Abstract
This report reviews findings from studies that have investigated whether abnormalities in reward from food intake and anticipated food intake increase risk for obesity. Self-report and behavioral data suggest that obese relative to lean individuals show elevated anticipatory and consumatory food reward. Brain imaging studies suggest that obese relative to lean individuals show greater activation of the gustatory cortex (insula/frontal operculum) and oral somatosensory regions (parietal operculum and Rolandic operculum) in response to anticipated intake and consumption of palatable foods. Yet, data also suggest that obese relative to lean individuals show less activation in the dorsal striatum in response to consumption of palatable foods and reduced striatal D2 dopamine receptor density. Emerging prospective data also suggest that abnormal activation in these brain regions increases risk for future weight gain and that genotypes associated with lowered dopamine signaling amplify these predictive effects. Results imply that individuals who show greater activation in the gustatory cortex and somatosensory regions in response to anticipation and consumption of food, but who show weaker activation in the striatum during food intake, may be at risk for overeating, particularly those at genetic risk for lowered dopamine receptor signaling.
Keywords: Obesity, anticipatory and consummatory food reward, neuroimaging review
Obesity is associated with increased risk for mortality, atherosclerotic cerebrovascular disease, coronary heart disease, colorectal cancer, hyperlipidemia, hypertension, gallbladder disease, and diabetes mellitus, resulting in over 111,000 deaths annually in the US [1]. Currently, 65% adults and 31% of adolescents in the US are overweight or obese [2]. Unfortunately, the treatment of choice for obesity (behavior weight loss treatment) only results in moderate and transient reduction in body weight [3] and most obesity prevention programs do not reduce risk for future weight gain [4]. The limited success of these interventions may be due to an incomplete understanding of the factors that increase risk for obesity. Although twin studies imply that biological factors play a key etiologic role in obesity, few prospective studies have identified biological factors that increase risk for future weight gain.
Reward from Food Intake
Theorists have posited that obesity results from abnormalities in reward processing. However, the findings seem somewhat inconsistent, which has prompted competing models regarding the relation of abnormalities in reward processing to the etiology of obesity. Some researchers propose that a hyper-responsiveness of reward circuitry to food intake increases risk for overeating [5,6]. This is similar to the reinforcement sensitivity model of substance abuse, which posits that certain people show greater reactivity of brain reward systems to reinforcing drugs [6]. Others hypothesize that obese individuals show hypo-responsiveness of reward circuitry, which leads them to overeat to compensate for this deficiency [7,8]. This Reward Deficiency Syndrome may contribute to other motivated behaviors, including substance abuse and gambling [9].
Consistent with the hyper-responsiveness model, obese individuals rate high-fat and high-sugar foods as more pleasant and consume more of such foods than lean individuals [10,11,12]. Children at risk for obesity by virtue of parental obesity prefer the taste of high-fat foods and show a more avid feeding style than children of lean parents [13,14,15]. Preferences for high-fat and high-sugar foods predict elevated weight gain and increased risk for obesity [16,17]. Obese versus lean individuals report that food intake is more reinforcing [18,19,20]. Self-report measures of general sensitivity to reward correlate positively with overeating and body mass [21,22].
Brain imaging studies have identified regions that appear to encode subjective reward from food consumption. Consumption of palatable foods, relative to consumption of unpalatable foods or tasteless foods, results in greater activation of the right lateral orbitofrontal cortex (OFC), frontal operculum and insula [23,24]. Consumption of palatable food also results in dopamine release in the dorsal striatum [25]. Microdialysis studies in rodents indicate that appetitive tastes also release dopamine in the nucleus accumbens shell and core, as well as the prefrontal cortex [26,27]. Animal studies indicate that bingeing on sugar increases extracellular dopamine in the nucleus accumbens shell [28]. Stimulation of the meso-limbic network using a μ-opioid receptor agonist [29] and lesions of the baslolateral amygdalar and lateral hypothalamus circuit can produce overeating [30], supporting the importance of this region’s neurochemistry in food consumption.
Accumulating data implicate deficiencies in dopamine receptors in obesity. Obese relative to lean rats show less D2 receptor density in the hypothalamus [31] and in the striatum [32] and reduced hypothalamic dopamine activity when fasting, but release more phasic statewise dopamine when eating and do not stop eating in response to insulin and glucose administration [33]. Obesity-prone Sprague-Dawley rats have reduced dopamine turnover in the hypothalamus compared to the diet-resistant strain before they become obese and only develop obesity when given a palatable high-energy diet [34,35]. D2 receptor blockade causes obese but not lean rats to overeat [31,36], suggesting that blockade of already low D2 receptor availability may sensitize obese rats to food [37]. Obese versus lean humans show reduced striatal D2 receptor density [38,39]. When exposed to the same high-fat diet, mice with lower D2 receptor density in the putamen show more weight gain than mice with higher D2 receptor density in this region [40]. Dopamine antagonists increase appetite, energy intake, and weight gain, whereas dopamine agonists reduce energy intake and produce weight loss [41,42,43,44].
Studies in neuroeconomics indicate that activation in several areas of the brain correlate positively with the size of the monetary reward and reward size [45]. Similar findings have emerged for food reward [46]. Moreover, such responses vary with hunger and satiety. Responses to food taste in the midbrain, insula, dorsal striatum, subcallosal cingulate, dorsolateral prefrontal cortex, and dorsal medial prefrontal cortex are stronger in a fasting versus a sated state, presumably reflecting the greater reward value of food induced by deprivation [47,48]. Such data suggest that responses to food in several brain regions can be used as an index of reward responsivity.
Although few brain imaging studies have compared lean and obese individuals using paradigms that assess activation of reward circuitry, certain findings align with the thesis that obese individuals show hyper-responsiveness in brain regions implicated in food reward. A Positron Emission Tomography (PET) study found that obese relative to lean adults showed greater resting metabolic activity in the oral somatosensory cortex, a region that encodes sensation in the mouth, lips, and tongue [8], prompting the authors to speculate that enhanced activity in this region may render obese individuals more sensitive to the rewarding properties of food and increase risk for overeating, though this has not been directly confirmed. Extending these findings, a functional magnetic resonance imaging (fMRI) study conducted by our lab to examine the neural response of obese and lean adolescents to a primary reward (food) found that obese versus lean adolescents showed greater activation in the oral somatosensory cortex in response to receipt of chocolate milkshake versus receipt of tasteless solution [49]. These data collectively suggest that obese relative to lean individuals have an enhanced neural architecture in this region. Future research should use voxel-based morphometry to test whether obese individuals show higher grey matter density or volume in this region relative to lean individuals.
Studies using PET found that the mid dorsal insula, midbrain, and posterior hippocampus remain abnormally responsive to consumption of food in previously obese individuals compared to lean individuals [50,51], prompting those authors to speculate that these abnormal responses may increase risk for obesity. Our lab has found that obese relative to lean adolescents show greater activation of the anterior insula/frontal operculum in response to food consumption [49]. The insular cortex has been implicated in a variety of functions related to the integration of autonomic, behavioral, and emotional responses [51]. Specifically, the human neuroimaging literature suggests that the insular cortex has anatomically distinct regions that sustain different functions regarding taste processing [52–55]. Mid insula has found to respond to perceived intensity of a taste irrespective of affective valuation, while valence-specific responses are observed in anterior insula/frontal operculum [54]. Interestingly obese versus lean individuals show increased activation in both regions during consumption of food, suggesting that they may perceive greater taste intensity as well as experience increased reward.
Animal research also implicates a hyper-responsiveness of the dopamine target regions in obesity. Specifically, Yang and Meguid [56] found that obese rats show more release of dopamine in the hypothalamus during feeding than do lean rats. However, to date no PET imaging study has tested whether obese humans showed greater dopamine release in response to food intake relative to lean humans.
Other findings stand in contrast to models of hyper-responsiveness and instead are consistent with the hypothesis that obese individuals show hypo-responsivity of reward circuitry. Obese relative to lean rodents show less striatal D2 receptor binding [32]. PET studies likewise find that obese relative to lean humans show less striatal D2 receptor binding [38,39], leading these authors to speculate that obese individuals experience less subjective reward from food intake because they have fewer D2 receptors and lower DA signal transduction. This is an intriguing hypothesis, though a few caveats warrant attention. First, the proposed inverse relation between D2 receptor availability and subjective reward from food intake is difficult to reconcile with the finding that humans with lower D2 receptor availability report greater subjective reward from methylphenidate than humans with more D2 receptors [57]. If reduced striatal D2 receptors availability produces attenuated subjective reward, it is unclear why individuals with lower D2 binding report that psychostimulants are more subjectively rewarding. Resolving this apparent paradox would advance our understanding of the relation between dopamine action and obesity. Methodological issues also warrant attention in interpreting the PET literature on D2 receptors. First, D2 receptors play both a post-synaptic and a pre-synaptic autoregulatory role. Whereas it is generally assumed that PET measures of D2 binding in the striatum are driven by post-synaptic receptors, the precise contribution of pre and post- synaptic signaling is uncertain, and lowered pre-synaptic receptor levels would have the opposite effect of fewer post-synaptic receptors. Second, because benzamide based PET ligands compete with endogenous dopamine, the finding of lowered D2 receptor availability, could arise due to increased tonic dopamine activity [58]. Yet, even though binding potential is modulated by endogenous DA, the correlation between D2 receptor binding in the normal and a dopamine depleted state is extremely high, which suggests that a larger proportion of the variance in D2 binding is due to creptor density and affinity, rather than differences in endogenous DA levels [59]. Another argument against greater tonic dopamine levels in the striatum of obese individuals emerges from data from rodents. Obese rats have decreased basal dopamine levels in the nucleus accumbens and decreased stimulated dopamine release in both the nucleus accumbens and dorsal striatum [60].
Additional animal research links reduced D2 functioning with weight gain. As noted, D2 receptor blockade causes obese but not lean rats to overeat [31,33] suggesting that blockade of already low D2 receptor availability may sensitize obese rats to food [61]. When exposed to the same high-fat diet, mice with lower D2 receptor density in the putamen show more weight gain than mice with higher D2 receptor density in this region [40]. Dopamine antagonists increase appetite, energy intake, and weight gain, whereas dopamine agonists reduce energy intake and produce weight loss [41,42,43,44]. Taken together these data suggest that D2 functioning is not simply a consequence of obesity, but rather increases risk for future weight gain.
Brain imaging data likewise suggest that obesity is associated with a hypo-responsive striatum. In two fMRI studies conducted by our lab, we found that obese versus lean adolescents show less activation in the dorsal striatum in response to food consumption [49,62]. Because we measured BOLD response, we can only speculate that the effects reflect lower D2 receptor density. This interpretation seems reasonable because the presence of the Taq1A A1 allele, which has been associated with reduced dopaminergic signaling in several post mortem and PET studies [63–67], significantly moderated the observed BOLD effects. That is, activation in this region showed a strong inverse relation to concurrent Body Mass Index (BMI) for those with the Taq1A A1 allele, and a weaker relation to BMI for those without this allele [49]. Yet, the blunted striatal activation may also implicate altered dopamine release from food intake rather than a lower D2 receptor density. Accordingly, it will be important to investigate DA release in response to food intake in obese versus lean individuals. The above findings echo evidence that addictive behaviors such as alcohol, nicotine, marijuana, cocaine, and heroin abuse are associated with low expression of D2 receptors and blunted sensitivity of reward circuitry to drugs and financial reward [68,69,70]. Wang and associates [8] posit that deficits in D2 receptors may predispose individuals to use psychoactive drugs or overeat to boost a sluggish dopamine reward system. As noted, a PET study found evidence that lower striatal D2 receptor availability among non-addicted humans was associated with greater self-reported liking in response to methylphenidate [57]. Further, lower D2 receptor availability in the striatum is associated with lower resting metabolism in the prefrontal cortex, which may increase risk for overeating because this latter region has been implicated in inhibitory control [38].
An alternative interpretation of the above findings is that consumption of a high-fat, high-sugar diet leads to down-regulation of D2 receptors [25], paralleling neural response to chronic use of psychoactive drugs [57]. Animal studies suggest that repeated intake of sweet and fatty foods results in down-regulation of post-synaptic D2 receptors, increased D1 receptor binding, and decreased D2 sensitivity and μ-opioid receptor binding [71,72,73]; changes that also occur in response to chronic substance abuse. Interestingly, there is also experimental evidence that increased intake of high-fat foods leads to greater taste preferences for high-fat foods: rats assigned to a high-fat maintenance diet preferred high-fat foods over high-carbohydrates foods, relative to control animals fed a moderate-fat diet or a high-carbohydrate diet [74,75]. These data imply that increased intake of an unhealthy high-fat food results in a preference for that same food type. Accordingly, a priority for research is to test whether abnormalities in brain reward circuitry predate obesity onset and increase risk for future weight gain.
