Abstract
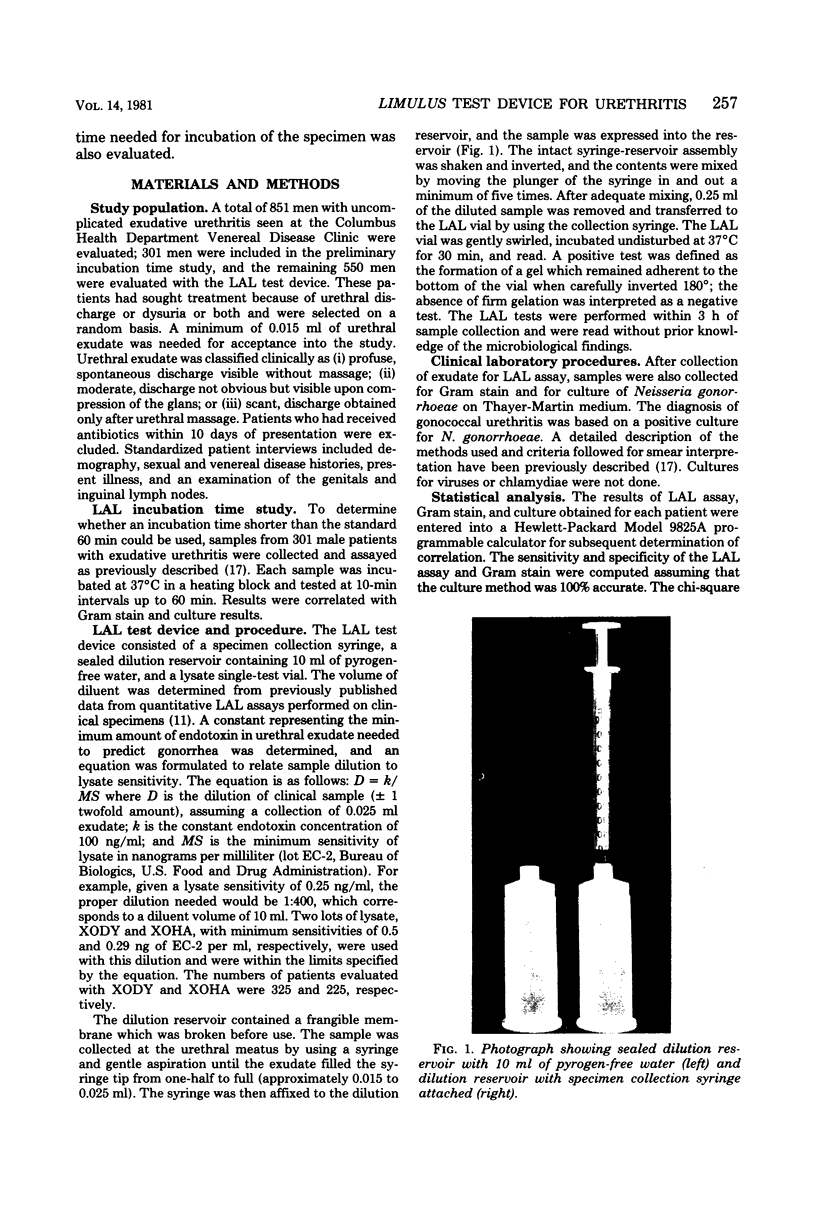
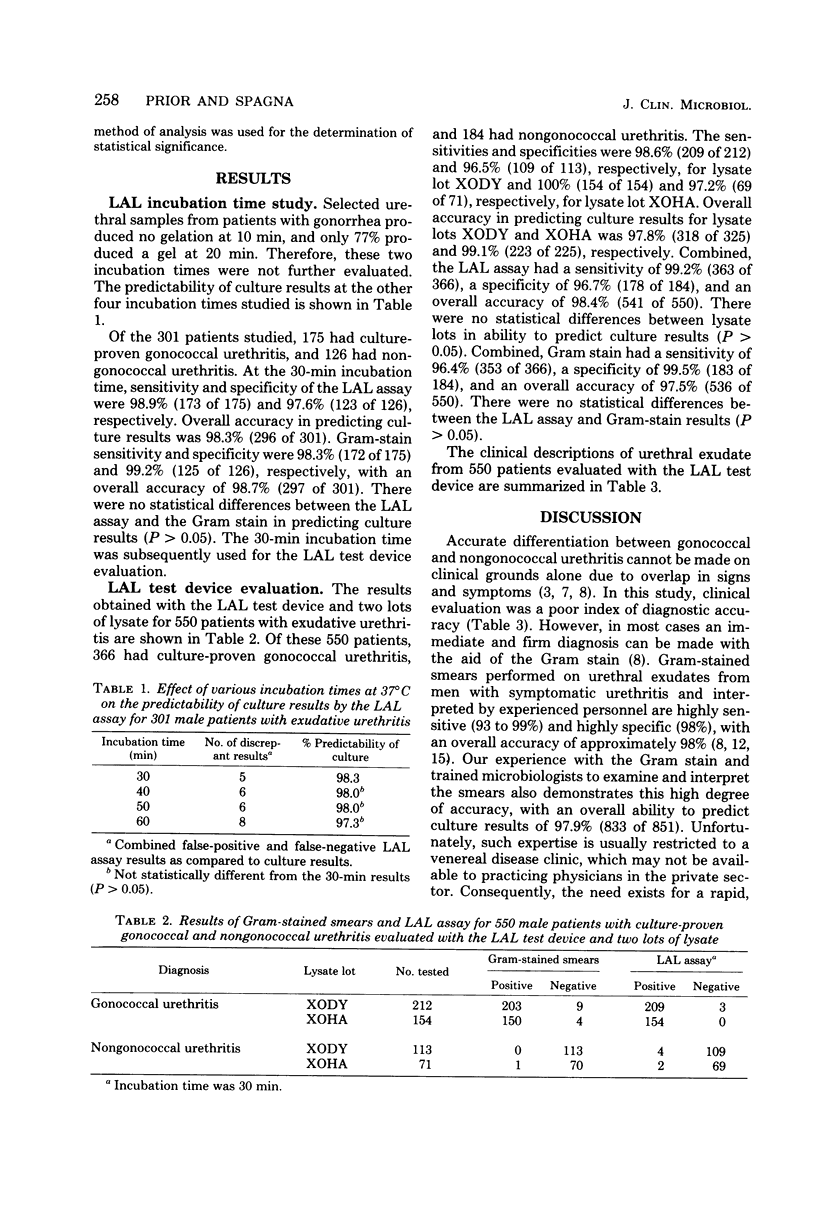
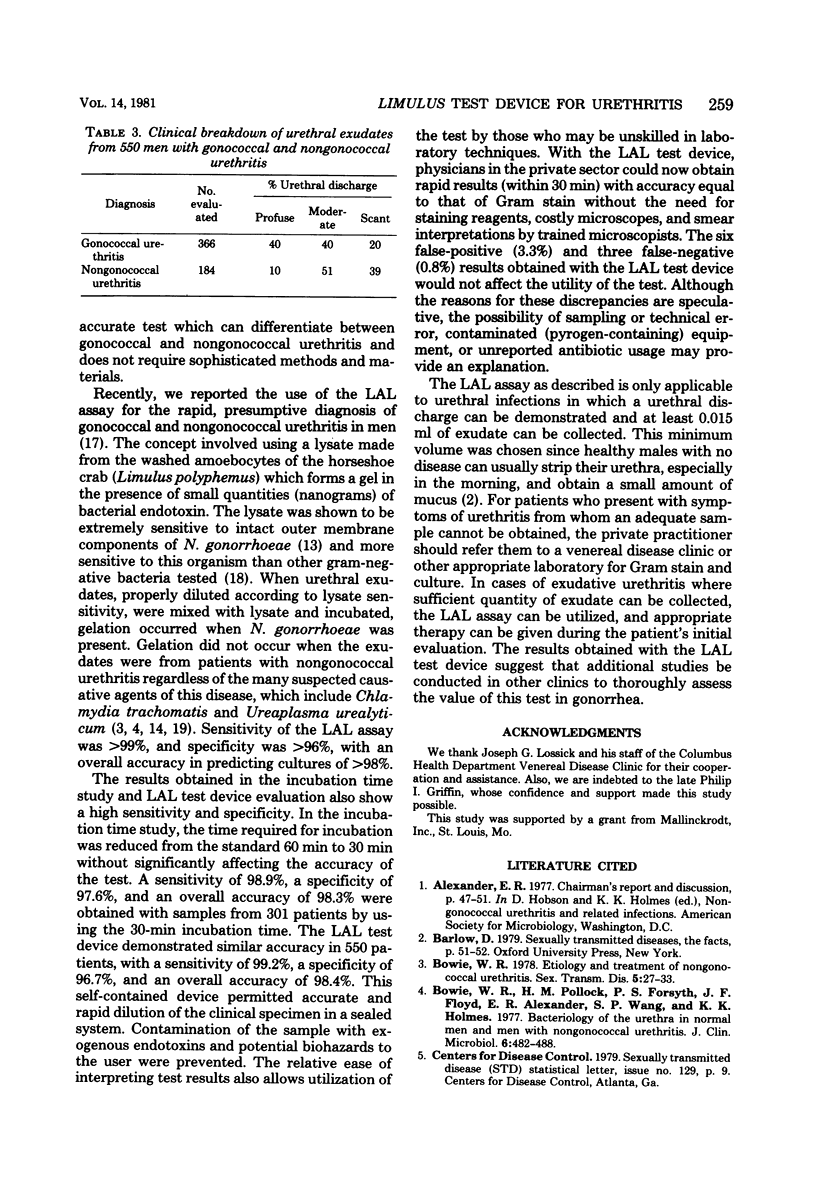
A test device incorporating Limulus amoebocyte lysate (Mallinckrodt, Inc., St. Louis, Mo.) was developed for the rapid, presumptive diagnosis of gonococcal and nongonococcal disease in males. The device, which was evaluated in 550 men with exudative urethritis, consisted of a specimen collection syringe, a dilution reservoir containing 10 ml of pyrogen-free water, and a Limulus amoebocyte lysate single-test vial. After specimen collection, the syringe was affixed to the dilution reservoir for rapid, accurate dilution of the clinical sample. Contamination of the specimen and potential biohazards to the user were prevented. The diluted sample was then transferred (via the collection syringe) to the lysate test vial for assay of endotoxin. Various incubation times at 37 degrees C were also studied in an additional 301 male patients, and time was reduced from the standard 60 to 30 min while still retaining equivalent predictability of culture results (P less than 0.05). Of the 550 males evaluated with the test device, 366 had positive cultures for Neisseria gonorrhoeae, and 184 were negative. A sensitivity of 99.2% and a specificity of 96.7% were obtained with the test device. Overall ability to predict culture results was 98.4%. Gram-stain sensitivity