Abstract
Background: previous studies have suggested a decline in the relationship between socioeconomic circumstances and health or functioning in later life, but this may be due to survival effects.
Objective: to examine whether wealth gradients in the incidence of illness decline with age, and, if so, whether this decline is explained by differential mortality.
Methods: the study included participants in the first two waves of the English Longitudinal Study of Ageing (ELSA), a large national longitudinal study of the population aged 50+ in England, who reported good health, no functional impairment, or no heart disease at baseline. Wealth inequalities in onset of illness over 2 years were examined across age groups, with and without the inclusion of mortality. Outcome measures were functional impairment, heart disease, self-reported health, and all-cause mortality (in conjunction with self-reported health and disability) or circulatory-related mortality (in relation to heart disease).
Results: wealth predicted onset of functional impairment equally across age groups. For self-reported health and heart disease, wealth gradients in the onset of illness declined with age. Selective mortality contributed to this decline in the oldest age groups.
Conclusions: socioeconomic inequality in developing new health problems persist into old age for certain illnesses, particularly functional impairment, but not for heart disease. Selective mortality explains only some of the decline in health inequalities with age.
Keywords: health inequalities, ageing, selective mortality
Introduction
Studies of socioeconomic inequalities in health in later life have had less consistent findings than similar studies of working age individuals. Many cross-sectional studies suggest a decline in the relationship between socioeconomic circumstances and health or functioning in later life [1–5] although Ross and Wu found that educational differences in health increased with increasing age [6]. Some longitudinal studies have shown that socioeconomic inequalities in health peak in late middle age and decline thereafter [7–13]. Declining strength of health inequalities in later life may be explained by selective mortality. A preponderance of premature mortality among disadvantaged respondents may dilute the ability of socioeconomic indicators to predict illness in later life, giving the appearance of a narrowing of health inequalities with age [14]. Only two previous studies have addressed the question of mortality selection as an explanation for the reduction in health inequalities with age in later life, and both found that the diminishing relationship between education and health in later life was not due to selective mortality [11, 12]. No previous studies of survival effects on age patterns in health inequalities in later life have been conducted outside the United States.
In addition to the effect of selective mortality, the declining association between socioeconomic circumstances and health with age raises questions about the most appropriate measures of social position in older age. Class, income and education have each been used to examine health inequalities in later life, and each of these is potentially problematic as a measure of socioeconomic position among retirees [15, 16]. For older individuals, accumulated wealth is likely to be the most useful indicator of lifetime economic status with past education, past occupation or pension income reflecting only part of the economic resources they can draw upon [17, 18].
In this study, we investigate survival effects on age patterns in the relationship between socioeconomic circumstances and health using a sample of English people aged 50 and over. First, we examine whether the strength of the relationship between wealth and onsets of new illness declines with age by examining wealth inequalities in deterioration of general health, the onset of functional impairment and incidence of ischaemic heart disease over a 2-year period. Second, we investigate whether any decline in the strength of the relationship between wealth and health is explained by differential mortality, by including deaths in the analysis of the onset of illness.
Methods
Sample
Data were taken from the first two waves of the English Longitudinal Study of Ageing (ELSA). ELSA is a panel study of people living in England who were aged 50 or over at baseline and had previously responded to the Health Survey for England (a nationally representative cross-sectional household survey). The baseline ELSA interview was conducted in 2002 and achieved a response rate of 67%. The follow-up interview was conducted in 2004 and achieved a response rate of 82% [19]. Ethical approval for ELSA was obtained from the North Thames Multi-centre Research Ethics Committee.
We selected individuals who completed a follow-up interview and were free of the disease in question at baseline for each of the three health outcomes examined. This resulted in slightly different samples for each of the three health outcomes: 6,371 for self-reported health, 6,911 for physical functioning and 7,171 for heart disease. These sample sizes increased when we added respondents who had died over the 2 years between baseline and follow-up. At follow-up, 204 of those who had good reported health at baseline and 246 of those who reported no functional impairment at baseline had died (from any cause), while 134 people without heart disease at baseline had died from diseases related to the circulatory system.
