Abstract
Objective
To test the effectiveness of two programmes to improve the treatment of acute depression in primary care.
Design
Randomised trial.
Setting
Primary care clinics in Seattle.
Patients
613 patients starting antidepressant treatment.
Intervention
Patients were randomly assigned to continued usual care or one of two interventions: feedback only and feedback plus care management. Feedback only comprised feedback and algorithm based recommendations to doctors on the basis of data from computerised records of pharmacy and visits. Feedback plus care management included systematic follow up by telephone, sophisticated treatment recommendations, and practice support by a care manager.
Main outcome measures
Blinded interviews by telephone 3 and 6 months after the initial prescription included a 20 item depression scale from the Hopkins symptom checklist and the structured clinical interview for the current DSM-IV depression module. Visits, antidepressant prescriptions, and overall use of health care were assessed from computerised records.
Results
Compared with usual care, feedback only had no significant effect on treatment received or patient outcomes. Patients receiving feedback plus care management had a higher probability of both receiving at least moderate doses of antidepressants (odds ratio 1.99, 95% confidence interval 1.23 to 3.22) and a 50% improvement in depression scores on the symptom checklist (2.22, 1.31 to 3.75), lower mean depression scores on the symptom checklist at follow up, and a lower probability of major depression at follow up (0.46, 0.24 to 0.86). The incremental cost of feedback plus care management was about $80 (£50) per patient.
Conclusions
Monitoring and feedback to doctors yielded no significant benefits for patients in primary care starting antidepressant treatment. A programme of systematic follow up and care management by telephone, however, significantly improved outcomes at modest cost.
Introduction
Despite the high prevalence and significant impact1,2 of depression among patients in primary care, management often falls short of expert recommendations: only a few patients receive recommended levels of pharmacotherapy or experience satisfactory clinical outcomes.3–5 Recent randomised trials show that organised treatment programmes—including both pharmacotherapy3,4,6 and structured psychotherapy4,6,7—greatly improve both quality of care and clinical outcomes. These models, however, require several visits to specialists, and available data show increased treatment costs of $300 (£187.50) to $600 (£375) per patient,8,9 which are likely to limit acceptance by patients and purchasers. Management of other health conditions shows that fairly simple and inexpensive interventions including computerised feedback and reminder systems10,11 and follow up by telephone12–14 can increase doctors' compliance with care guidelines, improve the management of chronic illness, and support change in health behaviour.
We examined the effects of two simple and inexpensive programmes to improve the treatment of depression in primary care: feedback only, which comprised computerised data on prescriptions and visits to provide doctors with feedback on patients and algorithm based recommendations for treatment; and feedback plus care management, which supplemented the feedback system with systematic follow up and care management by telephone. We aimed to test three of the key management strategies for disease described by Wagner and VonKorff15,16; a population based clinical information system, monitoring of adherence to treatment, and systematic follow up care. We hypothesised that both programmes would increase both the frequency of follow up visits and the dose and duration of antidepressant treatment and decrease the severity of depressive symptoms.
Methods
Protocol
Our study was conducted in five primary care clinics of Group Health Cooperative of Puget Sound, an organisation serving around 450 000 members in Washington state. The study protocol was approved by the group's review committee on human subjects.
A typical primary care clinic has around 20 000 members with a staff of eight to 10 doctors, three to five registered nurses, and eight to 10 licensed practical nurses or medical assistants. On average, adult members make four to five visits annually. Separate mental health clinics provide a range of services with emphasis on brief psychotherapy, pharmacotherapy, and group therapy. No referral or authorisation is required for uptake of mental health care. Outpatient psychotherapy typically covers 10 to 20 visits per year, subject to copayments for visits from $10 (£6.25) to $20 (£12.50) with no copayment or limit for visits for management of drugs. The utilisation and cost of all services are recorded on computer.