and specificity were 96.4% and 99.5%, respectively, with an overall accuracy of 97.5%. There were no statistical differences between the Limulus amoebocyte lysate test and Gram stain in predicting cultures (P less than 0.05). Thus, use of the Limulus amoebocyte lysate test device would enable the private physician to make an accurate, presumptive diagnosis of gonococcal and nongonococcal disease in males with exudative urethritis within 30 min without the need of a microscope and to initiate proper therapy during the patient's initial evaluation.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bowie W. R. Etiology and treatment of nongonococcal urethritis. Sex Transm Dis. 1978 Jan-Mar;5(1):27–33. doi: 10.1097/00007435-197801000-00009. [DOI] [PubMed] [Google Scholar]
- Bowie W. R., Pollock H. M., Forsyth P. S., Floyd J. F., Alexander E. R., Wang S. P., Holmes K. K. Bacteriology of the urethra in normal men and men with nongonococcal urethritis. J Clin Microbiol. 1977 Nov;6(5):482–488. doi: 10.1128/jcm.6.5.482-488.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming W. L., Brown W. J., Donohue J. F., Branigin P. W. National survey of venereal disease treated by physicians in 1968. JAMA. 1970 Mar 16;211(11):1827–1830. [PubMed] [Google Scholar]
- Handsfield H. H. Gonorrhea and nongonococcal urethritis. Recent advances. Med Clin North Am. 1978 Sep;62(5):925–943. doi: 10.1016/s0025-7125(16)31747-3. [DOI] [PubMed] [Google Scholar]