Measures
Health outcome measures
Three indicators of health were examined: self-reported health, functional impairment and heart disease. Response categories for self-reported health were ‘excellent’, ‘very good’, ‘good’, ‘fair’ and ‘poor’. Respondents who reported good health or better at baseline and fair or poor health at follow-up were considered to have an onset of poor reported health. Functional impairment was measured using six Activities of Daily Living (ADLs): bathing or showering, dressing oneself, getting in and out of bed, walking across a room, using the toilet and feeding oneself. Respondents reporting no difficulty at baseline but one or more at follow-up were considered to have an onset of functional impairment. Respondents were considered to have an onset of heart disease if they reported either a diagnosis of angina or MI or symptoms of MI (defined by the Rose angina questionnaire) at follow-up but not at baseline.
Mortality
Participants were ‘flagged’ with the NHS Central Register, run by the Office for National Statistics, which tracks death registrations. In relation to self-reported health and functional impairment, all-cause mortality is used. In relation to heart disease, deaths from circulatory diseases were used, defined as those in chapter I of the ICD-10.
Socioeconomic circumstances
Wealth is the main socioeconomic measure used, as it is considered to capture financial and other resources at older ages more accurately than the traditional measures of occupational class, income and tenure [17, 18]. Supplementary analyses (available at Age and Ageing online) include income and housing tenure in order to aid comparisons with previous work.
Wealth
Total non-pension net wealth for the household was collected at the baseline interview. The calculation of wealth is net of debt and includes value of home and other property (less mortgage), financial assets covering all the types of savings available in England, value of business assets (e.g. ownership or part ownership of business) and physical wealth such as artworks and jewellery. Information was obtained from over 95% of respondents for over 90% of the questions about wealth and from over 80% for the remaining wealth items. This high response rate was produced by using the ‘unfolding brackets’ technique, whereby respondents who are unable or refuse to give an exact answer receive a series of follow-up questions designed to elicit a range, as narrow as possible, within which the value lies. For our analyses, wealth quintiles based on the whole sample are used (age patterns in wealth gradients are similar if age-specific wealth quintiles are used) and pension wealth is omitted since it simply reflects annuitised pension income.
Income
Income is defined as total net income for the household at baseline and is the sum of income from employment, pension (private and state), other benefits, assets and any other source.
Housing tenure
Categories of housing tenure at baseline are outright ownership, buying homes with a mortgage or loan (including shared ownership: paying part rent and part mortgage) and renting (including people who report living rent free).
Age
Age of the respondent at baseline is used and broken into 5-year age groups.
Analytical techniques
First, the onset of disease was calculated by wealth quintiles within 5-year age groups; odds ratios and 95% confidence intervals for the socioeconomic trend within each age group were calculated using logistic regression. Next, the analysis was repeated with deaths combined with disease onset to give incidence of death or onset by wealth quintiles for each 5-year age group (following the recommendations of Diehr and colleagues [14]). The term ‘wealth gradient’ will be used and refers to the odds ratios (and 95% confidence intervals) of the health outcome for those in a particular wealth quintile relative to the odds for those belonging to the next (richer) quintile. This assumes that the relative odds are the same whether one is comparing the poorest and next poorest quintiles or the second wealthiest and richest quintiles. The estimate is obtained by treating wealth quintile as a continuous variable in a logistic regression equation. The analyses in this paper are supplemented by tables showing differences in proportions in the onset of illness (since small odds ratios can mask a large absolute difference and vice versa) and also identical analyses using household income and housing tenure rather than wealth, on the journal website (http://www.ageing.oxfordjournals.org/). Analysis conducted separately for men and women showed no significant differences in the findings, so men and women were combined. All analysis was conducted in SPSS version 12.
