Abstract
OBJECTIVE
This study explored the relationship between food insecurity and compensatory maternal feeding practices that may be perceived as buffers against periodic food shortages among urban Black families.
PATIENTS AND METHODS
We interviewed a convenience sample of Black mothers of children ages 2–13 years. Food security status (predictor) was assessed at the household level. Five maternal feeding practices (outcomes) were assessed. Two were based on Birch’s Child Feeding Questionnaire (CFQ): restricting access to certain desired foods and pressuring a child to eat; and 3 were derived from investigators’ clinical experience: the use of high calorie supplements, added sugar in beverages, and perceived appetite stimulants. Anthropometric data were collected from mothers and children.
RESULTS
278 mother-child dyads were analyzed, and 28% of these mothers reported being food insecure. Use of CFQ feeding practices was defined as the top quartile of responses. Use of nutritional supplements, defined as “at least 1–2 times monthly”, was common, ranging from 13%–25%. In logistic regression models adjusted for child age, BMI, and ethnicity and maternal BMI, mothers from food insecure households were significantly more likely to use high calorie supplements (OR, 2.1; 95% CI, 1.1–4.0) and appetite stimulants (OR, 3.2; 95% CI, 1.5–7.1). The odds of using the remaining compensatory feeding practices were elevated among food insecure households, but not reach statistical significance: adding sugars to beverages (OR, 2.1; 95% CI, 0.99–4.4), pressuring a child to eat (OR, 1.8; 95% CI, 0.98–3.2), and restricting access to certain foods (OR, 1.5; 95% CI 0.8–2.7).
CONCLUSIONS
Household food insecurity was independently associated with two of the five maternal compensatory feeding practices studied. Such practices may alter the feeding environment and increase the risk of overweight in children. Longitudinal research is necessary to determine how the relationship between food security and compensatory maternal feeding practices impacts child weight trajectories.
Keywords: Food insecurity, Feeding behavior, Overweight children, African American, Haitian
INTRODUCTION
Over a third of Black children and adolescents in the US are overweight or at risk of overweight.1 The increased prevalence of overweight in this population has led researchers to investigate risk factors that may contribute to obesity. One such factor is food insecurity2–4, which, in 2006, affected 11% of all US households and 15.6% of households with children5, 6. Food insecurity is higher in Black households, where 26.4% of such households with children are food insecure6.
The relationship between food insecurity and overweight is well established among adult women. Population-based studies show an association between obesity and moderate levels of food insecurity among women2–4. Several hypotheses have been offered, including overcompensation for periods when food is scarce, leading to overall increased intake; cycling food and energy intakes during periods of food scarcity and relative abundance, making the body more efficient in using dietary energy and leading to weight gain over time7; and increased consumption of energy dense foods, which are less expensive and may be more plentiful in food-insecure households, leading to an overall increase in energy intake8.
In contrast to adult women, the relationship between food insecurity and overweight among children is uncertain. Some studies report an association between household food insecurity and lower body mass index (BMI) among children9–11, others find that food insecurity is associated with higher BMI12–14 and one study found no association15. These seemingly contradictory findings have motivated researchers to further explore the complex dynamics of food insecurity and identify potential pathways whereby food insecurity impacts childhood weight status.
The aim of this study was to explore the relationship between food insecurity and maternal feeding practices in an ethnically diverse, urban Black population. We focused on this population because they have higher rates of both food insecurity5 and obesity16 than other populations in the US. From the literature17–19 and our own experience, we identified five feeding practices that mothers may view as protective and may have adopted to compensate for the household’s experience of periodic food shortages. These feeding practices have the potential to alter the child feeding environment and contribute to childhood overweight. We hypothesized that among Black households, food insecurity may result in increased use of such compensatory feeding practices.
