Abstract
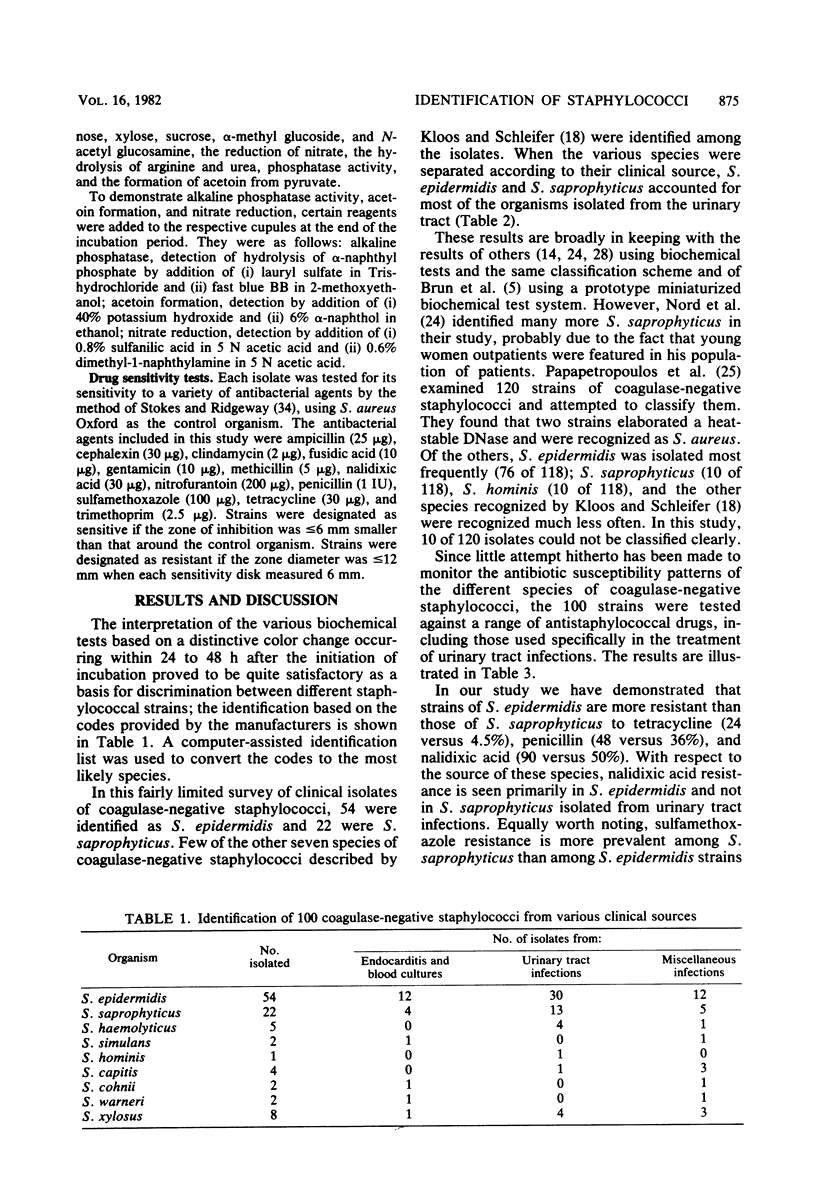
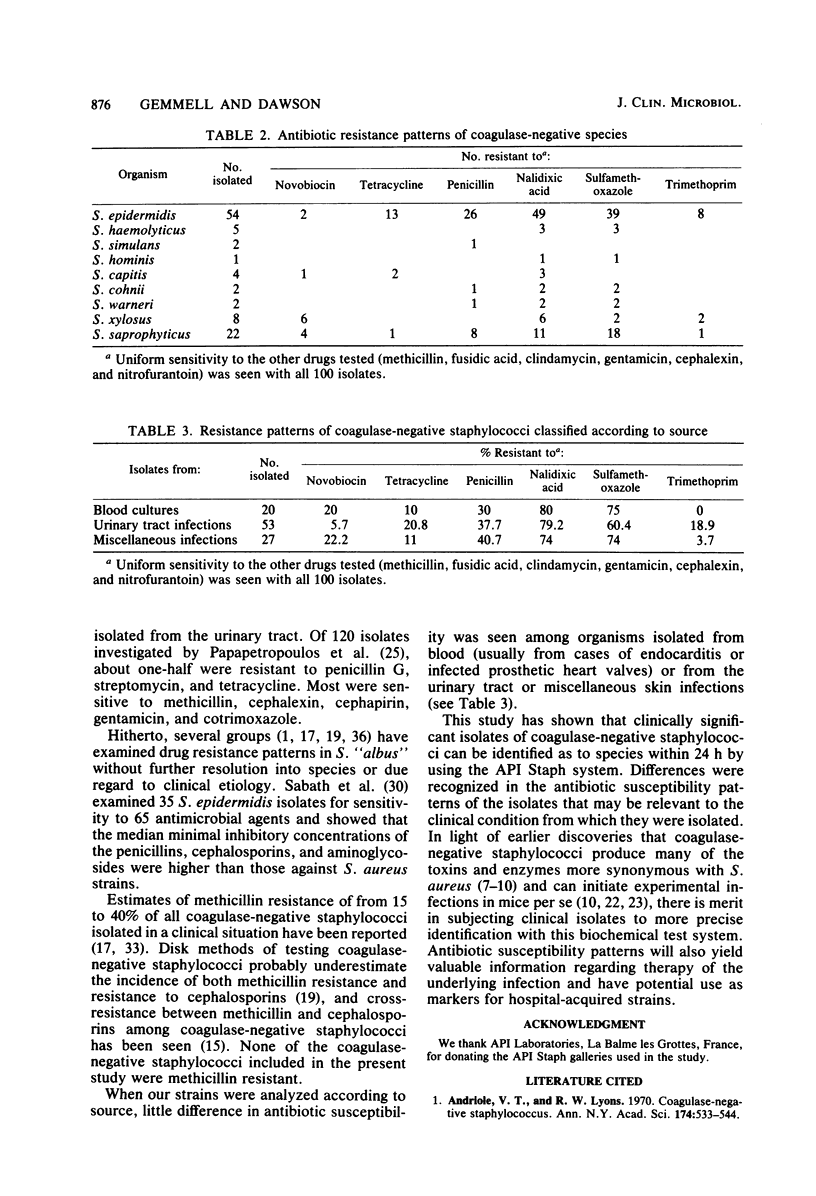
A kit for the identification of staphylococci based on the biochemical criteria proposed by Kloos and Schleifer (W.E. Kloos and K.H. Schleifer, J. Clin. Microbiol., 1:82-88, 1975) is now available commercially. The system was used to identify 100 strains of coagulase-negative staphylococci isolated from various body sites as the primary etiological agent of clinical infection. The increasing importance of staphylococci and their resistance to antibiotics provided the rationale for such an investigation. Over 90% of the Staphylococcus isolates were easily identified as to their species on the basis of their reaction profile to 19 biochemical tests included in the kit. The remainder, which showed minor variations, could also be assigned to the various species. Identification of the isolates was as follows: S. epidermidis, 54; S. haemolyticus, 5; S. simulans, 2; S. hominis, 1; S. capitis, 4; S. cohnii, 2; S. warneri, 2; S. xylosus, 8; and S. saprophyticus, 22. Antibiotic sensitivity patterns were determined for each of the isolates. Novobiocin resistance was detected in strains of S. saprophyticus and S. xylosus, a property hitherto recognized in Micrococcus sp. type 3 causing bacteriuria in young women. Resistance to penicillin was widespread among strains of several species, whereas resistance to tetracycline was mainly confined to strains of S. epidermidis. General resistance to sulfamethoxazole and nalidixic acid was found among all strains, with almost uniform sensitivity to the other drugs tested.
