Abstract
AIM: To investigate the role that single nucleotide polymorphisms (SNPs) in the promoter of the tumour necrosis factor-alpha (TNF-α) gene play in the risk of inflammatory bowel diseases (IBDs) in a New Zealand population, in the context of international studies.
METHODS: DNA samples from 388 patients with Crohn’s disease (CD), 405 ulcerative colitis (UC), 27 indeterminate colitis (IC) and 201 randomly selected controls, from Canterbury, New Zealand were screened for 3 common polymorphisms in the TNF-α receptor: -238 G→A, -308 G→A and -857C→T, using a TaqmanR assay. A meta-analysis was performed on the data obtained on these polymorphisms combined with that from other published studies.
RESULTS: Individuals carrying the -308 G/A allele had a significantly (OR = 1.91, χ2 = 17.36, P < 0.0001) increased risk of pancolitis, and a 1.57-fold increased risk (OR = 1.57, χ2 = 4.34, P = 0.037) of requiring a bowel resection in UC. Carrying the -857 C/T variant decreased the risk of ileocolonic CD (OR = 0.56, χ2 = 4.32, P = 0.037), and the need for a bowel resection (OR = 0.59, χ2 = 4.85, P = 0.028). The risk of UC was reduced in individuals who were smokers at diagnosis, (OR = 0.48, χ2 = 4.86, P = 0.028).
CONCLUSION: TNF-α is a key cytokine known to play a role in inflammatory response, and the locus for the gene is found in the IBD3 region on chromosome 6p21, known to be associated with an increased risk for IBD. The -308 G/A SNP in the TNF-α promoter is functional, and may account in part for the increased UC risk associated with the IBD3 genomic region. The -857 C/T SNP may decrease IBD risk in certain groups. Pharmaco- or nutrigenomic approaches may be desirable for individuals with such affected genotypes.
Keywords: Tumour necrosis factor alpha, Single nucleotide polymorphisms, Inflammatory bowel diseases, Crohn’s disease, Ulcerative colitis
INTRODUCTION
Inflammatory bowel diseases (IBDs) are chronic multifactorial disorders, commonly classified as autoimmune diseases, and comprise of Crohn’s disease (CD) and ulcerative colitis (UC). Up to 10%-15% of reported cases are described as “indeterminate colitis” (IC), where an unequivocal classification is not possible using established diagnostic criteria. Twin studies and segregation analysis strongly support IBD, especially CD, as complex genetic traits[1], whose etiology also involves immunological and environmental factors, including diet. Several IBD-susceptibility chromosomal regions have been replicated in a number of studies, and in some cases causative genes have been found. For example, the key gene in the IBD1 region on chromosome 16q12, has been identified as Nucleotide Oligomerization Domain 2 (NOD2)[2]. Three polymorphisms of this gene (R702W, G908R, and 1007fs) increase the susceptibility to IBD, especially CD.
The IBD3 region on chromosome 6p was initially described in a large European cohort[3] by Hampe and coworkers, who suggested that this observation was consistent with single nucleotide polymorphism (SNPs) in either the Human Leukocyte Antigen (HLA) and/or tumor necrosis factor (TNF) genes as being risk factors for IBD. Rioux et al[4] confirmed this association in a genome-wide search of 158 Canadian sib-pair families, a finding also replicated by Dechairo et al[5] in 284 IBD-affected sib pairs from 234 Caucasian families in the UK, showing an almost equal contribution to the linkage with CD and UC. Fisher et al[6] investigated 353 northern European sib pairs, and suggested that the strongest evidence for linkage in both CD and UC occurred at the IBD3 region on chromosome 6p21.3 (OMIM 604519). This effect appeared to be male-specific. It should be noted that the human TNF-alpha (TNF-α) gene is located on chromosome 6p21.3, spanning approximately 3 kb[7].
TNF-α is an important pro-inflammatory cytokine that is involved in systemic inflammation, and stimulates acute phase reactions[8,9]. TNF-α/TNF receptor interactions not only play a pivotal role in the pathogenesis of the inflammatory response, but also cause programmed cell death (apoptosis), cell proliferation and differentiation[10]. Ligand binding to TNF receptors causes a conformational change in the receptor, leading to several downstream effects including activation of the heterodimeric transcription factor and nuclear factor (NF)-κB. Through translocation to the nucleus, this mediates the transcription of a variety of proteins involved in cell survival and proliferation, as well as inflammatory response. Alterations in the regulation of TNF-α, especially TNF-α overproduction, have been implicated in a variety of symptoms associated with autoimmune disorders, including IBD, and especially CD. Inflammation, anorexia, and weight loss are all associated with increased levels of circulating TNF-α that is seen in CD. Indeed, a common treatment of CD is the use of TNF-α inhibitors such as the monoclonal antibody, infliximab (IFX).
Several SNPs in the TNF-α promoter region are known to affect the level of gene expression. For example, two SNPs located at nucleotides -238 and -308 represent substitutions of adenine for guanine in the TNF transcriptional start site[11]. Such variations in the TNF-α promoter region have previously been associated with susceptibility to a range of autoimmune disorders, including asthma[12,13], psoriasis[14] and rheumatoid arthritis[15]. The G→A polymorphism at position -238 in the TNF gene is associated with lower production of TNF-α in patients with UC[16]. Conversely, the -308A polymorphism is associated with enhanced TNF-α production in cells in vitro and in CD patients in vivo[16–18]. The -857 C→T SNP is functional through binding to the transcription factor octamer transcription factor-1 (OCT-1). Carriers of the -857C allele show higher levels of circulating TNF-α, and van Heel et al[19] suggested that the TNF -857C/T SNP increased the susceptibility to IBD in a UK population through it’s effects on the interaction between the OCT-1 gene and the NF-κB transcription factor.
The present study was designed to determine whether SNPs in the TNF-α promoter region confer susceptibility to CD or UC, and whether they are associated with the clinical phenotype, in a New Zealand Caucasian population.
MATERIALS AND METHODS
Study participants
The Canterbury IBD Project is a population-based study of genetic and environmental determinants of the aetiology IBD, which has been described in detail elsewhere[20]. The participants consented to the collection of peripheral blood for DNA extraction and genotyping. The subjects included in the present study were a random subset of the Caucasian participants of the Canterbury IBD Project. Both CD and UC were defined using standard diagnostic criteria[21]. The subjects were phenotyped according to the Montreal Classification systems, allowing genotype-phenotype analysis to be performed[22].
A total of 388 CD participants, 405 UC participants, and 27 IC participants were genotyped for this study. All participants self-reported European ancestry, and patients who self-reported having any Maori or other non-Caucasian ancestry are not included in the data set. Clinical and demographic characteristics of the Caucasian IBD cohort for this study are shown in Table 1.
Table 1.