From computerised pharmacy records we identified all patients at participating clinics who had received new prescriptions for antidepressants, with “new” defined as no antidepressant use in the previous 120 days. From computerised records of visits we excluded patients who had not been diagnosed with depression at any visit (non-depression indication for prescription); had been diagnosed with bipolar disorder or psychotic disorder in the previous two years; had been diagnosed with alcohol or other substance misuse in the previous 90 days; or had visited a psychiatrist in the previous 90 days.
We attempted to contact all eligible patients by telephone seven to 15 days after the initial prescription. After a complete description of study procedures, eligible and consenting patients completed a 20 item depression scale from the Hopkins symptom checklist.17
Assignment
After completion of the baseline interview participants were assigned to one of three groups according to computer generated random numbers (stratified by clinic): usual care, feedback only, or feedback plus care management.
Treatments
In the usual care group no services other than standard ones were provided to the patients or doctors. In the feedback only group doctors received a detailed report on each patient eight and 16 weeks after the initial prescription. These included computerised data (antidepressant dosage and repeat prescriptions, number of follow up visits, and arranged visits) and treatment recommendations on the basis of a computerised algorithm. Use of subtherapeutic doses of antidepressants led to the recommendation that if major symptoms persisted doctors should consider increasing the dose but that if side effects were not tolerable they should consider changing the drug. Absence of a scheduled follow up visit led to the recommendation that doctors should contact patients to arrange follow up visits. Recommendations were limited by the absence of information on drug side effects or current severity of depression.
Immediately after randomisation patients in the care management group received a five minute introductory telephone call from the care manager followed by two 10 to 15 minute telephone assessments eight and 16 weeks after the initial prescription. These assessments included current use of antidepressants, side effects, and severity of depressive symptoms. After each telephone assessment doctors received a feedback report including computerised data, assessment data, and sophisticated algorithm based recommendations. Doctors were advised to consider increasing drug doses if patients used drugs at moderate doses, reported minimal side effects, and had moderate symptoms of depression. Doctors were advised to consider changing drugs if there was a similar scenario but with more severe side effects (persistent symptoms at maximum tolerable dose). Recommendations for follow up visits varied with the severity of depressive symptoms. Care managers also supported doctors in implementation of recommendations including immediate communication of urgent recommendations, assistance with arranging follow up visits, telephoning patients who had discontinued treatment, and helping with referrals. Telephone contacts sometimes included general support and encouragement but did not include any specific psychotherapeutic content. The programme was presented to patients as a supplement to, rather than a replacement for, existing primary care treatment. Both care managers were experienced in telephone assessment and triage, but they had no specific training in antidepressant pharmacotherapy and were not expected to make prescribing decisions. Both received around 15 minutes of supervision a week from a psychiatrist (GS or JU). Each care manager could assume responsibility for 8-10 new patients a week (or a caseload of around 100 patients).
Blinding
Outcome assessments were conducted by independent telephone interviewers who were blinded to both treatment group and treatment received. Participants were advised not to reveal details of treatment received during blinded assessments.
Outcomes
Assessments three and six months after the initial prescription included the 20 item depression scale on the symptom checklist17 and the current depression module of the structured clinical interview for DSM-IV.18 From computerised pharmacy and visit data we assessed antidepressant treatment received (using previously developed and validated algorithms5) and follow up visits. Treatment costs were calculated with the 1997 Medicare fee schedule for visits and the health plan's actual costs for all other services. Medical comorbidity was assessed with the chronic disease score.19 Primary economic analyses considered only treatment costs for outpatient depression (antidepressant prescriptions, visits for mental health, and visits to primary care with depression diagnoses). Costs of care management were estimated from the care managers' time logs and actual labour and overhead costs. Secondary analyses examined costs for both total health services and time in treatment. Estimates for average hourly wage of the patients treated for depression ($15.95 (£9.97)) and average time spent attending an outpatient visit (2.7 hours) were taken from a previous study of depression treatment in primary care.20 Patient time required for assessments by a care manager was estimated as 15 minutes per contact.
