Abstract
The purpose of this study was to test whether the efficacy of prophylactic treatment with botulinum toxin A (BTX-A) on migraine frequency is related to the individual perception of the pain and its directionality, namely, exploding, imploding, or ocular migraine headache. Episodic and chronic migraine patients (n=82) previously treated with BTX-A were interviewed to characterize their migraine headache and its directionality. The magnitude of their response to treatment was analyzed vis-à-vis their individual type of headache. Patients showing a >67% drop in number of migraine days/month were classified as responders; those showing a drop smaller than 33% were labeled non-responders; patients showing a drop between 34% to 66% were considered questionable responders. After BTX-A treatment, the number of migraine days/month dropped 85.2±1.6% (from 20.1±1.5 to 2.8±0.4; p<0.0001) in 37 responders, 52.4±2.4% (from 16.3±3.5 to 7.2±1.5; p=0.003) in 11 questionable responders, and remained unchanged (21.2±1.8 vs. 21.1±1.7; p>0.78) in 34 non-responders. The frequency of headache types differed significantly (p<0.0001) across the 3 response sub-groups. Among non-responders, 83% described a buildup of pressure inside their head (exploding headache). Among responders and questionable responders, 84 and 64%, respectively, perceived their head to be crushed, clamped or stubbed by external forces (imploding headache) or an eye-popping pain (ocular headache). The prevalence of exploding, imploding, and ocular headache was similar between episodic and chronic migraine patients. Imploding/ocular migraine headache is more likely than exploding headache to be prevented by prophylactic BTX-A treatment. Further validation of this principle should await large-scale prospective, placebo-controlled studies.
Introduction
In a recent prospective study, we found that the success rate of preventing migraine attacks prophylactically using botulinum toxin A (BTX-A) was strikingly associated with the type of headache experienced by the individual patient. Patients who experienced a drastic decline in attack frequency during weeks 4–12 after BTX-A treatment perceived their head to be crushed, clamped, or stubbed by external forces, or testified to an eye-popping pain, which we dubbed, respectively, imploding and ocular headache (Jakubowski et al. 2006). In contrast, patients who did not benefit from BTX-A treatment testified to a buildup of pressure inside their head, which we dubbed exploding headache (Jakubowski et al. 2006). The prevalence of muscle tenderness, cutaneous allodynia, or any of the classical symptoms of migraine, including aura, photophobia, phonophobia, osmophobia, nausea, and throbbing, was similar between BTX-A responders and non-responder. These findings were confirmed in a triple-blind retrospective study in which patients from two other clinics were interviewed by the same investigator who conducted the prospective study. To test whether our original findings can be replicated, the present retrospective study was carried out by two independent neurologists who interviewed patients in their respective clinics who had already undergone routine prophylactic BTX-A treatment for episodic and chronic migraine.
Methods
Patient selection
The studies herein were carried out in compliance with 1983 revision of the 1975 Helsinki Declaration. The studies herein were carried out in compliance with 1983 revision of the 1975 Helsinki Declaration, and according to the ethical standards of the Committee on Clinical Investigation on Human Experimentation at Thomas Jefferson University and the Mayo Clinic Scottsdale. Included in the study were patients who met the criteria of the Second International Classification of Headache Disorders (ICHD-2) for episodic and chronic migraine (2004; Olesen 2006). Excluded were patients with secondary chronic daily headache, tension-type headache only, peripheral nervous system injuries, and those using opioids for reasons other than migraine.
Eighty two migraine patients (21–75 years of age) who received BTX-A injections for the purpose of migraine prophylaxis were interviewed retrospectively by Dr. Silberstein at Thomas Jefferson Headache Center, Philadelphia, PA (n=39) and by Dr. Dodick at the Mayo Clinic Headache Center, Scottsdale, AZ (n=43). The interview covered the following items: migraine history (age of onset and number of years with migraine); attack frequency before and after BTX-A treatment; and a detailed description of the migraine pain. This included pain site (e.g., ocular, frontal, parietal, occipital, unilateral, bilateral), pain characteristics (e.g., pressuring, crushing, stabbing, throbbing), and pain directionality (e.g., pressure buildup inside the head vs. piercing pain inflicted outside of the head).