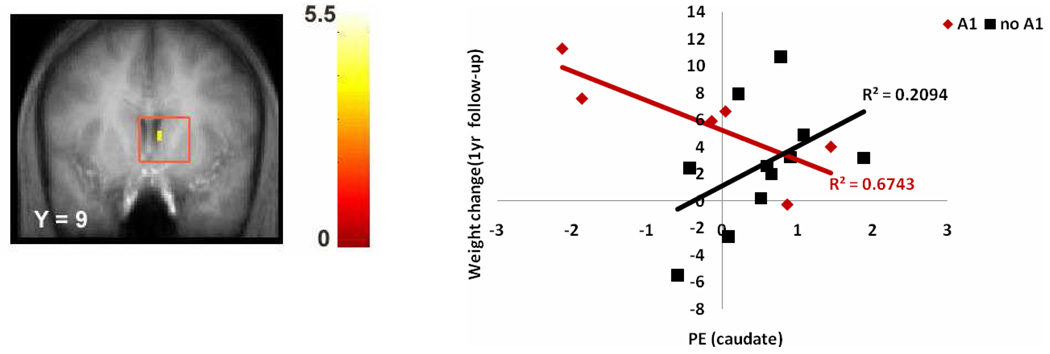
We recently tested whether the degree of activation of the dorsal striatum in response to receipt of a palatable food during an fMRI scan correlated with an increased risk for future weight gain [49]. Although the degree of activation of target brain regions did not show a main effect in predicting weight gain, the relation between abnormal dorsal striatum activation in response to food receipt and weight gain over the subsequent 1-year period was moderated by the A1 allele of the TaqIA gene, which is associated with lower levels of striatal D2 receptors (see section on genotypes that impact dopamine signaling below). Lower striatal activation in response to food receipt increased risk for future weight gain for those with the A1 allele of the TaqIA gene. Interestingly, data suggest that for individuals without the A1 allele, a hyper-responsiveness of the striatum to food receipt predicted weight gain (Fig 1). However, this latter effect was weaker than the strong inverse relation between the striatal response and weight gain in individuals with the A1 allele.
Fig 1.
Coronal section of weaker activation in the caudate (6, 9, 15, z = 2.98, puncorrected = .002) in response to milkshake receipt versus tasteless solution receipt predicting future weight change for each DRD2 allele type with the graph of parameter estimates (PE) from that region.
In sum, extant data suggest that obese relative to lean individuals show a hyper-responsive gustatory cortex and somatosensory cortex in response to food receipt, but that obese individuals also show hypo-responsiveness in the dorsal striatum in response to food intake relative to lean individuals. Thus, extant findings do not accord with a simple hyper-responsivity model or a simple hypo-responsivity model of obesity. A key priority for future research will be to reconcile these seemingly incompatible findings that appear to suggest that obese individuals show both hyper-responsivity and hypo-responsivity of brain regions implicated in food reward relative to lean individuals. As noted, it is possible that chronic intake of high-fat and high-sugar foods, which may result because of the hyper-responsitivity of the gustatory and somatosensory cortices, leads to down-regulation of striatal D2 receptors and the blunted response in this region to intake of palatable foods. Another possibility is that the curtailed reactivity of the dorsal striatum and reduced D2 receptor availability are a product of elevated tonic dopamine among obese relative to lean individuals, which reduces D2 receptor availability and responsivity of dopamine target regions such as the dorsal striatum in response to food receipt. Prospective studies that test whether the hyper-responsivity in the gustatory and somatosensory cortices and hypo-responsivity of the dorsal striatum increases risk for obesity onset should help distinguish abnormalities that are vulnerability factors for unhealthy weight gain versus consequences of a history of overeating or elevated body fat. To date, only one prospective study has tested whether abnormalities in brain regions implicated in food reward increase risk for future weight gain [49]. Another priority for future research will be to determine whether obese individuals show elevated sensitivity to reward in general or only elevated sensitivity to food reward. The evidence that receipt of food, alcohol, nicotine, and money activate similar regions of the brain [23,76,77] and that abnormalities in reward circuitry are associated with obesity, alcoholism, drug abuse, and gambling [9] suggests that obese individuals may show greater sensitivity to reward in general. Yet, it is difficult to draw conclusions because these studies did not assess sensitivity to both general reward and food reward. Obese individuals may show elevated sensitivity to general reward, but even greater sensitivity to food reward.
Anticipated Reward from Food Intake
The literature on reward makes an important distinction between appetitive and consummatory reward, or wanting versus liking [78]. This distinction may be critical for resolving some of the seeming discrepancy between hyper- and hypo- responsivity to food stimuli. Some theorists have hypothesized that the core issue in obesity relates to the anticipatory phase, with greater anticipated reward from food increasing the risk for overeating and obesity [79,80]. Incentive salience theory posits that consummatory and anticipatory reward processes operate in tandem in determining the reinforcement value of food, but that over repeated presentations of food, the hedonic value (liking) decreases, while anticipatory reward increases [81]. Jansen [82] proposed that cues such as the sight and smell of food eventually elicit physiological responses that trigger food craving, increasing risk for further overeating after conditioning.
Imaging studies have identified regions that appear to encode anticipatory food reward in humans. Anticipated receipt of a palatable food, versus unpalatable food or a tasteless food, activates the OFC, amygdala, cingulate gyrus, striatum (caudate nucleus and putamen), dopamine midbrain, parahippocampal gyrus, and fusiform gyrus in men and women [23,79].
Two studies have directly compared activation in response to consumption and anticipated consumption of food to isolate regions that show greater activation in response to one phase of food reward versus the other. Anticipation of a pleasant taste, versus actual taste, resulted in greater activation in the dopaminergic midbrain, ventral striatum, and the posterior right amygdala [23]. Anticipation of a pleasant drink resulted in greater activation in the amygdala and mediodorsal thalamus, whereas the receipt of the drink resulted in greater activation in the left insula/operculum [83]. These studies suggest that the amygdala, midbrain, ventral striatum, and mediodorsal thalamus are more responsive to anticipated consumption of food, whereas the frontal operculum/insula is more responsive to the consumption of food. Anticipation and receipt of money, alcohol, and nicotine also activate somewhat distinct regions that correspond to those that are implicated in anticipatory and consummatory food reward [76,84,85,86].
The ventral striatum and insula show greater activation in response to viewing images of high calorie versus low calorie foods [87,88], implying that activation in these regions is a response to the greater motivational salience of high-calorie foods. Responses to food images in the amygdala, parahippocampal gyrus, and anterior fusiform gyrus were stronger while fasting, verse sated [89], and responses to food images in the brainstem, parahippocampal gyrus, culmen, globus pallidus, middle temporal gyrus, inferior frontal gyrus, middle frontal gyrus, and lingual gyrus were stronger after 10% weight loss relative to initial overweight [90], presumably reflecting the greater reward value of food induced by deprivation. Increases in self-reported hunger in response to presentation of food cues were positively correlated with greater activation of the OFC, insula, and hypothalamus/thalamus [91,92,93]. Transcranial magnetic stimulation of the prefrontal cortex attenuates food craving [94], providing further evidence of the role of the prefrontal cortex in anticipatory food reward. Stimulation of this area also reduces urges to smoke and smoking [94], implying that the prefrontal cortex plays a broader role in anticipated reward.
A critical feature of reward coding shifts from food intake to anticipated food intake after conditioning. Naïve monkeys that had not received food in a particular setting showed activation of dopamine neurons only in response to food taste; however, after conditioning, dopaminergic activity began to precede reward delivery and eventually maximal activity was elicited by the conditioned stimuli that predicted the impending reward rather than by actual food receipt [95,96]. Kiyatkin and Gratton [97] found that the greatest dopaminergic activation occurred in an anticipatory fashion as rats approached and pressed a bar that produced food reward and activation actually decreases as the rat received and ate the food. Blackburn [98] found that dopamine activity was greater in the nucleus accumbens of rats after presentation of a conditioned stimulus that usually signaled food receipt than after delivery of an unexpected meal. These data do not argue against models of phasic dopamine firing that emphasize the role of dopamine in signaling positive prediction errors [99], but rather emphasize the importance of dopamine in the preparation for, and anticipation of food reward.
A history of elevated sugar intake may contribute to abnormal elevations in anticipatory reward from food [100]. Rats exposed to intermittent sugar availability show signs of dependence (escalation in bouts of an abnormally large intake of sugar, μ-opiod and dopamine receptor changes, and deprivation-induced sugar binges) and somatic, neurochemical, and behavioral signs of opioid withdrawal that are precipitated by administration of naloxone, as well as cross-sensitization with amphetamine [100,101]. Experimentally induced drug cravings among addicted adults activate the right OFC [102,103], paralleling activation in this region caused by exposure to food cues [93], suggesting that disrupted orbitofrontal activity could give rise to overeating.
Self-reported food cravings correlate positively with BMI and objectively measured caloric intake [22,104,105,106]. Obese individuals report stronger craving of high-fat, high-sugar foods than lean individuals [16,107,108]. Obese adults work harder for food and work for more food than lean adults [19,37,109]. Relative to lean children, obese children are more likely to eat in the absence of hunger [110] and work harder for food [111].
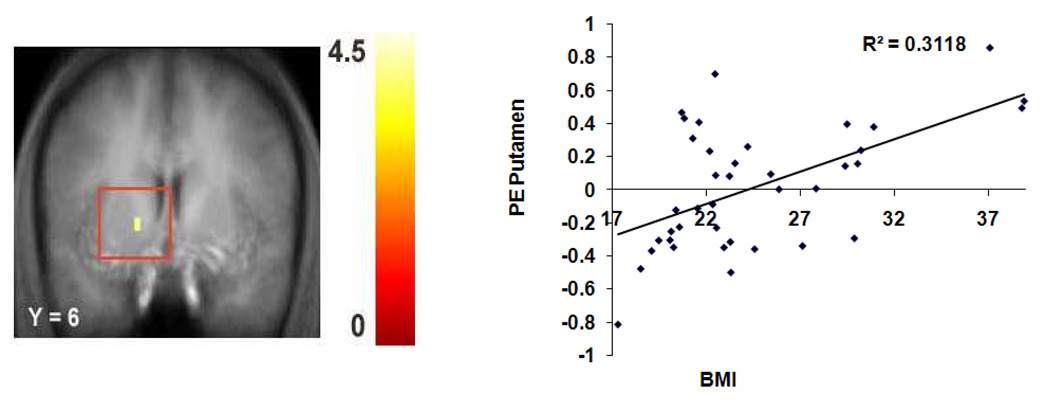
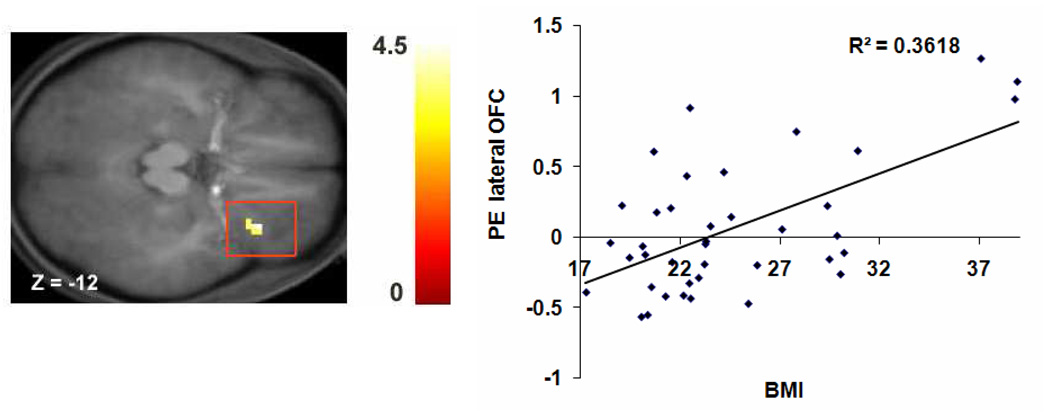
Studies have compared the brain activation in response to presentation of food cues among obese verse lean individuals. Karhunen [112] found increased activation in the right parietal and temporal cortices after exposure to food images in obese but not lean women and that this activation correlated positively with hunger ratings. Rothemund [113] found greater dorsal striatum responses to pictures of high-calorie foods in obese verse lean adults and that BMI correlated positively with response in insula, claustrum, cingulate, postcentral gyrus (somatosensory cortex) and lateral OFC. Stoeckel [114] found greater activation in the medial and lateral OFC, amygdala, ventral striatum, medial prefrontal cortex, insula, anterior cingulate cortex, ventral pallidum, caudate, and hippocampus in response to pictures of high-calorie versus low-calorie foods for obese relative to lean individuals. Stice, Spoor, and Marti [115] found that BMI correlated positively with activation in the putamen (Fig 2) in response to pictures of appetizing food versus unappetizing food and activation in the lateral OFC (Fig 3) and frontal operculum in response to pictures of appetizing food versus glasses of water.
