Abstract
Context:
Due to the chronic nature of cocaine dependence, long-term maintenance treatments may be required to sustain abstinence. Abstinence reinforcement is among the most effective means of initiating cocaine abstinence. Practical and effective means of maintaining abstinence reinforcement programs over time are needed.
Objective:
Determine whether employment-based abstinence reinforcement can be an effective long-term maintenance intervention for cocaine dependence.
Design:
Participants (N=128) were enrolled in a 6-month job skills training and abstinence initiation program. Participants who initiated abstinence, attended regularly, and developed needed job skills during the first six months were hired as operators in a data entry business and randomly assigned to an employment only (Control, n = 24) or abstinence-contingent employment (n = 27) group.
Setting:
A nonprofit data entry business.
Participants:
Unemployed welfare recipients who persistently used cocaine while enrolled in methadone treatment in Baltimore.
Intervention:
Abstinence-contingent employment participants received one year of employment-based contingency management, in which access to employment was contingent on provision drug-free urine samples under routine and then random drug testing. If a participant provided drug-positive urine or failed to provide a mandatory sample, then that participant received a temporary reduction in pay and could not work until urinalysis confirmed recent abstinence.
Main Outcome Measure:
Cocaine-negative urine samples at monthly assessments across one year of employment.
Results:
During the one-year of employment, abstinence-contingent employment participants provided significantly more cocaine-negative urine samples than employment only participants (79.3% and 50.7%, respectively; p = 0.004, OR = 3.73, 95% CI = 1.60 – 8.69).
Conclusions:
Employment-based abstinence reinforcement that includes random drug testing is effective as a long-term maintenance intervention, and is among the most promising treatments for drug dependence. Workplaces could serve as therapeutic agents in the treatment of drug dependence by arranging long-term employment-based contingency management programs.
Trial Registration:
clinicaltrials.gov. Identifier: NCT00249496
Keywords: Cocaine, Methadone, Employment, Contingency management, Abstinence reinforcement
Chronic drug use is a defining characteristic of drug dependence.1 Patterns of drug use frequently extend over many years.2-5 However, most treatments have not been designed to address drug dependence as a chronic problem.1 Recognizing the chronic nature of drug dependence, researchers have called for the use of long-term maintenance interventions.1,6 The development of long-term psychosocial interventions is especially critical for cocaine dependence, as no effective pharmacotherapy is currently available.7
Contingency management, in which patients receive desirable consequences contingent on providing objective evidence of drug abstinence, is one of the most effective treatments for cocaine dependence.8-14 Based on overwhelming evidence of the effectiveness of these contingency management interventions, the National Institute for Health and Clinical Excellence recommended their adoption by the National Health Service of the United Kingdom.15,16
Like other treatments, contingency management interventions have not historically addressed the chronicity of cocaine dependence and have typically been applied briefly. Although lasting effects have been noted after short-term exposure,17 relapse is common after discontinuation of the program.14,18 One study showed that cocaine abstinence could be maintained throughout a year-long exposure to voucher-based abstinence reinforcement.19 However, the use of an intervention of indeterminate length involving payment for drug-free urine samples is likely to be cost-prohibitive. A practical vehicle for arranging long-term abstinence reinforcement is required.
Employment-based abstinence reinforcement, in which access to employment is contingent on objective evidence of drug abstinence, has been proposed as an ideal long-term treatment for cocaine dependence, because workplaces control powerful reinforcers and facilitate regular and long-term monitoring of patients.20 Drug testing is used in workplaces, so its use in employment-based abstinence reinforcement programs is consistent with existing workplace practices.21-25
The therapeutic workplace is an employment-based abstinence reinforcement intervention. In the therapeutic workplace, unemployed drug dependent adults are invited to work, and are required to provide drug-free urine samples to maintain access to the workplace and maintain maximum rate of pay. In one randomized trial, pregnant and recently postpartum women in methadone treatment assigned to the therapeutic workplace had significantly higher rates of drug-free urine samples than usual care control participants.26,27 Additional studies showed that employment alone was not sufficient initiate cocaine abstinence, but that employment-based abstinence reinforcement significantly increased cocaine abstinence initiation.28,29 In light of these results, this study targeted two critical questions. First, does short-term exposure to employment-based reinforcement produce lasting abstinence after the abstinence contingency is discontinued? Second, can long-term employment-based reinforcement prevent relapse and maintain abstinence over an extended period of time?
The study was conducted in adults who used cocaine persistently during community methadone treatment. Eliminating cocaine use in this population is of particular public health significance because many of these individuals used crack cocaine and thus were at considerable risk for acquiring or transmitting HIV via high risk sexual behaviors, most notably trading sex for money or drugs.30-32
The study had two phases. In phase 1, all participants were exposed to employment-based abstinence reinforcement to initiate drug abstinence. Participants who initiated abstinence advanced to phase 2 and were hired as data entry operators in a nonprofit data entry business for one year, and randomly assigned to an employment only or abstinence-contingent employment group. Employment only participants worked independent of their urinalysis results, similar to typical employment. Abstinence-contingent employment participants were required to provide cocaine- and opiate-negative urine samples to work and continue earning maximum pay under a routine and then progressively more intermittent random drug testing schedule.
