Abstract
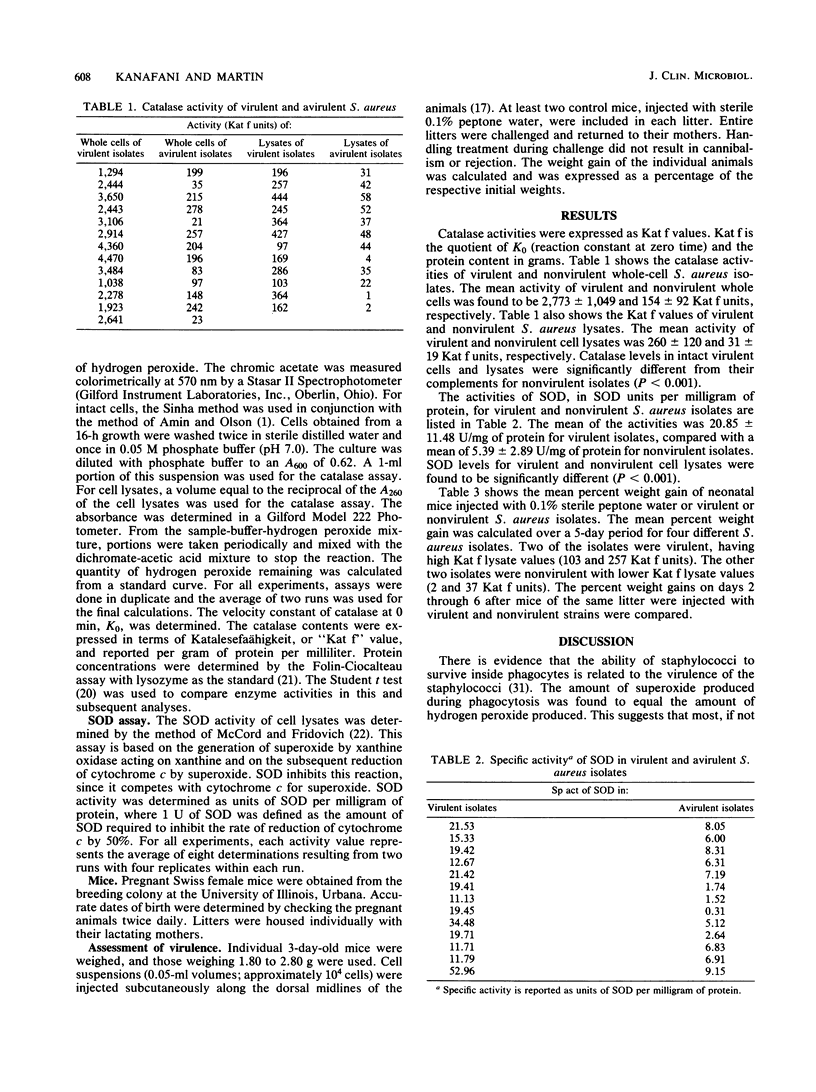
Catalase and superoxide dismutase (SOD) activities of virulent and nonvirulent isolates of Staphylococcus aureus were compared. The mean value of catalase activity for intact cell suspensions was 2,773 +/- 1,049 Kat f units (Kat f is defined as the ratio of the velocity constant of catalase at 0 min to the protein content in grams per milliliter); that of nonvirulent isolates was 154 +/- 92 Kat f units. The mean value of the catalase activities for lysates of virulent isolates was 260 +/- 120 Kat f units, and that of nonvirulent isolates was 31 +/- 19 Kat f units. Catalase levels in intact cells as well as in cell lysates were significantly different for virulent than for nonvirulent S. aureus isolates (P less than 0.001). The mean value of SOD activities was 20.85 +/- 11.48 U (1 U is defined as the amount of SOD required to inhibit the rate of reduction of cytochrome c by 50%) for virulent cell lysates, compared with a mean of 5.39 +/- 2.89 U for nonvirulent cell lysates. The SOD levels in virulent and nonvirulent isolates were significantly different (P less than 0.001). The virulence of the S. aureus isolates was determined by comparing weight gains of neonatal mice injected with virulent or nonvirulent strains. The percent weight gain of neonatal mice injected with virulent isolates was significantly lower than that of those injected with nonvirulent isolates.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Amin V. M., Olson N. F. Influence of catalase activity on resistance of coagulase-positive staphylococci to hydrogen peroxide. Appl Microbiol. 1968 Feb;16(2):267–270. doi: 10.1128/am.16.2.267-270.1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews G. P., Martin S. E. Catalase activity during the recovery of heat-stressed Staphylococcus aureus MF-31. Appl Environ Microbiol. 1979 Sep;38(3):390–394. doi: 10.1128/aem.38.3.390-394.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro C. E. Mechanisms of reaction of hemeproteins with oxygen and hydrogen peroxide in the oxidation of organic substrates. Pharmacol Ther. 1980;10(2):171–189. doi: 10.1016/0163-7258(80)90080-7. [DOI] [PubMed] [Google Scholar]
- Clifford D. P., Repine J. E. Hydrogen peroxide mediated killing of bacteria. Mol Cell Biochem. 1982 Dec 10;49(3):143–149. doi: 10.1007/BF00231175. [DOI] [PubMed] [Google Scholar]
- Curnutte J. T., Whitten D. M., Babior B. M. Defective superoxide production by granulocytes from patients with chronic granulomatous disease. N Engl J Med. 1974 Mar 14;290(11):593–597. doi: 10.1056/NEJM197403142901104. [DOI] [PubMed] [Google Scholar]
- Frank L., Massaro D. Oxygen toxicity. Am J Med. 1980 Jul;69(1):117–126. doi: 10.1016/0002-9343(80)90509-4. [DOI] [PubMed] [Google Scholar]
- Fridovich I. Superoxide dismutases. Annu Rev Biochem. 1975;44:147–159. doi: 10.1146/annurev.bi.44.070175.001051. [DOI] [PubMed] [Google Scholar]
