Abstract
Objective
To establish the long term cumulative prevalence of asthma in children admitted to hospital with pneumonia and to examine the hypothesis that some children admitted to hospital with pneumonia may be presenting with undiagnosed asthma.
Design
Prospective study of a cohort of children previously admitted to hospital with pneumonia, followed up by postal questionnaires to their general practitioners and the children or their parents.
Setting
General practices in southwest England.
Participants
78 children admitted to the Royal Devon and Exeter Hospital between 1989 and 1991 with a diagnosis of pneumonia confirmed on independent review of x ray films.
Main outcome measures
Any diagnosis of asthma, use of any treatment for asthma, and asthma symptom scores.
Results
On the basis of a 100% response rate from general practitioners and 86% from patients or parents, the cumulative prevalence of asthma was 45%. A diagnosis of asthma was associated with a family history of asthma (odds ratio 11.23; 95% confidence interval 2.57 to 56.36; P=0.0002). Mean symptom scores were higher for all children with asthma (mean score 2.4; χ2=14.88; P=0.0001) and for children with asthma not being treated (mean 1.4; χ2=6.2; P=0.01) than for those without asthma (mean 0.2) .
Conclusions
A considerable proportion of children presenting to a district general hospital with pneumonia either already have unrecognised asthma or subsequently develop asthma. The high cumulative prevalence of asthma suggests that careful follow up of such children is worth while. Asthma is undertreated in these children; a structured symptom questionnaire may help to identify and reduce morbidity due to undertreatment.
Introduction
Current guidelines on asthma management in children emphasise the importance of early diagnosis and treatment.1 We have reported that 28% of children presenting to hospital with pneumonia were asthmatic, and that a third of these were newly diagnosed at six weeks' follow up after discharge.2
That study was limited by its inability to distinguish between true cases of asthma and postinfective bronchial hyperreactivity, which is much more common and declines with time.3 In addition, for ethical reasons, results were obtained only for those children followed up in hospital, who represented about 75% of the cohort admitted. The present study was designed to determine how many in the entire cohort developed asthma during prolonged follow up and how many were receiving appropriate treatment.
Methods
In the original study all children aged 16 and under admitted to the Royal Devon and Exeter Hospital (Wonford) between January 1989 and July 1991 and discharged with a diagnosis of pneumonia were identified from the hospital discharge records. These children's notes were then examined for age; sex; personal and family respiratory history; atopy; dates and duration of admission, discharge, and follow up; and details of the diagnosis and subsequent follow up, including spirometry and use of any inhaled or oral treatment for asthma. Asthma was defined as a history of asthma recorded in the admission notes or a doctor's written diagnosis of asthma in the follow up notes. Pneumonia was a clinical diagnosis confirmed in all cases by chest radiography. The data were stored and analysed with Epi-Info version 5.0.4
For the present study efforts were made to follow up all of the 131 children who were admitted with a diagnosis of community acquired pneumonia during the original study period. The chest radiographs relating to the original admission were traced and reviewed independently by two radiologists (DATS and JMC) who had not previously reported on any of the films. To reduce reporting bias they were also asked to report on the chest radiographs of 50 children without a primary diagnosis of pneumonia taken during the same period as the original cohort. Each radiologist was asked to report the presence or absence of objective features of pneumonia.5
The addresses of the children's current general practitioners were obtained from the hospital records. The general practitioners were sent a short questionnaire requesting confirmation of the child's address and information on any diagnosis or treatment of asthma and of further episodes of pneumonia. Non-responders were followed up once by telephone and once more by letter. In the case of a final failure to respond, or where a reply reported that the patient had moved, the Devon Patient and Practitioners Service Agency was contacted for the name of the current general practitioner, and the above procedure was repeated. Children who had moved from Devon without a forwarding address were considered lost to follow up.