Data analysis
Data analyses compared each intervention group with the usual care control group based on original treatment assignment, regardless of treatment received. Clinical outcomes at three and six months were analysed as repeated measures using mixed linear regression models for continuous measures and mixed logistic regression models for categorical measures. No significant group by time interaction was observed for any measure, so we present analyses for the main effect of intervention across both follow up assessments. Adjusted incremental costs were estimated with mixed linear regression. All analyses incorporated two random intercept terms to account for clustering of patients within doctors and doctors within clinics. Mixed models were estimated with the MIXED procedure and GLIMMIX macro of the SAS software package (SAS, Cary, NC). Sample size was set at 200 patients per group based on the ability to detect a 10% difference in treatment costs for depression, with 80% statistical power and type 1 error rate of 5% (two sided).
Results
Participant flow and follow up
Of 872 eligible patients 101 could not be contacted by telephone and 157 declined to participate, leaving 613 patients (70% of those eligible and 80% of those contacted). Table 1 shows the baseline characteristics of the participants. Rates of participation in blinded follow up assessments were 97% at three months and 95% at six months. All analyses based on computerised data (prescriptions, visits, treatment costs) were limited to the 93% of patients remaining in the health plan for six months.
Table 1.
Baseline characteristics of participants
| Usual care (n=196) | Feedback only (n=221) | Care management (n=196) | |
|---|---|---|---|
| Age | 46.8 (15.3) | 46.5 (14.3) | 46.3 (14.9) |
| No (%) female | 141 (72) | 154 (70) | 144 (74) |
| Depression score* | 1.74 (0.77) | 1.67 (0.72) | 1.66 (0.76) |
| Chronic disease score | 1273 (1286) | 1329 (1285) | 1381 (1336) |
Based on Hopkins symptom checklist.
Overall, 97% of patients in the care management group completed the eight week contact with a care manager, and 93% completed the 16 week contact. In 60% of these contacts no further action (for example, direct contact with the doctor) was needed. Modest additional effort (for example, phone call to doctor, additional phone call to patient) was needed in 25% of cases, and substantial assistance (for example, multiple telephone calls, facilitation of specialty referral) was needed in 15%.
Analysis
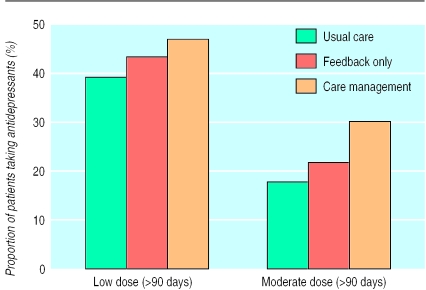
Figure 1 shows the proportion of patients receiving at least 90 days of antidepressant treatment using either a low dosing threshold21 (for example, 75 mg per day imipramine, 10 mg per day fluoxetine) or a moderate threshold around twice as high, reflecting doses considered adequate by psychiatrists. Patients in the care management group received adequate pharmacotherapy more often than those in the usual care group, but this difference was only statistically significant using the moderate threshold (odds ratios: low threshold 1.31, 95% confidence interval 0.86 to 1.98; moderate threshold 1.99, 1.23 to 3.22). The feedback only group and the usual care group did not differ significantly on either measure. Neither intervention had any apparent effect on number of visits for either primary care, mental health, or total follow up (table 2).
Figure 1.
Antidepressant use in six months after initial prescription for patients taking antidepressants for at least 90 days by dosage level and receiving usual care (n=196), feedback only (n=221), and care management (n=196)
Table 2.