PATIENTS AND METHODS
Study design and sample
The study was part of larger project to examine differences in maternal feeding practices among Black subpopulations. From November 2003 to September 2005, we conducted a cross-sectional survey of a convenience sample of mothers with children aged 2–13 years (survey available upon request). Our sample included Haitian and African American households. We defined the household as Haitian if the child, the child’s mother, or the child’s maternal grandmother was born in Haiti. We restricted the definition of African American to US-born Black children whose mothers and maternal and paternal grandmothers were also US-born to create a more culturally homogenous group. Subjects were recruited primarily from a pediatric primary care clinic of an urban teaching hospital. To increase the sample size of Haitian families, we extended recruitment to local churches with Haitian congregations. Children with major gastrointestinal anomalies or other medical conditions that interfered with ability to eat were excluded from this study. Families who met eligibility criteria completed a 30-minute face-to-face interview, based on Birch’s Child Feeding Questionnaire (CFQ)18, 20, 21. We added questions regarding food security status, the use of nutritional supplements, and maternal demographics. The interview was conducted in English or Haitian Creole based on the mother’s language preference. Anthropometric data for the mother and child were collected at the time of the interview. The study was approved by the Boston University Medical Center Institutional Review Board.
Measures
Food insecurity
Food insecurity, which is the primary predictor in our analyses, is conceptualized in four domains: 1) uncertainty or worry about food; 2) inadequate quality of food; 3) inadequate quantity of food; and 4) food acquired through socially unacceptable means22. We used the 6-item Short Form of the 12 Month Food Security Questionnaire to classify households as food secure, food insecure without evidence of hunger, and food insecure with hunger23–25. For analytic purposes, we combined the latter two groups to form the food insecure category. Households that affirmed ≤1 responses were classified as food secure and household that affirmed ≥2 responses were classified as food insecure, using our adapted definition.
Compensatory Maternal Feeding Practices
In this study, the outcome variables were five compensatory maternal feeding practices, two defined by the CFQ and three derived from clinical experience. The CFQ19 was designed to explore the relationship between parental control of feeding and the development of children’s eating habits based on responsiveness to hunger satiety cues. Birch expanded the CFQ to include questions about parental restriction to foods and pressuring children to eat to further examine factors that might elicit parents’ use of control in child feeding18, 21. She hypothesized that high levels of parental control may inhibit children’s feeding self-regulation and place children at risk of becoming overweight.
Pressuring a child to eat
This practice was assessed using 4 items from the CFQ, including “My child should always eat all of the food on her plate” and “I have to be especially careful that my child eats enough.” Each item was scored on a 5-point Likert scale. We determined an overall score for this practice (sum of item scores/# of items) and examined its distribution in the sample. We constructed a dichotomous variable, with the highest quartile of scores designated as affirmative for the feeding practice.
Restricting access to certain foods
Evidence of food restriction was examined using 8 items from the CFQ, including “I have to be sure that my child does not eat too many sweets” and “I have to be sure that my child does not eat too many high fat foods.” The items were scored and a dichotomous variable constructed in the manner described above.
The following three feeding practices were identified through the clinical experience of the investigators. For each practice we constructed a dichotomous variable, with the affirmative defined as engaging in the use of any of the products “at least 1–2 times monthly.”
Use of high calorie supplements
High calorie supplements were defined as nutritional supplements that increase caloric intake. Specific preparations included Pediasure, Boost, Carnation Instant Breakfast, and Malta, a beverage commonly given to children in the Caribbean and Latin America.
Use of added-sugar sweeteners
Added-sugar sweeteners referred to the practice of adding sugar to a child’s juice and milk.
Use of appetite stimulants
Appetite stimulants were substances that the mother believed would stimulate the child’s appetite, including Periactin (and its Canadian counterpart, Vimicon), vitamins, and bush teas. Items were included in this category only if the mother used it to stimulate the child’s appetite.
Child and Maternal BMI
Body mass index (BMI) (kg/m2) was calculated for mothers and children based on heights and weights obtained at the time of the interview. Measurements were obtained by trained medical assistants (hospital-based subjects) or research assistants (church-based subjects). For children, we calculated BMI percentiles by age and gender according to the Centers for Disease Control and Prevention guidelines,26 and categorized them as overweight (BMI ≥ 85th%), normal weight (85th % < BMI > 5th%), or underweight (BMI ≤ 5th%). Mothers with BMI ≥ 25 were classified as overweight, and BMI < 25 as normal weight.
