Abstract
Objective
To provide normative data for children tested with Early Treatment Diabetic Retinopathy Study (ETDRS) charts.
Design
Cross-sectional study.
Participants
252 Native American (Tohono O’odham) children 5 years through 12 years of age. Based on cycloplegic refraction conducted on the day of testing, all were emmetropic (myopia ≤ 0.25 diopter (D) spherical equivalent, hyperopia ≤ 1.00 D spherical equivalent, and astigmatism ≤ 0.50 D in both eyes).
Methods
Monocular visual acuity was tested at 4 m, using one ETDRS chart for the right eye (RE), and another for the left eye (LE).
Main Outcome Measure
Visual acuity was scored as the total number of letters correctly identified, by naming or by matching to letters on a lap card, and as the smallest letter size for which the child identified 3 of 5 letters correctly.
Results
Visual acuity results did not differ for the RE vs the LE, so data are reported for the RE only. Mean visual acuity for the 5-year-old group (0.16 logarithm of the minimum angle of resolution (logMAR) [20/29]) was significantly worse than for 8-, 9-, 10-, 11-, and 12-year-olds (0.05 logMAR [20/22] or better at each age). The lower 95% prediction limit for determining if a child has visual acuity within the normal range was 0.38 (20/48) for 5-year-olds and 0.30 (20/40) for 6–12-year-olds, which was reduced to 0.32 (20/42) for 5-year-olds and 0.21 (20/32) for 6–12-year-olds when recalculated with outlying data points removed. Mean interocular acuity difference did not vary by age, averaging less than 1 logMAR line at each age, with a lower 95% prediction limit of 0.17 log unit (1.7 logMAR lines) across all ages.
Conclusion
For monocular visual acuity based on ETDRS charts to be in the normal range, it must be better than 20/50 for 5-year-olds and better than 20/40 for 6–12-year-olds. Normal interocular acuity difference includes values of less than 2 logMAR lines. Normative ETDRS visual acuity values are not as good as norms reported for adults, suggesting that a child’s visual acuity results should be compared with norms based on data from children, not with adult norms.
In 1980, the Committee on Vision of the National Academy of Sciences–National Research Council recommended that visual acuity charts should use logarithmic scaling of the distance between letters on successive lines, logarithmic progression of lines, and the same number of letters on each line of the chart.1 The Early Treatment Diabetic Retinopathy Study (ETDRS) logarithm of the minimum angle of resolution (logMAR) charts2 meet these recommendations, and normative data are available for adults.3–5 However, although ETDRS charts have been used in studies of children as young as five years of age,6–9 only limited normative data are available for children ten years of age and younger,8,10–12 and no studies have examined whether norms vary with age in young children.
The purpose of the present study is to provide normative monocular visual acuity data for ETDRS charts for children who are five years through twelve years of age, and to determine if there is a developmental trend for improvement in normative visual acuity or in interocular acuity difference with age.
METHODS
Subjects
Subjects were 252 children between five and <13 years of age whose eye examination indicated they had no ocular pathology and whose cycloplegic refraction indicated that they were emmetropic, i.e., had ≤ 0.25 diopter (D) of myopia (spherical equivalent), ≤ 1.00 D of hyperopia (spherical equivalent), and ≤ 0.50 D of astigmatism in both eyes. The mean age of the subjects was 9.11 years (SD 2.16, range 5.17 to 12.96 years).
The 252 children who met the inclusion criteria represented 33.5% of 753 children who were participants in a prospective study of astigmatism-related amblyopia that enrolled astigmatic and non-astigmatic children in grades K-2 and 4–6 who attended one of five elementary schools on the Tohono O’odham Reservation in southern Arizona.7,8,13 Children in grades K-2 were examined during the 2003/2004 academic school year and children in grades 4–6 were examined during the 2001/2002 academic school year. Data are reported for the first study-related eye examination conducted on each child.
The research followed the tenets of the Declaration of Helsinki, was HIPAA compliant, and was approved by the Tohono O’odham Nation and by the Institutional Review Board of the University of Arizona. Parents provided written informed consent prior to testing.