The primary objective of this study was to evaluate the effectiveness of employment-based contingency management in maintaining long-term cocaine abstinence in methadone patients during a year of employment in a nonprofit data entry business. The secondary objectives were to determine if long-term exposure to employment-based contingency management increased opiate abstinence and reduced HIV-risk behaviors. We expected that many participants in the employment only group would relapse to regular cocaine use during the year of employment. In contrast, we expected that sustained exposure to employment-based abstinence reinforcement during employment would maintain abstinence in most participants throughout the year of employment in the data entry business.
METHOD
STUDY PARTICIPANTS
This study was approved by the Western Institutional Review Board. Participants were recruited in methadone clinics throughout Baltimore. Recruitment began in October 2003, and the study was completed in August 2007. Participants were eligible if they were at least 18 years old, were unemployed, were enrolled in a Baltimore methadone maintenance program, provided a urine sample at intake with a detectable concentration of cocaine metabolite (>30 ng/mL) or provided a cocaine positive sample during regular urinalysis testing at their methadone maintenance program, met DSM-IV criteria for cocaine dependence, were receiving welfare benefits in Baltimore, and scored ≥80% correct on the reading assessment. Participants were excluded if they were at imminent risk of suicide, reported hallucinations, were currently incarcerated or otherwise under constant monitoring, earned ≥$200 in unreported taxable income from legal activity in the previous month, or had physical limitations that prevented typing. Of the 251 individuals assessed for eligibility, 128 met these criteria and were invited to participate in the study.
SETTING
The study was conducted at the Center for Learning and Health, Johns Hopkins School of Medicine, Baltimore, MD. The workplace included a sign-in station, a urinalysis laboratory, and three workrooms. The workrooms contained 47 computer workstations.
PRE-RANDOMIZATION PROCEDURES
Intake Assessment
At intake, participants signed informed consent and completed an interview. Urine samples were collected and tested for cocaine, opiates, benzodiazepines, methadone, and amphetamines. A questionnaire was administered to assess participants' capacity to operate a keyboard. The Composite International Diagnostic Interview (CIDI), 2nd ed.33,34 was administered to assess drug dependence. Other assessment tools included the Addiction Severity Index – Lite (ASI-Lite),35 the Risk Assessment Battery (RAB),36 the Wide Range Achievement Test (WRAT-3),37 and a reading assessment. Participants were paid $30 in vouchers for completing the interview.
Workroom and Urinalysis Procedures
Eligible participants were enrolled in phase 1 and could work in the workplace from 10 am-12 pm and 1 pm-3 pm every weekday for 6 months. During this phase, participants worked on computerized training programs designed to teach them to become data entry operators. On Monday, Wednesday and Friday, participants provided a urine sample under observation. Breath samples were tested for alcohol. Urine samples were tested for opiates and cocaine and participants received graphs showing current and prior drug test results. Participants earned a base pay of $8.00 per hour in vouchers. Additionally, participants could earn approximately $2.00 per hour in vouchers in productivity pay for working on training programs. Earnings accumulated in the participant's account until exchanged for a gift card or other approved goods and services.
Initially, participants could attend the workplace independent of their urinalysis results. This “workplace induction” continued for at least 4 weeks and until the participant worked for at least 5 min on 15 workdays. After workplace induction, participants were required to provide evidence of cocaine abstinence to work and to maintain maximum pay. Specifically, participants gained access to their workrooms if urinary benzoylecgonine concentration was <300 ng/mL or at least 20% lower per day since the last sample submitted. Participants who provided a cocaine-positive urine sample could not work until they provided a new sample that met the criteria. Upon return to work, the rate of base pay was reduced to $1.00 per hour. Base pay was then increased by $1.00 per hour every day that a participant provided a sample that met the criteria and worked at least 5 minutes until reaching $8.00 per hour. Missing samples were treated as positive. After a participant provided cocaine-negative samples for three consecutive weeks, the abstinence contingency was extended to opiates (ie, urinary benzoylecgonine and morphine concentrations of <300 ng/mL, or decreases in benzoylecgonine and morphine concentrations by at least 20% per day since the last sample submitted). After providing cocaine- and opiate-negative samples for three consecutive weeks the contingency was expanded to include alcohol if the participant had provided alcohol positive (≥0.003 ng/L) samples during the opiate and cocaine contingency period. This stepped contingency program is described in detail elsewhere.28
The training programs were designed for individuals with no typing skills. The programs were divided into small steps. Participants practiced steps in one-minute intervals until meeting mastery criteria for the step. Participants earned $0.03 per 20 correct characters typed, and lost $0.01 per 2 incorrect characters typed. Additional productivity pay ranging from $0.25 to $2.00 was provided for achieving step mastery. Participants who finished the typing program proceeded to a data entry training program, which included similar productivity pay contingencies. A detailed report of the results of phase 1 is provided elsewhere.28
RANDOMIZATION
Eligibility for phase 2 was assessed at the end of the fifth month of phase 1. Participants who attended the workplace on at least 50% of possible days and provided urine samples that met the reinforcement criteria on at least 80% of the collection opportunities during the four weeks prior to assessment, and who attained minimal typing proficiency qualified to participate in phase 2. Individuals not meeting criteria at the end of the fifth month who were still attending the workplace at least occasionally were reevaluated in the sixth month. This reevaluation occurred for seven participants, all of whom were admitted to phase 2 of the study. After meeting phase 2 eligibility criteria, participants were randomly assigned to employment only (n = 24) or abstinence-contingent employment (n = 27), and hired as employees of the nonprofit data entry business for one year. One eligible person declined to participate in phase 2 due to fears of losing social security benefits due to employment, and another was assigned to a discontinued study group (see below). The two groups did not differ significantly on any demographic measure assessed at intake. The phase 2 participants' mean age was 43 years, 77% were female, 88% were black, and 98% were living in poverty.