Outpatient visits during six months after index antidepressant prescription. Sample is limited to those enrolled in health plan throughout follow up period
| Usual care (n=180)
|
Feedback only (n=207)
|
Care management (n=188)
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No (%) | Mean (SD) | Interquartile range | No (%) | Mean (SD) | Interquartile range | No (%) | Mean (SD) | Interquartile range | |||
| Primary care visits with depression diagnosis | 158 (88) | 1.89 (1.48) | 1-2 | 176 (85) | 1.94 (1.43) | 1-3 | 176 (85) | 2.05 (1.66) | 1-3 | ||
| Primary care visits without depression diagnosis | 121 (67) | 1.58 (1.66) | 0-2 | 143 (69) | 1.54 (1.76) | 0-2 | 143 (69) | 1.77 (2.13) | 0-3 | ||
| Mental health visits to prescribing provider | 11 (6) | 0.12 (0.58) | 0 | 12 (6) | 0.13 (0.59) | 0 | 12 (6) | 0.09 (0.52) | 0 | ||
| Mental health visits to non-prescribing provider | 49 (27) | 1.02 (4.07) | 0-1 | 56 (27) | 0.80 (2.65) | 0-1 | 56 (27) | 0.70 (1.74) | 0-1 | ||
| Total | 178 (99) | 4.61 (4.58) | 2-6 | 203 (98) | 4.40 (3.79) | 2-6 | 203 (98) | 4.62 (3.44) | 2-6 | ||
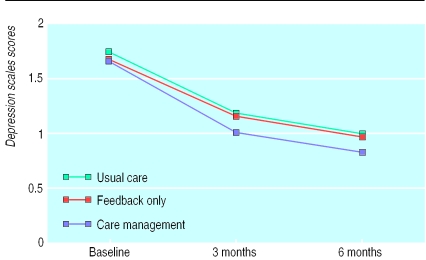
Figure 2 shows the average depression scores on the symptom checklist over time. After adjustment for age, sex, chronic disease score, and baseline depression score, depression score at follow up was significantly lower in the care management group than in the usual care group (t=2.59, P=0.008). The mean score in the feedback only group did not differ from that in the usual care group (t=0.22, P=0.82). The adjusted mean depression score at six months was 0.83 in the care management group compared with 0.98 (95% confidence interval for difference 0.02 to 0.27) in the usual care group.
Figure 2.
Course of scores over time on depression scale of symptom checklist in patients receiving usual care (n=196), feedback only (n=221), and care management (n=196)
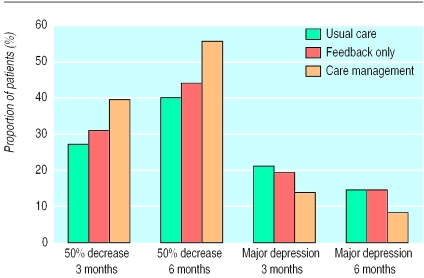
The care management group had a significantly higher probability of showing a 50% decrease in depression scores on the symptom checklist, a customary measure of treatment response (odds ratio 2.22, 1.31 to 3.75), and a significantly lower probability of persistent major depression at follow up (0.45, 0.24 to 0.86; fig 3). The feedback only intervention had no significant effect on either probability of treatment response (1.12, 0.73 to 1.73) or probability of major depression at follow up (0.89, 0.55 to 1.46).
Figure 3.
Categorical outcomes for depression (50% decrease in depression scores on symptom checklist and major depression by structured clinical interview for DSM-IV) since baseline assessment at three and six month blinded outcome assessments in patients receiving usual care (n=196), feedback only (n=221), and care management (n=196)
Table 3 shows the treatment costs over six months. Primary analyses considered treatment costs for outpatient depression (prescriptions, follow up visits, and costs of the interventions) over six months. After adjustment for age, sex, chronic disease score, and baseline depression score, mean incremental costs were $22 (£13.75) (95% confidence interval −$27 (£16.9) to $71 (£44.38)) for feedback only and $83 (£51.88) ($32 (£20) to $134 (£83.75)) for care management. Secondary analyses of costs for total health services and time in treatment are shown in table 3. Although the costs for total health services seemed higher in the care management group, this difference was attributable to one patient with costs of $120 000 (£75 000). Analyses that exclude this single outlier or analyses of log transformed costs (less sensitive to extreme observations) showed no difference in costs for total health services among the three groups. As expected from data on number of follow up visits, costs for time in treatment did not differ by treatment assignment.