Full text
PDF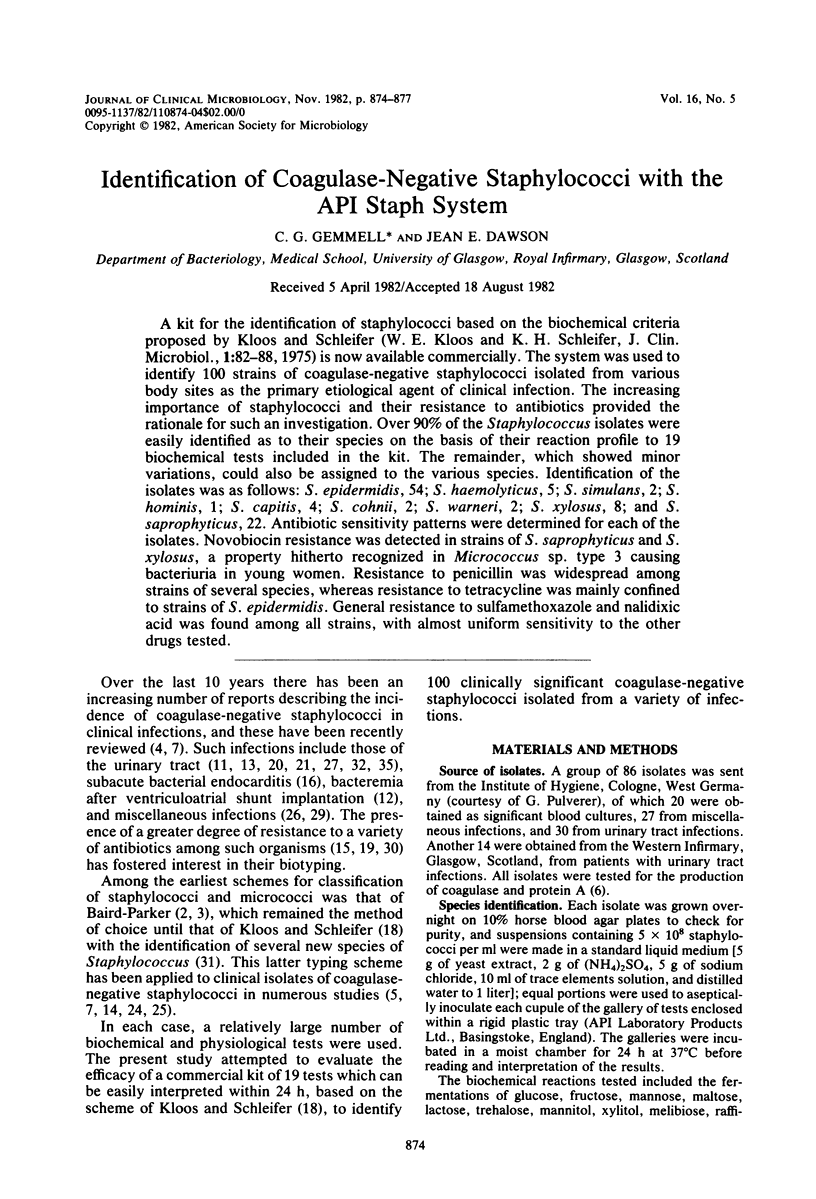

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andriole V. T., Lyons R. W. Coagulase-negative staphylococcus. Ann N Y Acad Sci. 1970 Oct 30;174(2):533–544. doi: 10.1111/j.1749-6632.1970.tb45579.x. [DOI] [PubMed] [Google Scholar]
- BAIRD-PARKER A. C. A classification of micrococci and staphylococci based on physiological and biochemical tests. J Gen Microbiol. 1963 Mar;30:409–427. doi: 10.1099/00221287-30-3-409. [DOI] [PubMed] [Google Scholar]
- BAIRD-PARKER A. C. THE CLASSIFICATION OF STAPHYLOCOCCI AND MICROCOCCI FROM WORLD-WIDE SOURCES. J Gen Microbiol. 1965 Mar;38:363–387. doi: 10.1099/00221287-38-3-363. [DOI] [PubMed] [Google Scholar]
- Brun Y., Fleurette J., Forey F. Micromethod for biochemical identification of coagulase-negative staphylococci. J Clin Microbiol. 1978 Nov;8(5):503–508. doi: 10.1128/jcm.8.5.503-508.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsgren A. Significance of protein a production by staphylococci. Infect Immun. 1970 Nov;2(5):672–673. doi: 10.1128/iai.2.5.672-673.1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gemmell C. G., Roberts E. Toxins and enzymes of coagulase negative staphylococci isolated from human infections. J Hyg Epidemiol Microbiol Immunol. 1974;18(3):276–280. [PubMed] [Google Scholar]
- Gemmell C. G. The staphylococcus--new features 100 years after its discovery. J Infect. 1982 Jan;4(1):5–15. doi: 10.1016/s0163-4453(82)90843-x. [DOI] [PubMed] [Google Scholar]
- Gemmell C. G., Thelestam M. Toxinogenicity of clinical isolates of coagulase-negative staphylococci towards various animal cells. Acta Pathol Microbiol Scand B. 1981 Dec;89(6):417–421. [PubMed] [Google Scholar]
- Gillespie W. A., Sellin M. A., Gill P., Stephens M., Tuckwell L. A., Hilton A. L. Urinary tract infection in young women, with special reference to Staphylococcus saprophyticus. J Clin Pathol. 1978 Apr;31(4):348–350. doi: 10.1136/jcp.31.4.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt R. The classification of staphylococci from colonized ventriculo-atrial shunts. J Clin Pathol. 1969 Jul;22(4):475–482. doi: 10.1136/jcp.22.4.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovelius B., Thelin I., Mårdh P. A. Staphylococcus saprophyticus in the aetiology of nongonococcal urethritis. Br J Vener Dis. 1979 Oct;55(5):369–374. doi: 10.1136/sti.55.5.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John J. F., Jr, Gramling P. K., O'Dell N. M. Species identification of coagulase-negative staphylococci from urinary tract isolates. J Clin Microbiol. 1978 Oct;8(4):435–437. doi: 10.1128/jcm.8.4.435-437.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John J. F., Jr, McNeill W. F. Activity of cephalosporins against methicillin-susceptible and methicillin-resistant, coagulase-negative staphylococci: minimal effect of beta-lactamase. Antimicrob Agents Chemother. 1980 Feb;17(2):179–183. doi: 10.1128/aac.17.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KJELLANDER J. O., KLEIN J. O., FINLAND M. IN VITRO ACTIVITY OF PENICILLINS AGAINST STAPHYLOCOCCUS ALBUS. Proc Soc Exp Biol Med. 1963 Aug-Sep;113:1023–1031. doi: 10.3181/00379727-113-28563. [DOI] [PubMed] [Google Scholar]
