Abstract
Infection with a wide variety of viruses often perturbs host cell signaling pathways including the Jun NH2-terminal kinase/stress-activated kinase (JNK/SAPK) and the p38 mitogen-activated protein kinase (p38/MAPK), which are important components of cellular signal transduction pathways. The present study demonstrated for the first time that porcine circovirus type 2 (PCV2), which is the primary causative agent of an emerging swine disease, postweaning multisystemic wasting syndrome, can activate JNK1/2 and p38 MAPK pathways in PCV2-infected PK15 cells. However, PCV2 at an early stage of infection, as well as UV-irradiated PCV2, failed to activate these two MAPK families, which demonstrated that PCV2 replication was necessary for their activation. We further found that PCV2 activated the phosphorylation of JNK1/2 and p38 MAPK downstream targets c-Jun and ATF-2 with virus replication in the cultured cells. The roles of these kinases in PCV2 infection were further evaluated using specific inhibitors: the JNK inhibitor 1 for JNK1/2 and SB202190 for p38. Inhibition of JNK1/2 and p38 kinases by these specific inhibitors did result in significant reduction of PCV2 viral mRNA transcription and protein synthesis, viral progeny release, and blockage of PCV2-induced apoptotic caspase-3 activation in the infected cells. Taken together, these data suggest that JNK/SAPK and p38 MAPK pathways play important roles in the PCV2 replication and contribute to virus-mediated changes in host cells.
Porcine circovirus (PCV) is classified in the genus Circovirus of the family Circoviridae (52). PCV was first discovered in 1974 as a contaminant of a continuous porcine kidney cell line (PK15) (49). Two genotypes of PCV have been identified. PCV type 1 (PCV1) is known to be nonpathogenic to pigs (1). A high prevalence of anti-PCV1 antibodies has been detected in the swine population, but no disease is correlated with PCV1 infection (33, 50). In contrast, infection with PCV2 occurs in all swine-producing areas of the world, and related PCV2-associated diseases are increasingly recognized as serious threats to global pig production (2, 7, 11, 13, 34, 39, 43). A primary manifestation of PCV2 infection is postweaning multisystemic wasting syndrome (PMWS), which appears in pigs aged 5 to 18 weeks and is clinically characterized by fever, wasting or unthriftiness, respiratory distress, enlarged lymph nodes and, occasionally, jaundice and diarrhea (8, 19, 43). Mortality rates may vary from 1 to 2% up to 30% in complicated cases when coinfections with porcine reproductive and respiratory syndrome virus, porcine parvovirus, or Mycoplasma hyopneumoniae (12). Microscopic lesions are characterized by lymphocyte depletion of follicular and interfollicular areas together with macrophage infiltration of lymphoid tissues in PMWS-affected pigs. Several lines of field and experimental evidence have suggested that severely PMWS affected pigs may develop immunosuppression (44).
PCV genome is a circular single-stranded DNA molecule of ∼1.7 kb. Two major open reading frames (ORFs) have been recognized for PCV: ORF1, called the rep gene, which encodes a protein of 35.7 kDa involved in virus replication (35), and ORF2, called the cap gene, which encodes the major immunogenic capsid protein of 27.8 kDa (5, 38). In addition to the replicase ORF1 and the capsid protein ORF2, a novel protein, ORF3, has been detected in PCV2 productive infection and is not essential for PCV2 replication in the cultured cells but is involved in viral pathogenesis via an apoptotic function (30, 31). In a recent report, we demonstrated that PCV2 infection induces NF-κB activation in the cultured cells and further found the role of NF-κB activation in PCV2 replication and PCV2-induced apoptotic caspase activity (56). However, whether other signaling pathways may also contribute to PCV2 infection in the cultured cells remains unclear.
Mitogen-activated protein kinases (MAPKs), including extracellular signal-regulated kinases (ERK1/2), c-Jun NH2-terminal kinase/stress-activated protein kinase (JNK/SAPK), and p38 MAPK, are central components of signal transduction pathways in the regulation of cell proliferation and differentiation, cytokine production, and apoptosis (17). ERK1/2 is primarily activated by growth factors, cytokines, and phagocytosis, whereas JNK and p38 are potently induced by proinflammatory cytokines, bacterial endotoxins, and environmental stresses (17, 26). Although there is coordinated regulation of JNK/SAPK and p38 MAPK, they have corresponding downstream targets. Activated JNK/SAPK and p38 MAPK can phosphorylate numerous substrates, including a variety of transcription factors. The transcription factor c-Jun is specifically phosphorylated by JNK/SAPK, while ATF-2 is phosphorylated by both JNK/SAPK and p38 MAPK (9, 18, 29). Phosphorylation and activation of these downstream substrates ultimately alters gene expression, thereby manifesting the biological consequences of JNK/SAPK and p38 MAPK activation (57).
It has been shown that viruses are ultimately dependent on the host cell for their replication via altering cellular signal transduction pathways, including MAPK cascades. For instance, modulation of JNK and/or p38 MAPK pathways is required for infection and replication of human immunodeficiency virus type 1 (27), herpes simplex virus type 1 (HSV-1) (60), Epstein-Barr virus (16), Kaposi's sarcoma-associated herpesvirus (41, 58), echovirus 1 (24), Sindbis virus (37), encephalomyocarditis virus (21), coxsackievirus B3 (46), and varicella-zoster virus (42, 61). However, there is still no report on the activation of JNK/SAPK and p38 MAPK induced by PCV2 replication and the effects of their activation on PCV2 replication.
The present study was initiated to determine whether JNK/SAPK and p38 MAPK play a role in the replication of PCV2. Here, we report that phosphorylation of JNK/SAPK and p38 MAPK is increased during PCV2 replication and demonstrate that activation of these two MAPK pathways is essential for efficient PCV2 replication. Inhibition of these two MAPK activations reduces viral mRNA transcription and protein synthesis, viral progeny release, and PCV2-induced apoptotic caspase activity. These findings indicate that the JNK/SAPK and p38 MAPK pathways are involved in the PCV2 replication and contribute to virus-mediated changes in host cells.
MATERIALS AND METHODS
Virus and cells.
The permanent PK15 cell line, which was free of PCV, was maintained in minimal essential medium supplemented with 5% heat-inactivated fetal bovine serum (FBS), 5% l-glutamine, 100 U of penicillin G/ml, and 100 μl of streptomycin/ml at 37°C in a humidified 5% CO2 incubator. The PCV2 used in the study was originally isolated from a kidney tissue sample of a pig with naturally occurring PMWS (strain BJW) (31).
For PCV2 infection, PK15 cells seeded the day before were infected with PCV2 strain BJW at a multiplicity of infection (MOI) of 1 50% tissue culture infective dose (TCID50). Cells were additionally treated with 300 mM d-glucosamine at 24 h after infection as described previously (51).
Reagents and antibodies.