A large number of interviews (N= 163) were missing maternal height data, and an additional 53 were missing both maternal height and weight.* We classified women as overweight (N=103) if they weighed ≥164 pounds, which corresponds to a BMI of 25 for the 95th percentile for height (i.e., 68 inches)27. For women who weighed < 164lbs (N= 60) or were missing both height and weight, we imputed their overweight status (see Statistical Methods section). There were no differences in food security status or outcomes between those with and without anthropometric data.
Statistical Methods
For women with missing heights whose weights were < 164lbs or with missing weight (N= 113), we imputed a dichotomous BMI categorization of “Normal” or “Overweight” using the Multiple Imputation (MI) Procedure in SAS for Windows, Version 928. We believe that height and weight values were missing at random, thus meeting requirements for MI. The MI Procedure generated 5 data sets tabulating the pattern of missing BMI categorization. The missing values were approximated using the Bayesian posterior predictive distribution of the parameters from a logistic regression29. The MIANALYZE Procedure was used to adjust standard errors to account for the imputations. In a sensitivity analysis, we found no significant differences in the distribution of maternal BMI among those with and without complete anthropometric data.
To assess potential confounding and effect modification, we examined bivariate associations between food security, selected covariates and maternal feeding practices using χ2 analyses. Logistic regression models were used to further explore associations between compensatory maternal feeding practices (outcomes) and food insecurity (predictor). Covariates were identified from the literature or from bivariate analyses, and included child age, gender, ethnicity, and BMI percentile and maternal age and BMI.
Our model building strategy involved entering covariates in a stepwise progression to determine their impact on food insecurity. After determining the unadjusted odds ratio for food insecurity, we entered child age and gender, then ethnicity, and finally maternal BMI into the model. The final model used the imputed maternal BMI categories. For logistic regression models, odds ratios (OR) and 95% confidence intervals (CI) are reported. For this analysis, the lack of published information concerning maternal feeding practices in our study population prevented us from conducting a priori sample size calculations. Post-hoc calculations revealed an 80% or greater power to detect differences by food security status for all outcome variables.
RESULTS
We interviewed 306 mothers. We excluded 10 interviews because the child’s BMI percentile was missing or less than the 5th percentile. Use of nutritional supplements may have been medically indicated for underweight children. Nine interviews were excluded due to missing child age, precluding our ability to calculate a BMI percentile. An additional seven interviews were excluded due to missing food security data. Finally, we excluded two interviews that were missing data on more than one outcome. A comparison of demographic characteristics (ethnicity, BMI percentile, age, and gender) showed that excluded subjects did not differ significantly from the study sample. Our final analytic sample included 278 mother-child pairs.
Food Security Status
A description of the sample characteristics by food security status is depicted in Table 1. Seventy-nine households (28%) in the study were food insecure. The food secure and insecure groups differed significantly by ethnicity and child’s age. Compared to African American families, Haitian families were significantly more likely to be food insecure. While 50% of the sample was Haitian, they represented 64% of those who were food insecure. Families with older children were also disproportionately more likely to be food insecure. Comprising 14% of the sample, children 11–14 years represented 26% of those who were food insecure. Nearly 60% of children had elevated BMI percentile, however, it was not associated with food security.
Table 1.
Population Characteristics by Food Security Status
| Study population n = 278 n (%) |
Food secure n = 199 n (%) |
Food insecure n = 79 n (%) |
|
|---|---|---|---|
| Ethnicity* | |||
| African American | 138 (50) | 110 (56) | 28 (36) |
| Haitian | 140 (50) | 89 (44) | 51 (64) |
|
| |||
| Child characteristics | |||
| Age* | |||
| 2–5 years | 116 (42) | 87 (44) | 29 (36) |
| 6–10 years | 121 (44) | 91 (46) | 30 (38) |
| 11–14 years | 41 (14) | 21 (10) | 20 (26) |
| Male gender | 119 (44) | 79 (40) | 40 (52) |
| Child BMI | |||
| 5th – 85th% | 115 (42) | 83 (42) | 32 (40) |
| >85th% | 163 (58) | 116 (58) | 47 (60) |
|
| |||
| Maternal characteristics | |||
| Age | |||
| <30 years | 65 (24) | 51 (26) | 14 (18) |
| 30 – 40 years | 120 (44) | 86 (44) | 34 (44) |
| >40 years | 87 (32) | 57 (30) | 30 (38) |
Significant differences in ethnicity and child age between food secure and food insecure groups (P < 0.05)
Compensatory Feeding Practices
CFQ feeding practices (restriction of certain foods and pressuring a child to eat) were defined a priori as the top quartile of responses in our sample. The use of nutritional supplements was common in this population of low-income, urban African American and Haitian families. Routine use of high calorie boosters, added sugars, and appetite stimulants was reported by 25%, 13% and 13% of all households, respectively.