Table 3.
Costs for treatment of outpatient depression (from insurer perspective), time in treatment costs, and missed work costs for six months after index antidepressant prescription. Sample is limited to those enrolled in health plan throughout follow up period. Values are in $
| Usual care (n=180)
|
Feedback only (n=207)
|
Care management (n=188)
|
||||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Interquartile range | Mean (SD) | Interquartile range | Mean (SD) | Interquartile range | |||
| Antidepressant prescriptions | 135 (149) | 37-192 | 156 (145) | 33-242 | 167 (159) | 40-260 | ||
| Primary care visits | 134 (81) | 86-181 | 134 (94) | 68-184 | 148 (109) | 68-191 | ||
| Mental health specialty visits | 119 (151) | 0-50 | 114 (114) | 0-50 | 118 (114) | 0-99 | ||
| Intervention programme | 0 | 0 | 10 (0) | 10-10 | 51 (23) | 31-74 | ||
| Total depression treatment costs | 388 (269) | 166-466 | 414 (253) | 198-497 | 484 (269) | 249-583 | ||
| Total health services costs | 1645 (2646) | 408-1568 | 1673 (3072) | 374-1529 | 2327 (8803) | 491-1602 | ||
| Total health services costs (with single outlier removed*) | 1645 (2646) | 408-1568 | 1673 (3072) | 374-1529 | 1729 (3379) | 491-1602 | ||
| Time in treatment costs | 244 (215) | 129-301 | 232 (199) | 86-301 | 249 (194) | 129-301 | ||
After removal of single outlier with cost of $112 000 ($85 000 greater than next highest observation).
Discussion
In primary care the implementation of an organised programme of care monitoring, follow up by telephone, feedback to doctors, and practice support by a care manager had no effect on number of follow up visits of patients with depression but led to significant improvements in the intensity of antidepressant treatment and in clinical outcomes. Incremental costs for depression treatment (including costs of the intervention) were around $80 (£50) per patient. A programme limited to monitoring and feedback using available computerised data had no significant effect on treatment received or patient outcomes.
Our results contrast with previous research showing that feedback of computerised data can improve the quality of ambulatory care,22 increase compliance with screening guidelines,10,11 and improve laboratory monitoring.11 We propose two explanations. Firstly, feedback arrived separately from patient visits when implementation of reminder suggestions would have required active outreach. Secondly, automated reminders may be sufficient to influence one time decisions but insufficient to support the regular follow up and treatment adjustments necessary for management of chronic illness.
Our findings are consistent with previous studies showing the benefits of follow up by telephone in the management of chronic illness12,13 and change in health behaviour.14 Follow up by telephone initiated by a doctor (“active”) may be a cost effective substitute for patients making visits to clinics. Follow up by telephone can reduce the time costs of treatment (travel and waiting time) and improve access for patients with limitations to mobility and those living in rural areas.
We cannot be certain whether the benefits of the care management programme are attributable to more intensive pharmacotherapy, more appropriate follow up care, or the non-specific effects of supportive contact with the care manager. Our findings might not be generalised to primary care doctors with different levels of knowledge, motivation, or experience in the management of depression. Our study was also limited to patients with new antidepressant prescriptions, excluding those who were unrecognised, untreated, or not given an initial prescription.
Our care management intervention seems to lie between more intensive depression interventions that have shown robust clinical effects3,4,6,7 and less intensive interventions (such as screening programmes not linked to structured intervention23 and physician training programmes24) that have proved ineffective. Organised and consistent follow up care seems necessary to improve the management of depression, but modest interventions can yield significant benefits.
