Abstract
Recombinant tissue-type plasminogen activator (tPA) is the fibrinolytic drug of choice to treat stroke patients. However, a growing body of evidence indicates that besides its beneficial thrombolytic role, tPA can also have a deleterious effect on the ischaemic brain. Although ageing influences stroke incidence, complications and outcome, age-dependent relationships between endogenous tPA and stroke injuries have not been investigated yet. Here, we report that ageing is associated with a selective lowering of brain tPA expression in the murine brain. Moreover, our results show that albumin D site-binding protein (DBP) as a key age-associated regulator of the neuronal transcription of tPA. Additionally, inhibition of DBP-mediated tPA expression confers in vitro neuroprotection. Accordingly, reduced levels of tPA in old mice are associated with smaller excitotoxic/ischaemic injuries and protection of the permeability of the neurovascular unit during cerebral ischaemia. Likewise, we provide neuroradiological evidence indicating the existence of an inverse relationship between age and the volume of the ischaemic lesion in patients with acute ischaemic stroke. Together, these results indicate that the relationship among DBP, tPA and ageing play an important role in the outcome of cerebral ischaemia.
Keywords: ageing, tissue-type plasminogen activator, neurovascular unit, albumin D site-binding protein, stroke
Introduction
One of the earliest pathological processes leading to ischaemic stroke is the aggregation of platelets with local activation of coagulation factors and the generation of a fibrin-rich clot that interrupts the blood supply to the brain. Under physiological conditions fibrinolysis is the resultant of the interaction between plasminogen/plasmin and plasminogen activators (tissue-type plasminogen activator—tPA—and urokinase) and its inhibitors. Accordingly, the administration of recombinant plasminogen activators for the treatment of thrombotic or embolic conditions has been intensively studied. This has led to the approval of recombinant tPA (Actilyse®) for the treatment of patients with acute ischaemic stroke. Unfortunately, besides its beneficial thrombolytic role (NINDS, 1995), tPA also has a deleterious pro-haemorrhagic effect and a short therapeutic window, which has resulted in the regrettable fact that only 3%–8.5% of acute ischaemic stroke are currently treated with tPA (Bambauer et al., 2006).
tPA is not just a circulating protease. Indeed, tPA is expressed not only in endothelial cells but also in neurons and glia, where it has been shown to play a role in the regulation of the permeability of the neurovascular unit (Montaner et al., 2003; Yepes et al., 2003) and to have a pro-neurotoxic effect (Benchenane et al., 2004; Samson and Medcalf, 2006; Yepes et al., 2009). Accordingly, an increase in tPA activity in the brain parenchyma has been associated with exacerbation of brain injury by promoting extracellular matrix degradation (McGuire and Seeds, 1990), microglia activation through annexin II (Siao and Tsirka, 2002), excitotoxicity by interaction with NMDA receptors (Nicole et al., 2001; Fernandez-Monreal et al., 2004; Pawlak et al., 2005) and neuronal and endothelial apoptosis (Liu et al., 2004). Likewise, the interaction between tPA and the low-density lipoprotein receptor-related protein (LRP1) results in detachment of astrocytic end-feet processes from the basement membrane with increase in the permeability of the neurovascular unit (Yepes et al., 2003; Cheng et al., 2006), NF-κB activation, Akt phosphorylation (An et al., 2008) and a cleavage of PDGF-cc (Su et al., 2008). Importantly, experimental evidence indicates that tPA can cross from the intravascular space into the ischaemic tissue, raising the possibility that recombinant tPA, given for the treatment of acute ischaemic stroke, may also permeate the ischaemic tissue to promote brain injury (Benchenane et al., 2005a).
Paradoxically, studies are essentially conducted in young healthy animals, while the incidence of ischaemic stroke increases with age and the prevalence and severity of some of its complications like increased blood–brain barrier permeability and cerebral oedema, seems to be higher in younger patients (Jaramillo et al., 2006). Despite these clinical observations, the effect of age is seldom studied in experimental models or considered in clinical trials. Similarly, while controlling the endogenous availability of tPA could be of therapeutic interest, it's transcriptional regulation of tPA in nerve cells remains poorly investigated (Shin et al., 2004; Lee et al., 2008).
Here, we demonstrate that ageing is associated with a decrease in the expression and activity of tPA in the brain parenchyma, and that this results in a decrease in the volume of the ischaemic lesion and protection of the barrier function of the neurovascular unit during cerebral ischaemia. Importantly, our data indicates that the basic region/leucine zipper protein, albumin D site-binding protein (DBP) is a key regulator of the neuronal transcription of tPA.
Methods
Sample collection
C57BL6/J mice (Charles River; L’Arbresle, France) were housed in a temperature controlled room with food and water ad libitum. Experiments were performed in accordance with French (Act no. 87–848; Ministère de l’Agriculture et de la Forêt) and European Communities Council (Directives of November 24, 1986, 86/609/EEC) guidelines. For transcription/expression analyses, at selected ages, animals were anaesthetized (between 10:00 and 11:00 AM) by chloral hydrate (i.p. 150 mg/kg) and transcardially perfused with ice-cold 0.9% NaCl with 5% heparin. At the initiation of the perfusion, a blood sample was collected. The striatum, cortex, cerebellum, hippocampus and spinal cord were harvested and separated into two halves for biochemical and mRNA analyses.
Protein and RNA extractions
Tissues were dissociated in ice-cold TNT buffer (50 mM Tris–HCl pH 7.4; 150 mM NaCl; 0.5% Triton X-100). After centrifugation (10 000g, 4°C, 15 min), protein quantification was performed on supernatants through the BCA method (Pierce, France). RNAs were extracted by using Nucleospin RNA II columns (Macherey-Nagel, France).
Enzymatic assay
A fluorogenic substrate (Spectrozyme XF444, 5 µmol/l, American Diagnostica, USA) was incubated with proteins (100 µg in 50 µl) or plasma (50 µl). Measurements were performed at 37°C over 2 h using a multiplate reader (Chameleon, Hidex, Finland).
ELISA
ELISA for total tPA was performed on 200 μg of protein extracts, according to the manufacturer's instructions (Molecular Innovation®, USA).
Quantitative real-time RT–PCR
Total RNAs were reverse-transcribed using the Promega RT-system (Promega, Charbonnières, France). Two primers were designed for each gene using the Beacon Designer software (BioRad, Marnes-la-Coquette, France). tPA forward primer (F): ctccgacccatgctcagaa; and reverse primer (R): ttgtaccaggccgctgttg; DBP (F): ccgctgatctcgccctgtc; and (R): cacctggactttccttgccttc; GAPDH (F): ccaatgtgtccgtcgtggatc; and (R): gccctcagatgcctgcttca; NR1 (F): ctctagccaggtctacgctatcc; and (R): gacggggattctgtagaagcca. Assays using the IQ-SYBR Green Supermix and Hot Goldstar were run in triplicate on the iCycler iQ real-time PCR detection system (BioRad, Marnes-la-Coquette, France). Gene expression levels were computed with respect to glyceraldehyde-3-phosphate dehydrogenase (GAPDH) mRNA expression levels for in vivo experiments and with NMDA receptor subunit 1 (NR1) for neuronal cultures using the formula: relative mRNA expression = 2–(Ct gene of interest – Ct housekeeping gene).
Microarray experiments
For each age (4 and 21 months), samples were prepared by pooling an equal amount of RNA from three individuals. Five micrograms of total RNAs were reverse-transcribed with 7.5 µM random hexamers (GE Healthcare), 75 µM aminoallyl-dUTP (Sigma-Aldrich) and 100 U Rtases Reverse-iT Blend (Thermo-Scientific) overnight at 37°C. Aminoallyl cDNAs were then labelled with Cy5 or Cy3 mono-Reactive Dye (GE Healthcare) according to the manufacturer's instructions. Labelled cDNAs were then purified on Qiaquick PCR purification kit (Qiagen) and hybridized to the RNG-MRC_MM25k_EVRY microarrays (Le Brigand et al., 2006) (http://www.microarray.fr:8080/merge/index). Each pool was hybridized in duplicate dye-swap independent experiments.
