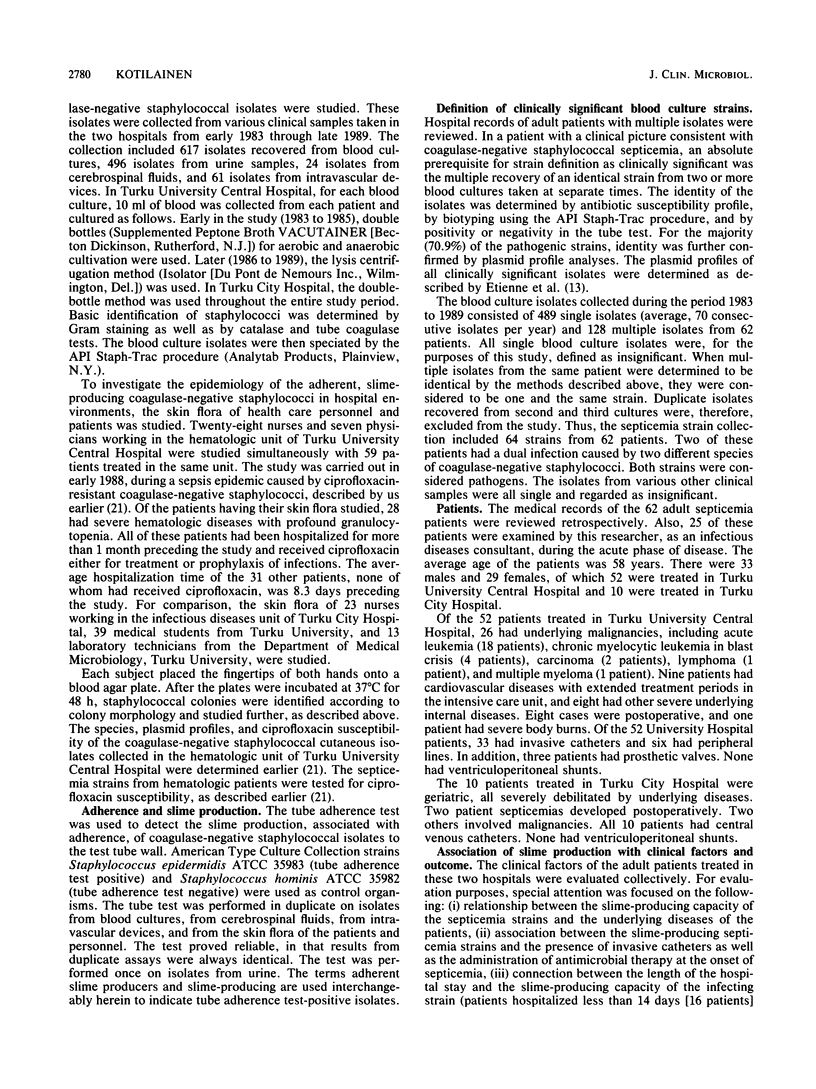
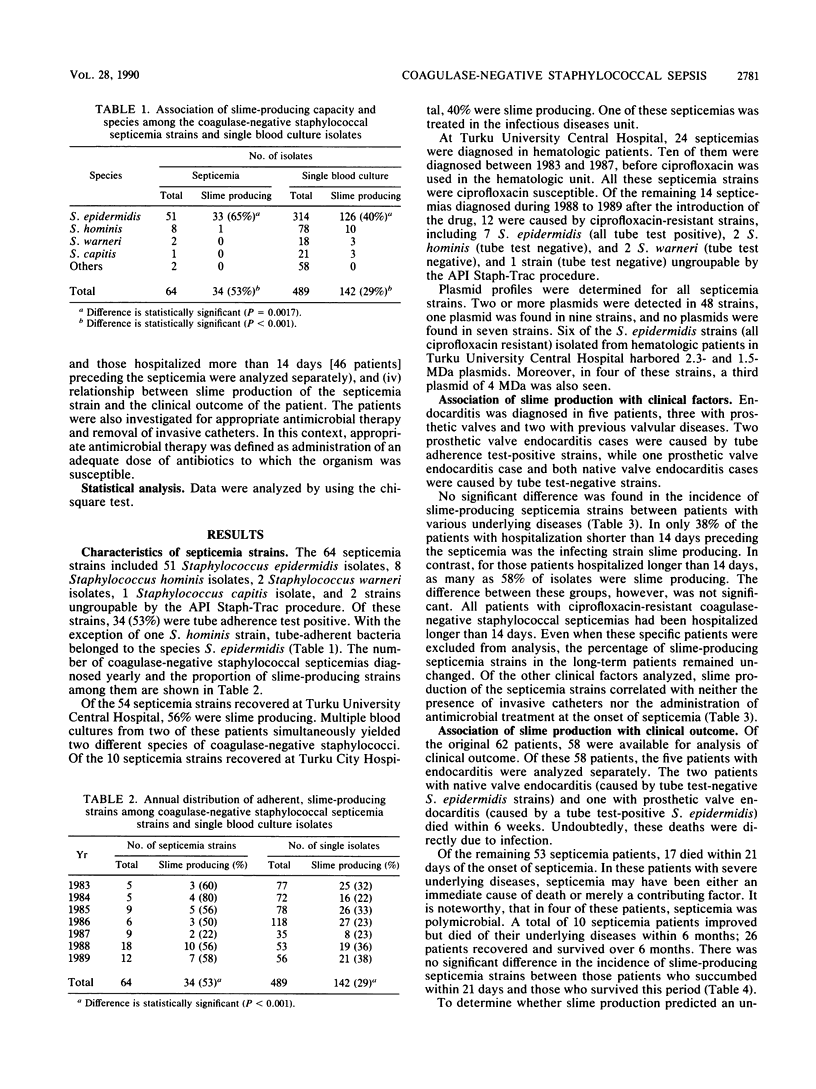
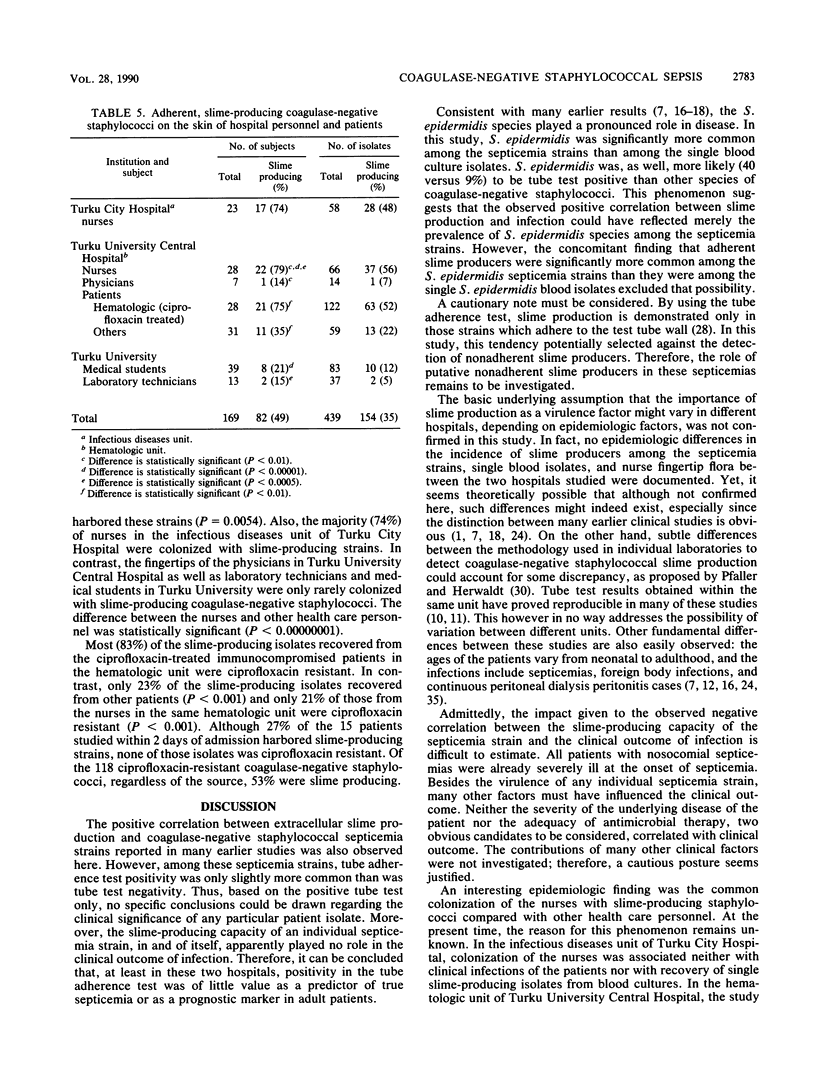
The relationship of coagulase-negative staphylococcal slime production and adherence with the development and outcome of bloodstream infections in two Finnish hospitals was evaluated. Analysis of 64 strains from 62 adult septicemias disclosed 34 (53%) adherent slime producers. In comparison, only 142 (29%) of 489 single blood culture isolates were adherent slime producers. Although tube adherence test-positive strains were significantly (P less than 0.001) more common among the septicemia strains than among clinically insignificant isolates, almost half of the septicemia cases were caused by tube test-negative strains. Thus, regarding any single patient isolate, a cautious posture to the clinical impact of positivity in the tube adherence test seems warranted. Moreover, adherence and slime production, as such, apparently played no role in the clinical outcome of these infections. The epidemiologic findings revealed that slime-producing coagulase-negative staphylococci were common in the hospital environment and suggested that epidemic spread of such strains was influenced by antimicrobial therapy. Collectively, these results indicate that, at least in these two hospitals, positivity in the tube was of minor importance in guiding clinical decisions in treating adult septicemias.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alexander W., Rimland D. Lack of correlation of slime production with pathogenicity in continuous ambulatory peritoneal dialysis peritonitis caused by coagulase negative staphylococci. Diagn Microbiol Infect Dis. 1987 Dec;8(4):215–220. doi: 10.1016/0732-8893(87)90052-6. [DOI] [PubMed] [Google Scholar]
- Baddour L. M., Christensen G. D., Hester M. G., Bisno A. L. Production of experimental endocarditis by coagulase-negative staphylococci: variability in species virulence. J Infect Dis. 1984 Nov;150(5):721–727. doi: 10.1093/infdis/150.5.721. [DOI] [PubMed] [Google Scholar]