All stratification and randomization procedures were computerized and carried out by a data coordinator who did not have contact with participants. Participants were stratified according to whether 50% or more of the urine samples collected during the first four weeks of the induction period were positive for opiates; whether 75% or more of these samples were positive for cocaine; and whether they achieved an exceptionally high level of typing proficiency. Personnel who conducted monthly assessments were blind to group assignment.
POST-RANDOMIZATION PROCEDURES
Phase 2 Assessments
An interview was conducted immediately prior to randomization that included drug testing, the ASI-Lite, the RAB, the Vocational Educational Assessment (VEA, for assessing attitudes about work and employment history),38 and the Treatment Services Review (TSR, for assessing the use of professional services),39 and questionnaires covering adverse events and workplace satisfaction. These assessments were repeated every 30 days, except for the RAB, which was only conducted during the 6th and 12th months.
Phase 2 Employment Procedures
Upon enrollment in phase 2, participants began employment as data entry operators in Hopkins Data Services.40 While employed by Hopkins Data Services, participants could work from 9 am to 4 pm, with 1 hour for lunch. Participants earned an hourly wage slightly higher than or equal to the legal minimum (originally $5.25 per hour, but increased to $6.15 per hour when the minimum wage in Maryland increased) and pay for productivity. Contingencies for productivity pay were programmed such that participants would earn approximately $4.00 per hour in productivity pay for normative performance. Participants received regular bi-weekly paychecks instead of vouchers. Although prior employees of Hopkins Data Services performed data entry jobs for paying customers,40 given the nature of the control group (ie, no contingencies on drug abstinence), participants in this study performed data entry jobs in which they entered data batches from completed orders.
Study Groups
Participants assigned to the abstinence-contingent employment group were required to provide drug negative urine samples to access the workrooms on mandatory collection days. Initially, all Mondays, Wednesdays, and Fridays were mandatory days. If a participant in this group provided a positive sample or failed to provide a sample on a mandatory day, then the participant was denied access to the workplace on that day, and until the participant provided a sample that met the criteria. In addition, participants whose urine sample did not meet the criteria were given a reset in productivity pay from $4.00 per hour to $1.00 per hour. After a reset, a participant's productivity pay increased by $1.00 per hour per day that the participant worked for a minimum of five minutes, until the standard rate of approximately $4.00 per hour was reinstated.
Participants in the abstinence-contingent employment group who provided urine samples that met the criteria on 30 consecutive calendar days were placed on a random mandatory urine testing schedule. Initially, a schedule was established in which an average of one out of every two Mondays, Wednesdays, and Fridays were designated as mandatory collection and testing days. After every 30 days in which all mandatory samples met the abstinence criteria the average was further reduced by one, until an average of one out of every six Mondays, Wednesdays, and Fridays were randomly designated as mandatory days. Participants could call the workplace to inquire whether that day's urine sample collection was mandatory. If a participant provided a positive sample on a mandatory day or missed a mandatory sample then routine mandatory testing was reinstated and the schedule-thinning process repeated from the beginning. Participants were informed of schedule changes by the workplace manager and given a written notice describing the change. Participants received urinalysis feedback graphs similar to phase 1, however, only the results of mandatory tests were displayed on the graph.
Participants assigned to the employment only group were required to provide urine samples, but were permitted to work independent of the results of urinalysis. Rate of pay was also unaffected by the urinalysis results. In order to equate the urinalysis feedback across groups, employment only participants were placed on a thinning schedule of feedback in which the progressive thinning occurred every 30 days, independent of the participant's urinalysis results. Urine samples from participants in both groups were collected for data purposes every Monday, Wednesday, and Friday that a participant attended the workplace, although participants were only given feedback about the urinalysis results on selected days.
OUTCOME MEASURES
The primary outcome measure was cocaine-negative urine samples (urinary benzoylecgonine concentration of <300 ng/mL) based on samples collected at monthly assessments throughout phase 2. Secondary measures were opiate-negative urine samples (urinary morphine concentration of <300 ng/mL) based on samples collected at monthly assessments throughout phase 2 and drug-related HIV-risk behaviors assessed at 6- and 12-month time points in phase 2. Additional secondary measures were collected at 18 and 24 month follow-up after, although analyses of those results are not included here.
SAMPLE SIZE
A power analysis was conducted to determine the sample size that would be required to detect a medium effect size of 0.25 (power = 0.8, alpha = 0.05) in a three group design that included a usual care control group in addition to the groups described above. This analysis suggested an N of 52 per group. Early in the course of conducting the study it became clear that rates of attendance in the workplace far exceeded the expected levels, thus we would not be able to accommodate the originally planned number of participants in the workplace. As a result, we discontinued a usual care group (not described above) because including this group would have required approximately 50% more participants to enroll in the study and to initiate abstinence in phase 1. Recruitment continued as long as the grant funding allowed.