- Jacobs N. F., Kraus S. J. Gonococcal and nongonococcal urethritis in men. Clinical and laboratory differentiation. Ann Intern Med. 1975 Jan;82(1):7–12. doi: 10.7326/0003-4819-82-1-7. [DOI] [PubMed] [Google Scholar]
- Prior R. B., Spagna V. A. Comparative evaluation of the tube and microdilution Limulus lysate techniques for rapid presumptive diagnosis of gonococcal urethritis in men. J Clin Microbiol. 1980 Apr;11(4):340–342. doi: 10.1128/jcm.11.4.340-342.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prior R. B., Spagna V. A. Response of several Limulus amoebocyte lysates to native endotoxin present in gonococcal and nongonococcal urethral exudates from human males. J Clin Microbiol. 1981 Jan;13(1):167–170. doi: 10.1128/jcm.13.1.167-170.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riccardi N. B., Felman Y. M. Laboratory diagnosis in the problem of suspected gonococcal infection. JAMA. 1979 Dec 14;242(24):2703–2705. [PubMed] [Google Scholar]
- Rice P. A., Kasper D. L. Characterization of gonococcal antigens responsible for induction of bactericidal antibody in disseminated infection. J Clin Invest. 1977 Nov;60(5):1149–1158. doi: 10.1172/JCI108867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Root T. E., Edwards L. D., Spengler P. J. Nongonococcal urethritis: a survey of clinical and laboratory features. Sex Transm Dis. 1980 Apr-Jun;7(2):59–65. [PubMed] [Google Scholar]