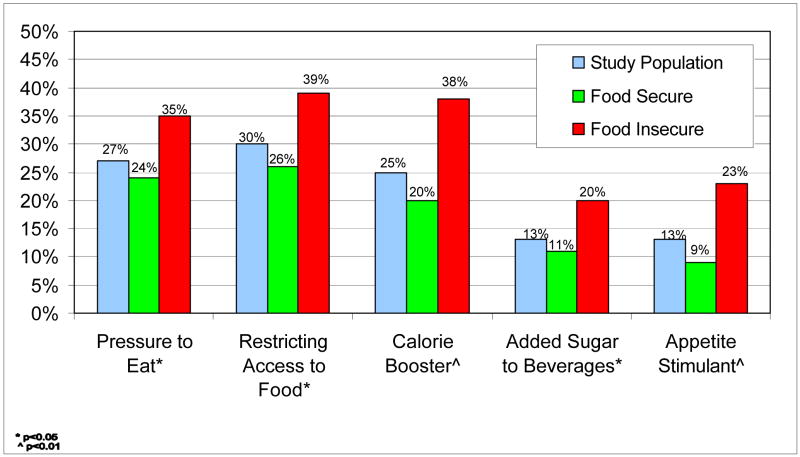
In bivariate analyses, mothers reporting household food insecurity were significantly more likely (P<0.05) to fall within the upper quartile of scores for restriction of certain foods and pressuring a child to eat (see Figure 1). Mothers in food-insecure households were also significantly more likely to give their child high calorie boosters, added sugars and appetite stimulants than mothers in food secure homes. In addition, Haitian mothers were significantly more likely to engage in a variety of compensatory feeding practices (Table 2). However, we found that child gender was neither associated with food security status nor with any of the 5 maternal feeding practices that served as study outcomes, and thus we dropped it from multivariate models. Maternal age was highly correlated with child age, therefore, we elected to retain child age and remove maternal age from multivariate analyses. The remaining covariates were included in final models: child age, child BMI percentile, ethnicity and maternal BMI.
Figure 1.
Unadjusted Proportions of Compensatory Feeding Practices by Food Security Status
Table 2.
Bivariate Analyses by Compensatory Feeding Practice
| Pressure to eat % | Restricting access to food % | Calorie booster % | Appetite stimulant % | Added sugar to beverages % | |
|---|---|---|---|---|---|
| Food security status | |||||
| Secure | 23.6 ‡ |
26.0 ‡ |
20.1 # |
9.0 # |
10.6 ‡ |
| Insecure | 35.4 | 39.2 | 38.0 | 22.8 | 20.3 |
|
| |||||
| Child age | |||||
| 2–5 years | 28.4 | 26.2 | 27.6 | 12.9 | 19.8 |
| 6–10 years | 27.3 | 29.8 | 27.3 | 14.0 | 8.3 ‡ |
| 11–13 years | 22.0 | 39.5 | 12.2 | 9.8 | 9.8 |
|
| |||||
| Child BMI | |||||
| 5th – 85th% | 33.0 | 29.0 | 27.8 | 17.4 | 14.8 |
| ≥85th% | 22.7 | 30.3 | 23.3 | 9.8 | 12.3 |
|
| |||||
| Child gender | |||||
| Female | 24.3 | 30.9 | 21.1 | 12.5 | 12.5 |
| Male | 31.1 | 29.4 | 31.1 | 13.4 | 14.3 |
|
| |||||
| Maternal age | |||||
| <30 years | 27.7 | 25.9 | 32.3 | 15.4 | 15.4 |
| 30–39 years | 24.2 | 22.2 # |
25.8 | 14.2 | 15.8 |
| ≥40 years | 27.6 | 42.2 | 18.4 | 10.3 | 8.0 |
|
| |||||
| Maternal BMI | |||||
| <25 | 12.5 | 50.0 | 37.5 | 25.0 | 12.5 |
| ≥25 | 25.5 | 28.6 | 26.1 | 10.8 | 12.1 |
|
| |||||
| Ethnicity | |||||
| African American | 24.6 | 19.7 # |
7.2 # |
9.4 | 7.2 # |
| Haitian | 29.3 | 39.8 | 42.9 | 16.4 | 19.3 |
p<0.05
p<0.01
Logistic regression analyses
Results from an adjusted logistic regression model are shown in Table 3. In the fully adjusted model, compared to food secure households, mothers in food insecure households were significantly more likely to engage in two of the five hypothesized compensatory feeding practices: use of high calorie boosters (OR, 2.1; 95% CI, 1.1–4.0), and use of a perceived appetite stimulant (OR, 3.2; 95% CI, 1.5–7.1). Two additional practices approached statistical significance: adding sugar to beverages (OR, 2.1; 95% CI, 0.99–4.4) and pressuring a child to eat (OR, 1.8, 95% CI 0.98–3.2). Because ethnicity was highly associated with compensatory feeding practices, we conducted a subsequent analysis that included the interaction between ethnicity and food security, and found that there was no differential effect of food security on any of the outcomes by ethnicity.
DISCUSSION