DATA ANALYSIS
Groups were compared on intake measures using Fisher's exact tests for dichotomous variables and Mann-Whitney tests for continuous measures. Dichotomous outcome measures assessed as single time points (eg, end of phase 1) were analysed with logistic regression. Dichotomous outcome measures assessed repeatedly over time were analysed using general estimating equations (GEE).41 Results of these analyses are reported as odds ratios (OR) and 95% confidence intervals (CI). Analyses were conducted using SAS 9.1, included intent-to-treat samples, were two-tailed, and were considered significant at p ≤ .05. For urinalysis measures and self-report measures of drug use collected using the ASI-Lite, missing samples were treated as positive. For urinalysis and self-report measures, additional analyses were conducted in which missing samples were counted as missing, and in which missing samples were interpolated. These analyses were not appreciably different from the missing positive analyses and are not presented. For HIV-risk behaviors, the only missing data were from a participant in the abstinence-contingent employment group who died during the course of the trial (see adverse events). This participant was excluded from the analysis of HIV-risk behaviors, but included in all other analyses. No assessments were missing at intake or at the end of phase 1. During phase 2, 99.7 and 94.4 percent of assessments were collected for employment only and abstinence-contingent employment groups, respectively (p = 0.19).
RESULTS
DRUG ABSTINENCE
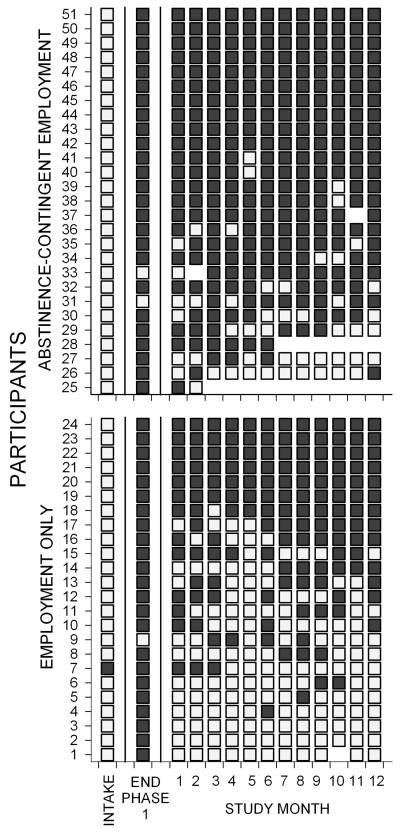
Figure 1 shows that almost all participants in both groups provided cocaine-negative urine samples at the end of phase 1. During the year of employment in phase 2 abstinence-contingent employment participants provided significantly higher rates of cocaine-negative urine samples (Figure 1 and Table 1). Many employment-only participants relapsed to regular cocaine use early in phase 2. Early relapse to cocaine use was relatively rare in abstinence-contingent employment participants; 18.5% of abstinence-contingent employment participants provided cocaine positive urine samples in the first month assessment of phase 2, compared to 45.8% of employment only participants.
Figure 1.
Cocaine urinalysis results at intake, end of phase 1, and across consecutive months during the intervention (phase 2). Within each panel, rows of data represent the cocaine urinalysis results for individual participants. Filled squares indicate cocaine-negative urine samples, and open squares indicate cocaine positive urine samples. Empty sections indicate missing samples. Within each panel, participants are arranged from those showing the least abstinence (fewest cocaine-negative urine samples) on the bottom to those with the most abstinence on the top.
TABLE 1.