- Bayston R. A model of catheter colonisation in vitro and its relationship to clinical catheter infections. J Infect. 1984 Nov;9(3):271–276. doi: 10.1016/s0163-4453(84)90596-6. [DOI] [PubMed] [Google Scholar]
- Bayston R., Penny S. R. Excessive production of mucoid substance in staphylococcus SIIA: a possible factor in colonisation of Holter shunts. Dev Med Child Neurol Suppl. 1972;27:25–28. doi: 10.1111/j.1469-8749.1972.tb09769.x. [DOI] [PubMed] [Google Scholar]
- Christensen G. D., Baddour L. M., Simpson W. A. Phenotypic variation of Staphylococcus epidermidis slime production in vitro and in vivo. Infect Immun. 1987 Dec;55(12):2870–2877. doi: 10.1128/iai.55.12.2870-2877.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen G. D., Parisi J. T., Bisno A. L., Simpson W. A., Beachey E. H. Characterization of clinically significant strains of coagulase-negative staphylococci. J Clin Microbiol. 1983 Aug;18(2):258–269. doi: 10.1128/jcm.18.2.258-269.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen G. D., Simpson W. A., Bisno A. L., Beachey E. H. Adherence of slime-producing strains of Staphylococcus epidermidis to smooth surfaces. Infect Immun. 1982 Jul;37(1):318–326. doi: 10.1128/iai.37.1.318-326.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen G. D., Simpson W. A., Younger J. J., Baddour L. M., Barrett F. F., Melton D. M., Beachey E. H. Adherence of coagulase-negative staphylococci to plastic tissue culture plates: a quantitative model for the adherence of staphylococci to medical devices. J Clin Microbiol. 1985 Dec;22(6):996–1006. doi: 10.1128/jcm.22.6.996-1006.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davenport D. S., Massanari R. M., Pfaller M. A., Bale M. J., Streed S. A., Hierholzer W. J., Jr Usefulness of a test for slime production as a marker for clinically significant infections with coagulase-negative staphylococci. J Infect Dis. 1986 Feb;153(2):332–339. doi: 10.1093/infdis/153.2.332. [DOI] [PubMed] [Google Scholar]