This study is one of first to quantitatively examine the relationship between food insecurity and specific maternal feeding practices. In this sample of ethnically-diverse, urban Black families, household food insecurity is significantly associated with two of the five compensatory feeding practices that may increase the risk of overweight in a population where prevalence of childhood overweight is high, and the odds are elevated for the other feeding practices studied. These findings contribute to the growing body of research documenting wide-reaching negative impacts of food insecurity on the health and development of America’s children13, 14, 30–35.
This study is one of the first to use CFQ subscales, pressuring a child to eat and restricting access to desired foods, to examine maternal control of feeding when resources are limited and under-nutrition is a perceived risk. Our study findings suggest a possible association between these feeding practices and food insecurity in an urban, low-income Black population. However, previous work by Matheson et al found that food-related parenting attitudes among Mexican-American mothers, using the same two CFQ subscales, did not differ significantly between food-secure and food-insecure households36. The CFQ, which was initially validated in a predominantly middle- to high-income populations18, 20, 21, needs to be examined further to assess its properties among lower-income, more food insecure groups.
The increased use of high calorie supplements and appetite stimulants among food-insecure families was somewhat surprising, given their cost. Local offices of the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) confirmed that they provide such supplements only to children who are clinically defined as underweight, children excluded from these analyses. Mothers may perceive these strategies as protective against under-nutrition in their children, believing that ensuring a child’s ‘good appetite’ and willingness to eat whatever food is available may buffer them during periods of limited food access.
The mechanisms linking food insecurity and maternal feeding practices are uncertain. However, researchers37–39 have identified a common pattern of managing food resources in response to increasing family economic stress. Mothers, in particular, are likely to sacrifice food quality and variety to preserve children’s usual levels of food intake, which tend to be disrupted only in dire situations. Hamelin et al describes the phenomenon of worrying about having enough food in the future as a key feature of food insecurity40. Worry about food sufficiency may manifest at the household level through modifications of eating pattern and ritual – both during periods of food adequacy and shortage. This model suggests that the experience of food insecurity may lead to feeding practices that mothers view as protective.
This study has several limitations. First, we cannot directly link the compensatory feeding practices identified in this study to childhood overweight. Although the prevalence of these feeding practices and childhood overweight was high in our sample, the study was not designed to evaluate causality. Second, we used a convenience sample that introduces the possibility of selection bias. While these results may not be generalizable to other populations, the sampling approach should not influence internal associations. Third, there were a large number of missing maternal weight and height data. We addressed this issue by using multiple imputation methods to compare findings with and without complete data. Overall, results were stable between the two analyses, but this study needs to be replicated using complete maternal anthropometric data.