Fig 2.
Coronal section of increased activation in the putamen (-15, 6, 3, z = 3.59, puncorrected < .001) in response to appetizing food – unappetizing food as a function of BMI with the graph of parameter estimates (PE) from that region.
Fig 3.
Axial section of increased activation in the lateral orbitofrontal cortex (OFC) (33, 27, −12, z = 4.01, puncorrected < .001) in response to appetizing food versus water as a function of BMI with the graph of parameter estimates (PE) of that region.
Although the above neuroimaging studies have advanced our understanding of the responsivity of certain brain regions to food images, it is not clear whether these studies capture anticipation of food intake, since they did not involve consumption of the food stimuli during scanning. To our knowledge, only one imaging study has compared obese to lean individuals using a paradigm in which anticipated receipt of food was investigated. We found that obese adolescents showed greater activation of Rolandic, temporal, frontal and parietal opercular regions in response to anticipation of food consumption relative to lean adolescents [49].
In sum, self-report, behavioral, and brain imaging data suggest that obese individuals show greater anticipated food reward than lean individuals. Thus, obesity may arise as a consequence of a hyper-responsiveness in the anticipatory “wanting” system. We believe the field would benefit from more imaging studies that directly test whether obese individuals show evidence of greater anticipatory food reward in response to presentation of actual food as opposed to foods that are not obtainable. Importantly, no imaging studies to date have tested whether elevations in anticipatory food reward increase risk for unhealthy weight gain and obesity onset, making this a key priority for future research. It will also be important to test whether elevated intake of high-fat and high-sugar foods contributes to elevated anticipatory food reward.
Moderators of Reward Sensitivity
Two lines of evidence suggest that it is important to examine moderators that interact with abnormalities in food reward to increase risk for obesity. Data indicates that food, psychoactive substance use, and monetary reward activate similar brain regions [23,76,77,86]. Additionally, abnormalities in reward circuitry are associated with obesity, substance abuse, and gambling [9,116]. Indeed, there is mounting evidence of a relation between food and drug reinforcement. Food deprivation increases the reinforcement value of food and psychoactive drugs [117,118], an effect that is at least partially mediated through changes in dopamine signal [119]. Elevated sucrose preference in animals is associated with greater self-administration of cocaine [120] and sucrose intake reduces cocaine’s reinforcing value [121]. Neuroimaging data also suggest similarities in the dopamine profiles of drug abusers and obese individuals [39,122].
Although there are numerous factors that may moderate the relation between abnormalities in food reward and obesity, three in particular seem theoretically reasonable: (1) the presence of genotypes associated with reduced dopamine signaling in reward circuitry (DRD2, DRD4, DAT, COMT), (2) trait impulsivity, which theoretically increases risk for responding to a variety of appetitive stimuli, and (3) an unhealthy food environment.
Genotypes that impact dopamine signaling
Given that dopamine plays a key role in the reward circuitry and is involved in food reward [25,123,124], it follows that genetic polymorphisms that affect the availability of dopamine and functioning of dopamine receptors could moderate the effects of abnormalities in food reward on risk for overeating. Several genes influence dopamine functioning, including those that affect dopamine receptors, transport, and breakdown.
To date, the strongest empirical support has emerged for the TaqIA polymorphism of the DRD2 gene. The TaqIA polymorphism (rs1800497) has three allelic variants: A1/A1, A1/A2, & A2/A2. TaqIA was originally thought to be located in the 3’ –untranslated region of DRD2, but it actually resides in the neighboring ANKK1 gene [125]. Estimates suggest that individuals with genotypes containing one or two copies of the A1 allele have 30–40% fewer striatal D2 receptors and compromised brain dopamine signaling than those without an A1 allele [126,127,128]. Those with the A1 allele have reduced resting glucose utilization in striatal regions (putamen and nucleus accumbens), prefrontal, and insula [70] - regions implicated in food reward. Theoretically, the A1 allele is associated with hypofunctioning of the meso-limbic regions, prefrontal cortex, hypothalamus, and amygdala [9]. Low D2 receptor density associated with the A1 allele putatively makes individuals less sensitive to the activation of dopamine-based reward circuitry, rendering them more likely to overeat, use psychoactive substances, or engage in other activities like gambling to overcome this dopamine deficit [57]. In genetically homogeneous and heterogeneous samples, the A1 allele is associated with elevated obesity [129,130,131,132,133,134,135]. Perhaps because of conditioning that occurs during overeating bouts, individuals with the A1 allele report greater food craving, work for more food in operant tasks, and consume more food ad lib than those without this allele [37,116].
Importantly, the relation between abnormalities in food reinforcement and objectively measured food intake is moderated by the A1 allele. Epstein [136] found an interaction between A1 allele and anticipatory food reward among adults, such that the greatest food intake occurred for those who reported elevated reinforcement from food and had the A1 allele. Likewise, Epstein [37] found a significant interaction between the A1 allele and anticipatory food reward among adults, such that the greatest food intake occurred among those who worked the hardest to earn snacks and had the A1 allele. As noted, Stice [49] found that the relation between a blunted dorsal striatal response to food receipt predicted increased risk for future weight gain over a 1-year follow-up for individuals with an A1 allele.
The 7-repeat or longer allele of the DRD4 (DRD4-L) gene has been linked to reduced D4 receptor signaling in an in vitro study [137], to poorer response to methylphenidate in attention deficit/hyperkinetic disorders [138,139], and to less dopamine release in the ventral striatum after nicotine use [140], suggesting it may be related to reward sensitivity. The DRD4 is a postsynaptic receptor that is principally inhibitory of the second messenger adenylate cyclase. Thus, it has been conjectured that those with the DRD4-L allele may show greater impulsivity [138]. D4 receptors are predominantly localized in areas that are innervated by mesocortical projections from the ventral tegmental area, including the prefrontal cortex, cingulate gyrus, and insula [141]. Humans with versus without the DRD4-L allele have shown higher maximum lifetime BMI in samples at risk for obesity, including individuals with Seasonal Affective Disorder who report overeating [142], individuals with bulimia nervosa [143], and African-American adolescents [144], but this relation did not emerge in two samples of adolescents [145,146]. It may be difficult to detect genetic effects in a sample of individuals who have not yet passed through the period of greatest risk for obesity onset. Adults with versus without the DRD4-L allele have shown increased food cravings in response to food cues [147], increased smoking cravings and activation of the superior frontal gyrus and insula in response to smoking cues [148,149], increased alcohol cravings in response to tasting alcohol [150], and increased heroine craving in response to heroine cues [151].
Phasically released dopamine is normally eliminated by rapid reuptake through the dopamine transporter (DAT), which is abundant in the striatum [152]. DAT regulates synaptic dopamine concentration by reuptake of the neurotransmitter into presynaptic terminals. Lower DAT expression, which is associated with the 10 repeat allele (DAT-L), may reduce synaptic clearance and therefore produce higher basal dopamine levels, but blunted phasic dopamine release [140]. Pecina [153] found that disruption of the DAT gene produced increased synaptic dopamine along with an elevated energy intake and preference for palatable foods in mice. A high-fat diet significantly decreased DAT density in the dorsal and ventral parts of the caudal caudate putamen compared to a low-fat diet in mice [154]. Lower striatal DAT availability has been associated with elevated BMI in humans [155]. DAT-L has been associated with obesity in African American smokers, but not in other ethnic groups [156]. Adults with versus without the DAT-L allele showed blunted phasic release of dopamine in response to cigarette smoking [140].
Catechol-o-methyltransferase (COMT) regulates extrasynaptical dopamine breakdown, particularly in the prefrontal cortex, where COMT is more abundant than in the striatum [157]. However, COMT also has a small local effect in the striatum [158] and influences dopamine levels in the striatum via the glutamatergic efferents from the prefrontal cortex to the striatum [159]. A single nucleotide exchange in the COMT gene, which causes a valine to methionine (Val/Met-158) substitution produces a 4-fold reduction in COMT activity in Met relative to Val homozygotes, putatively causing the Met homozygotes to have increased tonic dopamine levels in the prefrontal cortex and striatum and less phasic release of dopamine [140,159]. People with versus without the Met allele show elevated general reward sensitivity as indexed by BOLD responses during reward anticipation or reward selection [160,161] and substance use [162]. Wang [154] found that individuals with the Met allele versus without were more likely to show at least a 30% increase in BMI from age 20 to age 50 (based on retrospective reports).
Trait impulsivity
It has been theorized that impulsive individuals are more sensitive to cues for reward and more vulnerable to the omnipresent temptation of palatable foods in our obesogenic environment [164,165] leading to the hypothesis that the greatest weight gain will occur for youth showing food reward abnormalities and trait impulsivity. Self-reported impulsivity correlates positively with obesity status [166,167,168] objectively measured caloric intake [169] and negatively with weight loss during obesity treatment [169,170,171]. Obese relative to lean individuals show more difficulties with response inhibition on behavioral go-no-go and stop-signal tasks and show more sensitivity to reward in a gambling task [172,173]. Overweight versus lean children consume more calories after exposure to food cues, such as smelling and tasting a palatable food [174], suggesting that the former are more likely to give in to cravings resulting from food cues. Obese relative to lean individuals have shown a preference for high immediate gain, but larger future losses on behavioral measures in some studies [5,175], but not others [173,176].
Affect regulation expectancies
We also hypothesize that among individuals with abnormalities in food reward, those who believe that eating reduces negative affect and enhances positive affect would be more likely to overeat and show excessive weight gain relative to those not holding these beliefs. Indeed, different affect-regulation expectancies may be a key moderator that determines whether individuals with abnormalities in general reward sensitivity show onset of obesity, versus substance abuse; we posit that those who believe eating improves affect are more likely to go the former route, whereas those who believe that substance use improves affect may be more likely to go the latter route. Corr [177] has likewise posited that the relation between reward sensitivity and response to that reward is moderated by individual differences in affect-regulation expectancies. In support, self-reported reward sensitivity was only related to reward responsivity on a behavioral task for participants who expected the task to be reinforcing [178]. More generally, individuals who believe that eating reduces negative affect and improves positive affect are more likely to show increases in binge eating over a 2-year follow-up than those not holding this belief [179]. We found that among individuals who binge eat, those who believe that eating reduces negative affect and improves positive affect are more likely to show persistence of binge eating over a 1-year follow-up relative to those not holding this belief [180]. Further, individuals who believe that smoking and alcohol use improves affect are more likely to show increases in their smoking and alcohol use relative to those not holding these affect-regulation expectances [181,182].
Food Environment
Researchers have argued that the prevalence of high-fat and high-sugar foods in the home, schools, grocery stores, and restaurants increases risk for obesity [183,184,185]. Theoretically, cues for unhealthy foods (sight of the packaging, the smell of French fries) increase the likelihood of intake of these foods, which contributes to unhealthy weight gain [186]. Individuals who live in homes with many high-fat and high-sugar foods eat more of these unhealthy foods, whereas those who live in homes with fruits and vegetables eat more of these healthy foods [187,188,189]. Most foods sold in vending machines and a la carte at schools are high in fat and sugar [185,190]. Students at schools with vending machines and a la carte shops consume more fat and less fruits and vegetables than students in other schools [190]. Over 35% of adolescents eat fast food daily and those who frequent these restaurants consume more calories and fat than those who do not [191]. Fast food restaurants are often closely located to schools [192]. At the regional level, fast food restaurant density is associated with obesity and obesity-related morbidity [193,194,195], though null findings have also been reported [196,197]. Thus, we hypothesize that the relation of abnormalities in food reward to risk for future weight gain will be stronger for participants in an unhealthy food environment.