Summary of clinical and demographic data on Caucasian IBD patients genotyped for at least one TNF-α polymorphism n (%)
| CD | UC | IC | |
| Gender | 388 | 405 | 27 |
| Female | 249 (64.2) | 214 (52.8) | 15 (55.6) |
| Male | 139 (35.8) | 191 (47.2) | 12 (44.4) |
| Age at first diagnosis | |||
| Below 17 | 39 (10.0) | 26 (6.4) | 0 |
| Between 17 and 40 | 199 (51.3) | 184 (45.4) | 15 (55.6) |
| Above 40 | 150 (38.7) | 195 (48.2) | 12 (44.4) |
| CD location | |||
| Ileal | 125 (32.2) | ||
| Colonic | 169 (43.6) | ||
| Ileocolonic | 90 (23.2) | ||
| Unknown (U + UN) | 4 (1.0) | ||
| UC location | |||
| Proctitis | 140 (34.6) | 3 (11.1) | |
| Left colon | 107 (26.4) | 5 (18.5) | |
| Pancolitis | 154 (38.0) | 19 (70.4) | |
| Unknown | 4 (1.0) | 0 | |
| Behaviour | |||
| Non-structuring, non-penetrating perianal disease: With | 47 (21.5) | ||
| Without | 172 (78.5) | ||
| Structuring perianal disease: With | 46 (38.0) | ||
| Without | 75 (62.0) | ||
| Penetrating perianal disease: With | 17 (35.4) | ||
| Without | 31 (64.6) | ||
| Any relative with IBD: Yes (n = 143) | 74 (19.1) | 65 (16.1) | 5 (18.5) |
| Bowel resection: Yes (n = 214) | 142 (36.6) | 70 (17.3) | 2 (7.4) |
| Smoker at diagnosis: Yes (n = 147) | 97 (25.7) | 49 (12.3) | 2 (7.7) |
| Ever used immunomo- dulators: Yes (n = 296) | 203 (52.3) | 86 (21.2) | 8 (29.6) |
| Extra intestinal manifestations: Yes (n = 142) | 75 (19.3) | 64 (15.8) | 3 (11.1 |
The New Zealand Caucasian controls used in this study were selected at random from the electoral roll, comprising 93% of the population over eighteen years of age in Canterbury, New Zealand[23].
Criteria for SNP selection
The TNF-α region is complex, and a considerable number of SNPs are necessary to haplotype tag this region[24]. Therefore, we elected to study 3 SNPs in the promoter region for which functionality has been shown previously[16,25]. The SNPs studied were: -238 G→A (rs361525), -308 G→A (rs1800629) and -857C→T (rs1799724).
Applied biosystems TaqMan®SNP genotyping assay for TNF-α variants
The three alleles were genotyped using the ABI TaqMan MGB diallelic discrimination system. A custom made, quality controlled and functionally tested genotyping assay (Assay-by-Design online service) for all three variants was obtained from Applied Biosystems (Melbourne, Australia) (Table 2). The reactions were prepared by using 2 × TaqMan Universal Master Mix, 20 × SNP Genotyping Assay Mix, DNase-free water, 10 ng genomic DNA in a final volume of 5l per reaction. The PCR amplification was performed using the ABI Prism 7900 HT sequence-detector machine under the following conditions: 10 min 95°C enzyme activation followed by 40 cycles at 92°C for 15 s and 60°C for 1 min.
Table 2.
Primer and probe sequences for custom made TaqMan SNP genotyping assay for TNF-α -857C/T, TNF-α -308G/A and TNF-α -238G/A
| TaqMan SNP genotyping assay | DNA sequence |
| TNF-α_-857C/T _forward primer | 5’-GGGCTATGGAAGTCGAGTATGG -3’ |
| TNF-α_-857C/T _reverse primer | 5’-GTCCTGGAGGCTCTTTCACT -3’ |
| TNF-α_-857C/T_VIC probe | 5’-CCCTGTCTTCGTTAAGG -3’ |
| TNF-α_-857C/T _FAM probe | 5’-CCTGTCTTCATTAAGG -3’ |
| TNF-α_-308G/A_forward primer | 5’-CCAAAAGAAATGGAGGCAATAGGTT -3’ |
| TNF-α_-308G/A _reverse primer | 5’-GGACCCTGGAGGCTGAAC -3’ |
| TNF-α_-308G/A _VIC probe | 5’-CCCGTCCCCATGCC -3’ |
| TNF-α_-308G/A _FAM probe | 5’-CCCGTCCTCATGCC -3’ |
| TNF-α_-238G/A_forward primer | 5’-CAGTCAGTGGCCCAGAAGAC -3’ |
| TNF-α_-238G/A _reverse primer | 5’-CCCTCACACTCCCCATCCT -3’ |
| TNF-α_-238G/A _VIC probe | 5’-CTCGGAATCGGAGCAG -3’ |
| TNF-α_-238G/A _FAM probe | 5’-CTCGGAATCAGAGCAG -3’ |
Statistical analysis
The allelic trend test[26] and Fisher’s exact genotypic test were used to compare patients and control allele frequencies. An exact test was used to test for departures from Hardy-Weinberg equilibrium (HWE) in the patient and the control samples[27]. Allelic odds ratios were calculated and confidence intervals for the allelic odds ratio were calculated under the assumption of HWE in the patient and the control groups. Within the region of TNF-α, HAPLO. SCORE in R was used to estimate haplotypes and to test for association of these haplotypes within the patient-control population. Meta-analysis was carried out to obtain an overall index of the effect magnitude of the studied relationship. These analyses were carried out using R and SAS (V9.1 SAS Institute., Cary, NC, USA). We also performed an exploratory analysis of allele frequency differences between controls and patient subgroups, using the clinical characteristics shown in Table 1.
RESULTS
For each of the polymorphisms studied, the risks of carrying the variant was compared between CD, UC and control groups, as shown in Tables 3 and 4. Those individuals carrying the variant TNF-α -238A allele showed no statistically significant effect on the patterns of disease risk. There were no significant differences between males and females in the risk for CD or UC (Table 5).
Table 3.
Genotype and allele counts for TNF-α variants in New Zealand IBD patients and Caucasians
| SNP | Controls | CD | UC | CD + UC | IC |
| TNF-α -238 G/A | |||||
| AA | 0 | 2 (0.5) | 2 (0.5) | 4 (0.5) | 0 |
| AG | 50 (12.1) | 47 (12.1) | 39 (9.6) | 86 (10.9) | 2 (7.4) |
| GG | 365 (87.9) | 338 (87.3) | 364 (89.9) | 702 (88.6) | 25 (92.6) |
| Genotype P | 0.51 | 0.19 | 0.37 | ||
| HWE P | 0.38 | 0.68 | 0.31 | 0.35 | 1 |
| A | 50 (6.0) | 51 (6.6) | 43 (5.3) | 94 (5.9) | 2 (3.7) |
| G | 780 (94.0) | 723 (93.4) | 767 (94.7) | 1490 (94.1) | 52 (96.3) |
| OR (95%CI) | 1.10 (0.72, 1.68) | 0.87 (0.56, 1.36) | 0.98 (0.68, 1.42) | ||
| Allelic P | 0.64 | 0.53 | 0.93 | ||
| TNF-α -308 G/A | |||||
| AA | 10 (2.4) | 16 (4.1) | 23 (5.7) | 39 (4.9) | 1 (4.0) |
| AG | 123 (29.7) | 112 (28.9) | 122 (30.3) | 234 (29.6) | 4 (16.0) |
| GG | 282 (67.9) | 260 (67.0) | 258 (64.0) | 518 (65.5) | 20 (80.0) |
| Genotype P | 0.41 | 0.049 | 0.1 | ||
| HWE P | 0.49 | 0.4 | 0.1 | 0.07 | 0.29 |
| A | 143 (17.2) | 144 (18.6) | 168 (20.8) | 312 (19.7) | 6 (12.0) |
| G | 687 (82.8) | 632 (81.4) | 638 (79.2) | 1270 (80.3) | 44 (88.0) |
| OR (95% CI) | 1.09 (0.84, 1.42) | 1.27 (0.98, 1.63) | 1.18 (0.94, 1.48) | ||
| Allelic P | 0.49 | 0.06 | 0.14 | ||
| TNF-α -857C/T | |||||
| CC | 359 (88.2) | 332 (86.0) | 358 (88.4) | 690 (87.2) | 21 (77.8) |
| CT | 45 (11.1) | 51 (13.2) | 41 (10.1) | 92 (11.6) | 6 (22.2) |
| TT | 3 (0.7) | 3 (0.8) | 6 (1.5) | 9 (1.1) | 0 |
| Genotype P | 0.61 | 0.57 | 0.85 | ||
| HWE P | 0.2 | 0.45 | 0.004 | 0.01 | 1 |
| C | 763 (93.7) | 715 (92.6) | 757 (93.5) | 1472 (93.0) | 48 (88.9) |
| T | 51 (6.3) | 57 (7.4) | 53 (6.5) | 110 (7.0) | 6 (11.1) |
| OR (95% CI) | 0.84 (0.56,1.26) | 0.95 (0.63,1.45) | 0.89 (0.63,1.28) | ||
| Allelic P | 0.38 | 0.82 | 0.52 |
Table 4.
