Abstract
The type A subspecies of Francisella tularensis is a highly virulent facultative intracellular bacterial pathogen, and a potential biological weapon. Recently, there has been renewed interest in developing new vaccines and therapeutics against this bacterium. Natural cases of disease, tularemia, caused by the type A subspecies are very rare. Therefore, the United States Food and Drug Administration will rely on the so called Animal Rule for efficacy testing of anti-Francisella medicines. This requires the human disease to be modeled in one or more animal species in which the pathogenicity of the agent is reasonably well understood. Mice are natural hosts for F. tularensis, and might be able to satisfythis requirement. Tularemia pathogenesis appears to be primarily due to the host inflammatory responsewhich is poorly understood at the molecular level. Additionally, the extent to which this response varies depending on host and pathogen genetic background, or by pathogen challenge route or dose is unknown. Therefore, the present study examined sera and infected tissues from C57BL/6 and BALB/c mice challenged by natural intradermal and respiratory routes with one of two distinct type A strains of the pathogen for cytokine and chemokine responses that might help explain the morbidity associated with tularemia. The results show that the molecular immune response was mostly similar regardless of the variables examined. For instance, mRNA for the proinflammatory cytokine IL-6, and chemokines KC, and IP-10 was consistently upregulated at all sites of infection. Upregulation of mRNA for several other cytokines and chemokines occurred in a more tissue restricted manner. For instance, IFNIFN-γ was highly upregulated in the skin of BALB/c, but not C57BL/6 mice after ID inoculation of the pathogen, whilst IL-10 mRNA upregulation was only consistently seen in the skin and lungs.
1. Introduction
Francisella tularensis subspecies tularensis (type A subspecies) is a highly infectious and virulent facultative intracellular bacterial pathogen of many mammalian species including humans (reviewed in Sjostedt, 2007). It causes a spectrum of diseases collectively called tularemia and it was once developed on an industrial scale as a biological weapon (Dennis et al., 2001; Ellis et al., 2002). Nowadays, there are renewed concerns about the abuse of this pathogen which has led to the call for the development of new countermeasures (Dennis et al., 2001). A major barrier to this aim is the natural clinical rarity of tularemia caused by type A F. tularensis. This makes it impossible to test the efficacy of anti-Francisella drugs and vaccines in human clinical trails. To circumvent this problem the United States Food and Drug Administration (FDA) developed regulations that allow the efficacy of countermeasures to be demonstrated in animal models considered to mimic the human disease (http://www.fda.gov/cber/rules/humeffic.htm). A major tenet of these regulations, referred to as the “Animal Rule,” is that the mechanism of pathogenicity of the disease agent is reasonably well-understood. Applying the Animal Rule to the development of F. tularensis countermeasures is not straightforward, since its pathogenicity is not well characterized (reviewed in Conlan and Oyston, 2007). F. tularensis does not elaborate any obvious exotoxins, and its lipopolysaccharide lacks endotoxicity. Instead, F. tularensis appears to cause disease by proliferating extensively in various host tissues and eliciting a cellular inflammatory response therein that disrupts normal physiology. Histopathological changes in the organs of humans or experimentally-infected model animals including mice support this view (Lillie and Francis, 1936; Baskerville and Hambleton, 1976; Baskerville et al., 1978; Conlan et al., 2003). Similarities in the histopathology of human and murine tularemia suggest that mice are a host species that may at least partially satisfy the Animal Rule for tularemia vaccines. However, it remains to be determined whether mouse and human tularemia pathogenesis is similar at the molecular level.
Inflammation is coordinated by multiple cytokines and chemokines operating in concert (Murdoch and Finn 2000; Borish and Steinke, 2003; Elenkov et al., 2005) and understanding their production during tularemia will be pivotal for refining our understanding of F. tularensis pathogenicity and potentially provide data that would facilitate the application of the Animal Rule to medical countermeasures against it. Immune responses can be influenced by a multitude of parameters including host and pathogen genetic background, and route and dose of infection that can limit the utility of experimental models. Therefore, in the present study we undertook a detailed comparison of the serum and tissue cytokine and chemokine response of BALB/c and C57BL/6 mice infected by intradermal (ID) or respiratory routes with various doses of either of two distinct type A strains of F. tularensis. Overall, regardless of these variables, the results show that a broadly similar cytokine/chemokine response occurred during all cases of primary murine tularemia.
2. Materials and methods
2.1. Bacterial strains
A squirrel isolate of type A F. tularensis strain, FSC 033, and an isolate, FSC 237, of the clinical strain, SCHU S4, was obtained from the Francisella Strain Collection of the Swedish Defense Department. Working stocks of both isolates were prepared as previously described (Twine et al., 2006).