Procedures
All children underwent an eye examination that was conducted at their school. Initially, monocular distance visual acuity was assessed at 4 m, using ETDRS logMAR charts (Precision Vision, Inc., La Salle, IL),2 mounted in a chart illuminator box (Precision Vision, La Salle, IL). An adhesive eye patch of 5-cm wide adhesive paper tape (3M Micropore, Minneapolis, MN) was placed over the child’s left eye (LE), and the visual acuity of the right eye (RE) was tested using ETDRS chart 1 (Precision Vision catalog item no. 2121). Testing began with the top line on the chart (20/200), and the child was asked to name, or to match to letters on a lap card, all letters on each line until they reached a line on which they could not correctly identify any of the 5 letters. Masking of adjacent lines or letters was not allowed, but the tester was permitted to place a pointer beneath a letter to direct the child’s attention to the letter. Visual acuity was recorded as the total number of letters correctly identified (letter by letter scoring), and also as the smallest letter size at which the child identified at least three of the five letters correctly (line by line scoring). Testing of the RE was followed by testing of the LE with ETDRS chart 2 (Precision Vision catalog item no. 2122). Visual acuity scores were converted to logMAR values prior to analyses.
Visual acuity testing was followed by assessment of eye alignment using the cover-uncover test at distance and near, measurement of refractive error 40 to 60 min after instillation of one drop of proparacaine (0.5%) and two drops of cyclopentolate (1%) in each eye, and examination of the external eye and the fundus for abnormalities.7,14 Cycloplegic refractive error was measured with the Retinomax K+ autorefractor (Nikon, Inc., Melville, NY, now manufactured by Righton Manufacturing Co., Tokyo), followed by verification of autorefractor measurements by an experienced retinoscopist (JMM) and, when possible, by subjective refinement, both under cycloplegia.14 The final estimate, i.e., the estimate confirmed by retinoscopy and, when possible, by subjective refinement, was used for determination of each subject’s refractive error.
Data Analysis
The primary analyses were conducted with visual acuity data scored based on the total number of letters identified correctly. Using the following formula, which assigns a value of 0.02 log unit to each letter identified, scores were transformed to logMAR values:
where Tc = the total number of letters identified correctly. This letter-by-letter scoring method provides better reliability of scores than does the line by line scoring.15 However, because in clinical settings visual acuity is often scored as the last line on which the patient identifies three letters correctly we also provide, in the Tables and Figure, data based on this line by line scoring method.
Separate repeated measures analyses of variance (RM-ANOVAs) were conducted to determine if there was a difference in acuity across age (separate analyses for RE (tested first) and LE), and differences in interocular acuity difference across age.
For visual acuity results and for interocular acuity difference results, 95% prediction limits16 were calculated to determine the visual acuity or the interocular acuity difference value that would indicate that a newly-tested individual’s score was within normal limits with 95% probability. A visual acuity score below the lower 95% prediction limit would indicate a below-normal acuity score, and an interocular acuity difference greater than the lower 95% prediction limit would indicate an abnormally large difference in visual acuity between eyes. The formula used for the 95% prediction limits was:
where tα/2 = two-tailed value for alpha of 0.05 from the Student’s t distribution, n = number of subjects, and SD = standard deviation.
RESULTS
Monocular Visual Acuity
RM-ANOVAs revealed no significant difference in visual acuity between RE (tested first) and LE (tested second) as a function of the child’s age, and no interaction between eye and age (all p > 0.05). There was also no systematic tendency for acuity to be better in the RE or the LE, with mean differences between eyes of 0.03, −0.01, −0.01, −0.01, −0.03, 0, −0.01, and −0.04 log unit (positive numbers indicate better LE acuity and negative numbers indicate better RE acuity) at 5 to <6, 6 to <7, 7 to <8, 8 to <9, 9 to <10, 10 to <11, and 11 to <12 years, and 12 to <13 years, respectively. Therefore, visual acuity data are presented for RE only.