After hybridization, median signal and background intensities were extracted using Genepix 4.1 software (Axon Instruments). The level of expression of each gene has first been evaluated by calculating the mean ratio ‘signal/background’ for each corresponding spot from the two dye-swap experiments. Genes were considered to be expressed only if their mean ratio was ≥1.2. These filtered data were then submitted to VARAN (http://www.bionet.espci.fr/) for normalization by lowess fit and differential expression analysis (Golfier et al., 2004). Normalized log2 ratio 21/4 months were then used for further statistical analysis by SAM software (Tusher et al., 2001) and t-test with a P-value equal to 5% using TIGR Multiexperiment Viewer (TM4:MeV, http://www.tm4.org/mev.html). The final list (http://www.ncbi.nlm.nih.gov/geo/, accession number GSE9004, Supplementary Table 1) of differentially expressed genes was established by comparing the results obtained with the three methods.
Immunohistochemistry
Mice were anesthetized with 0.1 g/ml chloral hydrate (150 mg/kg) and perfused transcardially with cold heparinized NaCl 0.9% followed by 2% paraformaldehyde, 0.2% picric acid in 0.1 M sodium phosphate buffer pH 7.4. Brains were removed, post-fixed overnight at 4°C in the same fixative, rinsed in veronal buffer containing 20% sucrose and frozen in Tissue-Tek (Miles Scientific, Naperville, IL). Coronal sections of 10 µm were incubated overnight at room temperature with a primary antibody directed against either tPA (rabbit anti-tPA, 1:5000; from Pr. Carmeliet, University of Leuven, Belgium), DBP (rabbit anti-DBP, 1:600; Abcam), Microtubule-associated protein 2 (MAP-2; chicken anti-MAP-2, 1:6000; Abcam) or Glial Fibrillary Acidic Protein (GFAP; rabbit anti-GFAP, 1:1000; Sigma). Detection was performed using the corresponding fluorescein isothiocyanate (FITC, green) or tetramethyl rhodamine isothiocyanate (TRITC, red)—conjugated donkey anti IgG secondary antibody (1:300, Jackson Immunoresearch, West Grove, USA). Before being cover slipped with antifed medium containing DAPI, sections were incubated for 5 min with a solution of Sudan Black B (Sigma-Aldrich) in 20% alcohol to reduce the autofluorescence observed in oldest mice (Schnell et al., 1999). Sections were examined with a Leica DM6000 microscope. Images were digitally captured using a coolsnap camera and visualized with Metavue software. DAPI positive cells were quantified by the application software Meta Imaging Series 6.3. Values are the means of 10 serial sections for each animal (n = 3).
Decoy oligonucleotide and shRNA assays
Neuronal cortical cultures were prepared from foetal mice (E15–E16) as described earlier (Nicole et al., 2001). Decoy double-stranded oligonucleotides mimicking the DBP DNA binding sequence within the mouse tPA promoter (Eurogentec, France) or short hairpin RNA interference targeting the expression of DBP (Sigma, France) were transiently transfected in murine cortical neurons (DIV 8–10) with the lipofectamin 2000 reagent (InVitrogen, France) with modifications of the protocol provided by the manufacturer. The sequences of the decoy oligonucleotides used were: (F) primer: aacactataatgtaaacag and (R) primer: ctgtttacattatagtgtt. shRNA sequences used were: for DBP 86023 (shDBP1): ccggcggaggtacaagaacaatgaactcgagttcattgttcttgtacctccgtttttg; for DBP 86024 (shDBP2): ccggccggaggtacaagaacaatgactcgagtcattgttcttgtacctccggtttttg. Forty-eight hours post-transfection, cells were either subjected to NMDA-mediated neuronal death as described below or assessed for tPA, DBP, NMDA receptor subunits expression and tPA proteolytic activity (Q-RT–PCR, spectrozyme and/or zymography assays).
Zymography assays
Zymography was performed by adding plasminogen (4.5 µg/ml) and casein (5 mg) to a 12.6% SDS–PAGE. Electrophoresis was performed at 4°C. Gels were washed with Triton X-100 (2.5%) and incubated at 37°C. Caseinolytic bands were visualized after Coomassie staining.
Neuronal toxicity assay
Slowly triggered excitotoxicity was induced at 37°C by a 24 h exposure to 10 μM NMDA in DMEM supplemented with glycine (10 μM). Neuronal death was assessed by phase-contrast microscopy and quantified by measurement of lactate dehydrogenase (LDH) release by damaged cells into the bathing medium. The LDH level corresponding to near-complete neuronal death was determined in sister wells exposed to 200 μM NMDA for 24 h in DMEM supplemented with glycine. Background LDH levels were determined in sister wells subjected to sham wash and subtracted from experimental values to yield the signal specific to experimentally induced injury.
Animal model of cerebral ischaemia
All procedures were approved by the Emory University Institutional Animal Care and Use and classically randomized. tPA deficient (tPA–/–) mice and their C57BL/6J wild-type (WT) controls (2- to 24-month-old) were anaesthetized with 4% chloral hydrate (400 mg/kg IP). The rectal temperature was controlled at 37°C with a homeothermic blanket. Cerebral perfusion (CP) in the middle cerebral artery territory was monitored throughout the surgical procedure with a laser Doppler (Perimed Inc., North Royalton, OH, USA) and only animals with a >80% decrease in CP were included. The middle cerebral artery was exposed and distally occluded (MCAO) with a 10-0 suture (Wang et al., 1998; Yepes et al., 2003). Immediately after MCAO, a subgroup was placed on a stereotactic frame and intracortically injected (unilateral injection) over 5 min with 2 μl murine tPA (1 μM; Molecular Innovations Inc., Royal Oak, Michigan, USA) at bregma: –1 mm, mediolateral: 3 mm and dorsoventral: 3 mm (Paxinos and Franklin's stereotaxic atlas). The dose of tPA injected was chosen based on our previous observations (Yepes et al., 2003). None of the operated animals died. Forty-eight hours after MCAO, animals were sacrificed by anaesthetic overdose. To measure the volume of the ischaemic lesion brains were harvested, placed in a matrix and cut onto eight 1-mm sections, followed by incubation in 2% 2,3,5-triphenyltetrazolium chloride (TTC) in saline for 30 min at 37°C and fixation with 4% formalin in PBS (Wang et al., 1998). With this procedure, the necrotic infarct area remains unstained. The infarct volume was determined with the NIH-image analyser system as the sum of the unstained areas of the sections multiplied by their thickness according to the equation: Vischemic lesion = ∑(Areas of ischaemic lesion) × distance between sections. The rostral and caudal limits for the integration were set at the frontal and occipital poles of the cortex. This method has been validated previously, demonstrating an excellent reproducibility of the volumetric assessment of the ischaemic lesion (Osborne et al., 1987). To study the permeability of the blood–brain barrier, a subgroup of animals was intravenously treated with 2% Evans blue (Sigma-Aldrich) in saline immediately after MCAO, followed 6 h later by transcardiac perfusion. Brains were removed, divided into ipsilateral and contralateral hemispheres, weighed, homogenized in N,N-dimethylformamide (400 μl) and centrifuged (21 000g, 30 min). Evans blue was quantified in supernatants from the absorbance at 620 nm minus the background calculated from the baseline absorbance between 500 and 740 nm, and divided by the wet weight of each hemisphere. Each observation was repeated six times.