CONCLUSIONS
In this study, we offer a model of household food insecurity that provides a rationale for compensatory maternal feeding practices that may promote childhood overweight. Our study findings suggest that food insecurity may alter the feeding environment and highlight the importance of including questions about food security, nutritional supplements, and perceived appetite stimulants as a routine part of dietary history. A positive response to questions about use of nutritional supplements can serve as a prompt to pediatric providers to further probe household food adequacy and consistent access to quality food, and link families to community-based food programs as needed. Further research is needed to replicate study findings in a larger, more ethnically diverse sample. In addition, the relationship between food insecurity and childhood overweight is not well established and remains a topic of investigation. Following children longitudinally could provide insight on how food security status might alter maternal feeding practices and child weight trajectories.
Acknowledgments
Funding: American Nurses Foundation, Gloria Smith Scholar (Feinberg); NIH T32 Grant (HP1001414) (Kavanagh); HRSA 2-D14-HP-00055 (Prudent)
This study was supported in part by the American Nurses Foundation, Gloria Smith Scholar (Dr.Feinberg), NIH T32 Grant (HP1001414) (Dr. Kavanagh), and HRSA 2-D14-HP-00055 (Dr. Prudent). We thank Marie Foureau, MD, for project coordination and Mario Malivert MD, MPH, for database design and management. We are grateful to Milton Kotelchuck, PhD, MPH and Howard Bauchner, MD for their thoughtful review of the manuscript.
Abbreviations
- BMI
body mass index
- CFQ
Child Feeding Questionnaire
- OR
odds ratio
- CI
confidence interval
Footnotes
Financial Disclosure: None
Conflict of Interest: None
Missing maternal anthropometric data is due to study procedures, not maternal reasons Maternal weight was not collected during the study pilot phase (N= 29 interviews). Maternal height was not collected until midway through the study.
Contributor Information
Emily Feinberg, Assistant Professor, Department of Maternal & Child Health, Boston University School of Public Health, Boston, MA, Department of Pediatrics, Boston University School of Medicine/Boston Medical Center, Boston, MA.
Patricia L. Kavanagh, Fellow, General Pediatrics, Department of Pediatrics, Boston University School of Medicine/Boston Medical Center, Boston, MA.
Robin L. Young, Doctoral Student, Department of Biostatistics, Boston University School of Public Health, Boston, MA.
Nicole Prudent, Department of Pediatrics, Boston University School of Medicine/Boston Medical Center, Boston, MA, Haitian Health Institute, Boston Medical Center.
References
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of Overweight and Obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Adams EJ, Grummer-Strawn L, Chavez G. Food insecurity is associated with increased risk of obesity in California women. J Nutr. 2003;133:1070–1074. doi: 10.1093/jn/133.4.1070. [DOI] [PubMed] [Google Scholar]
- 3.Townsend MS, Peerson J, Love B, Achterberg C, Murphy SP. Food insecurity is positively related to overweight in women. J Nutr. 2001;131:1738–1745. doi: 10.1093/jn/131.6.1738. [DOI] [PubMed] [Google Scholar]
- 4.Frongillo EA, Olson CM, Rauschenbach BS, Kendall A. Nutritional consequences of food insecurity in a rural New York state county. Discussion Paper no. 1120–97. Madison, WI: Institute for Research on Poverty, University of Wisconsin; 1997. [Google Scholar]
- 5.Nord M, Hopwood H. Recent Advances Provide Improved Tools for Measuring Children’s Food Security. J Nutr. 2007;137(3):533–536. doi: 10.1093/jn/137.3.533. [DOI] [PubMed] [Google Scholar]
- 6.Nord M, Andrews M, Carlson S. Household Food Security in the United States, 2006. US Dept of Agriculture, Econ Res Serv. 2007 November;:ERR-49. [Google Scholar]
- 7.Wing R. Weight cycling in humans: a review of the literature. Ann Behav Med. 1992;14:113–119. [Google Scholar]
- 8.Drewnowski A. Fat and sugar: an economic analysis. J Nutr. 2003;133:838S–840S. doi: 10.1093/jn/133.3.838S. [DOI] [PubMed] [Google Scholar]