- Kloos W. E., Schleifer K. H. Simplified scheme for routine identification of human Staphylococcus species. J Clin Microbiol. 1975 Jan;1(1):82–88. doi: 10.1128/jcm.1.1.82-88.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laverdiere M., Peterson P., Verhoef J., Williams D. N., Sabath L. D. In vitro activity of cephalosporins against methicillin-resistant, coagulase-negative staphylococci. J Infect Dis. 1978 Mar;137(3):245–250. doi: 10.1093/infdis/137.3.245. [DOI] [PubMed] [Google Scholar]
- Maskell R. Importance of coagulase-negative staphylococci as pathogens in the urinary tract. Lancet. 1974 Jun 8;1(7867):1155–1158. doi: 10.1016/s0140-6736(74)90634-5. [DOI] [PubMed] [Google Scholar]
- Namavar F., De Graaff J., De With C., MacLaren D. M. Novobiocin resistance and virulence of strains of Staphylococcus saprophyticus isolated from urine and skin. J Med Microbiol. 1978 Aug;11(3):243–248. doi: 10.1099/00222615-11-3-243. [DOI] [PubMed] [Google Scholar]
- Papapetropoulos M., Pappas A., Papavassiliou J., Legakis N. J. Distribution of coagulase-negative staphylococci in human infections. J Hosp Infect. 1981 Jun;2(2):145–153. doi: 10.1016/0195-6701(81)90023-2. [DOI] [PubMed] [Google Scholar]
- Pead L., Crump J., Maskell R. Staphylococci as urinary pathogens. J Clin Pathol. 1977 May;30(5):427–431. doi: 10.1136/jcp.30.5.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabath L. D., Garner C., Wilcox C., Finland M. Susceptibility of Staphylococcus aureus and Staphylococcus epidermidis to 65 antibiotics. Antimicrob Agents Chemother. 1976 Jun;9(6):962–969. doi: 10.1128/aac.9.6.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrestha T. L., Darrell J. H. Urinary infection with coagulase-negative staphylococci in a teaching hospital. J Clin Pathol. 1979 Mar;32(3):299–302. doi: 10.1136/jcp.32.3.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siebert W. T., Moreland N., Williams T. W., Jr Methicillin-resistant Staphylococcus epidermidis. South Med J. 1978 Nov;71(11):1353–1355. doi: 10.1097/00007611-197811000-00011. [DOI] [PubMed] [Google Scholar]
- Wallmark G., Arremark I., Telander B. Staphylococcus saprophyticus: a frequent cause of acute urinary tract infection among female outpatients. J Infect Dis. 1978 Dec;138(6):791–797. doi: 10.1093/infdis/138.6.791. [DOI] [PubMed] [Google Scholar]
- Zygmunt W. A., Browder H. P., Tavormina P. A. Susceptibility of coagulase-negative staphylococci to lysostaphin and other antibiotics. Appl Microbiol. 1968 Aug;16(8):1168–1173. doi: 10.1128/am.16.8.1168-1173.1968. [DOI] [PMC free article] [PubMed] [Google Scholar]