Results
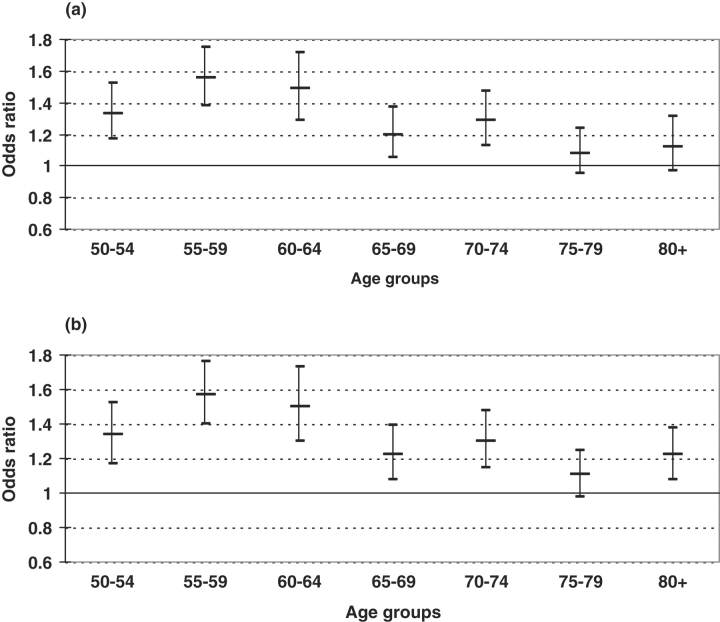
Self-reported health
Overall, 14.8% of people in good health at baseline had an onset of poor reported health in the 2 years between baseline and follow-up. Figure 1a shows the wealth gradient for each age group. A significant inverse wealth gradient in the onset of reporting poor health appears up to age 75. Among people aged 75 and over there is no significant wealth gradient in the onset of reporting poor health.
Figure 1.
(a) Odds ratio for wealth gradient in the onset of reporting fair or poor health over a 2-year period. (b) Odds ratio for wealth gradient in the onset of reporting fair or poor health or death over a 2-year period.
The addition of mortality strengthens the gradient for people age 80 and over, with the odds ratio for this group increasing from 1.12 (0.97–1.31) before the inclusion of mortality to 1.22 (1.08–1.38) after (Figure 1b). Otherwise, the odds ratios of the gradient for each age group were almost identical in Figure 1a and b. (A similar pattern for absolute differences in the wealth gradient for these outcomes is shown in supplementary table 1a and b available at Age and Ageing online.)
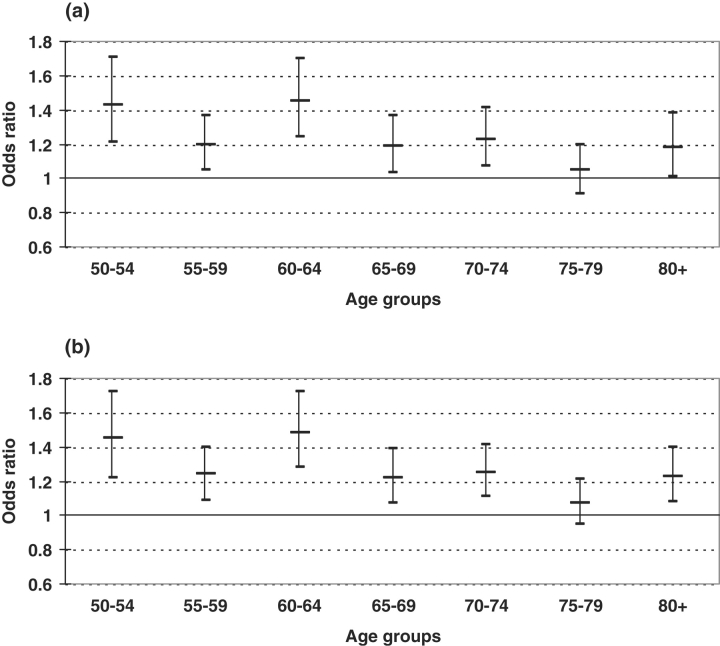
Functional impairment
Overall, 10.4% of respondents without impairment at baseline had an onset of functional impairment. Figure 2a shows that a significant inverse wealth gradient in the onset of functional impairment exists in all age groups except those aged 75–79.
Figure 2.
(a) Odds ratio for wealth gradient in the onset of reporting difficulty with 1+ ADL over a 2-year period. (b) Odds ratio for wealth gradient in the onset of reporting difficulty with 1+ ADL or death over a 2-year period.