- Diaz-Mitoma F., Harding G. K., Hoban D. J., Roberts R. S., Low D. E. Clinical significance of a test for slime production in ventriculoperitoneal shunt infections caused by coagulase-negative staphylococci. J Infect Dis. 1987 Oct;156(4):555–560. doi: 10.1093/infdis/156.4.555. [DOI] [PubMed] [Google Scholar]
- Dunne W. M., Jr, Nelson D. B., Chusid M. J. Epidemiologic markers of pediatric infections caused by coagulase-negative staphylococci. Pediatr Infect Dis J. 1987 Nov;6(11):1031–1035. [PubMed] [Google Scholar]
- Etienne J., Brun Y., el Solh N., Delorme V., Mouren C., Bes M., Fleurette J. Characterization of clinically significant isolates of Staphylococcus epidermidis from patients with endocarditis. J Clin Microbiol. 1988 Apr;26(4):613–617. doi: 10.1128/jcm.26.4.613-617.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farber B. F., Kaplan M. H., Clogston A. G. Staphylococcus epidermidis extracted slime inhibits the antimicrobial action of glycopeptide antibiotics. J Infect Dis. 1990 Jan;161(1):37–40. doi: 10.1093/infdis/161.1.37. [DOI] [PubMed] [Google Scholar]
- Gray E. D., Peters G., Verstegen M., Regelmann W. E. Effect of extracellular slime substance from Staphylococcus epidermidis on the human cellular immune response. Lancet. 1984 Feb 18;1(8373):365–367. doi: 10.1016/s0140-6736(84)90413-6. [DOI] [PubMed] [Google Scholar]
- Hall R. T., Hall S. L., Barnes W. G., Izuegbu J., Rogolsky M., Zorbas I. Characteristics of coagulase-negative staphylococci from infants with bacteremia. Pediatr Infect Dis J. 1987 Apr;6(4):377–383. doi: 10.1097/00006454-198704000-00007. [DOI] [PubMed] [Google Scholar]
- Hamory B. H., Parisi J. T., Hutton J. P. Staphylococcus epidermidis: a significant nosocomial pathogen. Am J Infect Control. 1987 Apr;15(2):59–74. doi: 10.1016/0196-6553(87)90003-4. [DOI] [PubMed] [Google Scholar]
- Ishak M. A., Gröschel D. H., Mandell G. L., Wenzel R. P. Association of slime with pathogenicity of coagulase-negative staphylococci causing nosocomial septicemia. J Clin Microbiol. 1985 Dec;22(6):1025–1029. doi: 10.1128/jcm.22.6.1025-1029.