The JNK peptide inhibitor 1 and SB202190 were purchased from Calbiochem (La Jolla, CA). PK15 cells were treated with either dimethyl sulfoxide (DMSO), which is the solvent for JNK peptide inhibitor 1 and SB202190, or various concentrations (5 to 20 μM) of these two inhibitors for 1 h prior to infection. After 1 h of virus adsorption, the virus inoculum was removed, and fresh basal medium containing fresh inhibitor was added to the culture. The cytotoxicity of the inhibitors on PK15 cells was determined by trypan blue exclusion dye staining. It was noted that throughout all doses of the inhibitors used in the present study, cell viability assay showed no detectable cell death in the PK15 cells.
Rabbit antibodies against c-Jun, ATF-2, phosphorylated c-Jun (p-c-Jun), phosphorylated ATF-2 (p-ATF-2), and β-actin were purchased from Santa Cruz Biotechnology. Antibodies specific for p38 and JNK, as well as phosphorylated forms of p38 (p-p38) and JNK (p-JNK), were obtained from Cell Signaling Technology. Horseradish peroxidase (HRP)-linked secondary antibodies were purchased from Sigma.
FACE.
Fast-activated cell-based enzyme-linked immunosorbent assay (FACE) kits to monitor the levels of JNK1/2 and p38 MAPK activation were obtained from Active Motif. Procedures were performed strictly according to the manufacturer's instructions. Briefly, PK15 cells seeded in 96-well plates 1 day were infected with PCV2 strain BJW and fixed with 4% formaldehyde in phosphate-buffered saline (PBS) at the indicated time points after infection. After washing and blocking steps, the cells were reacted overnight with an anti-JNK, anti-phospho-JNK, anti-p38, or anti-phospho-p38 antibody. After incubation with a HRP-conjugated secondary antibody, colorimetric analysis was performed. The A450 was determined by using a plate spectrophotometer.
RT-PCR.
The spliced cap mRNA during the course of PCV2 infection in the cultured cells was assayed by reverse transcription-PCR (RT-PCR) as described elsewhere (59). Briefly, total cell RNAs were prepared from virus-infected PK15 cells 24 h after being treated with various concentrations of JNK inhibitor 1 or p38 inhibitor SB202190 by using TRIzol RNA extract reagent (Invitrogen) for RT-PCR. The RNA samples were incubated with DNase I for 60 min at 37°C to remove any contaminating viral DNA. A sense primer (5′-TTTACTTAGGGGTCATAGGTGAG-3′) and an antisense primer (5′-AGACTCCCGCTCTCCAACAAG-3′) were used to amplify a 515-bp product from the spliced cap mRNA. cDNAs were reverse transcribed from total RNAs by the use of the antisense primer and the first-strand synthesis system (AMV reverse transcriptase kit; Roche). In addition, β-actin gene was used as an internal standard and amplified by using a pair of primers (forward, 5′-CCTCCCTGGAGAAGAGCTAC-3′; reverse, 5′-GATCCACACGGAGTACTTGA-3′). The PCR consisted of an initial denaturation at 94°C for 5 min, followed by 94°C for 45 s, annealing at 52°C for 45 s, extension at 72°C for 1 min, and a final extension at 72°C for 10 min. The PCR product was electrophoresed in 1% agarose gel and photographed.
Immunochemical staining (ICS).
PK15 monolayer cells seeded in 24-well culture plates were infected with PCV2 strain BJW. At 72 h, the cells were washed with PBS and fixed in 4% paraformaldehyde. After three washes, the cells were incubated with mouse anti-ORF2 antibody (56) diluted in 3% bovine serum albumin-PBS at room temperature for 1 h. After three further washes, cells were incubated with HRP-conjugated anti-mouse immunoglobulin G (Sigma) at room temperature for 1 h and washed with PBS three times. Color development was carried out with 3,3′-diaminobenzidine tetrahydrochloride (Pierce) substrate and then stopped with distilled water. The cells were examined under a microscope, and cells positive for PCV2 viral antigens were counted in six fields of view.
Whole-cell lysates.
Whole-cell lysate extracts from PK15 cells at various time points after infection were prepared with a nuclear extract kit (Active Motif) according to the manufacturer's protocol. Protein concentration was determined by using a protein assay (Bio-Rad, Hercules, CA) with bovine serum albumin as a standard.
Western blotting.
The whole-cell lysate extracts prepared as described above were diluted in 2× sample buffer and boiled for 5 min. Portion (20 μg) of each extract were resolved by sodium dodecyl sulfate-10% polyacrylamide gel electrophoresis (SDS-10% PAGE) and blotted onto nitrocellulose (NC) membranes (Stratagene) with a semidry transfer cell (Bio-Rad). The membranes were blocked for 2 h at room temperature in blocking buffer TBST (20 mM Tris-HCl [pH 7.4], 150 mM NaCl, 0.1% Tween 20) containing 5% skim milk powder to prevent nonspecific binding and then incubated with specific primary antibodies raised against ORF2, JNK1/2, p38, c-Jun, ATF-2, p-JNK1/2, p-p38, p-c-Jun, and p-ATF-2, as well as β-actin, at room temperature for 2 h. The membranes were washed three times with TBST buffer and then incubated for 2 h at room temperature with HRP-conjugated secondary antibodies diluted in blocking buffer (1:2,000). Immunoreactive bands were visualized by using an enhanced chemiluminescence system (Amersham Biosciences).
Fluorimetric assay of caspase-3 activity.
Spectrofluorometric assays of proteolytic activity were carried out using the synthetic fluorogenic substrate 7-amino-4-trifluoromethyl coumarin (AFC) to measure caspase-3 activity. A BD ApoAlert caspase fluorescent assay kit (Clontech) was used to determine caspase-3 activity. In brief, 80% confluent monolayers of PK15 cells grown on T-25 flasks were infected with PCV2 at an MOI of 1 TCID50 with various amounts of JNK1/2 or p38 MAPK inhibitor treatment. At 72 h postinfection, cells were harvested at 400 × g for 5 min. Cells (2 × 106 to 3 × 106) were lysed in 50 μl of lysis buffer on ice for 10 min and centrifuged at 16,000 × g for 10 min, and the supernatant was collected. A 50-μl supernatant was added to an equal volume of 2× reaction-dithiothreitol buffer supplemented with caspase-3 substrate DEVD-AFC and then incubated at 37°C for 2 h. The optical densities at 400 nm for caspase-3 were determined. The nanomoles of AFC (released) expressed per hour were calculated from the standard curve.
Statistical analysis.
Results are presented as averages ± the standard deviations (SD) or standard errors of the means, as indicated. Statistical comparisons are made by using a Student t test, and differences between groups were considered significant if the P value was <0.05.
RESULTS
Activation of JNK/SAPK and p38 MAPK during PCV2 infection.