Study population and clinical protocol
A total of 93 patients with an acute ischaemic stroke admitted to the Emergency Department of a University Hospital within 3 h of symptom onset (Vall d'Hebron, Barcelona, Spain) were included (Supplementary Table 2). All had a MCAO documented by transcranial Doppler (TCD). No important disease affecting the functional status of the patients was allowed in this cohort, since only those with a modified historical Rankin of 0 or 1 were included (this excluded dementia or any other important disease that affected daily life of those patients). Also patients with infections or any other immunological or tumoural disease at the moment of suffering the index stroke were excluded. Serial magnetic resonance imaging (MRI) exams were performed to study infarct volume evolution. A baseline MRI including diffusion- (DWI) and perfusion-weighted (PWI) sequences was performed within the first 3 h after stroke onset. A detailed history of vascular risk factors was obtained from each patient and a clinical examination performed on admission and serially until discharge. Stroke severity and neurological outcome were assessed using the National Institutes of Health Stroke Scale (NIHSS). TCD assessments were performed by an experienced neurologist using a Multi-Dop® X4 (DWL Elektroniche Systeme GmbH, Sipplingen, Germany) device, to assess location of MCAO. The study was approved by the Ethics Committee and conducted in accordance with the Declaration of Helsinki. All patients or relatives gave informed consent.
MRI protocol and volumetric assessment of lesion size
All MRI studies were performed as previously described (Rosell et al., 2005) with a 1.5 T whole-body imaging system with 24-mT/m gradient strength, 300 ms rise time and an echo-planar-capable receiver equipped with a gradient overdrive (Magnetom Vision Plus, Siemens Medical Systems, Germany). The perimeter of the area of abnormal high-signal intensity was traced on each DWI and TTP map. Measured areas were multiplied by the slice distance to obtain the total lesion volumes for both the DWI and TTP maps (cubic centimeters, cc).
Statistical analyses
For tPA activity/expression studies and DBP expression studies, data were expressed as mean ± SEM and statistical analyses consisted in a Kruskal–Wallis test, followed by a Mann–Whitney test for comparisons between groups. For human data, descriptive and frequency statistical analysis were obtained and comparisons were made by use of the SPSS statistical package, version 12.0. Statistical significance for intergroup age differences was assessed by Mann–Whitney U-test (two groups) and Kruskal–Wallis test (more than two groups). Correlations between numerical variables were assessed by Spearman's correlation coefficient. Receiving operating characteristic (ROC) curves were conducted to select the age with better sensitivity and specificity to differentiate large and small MRI lesions (above the median value). A multiple logistic regression analysis was performed to determine independent predictors of DWI and PWI extend. A P < 0.05 was considered statistically significant. For the animal studies of cerebral ischaemia the Wilcoxon two sample rank sum test was used and a P < 0.05 was considered as significant.
Results
Age-related decline in tPA cerebral expression and activity in mice
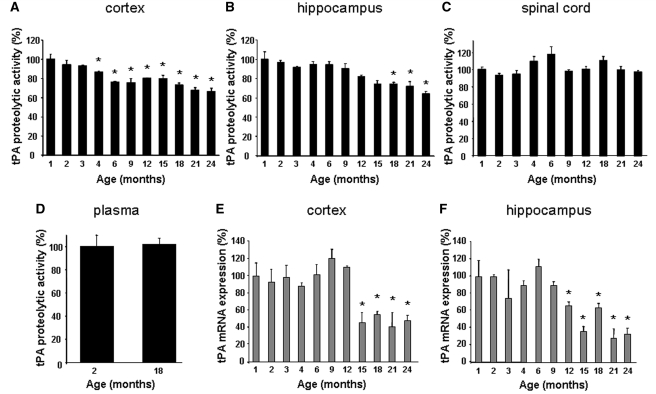
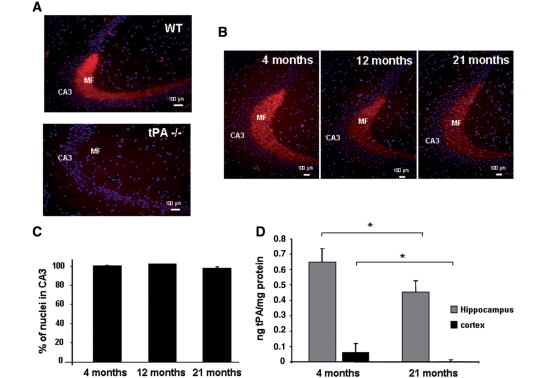
We first investigated the effects of ageing on tPA's catalytic activity and transcription in WT female mice aged 1–24 months. With ageing, there was a significant decrease in the proteolytic activity of tPA in the cerebral cortex, hippocampus (Fig. 1A and B), striatum and cerebellum (Supplementary Fig. 1A and B; P < 0.001). In contrast, no age-associated changes were observed in the spinal cord (Fig. 1C) and plasma (Fig. 1D and concordant ELISA assays for tPA antigen levels, not shown). Similarly, tPA transcription was reduced with ageing in the cortex (P < 0.001; Fig. 1E), hippocampus (P < 0.001; Fig. 1F), striatum (P < 0.005; Supplementary Fig. 1C) and cerebellum (P < 0.001; Supplementary Fig. 1D), but not in the spinal cord (Supplementary Fig. 2A). Immunohistological analyses (see specific labelling in WT versus tPA-deficient mice, Fig. 2A) demonstrate a reduction of ∼50% in tPA immunoreactivity between 4 and 21 months of age in mossy fibres (Fig. 2B) with no change in the number of DAPI-labelled cells (Fig. 2C) or NeuN-labelled cells (not shown). ELISA for total tPA in the cortex and hippocampus confirmed the age-dependent decrease in tPA levels (Fig. 2D). Interestingly, age-associated reductions in tPA activity/transcription were also observed in male cortices and hippocampi (Supplementary Fig. 3A and B).
Figure 1.
Effect of ageing on tPA proteolytic activity and transcription in the CNS and the plasma. tPA proteolytic activity was normalized to mean values of 1-month-old C57BL6/J female mice in the perfused cortex (A), hippocampus (B) and spinal cord (C) (n = 4 per group). (D) Similar experiments performed on plasma samples from mice aged 2 and 18 months (n = 6 per group). Levels of tPA transcription analysed by Q-RT–PCR were normalized to mean value of 1 month old C57BL6/J female mice in the perfused cortex (E) and hippocampus (F) (n = 4 per group). *Significantly different from 1-month-old mice, P < 0.05.
Figure 2.
Effect of ageing on tPA protein levels in the CNS. Control immunostainings for tPA (red) in WT and tPA-deficient mice (A; n = 3). Immunostainings for tPA (red) on perfused brain sections of 4-, 12- and 21-month-old WT mice (B) and corresponding nuclei counting using DAPI (blue) counterstaining (C; n = 3 per group). Scale bars, 100 µm. ELISA for total tPA performed on perfused brain extracts of WT mice at 4- and 21-months-old (cortex and hippocampus) (D; n = 4). *P < 0.05.
DBP as a candidate transcriptional regulator of tPA cerebral expression
Microarray analysis comparing gene expression in the cortex revealed that for a total of 15 189 genes analysed (15 189 expressed out of 24 081 tested), 180 were upregulated and 27 downregulated at 21 months of age when compared with 4-month-old mice (http://www.ncbi.nlm.nih.gov/geo/, accession number GSE9004, Supplementary Table 1). Interestingly, several specific pre- and postsynaptic neuronal markers including SAP-102, PSD95, synaptophysin and synaptotagmin were unaltered. Similarly, genes related to tPA functions, like LRP, annexin-II and NMDA receptor subunits (NR1, NR2a-d, NR3) were unaltered. Regarding the endogenous tPA inhibitors (the type 1 inhibitor of plasminogen activator (PAI-1), protease nexin-1 and neuroserpin), a striking increased transcription of PAI-1 between 4 and 21 months, could participate in the reduced tPA activity (Q-RT–PCR experiment, not shown).