2.2 Infection of mice
Specific-pathogen-free female BALB/c and C57BL/6 mice were purchased from Charles Rivers Laboratories (St. Constant, Que.), and entered experiments when they were 6-8 weeks old. Mice were maintained and used in accordance with the recommendations of the Canadian Council on Animal Care Guide to the Care and Use of Experimental Animals. ID inocula (50 μl / mouse) were injected into a fold of skin in the shaved mid-belly. Mice were exposed to aerosols of the pathogen using a customized commercial nose-only exposure apparatus (In-tox Products, Albuquerque, NM) as previously described (Conlan et al., 2003, 2005; Chen et al., 2003, 2004; Shen et al., 2004). All work involving type A F. tularensis was performed in a federally-licensed, and Select-Agent-approved small animal containment level 3 facility. Mice that became terminally ill were killed by CO2 asphyxiation and, based on experience, it was assumed that they would have died naturally one day later.
2.3 Quantitative bacteriology
At various times of infection, mice were killed by CO2 asphyxiation. For bacteriology, livers, spleens, and lungs were removed, minced with scissors, and homogenized using aerosol-proof homogenizers. Additionally, for mice challenged ID, a 1 cm2 piece of skin surrounding the inoculum site was removed and processed as above. Organ homogenates were diluted in sterile saline and plated for CFU counts.
2.4. Cytokine and chemokine determinations
For cytokine/chemokine analysis, groups of mice (n=3/group) were killed on days 1-4 post-challenge. Sera were prepared from blood collected by cardiac puncture, and were filter sterilized (0.22 μm) and stored at -20°C until needed. Serum levels of cytokines and chemokines were determined using Beadlyte® Mouse 21-plex Cytokine Detection System on a Luminex® 100 IS system (Luminex, Austin, TX) as specified by the manufacturer. Analyses were done in duplicate, and the cytokine/chemokine concentrations were calculated against the standards using Beadview® software version 1.03.
Spleen, liver, lungs, and skin were dissected and immersed immediately in RNAlater (Qiagen, Germantown, MD) and stored as above until needed. Relative amounts of cytokine and chemokine mRNA in infected tissues over the course of infection were estimated by real-time PCR essentially as described elsewhere (Johnson et al., 2003; Andersson et al., 2006). Briefly, total RNA was extracted from tissues, cDNA prepared, amplified and quantified using primers and probes designed with the Primer3 program available at http://frodo.wi.mit.edu/cgi-bin/primer3/primer3_www.cgi. Levels of PCR product were normalized to a housekeeping gene (beta-2-microglobulin (β2m), and data presented as the average of relative expression values compared to those in the corresponding tissues of uninfected mice.
3.0 Results
3.1 Infection kinetics following ID or aerosol challenge with type A isolates of F. tularensis
BALB/c and C57BL/6 mice were infected ID with 103 cfu of type A isolate FSC 033. Additional groups of BALB/c mice were infected by aerosol with 101 or 103 of SCHU S4 (FSC237). The ensuing kinetics of these infections are shown in Table 1. Regardless of challenge dose or route, infection disseminated to the liver and spleen by day 2 and over the next 2 days grew rapidly therein. BALB/c and C57BL/6 mice appeared equally susceptible to ID challenge in that each died 3 to 4 days after challenge with similar bacterial burdens in their organs. However, BALB/c mice invariably showed overt signs of infection much earlier than C57BL/6 mice. BALB/c mice always exhibited clear signs of infection (ruffled fur) by day 2 of infection that became progressively worse on each successive day (lethargy, hunching, anorexia, cold to the touch, conjunctivitis) whereas C57BL/6 mice only became obviously sick during the final day of infection by which time BALB/c mice appeared moribund. Moreover, overt inflammation at the skin inoculation site was much more pronounced in BALB/c versus C57BL/6 mice by day 4 of infection (not shown). BALB/c mice challenged with low or high dose aerosols of SCHU S4 also showed progressive signs of infection from day 2 onwards, but mice challenged with the higher dose died 1-2 days earlier. The data presented above is consistent with that we have previously generated for BALB/c and C57BL/6 mice challenged ID and by aerosol with low doses of FSC 033 or SCHU S4 (Conlan et al., 2003, 2005; Chen et al., 2003, Twine et al.,2006). Similar results were reported by others for another distinct type A isolate (Wu et al., 2005).
Table 1.