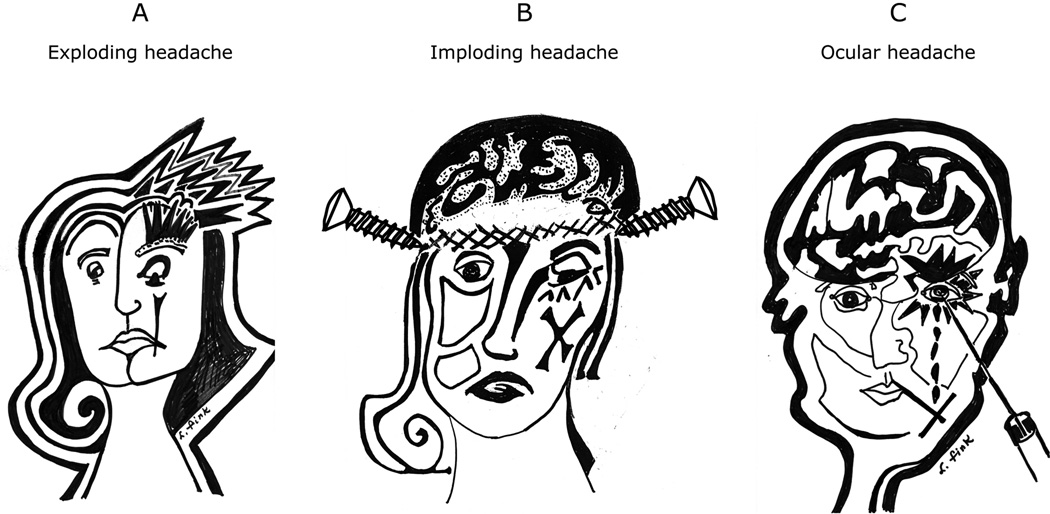
Patients were presented with graphic illustrations and testimonies describing 3 types of migraine pain and were asked to characterize their pain perception using the following options: (a) exploding headache; (b) imploding headache; (c) ocular headache; (d) cannot tell. Patients with exploding headache perceived a buildup of pressure inside their head as if the skull were about to split open (Fig 1A). Patients with imploding headache perceived their skull to be assaulted by external forces typically referred to as crushing, clamping, or stubbing (Fig 1B). Patients with ocular headache attested to an eye-popping pain (Fig 1C). Patients were oblivious to any connection between the characteristics of the pain and the outcome of the treatment.
Figure 1.
Illustrations of migraine pain and its directionality based on patients’ testimonies. A. exploding headache, B. Imploding headache, C. Ocular headache.
Statistical analysis
Patients were divided into 3 subgroups based on the percent drop in migraine days/month after BTX-A treatment: >66.7% drop (responders); between 33.4 and 66.6% drop (questionable responders); <33.3% drop (non-responders). Data analysis was performed using non-parametric statistics (Siegel 1956). Ordinal measurements (e.g., age, attack frequency, attack duration, pain intensity) were compared between responders and non-responders using Mann-Whitney U test. Repeated ordinal measurements (i.e., before and after treatment) were compared within each group using Wilcoxon matched-pairs signed-rank test. Nominal data were analyzed using either simple χ2 test or Fisher exact probability test, depending on sample size and expected frequencies (Siegel 1956). The level of significance was set at 0.05.
Results
Patients included in this study (69 women, 13 men) were 50.9±1.2 years of age (mean±SEM), with a history of 29.9±1.9 years of migraine (onset at 21.3±1.9 years of age). Of these 82 patients, 33% had episodic migraine and 67% had chronic migraine. Before BTX-A treatment, the number of migraine days per month was 7.9±0.6 (between 2 and 13) in episodic migraine patients and 26.4±0.8 (between 15 and 30) in chronic migraine patients. Of the 27 episodic migraine patients, 52% attested to exploding headache and 48% to imploding headache. Of the 55 chronic migraine patients, 40% had exploding headache, 56% had imploding or ocular headache, and 4% were undecided. The distribution of the different types of migraine headache is summarized in Table 1.
Table 1.
Distribution of the types of migraine headache
| Type of headache | ||||
|---|---|---|---|---|
| Type of migraine | N | Exploding | Imploding or ocular | Unsure |
| Episodic | 27 | 52% | 48% | - |
| Chronic | 55 | 40% | 56% | 4% |
| All patients | 82 | 44% | 54% | 2% |
Overall response to BTX-A
In the 82 studied patients, the mean±SEM number of days of migraine per month dropped 43.8±5.2% (from 20.3±1.1 to 11.0±1.2; p<0.0001). This relatively modest drop, however, included patients who showed no change and those who showed significant change.