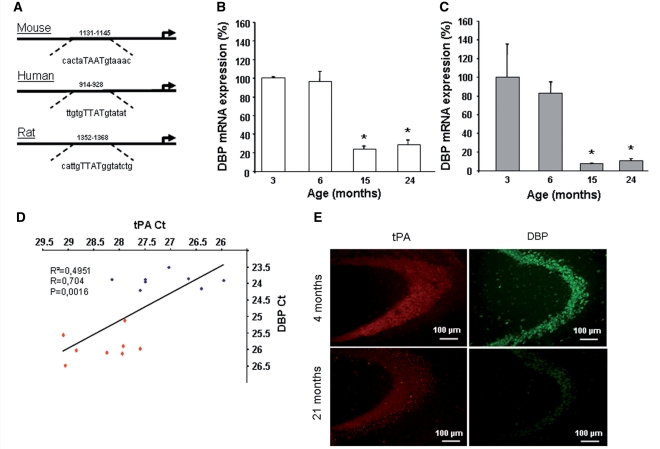
We then postulated that among the genes encoding for transcription factors downregulated between 4 and 21 months of age, some could be critical for the transcriptional regulation of tPA. Among 12 candidates differentially expressed with ageing (Supplementary Table 3), only two were downregulated, both matching with a map of the known binding sites for transcription factors on the mouse tPA promoter (NT 039457), obtained with the Genomatix software: the GATA zinc finger domain-containing protein 1 and the basic region/leucine zipper D-site albumin binding protein (DBP). Interestingly, the recognition site for DBP is conserved for all the tPA promoters identified so far (Fig. 3A).
Figure 3.
Effect of ageing on DBP's transcription and protein levels in the cortex. tPA promoters analysis for the transcription factor DBP (albumin D-site binding protein) sequence in the different species analysed (A). Q-RT–PCR analysis for DBP in the perfused cortex (B) or hippocampus (C) as a function of age (n = 4). (D) The positive correlation between DBP and tPA mRNA cortical levels during ageing (blue squares: young animals; red squares: old animals). Immunostaining for tPA and DBP (E) in the perfused hippocampus with positive staining in mossy fibres and neuronal bodies, respectively. *Significantly different from 3-month-old mice, P < 0.05.
To confirm the microarray results, Q-RT–PCR were performed for DBP and tPA from the cortex and hippocampus of mice at different ages (n = 4 per age). As previously demonstrated for tPA (Fig. 1E and F), DBP mRNA levels were dramatically reduced between 3–6 and 15–24 months in the cortex (–75%) and hippocampus (–85%) (Fig. 3B and C). Accordingly, we observed a positive correlation (P = 0.0016) between tPA and DBP mRNA levels whatever the age considered (Fig. 3D). Immunohistochemistry on hippocampal sections confirmed a decrease in tPA protein levels in mossy fibres with age, associated with a similar decrease in DBP protein levels in adjacent neuronal bodies (Fig. 3E). Interestingly, in the spinal cord, as observed for tPA mRNA levels, there was no age-associated modification of DBP mRNA levels (Supplementary Fig. 2B).
Impact of age-related tPA decline under ischaemic conditions in mice
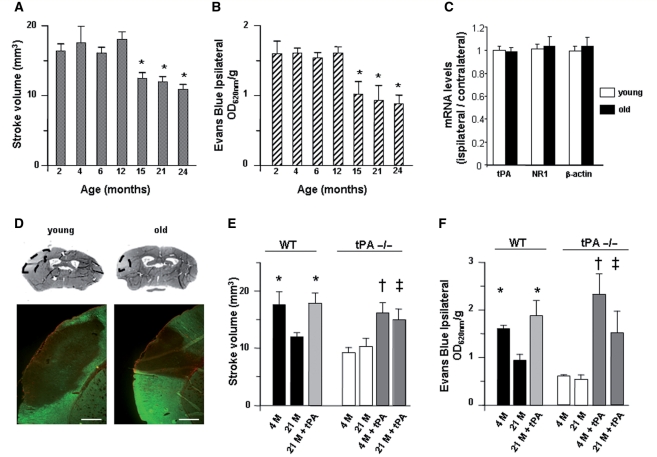
tPA-deficient mice are resistant to excitotoxic/ischaemic damages, which can be reversed by injection of tPA directly into the brain or intravenously (Tsirka et al., 1995; Wang et al., 1998; Nagai et al., 1999). Although tPA can cross the blood–brain barrier by a LRP-dependent mechanism (Benchenane et al., 2005b), it also promotes blood–brain barrier leakage (Yepes et al., 2003). Here, we measured the ischaemic lesion volume and the blood–brain barrier permeability after permanent MCAO in 2- to 24-month-old mice by TTC staining and Evans blue extravasation. Figure 4A and B shows that the ischaemic lesion and the permeability of the blood–brain barrier after ischaemic stroke were significantly reduced (40%) in WT 15-month-old mice and older, with a profile similar to that observed for tPA mRNA levels (Fig. 1E). Q-RT–PCR experiments revealed that the tPA mRNA cortical levels remained unaffected in the ischaemic hemisphere (when compared with the non-ischaemic side) in both young and old animals (Fig. 4C). An immunohistological analysis confirmed that the smaller lesion in old animals observed by regular thionin staining was correlated to a less important loss of MAP-2 (Microtubule-Associated Protein-2, a neuronal marker) immunoreactivity when compared with young mice (Fig. 4D). There was no major difference in the extent of astrogliosis between both ages (Fig. 4D). We then observed that 4 month-old tPA-deficient mice displayed a significant reduction in the ischaemic lesion volume and the blood–brain barrier permeability when compared with age-matched WT mice, but no difference when compared with 21-month-old WT mice (Fig. 4E and F). In contrast to WT mice, no difference was observed between tPA-deficient mice at 4- and 21-month old. Difference between 4-month-old WT and tPA-deficient mice disappeared when tPA-deficient mice were injected with tPA into the ischaemic tissue immediately after the onset of the insult (Fig. 4E and F). Likewise, recombinant tPA increased the ischaemic lesion volume and blood–brain barrier permeability in WT mice (21-month old) to values comparable to those observed in 4-month-old WT mice. Interestingly, intrastriatal NMDA injection led to smaller lesion in old than in young animals (21- versus 4-months old) (Supplementary Fig. 4). Lower levels of tPA thus lead to a decrease in excitotoxic neuronal death, lesion volume and permeability of the blood–brain barrier following ischaemic stroke in older animals.
Figure 4.
Effect of ageing on ischaemia-induced blood–brain barrier leakage and infarct volumes. (A) Mean volume of the ischaemic lesion 48 h after MCAO in WT mice 2–24 months of age (n = 6 for each observation). *P < 0.05. (B) Evans blue dye extravasation 48 h after MCAO in WT mice 2–24 months of age (n = 6 for each observation). *P < 0.05. (C) Q-RT–PCR analysis for tPA, NR1 and β-actin 48 h after MCAO in WT mice at 4 and 21 months of age (n = 4 for each observation; histograms represent the ratio between mRNA levels in the ischaemic versus non-ischaemic cortex). (D) Illustrative photomicrographs of the ischaemic lesion in WT mice at 4 and 21 months of age [upper panel: thionin staining; lower panel: immunohistochemistry for MAP-2 (green) and GFAP (red); Scale bar: 500 µm]. (E) Mean volume of the ischaemic lesion 48 h after MCAO in WT, WT mice injected with rtPA, tPA–/– mice, tPA–/– mice injected with rtPA at 4 and 21 months of age (n = 6 for each observation). *P < 0.05 versus WT and tPA–/–treated mice, †P < 0.05 versus tPA–/– mice (4 months old), ‡P < 0.05 versus WT and untreated tPA–/– mice (21 months old). (F) Evans blue extravasation 48 h after MCAO in WT or tPA–/– mice (4 and 21 months of age), injected or not with rtPA (n = 6 for each observation). *P < 0.05 versus tPA–/– mice (4 months old), *P < 0.05 versus tPA–/– and WT mice (4 and 21 months old). M: age in months.