URINALYSIS AND HIV RISK BEHAVIOR
| Overall percentage | ||||
|---|---|---|---|---|
| Employment only |
Abstinence- contingent employment |
p | OR (95% CI) | |
| Cocaine-negative urinalysis | ||||
| Intake | 4.2 | 0 | 0.47 | - |
| End of phase 1 | 95.8 | 92.6 | 1.0 | 1.84 (0.16 – 21.67) |
| Intervention | 50.7 | 79.3 | 0.004 | 3.73 (1.60 – 8.69) |
| Reported cocaine abstinence * | ||||
| Intake | 0 | 0 | - | - |
| End of phase 1 | 87.5 | 88.9 | 1.0 | 0.875 (0.16 – 4.81) |
| Intervention | 61.1 | 78.7 | 0.045 | 2.35 (1.06 – 5.21) |
| Reported no injection drug use * | ||||
| Intake | 66.7 | 70.4 | 1.0 | 0.84 (0.26 – 2.75) |
| End of phase 1 | 95.8 | 96.3 | 1.0 | 0.88 (0.05 – 14.96) |
| Intervention | 95.1 | 94.1 | 0.820 | 0.82 (0.17 – 3.86) |
| Reported no crack use * | ||||
| Intake | 29.2 | 37.0 | 0.767 | 0.70 (0.22 – 2.27) |
| End of phase 1 | 100 | 92.6 | 0.492 | - |
| Intervention | 71.5 | 81.2 | 0.174 | 1.72 (0.80 – 3.69) |
| Reported sharing injection equipment † | ||||
| Intake | 33.3 | 7.7 | 0.035 | 0.17 (0.03 – 0.89) |
| End of phase 1 | 4.2 | 7.7 | 1.0 | 1.92 (0.16 – 22.61) |
| Intervention | 0 | 3.8 | 1.0 | - |
| Reported going to shooting gallery or crack house † |
||||
| Intake | 33.3 | 26.9 | 0.759 | 0.70 (0.21 – 2.34) |
| End of phase 1 | 8.3 | 3.8 | 0.596 | 0.42 (0.04 – 4.99) |
| Intervention | 0.0 | 0.0 | - | - |
| Reported trading sex for drugs/money † | ||||
| Intake | 33.3 | 23.1 | 0.533 | 0.60 (0.17 – 2.09) |
| End of phase 1 | 4.2 | 3.8 | 1.0 | 0.92 (0.05 – 15.58) |
| Intervention | 16.7 | 0.0 | 0.046 | - |
from the Addiction Severity Index-Lite;
from the Risk Assessment Battery
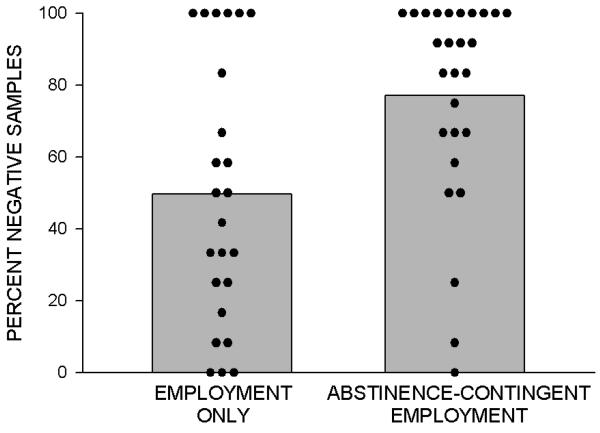
Figure 2 shows the mean percentage of urine samples that were negative for both opiates and cocaine during the year of phase 2 for each group. A GEE analysis showed that the difference was statistically significant (p = 0.002, OR = 4.2, 95% CI 1.79-9.87). Participants the abstinence-contingent employment and employment only groups provided opiate-negative urine samples 88.6% and 90.6% (p = 0.57, OR = 0.8, 95% CI = 0.26-2.43) of the 30-day assessments.
Figure 2.
Percentage of urine samples negative for cocaine and opiates during the year of intervention (phase 2) for employment only (left) and abstinence-contingent employment (right) groups. Bars show group means, and filled circles show percentages for individual participants. Data are based on results of monthly urinalysis. All missing samples were considered positive.
HIV-RISK BEHAVIORS
In general, lower percentages of individuals in both groups reported engaging in HIV-risk behaviors at the end of phase 1 than at intake (Table 1). During phase 2, significantly (p =0.046) more employment only participants (16.7%) reported trading sex for drugs or money than abstinence-contingent employment participants (0%).
RETENTION, ATTENDANCE AND PRODUCTIVITY
The abstinence-contingent employment and employment only groups attended the workplace at similar rates (70 and 71% of days attended, respectively; p =0.69), and most participants in both groups were retained throughout the year of phase 2 (89% and 95%, respectively; p = 0.61). Participants in both groups earned similar hourly wages on average ($10.10 and $10.56 per hour, respectively; p =0.43), and showed similar levels of accuracy in data entry (96.4% and 95.9%, respectively; p=0.61). The abstinence-contingent employment group had a higher mean rate of work output than the employment only group, but this difference was not significant (62.1 and 50.4 characters typed per minute, respectively, p=0.23).
ADVERSE EVENTS
Participant 25 (Figure 1) died during phase 2 of the trial. We were unable to determine the cause of death, but do not believe that it was related to study participation.
COMMENT
This randomized clinical trial showed that employment-based abstinence reinforcement can be an effective long-term maintenance intervention for the treatment of cocaine dependence. Participants were enrolled in this study because they used cocaine persistently during methadone treatment in Baltimore. All participants attended a therapeutic workplace for six months where they experienced employment-based abstinence reinforcement designed to initiate cocaine abstinence. Participants who initiated sustained cocaine abstinence were offered employment for one year and randomly assigned to an employment only or an abstinence-contingent employment group. Abstinence-contingent employment participants received an employment-based contingency management intervention, while employment only participants worked and earned wages independent of their urinalysis results, similar to typical employment. Abstinence-contingent employment participants maintained significantly and substantially higher rates of cocaine-negative urine samples than the employment only group during the year of employment, and many employment only group participants quickly relapsed to cocaine use. Although employment alone often failed to maintain cocaine abstinence, employment-based abstinence reinforcement was highly effective in maintaining cocaine abstinence for an entire year while participants held jobs as data entry operators.