Bacterial growth in the organs of mice infected with various concentrations of different strains of type A F. tularensis by ID and aerosol routes.
| Expt. No. |
Mouse strain |
Francisell a strain |
Route/dose | TTD in days |
organ | Log 10 CFU± SD on day of infection proportion infe n=3-4 |
|||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||||||
| 1 | BALB/c | FSC033 | ID /103 CFU | 3-4 | skin | 6.03 ± 0.15 | 7.74 ±0.30 | 7.51± 0.80 | 8.30 ±0.10 |
| liver | 3.87 (1/3) | 5.0 ±0.14 | 7.49 ±0.85 | >10.0 (3/3) | |||||
| spleen | 2.89 (2/3) | 5.24 ±0.14 | 8.02 ±1.23 | 9.70 ±0.22 | |||||
| lung | 1.60 (1/3) | 2.45 (2/3) | 5.63 ±1.30 | 8.86 ±0.12 | |||||
| 2 | C57BL/6 | FSC033 | ID /103 CFU | 3-4 | skin | 5.66 ± 0.45 | 7.15 ±0.18 | 6.80 ±0.18 | 7.60 ±0.18 |
| liver | <2.30 (0/3) | 6.24 ±0.99 | 7.93 ±0.25 | >10.0 (3/3) | |||||
| spleen | 1.45 (2/3) | 6.77 ±1.20 | 8.68± 0.06 | 9.42 ±0.16 | |||||
| lung | <1.3 (0/3) | 4.08 ± 0.70 | 6.04 ±0.39 | 8.59 ±0.17 | |||||
| 3 | BALB/c | SCHU S4 (FSC237) |
aerosol / 10 CFU | 5-6 | skin | ND | ND | ND | ND |
| liver | <1.6 (0/4) | 3.65 ± 1.43 | 5.65 ± 0.30 | 7.71 ± 0.18 | |||||
| spleen | <1.6 (0/4) | 3.67 ± 1.24 | 6.14 ± 0.40 | 8.74 ± 0.32 | |||||
| lung | 4.03 ± 0.19 | 5.73 ± 0.21 | 6.77 ± 0.15 | 7.39 ± 0.32 | |||||
| 4 | BALB/c | SCHU S4 (FSC 237) |
aerosol / 103 CFU | 4 | skin | ND | ND | ND | ND |
| liver | <1.6 (0/4) | 5.58±0.41 | 7.32±0.35 | 8.93±0.09 | |||||
| spleen | <1.6 (0/4) | 4.76±0.63 | 7.74±1.20 | 8.83±0.72 | |||||
| lung | 4.76±0.32 | 6.99±0.25 | 7.96±0.15 | 8.39±0.04 | |||||
TTD, time to death. ND, not done
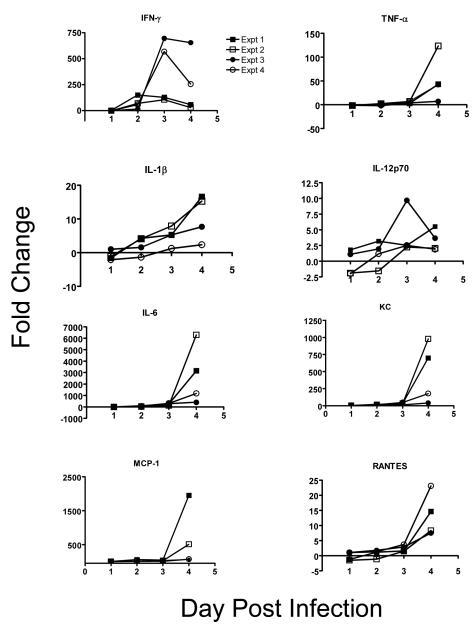
3.2 Changes in serum cytokine and chemokine levels during primary tularemia
The levels of a panel of 21 cytokines and chemokines in the sera of representative mice (n=3 /group) from the experiments depicted in Table 1 were measured on various days post-challenge, and the most pronounced increases are shown in figure 1. In all cases by day 4 of infection, statistically-significant (P<0.05) and often substantial increases were observed in the levels of IFN-γ (100-700-fold), TNF-α (7-120-fold), IL-6 (400-6300-fold), IL-1β (2.5-16-fold), IL-12p70 (2-9-fold), KC (40-980-fold), MCP-1 (65-1950-fold), and RANTES (8-14-fold) in the serum (range in parentheses in the maximum average increase recorded on any day for each of experiments 1-4 shown in Table 1). Some of these changes were evident as early as day 1, and most changes were evident by day 2 of infection. In all cases, serum IFN-γ levels peaked on day 3 of infection whereas all other cytokines and chemokines, except IL-12p70, peaked at day 4. Fold-increases in IFN-γ levels peaked aerosol versus higher ID challenged mice, whereas the opposite was the case for IL-6, KC, and MCP-1. No such clear distinctions were evident with TNFα, IL-1β, IL-12p40, or RANTES. There were no obvious differences in serum cytokine and chemokine levels between BALB/c and C57BL/76 mice challenged ID. Among the other cytokines and chemokines examined, IL-9 was significantly elevated in three of the four experimental groups (peak increase 6-9-fold), and IL-10 (peak increase 2-5-15-fold) and VEGF (peak increase 3.5-7.0-fold) in ID challenged mice only (not shown). In contrast, decreases in IL-5 (2-3-fold) and IL-13 (2-5-14-fold) were observed in all experimental groups, but these were not always statistically significant (not shown). Finally, IL-1α, IL-2, IL-3, IL-4, IL12p40, IL-17, GM-CSF, or MIP-1β levels were either unchanged, or only slightly increased or decreased in one or two experiments (data not shown). For simplicity, we have assumed that the latter results were random noise.