Interval analysis of response to BTX-A
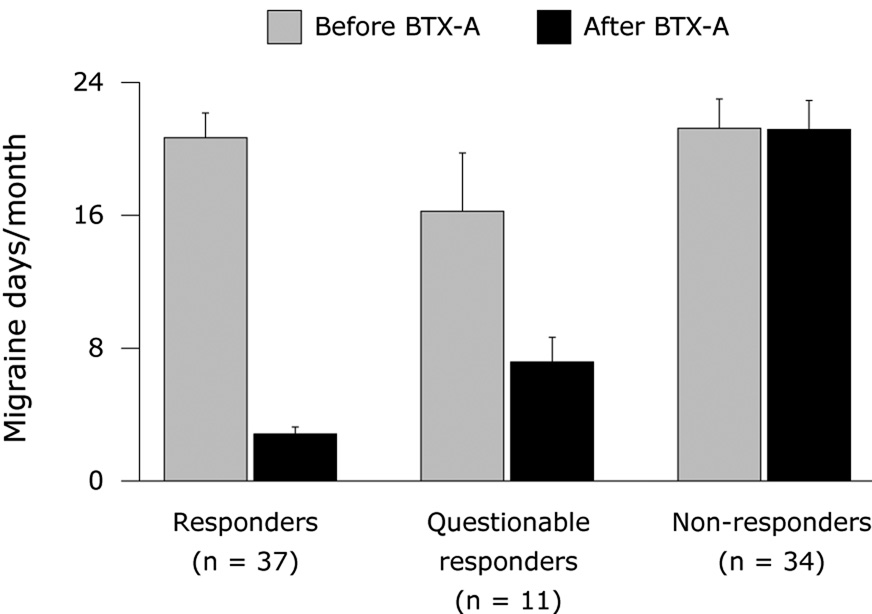
The number of migraine days/month dropped by >66.7% in 37 patients (responders), between 33.4 and 66.6% in 11 patients (questionable responders), and <33.3% in 34 patients (non-responders). As shown in Figure 2, the mean±SEM number of days of migraine per month dropped 85.2±1.6% (from 20.1±1.5 to 2.8±0.4; p<0.0001) in responders, 52.4±2.4% (from 16.3±3.5 to 7.2±1.5; p=0.003) in questionable responders, and remained unchanged (21.2±1.8 vs. 21.1±1.7; p>0.78) in non-responders.
Figure 2.
Effects of BTX-A on mean±SEM number of days of migraine per month (attack frequency×attack duration) in responders (>66.7% drop), questionable responders (between 33.4 and 66.6% drop), and non-responders (<33.3% drop).
Response to BTX-A in episodic vs. chronic migraine
There was no significant difference (χ2=0.96; p>0.6) in the distribution of the 3 response subgroups between the episodic migraine patients and the chronic migraine patients. Of the 27 episodic migraine patients, 41% were responders, 18% questionable responders, and 41% non-responders. Of the 55 chronic migraine patients, 47% were responders, 11% questionable responders, and 42% non-responders.
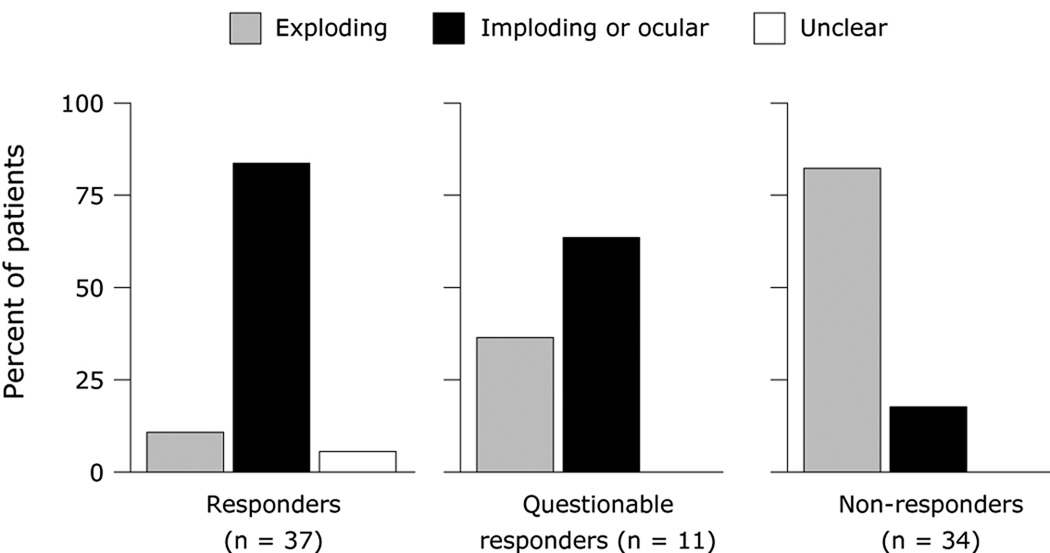
Response to BTX-A in exploding vs. imploding/ocular headache
The prevalence of headache types differed significantly (p<0.0001) across the 3 response sub-groups (Figure 3): non-responders had predominantly exploding headache as oppose to responders (p<0.0001) or questionable responders (p<0.007), who had predominantly imploding or ocular headache. Among 44 patients with imploding or ocular headache, 31 (70%) were responders, 7 (16%) questionable responders, and 6 (14%) non-responders. Among 36 patients with exploding headache, 4 (11%) were responders, 4 (11%) questionable responders, and 28 (78%) non-responders.