Allelic odds ratios and 95% confidence intervals for comparison of TNF-α variants with IBD status in New Zealand IBD patients and Caucasians
|
TNF-α_361525 (-238 G/A) |
TNF-α_1799724 (-857C/T) |
TNF-α_1800629 (-308 G/A) |
||||||||||
| CD | UC | CD | UC | Crohn's | UC | |||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Female | 1.00 | 0.59-1.69 | 0.64 | 0.35-1.18 | 1.06 | 0.65-1.74 | 1.07 | 0.64-1.79 | 1.01 | 0.72-1.41 | 1.19 | 0.85-1.67 |
| Male | 1.29 | 0.69-2.41 | 1.15 | 0.63-2.08 | 1.08 | 0.62-1.89 | 1.46 | 0.84-2.53 | 1.26 | 0.85-1.87 | 1.34 | 0.93-1.93 |
| Age at first diagnosis | ||||||||||||
| 0-16 yr | 1.30 | 0.54-3.14 | 0.31 | 0.04-2.29 | 1.67 | 0.51-5.48 | 0.8 | 0.28-2.31 | 1.66 | 0.97-2.85 | 1.60 | 0.83-3.07 |
| 17-40 yr | 0.92 | 0.55-1.54 | 0.8 | 0.46-1.39 | 0.85 | 0.53-1.36 | 0.75 | 0.47-1.20 | 1.01 | 0.74-1.39 | 1.23 | 0.90-1.68 |
| > 40 yr | 1.30 | 0.78-2.17 | 1.02 | 0.62-1.69 | 0.72 | 0.44-1.18 | 1.31 | 0.76-2.25 | 1.08 | 0.77-1.52 | 1.26 | 0.93-1.71 |
| CD location | ||||||||||||
| Ileal | 0.93 | 0.51-1.71 | 0.98 | 0.55-1.75 | 1.00 | 0.69-1.45 | ||||||
| Colonic | 1.09 | 0.65-1.83 | 1.00 | 0.59-1.69 | 1.25 | 0.91-1.72 | ||||||
| Ileocolonic | 1.44 | 0.79-2.63 | 0.56 | 0.32-0.97 | 0.92 | 0.59-1.42 | ||||||
| UC location | ||||||||||||
| Proctitis | 1.07 | 0.61-1.87 | 0.68 | 0.41-1.12 | 0.90 | 0.62-1.30 | ||||||
| Left colon | 0.76 | 0.38-1.52 | 1.36 | 0.68-2.73 | 0.97 | 0.65-1.45 | ||||||
| Pancolitis | 0.74 | 0.40-1.36 | 1.08 | 0.62-1.88 | 1.91 | 1.41-2.60 | ||||||
| CD Behaviour | ||||||||||||
| Inflammatory | 1.27 | 0.81-2.00 | 1.05 | 0.64-1.71 | 1.19 | 0.89-1.60 | ||||||
| Structuring | 1.19 | 0.67-2.10 | 0.66 | 0.39-1.11 | 1.01 | 0.69-1.47 | ||||||
| Penetrating | 0.16 | 0.02-1.17 | 0.65 | 0.31-1.37 | 0.89 | 0.50-1.59 | ||||||
| Ileal/Structuring | 1.34 | 0.70-2.58 | 0.95 | 0.47-1.92 | 1.04 | 0.66-1.64 | ||||||
| Colonic/Inflammatory | 1.29 | 0.77-2.17 | 1.06 | 0.60-1.87 | 1.29 | 0.92-1.80 | ||||||
| TNF-α_361525 (-238 G/A) | TNF-α_1799724 (-857C/T) | TNF-α_1800629 (-308 G/A) | ||||||||||
| Any relative with IBD | 1.15 | 0.57-2.32 | 0.89 | 0.39-2.01 | 1.02 | 0.49-2.12 | 1.02 | 0.47-2.20 | 1.49 | 0.98-2.27 | 0.98 | 0.60-1.60 |
| Bowel resection | 1.12 | 0.65-1.93 | 0.7 | 0.29-1.66 | 0.59 | 0.37-0.95 | 0.97 | 0.47-2.02 | 0.93 | 0.65-1.34 | 1.57 | 1.02-2.41 |
| Smoker at diagnosis | 1.04 | 0.54-1.99 | 0.66 | 0.23-1.87 | 1.00 | 0.52-1.91 | 0.48 | 0.25-0.94 | 0.84 | 0.54-1.30 | 1.08 | 0.63-1.86 |
| Ever used immunomodulators | 1.07 | 0.66-1.75 | 0.66 | 0.29-1.48 | 0.93 | 0.57-1.51 | 0.75 | 0.41-1.39 | 1.09 | 0.80-1.48 | 1.46 | 0.98-2.17 |
| Any EIMs | 1.11 | 0.55-2.24 | 0.5 | 0.18-1.41 | 1.60 | 0.67-3.80 | 2.07 | 0.74-5.83 | 1.46 | 0.96-2.22 | 1.28 | 0.81-2.03 |
Table 5.