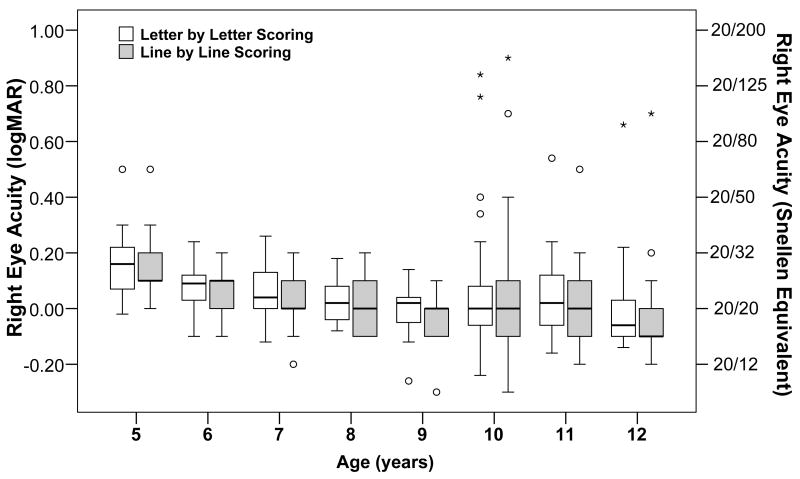
Table 1 and Figure 1 present VA results, grouped by age. ANOVA showed a significant effect of age on mean visual acuity (F(7,244) = 4.42, p<0.001). Post hoc analysis (with Bonferroni correction) indicated a significant difference between visual acuity in the five-year age group and visual acuity in the eight-(p<0.02), nine- (p<0.001), ten- (p<0.02), eleven- (p<0.008), and twelve-(p<0.002) year age groups, but no other significant age differences.
Table 1.
Mean and standard deviation (SD) of the logarithm of the minimum angle of resolution (logMAR) recognition visual acuity and Snellen equivalent for testing with Early Treatment Diabetic Retinopathy Study (ETDRS) charts in the present study. Subjects were emmetropic children who had ≤ 0.25 diopter (D) of myopia (spherical equivalent), ≤ 1.00 D of hyperopia (spherical equivalent) and ≤ 0.50 D cylinder in both eyes.
| 5 to <6 yrs n=27 | 6 to <7 yrs n=28 | 7 to <8 yrs n=35 | 8 to <9 yrs n=25 | 9 to < yrs 10 n=28 | 10 to <11 yrs n=50 | 11 to <12 yrs n=39 | 12 to <13 yrs n=20 | ||
|---|---|---|---|---|---|---|---|---|---|
| Present | Mean | 0.16 | 0.09 | 0.06 | 0.03 | −0.01 | 0.05 | 0.04 | −0.00 |
| Study | SD | 0.10 | 0.08 | 0.10 | 0.08 | 0.08 | 0.19 | 0.13 | 0.18 |
| (letter by letter scoring*) | Snellen equivalent | [20/29] | [20/25] | [20/23] | [20/21] | [20/20] | [20/22] | [20/22] | [20/20] |
| Present | Mean | 0.13 | 0.07 | 0.04 | 0.01 | −0.05 | 0.02 | 0.00 | −0.02 |
| Study | SD | 0.11 | 0.08 | 0.10 | 0.09 | 0.08 | 0.20 | 0.13 | 0.19 |
| (line by line scoring**) | Snellen equivalent | [20/27] | [20/24] | [20/22] | [20/20] | [20/18] | [20/21] | [20/20] | [20/19] |
letter by letter scoring – based on number of letters correctly identified
line by line scoring – based on smallest line on which child identified at least 3 letters correctly
Figure 1.
Box plots of visual acuity results for each age group, plotted as logarithm of the minimum angle of resolution (logMAR), with Snellen equivalent values provided on the right-hand axis. At each age, results are shown for letter by letter scoring (in which visual acuity is based on the total number of letters correctly identified when the child is asked to read all letters on the Early Treatment Diabetic Retinopathy Study (ETDRS) chart), and for line by line scoring (in which visual acuity is based on the last line on which the child correctly identified at least three letters). The median is identified by a line inside the box. The length of the box is the inter-quartile range (IQR) (25% to 75%). Values more than three IQR’s from the end of a box are labeled as extreme, denoted with an asterisk (*), and values more than 1.5 IQR’s but less than 3 IQR’s from the end of the box are labeled as outliers (o). Whiskers represent the maximum and minimum values excluding outliers.