- 9.Matheson DM, Varady J, Varady A, Killen JD. Household food security and nutritional status of Hispanic children in the fifth grade. Am J Clin Nutr. 2002;76:210–217. doi: 10.1093/ajcn/76.1.210. [DOI] [PubMed] [Google Scholar]
- 10.Rose D, Bodor N. Household food insecurity and overweight status in young school children: Results from the Early Childhood Longitudinal Study. Pediatrics. 2006;117(2):464–473. doi: 10.1542/peds.2005-0582. [DOI] [PubMed] [Google Scholar]
- 11.Jones SJ, Jahns L, Laraia BA, Haughton B. Lower risk of overweight in school-aged food insecure girls who participate in food assistance. Arch Pediatr Adolesc Med. 2003;157:780–784. doi: 10.1001/archpedi.157.8.780. [DOI] [PubMed] [Google Scholar]
- 12.Bronte-Tinkew J, Zaslow M, Capps R, Horowitz A, McNamara M. Food insecurity works through depression, parenting, and infant feeding to influence overweight and health in toddlers. J Nutr. 2007;137:2160–2165. doi: 10.1093/jn/137.9.2160. [DOI] [PubMed] [Google Scholar]
- 13.Casey PH, Szeto K, Lensing S, Bogle M, Weber J. Children in food-insufficient, low-income families: Prevalence, health, and nutrition status. Arch Pediatr Adolesc Med. 2001;155(4):508–514. doi: 10.1001/archpedi.155.4.508. [DOI] [PubMed] [Google Scholar]
- 14.Jyoti DF, Frongillo EA, Jones SJ. Food insecurity affects school children’s academic performance, weight gain and social skills. J Nutr. 2005;135:2831–2839. doi: 10.1093/jn/135.12.2831. [DOI] [PubMed] [Google Scholar]
- 15.Alaimo K, Olson CM, Frongillo EA., Jr Low Family Income and Food Insufficiency in Relation to Overweight in US Children: Is There a Paradox? Arch Pediatr Adolesc Med. 2001;155(10):1161–1167. doi: 10.1001/archpedi.155.10.1161. [DOI] [PubMed] [Google Scholar]
- 16.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of Overweight and Obesity Among US Children, Adolescents, and Adults, 1999–2002. JAMA. 2004;291(23):2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 17.Birch LL, Fisher JO. Development of Eating Behaviors Among Children and Adolescents. Pediatrics. 1998;101(3):539–549. [PubMed] [Google Scholar]
- 18.Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire: a measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36:201–210. doi: 10.1006/appe.2001.0398. [DOI] [PubMed] [Google Scholar]
- 19.Costanzo PR, Woody EZ. Domain-specific parenting styles and their impact on the child’s development of particular deviance: the example of obesity proneness. J Clin Social Psych. 1985;3:425–445. [Google Scholar]
- 20.Birch LL, Fisher JO. Mothers’ child-feeding practices influence daughters’ eating and weight. Am J Clin Nutr. 2000;71(5):1054–1061. doi: 10.1093/ajcn/71.5.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fisher JO, Birch LL. Restricting access to palatable foods affects children’s behavioral response, food selection, and intake. Am J Clin Nutr. 1999;69(6):1264–1272. doi: 10.1093/ajcn/69.6.1264. [DOI] [PubMed] [Google Scholar]
- 22.Coates J. Experience and Expression of Food Insecurity Across Cultures:Practical Implications for Valid Measurement. Washington, D.C: Food and Nutrition Technical Assistance Project, Academy for Educational Development; 2004. [Google Scholar]
- 23.Blumberg S, Bialostosky K, Hamilton W, Briefel R. The effectiveness of a short form of the Household Food Security Scale. AJPH. 1999;89(8):1231–1234. doi: 10.2105/ajph.89.8.1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamilton W, Cook J, Thompson W, et al. Household food security in the United States in 1995: A technical report. Alexandria, VA: Prepared for the U.S. Department of Agriculture Food and Nutrition Service; 1997. [Google Scholar]
- 25.Hamilton W, Cook J, Thompson W, et al. Household food security in the United States in 1995: Summary report of the Food Security Measurement Project. Alexandria, VA: Prepared for the U.S. Department of Agriculture Food and Nutrition Service; 1997. [Google Scholar]
- 26.Centers for Disease Control and Prevention, National Center for Health Statistics. [Accessed October 2006];CDC growth charts: United States. 2000 May 30; http://www.cdc.gov/growthcharts.