Figure 1.
Selected serum cytokine and chemokine levels in BALB/c (expts 1,3,4,) and C57BL/6 mice (expts 2) challenged ID (expts 1,2) or by aerosol (expts 3,4) with type A F. tularensis. Sera were obtained from 3 mice / group / time-point and examined by Luminex for a panel of 21 cytokines or chemokines. Data were analyzed by t test and were considered significantly different from control sera at P<0.05.
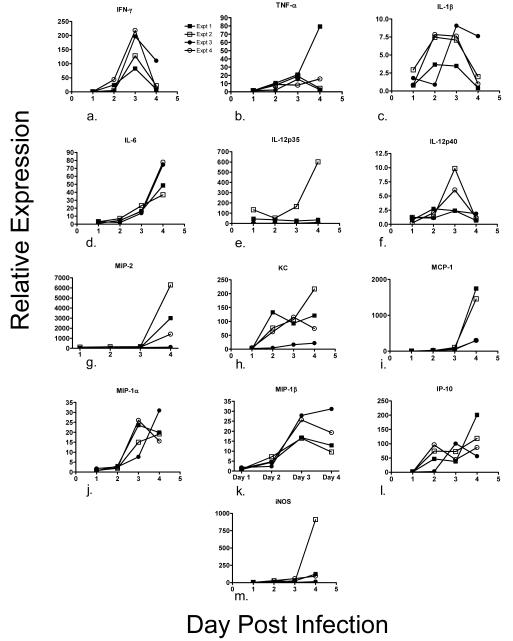
3.3 Changes in tissue cytokine and chemokine mRNA levels during primary tularemia
In addition to serum protein levels, mRNA levels for a semi-overlapping series of 17 cytokines and chemokines in liver, spleen, lungs, and, for ID challenged mice the skin were determined by qPCR (n=3 mice /group). We considered an increase in the mRNA level of ≥ 2-fold on two or more days of infection, or a single day increase of ≥ 5-fold to be potentially relevant, and any other results were considered to be noise. By these criteria, in the liver (Figure 2), mRNA for IFN-γ (82-218-fold), TNF-α (15-79-fold), IL-1 β (4-9-fold), IL-6 (36-78-fold), IL-12p35 (8-600-fold), IL-12p40 (2-10-fold), MIP-2 (125-6295-fold), KC (22-217-fold), MCP-1 (294-1458-fold), MIP-1α (19-31-fold), MIP-1β (16-31-fold), IP-10 (96-201-fold), and iNOS (15-91-fold) were elevated in all four groups of challenged mice (range in parentheses in the maximum average increase recorded on any day for each of experiments 1-4 shown in Table 1). In contrast, IL-12p-40 was only sporadically elevated in all four groups, and IL-10 mRNA was only consistently over-expressed in BALB/c mice (2-6-fold; not shown). Liver mRNA for IL-4 was consistently over-expressed (3-20-fold) in three of the four groups, whereas RANTES mRNA was only elevated on day 4 (9-fold) in C57BL/6 mice challenged ID with FSC033, or (2-3-fold) on three out of four days in BALB/c mice challenged with a low dose aerosol of SCHU S4 (not shown). IL-2 mRNA was never increased on any day of infection in any experiment (not shown). As with serum protein levels, liver mRNA levels for IFN-γ peaked on day 3 of infection in all cases. Liver mRNAs for IL-6, MIP-2, MCP-1, and iNOS all peaked on day 4 of infection. Liver mRNA for IL-12p35, MIP-2 and MCP-1 peaked at higher levels in ID versus aerosol challenged mice. Levels of IL-4, IL-12p35, and iNOS mRNAs peaked higher in C57BL/6 mice.
Figure 2.
Selected cytokine and chemokine mRNA levels in the livers of BALB/c (expts 1,3,4) and C57BL/6 mice (expt 2) challenged ID (expts 1,2) or by aerosol (expts 3,4) with type A F. tularensis. Liver mRNA was extracted from 3 mice / group / timepoint and examined by qPCR for a panel of 17 cytokines or chemokines.