The lower 95% prediction limit was 0.38 (20/48) for five-year-olds, and 0.30 (20/40) for six- through twelve-year-olds, the age range for which there was no variation in visual acuity by age group. Recalculation of the lower 95% prediction limits with data removed from outliers (indicated as circles and asterisks in Figure 1) resulted in a value of 0.32 (20/42) for five-year-olds and 0.21 (20/32) for six- through twelve-year-olds.
Interocular Acuity Difference
Table 2 presents interocular acuity difference results, grouped by age. ANOVA showed no effect of age on interocular acuity difference. At all ages, the mean absolute difference between eyes was less than one line (0.10 log unit) on the logMAR chart, and the median difference was one line or less. The lower 95% prediction limit for the entire sample is 0.17 log unit (1.7 logMAR lines).
Table 2.
Median, mean, and standard deviation (SD) for the interocular acuity difference (absolute value of right eye logarithm of the minimum angle of resolution (logMAR) visual acuity – left eye logMAR visual acuity) in log units for emmetropic children who had ≤ 0.25 diopter (D) of myopia (spherical equivalent), ≤ 1.00 D of hyperopia (spherical equivalent) and ≤ 0.50 D cylinder in both eyes.
| 5 to <6 years n=27 | 6 to <7 years n=28 | 7 to <8 years n=35 | 8 to <9 years n=25 | 9 to <10 years n=28 | 10 to <11 years n=50 | 11 to <12 years n=39 | 12 to <13 years n=20 | Adults17 | |
|---|---|---|---|---|---|---|---|---|---|
| Median* | 0.06 | 0.06 | 0.06 | 0.04 | 0.04 | 0.04 | 0.04 | 0.06 | |
| Mean* | 0.07 | 0.07 | 0.07 | 0.05 | 0.05 | 0.06 | 0.05 | 0.06 | 0.04* |
| SD* | 0.06 | 0.06 | 0.06 | 0.04 | 0.05 | 0.07 | 0.05 | 0.04 | 0.05* |
| Median† | 0.10 | 0.10 | 0.10 | 0.10 | 0.00 | 0.10 | 0.00 | 0.10 | |
| Mean† | 0.07 | 0.08 | 0.09 | 0.06 | 0.05 | 0.08 | 0.05 | 0.08 | |
| SD† | 0.07 | 0.07 | 0.09 | 0.06 | 0.07 | 0.09 | 0.07 | 0.06 | |
letter by letter scoring – based on number of letters correctly identified
line by line scoring – based on smallest line on which child identified at least 3 letters correctly
DISCUSSION
The results of the present study provide normative data in one-year age groups for visual acuity measured with ETDRS charts2 in children five years through twelve years of age. The data indicate a developmental trend, with five-year-olds showing, on average, visual acuity that is one logMAR line poorer than visual acuity of children eight years of age and older. In contrast, there were no age differences in mean acuity for children from age six through twelve years, which suggests that a single normative value can be used across this age range.
Data from the present study (presented in Table 1) agree well with data previously published for ETDRS visual acuity testing of children between ages five and twelve years8,10–12 (shown in Table 3). With the exception of the high variability in visual acuity results in ten-year-olds in the present study, variability of visual acuity results was similar in the present study to that reported previously for children between five and twelve years of age, as indicated by similarity in the standard deviation values shown in Tables 1 and 3. Data from studies of adults (summarized in Table 3) indicate that the mean ETDRS visual acuity of adults 17 to 46 years of age3–5 is, on average, at least one line better than that of children younger than 13 years of age. It is unclear whether the poorer visual acuity scores shown by the youngest children, and the difference in mean visual acuity between children and adults, are due to acuity development during childhood, or to behavioral causes, for example, children’s difficulty attending to the visual acuity task and/or their reluctance to guess the identity of letters that are difficult to see.
Table 3.