We believe that these results support the implementation of organised monitoring and care management programmes to improve the management of depression. Similar programmes might prove valuable in the management of other common chronic illnesses. Such programmes, however, are only one component of a population based approach to treatment of depression. When persistent depression results from inadequate monitoring and follow up, more organised treatment significantly improves outcomes. When depression persists despite optimal primary care management, specialty consultation or referral may be needed. Achieving good clinical outcomes may prove neither simple nor inexpensive for patients with more severe or complicated depression.
What is already known on this topic
Management of depression in primary care often falls short of evidence based recommendations
Several randomised trials have shown that organised treatment programmes significantly improve quality of depression treatment and patient outcomes, but these programmes typically require several visits to specialists and additional expenditures of $500 (£312.50) or more per patient
What this study adds
A programme of two telephone monitoring contacts (eight and 16 weeks after initiation of depression treatment) followed by feedback to the doctor and care management by telephone when required showed significant benefits in the treatment of depression in primary care
In contrast, a programme limited to feedback of available computerised information (number of visits and prescriptions) had no effect
Acknowledgments
We thank Ky Haverkamp and Steve Tutty (the care managers) and Jurgen Unutzer for clinical supervision of the care managers.
Footnotes
Funding: US National Institute of Mental Health (grant number MH51338).
Competing interests: All authors are employees of Group Health Cooperative of Puget Sound.
References
- 1.Spitzer R, Kroenke K, Linzer M, Hahn SR, Williams JBW, de Gruy FV, et al. Health-related quality of life in primary care patients with mental disorders. JAMA. 1995;274:1511–1517. [PubMed] [Google Scholar]
- 2.Ormel J, VonKorff M, Ustun TB, Pini S, Korten A, Oldehinkel T. Common mental disorders and disability across cultures. JAMA. 1994;272:1741–1748. doi: 10.1001/jama.272.22.1741. [DOI] [PubMed] [Google Scholar]
- 3.Katon W, VonKorff M, Lin E, Walker E, Simon G, Bush T, et al. Collaborative management to achieve treatment guidelines: impact on depression in primary care. JAMA. 1995;273:1026–1031. [PubMed] [Google Scholar]
- 4.Katon W, Robinson P, VonKorff M, Lin E, Bush T, Ludman E, et al. A multifaceted intervention to improve treatment of depression in primary care. Arch Gen Psychiatry. 1996;53:924–932. doi: 10.1001/archpsyc.1996.01830100072009. [DOI] [PubMed] [Google Scholar]
- 5.Simon G, Lin EHB, Katon W, Saunders K, VonKorff M, Walker E, et al. Outcomes of “inadequate” antidepressant treatment in primary care. J Gen Int Med. 1995;10:663–670. doi: 10.1007/BF02602759. [DOI] [PubMed] [Google Scholar]
- 6.Schulberg H, Block MR, Madonia MJ, et al. Treating major depression in primary care practice: eight-month clinical outcomes. Arch Gen Psychiatry. 1996;53:913–919. doi: 10.1001/archpsyc.1996.01830100061008. [DOI] [PubMed] [Google Scholar]
- 7.Mynors-Wallis L, Gath DH, LLoyd-Thomas AR, Tomlinson D. Randomised controlled trial comparing problem solving treatment with amitriptyline and placebo for major depression in primary care. BMJ. 1995;310:441–445. doi: 10.1136/bmj.310.6977.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lave J, Frank R, Schulberg H, Kamlet M. Cost-effectiveness of treatments for major depression in primary care practice. Arch Gen Psychiatry. 1998;55:645–651. doi: 10.1001/archpsyc.55.7.645. [DOI] [PubMed] [Google Scholar]