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson G. M., Lee D. A., Regelmann W. E., Gray E. D., Peters G., Quie P. G. Interference with granulocyte function by Staphylococcus epidermidis slime. Infect Immun. 1986 Oct;54(1):13–20. doi: 10.1128/iai.54.1.13-20.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karchmer A. W., Archer G. L., Dismukes W. E. Staphylococcus epidermidis causing prosthetic valve endocarditis: microbiologic and clinical observations as guides to therapy. Ann Intern Med. 1983 Apr;98(4):447–455. doi: 10.7326/0003-4819-98-4-447. [DOI] [PubMed] [Google Scholar]
- Kotilainen P., Nikoskelainen J., Huovinen P. Emergence of ciprofloxacin-resistant coagulase-negative staphylococcal skin flora in immunocompromised patients receiving ciprofloxacin. J Infect Dis. 1990 Jan;161(1):41–44. doi: 10.1093/infdis/161.1.41. [DOI] [PubMed] [Google Scholar]
- Kristinsson K. G., Spencer R. C., Brown C. B. Clinical importance of production of slime by coagulase negative staphylococci in chronic ambulatory peritoneal dialysis. J Clin Pathol. 1986 Jan;39(1):117–118. doi: 10.1136/jcp.39.1.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowy F. D., Hammer S. M. Staphylococcus epidermidis infections. Ann Intern Med. 1983 Dec;99(6):834–839. doi: 10.7326/0003-4819-99-6-834. [DOI] [PubMed] [Google Scholar]
- Ludlam H. A., Noble W. C., Marples R. R., Bayston R., Phillips I. The epidemiology of peritonitis caused by coagulase-negative staphylococci in continuous ambulatory peritoneal dialysis. J Med Microbiol. 1989 Nov;30(3):167–174. doi: 10.1099/00222615-30-3-167. [DOI] [PubMed] [Google Scholar]
- Ludwicka A., Uhlenbruck G., Peters G., Seng P. N., Gray E. D., Jeljaszewicz J., Pulverer G. Investigation on extracellular slime substance produced by Staphylococcus epidermidis. Zentralbl Bakteriol Mikrobiol Hyg A. 1984 Dec;258(2-3):256–267. doi: 10.1016/s0176-6724(84)80043-7. [DOI] [PubMed] [Google Scholar]
- Needham C. A., Stempsey W. Incidence, adherence, and antibiotic resistance of coagulase-negative Staphylococcus species causing human disease. Diagn Microbiol Infect Dis. 1984 Sep;2(4):293–299. doi: 10.1016/0732-8893(84)90060-9. [DOI] [PubMed] [Google Scholar]