Mean and standard deviation (SD) of the logarithm of the minimum angle of resolution (logMAR) recognition visual acuity and Snellen equivalent reported in previous studies of children and adults tested with Early Treatment Diabetic Retinopathy Study (ETDRS) charts.
| Study | N | Age (Years) | logMAR Mean | logMAR SD | Snellen Equivalent |
|---|---|---|---|---|---|
| Chen et al 200611 | 11 | 3.6–11 | 0.10 | 0.09 | 20/25 |
| Harvey et al 20077 | 446 | 4–13 | 0.04 | 0.15 | 20/22 |
| Stewart et al 200612 | 27 | 6.05±0.63 | 0.02 | 0.05 | 20/21 |
| Myers et al 199910 | 106 | 9.7–10.9 | −0.01 | 0.08 | 20/20 |
| Elliott & Whitaker 19914 | 20 | 20–30 | −0.13 | --- | 20/15 |
| Beck et al. 19933 | 140 | 18–46 | −0.12 | 0.10 | 20/15 |
| Ohlsson & Villarreal 20055 | 107 | 17–18 | −0.12 | 0.07 | 20/15 |
Clinically, it is useful to know the visual acuity score that would indicate that a child’s visual acuity is below the normal range for age. For five-year-olds, the lower 95% prediction limit was 0.38 logMAR (20/48), indicating that a child would be within the normal range if he/she passed the 20/50 line on the ETDRS chart. For six- through twelve-year-olds, it was 0.30 logMAR (approximately 20/40), indicating that children six through twelve years of age would be within the normal range if they pass the 20/40 line. Recalculation of these values with outlying data points removed tightened the values, and indicated that a five-year-old child with acuity of 20/40 or better would be within the normal range, and a six-through twelve-year-old child with acuity of 20/32 or better would be within the normal range.
In contrast to the age-related findings seen for visual acuity scores, there was no relation between age and the difference in visual acuity between eyes (Table 2). Overall, the average absolute difference in visual acuity between eyes was 0.06 log unit, or less than one logMAR line. Adults tested with ETDRS charts also show, on average, an interocular acuity difference of less than one logMAR line,5 although the mean difference between eyes of 0.04 log unit for adults is smaller than that shown by children, perhaps due to more variability in visual acuity data obtained from children. Important for clinical testing and screening is the finding that, based on the 95% prediction limit, an interocular acuity difference greater than 0.17 log unit (i.e., greater than 1.7 logMAR lines) would be considered abnormal.
Strengths and Limitations
The present study has a number of strengths. First, the sample is large enough to include at least 20 children in each of eight one-year age groups. Second, the sample is school-based, which is more representative of the general population than one would expect with a patient-based population.9,10 Third, all children had a cycloplegic refraction on the same day on which the visual acuity test was conducted, so that the data indicating that the children were emmetropic were concurrent. Fourth, visual acuity testing was conducted using a standardized protocol, by testers who were unaware of the refractive error status of the children and who were therefore unlikely to have biased the visual acuity outcomes that were obtained.
The study also has several limitations. First, the sample is ethnically-based, in that the participants are members of a Native American tribe. There is no evidence, however, that visual acuity in emmetropic individuals varies with ethnicity. Second, order of testing of eyes was not varied; the right eye was always first. However, the fact that there was no significant difference in right eye versus left eye visual acuity suggests that neither learning nor fatigue affected visual acuity results for the second eye. Third, no adults were tested in the present study, so that comparison of the present results with those of adults (Tables 2 and 3) requires comparison with other published data.
In conclusion, the present study provides the first normative ETDRS monocular visual acuity data from emmetropic children with no ocular pathology, categorized in one-year age groups, between five and twelve years of age. The results suggest that an age-specific visual acuity norm should be used for five-year-olds, but that a single normative value can be used for children between six and twelve years of age, because mean visual acuity is similar across this age range. There was no age-based variation in interocular acuity difference across the age range tested, suggesting that there is no need for specific, age-based norms for interocular acuity difference in children five through twelve years of age.
Comparison of the present data with previously-published normative ETDRS visual acuity data from adults3–5 indicates that there is a one logMAR line improvement in acuity between the child and adult years. In addition, mean interocular acuity difference in adults5 has been reported to be smaller than mean interocular acuity difference in the five- through twelve-year-old children tested in the present study. These findings emphasize the importance of using child-based rather than adult-based norms for acuity and interocular acuity difference.
Acknowledgments
Supported by grants from the National Eye Institute, National Institutes of Health, Department of Health and Human Services, Bethesda, MD (EY11155 (JMM) and EY13153 (EMH)), and Research to Prevent Blindness, New York, NY (Unrestricted grant to University of Arizona Department of Ophthalmology and Vision Science (JMM), The Walter E. and Lilly Disney Award for Amblyopia Research (JMM) and a Career Development Award (EMH)).