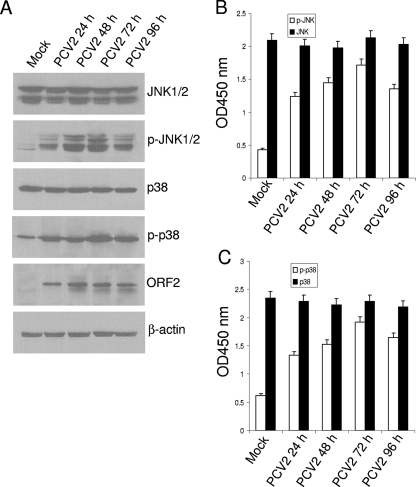
It was reported that JNK/SAPK and p38 MAPK are phosphorylated during various virus infection. In order to assess whether activation of these two MAPK signaling pathways occurred in the cultured cells during the course of PCV2 infection, the degrees of JNK1/2 and p38 phosphorylation in the PCV2-infected cells were examined by Western blotting. PK15 cells were infected with PCV2 strain BJW at an MOI of 1 TCID50, and whole-cell lysates were prepared at 24, 48, 72, and 96 h after infection. Incubation with PBS served as mock-infected controls. As shown in Fig. 1A, infection with PCV2 led to progressive accumulation of p-JNK1/2 signals over time, and the maximal induction was seen at 72 h postinfection. The kinetics of p-p38 accumulation in the PCV2-infected cells was similar to that of the accumulation of phosphorylated JNK (Fig. 1A). The increased levels of JNK and p38 MAPK phosphorylation were concurrent with the expression of viral capsid protein ORF2 in the infected cells (Fig. 1A). In contrast, the protein levels of total amounts of JNK1/2 and p38 remained unchanged in the PCV2-infected cells at various time points after infection compared to that in the mock-infected cells. A loading control, β-actin in each sample, was comparable.
FIG. 1.
PCV2 infection activates JNK1/2 and p38 MAPK signaling pathways in the cultured cells. (A) Whole-cell lysates from PK15 cells after infection with PCV2 strain BJW at an MOI of 1 TCID50. PCV2-infected cells were harvested at 24, 48, 72, and 96 h postinfection, and whole-cell lysates were prepared and resolved by SDS-PAGE, transferred to nitrocellulose membranes, and immunoblotted. The protein levels of JNK1/2 and p38 and their phosphorylated forms, as well as PCV2 viral capsid protein, were analyzed. The amounts of β-actin were also assessed to monitor the equal loadings of protein extracts. (B and C) JNK1/2 (B) and p38 MAPK (C) activation induced by PCV2 infection was determined by using FACE assay. PK15 cells were fixed at the indicated time points with 4% formaldehyde and incubated with antibodies directed against JNK1/2 or p38 or their phosphorylated forms followed by HRP-conjugated immunoglobulin G antibodies. JNK1/2 and p38 and their phosphorylated forms were each assayed in triplicate. Cell numbers were normalized by using crystal violet. These results are representative of three independent experiments. Values are means ± the SD from triplicate wells. p-, Phosphorylated.
To further determine activated JNK and p38 MAPK quantitatively in the infected cells, we used FACE assays to investigate the levels of ability of JNK and p38 MAPK phosphorylation at the indicated time points after PCV2 infection. As shown by Fig. 1B and C, there was a time-dependent increase in the JNK1/2 and p38 phosphorylation in the PCV2-infected cells at 72 h postinfection which decreased thereafter. At 72 h after infection, the activations of phosphorylated JNK and p38 showed approximately 4.3- and 3.1-fold increases, respectively, versus those in the mock-infected cells. In addition, the levels of total JNK and p38 remained unchanged in the PCV2-infected cells at various time points after infection compared to that in the mock-infected cells. These data indicate that PCV2 infection induces the activation of JNK and p38 MAPK signaling pathways.
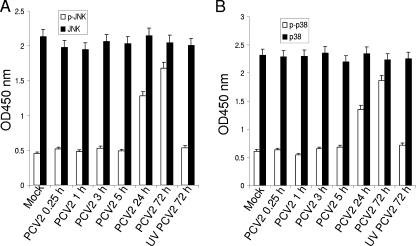
PCV2 replication is required for JNK/SAPK and p38 MAPK phosphorylation.
It has been shown that replicating virus can be detected in PCV2-infected PK15 cells as early as 14 h postinfection (59). Therefore, we used the FACE assay to determine whether PCV2 replication was required for JNK and p38 MAPK phosphorylation during the early phase of PCV2 infection. As shown in Fig. 2, no significant increase in activation of phosphorylated JNK or p38 MAPK was observed from 0.25 h through 5 h postinfection. In contrast, the levels of JNK and p38 MAPK phosphorylation increased by 1.8- and 2.3-fold, respectively, at 24 h postinfection. The levels of total JNK and p38 remained unchanged in the PCV2-infected cells at various time points after infection compared to that in the mock-infected cells. In addition, no replicating virus was detected in the PCV2-inoculated cells from 0.25 h to 5 h postinoculation, whereas the accumulation of PCV2 cap spliced transcript was observed at 24 h postinoculation (data not shown).
FIG. 2.
PCV2 replication is required for JNK1/2 and p38 MAPK phosphorylation. Monolayer PK15 cells were infected with PCV2 strain BJW at an MOI of 1 TCID50. PCV2-infected cells at 0.25, 1, 3, 5, and 24 h as well as UV-irradiated PCV2-infected cells at 72 h were fixed with 4% formaldehyde. A FACE assay was used for determination of JNK1/2 (A) or p38 (B) activation. JNK1/2 and p38 and their phosphorylated forms were each assayed in triplicate. Cell numbers were normalized by using crystal violet. These results are representative of three independent experiments. Values are means ± the SD from triplicate wells. p-, Phosphorylated.
We further used an UV light-irradiated PCV2 to determine whether phosphorylation of JNK1/2 and p38 MAPK was associated with PCV2 replication. Culture fluid from both PCV2-infected PK15 cells and mock-infected PK15 cells was collected at 72 h postinfection and exposed to UV light (wavelength, 253 nm) for 20 min. In the UV-irradiated PCV2-infected cells at 72 h postinfection, the level of JNK or p38 phosphorylation fell to its basal level as seen in the mock-infected cells (Fig. 2). These results demonstrated that PCV2 replication was required for JNK and p38 MAPK phosphorylation and eliminated the possibility that attachment of PCV2 to cell surface receptors alone was responsible for JNK and p38 MAPK phosphorylation in the infected cells.
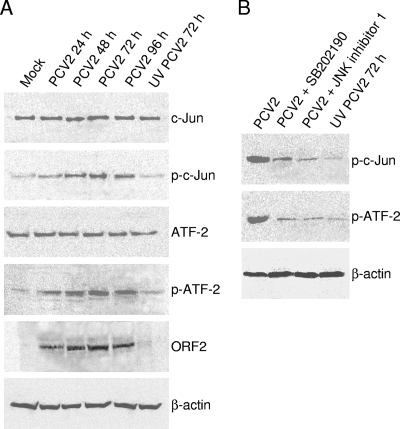
Phosphorylated JNK/SAPK and p38 MAPK in infected cells activate downstream targets.