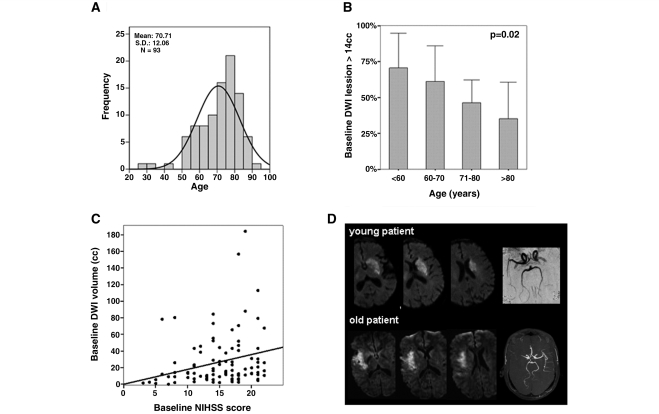
Impact of age in human stroke patients
DWI- and PWI-weighted imaging studies performed in patients (see demographic data on Fig. 5A) with acute ischaemic stroke upon arrival to the emergency department demonstrate that, compared with younger patients, older people have smaller infarcts (see MRI of representative patients on Fig. 5D). Median lesion volume measured in 93 stroke patients at baseline DWI was 14 cc (Fig. 5B), median baseline PWI was 191 cc (data not shown). Patients with larger lesion volumes were significantly younger than patients with smaller lesion volumes: those with baseline DWI < 14 cc had a mean age of 73.36 versus 68.23 years for DWI > 14 cc (P = 0.017); those with baseline PWI < 191 cc had a mean age of 73.98 versus 67.51 years for PWI > 191 cc (P = 0.025). ROC curves used to study sensitivity and specificity of different ages to predict infarct volume, identified age of 74 years as the best cut-off to differentiate small or large lesion volumes. Only 38% of patients older than 74 years had a baseline DWI > 14 cc as compared with 63% of those younger than 74 years (P = 0.018). Similarly, 38% of patients older than 74 years had a baseline PWI > 191 cc as compared with 61% of those younger than 74 years (P = 0.029). A logistic regression analysis showed that older age (OR 1.052; B = 0.051, CI 1.01–1.09, P = 0.015) and lower baseline NIHSS (OR 0.87; B = –0.13; CI 0.78–0.96; P = 0.007) were independent predictors of smaller DWI lesions (baseline DWI < 14 cc) and also of smaller baseline PWI lesions (age OR 1.067; B = 0.064; CI 1.021–1.114; P = 0.004 and NIHSS OR 0.87; B = –0.12; CI 0.794–0.973; P = 0.013). After correcting the logistic regression by cardiovascular risk factors those were still the main independent predictors of infarct volumes with slight modifications in their statistical significance (i.e. older age OR 1.051; B = 0.05, CI 1.003–1.10, P = 0.03) and lower baseline NIHSS (OR 0.84; B = –0.16, CI 0.76–0.94, P = 0.003) were independent predictors of smaller DWI lesions (baseline DWI < 14 cc); interestingly, some of those cardiovascular risk factors (i.e. diabetes) showed a non-significant trend to influence infarct volume (OR 3.5; B = 1.26; CI 0.95–13; P = 0.058). Older age was an independent predictor of smaller infarcts at arrival even when corrected by MCAO location or time from stroke onset to MRI (data not shown). In fact, patients with a proximal MCAO tended to be older than those with distal MCAO (72 versus 66 years, P = 0.07), giving even more power to our findings of smaller lesions among the eldest since larger infarctions might be presumed in those with proximal occlusions. We also found a positive correlation between DWI lesion volume and neurological scores at arrival (r = 0.27, P = 0.008) as shown in Fig. 5C.
Figure 5.
Age-related reduction in the volume of the ischaemic lesion in patients with acute ischaemic stroke and effect of thrombolysis. (A) Distribution of ages among the studied stroke population. (B) Proportion of patients having a lesion volume larger than 14cc at DWI performed at arrival regarding age decades. (C) Correlation between neurological scores (NIHSS) and infarct extension (DWI) both measured at stroke patient arrival at the emergency department. (D) MRI of two representative cases of human MCAO with ischaemic infarct observed at emergency department arrival (within 3 h of stroke onset). Both cases have similar location of the MCAO, however, upper case (36 years) has a measured DWI volume of 21cc as compared with bottom case (79 years) with DWI volume of 12cc at arrival.
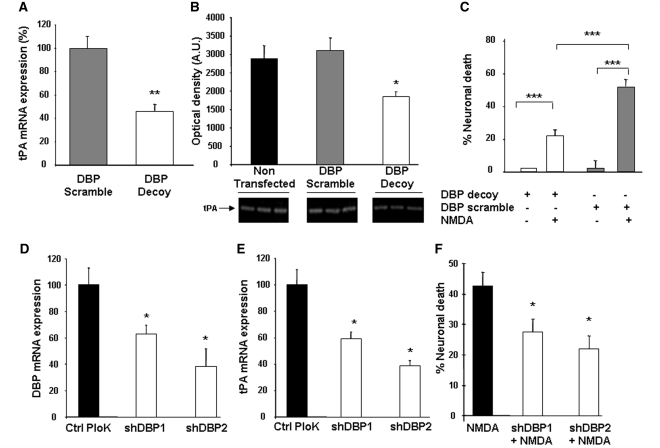
Neuronal DBP functional ‘knock-down’ reduces both tPA levels and NMDA-mediated neurotoxicity
At this stage, we hypothesized that an age-associated reduction in DBP-mediated control of tPA transcription could sustain less deleterious effects of tPA in oldest individuals. We thus investigated whether the binding of DBP to the mouse tPA promoter could influence the neuronal tPA transcription and subsequent potentiation of NMDA-mediated neurotoxicity. A double-stranded decoy oligonucleotide corresponding to the DBP cis-acting element in the mouse tPA promoter (position 1131–1145: aacactataatgtaaacag) and a control scramble decoy were generated and transiently transfected in cultured mouse cortical neurons as previously described (Ahn et al., 2004). After 48 h, the neuronal transcription of tPA was specifically reduced by the DBP decoy oligonucleotide (–54%, P < 0.001, Fig. 6A), while DBP and NMDA receptor subunits mRNA levels remained unchanged (not shown). Zymography assays performed in the corresponding bathing media confirmed a significant decrease (∼30%, P < 0.05) in extracellular tPA activity levels (Fig. 6B) when compared with the scramble control. In agreement with the known pro-excitotoxic effect of tPA (Nicole et al., 2001), DBP decoy-transfected nurons exposed to NMDA (10 µM) are less sensitive to NMDA-mediated excitotoxicity than control cells (–29.7% versus scramble decoy; P < 0.0001, Fig. 6C). Similarly, DBP specific shRNAs reducing DBP transcription (–30% with shDBP1 and –60% with shDBP2, Fig. 6D) reduced tPA mRNA levels (Fig. 6E) and conferred resistance of cortical nurons to NMDA-mediated excitotoxicity (–35% with shDBP1 and –50% with shDBP2, P < 0.05; Fig. 6F).
Figure 6.