- 27.McDowell MA, Fryar CD, Hirsch RCLO. Advance data from Vital and Health Statistics, no. 361. Hyattsville, MD: National Center for Health Statistics; 2005. Anthropometric reference data for children and adults: US population, 1999–2002. [Google Scholar]
- 28.SAS for Windows, Version 9 computer program. Cary, NC: SAS Institute; [Google Scholar]
- 29.Rubin DB, Schenker N. Multiple Imputation for Interval Estimation From Simple Random Samples With Ignorable Nonresponse. Journal of the American Statistical Association. 1986;81(394):366–374. [Google Scholar]
- 30.Alaimo K, Olson CM, Frongillo EA., Jr Food Insufficiency and American School-Aged Children’s Cognitive, Academic, and Psychosocial Development. Pediatrics. 2001;108(1):44–53. [PubMed] [Google Scholar]
- 31.Casey PH, Szeto KL, Robbins JM, et al. Child Health-Related Quality of Life and Household Food Security. Arch Pediatr Adolesc Med. 2005;159(1):51–56. doi: 10.1001/archpedi.159.1.51. [DOI] [PubMed] [Google Scholar]
- 32.Connell CL, Lofton KL, Yadrick K, Rehner TA. Children’s Experiences of Food Insecurity Can Assist in Understanding Its Effect on Their Well-Being. J Nutr. 2005;135(7):1683–1690. doi: 10.1093/jn/135.7.1683. [DOI] [PubMed] [Google Scholar]
- 33.Cook JT, Frank DA, Levenson SM, et al. Child Food Insecurity Increases Risks Posed by Household Food Insecurity to Young Children’s Health. J Nutr. 2006;136(4):1073–1076. doi: 10.1093/jn/136.4.1073. [DOI] [PubMed] [Google Scholar]
- 34.Whitaker R, Phillips S, Orzol S. Food insecurity and risk of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics. 2006;118(3):e859–e868. doi: 10.1542/peds.2006-0239. [DOI] [PubMed] [Google Scholar]
- 35.Cook JT, Frank DA. Food Security, Poverty and Human Development in the United States. Ann NY Acad Sci. 2007 doi: 10.1196/annals.1425.001. http://www.annalsnyas.org/cgi/rapidpdf/annals.1425.001v2. [DOI] [PubMed]
- 36.Matheson DM, Robinson T, Varady A, Killen JD. Do Mexican-American mothers’ food-related parenting practices influence their childrens’ weight and dietary intake? J Am Diet Assoc. 2006;106:1861–1865. doi: 10.1016/j.jada.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 37.Coates J, Frongillo EA, Rogers BL, Webb P, Wilde PE, Houser R. Commonalities in the Experience of Household Food Insecurity across Cultures: What Are Measures Missing? J Nutr. 2006;136(5):1438S–1448. doi: 10.1093/jn/136.5.1438S. [DOI] [PubMed] [Google Scholar]
- 38.Radimer KL, Olson CM, Campbell CC. Development of indicators to assess hunger. J Nutr. 1990;120:1544–1548. doi: 10.1093/jn/120.suppl_11.1544. [DOI] [PubMed] [Google Scholar]
- 39.Radimer KL, Olson CM, Greene JC, Campbell CC, Habicht J-P. Understanding hunger and developing indicators to assess it in women and children. J Nutr Educ. 1992;24:36S–45S. [Google Scholar]
- 40.Hamelin A-M, Beaudry M, Habicht J-P. Food insecurity: Consequences for the household and broader social implications. J Nutr. 1999;129:525S–528S. doi: 10.1093/jn/129.2.525S. [DOI] [PubMed] [Google Scholar]