Activated JNK and p38 perform Ser/Thr phosphorylation of c-Jun inducing transcription factor and ATF-2, respectively. To confirm that phosphorylation of JNK and p38 MAPK after PCV2 infection truly activated their downstream substrates c-Jun and ATF-2, respectively, the phosphorylation of these two downstream substrates was measured in the infected cells by Western blotting. As shown in Fig. 3A, no activation of c-Jun and ATF-2 was detected in the mock-infected PK15 cells. Consistent with the activation of JNK and p38, a concomitant increase in c-Jun and ATF-2 phosphorylation was observed, which peaked at 72 h postinfection and then declined (Fig. 3A). In contrast, the protein levels of total amounts of c-Jun and ATF-2 remained unchanged in the PCV2-infected cells at various time points after infection compared to that in the mock-infected cells. Cells exposed to the UV-irradiated virus sample also failed to phosphorylate c-Jun or ATF-2 (Fig. 3A). The level of β-actin, used as a loading control, remained constant.
FIG. 3.
Phosphorylated JNK1/2 and p38 MAPK activate downstream targets c-Jun and ATF-2 signals. (A) PK15 cells were infected with PCV2 strain BJW at an MOI of 1 TCID50. PCV2-infected cell lysates at 24, 48, 72, and 96 h, as well as UV-irradiated PCV2-infected cell lysates at 72 h, were harvested and resolved by SDS-PAGE, transferred to nitrocellulose membranes, and immunoblotted. The protein levels of c-Jun and ATF-2 and their phosphorylated forms, as well as of PCV2 viral capsid protein, were analyzed. (B) PK15 cells were infected in the absence or presence of JNK inhibitor 1 (20 μM) or p38 inhibitor SB202190 (20 μM). Cell lysates at 72 h postinfection were harvested to examine c-Jun and ATF-2 phosphorylation. β-Actin was probed as the loading control. p-, Phosphorylated.
We then determined the effects of JNK inhibitor (the JNK inhibitor 1) or p38 MAPK inhibitor (SB202190) on the activation of JNK or p38 MAPK downstream substrates. As determined by testing for cell viability by trypan blue exclusion staining, the concentrations (5 to 20 μM for the JNK inhibitor 1 and SB202190) had no toxic effects on the treated cells (data not shown). In addition, the selected concentrations of these two inhibitors were tested to show their effectiveness in inhibiting virus-induced JNK or p38 MAPK activity by the FACE assay, which demonstrated that activation of JNK and p38 MAPK decreased dose dependently after treatment with their corresponding inhibitors (data not shown).
We treated the infected cells with the JNK inhibitor 1 or SB202190 at a concentration of 20 μM and determined the levels of phosphorylated c-Jun and ATF-2 by Western blotting analysis. As shown in Fig. 3B, the phosphorylation of ATF-2, which is phosphorylated by the p38 MAPK pathway, was blocked by the p38 MAPK-specific inhibitor SB202190, while the activation of ATF-2 was substantially increased after PCV2 infection. In addition, the phosphorylation of c-Jun, which is phosphorylated by the JNK pathway, was also inhibited by treatment with SB202190 (Fig. 3B). While we examined the phosphorylation of c-Jun and ATF-2 after treatment with the JNK inhibitor 1, we also found that the inhibitor was able to reduce PCV2-induced c-Jun and ATF-2 phosphorylation (Fig. 3B).
Inhibition of ATF-2 activation by treatment with JNK inhibitor 1 and p38 inhibitor SB202190 was due to both JNK and p38 phosphorylated ATF-2 in the PCV2-infected cells, In addition, we also observed that p38 inhibitor SB202190 reduced c-Jun activation, which is only phosphorylated by JNK. This suggests that an indirect inhibition of c-Jun activation might be related to reduction of PCV2 replication when the PCV2-infected cells were treated with p38 inhibition. Therefore, these data suggested that phosphorylation of these two MAPKs as a consequence of PCV2 infection led to the activation of downstream targets.
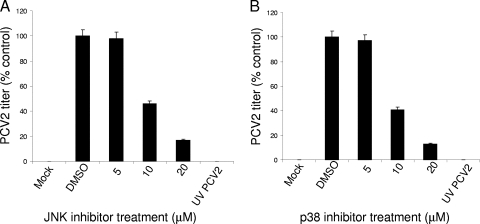
JNK/SAPK and p38 MAPK regulate PCV2 replication.
To determine whether activated JNK/SAPK and p38 MAPK play any role in the replication of PCV2, we examined the effect of these kinases on progeny virus production in the PCV2-infected PK15 cells by treatment with these kinase inhibitors. We infected PK15 cells with PCV2 in the presence of JNK inhibitor 1 (5 to 20 μM) or the p38 inhibitor SB202190 (5 to 20 μM) and determined the virus titers in the cell culture supernatant at 72 h postinfection by using an ICS assay. PCV2 replication in PK15 cells was not significantly altered by the presence of JNK or p38 inhibitors at 5 μM (Fig. 4). At 10 and 20 μM, the JNK inhibitor reduced PCV2 growth in the cultured cells by 54 and 83%, respectively. Treatment with the p38 inhibitor SB202190 at 10 and 20 μM reduced PCV2 growth by 59 and 87%, respectively. As expected, the UV-irradiated PCV2 failed to grow compared to the mock-infected cells (Fig. 4). These results suggested that the activation of MAPK pathways involving JNK and p38 regulate the efficient replication of PCV2 in the PK15 cells.
FIG. 4.
Inhibition of JNK1/2 and p38 MAPK phosphorylation blocks PCV2 replication. Supernatants of PCV2-infected PK15 cells at 72 h after treatment with various concentrations of JNK inhibitor 1 (A) or SB202190 (B), as well as UV-irradiated PCV2-infected cell supernatants at 72 h, were inoculated on monolayers of PK15 cells. Virus production was assayed by ICS under a microscope. The values represent the means of results for three independent experiments; error bars indicate the SD.
Effect of JNK/SAPK and p38 MAPK inhibition on PCV2 viral transcription and protein synthesis.
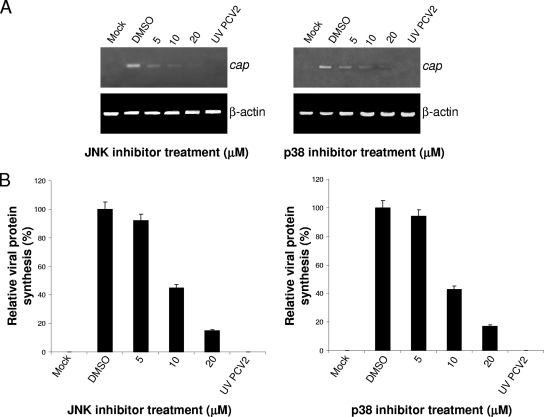
Because the JNK inhibitor and SB202190 inhibited PCV2 replication in PK15 cells, we determined which phase of the replication cycle, viral transcription or protein synthesis, is affected. The PCV2 viral transcription was examined by RT-PCR analysis with RNA extracted from the PCV2-infected PK15 cells 24 h after treatment with the JNK inhibitor 1 or p38 inhibitor SB202190 at various concentrations. The abundance of the target fragment corresponding to the spliced cap mRNA was dose dependently decreased in the PCV2-infected cells with these two inhibitors tested (Fig. 5A). In contrast, the fragment was detected in the DMSO-treated infected cells as seen in the DMSO-untreated infected cells (Fig. 5A and data not shown). No product was amplified from RNA extracted from cells infected with the UV-irradiated PCV2, as well as from the mock-infected PK15 cells (Fig. 5A).