Conclusions and Directions for Future Research
In this report we reviewed recent findings from studies that have investigated whether abnormalities in reward from food intake and anticipated food intake correlate with concurrent BMI and future increases in BMI. Overall, the literature suggests that obese versus lean individuals anticipate greater reward from food intake; relatively consistent findings have emerged from studies using brain imaging, self-report and behavioral measures to assess anticipatory food reward. Further, studies using self-report and behavioral measures found that obese relative to lean individuals report greater reward from food intake and that preferences for high-fat and high-sugar foods predict elevated weight gain and increased risk for obesity. Brain imaging studies have likewise found that obese compared to lean individuals show greater activation in the gustatory cortex and somatosensory cortex in response to food receipt, which may imply that consuming food is more pleasurable from a sensory perspective. However, several imaging studies also found that obese showed less activation in the dorsal striatum in response to food intake relative to lean individuals, suggesting blunted activation of reward circuitry. Thus, as noted, extant data do not lend clear support to a simple hyper-responsivity or a simple hypo-responsivity model of obesity.
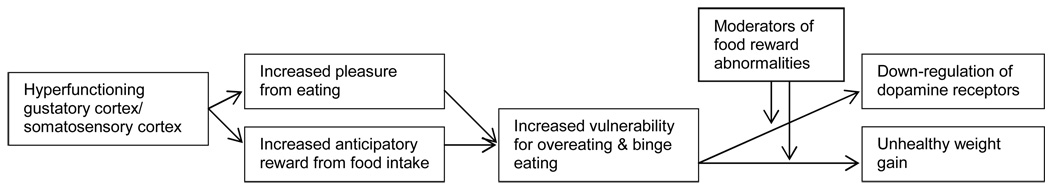
Given this set of affairs, and the evidence from animal studies suggesting that intake of high-fat and high-sugar foods results in down-regulation of D2 receptors, we propose a provisional working conceptual model (Fig 4) in which we posit that people at risk for obesity initially show a hyperfunctioning in the gustatory cortex as well as in the somatosensory cortex that makes consuming food more pleasurable from a sensory perspective, which may lead to greater anticipatory reward from food and increased vulnerability to overeating, resulting in consequent unhealthy weight gain. We hypothesize that this overeating may lead to receptor down-regulation in the striatum secondary to excessive intake of overly rich foods, which may increase the likelihood of further overeating and continued weigh gain. Yet, it is important to note that obese compared to lean showed elevated activation in the dorsal striatum in response to anticipated food intake, suggesting a differential impact on anticipatory and consummatory food reward.
Fig 4.
Working conceptual model presenting the relation between abnormalities in food reward and risk for unhealthy weight gain.
A priority for future research will be to test whether abnormalities in brain reward circuitry increase risk for unhealthy weight gain and onset of obesity. Only one prospective study thus far has tested whether abnormalities in brain regions implicated in anticipatory and consummatory food reward increase risk for future weight gain. Specifically, future studies should examine whether somatosensory and striatum disturbances are primary or secondary to a chronic intake of a high-fat, high-sugar diet. It will be important to test key assumptions regarding the interpretation of these findings, such as whether reduced sensitivity of the somatosensory and gustatory regions translates into reduced subjective pleasure during food intake. Future research should also strive to resolve the apparently inconsistent findings suggesting that obese individuals show hyper-responsivity of some brain regions to food intake, but hypo-responsivity of other brain regions, relative to lean individuals. There is a particular need to integrate measurement of dopamine functioning with functional MRI measures of striatal and cortical responses to food. The literature review suggests that dopamine functioning is linked to differences in food reward sensitivity. However, because existing studies in humans have either used functional MRI measures of responses to food, or PET measures of DA binding, but have never measured both in the same participants, it is unclear to what extent food reward sensitivity is dependent on DA mechanisms and whether this explains the differential responsivity in obese versus lean individuals. Thus, studies taking a multimodal imaging approach utilizing both PET and functional MRI would contribute to an improved understanding of the etiologic processes that give rise to obesity. Finally, recent data from brain imaging studies have allowed us to begin exploring how these abnormalities in food reward may interact with certain genetic and environmental factors, such as genes related to reduced dopamine signaling, trait impulsivity, affect regulation expectancies, and an unhealthy food environment. Future research should continue to explore factors that moderate the risk conveyed by abnormalities in reward circuitry in response to food receipt and anticipated receipt to increase risk for unhealthy weight gain.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Eric Stice, Oregon Research Institute.
Sonja Spoor, University of Texas at Austin.
Janet Ng, University of Oregon.
David H. Zald, Vanderbilt University
References
- 1.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 2.Hedley AA, Odgen CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2000. JAMA. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 3.Jeffery R, Drewnowski A, Epstein LH, Stunkard AJ, Wilson GT, Wing RR, Hill D. Longterm maintenance of weight loss: Current status. Health Psychology. 2000;19:5–16. doi: 10.1037/0278-6133.19.suppl1.5. [DOI] [PubMed] [Google Scholar]
- 4.Stice E, Shaw H, Marti CN. A meta-analytic review of obesity prevention programs for children and adolescents: The skinny on interventions that work. Psychological Bulletin. 2006;132:667–691. doi: 10.1037/0033-2909.132.5.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davis C, Strachan S, Berkson M. Sensitivity to reward: Implications for overeating and obesity. Appetite. 2004;42:131–138. doi: 10.1016/j.appet.2003.07.004. [DOI] [PubMed] [Google Scholar]
- 6.Dawe S, Loxton NJ. The role of impulsivity in the development of substance use and eating disorders. Neuroscience and Biobehavioral Review. 2004;28:343–351. doi: 10.1016/j.neubiorev.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Blum K, Braverman ER, Holder JM, Lubar JF, Monastra VJ, Miller D, et al. Reward deficiency syndrome: A biogenic model for the diagnosis and treatment of impulsive, addictive, and compulsive behaviors. Journal of Psychoactive Drugs. 2000 doi: 10.1080/02791072.2000.10736099. 32S:1-vi. [DOI] [PubMed] [Google Scholar]
- 8.Wang GJ, Volkow ND, Fowler JS. The role of dopamine in motivation for food in humans: implications for obesity. Expert Opinion on Therapeutic Targets. 2002;6:601–609. doi: 10.1517/14728222.6.5.601. [DOI] [PubMed] [Google Scholar]
- 9.Bowirrat A, Oscar-Berman M. Relationship between dopaminergic neurotransmission, alcoholism, and reward deficiency syndrome. American Journal of Medical Genetics. Neuropsychaitric. 2005;132B:29–37. doi: 10.1002/ajmg.b.30080. [DOI] [PubMed] [Google Scholar]
- 10.McGloin AF, Livingstone MB, Greene LC, Webb SE, Gibson JM, Jebb SA, et al. Energy and fat intake in obese children and lean children at varying risk of obesity. International Journal of Obesity. 2002;26:200–207. doi: 10.1038/sj.ijo.0801883. [DOI] [PubMed] [Google Scholar]
- 11.Nicklas TA, Yang SJ, Baranowski T, Zakeri I, Berenson G. Eating patterns and obesity in children: The Bogalusa heart study. American Journal of Preventive Medicine. 2003;25:9–16. doi: 10.1016/s0749-3797(03)00098-9. [DOI] [PubMed] [Google Scholar]
- 12.Rissanen A, Hakala P, Lissner L, Mattlar CE, Koskenvuo M, Ronnemaa T. Acquired preference especially for dietary fat and obesity: A study of weight-discordant monozygotic twin pairs. International Journal of Obesity. 2002;26:973–977. doi: 10.1038/sj.ijo.0802014. [DOI] [PubMed] [Google Scholar]
- 13.Fisher JO, Birch LL. Fat preferences and fat consumption of 3- to 5-year-old children are related to parental adiposity. Journal of the American Dietetic Association. 1995;95:759–764. doi: 10.1016/S0002-8223(95)00212-X. [DOI] [PubMed] [Google Scholar]
- 14.Stunkard AJ, Berkowitz RI, Stallings VA, Schoeller DA. Energy intake, not energy output, is a determinant of body size in infants. American Journal of Clinical Nutrition. 1999;69:524–530. doi: 10.1093/ajcn/69.3.524. [DOI] [PubMed] [Google Scholar]
- 15.Wardle J, Guthrie C, Sanderson S, Birch D, Plomin R. Food and activity preferences in children of lean and obese parents. International Journal of Obesity. 2001;25:971–977. doi: 10.1038/sj.ijo.0801661. [DOI] [PubMed] [Google Scholar]
- 16.Drewnowski A, Kurth C, Holden-Wiltse J, Saari J. Food preferences in human obesity: Carbohydrates versus fats. Appetite. 1996;18:207–221. doi: 10.1016/0195-6663(92)90198-f. [DOI] [PubMed] [Google Scholar]
- 17.Salbe AD, DelParigi A, Pratley RE, Drewnowski A, Tataranni PA. Taste preferences and body weight changes in an obesity-prone population. The American Journal of Clinical Nutrition. 2004;79:372–378. doi: 10.1093/ajcn/79.3.372. [DOI] [PubMed] [Google Scholar]
- 18.Jacobs SB, Wagner MK. Obese and nonobese individuals: Behavioral and personality characteristics. Addictive Behaviors. 1984;9:223–226. doi: 10.1016/0306-4603(84)90062-5. [DOI] [PubMed] [Google Scholar]
- 19.Saelens BE, Epstein LH. The reinforcing value of food in obese and non-obese women. Appetite. 1996;27:41–50. doi: 10.1006/appe.1996.0032. [DOI] [PubMed] [Google Scholar]
- 20.Westenhoefer J, Pudel V. Pleasure from food: Importance for food choice and consequences of deliberate restriction. Appetite. 1993;20:246–249. doi: 10.1006/appe.1993.1029. [DOI] [PubMed] [Google Scholar]
- 21.Davis C, Patte K, Levitan R, Reid C, Tweed S, Curtis C. From motivation to behaviour: a model of reward sensitivity, overeating, and food preferences in the risk profile for obesity. Appetite. 2007;48:12–19. doi: 10.1016/j.appet.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 22.Franken IH, Muris P. Individual differences in reward sensitivity are related to food craving and relative body weight in healthy weight women. Appetite. 2005;45:198–201. doi: 10.1016/j.appet.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 23.O’Doherty JP, Deichmann R, Critchley HD, Dolan RJ. Neural responses during anticipation of a primary taste reward. Neuron. 2002;33:815–826. doi: 10.1016/s0896-6273(02)00603-7. [DOI] [PubMed] [Google Scholar]
- 24.Gottfried J, Small DM, Zald DH. Chemosensory processing. In: Zald DH, Rauch SL, editors. The Orbitofrontal Cortex. Oxford: Oxford University Press; 2006. pp. 125–172. [Google Scholar]
- 25.Small DM, Jones-Gotman M, Dagher A. Feeding-induced dopamine release in dorsal striatum correlates with meal pleasantness ratings in healthy human volunteers. Neuroimage. 2003;19:1709–1715. doi: 10.1016/s1053-8119(03)00253-2. [DOI] [PubMed] [Google Scholar]