Comparison of TNF-α variants with IBD status between Males and Females in New Zealand IBD patients and Caucasians
| Gender | n |
TNF-α -238 |
TNF-α -857 |
TNF-α -308 |
||||
| OR (95% CI) | P | OR(95% CI) | P | OR (95% CI) | P | |||
| CD vs Control | F | 248/239 | 1.31 (0.99-1.75) | 0.06 | 1.30 (0.98-1.73) | 0.07 | 1.32 (0.99-1.75) | 0.056 |
| M | 139/176 | 1.00 | 1.00 | 1.00 | ||||
| UC vs Control | F | 214/239 | 0.83 (0.63-1.09) | 0.17 | 0.82 (0.62-1.08) | 0.16 | 0.83 (0.63-1.09) | 0.17 |
| M | 191/176 | 1.00 | 1.00 | 1.00 | ||||
Carrying the TNF-α -308 G/A allele again showed no statistically significant effect on patterns of disease risk, and there was no significant difference between males and females in the risk for CD or UC (Table 5). Having the A allele increased the probability of the risk for pancolitis in UC, from 0.17 (for controls) to 0.28, giving an odds ratio of 1.91 (OR = 1.91, CI = 1.41-2.60, P < 0.0001). Carrying this polymorphism, significantly increased the necessity for bowel resection in UC (OR = 1.57, CI = 1.02-2.41, P = 0.037).
Carrying the TNF-α -857 C/T variant did not result in any statistically significant changes in the overall disease risk, or a significant male-female imbalance. However, in individuals carrying the variant allele, the risk of having CD in an ileocolonic location was reduced compared to control subjects (OR = 0.56, CI = 0.32-0.97, P = 0.037), and the risk of requiring a bowel resection was also significantly reduced to 0.59 (CI = 0.37-0.95, P = 0.028) (Table 4). Only in individuals who were smokers at the time of diagnosis, did this allele have a significant impact on UC (OR = 0.48, CI = 0.25-0.94, P = 0.028).
Haplotype analysis
Haplotype analysis of two-SNPs was performed using HAPLO.SCORE. The results are summarized in Table 6. Haplotype frequencies were estimated, and association analyses were performed with respect to CD and UC and Caucasian controls. A score for each haplotype (Hap-score) was calculated and P-value was obtained for the significance of each Hap-score. A positive hap-score implied that the haplotype occurred more frequently in the CD or UC patient group. A global P-value indicated the overall association between haplotypes and the response. The results showed that there was no significant association between these haplotypes for either CD or UC patients as compared with control subjects, P = 0.82 and P = 0.18 respectively (Table 6).
Table 6.
Haplotype analysis of two-SNP TNF-α haplotype in IBD status in New Zealand IBD patients and Caucasians
| Haplotype | Case subject frequency (%) | Control subject frequency (%) | Hap-score | Haplotype-specific scores P | Global score statistics | |
| CD | Two SNPs TNF-α region | |||||
| [-308 (rs1800629), -238 (rs361525)] | ||||||
| GG | 75.3 | 76.7 | -0.76 | 0.45 | χ2 = 0.85, df = 3, P = 0.82 | |
| GA | 6.2 | 6.0 | 0.32 | 0.75 | ||
| AG | 18.2 | 17.3 | 0.59 | 0.56 | ||
| UC | Two SNPs TNF-a region | |||||
| [-308 (rs1800629), -238 (rs361525)] | ||||||
| GG | 73.9 | 76.4 | -1.31 | 0.19 | χ2 = 3.37, df = 2, P = 0.18 | |
| GA | 5.3 | 6.0 | -0.63 | 0.53 | ||
| AG | 20.8 | 17.5 | 1.79 | 0.07 |
In the analysis of the two SNPs (rs1800629, rs361525) in CD, the haplotypes in patient and control subjects occurred at equal frequencies (P > 0.05, Table 6). Frequency haplotype AA was uncommon in both CD and UC subjects, 0.3% and 0% respectively and 0% for control subjects.
Meta-analysis
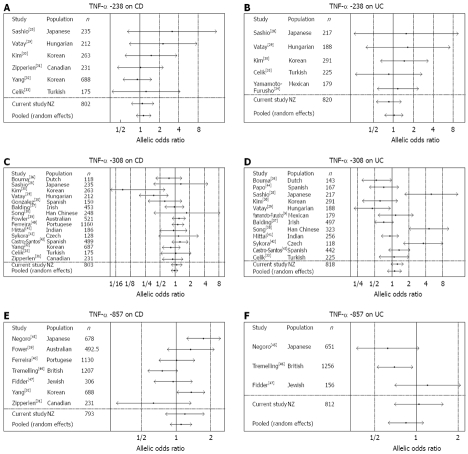
Forest plots in Figure 1 show the results of the meta-analysis of three common polymorphisms in the TNF-α receptor: -238, -308, and -857. Four to sixteen studies satisfied, depending on the TNF-α receptor, the inclusion criteria. All studies provided description of the participants, CD and UC status, and compared the control group with CD or UC subjects. We included our own data along with the other studies. Cochran’s Q test and I2 index were performed in order to examine the heterogeneity of the outcomes of the studies.
Figure 1.
Tree plots for meta-analysis. A: TNF-α -238 on CD; B: TNF-α -238 on UC; C: TNF-α -308 on CD; D: TNF-α -308 on UC; E: TNF-α -857 on CD; F: TNF-α -857 on UC.
TNF-α -238: The forest plot in Figure 1A shows the risk of CD in each study. These seven studies appeared to be homogeneous in results (Q statistic = 4.10, df = 6, P = 0.66) and I2 index was negative (I2 < 0). The pooled odds ratio for these studies was 1.15 (95% CI = 0.88-1.49), indicating that carrying the variant TNF-α -238G/A allele did not significantly affect the overall risk of CD. The forest plot of six studies on UC subjects with controls is shown in Figure 1B. These studies were reasonably homogeneous (Q statistic = 2.24, df = 5, P = 0.82, I2 < 0) and the pooled odds ratio was 1.04 (95% CI = 0.77-1.42), indicating that carrying the variant TNF-α -238G/A allele was not significantly associated with the overall risk of UC.
TNF-α -308: The forest plot of sixteen studies assessing the effect of carrying the variant allele on risk of CD is shown in Figure 1C. The combined estimate of odds ratio for these studies was 0.99 (95% CI = 0.84-1.15) by the random effect model with no homogeneity (Q statistic = 17.4, df = 15, P = 0.30, I2 = 0.14). This finding indicates that carrying the variant TNF-α -308G/A allele was not significantly associated with the risk of CD. In addition, Figure 1D provides a graphical summary of the risk of carrying the variant TNF-α -308G/A allele in UC. The results indicate that this variant was not significantly associated with the overall risk of UC. The pooled odds ratio for the thirteen studies was 1.14 (95% CI = 0.84-1.54) by the random effect model (Q statistic = 9.5, df = 12, P = 0.08, I2 = 0.39).
TNF-α -857: The forest plot Figure 1E shows the risk of CD in each study of carrying the variant TNF-α -857C/T allele. The overall estimate of odds ratio for the eight studies was 1.11 (95% CI = 0.89-1.38) by the random effect model with no homogeneity (Q statistic = 6.73, df = 7, P = 0.46, I2 < 0). Carrying the variant TNF-α -857C/T allele was not significantly associated with the risk of CD. In addition, the random effect model gave a pooled odds ratio of 0.84 (95% CI = 0.63-1.13) with no homogeneity (Q statistic = 3.1, df = 3, P = 0.38, I2 = 0.03) for carrying the variant TNF-α -857C/T allele in UC (Figure 1F).
The present meta-analysis shows that carrying the TNF-α receptor SNPs -238, -308, or -857 was not significantly associated with the risk of IBD, both in the New Zealand population as well as in the international studies. However, the present analysis does not provide any information on male-female differences or site specificity.