- 9.VonKorff M, Katon W, Bush T, Lin EHB, Simon GE, Saunders K, et al. Treatment costs, cost offset, and cost-effectivness of collaborative management of depression. Psychosom Med. 1998;60:143–149. doi: 10.1097/00006842-199803000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Litzelman D, Dittus R, Miller M, Tierney WM. Requiring physicians to respond to computerized reminders improves their compliance with preventive care protocols. J Gen Int Med. 1993;8:311–317. doi: 10.1007/BF02600144. [DOI] [PubMed] [Google Scholar]
- 11.McDonald C, Hui S, Smith D, Tierney WM, Cohen SJ, Weinberger M, et al. Reminders to physicians from an introspective computer medical record. A two-year randomized trial. Ann Intern Med. 1984;100:130–138. doi: 10.7326/0003-4819-100-1-130. [DOI] [PubMed] [Google Scholar]
- 12.Wasson J, Gaudette C, Whaley F, Sauvigne A, Baribeau P, Welch H. Telephone care as a substitute for routine clinic follow-up. JAMA. 1992;267:1788–1793. [PubMed] [Google Scholar]
- 13.Weinberger M, Tierney W, Cowper P, Katz B, Booher P. Cost-effectiveness of increased telephone contact for patients with osteoarthritis. A randomized, controlled trial. Arthritis Rheum. 1993;36:243–246. doi: 10.1002/art.1780360216. [DOI] [PubMed] [Google Scholar]
- 14.Curry S, McBride C, Grothaus L, Louie D, Wagner E. A randomized trial of self-help materials, personalized feedback, and telephone counseling with nonvolunteer smokers. J Consult Clin Psychol. 1995;63:1005–1014. doi: 10.1037//0022-006x.63.6.1005. [DOI] [PubMed] [Google Scholar]
- 15.Wagner E, Austin B, VonKorff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511–544. [PubMed] [Google Scholar]
- 16.VonKorff M, Gruman J, Schaefer J, Curry S, Wagner E. Collaborative management of chronic illness. Ann Intern Med. 1997;127:1097–1102. doi: 10.7326/0003-4819-127-12-199712150-00008. [DOI] [PubMed] [Google Scholar]
- 17.Derogatis L, Rickels K, Uhlenhuth EH, Covi L. The Hopkins symptom checklist: a measure of primary symptom dimensions. In: Pichot P, editor. Psychological measurements in psychopharmacology: problems in psychopharmacology. Basel: Kargerman; 1974. pp. 79–110. [Google Scholar]
- 18.First M, Spitzer R, Gibbon M, Williams J. Structured clinical interview for DSM-IV axis I disorders (SCID-I), clinician version. Washington: American Psychiatric Press; 1997. [Google Scholar]
- 19.Clark D, VonKorff M, Saunders K, Baluch WM, Simon GE. A chronic disease score with empirically derived weights. Med Care. 1995;33:783–795. doi: 10.1097/00005650-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Simon G, VonKorff M, Heiligenstein JH, Revicki DA, Grothaus L, Katon W, et al. Initial antidepressant selection in primary care: effectiveness and cost of fluoxetine vs tricyclic antidepressants. JAMA. 1996;275:1897–1902. [PubMed] [Google Scholar]
- 21.Agency for Health Policy and Research. Depression guideline panel. Clinical practice guideline No 5: depression in primary care. 2: treatment of major depression. Rockville, MD: US Department of Health and Human Services. AHCPR; 1993. . (Publication No 93-0550). [Google Scholar]
- 22.Balas E, Austin S, Mitchell J, Weigman B, Bopp K, Brown G. The clinical value of computerized information services. A review of 98 randomized clinical trials. Arch Fam Med. 1996;5:271–278. doi: 10.1001/archfami.5.5.271. [DOI] [PubMed] [Google Scholar]
- 23.Dowrick C, Buchan I. Twelve month outcome of depression in general practice: does detection or disclosure make a difference? BMJ. 1995;311:1274–1277. doi: 10.1136/bmj.311.7015.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goldberg H, Wagner E, Fihn S, Martin DP, Horowitz CR, Christensen DB, et al. A randomized controlled trial of CQI teams and academic detailing: can they alter compliance with guidelines? Jt Comm J Qual Impr. 1998;24:130–142. doi: 10.1016/s1070-3241(16)30367-4. [DOI] [PubMed] [Google Scholar]