- 26.Bassareo V, Di Chiara G. Differential influence of associative and nonassociateive learning mechanisms on the responsiveness of prefrontal and accumbal dopamine transmissioin to food stimuli in rats fed ad libitum. Journal of Neuroscience. 1997;17:851–861. doi: 10.1523/JNEUROSCI.17-02-00851.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hajnal A, Smith GP, Norgren R. Oral sucrose stimulation increases accumbens dopamine in the rat. American J Physiology Regulatory Integrative Comp Physiology. 2004;286:R31–R37. doi: 10.1152/ajpregu.00282.2003. [DOI] [PubMed] [Google Scholar]
- 28.Rada P, Avena NM, Hoebel BG. Daily bingeing on sugar repeatedly releases dopamine in the accumbens shell. Neuroscience. 2005;134:737–744. doi: 10.1016/j.neuroscience.2005.04.043. [DOI] [PubMed] [Google Scholar]
- 29.Kelley AE. Ventral striatal control of appetitive motivation: Role in ingestive behavior and rewardrelated learning. Neuroscience and Biobehavioral Review. 2004;27:765–776. doi: 10.1016/j.neubiorev.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 30.Petrovich GD, Setlow B, Holland PC, Gallagher M. Amygdalo-hypothalamic circuit allows learned cues to override satiety and promote eating. Journal of Neuroscience. 2002;22:8746–8753. doi: 10.1523/JNEUROSCI.22-19-08748.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fetissov SO, Meguid MM, Sato T, Zhang LH. Expression of dopaminergic receptors in the hypothalamus of lean and obese Zucker rates and food intake. American Journal of Physiology - Regulatory, integrative and comparative psychology. 2002;283:R905–R910. doi: 10.1152/ajpregu.00092.2002. [DOI] [PubMed] [Google Scholar]
- 32.Hamdi A, Porter J, Prasad C. Decreased striatal D2 dopamine receptors in obese Zucker rats: Changes during aging. Brain Research. 1992;589:338–340. doi: 10.1016/0006-8993(92)91296-q. [DOI] [PubMed] [Google Scholar]
- 33.Orosco M, Rouch C, Nicolaidis S. Rostromedial hypothalamic monoamine changes in response to intravenous infusions of insulin and glucose in freely feeding obese Zucker Rats: A microdialysis study. Appetite. 1996;26:1–20. doi: 10.1006/appe.1996.0001. [DOI] [PubMed] [Google Scholar]
- 34.Levin B, Dunn-Meynell A, Balkan B, Keesey R. Selective breeding for diet-induced obesity and resistance in Sprague-Dawley rats. Am J Physiol Regul Integr Comp Physiol. 1997;273:R725–R730. doi: 10.1152/ajpregu.1997.273.2.R725. [DOI] [PubMed] [Google Scholar]
- 35.Levin B, Dunn-Meynell A. Reduced central leptin sensitivity in rats with diet-induced obesity. Am Physiological Soc. 2002;283:R941–R948. doi: 10.1152/ajpregu.00245.2002. [DOI] [PubMed] [Google Scholar]
- 36.Orosco M, Gerozisis K, Rouch C, Meile MJ, Nicolaidis S. Hypothalamic monoamines and insulin in relation to feeding in the genetically obese Zucker rat as revealed by microdialysis. Obesity Research. 1995;3:S655–S665. doi: 10.1002/j.1550-8528.1995.tb00483.x. [DOI] [PubMed] [Google Scholar]
- 37.Epstein LJ, Leddy JJ, Temple JL, Faith MS. Food reinforcement and eating: A multilevel analysis. Psychological Bulletin. 2007;133:884–906. doi: 10.1037/0033-2909.133.5.884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Volkow ND, Wang GJ, Telang F, Fowler JS, Thanos PK, Logan J, et al. Low dopamine striatal D2 receptors are associated with prefrontal metabolism in obese subjects: Possible contributing factors. Neuroimage. 2008;42:1537–1543. doi: 10.1016/j.neuroimage.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang GJ, Volkow ND, Logan J, Pappas NR, Wong CT, Zhu W, et al. Brain dopamine and obesity. Lancet. 2001;357:354–357. doi: 10.1016/s0140-6736(00)03643-6. [DOI] [PubMed] [Google Scholar]
- 40.Huang XF, Zavitsanou K, Huang X, Yu Y, Wang H, Chen F, et al. Dopamine transporter and D2 receptor binding densities in mice prone or resistant to chronic high fat diet-incuded obesity. Behavioural Brain Research. 2006;175:415–419. doi: 10.1016/j.bbr.2006.08.034. [DOI] [PubMed] [Google Scholar]
- 41.Baptista T, Lopez M, Teneud L, Contreras Q, Alastre T, De Quijada M, Alternus E, Weiss R, Museeo E, Paez X, Hernandez L. Amantadine in the treatment of neuroleptic-induced obesity in rats: Behavioral, endocrine and neurochemical correlates. Pharmacopsychiatry. 1997;30:43–54. doi: 10.1055/s-2007-979482. [DOI] [PubMed] [Google Scholar]
- 42.Bina KG, Cincotta AH. Dopaminergic agonists normalize elevated hypothalamic neuropeptide Y and corticotropin-releasing hormone, body weight gain, and hyperglycemia in ob/ob mice. Neuroendocrinology. 2000;71:68–78. doi: 10.1159/000054522. [DOI] [PubMed] [Google Scholar]
- 43.Leddy JJ, Epstein LH, Jaroni JL, Roemmich JN, Paluch RA, Goldfield GS, et al. The influence of methylphenidate on eating in obese men. Obesity Research. 2004;12:224–232. doi: 10.1038/oby.2004.29. [DOI] [PubMed] [Google Scholar]
- 44.Lee MD, Clifton PG. Meal patterns of free feeding rats treated with clozapine, olanzapine, or haloperidol. Pharmacology Biochemistry and Behaivor. 2002;71:147–154. doi: 10.1016/s0091-3057(01)00630-x. [DOI] [PubMed] [Google Scholar]
- 45.Montague PR, Berns GS. Neural economics and the biological substrates of valuation. Neuron. 2002;36:265–284. doi: 10.1016/s0896-6273(02)00974-1. [DOI] [PubMed] [Google Scholar]
- 46.Kringelbach ML, O’Doherty J, Rolls ET, Andrews C. Activation of the human orbitofrontal cortex to a liquid food stimulus is correlated with its subjective pleasantness. Cereb Cortex. 2003;13:1064–1071. doi: 10.1093/cercor/13.10.1064. [DOI] [PubMed] [Google Scholar]
- 47.Small DM, Zatorre RJ, Dagher A, Evans AC, Jones-Gotman M. Changes in brain activity related to eating chocolate: From pleasure to aversion. Brain. 2001;124:1720–1733. doi: 10.1093/brain/124.9.1720. [DOI] [PubMed] [Google Scholar]
- 48.Uher R, Treasure J, Heining M, Brammer MJ, Campbell IC. Cerebral processing of food related stimuli: Effects of fasting and gender. Behavioural Brain Research. 2006;169:111–119. doi: 10.1016/j.bbr.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 49.Stice E, Spoor S, Bohon C, Small DM. Relation between obesity and blunted striatal response to food is moderated by TaqlA1 DRD2 gene. Science. 2008;322:449–452. doi: 10.1126/science.1161550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Del Parigi A, Chen K, Hill DO, Wing RR, Reiman E, Tataranni PA. Persistence of abnormal neural responses to a meal in potobese individuals. International Journal of Obesity. 2004;28:370–377. doi: 10.1038/sj.ijo.0802558. [DOI] [PubMed] [Google Scholar]
- 51.Del Parigi A, Chen K, Salbe AD, Reiman EM, Tataranni PA. Sensory experience of food and obesity: A positron emission tromography study of the brain regions affected by tasting a liquid meal after a prolonged fast. NeuroImage. 2005;24:436–443. doi: 10.1016/j.neuroimage.2004.08.035. [DOI] [PubMed] [Google Scholar]
- 52.Pritchard TC, Macaluso DA, Eslinger PJ. Taste perception in patients with insular cortex lesions. Behavioral Neuroscience. 1999;113:663–671. [PubMed] [Google Scholar]
- 53.de Araujo IET, Kringelbach ML, Rolls ET, McGlone F. Human cortical responses to water in the mouth, and the effects of thirst. Journal of Neurophysiology. 2003;90:1865–1876. doi: 10.1152/jn.00297.2003. [DOI] [PubMed] [Google Scholar]
- 54.Small DM, Geregory MD, Mak YE, Gitelman D, Mesulam MM, Parrish T. Dissociation of neural representation of intensity and affective valuation in human gestation. Neuron. 2003;39:70–711. doi: 10.1016/s0896-6273(03)00467-7. [DOI] [PubMed] [Google Scholar]
- 55.Veldhuizen MG, Bender G, Constable RT, Small DM. Trying to detect taste in a tasteless solution: modulation of early gustatory cortex by attention to taste. Chemical Senses. 2007;32:569–581. doi: 10.1093/chemse/bjm025. [DOI] [PubMed] [Google Scholar]
- 56.Yang ZJ, Meguid MM. Lha dopaminergic activity in obese and lean zucker rats. Neuroreport. 1995;6:1191–1194. doi: 10.1097/00001756-199505300-00029. [DOI] [PubMed] [Google Scholar]
- 57.Volkow ND, Fowler JS, Wang GJ. Role of dopamine in drug reinforcement and addiction in humans: Results from imaging studies. Behavioral Pharmacology. 2002;13:355–366. doi: 10.1097/00008877-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 58.Laruelle M, Huang Y. Vulnerability of positron emission tomography radiotracers to endogenous competition. New insights Q J Nucl Med. 2001;45:124–138. [PubMed] [Google Scholar]
- 59.Laruelle M, D'Souza C, Baldwin R, Abi-Dargham A, Kanes S, Fingado C, Seibyl J. Imaging D2 receptor occupancy by endogenous dopamine in humans. Neuropsychopharmacology. 1997;17:162–174. doi: 10.1016/S0893-133X(97)00043-2. [DOI] [PubMed] [Google Scholar]
- 60.Geiger B, Behr G, Frank L, Caldera-Siu A, Beinfeld M, Kokkotou E, Pothos N. Evidence for defective mesolimbic dopamine exocytosis in obesity-prone rats. The FASEB Journal. 2008;22:2740–2746. doi: 10.1096/fj.08-110759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Epstein LJ, Temple JL, Neaderhiser BJ, Salis RJ, Erbe RW, Leddy J. Food reinforcement, the dopamine D2 receptor genotype, and energy intake in obese and nonobese humans. Behavioral Neuroscience. 2007;121:877–886. doi: 10.1037/0735-7044.121.5.877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Stice E, Spoor S, Bohon C, Veldhuizen M, Small DM. Relation of reward from food intake and anticipated intake to obesity: A functional magnetic resonance imaging study. Journal of Abnormal Psychology. doi: 10.1037/a0013600. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Thompson, et al. D2 dopamine receptor gene (DRD2) Taq1 A polymorphism: reduced dopamine D2 receptor binding in the human striatum associated with the A1 allele. Pharmacogenetics. 1997;7:479–484. doi: 10.1097/00008571-199712000-00006. [DOI] [PubMed] [Google Scholar]
- 64.Pohjalainen T, et al. The A1 allele of the human D2 dopamine receptor gene predicts low D2 receptor availability in healthy volunteers. Molecular Psychiatry. 1998;3:256–260. doi: 10.1038/sj.mp.4000350. [DOI] [PubMed] [Google Scholar]
- 65.Jonsson EG, et al. Polymorphisms in the dopamine D2 receptor gene and their relationships to striatal dopamine receptor density of healthy volunteers. Molecular Psychiatry. 1999;4:290–296. doi: 10.1038/sj.mp.4000532. [DOI] [PubMed] [Google Scholar]
- 66.Ritchie T, Noble EP. Association of seven polymorphisms of the D2 dopamine receptor gene with brain receptor-binding characteristics. Neurochemistry Research. 2003;28:73–82. doi: 10.1023/a:1021648128758. [DOI] [PubMed] [Google Scholar]
- 67.Tupala E, Hall H, Bergströ K, Mantere T, Rösönen P, Sörkioja T, Tiihonen J. Dopamine D2 receptors and transporters in type 1 and 2 alcoholics measured with human whole hemisphere autoradiography. Human Brain Mapping. 2003;20:91–102. doi: 10.1002/hbm.10129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Goldstein R, Klein A, Tomasi D, Zhang L, Cottone L, Maloney T et al. Is decreased prefrontalcortical sensitivity to monetary reward associated with impaired motivation and selfcontrol in cocaine addiction? American Journal of Psychiatry. 2007;164:43–51. doi: 10.1176/appi.ajp.164.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Martinez D, Gil R, Slifstein M, Hwang DR, Huang Y, Perez A, et al. Alcohol dependence is associated with blunted dopamine transmission in the ventral striatum. Biological Psychiatry. 2005;58:779–786. doi: 10.1016/j.biopsych.2005.04.044. [DOI] [PubMed] [Google Scholar]