These results suggest that workplace drug testing can be used for therapeutic purposes. Drug testing is used to maintain drug-free workplaces throughout the United States21 and the world.22,23 Workplaces in the United States most commonly use drug testing as part of pre-employment screening.24 Employers occasionally mandate drug testing for employees who have been identified as having a drug problem,24 and terminate employees who persist in using during their employment.25 Given the chronic nature of drug dependence, employees with histories of drug use may experience lapses, and could be subject to termination under a typical drug testing program. In this study, many participants in the abstinence-contingent employment group provided one or two drug-positive urine samples (Figure 1, Participants 31-41). Employees in the abstinence-contingent group were never terminated for drug use. Instead of termination, they experienced a brief reduction in rate of pay and a one-day suspension. This study provides a clear and carefully controlled demonstration that workplace drug testing can be used effectively to maintain long-term cocaine abstinence when drug testing is used to implement an employment-based abstinence reinforcement program.
Maintaining abstinence through employment-based abstinence reinforcement does not appear to require a high frequency of drug testing. Although abstinence-contingent employment participants experienced frequent drug testing at the beginning of the employment period, successful participants were ultimately evaluated once every two weeks on average according to a random schedule. This suggests that infrequent random testing may be effective in maintaining abstinence in a workplace. Further establishing the extent to which low-frequency, low-probability drug testing is effective in maintaining abstinence could enhance the convenience and feasibility of the intervention.
Employment-based abstinence reinforcement may offer additional public health benefits by reducing rates of HIV-risk behaviors. Methadone patients who persistently use crack and cocaine are at risk of acquiring or transmitting HIV infection.30-32 Importantly, this study showed that employment-based abstinence reinforcement could reduce participants' reports of trading sex for drugs or money, presumably by reducing their cocaine use. This finding is novel in that this is the first time a statistically significant reduction in trading sex for drugs or money has been reported in a randomized clinical trial of a long-term abstinence reinforcement intervention.
These results may have limited generality. Our participants were unemployed adults living in poverty. Prior descriptive research with physicians who used cocaine suggests that employment-based contingency management could be effective with that population;42 but the relevance of the present results to other populations (from construction workers to physicians) is not known. Even among the targeted population, only 53 of 126 individuals (42%) who enrolled in phase 1 were eligible for phase 2. Prior analysis of phase 1 data indicated that the percentage of minutes worked and average earnings per day during the induction period were each independently predictive of treatment outcome,28 suggesting that employment-based abstinence reinforcement may not be useful for individuals who attend the workplace infrequently and who maintain relatively low earnings. These data and previous studies43,44 suggest that higher wages could produce better treatment outcomes.
Employment-based abstinence reinforcement was evaluated in this study in a nonprofit social business,45,46 which existed to address drug dependence and poverty. While this research could have direct relevance to other nonprofit social businesses, the relevance of this research to other business models should be established in future research.
The development of long-term maintenance interventions that address the chronicity of use and propensity to relapse is among the most important challenges in substance abuse treatment research. Voucher-based abstinence reinforcement interventions have been shown to be highly effective in treating cocaine dependence, even in refractory individuals. The present study shows that this method can be adapted to a workplace setting through the use of employment-based abstinence reinforcement and used as a long-term maintenance intervention to address the chronic nature of cocaine dependence. Developing methods to disseminate employment-based abstinence reinforcement could further enhance this promising treatment for cocaine dependence.
Acknowledgements
This work was supported by National Institute on Drug Abuse grants R01DA13107 and T32 DA07209. All authors report no conflict of interest. The first author had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Additional contributors include: Paul Nuzzo - data analysis and statistical testing; Karly Diemer - study protocol and trial management; Mick Needham - workplace management; Jackie Hampton – assessments, recruitment and outreach; Kylene Broadwater - data management
This work was supported by National Institute on Drug Abuse grants R01DA13107 and T32 DA07209.
REFERENCES