DISCUSSION
The present study adds to the international database available for all 3 alleles. In both males and females, carrying the variant TNF-α -238 G→A allele had no significant effect in our study population. Previous reports suggesting that this allele was a risk factor for IBD, especially CD, have generally used small sample sizes, and the data were not consistent. The initial publications reported positive data in Japanese, Hungarian and Korean groups, albeit with small numbers of patients. Kim et al[30] in a study on Korean patients observed a significantly higher frequency of -238A allele of TNF-α in CD patients with perianal lesions compared with patients without perianal disease. Vatay et al[29] also showed an increased risk in their study on Hungarian subjects. However, several negative studies have been published, including Levine et al[48] who examined a pediatric Jewish population, and Sashio et al[28] in a study on Japanese patients. In particular, the latter authors found a difference in the carrier frequency for haplotype AG (-308 A, -238 G) between UC patients and controls, and suggested that one of the genes responsible for UC may be the TNF gene. Our own haplotype analysis failed to confirm these findings. However, we observed that this SNP led to lower production of TNF-α in IBD patients[16].
The overall risk of either UC or CD was not significantly affected by carrying the TNF-α -308 G→A allele in our study. The meta-analysis shows 8 positive and 8 negative studies, leading to an overall allelic odds ratio of almost exactly zero. The published data are somewhat skewed by the strong negative association with CD found by Kim et al in the Korean population[30]. The data for UC are also somewhat dominated by the strong positive association reported by Sashio (Japanese)[28], Song (Han Chinese)[38] and Sykora (Czech)[42]. Our own data is close to the overall figure based on the meta-analysis on UC patients.
Subgroup analysis may provide greater information on this allele. The present study shows that individuals carrying the variant TNF-α -308 G→A allele have a significantly greater risk of pancolitis in UC, and are also more likely to require bowel resection. The probable need for bowel resection in these individuals is consistent with other reports. Cucchiara et al[49] reported that Italian CD patients carrying this allele were more frequently resistant to steroids compared with non-carriers, and were more likely to require surgical resection. They suggested a causal relationship between these two events. This is in contrast to the findings of Louis et al[50] who found that the presence of this variant favoured steroid-dependent disease and to a lesser extent fistulizing and colonic disease. Both authors suggested that this genotype indicated a more intense TNF-α-driven inflammatory reaction at the mucosal level.
The increased need for surgery in our subjects carrying the variant TNF-α -308 G→A allele is consistent with the observations of other authors, including Cucchiara et al[49] in an Italian pediatric cohort and Sykora et al[42], in their studies on Czech subjects. The latter group not only genotyped the TNF-α 308 G→A polymorphism, but also measured the serum levels of inflammatory C-reactive protein (CRP), in relation to disease activity. Both UC and CD patients carrying the TNF-α -308 A variant showed a significant increase in CRP. The authors concluded that the TNF-α 308 A polymorphism may play a role in modifying the IBD phenotype, influencing disease activity and leading to a more intense inflammatory activity. Other authors have also associated this genotype with inflammation, as measured by CRP or other measures[29,35,51].
Carrying the TNF-α -857C→T variant failed to modify the overall risk in our study. The tree diagram shows that the international database provides a good number of Japanese and Australian individuals with an increased risk for CD, whereas a small study on Canadian subjects suggests a strong protective effect. Although the overall risk of CD is somewhat increased, there appears to be a comparable decreased risk for UC associated with carrying the variant allele. However, the TNF-α -857C→T variant significantly decreased the risk of specific types and locations of CD. The risk of disease in an ileocolonic location decreased to 0.56 (limits 0.32-0.97), and the risk of requiring a bowel resection reduced to 0.59 (0.37-0.95). Only in individuals who were smokers at diagnosis, did this allele have an impact on UC [OR 0.48 (0.25-0.94)].
Fowler et al[39] identified a possible association of TNF-α -857 variant with an increased CD risk, especially in patients with structuring disease, in their case-control study on Australian subjects. Additionally, the TNF-α -857 CC genotype was independently associated with familial CD. The CD risk in their study was the strongest when individuals carried polymorphisms in both 308G/A and -857C/T. However, in a study in the UK, van Heel et al[25] showed an association of TNF-857C with IBD overall and with sub-phenotypes in either UC or CD, only in patients not carrying other common mutations. The transcription factor OCT1 binds TNF-857T but not TNF-857C, and interacts in vitro and in vivo with the pro-inflammatory NF-κB p65 subunit RELA at an adjacent binding site. van Heel et al[25] hypothesized that interaction of these transcription factors with specific alleles of TNF-α in gut tissue may be relevant in the pathogenesis of IBD.
Infliximab (IFX) is a monoclonal antibody against TNF-α that is commonly used as an IBD treatment. Ozeki et al[52] found that the -857T allele was in linkage with a lymphotoxin alpha (LTA) haplotype. They suggested that differences in therapeutic effects of IFX among patients with CD may be explained in part by the induction ability of TNF-α via the -857C/T polymorphism.
Each of the alleles in the present study appeared to enhance the risk in males as compared to females. Unfortunately, such gender stratification was not carried out in many of the other published studies. Therefore, it is not possible to determine whether this is true in other populations. However, it should be noted that such a sex imbalance is characteristic of the risks that have previously been associated with the IBD3 locus[6]. The TNF-α gene is closely linked to HLA-B[53], and both Satsangi et al[54] and Ruuls and Sedgewick[55] pointed to the difficulties of distinguishing the effect of TNF genes from that of other genes of the Major Histocompatibility Complex, including HLA, to susceptibility and disease phenotype in IBD. It is possible that genes in this region interact with one another to influence IBD risk, as has been suggested in cardiovascular disease[56]. We propose that our data is consistent with TNF-α itself being the key factor in the increased IBD risk that has so consistently been associated with the IBD3 region.
The analysis of SNPs in the TNF-α promoter may suggest both pharmacogenomic and nutrigenomic approaches to overcoming the pathway defect. Stio et al[57] observed that TX 527 [19-nor-14,20-bisepi-23-yne-1,25(OH)(2)D(3)], a Vitamin D analogue, could exert an immunosuppressive effect on TNF-α production in CD patients, and that this effect was mediated by NF-κB down-regulation. The activation of NF-κB leads to it’s migration into the nucleus where it binds to the DNA response elements in gene promoter regions. TX 527 inhibited the activation of NF-κB through the activation of the Vitamin D receptor (VDR). Thus, natural or synthetic vitamin D analogues may provide a basis for nutrigenomic or pharmacogenomic interventions that could be especially beneficial in individuals carrying variant alleles in the TNF-α promoter.
COMMENTS
Background
There is international recognition that the IBD3 region, on chromosome 6p21, IBD3 (MIM604519), confers susceptibility to inflammatory bowel disease (IBD). However, the nature of the relevant gene has been debated. Tumor necrosis factor-alpha (TNF-α) is a strong possibility, and variant single nucleotide polymorphisms (SNPs) in the TNF-α promoter have previously been associated in some studies with increased risk of IBD, while other studies have produced conflicting results. The present study provides data based on a substantial New Zealand cohort, and a meta-analysis, that suggests increased IBD risk in individuals carrying any of three functional SNPs in the TNF-α promoter.