FIG. 5.
Inhibition of JNK1/2 and p38 MAPK phosphorylation decreases viral transcription and protein synthesis in the PCV2-infected PK15 cells. (A) Effects of JNK and p38 inhibitors on PCV2 spliced cap mRNA synthesis in infected cells. Total RNAs (1 μg) isolated from PCV2-infected cells at 24 h after treatment with JNK inhibitor 1 or SB202190 at the indicated concentrations were subjected to RT-PCR analysis of PCV2 spliced cap mRNA synthesis. The products were separated on a 1% agarose gel. β-Actin was used as an internal control. The results are representative of at least three independent experiments. (B) JNK inhibitor 1 and SB202190 reduce PCV2 protein expression. PCV2-infected PK15 cells at 72 h in the presence of the JNK inhibitor 1 (20 μM) or SB202190 (20 μM), as well as UV-irradiated PCV2-infected cells at 72 h, were assayed for the amount of PCV2 viral antigen by ICS. The amounts of PCV2 ORF2 protein expression are shown as percentages of PCV2-positive signals in cells infected with PCV2 alone. The data are mean values ± the SD based on three independent experiments; error bars show the SD.
To help delineate the effect of JNK and p38 inhibition on virus translation, the expression of PCV2 capsid protein ORF2 in the PK15 cells infected with PCV2 in the presence or absence of the inhibitors was analyzed by ICS. The ORF2 protein expressions were significantly reduced when cells were treated with these two inhibitors, as demonstrated by the increased number of PCV2-positive cells observed in the DMSO-treated infected cells (Fig. 5B). No significant differences were seen in the ORF2 protein expression between DMSO-treated infected cells and untreated infected cells (data not shown). No ORF2 protein expression was detected in the UV-irradiated PCV2-infected cells, as well as in the mock-infected cells (Fig. 5B). These results suggested that inhibitors of these two MAPK pathways decreased PCV2 viral RNA transcription and protein synthesis.
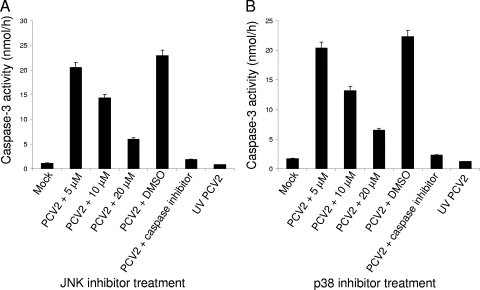
Inhibition of JNK/SAPK and p38 MAPK activation prevents PCV2-mediated caspase activation.
PCV2 has been shown to induce apoptosis in cultured cells through the activation of caspase-8, followed by activation of the caspase-3 pathway (31). As demonstrated above, PCV2 replication was strongly prevented after treatment with these kinase inhibitors. Therefore, to determine whether JNK1/2 and p38 MAPK activation is required for PCV2-induced apoptosis, caspase-3 activity was assayed in the PCV2-infected PK15 cells at 72 h postinfection after treatment with the indicated amounts of these inhibitors. As expected, PCV2 alone induced activation of caspase-3 in the infected cells, whereas its activity was significantly reduced when the infected cells were treated with Ac-DEVD-CHO, a peptide inhibitor of caspase-3 activity (Fig. 6). A basal caspase-3 activity was detected in the UV-irradiated PCV2-infected cells, as well as in the mock-infected cells (Fig. 6). Furthermore, activation of caspase-3 was dose dependently decreased in the infected cells when treated with increasing amounts of the JNK or p38 inhibitor (Fig. 6). Therefore, we believe that the activation of MAPK pathways involving JNK and p38 is required for PCV2-induced apoptosis, but this can be an indirect effect due to a decrease in virus replication when PCV2-infected cells were treated with JNK or p38 inhibition (Fig. 4).
FIG. 6.
Inhibition of JNK1/2 and p38 MAPK phosphorylation reduces PCV2-induced caspase-3 activity. Whole-cell lysates harvested from PCV2-infected cells at 72 h after treatment with various concentrations of the JNK inhibitor 1 (A) or SB202190 (B), as well as UV-irradiated PCV2-infected cells at 72 h, were assayed for DEVDase activity using the caspase-3 colorimetric DEVD-AFC. In addition, cells infected with PCV2 alone were treated with the caspase-3 inhibitor DEVD-CHO. Mock-infected cells were used as a negative control. The values shown are means from duplicate experiments.
DISCUSSION
Viral infections are known to activate various cellular signaling pathways, which can affect cellular function and virus replication. In this report, we show that JNK1/2 and p38 MAPK pathways were activated during the course of PCV2 infection in PK15 cells and that activation of these two MAPK pathways was required for active replication of PCV2. We further show that inhibitors of these two MAPK pathways lead to a reduction of viral activity, as determined by decreases in viral transcription, virus protein synthesis and progeny production, and decreased cell death. This study has demonstrated for the first time that the MAPK signaling pathways involving JNK1/2 and p38 are manipulated by PCV2 and that these two pathways play beneficial roles in the PCV2 replication.
The effect of JNK and p38 MAPK on virus replication has been studied in a number of viruses. We determined whether PCV2-induced JNK and p38 MAPK are involved in viral replication by examining the effects of inhibitors of the MAPK pathways on PCV2 production and found that JNK inhibitor 1 and SB202190 significantly reduced the production of progeny virus (Fig. 4). This shows that optimal PCV2 replication requires these two MAPK activities and raises the possibility that PCV2 has acquired the ability to activate these two MAPK kinases to aid its replication. MAPK activation has been shown to be required for the optimal replication of many other viruses. For instance, rotavirus replication was significantly reduced after JNK and p38 inhibition (22). JNK and p38 activation by HSV requires the expression of particular viral proteins, and blockage of JNK translocation to the nucleus resulted in decreased virus production (10, 20, 36). Coxsackievirus B3 activates JNK and p38 MAPK, which appears to facilitate virus replication and virion release (46). Treatment of HSV-1-infected cells with p38 inhibitor resulted in a decrease in virus titer (60). Human immunodeficiency virus type 1 production was increased in p38 MAPK-activated cells (45). Like the above-mentioned viruses, PCV2-induced activation of JNK and p38 MAPK are truly involved in the replication of PCV2 in PK15 cells.