- 1.McLellan AT, Lewis DC, O'Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment insurance and outcomes evaluation. JAMA. 2000;284(13):1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 2.Dobler-Mikola A, Hättenschwiler J, Meili D, Beck T, Böni E, Modestin J. Patterns of heroin, cocaine, and alcohol abuse during long-term methadone maintenance treatment. J Subst Abuse Treat. 2005;29(4):259–265. doi: 10.1016/j.jsat.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 3.Hser YI, Huang D, Chou CP, Anglin MD. Trajectories of heroin addiction: growth mixture modeling results based on a 33-year outcome study. Eval Rev. 2007;31(6):548–563. doi: 10.1177/0193841X07307315. [DOI] [PubMed] [Google Scholar]
- 4.Krampe H, Stawicki S, Wagner T, Bartles C, Aust C, Rüther E, Poser W, Ehrenreich H. Follow-up of 180 alcoholic patients for up to 7 years after outpatient treatment: impact of alcohol deterrents on outcome. Alcohol Clin Exp Res. 2006;30(1):86–95. doi: 10.1111/j.1530-0277.2006.00013.x. [DOI] [PubMed] [Google Scholar]
- 5.Rathod NH, Addenbrooke WM, Rosenbach AF. Heroin dependence in an English town: 33-year follow up. Br J Psychiatry. 2005;187(5):421–425. doi: 10.1192/bjp.187.5.421. [DOI] [PubMed] [Google Scholar]
- 6.Dennis M, Scott CK. Managing addiction as a chronic condition. Addict Sci Clin Pract. 2007;4(1):45–55. doi: 10.1151/ascp074145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kalivas PW. Neurobiology of cocaine addiction: implications for new pharmacotherapy. Am J Addict. 2007;16(2):71–78. doi: 10.1080/10550490601184142. [DOI] [PubMed] [Google Scholar]
- 8.Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry. 2008;165(2):179–187. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- 9.Knapp WP, Soares BG, Farrel M, Lima MS. Psychosocial interventions for cocaine and psychostimulant amphetamines related disorders. Cochrane Database Syst Rev. 2007;147(2):81–88. doi: 10.1002/14651858.CD003023.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Prendergast M, Podus D, Finney J, Greenwell L, Roll J. Contingency management for treatment of substance use disorders: a meta-analysis. Addiction. 2006;101(11):1546–1560. doi: 10.1111/j.1360-0443.2006.01581.x. [DOI] [PubMed] [Google Scholar]
- 11.Higgins ST, Budney, AJ, Bickel WK, Foerg FE, Donham R, Badger GJ. Incentives improve outcome in outpatient behavioral treatment of cocaine dependence. Arch Gen Psychiatry. 1994;51(7):568–576. doi: 10.1001/archpsyc.1994.03950070060011. [DOI] [PubMed] [Google Scholar]
- 12.Higgins ST, Heil SH, Rogers RE, Chivers L. Cocaine. In: Higgins ST, Silverman K, Heil SH, editors. Contingency Management in Substance Abuse Treatment. Guliford Press; New York: 2008. pp. 19–41. [Google Scholar]
- 13.Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101(2):192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- 14.Silverman K, Higgins ST, Brooner RK, Montoya ID, Cone EJ, Schuster CR, Preston KL. Sustained cocaine abstinence in methadone maintenance patients through voucher-based reinforcement therapy. Arch Gen Psychiatry. 1996;53(5):409–415. doi: 10.1001/archpsyc.1996.01830050045007. [DOI] [PubMed] [Google Scholar]
- 15.National Institute for Health and Clinical Excellence . NICE Clicial Guideline. Vol. 51. NICE; London: 2007. Drug addiction: psychosocial interventions. [Google Scholar]
- 16.Pilling S, Strang J, Gerada C. Psychosocial interventions and opioid detoxification for drug addiction: summary of NICE guidance. BMJ. 2007;335(7612):203–205. doi: 10.1136/bmj.39265.639641.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Higgins ST, Wong CJ, Badger GJ, Ogden DE, Dantona RL. Contingent reinforcement increases cocaine abstinence during outpatient treatment and 1 year of follow-up. J Consult Clin Psychol. 2000;68(1):64–72. doi: 10.1037//0022-006x.68.1.64. [DOI] [PubMed] [Google Scholar]
- 18.Silverman K, Wong CJ, Umbricht-Schneiter A, Montoya ID, Schuster CR, Preston KL. Broad beneficial effects of cocaine abstinence reinforcement among methadone patients. J Consult Clin Psychol. 1998;66(5):811–824. doi: 10.1037//0022-006x.66.5.811. [DOI] [PubMed] [Google Scholar]
- 19.Silverman K, Robles E, Mudric T, Bigelow GE, Stitzer ML. A randomized trial of long-term reinforcement of cocaine abstinence in methadone-maintained patients who inject drugs. J Consult Clin Psychol. 2004;72(5):839–854. doi: 10.1037/0022-006X.72.5.839. [DOI] [PubMed] [Google Scholar]
- 20.Silverman K. Exploring the limits and utility of operant conditioning in the treatment of drug addiction. The Behav Anal. 2004;27(2):209–230. doi: 10.1007/BF03393181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bush DM. The U.S. mandatory guidelines for federal workplace drug testing programs: current status and future considerations. Forensic Sci Int. 2008;174(2-3):111–119. doi: 10.1016/j.forsciint.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 22.Nolan S. Drug-free workplace programmes: New Zealand perspective. Forensic Sci Int. 2008;174(2-3):125–132. doi: 10.1016/j.forsciint.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 23.Verstraete AG, Pierce A. Workplace drug testing in Europe. Forensic Sci Int. 2001;121(1-2):2–6. doi: 10.1016/s0379-0738(01)00445-5. [DOI] [PubMed] [Google Scholar]
- 24.Mørland J. Types of drug-testing programmes in the workplace. Bull Narc. 1993;45(2):83–113. [PubMed] [Google Scholar]