- Goldberg B., Stern A. Superoxide anion as a mediator of drug-induced oxidative hemolysis. J Biol Chem. 1976 Oct 25;251(20):6468–6470. [PubMed] [Google Scholar]
- HIRSCH J. G., COHN Z. A. Degranulation of polymorphonuclear leucocytes following phagocytosis of microorganisms. J Exp Med. 1960 Dec 1;112:1005–1014. doi: 10.1084/jem.112.6.1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homan-Müller J. W., Weening R. S., Roos D. Production of hydrogen peroxide by phagocytizing human granulocytes. J Lab Clin Med. 1975 Feb;85(2):198–207. [PubMed] [Google Scholar]
- Jackett P. S., Aber V. R., Lowrie D. B. Virulence and resistance to superoxide, low pH and hydrogen peroxide among strains of Mycobacterium tuberculosis. J Gen Microbiol. 1978 Jan;104(1):37–45. doi: 10.1099/00221287-104-1-37. [DOI] [PubMed] [Google Scholar]
- Kellogg E. W., 3rd, Fridovich I. Liposome oxidation and erythrocyte lysis by enzymically generated superoxide and hydrogen peroxide. J Biol Chem. 1977 Oct 10;252(19):6721–6728. [PubMed] [Google Scholar]
- Kellogg E. W., 3rd, Fridovich I. Superoxide, hydrogen peroxide, and singlet oxygen in lipid peroxidation by a xanthine oxidase system. J Biol Chem. 1975 Nov 25;250(22):8812–8817. [PubMed] [Google Scholar]
- Kinsman O. S., Arbuthnott J. P. Experimental staphylococcal infections in newborn mice: inhibition of weight gain as an index of virulence. J Med Microbiol. 1980 May;13(2):281–290. doi: 10.1099/00222615-13-2-281. [DOI] [PubMed] [Google Scholar]
- Klebanoff S. J. Antimicrobial mechanisms in neutrophilic polymorphonuclear leukocytes. Semin Hematol. 1975 Apr;12(2):117–142. [PubMed] [Google Scholar]
- LOWRY O. H., ROSEBROUGH N. J., FARR A. L., RANDALL R. J. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951 Nov;193(1):265–275. [PubMed] [Google Scholar]
- Lavelle F., Michelson A. M., Dimitrijevic L. Biological protection by superoxide dismutase. Biochem Biophys Res Commun. 1973 Nov 16;55(2):350–357. doi: 10.1016/0006-291x(73)91094-2. [DOI] [PubMed] [Google Scholar]
- MITCHISON D. A., SELKON J. B., LLOYD J. VIRULENCE IN THE GUINEA-PIG, SUSCEPTIBILITY TO HYDROGEN PEROXIDE, AND CATALASE ACTIVITY OF ISONIAZID-SENSITIVE TUBERCLE BACILLI FROM SOUTH INDIAN AND BRITISH PATIENTS. J Pathol Bacteriol. 1963 Oct;86:377–386. doi: 10.1002/path.1700860213. [DOI] [PubMed] [Google Scholar]
- McCord J. M., Fridovich I. Superoxide dismutase. An enzymic function for erythrocuprein (hemocuprein). J Biol Chem. 1969 Nov 25;244(22):6049–6055. [PubMed] [Google Scholar]
- McKay S. E., Arbuthnott J. P. Age-related susceptibility of mice to staphylococcal infection. J Med Microbiol. 1979 Feb;12(1):99–106. doi: 10.1099/00222615-12-1-99. [DOI] [PubMed] [Google Scholar]