MAPK regulation of viral replication can act at specific steps of the replication cycle, including entry, gene transcription, protein expression, and assembly. In some cases, inhibition of MAPK activation did not affect viral transcription and/or protein synthesis. For instance, inhibition of p38 MAPK by treatment of HSV-1-infected cells with inhibitor SB203580 did not affect the viral transcription program (25). Coxsackievirus B3 viral protein synthesis was reported to be unaffected by treatment with JNK or p38 inhibitors (46). On the other hand, inhibition of p38 MAPK reduced EMCV replication via inhibition of EMC viral protein synthesis, as well as a secondary effect on viral RNA synthesis (21). Reduced murine coronavirus production in p38 inhibitor SB203580-treated cells was in part due to a decrease in virus-specific protein synthesis and virus-specific mRNA accumulation (3). Efficient translation in HSV-1-infected cells is regulated by p38-dependent eukaryotic translation initiation factor 4E phosphorylation (54). PCV replicates via rolling-circle replication involving an intermediate double-stranded replicative form of DNA (6). In the present study, we further determine which step of PCV2 replication is affected by inhibition of JNK or p38 MAPK activation. Our data showed that treatment of cells with JNK inhibitor 1 or p38 inhibitor SB202190 suppressed PCV2 viral RNA transcription and protein synthesis, which is due to that viral transcription and protein synthesis are closely related in the replication of PCV2. Thus, the results suggest that JNK or p38 MAPK inhibition reduced the accumulation of both viral mRNA and structural protein, followed by causing a lowered production of infectious PCV2 particles in cells. However, our study does not exclude the possibility that these specific inhibitors have a preferential effect on PCV2 viral protein synthesis and/or RNA transcription.
Apoptosis has been shown to be regulated by the JNK and p38 MAPK cellular stress pathways (28, 48, 53). Virus infection can trigger an apoptogenic kinase cascade, leading to the phosphorylation and/or activation of JNK and p38 MAPK, which are responsible for inducing apoptotic cell death (47). Hepatitis B virus X protein-mediated apoptosis was reported to involve sustained activation of JNK and p38 pathways (55). Severe acute respiratory syndrome coronavirus 3a protein-induced apoptosis was dependent on the activation of p38 MAPK (40). In the present study, using the specific inhibitor of JNK or p38 MAPK activation, we demonstrated that interference with the JNK and p38 MAPK pathways leads to reduction of PCV2-induced apoptotic caspase activity (Fig. 6). This result suggests that JNK and p38 MAPK signaling pathways play a role in the mechanism by which PCV2 triggers an apoptotic program in infected cells. In nonstressed cells, nonphosphorylated JNK is complexed to p53, causing its ubiquitination, followed by proteasomal degradation (14, 15). Upon stimulation, the phosphorylated JNK mediates dissociation of p53, followed by its stabilization (14, 15). The role of p38 MAPK kinase in transcription of the p53-regulated Bax and Noxa genes also involves p53 phosphorylation (4, 23). Binding of PCV2 ORF3 protein to porcine p53-induced RING-H2 was reported to interfere with its function of ubiquitination of p53, followed by causing increased p53 level and thus suggesting that the PCV2-induced apoptosis in the cultured cells may be p53 mediated (32). Therefore, activation of JNK and p38 after PCV2 infection may participate in p53 stabilization and phosphorylation, ultimately leading to apoptosis.
In conclusion, the results reported here establish that PCV2 infection induces the activation of JNK and p38 and their involvement in c-Jun and ATF-2 activation in the cultured cells and demonstrate that the activation of JNK or p38 is required for efficient PCV2 replication, as well as PCV2-induced apoptotic cell death. The role of JNK and p38 activation in PCV2 infection and replication will contribute important information about the molecular mechanism of PCV2 pathogenesis.
Acknowledgments
This study was supported by grants from the National Natural Science Foundation (30871866) and the Beijing Municipal Science and Technology Contract Project (Z07010501780701), People's Republic of China.
Footnotes
Published ahead of print on 1 April 2009.
REFERENCES
- 1.Allan, G. M., F. McNeilly, J. P. Cassidy, G. A. Reilly, B. Adair, W. A. Ellis, and M. S. McNulty. 1995. Pathogenesis of porcine circovirus: experimental infections of colostrum-deprived piglets and examination of pig foetal material. Vet. Microbiol. 4449-64. [DOI] [PubMed] [Google Scholar]
- 2.Allan, G. M., F. McNceilly, S. Kennedy, B. Daft, E. G. Clark, J. A. Ellis, D. M. Haines, B. M. Meehan, and B. M. Adair. 1998. Isolation of porcine circovirus-like viruses from pigs with a wasting disease in the USA and Europe. J. Vet. Diagn. Investig. 103-10. [DOI] [PubMed] [Google Scholar]
- 3.Banerjee, S., K. Narayanan, T. Mizutani, and S. Makino. 2002. Murine coronavirus replication-induced p38 mitogen-activated protein kinase activation promotes interleukin-6 production and virus replication in cultured cells. J. Virol. 764937-5948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bulavin, D. V., S. Saito, M. C. Hollander, K. Sakaguchi, C. W. Anderson, E. Appella, and A. J. Fornace, Jr. 1999. Phosphorylation of human p53 by p38 kinase coordinates N-terminal phosphorylation and apoptosis in response to UV radiation. EMBO J. 186845-6854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheung, A. K. 2003. Transcriptional analysis of porcine circovirus type 2. Virology 305168-180. [DOI] [PubMed] [Google Scholar]
- 6.Cheung, A. K. 2006. Rolling-circle replication of an animal circovirus genome in a theta-replicating bacterial plasmid in Escherichia coli. J. Virol. 808686-8694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi, C., C. Chae, and E. G. Clark. 2000. Porcine postweaning multisystemic wasting syndrome in Korean pig: detection of porcine circovirus 2 infection by immunohistochemistry and polymerase chain reaction. J. Vet. Diagn. Investig. 12151-153. [DOI] [PubMed] [Google Scholar]
- 8.Darwich, L., J. Segales, and E. Mateu. 2004. Pathogenesis of postweaning multisystemic wasting syndrome caused by porcine circovirus 2: an immune riddle. Arch. Virol. 149857-874. [DOI] [PubMed] [Google Scholar]