As with self-reported health, the inclusion of mortality with the onset of functional impairment only influenced the strength of the wealth gradient for those aged 80 and over, with the odds ratio for this group increasing from 1.18 (1.01–1.38) before the inclusion of mortality to 1.23 (1.08–1.40) after (Figure 2b). Overall, the inclusion of mortality had very little influence on the age patterns in the relationship between wealth and incident functional impairment. (Absolute differences in the wealth gradient in the onset of functional impairment by age were similar, see supplementary Table 2a and b available at Age and Ageing online).
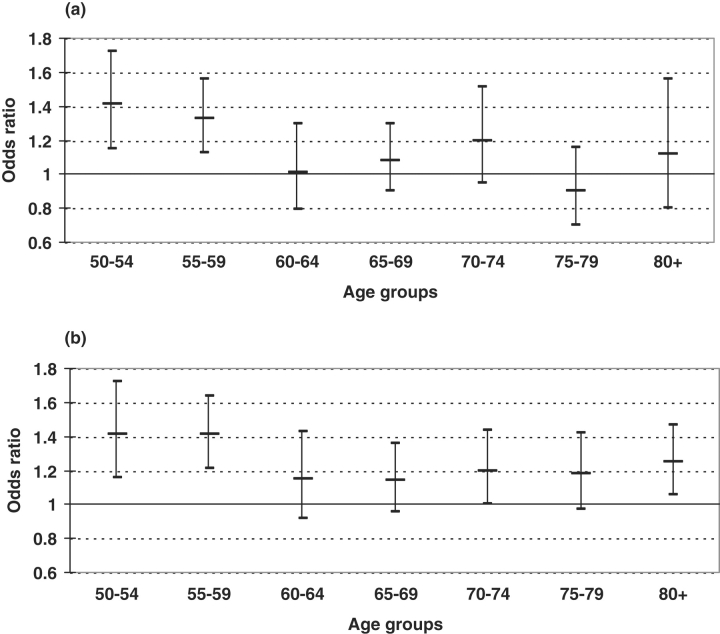
Heart disease
Between the 2 years between baseline and follow-up, 4.5% of people without IHD at baseline had an onset of heart disease. Figure 3a shows that the inverse wealth gradient in incidence of heart disease is only present for people in their fifties.
Figure 3.
(a) Odds ratio for wealth gradient in incidence of IHD over a 2-year period. (b) Odds ratio for wealth gradient in incidence of IHD or circulatory-related death over a 2-year period.
The inclusion of circulatory-related deaths with new cases of heart disease increased the strength of the wealth gradient in incident heart disease substantially for the two oldest age groups as well as for those aged 60–64 years (Figure 3b). For example, in the oldest age group, the odds ratio for the wealth gradient in incident heart disease increased from 1.12 (0.80–1.56) to 1.25 (1.06–1.47) when circulatory-related deaths were included, and from 1.01 (0.79–1.30) to 1.15 (0.92–1.43) for people in their early sixties. The odds ratio for the gradient in incident heart disease also became statistically significant for those aged 70–74 years. (For absolute differences in incidence of heart disease between those in the poorest and richest wealth quintiles by age, see supplementary Table 3a and b available at Age and Ageing online).
Tenure and income
Supplementary analyses showed that housing tenure behaved very similarly to wealth in its relationships with the onset of illness across age groups. With the exception of relative differences in onsets of poor reported health, income gradients in onsets of illness were much weaker than those for wealth or tenure, and the inclusion of mortality did not influence income gradients in any illness onset (see supplementary Tables 1a–3b and supplementary Figures 1a–3d available at Age and Ageing online).
Discussion
This study examined whether socioeconomic inequalities in the onset of illness declined with age, and, if so, whether this decline was explained by differential mortality. Wealth predicted onsets of new cases of functional impairment over a 2-year period fairly equally across age groups, while the strength of the relationship between wealth and onsets of illness was reduced from age 75 for self-reported health and from age 60 for heart disease. The lack of a wealth gradient in poor reported health that we see in the oldest age groups is in line with most previous studies of general health regardless of the socioeconomic measure chosen [7]. Chandola and colleagues found that self-reported health differentials by occupational grade increased with age, but inequality was only examined up to age 74 [20]. Our decreasing wealth gradient in incident heart disease is also similar to the pattern seen for self-reported health although stronger and beginning at the younger age of 60 years. The persistence of a wealth gradient in functional impairment in the oldest age groups is at odds with previous studies that have used other socioeconomic measures [10, 13] although our analysis of income gradients have some similarities with these findings. The differing results shown here for wealth (and tenure) may reflect that they more accurately represent socioeconomic position in later life. In a more recent study, Matthews and colleagues also found housing tenure to predict disability-free life expectancy better than income [21].