Research frontiers
While an overall association with risk was not found, the carriers of either the -308 or -857 variants showed modified risk of specific IBD phenotypes. In particular, the study provides strong evidence that those individuals carrying the -308 G/A variant allele had an increased risk of pancolitis, and bowel resection in ulcerative colitis (UC). In contrast, carrying the -857 C/T variant decreased the risk of Crohn’s disease (CD) in an ileocolonic location, and for the need for a bowel resection.
Innovations and breakthroughs
The present study reveals that specific variant polymorphisms either increase the risk of certain forms of IBD, while others actually decrease the risk. Until now, there has been an assumption that all variants may be detrimental, but the present data suggests that this is not the case.
Applications
There may be some justification for genotyping IBD patients for the presence of these polymorphisms, since this may indicate the need for surgery (or not) at an early stage. Further studies may usefully stratify patients according to gender and disease characteristics.
Terminology
An “allele” is one of several alternative forms of a gene occupying a given locus on a chromosome. “SNP” describes a polymorphism (variation in sequence between individuals) caused by a change in a single nucleotide. This is responsible for most of the genetic variation between individuals.
Peer review
This is a well written paper. The analysis is especially welcome considering the different conclusions from different researchers. This is an interesting paper which indicated that SNPs in the promoter of TNF-α gene may play a role in the risk of IBD in a New Zealand population.
Acknowledgments
We thank the Canterbury participants of our study. Nutrigenomics New Zealand is in collaboration between AgResearch Ltd., Crop & Food Research, HortResearch and The University of Auckland.
Supported by Foundation for Research, Science and Technology, C02X0403: Gene-specific Foods
Peer reviewer: Seyed A Taghavi, Associate Professor, Department of Internal Medicine, Nemazee Hospital, No.23, 59th Alley, Ghasrodasht St., Shiraz 71838-95453, Iran
S- Editor Li DL L- Editor Anand BS E- Editor Ma WH
References
- 1.Duerr RH. The genetics of inflammatory bowel disease. Gastroenterol Clin North Am. 2002;31:63–76. doi: 10.1016/s0889-8553(01)00005-x. [DOI] [PubMed] [Google Scholar]
- 2.Ogura Y, Bonen DK, Inohara N, Nicolae DL, Chen FF, Ramos R, Britton H, Moran T, Karaliuskas R, Duerr RH, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. Nature. 2001;411:603–606. doi: 10.1038/35079114. [DOI] [PubMed] [Google Scholar]
- 3.Hampe J, Schreiber S, Shaw SH, Lau KF, Bridger S, Macpherson AJ, Cardon LR, Sakul H, Harris TJ, Buckler A, et al. A genomewide analysis provides evidence for novel linkages in inflammatory bowel disease in a large European cohort. Am J Hum Genet. 1999;64:808–816. doi: 10.1086/302294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rioux JD, Silverberg MS, Daly MJ, Steinhart AH, McLeod RS, Griffiths AM, Green T, Brettin TS, Stone V, Bull SB, et al. Genomewide search in Canadian families with inflammatory bowel disease reveals two novel susceptibility loci. Am J Hum Genet. 2000;66:1863–1870. doi: 10.1086/302913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dechairo B, Dimon C, van Heel D, Mackay I, Edwards M, Scambler P, Jewell D, Cardon L, Lench N, Carey A. Replication and extension studies of inflammatory bowel disease susceptibility regions confirm linkage to chromosome 6p (IBD3) Eur J Hum Genet. 2001;9:627–633. doi: 10.1038/sj.ejhg.5200687. [DOI] [PubMed] [Google Scholar]
- 6.Fisher SA, Hampe J, Macpherson AJ, Forbes A, Lennard-Jones JE, Schreiber S, Curran ME, Mathew CG, Lewis CM. Sex stratification of an inflammatory bowel disease genome search shows male-specific linkage to the HLA region of chromosome 6. Eur J Hum Genet. 2002;10:259–265. doi: 10.1038/sj.ejhg.5200792. [DOI] [PubMed] [Google Scholar]
- 7.Nedwin GE, Naylor SL, Sakaguchi AY, Smith D, Jarrett-Nedwin J, Pennica D, Goeddel DV, Gray PW. Human lymphotoxin and tumor necrosis factor genes: structure, homology and chromosomal localization. Nucleic Acids Res. 1985;13:6361–6373. doi: 10.1093/nar/13.17.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Old LJ. Tumor necrosis factor (TNF) Science. 1985;230:630–632. doi: 10.1126/science.2413547. [DOI] [PubMed] [Google Scholar]
- 9.Locksley RM, Killeen N, Lenardo MJ. The TNF and TNF receptor superfamilies: integrating mammalian biology. Cell. 2001;104:487–501. doi: 10.1016/s0092-8674(01)00237-9. [DOI] [PubMed] [Google Scholar]
- 10.Gaur U, Aggarwal BB. Regulation of proliferation, survival and apoptosis by members of the TNF superfamily. Biochem Pharmacol. 2003;66:1403–1408. doi: 10.1016/s0006-2952(03)00490-8. [DOI] [PubMed] [Google Scholar]
- 11.Knight JC, Udalova I, Hill AV, Greenwood BM, Peshu N, Marsh K, Kwiatkowski D. A polymorphism that affects OCT-1 binding to the TNF promoter region is associated with severe malaria. Nat Genet. 1999;22:145–150. doi: 10.1038/9649. [DOI] [PubMed] [Google Scholar]
- 12.Moffatt MF, Cookson WO. Tumour necrosis factor haplotypes and asthma. Hum Mol Genet. 1997;6:551–554. doi: 10.1093/hmg/6.4.551. [DOI] [PubMed] [Google Scholar]
- 13.Witte JS, Palmer LJ, O'Connor RD, Hopkins PJ, Hall JM. Relation between tumour necrosis factor polymorphism TNFalpha-308 and risk of asthma. Eur J Hum Genet. 2002;10:82–85. doi: 10.1038/sj.ejhg.5200746. [DOI] [PubMed] [Google Scholar]
- 14.Balding J, Kane D, Livingstone W, Mynett-Johnson L, Bresnihan B, Smith O, FitzGerald O. Cytokine gene polymorphisms: association with psoriatic arthritis susceptibility and severity. Arthritis Rheum. 2003;48:1408–1413. doi: 10.1002/art.10935. [DOI] [PubMed] [Google Scholar]
- 15.Mulcahy B, Waldron-Lynch F, McDermott MF, Adams C, Amos CI, Zhu DK, Ward RH, Clegg DO, Shanahan F, Molloy MG, et al. Genetic variability in the tumor necrosis factor-lymphotoxin region influences susceptibility to rheumatoid arthritis. Am J Hum Genet. 1996;59:676–683. [PMC free article] [PubMed] [Google Scholar]