- Rothenberg R. B., Simon R., Chipperfield E., Catterall R. D. Efficacy of selected diagnostic tests for sexually transmitted diseases. JAMA. 1976 Jan 5;235(1):49–51. [PubMed] [Google Scholar]
- Spagna V. A., Prior R. B., Perkins R. L. Rapid presumptive diagnosis of gonococcal cervicitis by the limulus lysate assay. Am J Obstet Gynecol. 1980 Jul 1;137(5):595–599. doi: 10.1016/0002-9378(80)90702-4. [DOI] [PubMed] [Google Scholar]
- Spagna V. A., Prior R. B., Perkins R. L. Rapid presumptive diagnosis of gonococcal urethritis in men by the limulus lysate test. Br J Vener Dis. 1979 Jun;55(3):179–182. doi: 10.1136/sti.55.3.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spagna V. A., Prior R. B. The Limulus amebocyte lysate assay. Am Fam Physician. 1980 Sep;22(3):125–128. [PubMed] [Google Scholar]
- Swartz S. L., Kraus S. J., Herrmann K. L., Stargel M. D., Brown W. J., Allen S. D. Diagnosis and etiology of nongonococcal urethritis. J Infect Dis. 1978 Oct;138(4):445–454. doi: 10.1093/infdis/138.4.445. [DOI] [PubMed] [Google Scholar]
- Willcox R. R. How suitable are available pharmaceuticals for the treatment of sexually transmitted diseases? 1: Conditions presenting as genital discharges. Br J Vener Dis. 1977 Oct;53(5):314–323. doi: 10.1136/sti.53.5.314. [DOI] [PMC free article] [PubMed] [Google Scholar]