However, these studies were conducted amongst survivors only. Adding mortality into the analysis of onsets of illness increased the size of the wealth gradient in the oldest age groups in our study. The influence of mortality on age patterns was most dramatic for wealth differences in incident heart disease. The two previous studies to examine survival selection effects on converging health inequalities in later life both found that education differences in the prevalence of health problems or disability [11, 12] decreased with increasing age after respondents were in their early sixties even after including deaths in their analysis. Our results are broadly similar to previous results for general health and functional impairment in finding a small survival effect in the very oldest age group. In our study, the greatest survival effect was seen for incident heart disease, which does not appear to have been examined in previous work.
Selection bias may be a limitation in our study. The baseline sample excludes people in long-term care, was composed only of people who reported being well, and we know that attrition between the 2 years of the study was greater among those in more disadvantaged households [17]. Each of these factors may underestimate disease incidence among the poorer households relative to the richer, but would not necessarily influence age patterns in these inequalities. Another limitation is our inability to separate age from period or cohort effects in examining age differences over a 2-year period. Relationships between socioeconomic circumstances and health reflect complex life course processes that cannot be captured by the data used here. The life experiences of the youngest ELSA members are likely to differ substantially from those of the oldest.
In conclusion, to our knowledge, this is the only study to combine detailed wealth, health and mortality data to examine age patterns and the influence of selective mortality on health inequalities in a large study of older people in England. This study has shown that socioeconomic inequality in developing new health problems declines with age for certain illnesses, but not for the onset of functional impairment. Selective mortality appears to explain some of the decline in health inequalities at older ages, particularly in relation to heart disease.
Key points
Cross-sectional studies suggest that health inequalities decrease with increasing age. Results from longitudinal studies are inconsistent, but none of them take differential mortality into account. Disadvantaged people die younger than people in advantage socioeconomic circumstances. This may artificially weaken socioeconomic inequalities in health in later life.
- This study shows that:
- Wealth inequalities in new cases of heart disease and poor reported health decline with age.
Wealth inequalities in the onset of functional impairment remain constant with age.
Differential mortality contributes to the decrease in wealth inequalities with age in the oldest age groups.
Supplementary Material
Conflicts of interest
There are no conflicts of interest.
Funding
ESRC funding the project ‘Inequalities in health in an ageing population: patterns, causes and consequences’ (RES-000-23-0590) supported the work on this paper. The funding for ELSA is provided by the National Institute of Aging in the United States, and a consortium of UK Government departments coordinated by the Office for National Statistics. The developers and funders of ELSA do not bear any responsibility for the analyses or interpretations presented here.
Supplementary data
Supplementary data are available at Age and Ageing online.