- Melly M. A., Duke L. J., Liau D. F., Hash J. H. Biological properties of the encapsulated Staphylococcus aureus M. Infect Immun. 1974 Aug;10(2):389–397. doi: 10.1128/iai.10.2.389-397.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michelson A. M., Buckingham M. E. Effects of superoxide radicals on myoblast growth and differentiation. Biochem Biophys Res Commun. 1974 Jun 18;58(4):1079–1086. doi: 10.1016/s0006-291x(74)80254-8. [DOI] [PubMed] [Google Scholar]
- NAIR C. N., MACKAY-SCOLLAY E. M., RAMACHANDRAN K., SELKON J. B., TRIPATHY S. P., MITCHISON D. A., DICKINSON J. M. VIRULENCE IN THE GUINEA-PIG AND SUSCEPTIBLITY TO HYDROGEN PEROXIDE OF ISONIAZID-SENSITIVE TUBERCLE BACILLI FROM SOUTH INDIAN PATIENTS. Tubercle. 1964 Dec;45:345–353. doi: 10.1016/s0041-3879(64)80048-9. [DOI] [PubMed] [Google Scholar]
- Namavar F., de Graaff J., Veldhuizen R., Verhoef J. Proceedings: Netherlands Society for Microbiology meeting of the medical section at Bilthoven on 10 October 1974. Virulence of staphylococci in neonatal mice. Antonie Van Leeuwenhoek. 1975;41(2):211–211. doi: 10.1007/BF02565053. [DOI] [PubMed] [Google Scholar]
- Noble W. C. The production of subcutaneous staphylococcal skin lesions in mice. Br J Exp Pathol. 1965 Jun;46(3):254–262. [PMC free article] [PubMed] [Google Scholar]
- Paul B., Sbarra A. J. The role of the phagocyte in host-parasite interactions. 13. The direct quantitative estimation of H2O2 in phagocytizing cells. Biochim Biophys Acta. 1968 Feb 1;156(1):168–178. doi: 10.1016/0304-4165(68)90116-5. [DOI] [PubMed] [Google Scholar]
- ROGERS D. E., TOMPSETT R. The survival of staphylococci within human leukocytes. J Exp Med. 1952 Feb;95(2):209–230. doi: 10.1084/jem.95.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SBARRA A. J., KARNOVSKY M. L. The biochemical basis of phagocytosis. I. Metabolic changes during the ingestion of particles by polymorphonuclear leukocytes. J Biol Chem. 1959 Jun;234(6):1355–1362. [PubMed] [Google Scholar]
- Sinha A. K. Colorimetric assay of catalase. Anal Biochem. 1972 Jun;47(2):389–394. doi: 10.1016/0003-2697(72)90132-7. [DOI] [PubMed] [Google Scholar]
- Tally F. P., Goldin B. R., Jacobus N. V., Gorbach S. L. Superoxide dismutase in anaerobic bacteria of clinical significance. Infect Immun. 1977 Apr;16(1):20–25. doi: 10.1128/iai.16.1.20-25.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch D. F., Sword C. P., Brehm S., Dusanic D. Relationship between superoxide dismutase and pathogenic mechanisms of Listeria monocytogenes. Infect Immun. 1979 Mar;23(3):863–872. doi: 10.1128/iai.23.3.863-872.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ZUCKER-FRANKLIN D., HIRSCH J. G. ELECTRON MICROSCOPE STUDIES ON THE DEGRANULATION OF RABBIT PERITONEAL LEUKOCYTES DURING PHAGOCYTOSIS. J Exp Med. 1964 Oct 1;120:569–576. doi: 10.1084/jem.120.4.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Vijver J. C., van Es-Boon M. M., Michel M. F. A study of virulence factors with induced mutants of Staphylococcus aureus. J Med Microbiol. 1975 May;8(2):279–287. doi: 10.1099/00222615-8-2-279. [DOI] [PubMed] [Google Scholar]