- 70.Noble EP. D2 dopamine receptor gene in psychiatric and neurological disorders and its phenotypes. American Journal of Medical Genetics. 2003;116:103–125. doi: 10.1002/ajmg.b.10005. [DOI] [PubMed] [Google Scholar]
- 71.Bello NT, Lucas LR, Hajnal A. Repeated sucrose access influences dopamine D2 receptor density in the striatum. Neuroreport. 2002;13:1557–1578. doi: 10.1097/00001756-200208270-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Colantuoni C, Schwenker J, McCarthy J, Rada P, Ladenheim B, Cadet JL, et al. Excessive sugar intake alters binding to dopamine and mu-opioid receptors in the brain. Neuroreport. 2001;12:3549–3552. doi: 10.1097/00001756-200111160-00035. [DOI] [PubMed] [Google Scholar]
- 73.Kelley AE, Will MJ, Steininger TL, Zhang M, Haber SN. Restricted daily consumption of a highly palatable food (chocolate Ensure) alters striatal enkephalin gene expression. European Journal of Neuroscience. 2003;18:2592–2598. doi: 10.1046/j.1460-9568.2003.02991.x. [DOI] [PubMed] [Google Scholar]
- 74.Reefd DR, Friedman MI. Diet composition alters the acceptance of fat by rats. Appetite. 1990;14:219–230. doi: 10.1016/0195-6663(90)90089-q. [DOI] [PubMed] [Google Scholar]
- 75.Warwick ZS, Synowski SJ. Effect of food deprivation and maintenance diet composition on fat preference and acceptance in rats. Physiology and Behavior. 1999;68:235–239. doi: 10.1016/s0031-9384(99)00192-4. [DOI] [PubMed] [Google Scholar]
- 76.Hutchison KE, McGeary J, Smolen A, Bryan A, Swift RM. The DRD4 VNTR polymorphism moderates craving after alcohol consumption. Health Psychology. 2002;21:139–146. [PubMed] [Google Scholar]
- 77.Small DM, Gerber J, Mak YE, Hummel T. Differential neural responses evoked by orthonasal versus retronasal odorant perception in humans. Neuron. 2005;47:593–605. doi: 10.1016/j.neuron.2005.07.022. [DOI] [PubMed] [Google Scholar]
- 78.Berridge K. Food reward: Brain substrates of wanting and liking. Neuroscience & Biobehavioral Reviews. 1996;20:1–25. doi: 10.1016/0149-7634(95)00033-b. [DOI] [PubMed] [Google Scholar]
- 79.Pelchat ML, Johnson A, Chan R, Valdez J, Ragland JD. Images of desire: Food-craving activation during fMRI. NeuroImage. 2004;23:1486–1493. doi: 10.1016/j.neuroimage.2004.08.023. [DOI] [PubMed] [Google Scholar]
- 80.Roefs A, Herman CP, MacLeod CM, Smulders FT, Jansen A. At first sight: how do restrained eaters evaluate high-fat palatable foods? Appetite. 2005;44:103–114. doi: 10.1016/j.appet.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 81.Robinson TE, Berridge KC. Intra-accumbens amphetamine increases the conditioned incentive salience of sucrose reward: Enhancement of reward “wanting” without enhanced “liking” or response reinforcement. Journal of Neuroscience. 2000;20:s91–s117. doi: 10.1523/JNEUROSCI.20-21-08122.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jansen A. A learning model of binge eating: Cue reactivity and cue exposure. Behaviour Research and Therapy. 1998;36:257–272. doi: 10.1016/s0005-7967(98)00055-2. [DOI] [PubMed] [Google Scholar]
- 83.Small DM, Veldhuizen MG, Felsted J, Mak YE, McGlone F. Separable substrates for anticipatory and consummatory chemosensation. Neuron. 2008;57:786–797. doi: 10.1016/j.neuron.2008.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Delgado MR, Nystrom LE, Fissell C, Noll DC, Fiez JA. Tracking the hemodynamic response to reward and punishment in the striatum. Journal of Neurophysiology. 2000;84:3072–3077. doi: 10.1152/jn.2000.84.6.3072. [DOI] [PubMed] [Google Scholar]
- 85.Elliott R, Friston KJ, Dolan RJ. Dissociable neural responses in human reward systems. Journal of Neuroscience. 2000;20:6159–6165. doi: 10.1523/JNEUROSCI.20-16-06159.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Knutson B, Fong GW, Adams CM, Varner JL, Hommer D. Dissociation of reward anticipation and outcome with event-related fMRI. NeuroReport. 2001;12:3683–3687. doi: 10.1097/00001756-200112040-00016. [DOI] [PubMed] [Google Scholar]
- 87.Beaver JD, Lawrence AD, van Ditzhuijzen J Davis, Davis MH, Woods A, Calder AJ. Individual differences in reward drive predict neural response to images of food. Journal of Neuroscience. 2006;26:S160–S166. doi: 10.1523/JNEUROSCI.0350-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Stoeckel L, Weller R, Cook E, Twieg D, Knowlton R, Cox J. Widespread reward-system activation in obese women in response to pictures of high-calorie foods. Neuroimage. 2008;41:636–647. doi: 10.1016/j.neuroimage.2008.02.031. [DOI] [PubMed] [Google Scholar]
- 89.LaBar KS, Gitelman DR, Parrish TB, Kim YH, Nobre AC, Mesulam MM. Hunger selectively modulates corticolimbic activation to food stimuli in humans. Behavioral Neuroscience. 2001;115:493–500. doi: 10.1037/0735-7044.115.2.493. [DOI] [PubMed] [Google Scholar]
- 90.Rosenbaum M, Sy M, Pavlovich R, Leibel RL, Hirsch J. Leptin reverses weight loss-induced changes in regional neural activity responses to visual food stimuli. Journal of Clinical Investigation. 2008;118:2583–2591. doi: 10.1172/JCI35055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Del Parigi A, Gautier J, Chen K, Salbe A, Ravussin E, Reiman E, et al. Neuroimaging and obesity: Mapping the brain responses to hunger and satiation in humans using positron emission tomorgraphy. Ann N.Y.Academy of Science. 2002;967:389–397. [PubMed] [Google Scholar]
- 92.Morris JS, Dolan RJ. Involvement of the human amygdala and orbitofrontal cortex in hunger-enhanced memory for food stimuli. Journal of Neuroscience. 2001;21:5301–5310. doi: 10.1523/JNEUROSCI.21-14-05304.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wang GJ, Volkow ND, Telang F, Jayne M, Ma J, Rao M, et al. Exposure to appetitive food stimuli markedly activates the human brain. Neuroimaging. 2004;21:1790–1797. doi: 10.1016/j.neuroimage.2003.11.026. [DOI] [PubMed] [Google Scholar]
- 94.Uher R, Yoganathan D, Mogg A, Eranti V, Treasure J, Campbell IC, et al. Effect of left prefrontal repetitive transcranial magnetic stimulation on food craving. Biological Psychiatry. 2005;58:840–842. doi: 10.1016/j.biopsych.2005.05.043. [DOI] [PubMed] [Google Scholar]
- 95.Schultz W, Apicella P, Ljungberg T. Responses of monkey dopamine neurons to rewarded and conditioned stimuli during successive steps of learning a delayed response task. Journal of Neuroscience. 1993;13:900–913. doi: 10.1523/JNEUROSCI.13-03-00900.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Schulz W, Romo R. Dopamine neurons of the monkey midbrain: Contingencies of responses to stimuli eliciting immediate behavioral reactions. Journal of Neurophysiology. 1990;63:607–624. doi: 10.1152/jn.1990.63.3.607. [DOI] [PubMed] [Google Scholar]
- 97.Kiyatkin EA, Gratton A. Electrochemical monitoring of extracellular dopamine in nucleus accumbens of rats lever-pressing for food. Brain Research. 1994;652:225–234. doi: 10.1016/0006-8993(94)90231-3. [DOI] [PubMed] [Google Scholar]
- 98.Blackburn JR, Phillips AG, Jakubovic A, Fibiger HC. Dopamine and preparatory behavior: II A neurochemical analysis. Behavioral Neuroscience. 1989;103:15–23. doi: 10.1037//0735-7044.103.1.15. [DOI] [PubMed] [Google Scholar]
- 99.Schultz W, Dickinson A. Neuronal coding of prediction errors. Annual Review of Neuroscience. 2000;23:473–500. doi: 10.1146/annurev.neuro.23.1.473. [DOI] [PubMed] [Google Scholar]
- 100.Avena NM, Long KA, Hoebel BG. Sugar-dependent rats show enhanced responding for sugar after abstinence: Evidence of a sugar deprivation effect. Physiology and Behavior. 2005;84:359–362. doi: 10.1016/j.physbeh.2004.12.016. [DOI] [PubMed] [Google Scholar]
- 101.Colantuoni C, Rada P, McCarthy J, Patten C. Evidence that intermittent, excessive sugar intake causes endogenous opioid dependence. Obesity. 2002;10:478–488. doi: 10.1038/oby.2002.66. [DOI] [PubMed] [Google Scholar]
- 102.Bonson KR, Grant SJ, Contoreggi CS, Links JM, Metcalfe J, Weyl HL, et al. Neural systems and cue-induced cocaine craving. Neuropsychopharmacology. 2002;26:379–386. doi: 10.1016/S0893-133X(01)00371-2. [DOI] [PubMed] [Google Scholar]
- 103.Volkow ND, Wang GJ, Fowler JS, Hitzemann RJ, Angrist B, Gatley SJ, et al. Methylphenidate induced craving in cocaine abusers is associated with changes in right striato-orbitofrontal metabolism: Implications in addiction. American Journal of Psychiatry. 1999;156:19–26. doi: 10.1176/ajp.156.1.19. [DOI] [PubMed] [Google Scholar]
- 104.Delahanty LM, Meigs JB, Hayden D, Williamson DA, Nathan DM. Psychological and behavioral correlates of baseline BMI in the diabetes prevention program. Diabetes Care. 2002;25:1992–1998. doi: 10.2337/diacare.25.11.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Forman EM, Hoffman KL, McGrath KB, Herbert JD, Brandsma LL, Lowe MR. A comparison of acceptance- and control-based strategies for coping with food cravings: An analog study. Behavior Research and Therapy. 2007;45:2372–2386. doi: 10.1016/j.brat.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 106.Nederkoorn C, Smulders FT, Jansen A. Cephalic phase responses, cravings and food intake in normal subjects. Appetite. 2000;35:45–55. doi: 10.1006/appe.2000.0328. [DOI] [PubMed] [Google Scholar]
- 107.Drewnowski A, Krahn DD, Demitrack MA, Nairn K, Gosnell BA. Taste responses and preferences for sweet high-fat foods: Evidence for opioid involvement. Physiology and Behavior. 1992;51:371–379. doi: 10.1016/0031-9384(92)90155-u. [DOI] [PubMed] [Google Scholar]
- 108.White MA, Whisenhunt BL, Williamson DA, Greenway FL, Netemeyer RG. Development and validation of the Food-Craving Inventory. Obesity Research. 2002;10:107–114. doi: 10.1038/oby.2002.17. [DOI] [PubMed] [Google Scholar]
- 109.Johnson WG. Effect of cue prominence and subject weight on human food-directed performance. Journal of Personality and Social Psychology. 1974;29:843–848. doi: 10.1037/h0036390. [DOI] [PubMed] [Google Scholar]
- 110.Fisher JO, Birch LL. Eating in the absence of hunger and overweight in girls from 5 to 7 years of age. American Journal of Clinical Nutrition. 2002;76:226–231. doi: 10.1093/ajcn/76.1.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Temple JL, Legerski C, Giacomelli AM, Epstein LH. Food is more reinforcing for overweight than lean children. Addictive Behaviors. 2008;33:1244–1248. [Google Scholar]
- 112.Karhunen LJ, Lappalainen RI, Vanninen EJ, Kuikka JT, Uusitupa MI. Regional cerebral blood flow during food exposure in obese and normal-weight women. Brain. 1997;120:1675–1684. doi: 10.1093/brain/120.9.1675. [DOI] [PubMed] [Google Scholar]