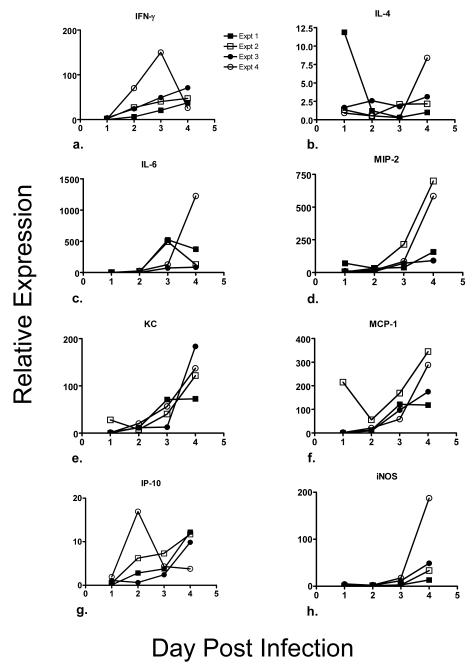
In the spleen (Figure 3), mRNA levels for IFN-γ (37-150-fold), IL-4 (2-12-fold),IL-6 (85-1226-fold), MIP-2 (92-699-fold), KC (72-184-fold), MCP-1 (121-345-fold), IP-10 (10-17-fold), and iNOS (13-187-fold) were elevated in all four groups (range in parentheses in the maximum average increase recorded on any day for each of experiments 1-4 shown in Table 1). MIP-2 mRNA peaked at a higher level in C57BL/6 mice versus BALB/c mice challenged ID with FSC 033 and in mice challenged by aerosol with 103 versus 10 cfu of SCHU S4. IL-10 mRNA was only consistently elevated (4-33-fold) in the spleens of BALB/c mice, whereas mRNA for IL-1β (3-7-fold), IL-12p35 (5-19-fold), MIP-1α (5-11-fold), MIP-1β (3-16-fold), and RANTES (5-9-fold) was elevated in the spleens in three of the four experimental groups (not shown). Spleen mRNA for IL-12p40 (3-4-fold) was only consistently elevated in BALB/c mice challenged by aerosol with 103 cfu of SCHU S4, whereas TNF-α mRNA (3-10-fold) was only consistently expressed in mice challenged with a 100-fold lower dose aerosol (not shown). MIP-2 mRNA peaked at a higher level in C57BL/6 mice versus BALB/c mice challenged ID with FSC 033 and in mice challenged by aerosol with 103 versus 10 cfu of SCHU S4. Splenic IL-2 mRNA was never elevated (not shown).
Figure 3.
Selected cytokine and chemokine mRNA levels in the spleens of BALB/c (expts 1,3,4) and C57BL/6 mice (expt 2) challenged ID (expts 1,2) or by aerosol (expts 3,4) with type A F. tularensis. Spleen mRNA was extracted from 3 mice / group / timepoint and examined by qPCR for a panel of 17 cytokines or chemokines.
In the lungs, mRNA levels for IFN-γ, (6-67-fold), IL-6 (57-185-fold), IL-10 (7-54-fold), IL-12p40 (3-12-fold), MIP-2 (18 -35-fold), KC (7-26-fold), MCP-1 (8-75-fold), MIP-1α (6-23-fold), and IP-10 (66-142-fold) were elevated on at least one day of infection in all groups (range in parentheses in the maximum average increase recorded on any day for each of experiments 1-4 shown in Table 1). In most cases, lung cytokine and chemokine mRNA were elevated earlier and at higher levels in mice challenged by aerosol versus ID, presumably reflecting the fact that it takes 2-3 days for the pathogen to disseminate from the skin to the lungs. However, mRNA levels for IL-10 and IP-10 were raised to similar levels on days 2-3 in all groups. Levels of mRNA for IL-1β (3-4-fold) were elevated in three of four groups, and MIP-1β mRNA (4-20-fold) was elevated in all groups except C57BL/6 mice challenged ID. TNF-α mRNA was over-expressed in the lungs of BALB/c mice challenged ID with 103 cfu of F. tularensis strain FSC 033 (2-28-fold), or by aerosol with 10 cfu of SCHU S4 (3-7-fold). Levels of iNOS mRNA were raised a maximum of 6-15-fold only in C57BL/6 mice challenged ID with 103 cfu of strain FSC 033 or BALB/c mice challenged by aerosol with 103 cfu of SCHU S4. Levels of mRNA for IL-2, IL-4, IL-12p35, and RANTES were never over-expressed in any group.