- Peters G., Locci R., Pulverer G. Adherence and growth of coagulase-negative staphylococci on surfaces of intravenous catheters. J Infect Dis. 1982 Oct;146(4):479–482. doi: 10.1093/infdis/146.4.479. [DOI] [PubMed] [Google Scholar]
- Peters G. New considerations in the pathogenesis of coagulase-negative staphylococcal foreign body infections. J Antimicrob Chemother. 1988 Apr;21 (Suppl 100):139–148. doi: 10.1093/jac/21.suppl_c.139. [DOI] [PubMed] [Google Scholar]
- Pfaller M. A., Herwaldt L. A. Laboratory, clinical, and epidemiological aspects of coagulase-negative staphylococci. Clin Microbiol Rev. 1988 Jul;1(3):281–299. doi: 10.1128/cmr.1.3.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ponce de Leon S., Wenzel R. P. Hospital-acquired bloodstream infections with Staphylococcus epidermidis. Review of 100 cases. Am J Med. 1984 Oct;77(4):639–644. doi: 10.1016/0002-9343(84)90354-1. [DOI] [PubMed] [Google Scholar]
- Sheth N. K., Franson T. R., Sohnle P. G. Influence of bacterial adherence to intravascular catheters on in-vitro antibiotic susceptibility. Lancet. 1985 Dec 7;2(8467):1266–1268. doi: 10.1016/s0140-6736(85)91552-1. [DOI] [PubMed] [Google Scholar]
- Wade J. C., Schimpff S. C., Newman K. A., Wiernik P. H. Staphylococcus epidermidis: an increasing cause of infection in patients with granulocytopenia. Ann Intern Med. 1982 Oct;97(4):503–508. doi: 10.7326/0003-4819-97-4-503. [DOI] [PubMed] [Google Scholar]
- West T. E., Walshe J. J., Krol C. P., Amsterdam D. Staphylococcal peritonitis in patients on continuous peritoneal dialysis. J Clin Microbiol. 1986 May;23(5):809–812. doi: 10.1128/jcm.23.5.809-812.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Younger J. J., Christensen G. D., Bartley D. L., Simmons J. C., Barrett F. F. Coagulase-negative staphylococci isolated from cerebrospinal fluid shunts: importance of slime production, species identification, and shunt removal to clinical outcome. J Infect Dis. 1987 Oct;156(4):548–554. doi: 10.1093/infdis/156.4.548. [DOI] [PubMed] [Google Scholar]