- 25.Knudsen HK, Roman PM, Johnson JA. The management of workplace deviance: organizational responses to employee drug use. J Drug Issues. 2004;34(1):121–143. [Google Scholar]
- 26.Silverman K, Svikis, D, Robles E, Stizer ML, Bigelow GE. A reinforcement-based therapeutic workplace for the treatment of drug abuse: six-month abstinence outcomes. Exp Clin Psychopharmacol. 2001;9(1):14–23. doi: 10.1037/1064-1297.9.1.14. [DOI] [PubMed] [Google Scholar]
- 27.Silverman K, Svikis D, Wong CJ, Hampton J, Stitzer ML, Bigelow, GE. A reinforcement-based therapeutic workplace for the treatment of drug abuse: three-year abstinence outcomes. Exp Clin Psychopharmacol. 2002;10(3):228–240. doi: 10.1037//1064-1297.10.3.228. [DOI] [PubMed] [Google Scholar]
- 28.Donlin WD, Knealing TW, Needham M, Wong CJ, Silverman K. Attendance rates in a workplace predict subsequent outcome of employment-based reinforcement of cocaine abstinence in methadone patients. J Appl Behav Anal. 2008;41(4):499–516. doi: 10.1901/jaba.2008.41-499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Silverman K, Wong CJ, Needham M, et al. A randomized trial of employment-based reinforcement of cocaine abstinence in injection drug users. J Appl Behav Anal. 2007;40(3):387–410. doi: 10.1901/jaba.2007.40-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Booth RE, Watters JK, Chitwood DD. HIV risk-related sex behaviors among injection drug users, crack smokers, and injection drug users who smoke crack. Am J Public Health. 1993;83(8):1144–1148. doi: 10.2105/ajph.83.8.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Edlin B, Irwin KL, Farque S, McCoy CB, Word C, Serrano Y, Inciardi JA, Bowser BP, Schilling RF, Holmberg SD. Intersecting epidemics--crack cocaine use and HIV infection among inner-city young adults. N Engl J Med. 1994;331(21):1422–1427. doi: 10.1056/NEJM199411243312106. [DOI] [PubMed] [Google Scholar]
- 32.Hoffman JA, Klein H, Eber M, Crosby H. Frequency and intensity of crack use as predictors of women's involvement in HIV-related sexual risk behaviors. Drug Alcohol Depend. 2000;58(3):227–236. doi: 10.1016/s0376-8716(99)00095-2. [DOI] [PubMed] [Google Scholar]
- 33.Cottler LB, Robins LN, Grant BF, Blaine, et al. The CIDI-core substance abuse and dependence questions: cross-cultural and nosological issues. The WHO/ADAMHA Field Trial. Br J Psychiatry. 1991;159(5):653–658. doi: 10.1192/bjp.159.5.653. [DOI] [PubMed] [Google Scholar]
- 34.Robins LN, Wing J, Wittchen HU, et al. The Composite International Diagnostic Interview. An epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry. 1988;45(12):1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- 35.McLellan AT, Cacciola JS, Zanis D. The Addiction Severity Index-“Lite” (ASI-“Lite”) Center for the Studies of Addiction, University of Pennsylvania/Philadelphia VA Medical Center; [Google Scholar]
- 36.Navaline HA, Snider EC, Petro CJ, et al. Preparations for AIDS vaccine trials. An automated version of the Risk Assessment Battery (RBA): enhancing the assessment of risk behaviors. AIDS Res Hum Retroviruses. 1994;10(Suppl 2):S281–S283. [PubMed] [Google Scholar]
- 37.Wilkinson GS. WRAT-3: Wide range achievement test administration manual. Wide Range, Inc; Wilmington, DE: 1993. [Google Scholar]
- 38.Zanis DA, Coviello D, Alterman AI, Appling SE. A community-based trial of vocational problem-solving to increase employment among methadone patients. J Subst Abuse Treat. 2001;21(1):19–26. doi: 10.1016/s0740-5472(01)00177-5. [DOI] [PubMed] [Google Scholar]
- 39.McLellan AT, Alterman AI, Cacciola J, Metzger D, O'Brien CP. A new measure of substance abuse treatment: Initial studies of the treatment services review. J Nerv Ment Dis. 1992;180(2):101–110. doi: 10.1097/00005053-199202000-00007. [DOI] [PubMed] [Google Scholar]
- 40.Silverman K, Wong CJ, Grabinski MJ, et al. A web-based therapeutic workplace for the treatment of drug addiction and chronic unemployment. Behav Modif. 2005;29(2):417–463. doi: 10.1177/0145445504272600. [DOI] [PubMed] [Google Scholar]
- 41.Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44(4):1049–1060. [PubMed] [Google Scholar]
- 42.Crowley TJ. Doctors' drug abuse reduced during contingency-contracting treatment. Alcohol Drug Res. 1985-1986;6(4):299–307. [PubMed] [Google Scholar]
- 43.Silverman K, Chutuape MA, Bigelow GE, Stitzer ML. Voucher-based reinforcement of cocaine abstinence in treatment-resistant methadone patients: effects of reinforcement magnitude. Psychopharmacol. 1999;146(2):128–138. doi: 10.1007/s002130051098. [DOI] [PubMed] [Google Scholar]
- 44.Dallery J, Silverman K, Chutuape MA, Bigelow GE, Stitzer ML. Voucher-based reinforcement of opiate plus cocaine abstinence in treatment-resistant methadone patients: effects of reinforcer magnitude. Exp Clin Psychopharmacol. 2001;9(3):317–325. doi: 10.1037//1064-1297.9.3.317. [DOI] [PubMed] [Google Scholar]
- 45.Yunus M, Weber K. Creating a world without poverty: Social Business and the Future of Capitalism. PublicAffairs™; New York, NY: 2007. [Google Scholar]
- 46.Yunus M. Speech presented at: Nobel Lectures. Oslo, Norway: Dec 10, 2006. The Nobel Peace Prize 2006 Nobel Lecture. http://nobelprize.org/nobel_prizes/peace/laureates/2006/yunus-lecture-en.html. Accessed October 10, 2008. [Google Scholar]