Effect of DBP repression on tPA transcription and proteolytic activity in neuronal cultures. Cultured cortical nurons were transiently transfected with either double stranded DBP-decoy or scramble oligonucleotides (A–C) or shRNAs targeting the expression of DBP (D–F) (n = 18 from three independent cultures per group). DBP decoy reduced tPA mRNA levels measured by Q-RT–PCR (A) and active tPA levels in the corresponding bathing media assessed by zymography (B) (n = 18 from three independent cultures per group). DBP decoy-transfected neurons were less sensitive to NMDA-mediated excitotoxicity than DBP scramble-transfected neurons (C). shRNAs reduced the transcription of DBP (D) and tPA (E), while the empty vector (Ctrl Plok) had no effect. Neuronal death induced by NMDA exposure was prevented by DBP shRNAs (F) (n = 12 from three independent cultures per group). *P < 0.05 **P < 0.01, ***P < 0.0001.
Discussion
While reperfusion remains undoubtedly the treatment to apply to treat ischaemic stroke patients (NINDS, 1995), both tPA-related blood–brain barrier leakage and neurotoxicity might be significant problems limiting the overall clinical benefit (Yepes et al., 2009). Accordingly, tPA levels in the vascular (Zlokovic et al., 1995; Wang et al., 1997) and parenchymal (Tsirka et al., 1995; Wang et al., 1998; Nagai et al., 1999) compartments might critically control the extent of stroke damages. However, to date, little was known about these parameters according to the age. The results presented here indicate that the expression of tPA in the brain parenchyma decreases in old mice and that this age-related effect is mediated by the transcription factor DBP. This reduced expression of tPA is associated in vitro with attenuation of excitotoxic damages and in vivo with decrease in the volume of the ischaemic lesion and preservation of the permeability of the neurovascular unit following middle cerebral artery occlusion. Importantly, we also show the existence of an inverse relation between age and the volume of the ischaemic lesion in human patients with acute ischaemic stroke.
DBP belongs to the conserved proline and acidic amino acid-rich basic leucine zipper (PAR bZip) transcription factor family (Khatib et al., 1994; Lopez-Molina et al., 1997; Gachon et al., 2004). The expression of DBP displays a robust circadian rhythm in tissues with high amplitudes of clock gene expression (like the suprachiasmatic nucleus) and constant levels in cerebral regions in which clock gene expression is stable (Lopez-Molina et al., 1997; Gachon et al., 2004). Interestingly, while hippocampal downregulation of DBP expression has a neuroprotective effect, viral over-expression of DBP enhances susceptibility to seizures (During et al., 2003; Klugmann et al., 2006). These observations agree with our results indicating that inhibition of the interaction between DBP and tPA promoter or reduction of its endogenous expression limits the neuronal transcription of tPA and the susceptibility to NMDA-induced injury. Without excluding the probable involvement of other transcription factors, our results indicate that DBP is a key regulator of the transcription of tPA in neurons.
As already stated, tPA has a dual role in the ischaemic brain, with a beneficial thrombolytic activity in the intravascular space and a deleterious effect on the neurovascular unit (Yepes et al., 2009). Our data indicates that whereas ageing does not have an effect on the expression and activity of tPA in the intravascular space, it has a significant impact in its expression and activity in the brain parenchyma, supporting previous observations in rats (Schmoll et al., 2001). The finding that the permeability of the neurovascular unit and the volume of the ischaemic lesion decreases in aged animals not only supports a deleterious role for parenchymal tPA during cerebral ischaemia, but also indicates that the expression and activity of tPA in neurons and glial cells have a direct effect on the final outcome following cerebral ischaemia. This observation is further supported by the data with acute ischaemic stroke patients. A further evidence of an age-dependent effect of tPA in the ischaemic brain is provided by the fact that the intracerebral injection of tPA increases the volume of the ischaemic lesion and the permeability of the neurovascular unit in aged WT mice and young and aged tPA deficient mice to values comparable with those observed in young WT animals.
These alterations in ischaemia-induced brain damages and blood–brain barrier permeability observed in older animals are most probably due to the reduced tPA levels per se, rather than to a general downregulation of transcriptional processes in the senescent organism. Indeed, first, we found more upregulated than downregulated genes in the aged brain (Supplementary Table 1). Second, the expression of the main actors mediating tPA effects in the brain remains unaffected by ageing.
While it is clearly established that the neonate/child brain displays a susceptibility to hypoxic/ischaemic insults different from that in adults, conflicting results arise from the sparse literature regarding old individuals. Ageing is generally described as a negative predictor of post-stroke recovery (Popa-Wagner et al., 2007), but some found no difference or even a better recovery in old versus young animals (Shapira et al., 2002). Moreover, though some authors hypothesized that a reduced density, sensitivity and function of NMDA receptors might lead to less excitotoxicity, they found an increased ischaemic lesion in aged rats at the cortical level but not in the striatum (Davis et al., 1995). However, others have reported that, apart from either a higher mortality rate or brain oedema, old rats subjected to focal ischaemia had similar damages than their young counterparts (Fotheringham et al., 2000; Shapira et al., 2002). Among potential explanations, differences in the ages, end-points and models studied might be candidates. Moreover, the temporal and regional profile of cellular (microglial activation, glial scarring, neurogenesis) and molecular (gene expression) responses are profoundly influenced by age (Petcu et al., 2008).
The dedicated literature is even more limited regarding the extent of ischaemic infarcts in humans, with two studies failing to evidence any difference with age (Nakayama et al., 1994; Engelter et al., 2003). However, in agreement with our data in mice, we provide supporting evidence by DWI- and PWI-weighted imaging in humans. We show that stroke patients display a reduced ischaemic lesion with ageing. This latter finding is of particular relevance with respect to a recent retrospective analysis, reporting that in stroke patients, both age and thrombolytic therapy are independent predictors of ‘Hyperintense Acute Injury Marker’, an index of early blood–brain barrier opening, correlated to poor functional outcome, haemorrhagic transformation and reperfusion (Kidwell et al., 2008). These data suggest that although rtPA-induced thrombolysis is beneficial for stroke patients, ageing and related parenchymal tPA levels should be considered for evaluation of new thrombolytic agents or neuroprotectants in future clinical trials for stroke. Our stroke population is similar to that of large stroke clinical trials, and therefore a representative stroke cohort; however, since we wanted to recruit a very homogeneous group of patients in the study to have patients with comparable brain areas of hypoperfusion, we selected those with a documented occlusion in the middle cerebral artery territory. Therefore, our results showing smaller hypoperfused and infracted areas in the older might not apply for other subtypes of ischaemic stroke such as lacunar infarction or those with a posterior territory infarction that are not represented among our cohort of stroke patients. Moreover, this human data is an indirect support to our experimental results, directly since testing tPA expression in the brains of stroke patients of different ages to demonstrate lower levels among the older is not possible.
In conclusion, age- and DBP-associated reductions in tPA cerebral expression, could have profound impacts in pathological conditions. A full elucidation of the molecular events related to age-associated tPA decreases could lead to innovative therapeutic approaches for seniors, the forgotten patients who, aged 80 years and older, accounted for less than 50 of the total number of patients included in the three initial randomized controlled tPA trials (NINDS, ECASS and ATLANTIS) (Poppe and Hill, 2008).
Supplementary material
Supplementary material is available at Brain Online.
Funding
INSERM, the French Ministry of Research and Technology; the Regional Council of Lower Normandy; the Fondation pour la Recherche Médicale; Fonds Européens de Développement Régional; the Paul Hamel Foundation; the Diagnosis in Molecular Imaging Program (FP6-projectDiMI-LSHB-CT-2005-512146-); National Institutes of Health (Grant NS-49478); Fondo de Investigaciones Sanitarias, The human stroke sub-study (FIS 05/322 and 06/0586, partial). The neurovascular Research Laboratory takes part into the Spanish stroke research network RENEVAS (RETICS 06/0026/0010).