- 9.Derijard, B., M. Hibi, I. H. Wu, T. Barrett, B. Su, T. Deng, M. Karin, and R. J. Davis. 1994. JNK1: a protein kinase stimulated by UV light and Ha-Ras that binds and phosphorylates the c-Jun activation domain. Cell 761025-1037. [DOI] [PubMed] [Google Scholar]
- 10.Diao, L., B. Zhang, C. Xuan, S. Sun, K. Yang, Y. Tang, W. Qiao, Q. Chen, Y. Geng, and C. Wang. 2005. Activation of c-Jun N-terminal kinase (JNK) pathway by HSV-1 immediate-early protein ICP0. Exp. Cell Res. 308196-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Edwards, S., and J. J. Sands. 1994. Evidence of circovirus infection in British pigs. Vet. Rec. 134680-681. [DOI] [PubMed] [Google Scholar]
- 12.Ellis, J., E. Clark, D. Haines, K. West, S. Krakowka, S. Kennedy, and G. M. Allan. 2004. Porcine circovirus-2 and concurrent infections in the field. Vet. Microbiol. 98159-163. [DOI] [PubMed] [Google Scholar]
- 13.Fenaux, M., P. G. Halbur, M. Gill, T. E. Toth, and X. J. Meng. 2000. Genetic characterization of type 2 porcine circovirus (PCV-2) from pigs with postweaning multisystemic wasting syndrome in different geographic regions of North America and development of a differential PCR-restriction fragment length polymorphism assay to detect and differentiate between infections with PCV-1 and PCV-2. J. Clin. Microbiol. 382494-2503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fuchs, S. Y., V. Adler, T. Buschmann, Z. Yin, X. Wu, S. N. Jones, and Z. Ronai. 1998. JNK targets p53 ubiquitination and degradation in nonstressed cells. Genes Dev. 122658-2663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fuchs, S. Y., V. Adler, M. R. Pincus, and Z. Ronai. 1998. MEKK1/JNK signaling stabilizes and activates p53. Proc. Natl. Acad. Sci. USA 9510541-10546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gao, X., H. Wang, and T. Sairenji. 2004. Inhibition of Epstein-Barr virus (EBV) reactivation by short interfering RNAs targeting p38 mitogen-activated protein kinase or c-myc in EBV-positive epithelial cells. J. Virol. 7811798-11806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garrington, T. P., and G. L. Johnson. 1999. Organization and regulation of mitogen-activated protein kinase signaling pathways. Curr. Opin. Cell Biol. 11211-218. [DOI] [PubMed] [Google Scholar]
- 18.Gupta, S., D. Campbell, B. Derijard, and R. J. Davis. 1995. Transcription factor ATF2 regulation by the NJK signal transduction pathway. Science 267389-393. [DOI] [PubMed] [Google Scholar]
- 19.Harding, J. C. 1996. Post-weaning multisystemic wasting syndrome (PMWS): preliminary epidemiology and clinical presentation. Proc. West Can. Assoc. Swine Pract. 199621. [Google Scholar]
- 20.Hargett, D., T. McLean, and S. T. Bachenheimer. 2005. Herpes simplex virus ICP27 activation of stress kinases JNK and p38. J. Virol. 798348-8360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hirasawa, K., A. Kim, H. S. Han, J. Han, H. S. Jun, and J. W. Yoon. 2003. Effect of p38 mitogen-activated protein kinase on the replication of encephalomyocarditis virus. J. Virol. 775649-5656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holloway, G., and B. S. Coulson. 2006. Rotavirus activates JNK and p38 signaling pathways in intestinal cells, leading to AP-1-driven transcriptional responses and enhanced virus replication. J. Virol. 8010624-10633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang, C., W. Y. Ma, A. Maxiner, Y. Sun, and Z. Dong. 1999. p38 kinase mediates UV-induced phosphorylation of p53 protein at serine 389. J. Biol. Chem. 27412229-12235. [DOI] [PubMed] [Google Scholar]
- 24.Huttunen, P., T. Hyypia, P. Vihinen, L. Nissinen, and J. Heino. 1998. Echovirus 1 infection induces both stress- and growth-activated mitogen-activated protein kinase pathways and regulates the transcription of cellular immediate-early genes. Virology 25085-93. [DOI] [PubMed] [Google Scholar]
- 25.Karaca, G., D. Hargett, T. I. McLean, J. S. Aguilar, P. Ghazal, E. K. Wagner, and S. L. Bachenheimer. 2004. Inhibition of the stress-activated kinase, p38, does not affect the virus transcriptional program of herpes simplex virus type 1. Virology 329142-156. [DOI] [PubMed] [Google Scholar]
- 26.Kujime, K., S. Hashimoto, Y. Gon, K. Shimizu, and T. Horie. 2000. p38 mitogen-activated protein kinase and c-Jun-NH2-terminal kinase regulate RANTES production by influenza virus-infected human bronchial epithelial cells. J. Immunol. 1643222-3228. [DOI] [PubMed] [Google Scholar]
- 27.Kumar, A., S. K. Manna, S. Dhawan, and B. B. Aggarwal. 1998. HIV-Tat protein activates c-Jun N-terminal kinase and activator protein-1. J. Immunol. 161776-781. [PubMed] [Google Scholar]
- 28.Kyriakis, J. M., and J. Avruch. 2001. Mammalian mitogen-activated protein kinase signal transduction pathways activated by stress and inflammation. Physiol. Rev. 81807-869. [DOI] [PubMed] [Google Scholar]
- 29.Kyriakis, J. M., P. Banerjee, E. Nikolakaki, T. Dai, E. A. Rubie, M. F. Ahmad, J. Avruch, and J. R. Woodgett. 1994. The stress-activated protein kinase subfamily of c-Jun kinases. Nature 369156-160. [DOI] [PubMed] [Google Scholar]
- 30.Liu, J., I. Chen, Q. Du, H. Chua, and J. Kwang. 2006. The ORF3 protein of porcine circovirus type 2 is involved in viral pathogenesis in vivo. J. Virol. 805065-5073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu, J., I. Chen, and J. Kwang. 2005. Characterization of a previously unidentified viral protein of porcine circovirus type 2-infected cells and its role in virus-induced apoptosis. J. Virol. 798262-8274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu, J., Y. Zhu, I. Chen, J. Lau, F. He, A. Lau, Z. Wang, A. K. Karuppannan, and J. Kwang. 2007. The ORF3 protein of porcine circovirus type 2 interacts with porcine ubiquitin E3 ligase Pirh2 and facilitates p53 expression in viral infection. J. Virol. 819560-9567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mahe, D., P. Blanchard, C. Truong, C. Arnauld, P. LeCann, R. Cariolet, F. Madec, E. Albina, and A. Jestin. 2000. Differential recognition of ORF2 protein from type 1 and type 2 porcine circoviruses and identification of immunorelevant epitopes. J. Gen. Virol. 811815-1824. [DOI] [PubMed] [Google Scholar]
- 34.Mankertz, A., M. Domingo, J. M. Folch, P. LeCann, A. Jestin, J. Segalés, B. Chmielewicz, J. Plana-Durán, and D. Soike. 2000. Characterization of PCV2 isolates from Spain, Germany, and France. Virus Res. 6665-77. [DOI] [PubMed] [Google Scholar]