- 16.Koss K, Satsangi J, Fanning GC, Welsh KI, Jewell DP. Cytokine (TNF alpha, LT alpha and IL-10) polymorphisms in inflammatory bowel diseases and normal controls: differential effects on production and allele frequencies. Genes Immun. 2000;1:185–190. doi: 10.1038/sj.gene.6363657. [DOI] [PubMed] [Google Scholar]
- 17.Wilson AG, Symons JA, McDowell TL, McDevitt HO, Duff GW. Effects of a polymorphism in the human tumor necrosis factor alpha promoter on transcriptional activation. Proc Natl Acad Sci USA. 1997;94:3195–3199. doi: 10.1073/pnas.94.7.3195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brinkman BM, Zuijdeest D, Kaijzel EL, Breedveld FC, Verweij CL. Relevance of the tumor necrosis factor alpha (TNF alpha) -308 promoter polymorphism in TNF alpha gene regulation. J Inflamm. 1995;46:32–41. [PubMed] [Google Scholar]
- 19.van Heel DA, Udalova IA, De Silva AP, McGovern DP, Kinouchi Y, Hull J, Lench NJ, Cardon LR, Carey AH, Jewell DP, et al. Inflammatory bowel disease is associated with a TNF polymorphism that affects an interaction between the OCT1 and NF(-kappa)B transcription factors. Hum Mol Genet. 2002;11:1281–1289. doi: 10.1093/hmg/11.11.1281. [DOI] [PubMed] [Google Scholar]
- 20.Gearry RB, Richardson A, Frampton CM, Collett JA, Burt MJ, Chapman BA, Barclay ML. High incidence of Crohn's disease in Canterbury, New Zealand: results of an epidemiologic study. Inflamm Bowel Dis. 2006;12:936–943. doi: 10.1097/01.mib.0000231572.88806.b9. [DOI] [PubMed] [Google Scholar]
- 21.Lennard-Jones JE. Classification of inflammatory bowel disease. Scand J Gastroenterol Suppl. 1989;170:2–6; discussion 16-19. doi: 10.3109/00365528909091339. [DOI] [PubMed] [Google Scholar]
- 22.Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR, Caprilli R, Colombel JF, Gasche C, Geboes K, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: Report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005;19 Suppl A:5–36. doi: 10.1155/2005/269076. [DOI] [PubMed] [Google Scholar]
- 23.Burt MJ, George PM, Upton JD, Collett JA, Frampton CM, Chapman TM, Walmsley TA, Chapman BA. The significance of haemochromatosis gene mutations in the general population: implications for screening. Gut. 1998;43:830–836. doi: 10.1136/gut.43.6.830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Allcock RJ, Windsor L, Gut IG, Kucharzak R, Sobre L, Lechner D, Garnier JG, Baltic S, Christiansen FT, Price P. High-Density SNP genotyping defines 17 distinct haplotypes of the TNF block in the Caucasian population: implications for haplotype tagging. Hum Mutat. 2004;24:517–525. doi: 10.1002/humu.20100. [DOI] [PubMed] [Google Scholar]
- 25.van Heel DA, Fisher SA, Kirby A, Daly MJ, Rioux JD, Lewis CM. Inflammatory bowel disease susceptibility loci defined by genome scan meta-analysis of 1952 affected relative pairs. Hum Mol Genet. 2004;13:763–770. doi: 10.1093/hmg/ddh090. [DOI] [PubMed] [Google Scholar]
- 26.Sasieni PD. From genotypes to genes: doubling the sample size. Biometrics. 1997;53:1253–1261. [PubMed] [Google Scholar]
- 27.Wigginton JE, Cutler DJ, Abecasis GR. A note on exact tests of Hardy-Weinberg equilibrium. Am J Hum Genet. 2005;76:887–893. doi: 10.1086/429864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sashio H, Tamura K, Ito R, Yamamoto Y, Bamba H, Kosaka T, Fukui S, Sawada K, Fukuda Y, Tamura K, et al. Polymorphisms of the TNF gene and the TNF receptor superfamily member 1B gene are associated with susceptibility to ulcerative colitis and Crohn's disease, respectively. Immunogenetics. 2002;53:1020–1027. doi: 10.1007/s00251-001-0423-7. [DOI] [PubMed] [Google Scholar]
- 29.Vatay A, Bene L, Kovacs A, Prohaszka Z, Szalai C, Romics L, Fekete B, Karadi I, Fust G. Relationship between the tumor necrosis factor alpha polymorphism and the serum C-reactive protein levels in inflammatory bowel disease. Immunogenetics. 2003;55:247–252. doi: 10.1007/s00251-003-0575-8. [DOI] [PubMed] [Google Scholar]
- 30.Kim TH, Kim BG, Shin HD, Kim JW, Kim CG, Kim JS, Jung HC, Song IS. [Tumor necrosis factor-alpha and interleukin-10 gene polymorphisms in Korean patients with inflammatory bowel disease] Korean J Gastroenterol. 2003;42:377–386. [PubMed] [Google Scholar]
- 31.Zipperlen K, Peddle L, Melay B, Hefferton D, Rahman P. Association of TNF-alpha polymorphisms in Crohn disease. Hum Immunol. 2005;66:56–59. doi: 10.1016/j.humimm.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 32.Yang SK, Lee SG, Cho YK, Lim J, Lee I, Song K. Association of TNF-alpha/LTA polymorphisms with Crohn's disease in Koreans. Cytokine. 2006;35:13–20. doi: 10.1016/j.cyto.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 33.Celik Y, Dagli U, Kilic MY, Toruner M, Ozen SC, Ozkan M, Soykan I, Cetinkaya H, Ulker A, Ozden A, et al. Cytokine gene polymorphisms in Turkish patients with inflammatory bowel disease. Scand J Gastroenterol. 2006;41:559–565. doi: 10.1080/00365520500349523. [DOI] [PubMed] [Google Scholar]
- 34.Yamamoto-Furusho JK, Uscanga LF, Vargas-Alarcon G, Rodriguez-Perez JM, Zuniga J, Granados J. Polymorphisms in the promoter region of tumor necrosis factor alpha (TNF-alpha) and the HLA-DRB1 locus in Mexican mestizo patients with ulcerative colitis. Immunol Lett. 2004;95:31–35. doi: 10.1016/j.imlet.2004.05.015. [DOI] [PubMed] [Google Scholar]
- 35.Gonzalez S, Rodrigo L, Martinez-Borra J, Lopez-Vazquez A, Fuentes D, Nino P, Cadahia V, Saro C, Dieguez MA, Lopez-Larrea C. TNF-alpha -308A promoter polymorphism is associated with enhanced TNF-alpha production and inflammatory activity in Crohn's patients with fistulizing disease. Am J Gastroenterol. 2003;98:1101–1106. doi: 10.1111/j.1572-0241.2003.07416.x. [DOI] [PubMed] [Google Scholar]
- 36.Bouma G, Xia B, Crusius JB, Bioque G, Koutroubakis I, Von Blomberg BM, Meuwissen SG, Pena AS. Distribution of four polymorphisms in the tumour necrosis factor (TNF) genes in patients with inflammatory bowel disease (IBD) Clin Exp Immunol. 1996;103:391–396. doi: 10.1111/j.1365-2249.1996.tb08292.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Balding J, Livingstone WJ, Conroy J, Mynett-Johnson L, Weir DG, Mahmud N, Smith OP. Inflammatory bowel disease: the role of inflammatory cytokine gene polymorphisms. Mediators Inflamm. 2004;13:181–187. doi: 10.1080/09511920410001713529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Song Y, Wu KC, Zhang L, Hao ZM, Li HT, Zhang LX, Qiao TD, Li CN, Fan DM. Correlation between a gene polymorphism of tumor necrosis factor and inflammatory bowel disease. Chin J Dig Dis. 2005;6:170–174. doi: 10.1111/j.1443-9573.2005.00226.x. [DOI] [PubMed] [Google Scholar]