- 113.Rothemund Y, Preuschhof C, Bohner G, Bauknecht H, Klingeblel R, Flor H, et al. Differential activation of the dorsal striatum by high-calorie visual food stimuli in obese individuals. Neuroimage. 2007;37:410–421. doi: 10.1016/j.neuroimage.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 114.Stoeckel L, Weller R, Cook E, Twieg D, Knowlton R, Cox J. Widespread reward-system activation in obese women in response to pictures of high-calorie foods. Neuroimage. 2008;41:636–647. doi: 10.1016/j.neuroimage.2008.02.031. [DOI] [PubMed] [Google Scholar]
- 115.Stice E, Spoor S, Marti N. Abnormalities of reward circuitry and genetic risk for impaired dopamine signaling predicts weight gain. In preparation. [Google Scholar]
- 116.Comings DE, Rosenthal RJ, Lesieur HR’, Rugle LJ, Muhleman D, Chiu C, et al. A study of the dopamine D2 receptor gene in pathological gambling. Pharmacogenetics. 1996;6:107–116. doi: 10.1097/00008571-199606000-00004. [DOI] [PubMed] [Google Scholar]
- 117.Carr KD. Augmentation of drug reward by chronic food restriction: Behavioral evidence and underlying mechanisms. Physiology and Behavior. 2002;76:353–364. doi: 10.1016/s0031-9384(02)00759-x. [DOI] [PubMed] [Google Scholar]
- 118.Raynor HA, Epstein LH. The relative-reinforcing value of food under differing levels of food deprivation and restriction. Appetite. 2003;40:15–24. doi: 10.1016/s0195-6663(02)00161-7. [DOI] [PubMed] [Google Scholar]
- 119.Wilson C, Nomikos GG, Collu M, Fibiger HC. Dopaminergic correlates of motivated behavior: Importance of drive. Journal of Neuroscience. 1995;15:5169–5178. doi: 10.1523/JNEUROSCI.15-07-05169.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Levine AS, Kotz CM, Gosnell BA. Sugars and fats: The neurobiology of preference. Journal of Nutrition. 2003;133:831S–834S. doi: 10.1093/jn/133.3.831S. [DOI] [PubMed] [Google Scholar]
- 121.Comer SD, Lac ST, Wyvell CL, Carroll ME. Combined effects of byprenorphine and nondrug alternative reinforcer in I.V.cocaine self-administration in rats maintained under FR schedules. Psychopharmacology (Berlin) 1996;125:355–360. doi: 10.1007/BF02246018. [DOI] [PubMed] [Google Scholar]
- 122.Worsley JN, Moszczynska A, Falardeau P, Kalasinsky KS, Schmunk G, Guttman M, et al. Dopamine D1 receptor protein is elevated in nucleus accumbens of human, chronic methamphetamine users. Molecular Psychiatry. 2000;5:664–672. doi: 10.1038/sj.mp.4000760. [DOI] [PubMed] [Google Scholar]
- 123.Martel P, Fantino M. Mesolimbic dopaminergic system activity as a function of food reward: A microdialysis study. Pharmacology Biochemistry and Behavior. 1996;53:221–226. doi: 10.1016/0091-3057(95)00187-5. [DOI] [PubMed] [Google Scholar]
- 124.Yamamoto T. Neural substrates for the processing of cognitive and affective aspects of taste in the brain. Archives of Histology and Cytology. 2006;69:243–255. doi: 10.1679/aohc.69.243. [DOI] [PubMed] [Google Scholar]
- 125.Fossella J, Green AE, Fan J. Evaluation of a structural polymorphism in the ankyrin repeat and kinase domain containing 1 (ANKK1) gene and the activation of executive attention networks. Cognitive, Affective, and Behavioral Neuroscience. 2006;6:71–78. doi: 10.3758/cabn.6.1.71. [DOI] [PubMed] [Google Scholar]
- 126.Jonsson EG, Nothen MM, Grunhage F, Farde L, Nakashima Y, Propping P, et al. Polymorphisms in the dopamine D2 receptor gene and their relationships to striatal dopamine receptor density of healthy volunteers. Molecular Psychiatry. 1999;4:290–296. doi: 10.1038/sj.mp.4000532. [DOI] [PubMed] [Google Scholar]
- 127.Pohjalainen T, Rinne JL, Nagren K, Lehikoinen P, Anttila K, Syvalahti EK, et al. The A1 allele of the human D2 dopamine receptor gene predicts low D2 receptor availability in healthy volunteers. Molecular Psychiatry. 1998;3:256–260. doi: 10.1038/sj.mp.4000350. [DOI] [PubMed] [Google Scholar]
- 128.Ritchie T, Noble EP. Association of seven polymorphisms of the D2 dopamine receptor gene with brain receptor-binding characteristics. Neurochemistry Research. 2003;28:73–82. doi: 10.1023/a:1021648128758. [DOI] [PubMed] [Google Scholar]
- 129.Comings DE, Flanagan SD, Dietz G, Muhleman D, Knell E, Gysin R. The dopamine D2 receptor (DRD2) as a major gene in obesity and height. Journal of the American Medical Association. 1993;266:1793–1800. doi: 10.1006/bmmb.1993.1059. [DOI] [PubMed] [Google Scholar]
- 130.Blum K, Braverman ER, Wood RC, Gill J, Li C, Chen TJ, et al. Increased prevalence of the TaqI A1 allelle of the dopamine receptor gene (DRD2) in obesity with comorbid substance use disorder: A preliminary report. Pharmacogenetics. 1996;6:297–305. doi: 10.1097/00008571-199608000-00003. [DOI] [PubMed] [Google Scholar]
- 131.Jenkinson CP, Hanson R, Cray K, Weidrich C, Knowler WC, Bogardus C, et al. Association of dopamine D2 receptor polymorphisms Ser311Cys and TaqIA with obesity or type 2 diabetes mellitus in Pima Indians. International Journal of Obesity and Related Metabolic Disorders. 2000;24:1233–1238. doi: 10.1038/sj.ijo.0801381. [DOI] [PubMed] [Google Scholar]
- 132.Noble EP, Noble RE, Ritchie R, Syndulko K, Bohlman MC, Noble LA, et al. D2 dopamine receptor gene and obesity. International Journal of Eating Disorders. 1994;15:205–217. doi: 10.1002/1098-108x(199404)15:3<205::aid-eat2260150303>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 133.Spitz MR, Detry MA, Pillow P, Hu YH, Amos CI, Hong WK, et al. Variant alleles of the D2 dopamine receptor gene and obesity. Nutrition Research. 2000;20:371–380. [Google Scholar]
- 134.Tataranni PA, Baier L, Jenkinson C, Harper I, Del Parigi A, Bogardus C. A Ser311Cys mutation in the human dopamine receptor D2 gene is associated with reduced energy expenditure. Diabetes. 2001;50:901–904. doi: 10.2337/diabetes.50.4.901. [DOI] [PubMed] [Google Scholar]
- 135.Thomas GN, Critchley JA, Tomlinson B, Cockram CS, Chan JC. Relationships between the TaqI polymorphism of the dopamine D2 receptor and blood pressure in hyperglycemic and normoglycemic Chinese subjects. Clinical Endocrinology. 2001;55:605–611. doi: 10.1046/j.1365-2265.2001.01404.x. [DOI] [PubMed] [Google Scholar]
- 136.Epstein LH, Wright SM, Paluch RA, Leddy JJ, Hawk LW, Jaroni JL, et al. Relation between food reinforcement and dopamine genotypes and its effect on food intake in smokers. American Journal of Clinical Nutrition. 2004;80:82–88. doi: 10.1093/ajcn/80.1.82. [DOI] [PubMed] [Google Scholar]
- 137.Asghari V, Sanyal S, Buchwaldt S, Paterson A, Jovanovic V, Van Tol HH. Modulation of intracellular cyclic AMP levels by different human dopamine D4 receptor variants. Journal of Neurochemistry. 1995;65:1157–1165. doi: 10.1046/j.1471-4159.1995.65031157.x. [DOI] [PubMed] [Google Scholar]
- 138.Hamarman S, Fossella J, Ulger C, Brimacombe M, Dermody J. Dopamine receptor 4 (DRD4) 7-repeat allele predicts methylphenidate dose response in children with attention deficit hyperactivity disorders: A pharmacogentic study. Journal of Child and Adolescent Psychopharmacology. 2004;14:564–574. doi: 10.1089/cap.2004.14.564. [DOI] [PubMed] [Google Scholar]
- 139.Seeger G, Schloss P, Schmidt MH. Marker gene polymorphisms in hyperkinetic disorder-predictors of clinical response to treatment with methylphenidate? Neuroscience Letters. 2001;313:45–48. doi: 10.1016/s0304-3940(01)02253-4. [DOI] [PubMed] [Google Scholar]
- 140.Brody AL, Mandelkern MA, Olmstead RE, Scheibal D, Hahn E, Shiraga S, et al. Gene variants of brain dopamine pathways and smoking-induced dopamine release in the ventral caudate/nucleus accumbens. Archives of General Psychiatry. 2006;63:808–816. doi: 10.1001/archpsyc.63.7.808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Noain D, Avale ME, Wedemeyer C, Calvo D, Peper M, Rubinstein M. Identification of brain neurons expression the dopamine D4 receptor gene using BAC transgenic mice. European Journal of Neuroscience. 2006;24:2429–2438. doi: 10.1111/j.1460-9568.2006.05148.x. [DOI] [PubMed] [Google Scholar]
- 142.Levitan RD, Masellis M, Lam RW, Muglia P, Basile VS, Jain U, et al. Childhood in-attention and dysphoria and adult obesity associated with the dopamine D4 receptor gene in overeating women with seasonal affective disorder. Neuropsychopharmacology. 2004;29:179–186. doi: 10.1038/sj.npp.1300314. [DOI] [PubMed] [Google Scholar]
- 143.Kaplan AS, Levitan RD, Yilmaz Z, Davis C, Tharmalingam S, Kennedy JL. A DRD4/BDNF gene-gene interaction associated with maximum BMI in women with bulimia nervosa. International Journal of Eating Disorders. 2008;41:22–28. doi: 10.1002/eat.20474. [DOI] [PubMed] [Google Scholar]
- 144.Guo G, North KE, Gordenf-Larsen P, Bulik CM, Choi S. Body mass, DRD4, physical activity, sedentary behavior, and family socioeconomic status: The Add Health Study. Obesity. 2007;15:1199–1206. doi: 10.1038/oby.2007.640. [DOI] [PubMed] [Google Scholar]
- 145.Fuemmeler BF, Agurs-Collins TD, McClernon FJ, Kollins SH, Kail ME, Bergen AW, Ashley-Koch AE. Genes implicated in serotonergic and dopaminergic functioning predict BMI categories. Obesity. 2008;16:348–355. doi: 10.1038/oby.2007.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Hinney A, Schneider J, Siegler A, Lehmkohl G, Poustka F, Schmidt MH, et al. No evidence for involvement of polymorphisms of the dopamine D4 receptor gene in anorexia nervosa, underweight, and obesity. American Journal of Medical Genetics. 1999;88:594–597. [PubMed] [Google Scholar]
- 147.Sobik L, Hutchison K, Craighead L. Cue-elicited craving for food: a fresh approach to the study of binge eating. Appetite. 2005;44:253–261. doi: 10.1016/j.appet.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 148.Hutchison KE, LaChance H, Niaura R, Bryan AD, Smolen A. The DRD4 VNTR polymorphism influences reactivity to smoking cues. Journal of Abnormal Psychology. 2001;111:134–142. doi: 10.1037//0021-843x.111.1.134. [DOI] [PubMed] [Google Scholar]
- 149.McClernon FJ, Hutchison KE, Rose JE, Kozink RV. DRD4 VNTR polymorphism is associated with transient fMRI-BOLD responses to smoking cues. Psychopharmacology. 2007;194:433–441. doi: 10.1007/s00213-007-0860-6. [DOI] [PubMed] [Google Scholar]
- 150.Hutchison KE, Swift R, Rohsenow DJ, Monti PM, Davidson D, Almeida A. Olanzapine reduces urge to drink after drinking cues and a priming dose of alcohol. Psychopharmacology. 2001;155:27–34. doi: 10.1007/s002130000629. [DOI] [PubMed] [Google Scholar]
- 151.Shao C, Li Y, Jiang K, Zhang D, Xu Y, Lin L, et al. Dopamine D4 receptor polymorphism modulates cue-elicited heroin craving in Chinese. Psychopharmacology. 2006;186:185–190. doi: 10.1007/s00213-006-0375-6. [DOI] [PubMed] [Google Scholar]
- 152.Floresco SB, West AR, Ash B, Moore H, Grace AA. Afferent modulation of dopamine neuron firing differentially regulates tonic and phasic dopamine transmission. Nat Neurosci. 2003;6:968–973. doi: 10.1038/nn1103. [DOI] [PubMed] [Google Scholar]