- 35.Mankertz, A., J. Mankertz, K. Wolf, and H. J. Buhk. 1998. Identification of a protein essential for replication of porcine circovirus. J. Gen. Virol. 79381-383. [DOI] [PubMed] [Google Scholar]
- 36.McLean, T. I., and S. L. Bachenheimer. 1999. Activation of c-Jun N-terminal kinase by herpes simplex virus type 1 enhances viral replication. J. Virol. 738415-8426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nakatsue, T., I. Katoh, S. Nakamura, Y. Takahashi, Y. Ikawa, and Y. Yoshinaka. 1998. Acute infection of Sindbis virus induces phosphorylation and intracellular translocation of small heat shock protein HSP27 and activation of p38 MAP kinase signalling pathway. Biochem. Biophys. Res. Commun. 25359-64. [DOI] [PubMed] [Google Scholar]
- 38.Nawagitgul, P., I. Morozov, S. R. Bolin, P. A. Harms, S. D. Sorden, and P. S. Paul. 2000. Open reading frame 2 of porcine circovirus type 2 encodes a major capsid protein. J. Gen. Virol. 812281-2287. [DOI] [PubMed] [Google Scholar]
- 39.Onuki, A., K. Abe, K. Togashi, K. Kawashima, A. Taneichi, and H. Tsunemitsu. 1999. Detection of porcine circovirus from lesions of a pig with wasting disease in Japan. J. Vet. Med. Sci. 611119-1123. [DOI] [PubMed] [Google Scholar]
- 40.Padhan, K., R. Minakshi, M. A. Towheed, and S. Jameel. 2008. Severe respiratory syndrome coronavirus 3a protein activates the mitochondrial death pathway through p38 MAP kinase activation. J. Gen. Virol. 891960-1969. [DOI] [PubMed] [Google Scholar]
- 41.Pan, H., J. Xie, F. Ye, and S. J. Gao. 2006. Modulation of Kaposi's sarcoma-associated herpesvirus infection and replication by MEK/ERK, JNK, and p38 multiple mitogen-activated protein kinase pathways during primary infection. J. Virol. 805371-5382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rahaus, M., N. Desloges, and M. H. Wolff. 2004. Replication of varicella-zoster virus is influenced by the levels of JNK/SAPK and p38/MAPK activation. J. Gen. Virol. 853529-3540. [DOI] [PubMed] [Google Scholar]
- 43.Segalés, J., and M. Domingo. 2002. Postweaning multisystemic wasting syndrome (PMWS) in pigs: a review. Vet. Q. 24109-124. [DOI] [PubMed] [Google Scholar]
- 44.Segalés, J., M. Domingo, F. Chianini, N. Majó, J. Domínguez, L. Darwich, and E. Mateu. 2004. Immunosuppression in postweaning multisystemic wasting syndrome affected pigs. Vet. Microbiol. 98151-158. [DOI] [PubMed] [Google Scholar]
- 45.Shapiro, L., K. A. Heidenreich, M. D. Meintzer, and C. A. Dinarello. 1998. Role of p38 mitogen-activated protein kinase in HIV type 1 production in vitro. Proc. Natl. Acad. Sci. USA 957422-7426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Si, X., H. Luo, A. Morgan, J. Zhang, J. Wong, J. Yuan, M. Esfandiarei, G. Gao, C. Cheung, and B. M. McManus. 2005. Stress-activated protein kinases are involved in coxsackievirus B3 viral progeny release. J. Virol. 7913875-13881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sumbayev, V. V., and I. M. Yasinska. 2006. Role of MAP kinase-dependent apoptotic pathway in innate immune responses and viral infection. Scand. J. Immunol. 63391-400. [DOI] [PubMed] [Google Scholar]
- 48.Tibbles, L. A., and J. R. Woodgett. 1999. The stress-activated protein kinase pathways. Cell. Mol. Life Sci. 551230-1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tischer, I., H. Glederblom, W. Vettermann, and M. A. Koch. 1982. A very small porcine virus with circular single-stranded DNA. Nature 29564-66. [DOI] [PubMed] [Google Scholar]
- 50.Tischer, I., W. Mields, D. Wolff, M. Vagt, and W. Griem. 1986. Studies on epidemiology and pathogenicity of porcine circovirus. Arch. Virol. 91271-276. [DOI] [PubMed] [Google Scholar]
- 51.Tischer, I., D. Peters, R. Rasch, and S. Pociuli. 1987. Replication of porcine circovirus: induction by glucosamine and cell cycle dependence. Arch. Virol. 9639-57. [DOI] [PubMed] [Google Scholar]
- 52.Todd, D., P. Biagini, M. Bendinelli, S. Hino, A. Mankertz, S. Mishiro, C. Niel, H. Okamoto, S. Raidal, B. W. Ritchie, and G. C. Teo. 2005. Circoviridae, p. 327-334. In C. M. Fauquet, M. A. Mayo, J. Maniloff, U. Desselberger, and L. A. Ball (ed.), Virus taxonomy. Eighth report of the International Committee for the Taxonomy of Viruses. Elsevier/Academic Press, New York, NY.
- 53.Wada, T., and J. M. Penninger. 2004. Mitogen-activated protein kinases in apoptosis regulation. Oncogene 232838-2849. [DOI] [PubMed] [Google Scholar]
- 54.Walsh, D., and I. Mohr. 2004. Phosphorylation of eIF4E by Mnk-1 enhances HSV-1 translation and replication in quiescent cells. Genes Dev. 18660-672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang, W. H., G. Gégori, R. L. Hullinger, and O. M. Andrisani. 2004. Sustained activation of p38 mitogen-activated protein kinase and c-Jun N-terminal kinase pathways by hepatitis B virus X protein mediates apoptosis via induction of Fas/FasL and tumor necrosis factor (TNF) receptor 1/TNF-α expression. Mol. Cell. Biol. 2410352-10365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wei, L., J. Kwang, J. Wang, L. Shi, B. Yang, Y. Li, and J. Liu. 2008. Porcine circovirus type 2 induces the activation of nuclear factor κB by IκBα degradation. Virology 378177-184. [DOI] [PubMed] [Google Scholar]
- 57.Weitzman, J. B., and M. Yaniv. 1998. Signal transduction pathways and modulation of gene activity. Clin. Chem. Lab. Med. 36535-539. [DOI] [PubMed] [Google Scholar]
- 58.Xie, J., H. Pan, S. Yoo, and S. J. Gao. 2005. Kaposi's sarcoma-associated herpesvirus induction of AP-1 and interleukin 6 during primary infection mediated by multiple mitogen-activated protein kinase pathways. J. Virol. 7915027-15037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yu, S., S. Carpenter, T. Opriessnig, P. G. Halbur, and E. Thacker. 2005. Development of a reverse transcription-PCR assay to detect porcine circovirus type 2 transcription as a measure of replication. J. Virol. Med. 123109-112. [DOI] [PubMed] [Google Scholar]
- 60.Zachos, G., B. Clements, and J. Conner. 1999. Herpes simplex virus type 1 infection stimulates p38/c-Jun N-terminal mitogen-activated protein kinase pathways and activates transcription factor AP-1. J. Biol. Chem. 2745097-5103. [DOI] [PubMed] [Google Scholar]
- 61.Zapata, H. J., M. Nakatsugawa, and J. F. Moffat. 2007. Varicella-zoster virus infection of human fibroblast cells activates the c-Jun N-terminal kinase pathway. J. Virol. 81977-990. [DOI] [PMC free article] [PubMed] [Google Scholar]