In two experiments (experiments 1 and 2 in Table 1), cytokine/chemokine mRNA levels in the skin following ID challenge of BALB/c and C57BL/6 mice with 103 cfu of FSC 033 were measured. In the skin mRNA levels for IL-1β (30-48-fold), IL-6 (38-204-fold), IL-12p35 (5-53-fold), MIP-2 (4-28-fold), KC (103-104-fold), MCP-1 (13-180-fold), IP10 (27-119-fold), MIP-1α (31-131-fold), MIP-1β (35-437-fold),RANTES (5-8-fold) were over-expressed in both mouse strains, (range in parentheses in the maximum average increase recorded on any day of infection). IFN-γ mRNA (8-338-fold) and IL-10 mRNA (3-6-fold) was consistently over-expressed only in BALB/c mice whereas the opposite was the case for IL-12p40 mRNA (4-23-fold), TNF-α mRNA (3-fold), and iNOS mRNA (8-fold; figures in parentheses show day-to-day range). IL-6, IL-12p35, MCP-1, MIP-1α, MIP-1β mRNA levels peaked at higher levels in BALB/c versus C57BL/6 mice. This was not the case with mRNA for IL-1β, KC or RANTES which were upregulated to similar peak levels in both mouse strains. IL-2 mRNA was never over-expressed.
4. Discussion
Because human infection with type A F. tularesis is clinically rare, it is currently impossible to demonstrate the efficacy of anti-Francisella drugs and vaccines in human clinical trials. Instead, licensure of medical countermeasures will need to rely on the application of FDA’s Animal Rule which allows the demonstration of efficacy in animal models. The Animal Rule requires a detailed understanding of the mechanisms of pathogenesis of experimental tularemia. Tularemia pathogenesis involves cellular and molecular immune responses occurring at various sites within the infected host. The cells involved have been reasonably well identified in murine models of tularemia caused by attenuated F. tularensis LVS and clinical isolates of the pathogen (Elkins et al., 2003; Cowley et al., 2005; Conlan et al., 2002, 2005; Chen et al., 2004; Fulop et al., 2001; Wu et al., 2005). These studies have revealed that various innate host defenses and B cells and the specific antibodies they produce are able to combat infection with LVS. In contrast, type A strains of F. tularensis appear to be completely resistant to murine innate and humoral immune defenses and can only be killed by specific T-cell-mediated immunity under the influence of IFN-γ. As confirmed by the current study, type A strains of F. tularensis rapidly kill mice before protective CMI responses can be generated. All common mouse strains appear to be equally susceptible to primary infection with type A F. tularensis, but only some of them (e.g. BALB/c but not C57BL/6 mice) develop early clinical signs of infection and can be protected by prior vaccination with LVS (Chen et al., 2003; Conlan et al., 2003, 2005; Shen et al., 2004; Wu et al., 2005). The reasons for these discrepancies remain unknown, but could reflect differences in host molecular inflammatory responses to the pathogen.
Very little is known about the molecular immune response to primary infection by type A F. tularensis, and how this is affected by host and pathogen genetic background, or route and dose of infection. The current study was undertaken to begin addressing these key issues. It showed that for a selection of cytokines and chemokines, the response to primary infection was qualitatively similar regardless of the aforementioned variables. In all variations of primary murine tularemia examined, increases occurred in serum protein levels of IFN-γ, TNF-α, IL-6, KC, RANTES and MCP-1 and in liver, spleen, and lung, mRNA for IFN-γ, IL-6, MCP-1, MIP-2, KC, and IP-10. In the skin, mRNA for IL-1β, IL-6, IL-12p35, MIP-2, MCP-1, KC, IP-10, MIP-1α, MIP-1β, and RANTES was upregulated in both BALB/c and C57BL/6 mice challenged ID. Some cytokines and chemokines showed a more restricted pattern of up-regulation. For instance, mRNA forIL-1β, IL-12p35 and MIP-1β was routinely elevated in the liver and skin only.
Recently, others examined a more limited cytokine and chemokine response in C57BL/6 mice challenged IP with a lethal dose or ID with a sublethal dose of F. tularensis LVS (Cole et al., 2006). As in the current study, the latter mice exhibited increases in serum, TNFα, IL-6, IFNγ, KC, and MCP-1. In the liver, both studies showed increased expression of mRNA for TNFα, IFN-γ, IL-12p35, IL-1β, IP-10, KC, MCP-1, and iNOS. In the spleen, upregulation of mRNA for IFN–γ, MCP-1,KC, and IP-10, and iNOS were commonly observed in both studies, as was mRNA for IFN- γ, IL-10, MCP-1,KC, and IP-10 in the lungs. Therefore, all of the aforementioned similarities should be considered as robust biomarkers of murine tularemia regardless of the pathogen strain, host genetic background, or challenge route or dose. The same could be true for the other cytokines and chemokines that were shown to be universally up-regulated in all challenge groups in the present study, but were not examined by the Cole et al study. Additionally, both studies recorded increases in serum IL-10, liver mRNA for IL-12p40 and RANTES, spleen mRNA for IL-1β, IL-10, and lung mRNA for IL-1β in C57BL/6 mice. However, compared to the present study, the Cole et al. study failed to show increased expression of mRNA for IL-12p40, and iNOS in the lungs, and for IL12p35, RANTES, or IL-4 mRNA in the spleen. These mainly minor discrepancies could be due to differences in the challenge routes employed or could reflect innate virulence differences between LVS and clinical type A strains of the pathogen.