The authors thank Luisa Mayer, PhD, for her in-depth advice concerning statistical analyses.
Footnotes
None of the authors have any financial/conflicting interests to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Recommended standard procedures for the clinical measurement and specification of visual acuity: report of Working Group 39. Adv Ophthalmol. 1980;41:103–48. [PubMed] [Google Scholar]
- 2.Ferris FL, III, Kassoff A, Bresnick GH, Bailey I. New visual acuity charts for clinical research. Am J Ophthalmol. 1982;94:91–6. [PubMed] [Google Scholar]
- 3.Beck RW, Diehl L, Cleary PA Optic Neuritis Study Group. The Pelli-Robson letter chart: normative data for young adults. Clin Vis Sci. 1993;8:207–10. [Google Scholar]
- 4.Elliott DB, Whitaker D. Changes in macular function throughout adulthood. Doc Ophthalmol. 1990–1991;76:251–9. doi: 10.1007/BF00142684. [DOI] [PubMed] [Google Scholar]
- 5.Ohlsson J, Villarreal G. Normal visual acuity in 17–18 year olds. Acta Ophthalmol Scand. 2005;83:487–91. doi: 10.1111/j.1600-0420.2005.00516.x. [DOI] [PubMed] [Google Scholar]
- 6.Cryotherapy for Retinopathy of Prematurity Cooperative Group. Multicenter trial of cryotherapy for retinopathy of prematurity: Snellen visual acuity and structural outcome at 5–1/2 years after randomization. Arch Ophthalmol. 1996;114:417–24. doi: 10.1001/archopht.1996.01100130413008. [DOI] [PubMed] [Google Scholar]
- 7.Harvey EM, Dobson V, Miller JM, Clifford-Donaldson CE. Amblyopia in astigmatic children: patterns of deficits. Vision Res. 2007;47:315–26. doi: 10.1016/j.visres.2006.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harvey EM, Dobson V, Clifford-Donaldson CE, Miller JM. Optical treatment of amblyopia in astigmatic children: the sensitive period for successful treatment. Ophthalmology. 2007;114:2293–301. doi: 10.1016/j.ophtha.2007.03.021. [DOI] [PubMed] [Google Scholar]
- 9.Pediatric Eye Disease Investigator Group. A randomized trial of atropine vs patching for treatment of moderate amblyopia: follow-up at age 10 years. Arch Ophthalmol. 2008;126:1039–44. doi: 10.1001/archopht.126.8.1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Myers VS, Gidlewski N, Quinn GE, et al. Distance and near visual acuity, contrast sensitivity, and visual fields of 10-year-old children. Arch Ophthalmol. 1999;117:94–9. doi: 10.1001/archopht.117.1.94. [DOI] [PubMed] [Google Scholar]
- 11.Chen SI, Chandna A, Norcia AM, et al. The repeatability of best corrected acuity in normal and amblyopic children 4 to 12 years of age. Invest Ophthalmol Vis Sci. 2006;47:614–9. doi: 10.1167/iovs.05-0610. [DOI] [PubMed] [Google Scholar]
- 12.Stewart CE, Hussey A, Davies N, Moseley MJ. Comparison of logMAR ETDRS chart and a new computerised staircased procedure for assessment of the visual acuity of children. Ophthalmic Physiol Opt. 2006;26:597–601. doi: 10.1111/j.1475-1313.2006.00407.x. [DOI] [PubMed] [Google Scholar]
- 13.Harvey EM, Dobson V, Miller JM, Clifford-Donaldson CE. Changes in visual function following optical treatment of astigmatism-related amblyopia. Vision Res. 2008;48:773–87. doi: 10.1016/j.visres.2007.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dobson V, Harvey EM, Miller JM, Clifford-Donaldson CE. Anisometropia prevalence in a highly astigmatic school-aged population. Optom Vis Sci. 2008;85:512–9. doi: 10.1097/OPX.0b013e31817c930b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arditi A, Cagenello R. On the statistical reliability of letter-chart visual acuity measurements. Invest Ophthalmol Vis Sci. 1993;34:120–9. [PubMed] [Google Scholar]
- 16.Whitmore GA. Prediction limits for a univariate normal observation. Am Stat. 1986;40:141–3. [Google Scholar]