Supplementary Material
Glossary
Abbreviations
- DBP
albumin D site-binding protein
- MCAO
middle cerebral artery occlusion
- NMDA
N-methyl-D-aspartate
- tPA
tissue-type plasminogen activator
- WT
wild-type
References
- Ahn JD, Morishita R, Kaneda Y, Kim HJ, Kim YD, Lee HJ, et al. Transcription factor decoy for AP-1 reduces mesangial cell proliferation and extracellular matrix production in vitro and in vivo. Gene Ther. 2004;11:916–23. doi: 10.1038/sj.gt.3302236. [DOI] [PubMed] [Google Scholar]
- An J, Zhang C, Polavarapu R, Zhang X, Zhang X, Yepes M. Tissue-type plasminogen activator and the low density lipoprotein receptor-related protein induce Akt phosphorylation in the ischemic brain. Blood. 2008;112:2787–94. doi: 10.1182/blood-2008-02-141630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bambauer KZ, Johnston SC, Bambauer DE, Zivin JA. Reasons why few patients with acute stroke receive tissue plasminogen activator. Arch Neurol. 2006;63:661–4. doi: 10.1001/archneur.63.5.661. [DOI] [PubMed] [Google Scholar]
- Benchenane K, Berezowski V, Ali C, Fernández-Monreal M, López-Atalaya JP, Brillault J, et al. Tissue-type plasminogen activator crosses the intact blood-brain barrier by low-density lipoprotein receptor-related protein-mediated transcytosis. Circulation. 2005a;111:2241–9. doi: 10.1161/01.CIR.0000163542.48611.A2. [DOI] [PubMed] [Google Scholar]
- Benchenane K, Berezowski V, Fernández-Monreal M, Brillault J, Valable S, Dehouck MP, et al. Oxygen glucose deprivation switches the transport of tPA across the blood-brain barrier from an LRP-dependent to an increased LRP-independent process. Stroke. 2005b;36:1065–70. doi: 10.1161/01.STR.0000163050.39122.4f. [DOI] [PubMed] [Google Scholar]
- Benchenane K, López-Atalaya JP, Fernández-Monreal M, Touzani O, Vivien D. Equivocal roles of tissue-type plasminogen activator in stroke-induced injury. Trends Neurosci. 2004;27:155–60. doi: 10.1016/j.tins.2003.12.011. [DOI] [PubMed] [Google Scholar]
- Cheng T, Petraglia AL, Li Z, Thiyagarajan M, Zhong Z, Wu Z, et al. Activated protein C inhibits tissue plasminogen activator-induced brain hemorrhage. Nat Med. 2006;12:1278–85. doi: 10.1038/nm1498. [DOI] [PubMed] [Google Scholar]
- Davis M, Mendelow AD, Perry RH, Chambers IR, James OF. Experimental stroke and neuroprotection in the aging rat brain. Stroke. 1995;26:1072–8. doi: 10.1161/01.str.26.6.1072. [DOI] [PubMed] [Google Scholar]
- During MJ, Cao L, Zuzga DS, Francis JS, Fitzsimons HL, Jiao X, et al. Glucagon-like peptide-1 receptor is involved in learning and neuroprotection. Nat Med. 2003;9:1173–9. doi: 10.1038/nm919. [DOI] [PubMed] [Google Scholar]
- Engelter ST, Provenzale JM, Petrella JR, DeLong DM, Alberts MJ. Infarct volume on apparent diffusion coefficient maps correlates with length of stay and outcome after middle cerebral artery stroke. Cerebrovasc Dis. 2003;15:188–91. doi: 10.1159/000068826. [DOI] [PubMed] [Google Scholar]
- Fernández-Monreal M, López-Atalaya JP, Benchenane K, Cacquevel M, Dulin F, Le Caer JP, et al. Arginine 260 of the amino-terminal domain of NR1 subunit is critical for tissue-type plasminogen activator-mediated enhancement of N-methyl-D-aspartate receptor signaling. J Biol Chem. 2004;279:50850–6. doi: 10.1074/jbc.M407069200. [DOI] [PubMed] [Google Scholar]
- Fotheringham AP, Davies CA, Davies I. Oedema and glial cell involvement in the aged mouse brain after permanent focal ischaemia. Neuropathol Appl Neurobiol. 2000;26:412–23. doi: 10.1046/j.1365-2990.2000.00265.x. [DOI] [PubMed] [Google Scholar]
- Gachon F, Fonjallaz P, Damiola F, Gos P, Kodama T, Zakany J, et al. The loss of circadian PAR bZip transcription factors results in epilepsy. Genes Dev. 2004;18:1397–412. doi: 10.1101/gad.301404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golfier G, Dang MT, Dauphinot L, Graison E, Rossier J, Potier MC. VARAN: a web server for variability analysis of DNA microarray experiments. Bioinformatics. 2004;20:1641–3. doi: 10.1093/bioinformatics/bth117. [DOI] [PubMed] [Google Scholar]
- Jaramillo A, Góngora-Rivera F, Labreuche J, Hauw JJ, Amarenco P. Predictors for malignant middle cerebral artery infarctions: a postmortem analysis. Neurology. 2006;66:815–20. doi: 10.1212/01.wnl.0000203649.60211.0e. [DOI] [PubMed] [Google Scholar]
- Khatib ZA, Inaba T, Valentine M, Look AT. Chromosomal localization and cDNA cloning of the human DBP and TEF genes. Genomics. 1994;23:344–51. doi: 10.1006/geno.1994.1510. [DOI] [PubMed] [Google Scholar]
- Kidwell CS, Latour L, Saver JL, Alger JR, Starkman S, Duckwiler G, et al. Thrombolytic toxicity: blood brain barrier disruption in human ischemic stroke. Cerebrovasc Dis. 2008;25:338–43. doi: 10.1159/000118379. [DOI] [PubMed] [Google Scholar]
- Klugmann M, Leichtlein CB, Symes CW, Klaussner BC, Brooks AI, Young D, et al. A novel role of circadian transcription factor DBP in hippocampal plasticity. Mol Cell Neurosci. 2006;31:303–14. doi: 10.1016/j.mcn.2005.09.019. [DOI] [PubMed] [Google Scholar]
- Le Brigand K, Russell R, Moreilhon C, Rouillard JM, Jost B, Amiot F, et al. An open-access long oligonucleotide microarray resource for analysis of the human and mouse transcriptomes. Nucleic Acids Res. 2006;34:e87. doi: 10.1093/nar/gkl485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SY, Kim HJ, Lee WJ, Joo SH, Jeon SJ, Kim JW, et al. Differential regulation of matrix metalloproteinase-9 and tissue plasminogen activator activity by the cyclic-AMP system in lipopolysaccharide-stimulated rat primary astrocytes. Neurochem Res. 2008;33:2324–34. doi: 10.1007/s11064-008-9737-2. [DOI] [PubMed] [Google Scholar]
- Liu D, Cheng T, Guo H, Fernández JA, Griffin JH, Song X, et al. Tissue plasminogen activator neurovascular toxicity is controlled by activated protein C. Nat Med. 2004;10:1379–83. doi: 10.1038/nm1122. [DOI] [PubMed] [Google Scholar]
- Lopez-Molina L, Conquet F, Dubois-Dauphin M, Schibler U. The DBP gene is expressed according to a circadian rhythm in the suprachiasmatic nucleus and influences circadian behavior. EMBO J. 1997;16:6762–71. doi: 10.1093/emboj/16.22.6762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire PG, Seeds NW. Degradation of underlying extracellular matrix by sensory neurons during neurite outgrowth. Neuron. 1990;4:633–42. doi: 10.1016/0896-6273(90)90121-u. [DOI] [PubMed] [Google Scholar]