Despite the qualitative similarities in the molecular immune response described above, some kinetic and quantitative differences between mouse challenge groups were evident in the current study. For instance, serum IFN-γ levels peaked at higher levels in aerosol versus ID challenged mice, whereas the opposite was the case for IL-6, KC, and MCP-1. In the liver mRNA for TNF-α, and IL-10 was more over-expressed in BALB/c versus C57BL/6 mice whereas the opposite was the case for IL-12p35 and iNOS mRNA. In the spleen, mRNA for MIP-2 and MCP-1 was more over-expressed in C57BL/6 mice. In the skin, mRNA for IFN-γ, and IL-10 was only over-expressed in BALB/c mice, whereas the opposite was the case for IL-12p40 and iNOS mRNA. Whether these differences explain why BALB/c mice develop more pronounced inflammation at the site of ID inoculation and more obvious clinical signs of infection remain to be determined.
Most of the cytokines and chemokines up-regulated during primary tularemia are known mediators of acute cellular inflammation which is a hallmark of this disease, and could also contribute directly to the accompanying tissue necrosis. However, determining the relative importance a given cytokine or chemokine to tularemia morbidity and mortality will not be straightforward. For example, not all of them are obviously over-expressed at all sites of infection. Additionally, despite differences in clinical signs, both BALB/c and C57BL/6 mice die at the same time after challenge with type A. F. tularensis. Furthermore, IFN-γ knock out mice develop less severe histopathology than normal mice, but still die at the same time after challenge with a low dose aerosol or ID inoculum of type A F. tularensis (Chen et al., 2004). Nevertheless, the current study has begun to refine our understanding of the mechanisms of F. tularensis infection necessary for development and regulatory approval of countermeasures against this highly virulent pathogen.
Acknowledgements
We thank Luc Lemay and Michel Cleroux for technical assistance, and Marianne Casey for administrative assistance. This project has been funded in whole or in part with Federal funds from the National Institute of Allergy and Infectious Diseases, National Institutes of Health, Department of Health and Human Services, under Contract No. HHSN26620050041C.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Andersson H, Hartmanova B, KuoLee R, Ryden P, Conlan W, Chen W, Sjostedt A. Transcriptional profiling of host response in mouse following aerosol infection with type A Fancisella tularensis. J. Med. Microbiol. 2006;55:263–271. doi: 10.1099/jmm.0.46313-0. [DOI] [PubMed] [Google Scholar]
- Baskerville A, Hambleton P. Pathogenesis and pathology of respiratory tularaemia in the rabbit. Brit. J. exp. Path. 1979;57:339–347. [PMC free article] [PubMed] [Google Scholar]
- Baskerville A, Hambleton P, Dowsett AB. The pathology of untreated and antibiotic-treated tularaemia in monkeys. Brit. J. exp. Path. 1978;59:615–23. [PMC free article] [PubMed] [Google Scholar]
- Borish LC, Steinke JW. Cytokines and chemokines. J. Allergy Clin. Immunol. 2003;111:S460–475. doi: 10.1067/mai.2003.108. [DOI] [PubMed] [Google Scholar]
- Chen W, Shen H, Webb A, KuoLee R, Conlan JW. Tularemia in BALB/c and C57BL/6 mice vaccinated with Francisella tularensis LVS and challenged intradermally, or by aerosol with virulent isolates of the pathogen; protection varies depending on pathogen virulence, route of exposure, and host genetic background. Vaccine. 2003;21:3690–3700. doi: 10.1016/s0264-410x(03)00386-4. [DOI] [PubMed] [Google Scholar]
- Chen W, KuoLee R, Shen H, Conlan JW. Susceptibility of immunodeficient mice to aerosol and systemic infection with virulent strains of Francisella tularensis. Microbial Pathogenesis. 2004;36:311–318. doi: 10.1016/j.micpath.2004.02.003. [DOI] [PubMed] [Google Scholar]
- Cole LE, Elkins KE, Michalek SM, Quereshi N, Eaton LJ, Rallabhandi P, Cuesta N, Vogel SN. Immunologic consequences of Francisella tularensis live vaccine strain infection: role of the innate immune response in infection and immunity. J. Immunol. 2006;176:6888–6899. doi: 10.4049/jimmunol.176.11.6888. [DOI] [PubMed] [Google Scholar]