Figure 3.
Incidence of types of migraine headache in responders (>66.7% drop), questionable responders (between 33.4 and 66.6% drop), and non-responders (<33.3% drop).
Discussion
The success rate of preventing migraine attacks using BTX-A was strongly associated with the headache perception of individual patients. The prevalence of ‘imploding’ or ‘ocular’ headache was highest among responders, lowest among non-responders, and intermediate among questionable responders. Conversely, the prevalence of ‘exploding’ headache was lowest among responders, highest among non-responders, and intermediate among questionable responders. This confirms our previous findings (Jakubowski et al. 2006) that migraineurs with imploding/ocular headache are highly likely to improve after BTX-A treatment. The validity of predicting response likelihood to BTX-A therapy on the basis of the type of headache is clear among responders and non-responders, but uncertain among questionable responders. The higher the prevalence of questionable responders, the lower the predictability of treatment outcome based on headache type.
The sharp dichotomy between responders and non-responders suggests that data pooled from all treated patients obfuscates the full magnitude of the treatment effect at the level of the individual patient. Indeed, our pooled data from all 82 patients indicated a 43% decrease in migraine days per month after BTX-A, which is in agreement with previous studies (Blumenfeld 2003; Dodick et al. 2005; Tepper et al. 2004). However, interval analysis of the response magnitude indicated an 85% drop in migraine days per month after BTX-A in the subgroup of responders vs. 0% change in the subgroup of non-responders. This strongly sugests that the efficacy of BTX-A therapy in migraine depends on the relative prevalence of imploding, ocular, and exploding headache types in the general population of migraineurs.
Our study calls for future epidemiological studies to establish the relative proportion of patients who are clear responders, clear non-responders, or questionable responders, as well as the relative proportions of patients having exploding, imploding, or ocular headache.
Acknowledgement
Supported by an unrestricted grant from Allergan, and by NIH grants NS051484 and NS035611 to Dr. Burstein. We thank Virginia artist Lorraine Fink for the illustrations in Fig. 1. Drs. Burstein, Dodick and Silberstein served as consultant to Allergan, served on Allergan’s advisory, received honorarium for lectures, received grant support.
References
- The International Classification of Headache Disorders. Second Edition. Vol. 24. Cephalalgia: 2004. pp. 1–160. [Google Scholar]
- Blumenfeld A. Botulinum toxin type A as an effective prophylactic treatment in primary headache disorders. Headache. 2003;43:853–860. doi: 10.1046/j.1526-4610.2003.03163.x. [DOI] [PubMed] [Google Scholar]
- Dodick DW, Mauskop A, Elkind AH, DeGryse R, Brin MF, Silberstein SD. Botulinum toxin type a for the prophylaxis of chronic daily headache: subgroup analysis of patients not receiving other prophylactic medications: a randomized double-blind, placebo-controlled study. Headache. 2005;45:315–324. doi: 10.1111/j.1526-4610.2005.05068.x. [DOI] [PubMed] [Google Scholar]
- Jakubowski M, McAllister PJ, Bajwa ZH, Ward TN, Smith P, Burstein R. Exploding vs. imploding headache in migraine prophylaxis with Botulinum Toxin A. Pain. 2006;125:286–295. doi: 10.1016/j.pain.2006.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olesen J. International Classification of Headache Disorders, Second Edition (ICHD-2): current status and future revisions. Vol. 26. Cephalalgia: 2006. pp. 1409–1410. [DOI] [PubMed] [Google Scholar]
- Siegel S. Nonparametric Statistics for the Behavioral Sciences. Tokyo: McGrow-Hill Kogakusha; 1956. p. 312. [Google Scholar]
- Tepper SJ, Bigal ME, Sheftell FD, Rapoport AM. Botulinum neurotoxin type A in the preventive treatment of refractory headache: a review of 100 consecutive cases. Headache. 2004;44:794–800. doi: 10.1111/j.1526-4610.2004.04147.x. [DOI] [PubMed] [Google Scholar]