- 39.Fowler EV, Eri R, Hume G, Johnstone S, Pandeya N, Lincoln D, Templeton D, Radford-Smith GL. TNFalpha and IL10 SNPs act together to predict disease behaviour in Crohn's disease. J Med Genet. 2005;42:523–528. doi: 10.1136/jmg.2004.027425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ferreira AC, Almeida S, Tavares M, Canedo P, Pereira F, Regalo G, Figueiredo C, Trindade E, Seruca R, Carneiro F, et al. NOD2/CARD15 and TNFA, but not IL1B and IL1RN, are associated with Crohn's disease. Inflamm Bowel Dis. 2005;11:331–339. doi: 10.1097/01.mib.0000158153.71579.b4. [DOI] [PubMed] [Google Scholar]
- 41.Mittal RD, Manchanda PK, Bid HK, Ghoshal UC. Analysis of polymorphisms of tumor necrosis factor-alpha and polymorphic xenobiotic metabolizing enzymes in inflammatory bowel disease: study from northern India. J Gastroenterol Hepatol. 2007;22:920–924. doi: 10.1111/j.1440-1746.2006.04538.x. [DOI] [PubMed] [Google Scholar]
- 42.Sykora J, Subrt I, Didek P, Siala K, Schwarz J, Machalova V, Varvarovska J, Pazdiora P, Pozler O, Stozicky F. Cytokine tumor necrosis factor-alpha A promoter gene polymorphism at position -308 G-->A and pediatric inflammatory bowel disease: implications in ulcerative colitis and Crohn's disease. J Pediatr Gastroenterol Nutr. 2006;42:479–487. doi: 10.1097/01.mpg.0000221917.80887.9e. [DOI] [PubMed] [Google Scholar]
- 43.Castro-Santos P, Suarez A, Lopez-Rivas L, Mozo L, Gutierrez C. TNFalpha and IL-10 gene polymorphisms in inflammatory bowel disease. Association of -1082 AA low producer IL-10 genotype with steroid dependency. Am J Gastroenterol. 2006;101:1039–1047. doi: 10.1111/j.1572-0241.2006.00501.x. [DOI] [PubMed] [Google Scholar]
- 44.Papo M, Quer JC, Gutierrez C, Broch M, Casellas F, Pastor RM, Olona M, Richart C. Genetic heterogeneity within ulcerative colitis determined by an interleukin-1 receptor antagonist gene polymorphism and antineutrophil cytoplasmic antibodies. Eur J Gastroenterol Hepatol. 1999;11:413–420. doi: 10.1097/00042737-199904000-00010. [DOI] [PubMed] [Google Scholar]
- 45.Negoro K, Kinouchi Y, Hiwatashi N, Takahashi S, Takagi S, Satoh J, Shimosegawa T, Toyota T. Crohn's disease is associated with novel polymorphisms in the 5'-flanking region of the tumor necrosis factor gene. Gastroenterology. 1999;117:1062–1068. doi: 10.1016/s0016-5085(99)70390-2. [DOI] [PubMed] [Google Scholar]
- 46.Tremelling M, Waller S, Bredin F, Greenfield S, Parkes M. Genetic variants in TNF-alpha but not DLG5 are associated with inflammatory bowel disease in a large United Kingdom cohort. Inflamm Bowel Dis. 2006;12:178–184. doi: 10.1097/01.MIB.0000217766.90766.37. [DOI] [PubMed] [Google Scholar]
- 47.Fidder HH, Heijmans R, Chowers Y, Bar-Meir S, Avidan B, Pena AS, Crusius JB. TNF-857 polymorphism in Israeli Jewish patients with inflammatory bowel disease. Int J Immunogenet. 2006;33:81–85. doi: 10.1111/j.1744-313X.2006.00572.x. [DOI] [PubMed] [Google Scholar]
- 48.Levine A, Karban A, Eliakim R, Shaoul R, Reif S, Pacht A, Wardi J, Yakir B, Silver EL. A polymorphism in the TNF-alpha promoter gene is associated with pediatric onset and colonic location of Crohn's disease. Am J Gastroenterol. 2005;100:407–413. doi: 10.1111/j.1572-0241.2005.41126.x. [DOI] [PubMed] [Google Scholar]
- 49.Cucchiara S, Latiano A, Palmieri O, Canani RB, D'Inca R, Guariso G, Vieni G, De Venuto D, Riegler G, De'Angelis GL, et al. Polymorphisms of tumor necrosis factor-alpha but not MDR1 influence response to medical therapy in pediatric-onset inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2007;44:171–179. doi: 10.1097/MPG.0b013e31802c41f3. [DOI] [PubMed] [Google Scholar]
- 50.Louis E, Belaiche J. Genetics of Crohn's disease behaviour. Acta Gastroenterol Belg. 2000;63:377–379. [PubMed] [Google Scholar]
- 51.Louis E, Vermeire S, Rutgeerts P, De Vos M, Van Gossum A, Pescatore P, Fiasse R, Pelckmans P, Reynaert H, D'Haens G, et al. A positive response to infliximab in Crohn disease: association with a higher systemic inflammation before treatment but not with -308 TNF gene polymorphism. Scand J Gastroenterol. 2002;37:818–824. [PubMed] [Google Scholar]
- 52.Ozeki T, Furuya Y, Nagano C, Matsui C, Takayanagi R, Yokoyama H, Yamada Y. Analysis of linkage between lymphotoxin alpha haplotype and polymorphisms in 5'-flanking region of tumor necrosis factor alpha gene associated with efficacy of infliximab for Crohn's disease patients. Mutat Res. 2006;602:170–174. doi: 10.1016/j.mrfmmm.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 53.Inoko H, Trowsdale J. Linkage of TNF genes to the HLA-B locus. Nucleic Acids Res. 1987;15:8957–8962. doi: 10.1093/nar/15.21.8957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Satsangi J, Jewell DP, Bell JI. The genetics of inflammatory bowel disease. Gut. 1997;40:572–574. doi: 10.1136/gut.40.5.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ruuls SR, Sedgwick JD. Unlinking tumor necrosis factor biology from the major histocompatibility complex: lessons from human genetics and animal models. Am J Hum Genet. 1999;65:294–301. doi: 10.1086/302517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Szalai C, Fust G, Duba J, Kramer J, Romics L, Prohaszka Z, Csaszar A. Association of polymorphisms and allelic combinations in the tumour necrosis factor-alpha-complement MHC region with coronary artery disease. J Med Genet. 2002;39:46–51. doi: 10.1136/jmg.39.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stio M, Martinesi M, Bruni S, Treves C, Mathieu C, Verstuyf A, d'Albasio G, Bagnoli S, Bonanomi AG. The Vitamin D analogue TX 527 blocks NF-kappaB activation in peripheral blood mononuclear cells of patients with Crohn's disease. J Steroid Biochem Mol Biol. 2007;103:51–60. doi: 10.1016/j.jsbmb.2006.07.008. [DOI] [PubMed] [Google Scholar]