- Conlan JW, Shen H, Webb A, Perry MB. Mice vaccinated with the O-antigen of Francisella tularensis LVS lipopolysaccharide conjugate to bovine serum albumin develop varying degrees of protective immunity against systemic or aerosol challenge with virulent type A and type B strains of the pathogen. Vaccine. 2002;20:3465–3471. doi: 10.1016/s0264-410x(02)00345-6. [DOI] [PubMed] [Google Scholar]
- Conlan JW, Chen W, Shen H, Webb A, KuoLee R. Experimental tularemia in mice challenged by aerosol or intradermally with virulent strains of Francisella tularensis: bacteriologic and histopathologic studies. Microbial Pathogenesis. 2003;34:239–248. doi: 10.1016/s0882-4010(03)00046-9. [DOI] [PubMed] [Google Scholar]
- Conlan JW, Shen H, KuoLee R, Zhao X, Chen W. Aerosol-, but not intradermal- immunization with the live vaccine strain of Francisella tularensis protects mice against subsequent aerosol challenge with a highly virulent type A strain of the pathogen by an αβ T cell- and interferon gamma- dependent mechanism. Vaccine. 2005;23:2477–2485. doi: 10.1016/j.vaccine.2004.10.034. [DOI] [PubMed] [Google Scholar]
- Conlan JW, Oyston PCF. Vaccines against Francisella tularensis. Ann. New York Acad. Sci. 2007;1105:325–50. doi: 10.1196/annals.1409.012. [DOI] [PubMed] [Google Scholar]
- Cowley SC, Hamilton E, Frelinger JA, Su J, Forman J, Elkins KE. CD4-CD8- T cells control intracellular bacterial infections both in vitro and in vivo. J. Exp. Med. 2005;202:309–319. doi: 10.1084/jem.20050569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis DT, Inglesby TV, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Fine AD, Friedlander AM, Hauer J, Layton M, Lillibridge SR, McDade JE, Osterholm MT, O’Toole T, Parker G, Perl TM, Russell PK, Tonat K. Tularemia as a biological weapon: medical and public health management. Jama. 2001;285:2763–2773. doi: 10.1001/jama.285.21.2763. [DOI] [PubMed] [Google Scholar]
- Elenkov IJ, Lezzoni DG, Daly A, Harris AG, Chrousos GP. Cytokine dysregulation, inflammation, and well-being. Neuroimmunomodulation. 2005;12:255–269. doi: 10.1159/000087104. [DOI] [PubMed] [Google Scholar]
- Ellis J, Oyston PCF, Green M, Titball RW. Tularemia. Clin. Microbiol. Reviews. 2002;15:631–646. doi: 10.1128/CMR.15.4.631-646.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkins KE, Cowley SC, Bosio CM. Innate and adaptive immune responses to an intracellular bacterium, Francisella tularensis live vaccine strain. Microbes and Infection. 2003;5:135–142. doi: 10.1016/s1286-4579(02)00084-9. [DOI] [PubMed] [Google Scholar]
- Fulop M, Mastroeni P, Green M, Titball RW. Role of antibody to lipopolysaccharide in protection against low- and high- virulence strains of Francisella tularensis. Vaccine. 2001;19:4465–4472. doi: 10.1016/s0264-410x(01)00189-x. [DOI] [PubMed] [Google Scholar]
- Johnson LL, Bergren KN, Szaba FM, Chen W, Smiley ST. Fibrin-mediated protection against infection-stimulated immunopathology. J. Exp. Med. 2003;197:801–806. doi: 10.1084/jem.20021493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lillie RD, Francis E. The pathology of tularemia. NIH bulletin. 1936;167:1–217. [Google Scholar]
- Murdoch C, Finn A. Chemokine receptors and their role in inflammation and infectious diseases. Blood. 2000;95:3032–3043. [PubMed] [Google Scholar]
- Shen H, Chen W, Conlan JW. Susceptibility of various mouse strains to systemically- or aerosol- initiated tularemia by virulent type A Francisella tularensis before and after immunization with the attenuated live vaccine strain of the pathogen. Vaccine. 2004;22:2116–2121. doi: 10.1016/j.vaccine.2003.12.003. [DOI] [PubMed] [Google Scholar]
- Sjostedt A. Tularemia: History, epidemiology, pathogen physiology and clinical manifestations. Ann. New York Acad. Sci. 2007;1105:1–29. doi: 10.1196/annals.1409.009. [DOI] [PubMed] [Google Scholar]
- Twine SM, Shen H, Kelly JF, Chen W, Sjostedt A, Conlan JW. Virulence comparison in mice of distinct isolates of type A Francisella tularensis. Microbial Pathogenesis. 2006;40:133–38. doi: 10.1016/j.micpath.2005.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu TH, Hutt JA, Garrison KA, Berliba LS, Zhou Y, Lyons CR. Intransal vaccination induces protective immunity against intranasal infection with virulent Francisella tularensis bovar A. Infect. Immun. 2005;73:2644–54. doi: 10.1128/IAI.73.5.2644-2654.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]