- Montaner J, Molina CA, Monasterio J, Abilleira S, Arenillas JF, Ribó M, et al. Matrix metalloproteinase-9 pretreatment level predicts intracranial hemorrhagic complications after thrombolysis in human stroke. Circulation. 2003;107:598–603. doi: 10.1161/01.cir.0000046451.38849.90. [DOI] [PubMed] [Google Scholar]
- Nagai N, De Mol M, Lijnen HR, Carmeliet P, Collen D. Role of plasminogen system components in focal cerebral ischemic infarction: a gene targeting and gene transfer study in mice. Circulation. 1999;99:2440–4. doi: 10.1161/01.cir.99.18.2440. [DOI] [PubMed] [Google Scholar]
- Nakayama H, Jørgensen HS, Raaschou HO, Olsen TS. The influence of age on stroke outcome. The Copenhagen Stroke Study. Stroke. 1994;25:808–13. doi: 10.1161/01.str.25.4.808. [DOI] [PubMed] [Google Scholar]
- Nicole O, Docagne F, Ali C, Margaill I, Carmeliet P, MacKenzie ET, et al. The proteolytic activity of tissue-plasminogen activator enhances NMDA receptor-mediated signaling. Nat Med. 2001;7:59–64. doi: 10.1038/83358. [DOI] [PubMed] [Google Scholar]
- Osborne KA, Shigeno T, Balarsky AM, Ford I, McCulloch J, Teasdale GM, et al. Quantitative assessment of early brain damage in a rat model of focal cerebral ischaemia. J Neurol Neurosurg Psychiatry. 1987;50:402–10. doi: 10.1136/jnnp.50.4.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawlak R, Melchor JP, Matys T, Skrzypiec AE, Strickland S. Ethanol-withdrawal seizures are controlled by tissue plasminogen activator via modulation of NR2B-containing NMDA receptors. Proc Natl Acad Sci USA. 2005;102:443–8. doi: 10.1073/pnas.0406454102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petcu EB, Sfredel V, Platt D, Herndon JG, Kessler C, Popa-Wagner A. Cellular and molecular events underlying the dysregulated response of the aged brain to stroke: a mini-review. Gerontology. 2008;54:6–17. doi: 10.1159/000112845. [DOI] [PubMed] [Google Scholar]
- Popa-Wagner A, Badan I, Vintilescu R, Walker L, Kessler C. Premature cellular proliferation following cortical infarct in aged rats. Rom J Morphol Embryol. 2007;27:215–28. [PubMed] [Google Scholar]
- Poppe AY, Hill MD. Acute ischaemic stroke in patients aged 80 years and older: focus on the tolerability of thrombolytic agents. Drugs Aging. 2008;25:95–103. doi: 10.2165/00002512-200825020-00002. [DOI] [PubMed] [Google Scholar]
- Rosell A, Alvarez-Sabín J, Arenillas JF, Rovira A, Delgado P, Fernández-Cadenas I, et al. A matrix metalloproteinase protein array reveals a strong relation between MMP-9 and MMP-13 with diffusion-weighted image lesion increase in human stroke. Stroke. 2005;36:1415–20. doi: 10.1161/01.STR.0000170641.01047.cc. [DOI] [PubMed] [Google Scholar]
- Samson AL, Medcalf RL. Tissue-type plasminogen activator: a multifaceted modulator of neurotransmission and synaptic plasticity. Neuron. 2006;50:673–8. doi: 10.1016/j.neuron.2006.04.013. [DOI] [PubMed] [Google Scholar]
- Schmoll H, Badan I, Fischer B, Wagner AP. Dynamics of gene expression for immediate early- and late genes after seizure activity in aged rats. Arch Gerontol Geriatr. 2001;32:199–218. doi: 10.1016/s0167-4943(01)00101-7. [DOI] [PubMed] [Google Scholar]
- Schnell SA, Staines WA, Wessendorf MW. Reduction of lipofuscin-like autofluorescence in fluorescently labeled tissue. J Histochem Cytochem. 1999;47:719–30. doi: 10.1177/002215549904700601. [DOI] [PubMed] [Google Scholar]
- Shapira S, Sapir M, Wengier A, Grauer E, Kadar T. Aging has a complex effect on a rat model of ischemic stroke. Brain Res. 2002;925:148–58. doi: 10.1016/s0006-8993(01)03270-x. [DOI] [PubMed] [Google Scholar]
- Shin CY, Kundel M, Wells DG. Rapid, activity-induced increase in tissue plasminogen activator is mediated by metabotropic glutamate receptor-dependent mRNA translation. J Neurosci. 2004;24:9425–33. doi: 10.1523/JNEUROSCI.2457-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siao CJ, Tsirka SE. Tissue plasminogen activator mediates microglial activation via its finger domain through annexin II. J Neurosci. 2002;22:3352–8. doi: 10.1523/JNEUROSCI.22-09-03352.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su EJ, Fredriksson L, Geyer M, Folestad E, Cale J, Andrae J, et al. Activation of PDGF-CC by tissue plasminogen activator impairs blood-brain barrier integrity during ischemic stroke. Nat Med. 2008;14:731–7. doi: 10.1038/nm1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333:1581–7. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- Tsirka SE, Gualandris A, Amaral DG, Strickland S. Excitotoxin-induced neuronal degeneration and seizure are mediated by tissue plasminogen activator. Nature. 1995;377:340–4. doi: 10.1038/377340a0. [DOI] [PubMed] [Google Scholar]
- Tusher VG, Tibshirani R, Chu G. Significance analysis of microarrays applied to the ionizing radiation response. Proc Natl Acad Sci USA. 2001;98:5116–21. doi: 10.1073/pnas.091062498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Kittaka M, Sun N, Schreiber SS, Zlokovic BV. Chronic nicotine treatment enhances focal ischemic brain injury and depletes free pool of brain microvascular tissue plasminogen activator in rats. J Cereb Blood Flow Metab. 1997;17:136–46. doi: 10.1097/00004647-199702000-00002. [DOI] [PubMed] [Google Scholar]
- Wang YF, Tsirka SE, Strickland S, Stieg PE, Soriano SG, Lipton SA. Tissue plasminogen activator (tPA) increases neuronal damage after focal cerebral ischemia in wild-type and tPA-deficient mice. Nat Med. 1998;4:228–31. doi: 10.1038/nm0298-228. [DOI] [PubMed] [Google Scholar]
- Wang X, Tsuji K, Lee SR, Ning M, Furie KL, Buchan AM, et al. Mechanisms of hemorrhagic transformation after tissue plasminogen activator reperfusion therapy for ischemic stroke. Stroke. 2004;35:2726–2730. doi: 10.1161/01.STR.0000143219.16695.af. [DOI] [PubMed] [Google Scholar]
- Yepes M, Roussel BD, Ali C, Vivien D. Tissue-type plasminogen activator in the ischemic brain: more than a thrombolytic. Trends Neurosci. 2009;32:48–55. doi: 10.1016/j.tins.2008.09.006. [DOI] [PubMed] [Google Scholar]
- Yepes M, Sandkvist M, Moore EG, Bugge TH, Strickland DK, Lawrence DA. Tissue-type plasminogen activator induces opening of the blood-brain barrier via the LDL receptor-related protein. J Clin Invest. 2003;112:1533–40. doi: 10.1172/JCI19212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zlokovic BV, Wang L, Sun N, Haffke S, Verrall S, Seeds NW, et al. Expression of tissue plasminogen activator in cerebral capillaries: possible fibrinolytic function of the blood-brain barrier. Neurosurgery. 1995;37:955–61. doi: 10.1227/00006123-199511000-00015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.