References
- 1.Blaxter M. Health and Lifestyles. London: Tavistock/ Routledge; 1990. [Google Scholar]
- 2.Damian J, Ruigomez A, Pastor V, Martin-Moreno JM. Determinants of self assessed health among Spanish older people living at home. J Epidemiol Community Health. 1999;53:412–16. doi: 10.1136/jech.53.7.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steel N, Huppert FA, McWilliams B, Melzer D. Physical and cognitive function. In: Marmot M, Banks J, Blundell R, Lessof C, Nazroo J, editors. Health, Wealth and Lifestyles of the Older Population in England: The 2002 English Longitudinal Study of Ageing. London: Institute for Fiscal Studies; 2003. pp. 249–300. [Google Scholar]
- 4.Smith KV, Goldman N. Socioeconomic differences in health among older adults in Mexico. Soc Sci Med. 2007;65:1372–85. doi: 10.1016/j.socscimed.2007.05.023. [DOI] [PubMed] [Google Scholar]
- 5.Merlo J, Gerdtham U-G, Lynch J, Beckman A, Norlund A, Lithman T. Social inequalities in health—do they diminish with age? Revisiting the question in Sweden 1999. Int J Equity Health. 2003;2:2–6. doi: 10.1186/1475-9276-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ross CE, Wu C. Education, age, and the cumulative advantage in health. J Health Soc Behav. 1996;37:104–120. [PubMed] [Google Scholar]
- 7.Mishra GD, Ball K, Dobson AJ, Byles JE. Do socioeconomic gradients in women's health widen over time and with age? Soc Sci Med. 2004;58:1585–95. doi: 10.1016/S0277-9536(03)00368-X. [DOI] [PubMed] [Google Scholar]
- 8.Wray LA, Alwin DF, McCammon RJ. Social status and risky health behaviors: results from the health and retirement study. J Gerontol. 2005;60B:85–92. doi: 10.1093/geronb/60.special_issue_2.s85. [DOI] [PubMed] [Google Scholar]
- 9.Deaton AS, Paxson CH. Aging and inequality in income and health. Am Econ Rev. 1998;88:248–53. [Google Scholar]
- 10.House JS, Lantz PM, Herd P. Continuity and change in the social stratification of aging and health over the life course: evidence from a nationally representative longitudinal study from 1986 to 2001/2002 (Americans’ Changing Lives Study) J Gerontol. 2005;60B:15–26. doi: 10.1093/geronb/60.special_issue_2.s15. [DOI] [PubMed] [Google Scholar]
- 11.Herd P. Do functional health inequalities decrease in old age? Educational status and functional decline among the 1931–1941 birth cohort. Res Aging. 2006;28:375–92. [Google Scholar]
- 12.Beckett M. Converging health inequalities in later life—an artifact of mortality selection? J Health Soc Behav. 2000;41:106–119. [PubMed] [Google Scholar]
- 13.Matthews RJ, Smith LK, Hancock RM, Jagger C, Spiers NA. Socioeconomic factors associated with the onset of disability in older age: a longitudinal study of people aged 75 years and over. Soc Sci Med. 2005;61:1567–75. doi: 10.1016/j.socscimed.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 14.Diehr P, Patrick DL, Johnson LL, Psaty B. Incorporating death into health-related variables in longitudinal studies. University of Washington Biostatistics Working Paper Series, 2004; 224. http://www.bepress.com/uwbiostat/paper224 .
- 15.Marmot MG, Shipley M. Do socioeconomic differences in mortality persist after retirement? 25-year follow-up of civil servants from the Whitehall study. BMJ. 1996;313:117–80. doi: 10.1136/bmj.313.7066.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spiers N, Matthews R, Barker G, Jagger C, Hancock R. Standard of living in the retirement survey: a predictor of six-year functional limitation onset and mortality in women, but not in men from ages 55–69 years. Disabil Rehabil. 2005;27:1415–23. doi: 10.1080/09638280500164347. [DOI] [PubMed] [Google Scholar]
- 17.Banks J, Karlsen S, Oldfield Z. Socio-economic position. In: Marmot M, Banks J, Blundell R, Lessof C, Nazroo J, editors. Health, Wealth and Lifestyles of the Older Population in England: The 2002 English Longitudinal Study of Ageing. London: Institute for Fiscal Studies; 2003. pp. 71–125. [Google Scholar]
- 18.Robert S, House JS. SES differentials in health by age and alternative indicators of SES. J Aging Health. 1996;8:359–88. doi: 10.1177/089826439600800304. [DOI] [PubMed] [Google Scholar]
- 19.Cheshire H, Cox K, Lessof C, Taylor R. Methodology. In: Banks J, Breeze E, Lessof C, Nazroo J, editors. Retirement, Health and Relationships of the Older Population in England: The 2004 English Longitudinal Study of Ageing. London: Institute for Fiscal Studies; 2006. pp. 367–83. [Google Scholar]
- 20.Chandola T, Ferrie J, Sacker A, Marmot M. Social inequalities in self reported health in early old age: follow-up of prospective cohort study. BMJ. 2007;334:990–96. doi: 10.1136/bmj.39167.439792.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matthews R, Jagger C, Hancock RM. Does socio-economic advantage lead to a longer, healthier old age? Soc Sci Med. 2006;62:2489–99. doi: 10.1016/j.socscimed.2005.11.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.