- 153.Pecina S, Cagniard B, Berridge KC, Aldrigde JW’, Zhuang X. Hyperdopaminergic mutant mice have higher “wanting” but not “liking” for sweet rewards. Journal of Neuroscience. 2003;23:9395–9402. doi: 10.1523/JNEUROSCI.23-28-09395.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.South T, Huang XF. High-fat diet exposure increases dopamine D2 receptor and decreases dopamine transporter receptor binding density in the nucleus accumbens and caudate putamen of mice. Neurochemical Research. 2008;33:598–605. doi: 10.1007/s11064-007-9483-x. [DOI] [PubMed] [Google Scholar]
- 155.Chen PS, Yang YK;, Yeh TL, Lee IH, Yao WJ, Chiu NT, Lu RB. Correlation between body mass index and striatal dopamine transporter availability in healthy volunteers: A SPECT study. Neuroimage. 2008;40:275–279. doi: 10.1016/j.neuroimage.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 156.Epstein L, Jaroni J, Paluch R, Leddy J, Vahue H, Hawk L, Wileyto P, Shields P, Lerman C. Dopamine transporter genotype as a risk factor for obesity in African-American smokers. Obesity. 2002;10 doi: 10.1038/oby.2002.168. 1232-1230. [DOI] [PubMed] [Google Scholar]
- 157.Matsumoto M, Weickert C, Akil M, Lipska B, Hyde T, Herman M, Kleinman J, Weinberger D. Catechol O-methyltransferase mRNA expression in human and rat brain: Evidence for a role in cortical neuronal function. Neuroscience. 2003;116:127–137. doi: 10.1016/s0306-4522(02)00556-0. [DOI] [PubMed] [Google Scholar]
- 158.Huotari M, Gogos J, Karayiorgou M, Koponen O, Forsberg M, Raasmaja A, Hyttinen J, Mannisto P. Brain catecholamine metabolism in catechol-O-methyltransferase (COMT)-deficient mice. European Journal of Neuroscience. 2002;15:246–256. doi: 10.1046/j.0953-816x.2001.01856.x. [DOI] [PubMed] [Google Scholar]
- 159.Bilder R, Volavka J, Lachman H, Grace A. The catechol-0-methyltransferase polymorphism: Relations to the tonic-phasic dopamine hypothesis and neuropsychiatric phenotypes. Neuropsychopharmacology. 2004;29:1943–1961. doi: 10.1038/sj.npp.1300542. [DOI] [PubMed] [Google Scholar]
- 160.Boettiger C, Mitchell J, Tavares V, Robertson M, Joslyn G, D’Esposito M, Fields H. Immediate reward bias in humans: Fronto-parietal networks and a role for the catechol-O-methyltransferase 158Val/Val genotype. Journal of Neuroscience. 2007;27:14383–14391. doi: 10.1523/JNEUROSCI.2551-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Yacubian J, Sommer T, Schroeder K, Glascher J, Kalisch R, Leuenberger B, Braus D, Buchel C. Gene-gene interaction associated with neural reward sensitivity. Proceedings of the National Academy of Sciences. 2007;104:8125–8130. doi: 10.1073/pnas.0702029104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Vandenbergh DJ, Rodriguez LA, Miller IT, Uhl GR, Lachman HM. High-activity catechol-O-methyltransferase allele is more prevalent in polysubstance abusers. American Journal of Medical Genetics. 1997;74:439–442. [PubMed] [Google Scholar]
- 163.Wang J, Miao D, Babu S, Yu J, Barker J, Klingensmith G, Rewers M, Eisenbarth G, Yu L. Prevalence of autoantibody-negative diabetes is not rare at all ages and increases with older age and obesity. Journal of Clinical Endocrinology & Metabolism. 2007;92:88–92. doi: 10.1210/jc.2006-1494. [DOI] [PubMed] [Google Scholar]
- 164.Nederkoorn C, van Eijs Y Jansen, Jansen A. Restrained eaters act on impulse. Personality and Individual Differences. 2004;37:1651–1658. [Google Scholar]
- 165.Pickering AD, Diaz A, Gray JA. Personality and reinforcement: An exploration using a maze learning task. Personality and Individual Differences. 1995;18:541–558. [Google Scholar]
- 166.Chalmers DK, Bowyer CA, Olenick NL. Problem drinking and obesity: A comparison in personality patterns and life-style. International Journal of Addiction. 1990;25:803–817. doi: 10.3109/10826089009056219. [DOI] [PubMed] [Google Scholar]
- 167.Ryden A, Sullivan M, Torgerson JS, Karlsson J, Lindroos AK, Taft C. Severe obesity and personality: A comparative controlled study of personality traits. International Journal of Obesity. 2003;27:1534–1540. doi: 10.1038/sj.ijo.0802460. [DOI] [PubMed] [Google Scholar]
- 168.Williamson DA, Kelley ML, Davis CJ, Ruggiero L, Blouin DC. Psychopathology of eating disorders: A controlled comparison of bulimics, obese, and normal subjects. Journal of Consulting and Clinical Psychology. 1985;53:161–166. doi: 10.1037//0022-006x.53.2.161. [DOI] [PubMed] [Google Scholar]
- 169.Jonsson B, Bjorvell H, Lavander S, Rossner S. Personality traits predicting weight loss outcome in obese patients. Acta Psyciatrica Scandinavia. 1986;74:384–387. doi: 10.1111/j.1600-0447.1986.tb06258.x. [DOI] [PubMed] [Google Scholar]
- 170.Nederkoorn C, Braet C, Van Eijs Y, Tanghe A, Jansen A. Why obese children cannot resist food: The role of impulsivity. Eating Behaviors. 2006;7:315–322. doi: 10.1016/j.eatbeh.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 171.Nederkoorn C, Jansen E, Mulkens S, Jansen A. Impulsivity predicts treatment outcome in obese children. Behaviour Research and Therapy. 2007;45:1071–1075. doi: 10.1016/j.brat.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 172.Guerrieri R, Nederkoorn C, Jansen A. The interaction between impulsivity and a varied food environment: Its influence on food intake and overweight. Int J Obes. 2008;32:708–714. doi: 10.1038/sj.ijo.0803770. [DOI] [PubMed] [Google Scholar]
- 173.Nederkoorn C, Smulders FT, Havermans RC, Roefs A, Jansen A. Impulsivity in obese women. Appetite. 2006;47:253–256. doi: 10.1016/j.appet.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 174.Jansen A, Theunissen N, Slechten K, Nederkoorn C, Boon B, Mulkens Sl, Roefs A. Overweight children overeat after exposure to food cues. Eating Behaviors. 2003;4:197–209. doi: 10.1016/S1471-0153(03)00011-4. [DOI] [PubMed] [Google Scholar]
- 175.Bonato DP, Boland FJ. Delay of gratification in obese children. Addictive Behaviors. 1983;8:71–74. doi: 10.1016/0306-4603(83)90059-x. [DOI] [PubMed] [Google Scholar]
- 176.Bourget V, White DR. Performance of overweight and normal-weight girls on delay of gratification tasks. International Journal of Eating Disorders. 1984;3:63–71. [Google Scholar]
- 177.Corr PJA. Gray’s reinforcement sensitivity theory and frustrative non-reward: A theoretical note on expectancies in reactions to rewarding stimuli. Personality and Individual Differences. 2002;32:1247–1253. [Google Scholar]
- 178.Kambouropoulos N, Staiger P. Personality and resonses to appetitive and aversive stimuli: The joint influence of behavioural approach and behavioural inhibition systems. Personaltiy and Individual Differences. 2004;37:1153–1165. [Google Scholar]
- 179.Smith G, Simmons J, Flory K, Annus A, Hill K. Thinness and eating expectancies predict subsequent binge-eating and purging behavior among adolescent girls. Journal of Abnormal Psychology. 2007;116:188–197. doi: 10.1037/0021-843X.116.1.188. [DOI] [PubMed] [Google Scholar]
- 180.Bohon C, Stice E, Burton E. Maintenance factors for persistence of bulimic pathology: A community-based natural history study. International Journal of Eating Disorders. 2008;42:173–178. doi: 10.1002/eat.20600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Sher K, Wood J, Wood P, Raskin G. Alcohol outcome expectancies and alcohol use: A latent variable cross-lagged panel study. Journal of Abnormal Psychology. 1996;105:561–574. doi: 10.1037/0021-843X.105.4.561. [DOI] [PubMed] [Google Scholar]
- 182.Wetter D, Kenford S, Welsch S, Smith S, Fouladi R, Fiore M, Baker T. Prevalence and predictors of transitions in smoking behavior among college students. Healthy Psychology. 2004;23:168–177. doi: 10.1037/0278-6133.23.2.168. [DOI] [PubMed] [Google Scholar]
- 183.Gorin AA, Crane M. The obesogenic environment. In: Jelalian E, Steele R, editors. Handbook of Child and Adolescent Obesity. New York, NY: Springer; 2008. pp. 139–150. [Google Scholar]
- 184.Wadden TA, Brownell KD, Foster GD. Obesity: Responding to the global epidemic. Journal of Consulting and Clinical Psychology. 2002;70:510–525. doi: 10.1037//0022-006x.70.3.510. [DOI] [PubMed] [Google Scholar]
- 185.French SA, Story M, Fulkerson JA, Gerlach AF. Food environment in secondary schools: A la carte, vending machines, and food policies and practices. American Journal of Public Health. 2003;93:1161–1167. doi: 10.2105/ajph.93.7.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Wadden T, Foster G. Behavioral treatment of obesity. Medical Clinics of North America. 2000;84:441–461. doi: 10.1016/s0025-7125(05)70230-3. [DOI] [PubMed] [Google Scholar]
- 187.Campbell K, Crawford D, Salmon J, Carver A, Garnett S, Baur L. Associations between the home food environment and obesity-promoting eating behaviors in adolescence. Obesity. 2007;15:719–730. doi: 10.1038/oby.2007.553. [DOI] [PubMed] [Google Scholar]
- 188.Hanson N, Neumark-Sztainer D, Eisenberg M, Story M, Wall M. Associations between parental report of the home food environment and adolescent intake of fruits, vegetables, and dairy foods. Public Health and Nutrion. 2005;8:77–85. doi: 10.1079/phn2005661. [DOI] [PubMed] [Google Scholar]
- 189.Raynor HA, Polley B, Wing RR, Jeffery RW. Is dietary fat intake related to liking or household availability of high- and low-fat foods? Obesity Research. 2004;12:816–823. doi: 10.1038/oby.2004.98. [DOI] [PubMed] [Google Scholar]
- 190.Kubik MY, Lytle LA, Hannan PJ, Perry CL, Story M. The association of the school food environment with dietary behaviors of young adolescents. American Journal of Public Health. 2003;93:1168–1173. doi: 10.2105/ajph.93.7.1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Bowman S, Gortmaker S, Ebbeling C, Pereira M, Ludwig D. Effects of fast-food consumption on energy intake and diet quality among children in a national household survey. Pediatrics. 2004;113:112–118. doi: 10.1542/peds.113.1.112. [DOI] [PubMed] [Google Scholar]
- 192.Austin SB, Melly SJ, Sanchez BN’, Patel A, Buka S, Gortmaker SL. Clustering of fast-food restaurants around schools: A novel application of spatial statistics to the study of food environments. American Journal of Public Health. 2005;95:1575–1581. doi: 10.2105/AJPH.2004.056341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Maddock J. The relation between obesity and the prevalence of fast food restaurants: State-level analysis. American Journal of Health Promotion. 2004;19:137–143. doi: 10.4278/0890-1171-19.2.137. [DOI] [PubMed] [Google Scholar]
- 194.Mehta NK, Chang VW. Weight status and restaurant availability: A multilevel analysis. American Journal of Preventive Medicine. 2008;34:127–133. doi: 10.1016/j.amepre.2007.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Alter DA, Eny K. The relation between the supply of fast-food chains and cardiovascular outcomes. Canadian Journal of Public Health. 2005;96:173–177. doi: 10.1007/BF03403684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Burdette H, Whitaker R. A national study of neighborhood safety, outdoor play, television viewing, and obesity in preschool children. Pediatrics. 2004;116:657–662. doi: 10.1542/peds.2004-2443. [DOI] [PubMed] [Google Scholar]
- 197.Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health. 2005;119:1059–1068. doi: 10.1016/j.puhe.2005.05.007. [DOI] [PubMed] [Google Scholar]