The children who had been traced through the general practitioners' questionnaire (or their parents if they were still under 16 years of age) were sent a further questionnaire to identify further cases of asthma and assess the current level of symptom control. This questionnaire (box) used nine standard questions previously validated against symptoms of bronchial reactivity and asthma, which had been shown to have a high sensitivity and specificity for a diagnosis of asthma where three or more symptoms were present (symptom score ⩾3).6
Standardised asthma symptom questionnaire
Questions apply to the previous four weeks; each “yes” is scored 1 point
1 If you run or climb stairs fast do you ever cough?
2 If you run or climb stairs fast do you ever wheeze?
3 If you run or climb stairs fast do you ever get tight in the chest?
4 Is your sleep ever broken by wheeze?
5 Is your sleep ever broken by difficulty in breathing?
6 Do you ever wake up in the morning with wheeze?
7 Do you ever wake up in the morning with difficulty in breathing?
8 Do you ever wheeze if you are in a smoky room?
9 Do you ever wheeze if you are in a very dusty space?
Results
The chest radiographs were traced and reviewed in 93 (76%) of the original 131 children. The 78 (84%) children whose radiographs were agreed by both radiologists to show signs of pneumonia (κ=0.865, P<0.001) formed the group studied. The general practitioners of 70 of these were identified, and they all replied to our questionnaire. On combining their reports with data from the first study,2 we had cummulative follow up information for all 78 children.
The median interval from admission to this follow up was 68 months (range 61 to 91 months). The children's median age at admission was 4 years (range <1 to 16 years) and at second follow up was 9 years (range 5 to 22 years); 44 (57%) were male. At this follow up, 35 children (45%) had asthma. There was a declining temporal relation between diagnosis of asthma and time of admission to hospital with pneumonia: 8 cases were diagnosed in the first year after admission, 3 in the second year, 2 in the third year, 3 in the fifth year, and 2 in the sixth year.
Children diagnosed as asthmatic were significantly more likely than non-asthmatic children to have a family history of asthma (odds ratio 11.23; 95% confidence interval 2.57 to 56.36; P=0.0002). Asthmatic and non-asthmatic children did not differ in age at admission, sex, duration of admission, or number of times they had previously had pneumonia.
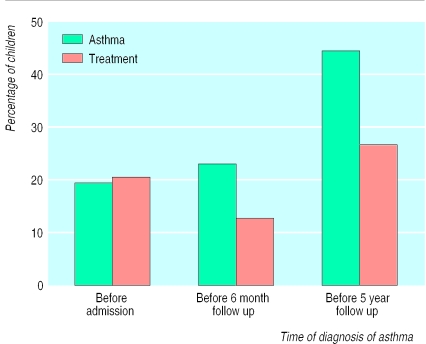
The rising cumulative prevalence of asthma throughout the study (χ2 for trend=11.8; P=0.0006) was not matched by a rise in the numbers receiving treatment for it (figure ).
All 70 patients whose general practitioners replied were sent the symptom questionnaire, and 60 returned completed forms (86% response rate). The mean symptom scores were 3.0 for all 28 children with asthma, 2.8 for the 19 asthmatic children receiving treatment, 1.6 for the 9 asthmatic children not receiving treatment, and 0.3 for the 32 children without asthma (P<0.0001 for asthma v no asthma; P<0.05 for treatment v no treatment; P=0.02 for no treatment v no asthma).
Discussion
The cumulative retrospective incidence of asthma 68 months after admission with pneumonia was 45%, which is much higher than expected in the general population. Children diagnosed as asthmatic were more likely to have a family history of asthma. The symptom scores of asthmatic children receiving treatment and those who were not were both significantly higher than those of non-asthmatic children.
This study achieved a high follow up rate due to the stability of the population studied: the current general practitioners of 90% of the children were traced, all of whom responded, and 86% of patients or their parents responded. The radiological review showed close agreement with the original diagnosis of pneumonia at admission and ensured the validity of the diagnosis in the cohort studied. The retrospective method of review, and the absence of a control group of children without a history of pneumonia, signal caution in interpreting the results; nevertheless we regard the method as a valid approach to establishing the cumulative prevalence of asthma in children with a history of pneumonia.
Incidence of asthma
Previous smaller controlled studies have shown a non-significant excess of asthma (7.8%) in children seven years7 and one year (6%)8 after infantile pneumonia, rising to 7% at eight year follow up of children under 2 admitted with pneumonia.9 In the current study the median age of children at admission was 4 years, and only 35% were aged 2 years or younger. Martinez has shown that over half of the children who wheeze at age 6 years had not done so before the age of 310; thus the older age of the children in this study may account for the higher incidence of asthma than in previous studies. This is supported by the large prospective study of Strachan et al, which showed a cumulative (prospective) incidence of wheezing illness of 18% by age 7, 24% by age 16, and 43% by age 33.11 The cumulative retrospective incidence of asthma by age 33 was 29%. The strongest associations of pneumonia with asthma in that study were in children aged over 2 years.
We believe that the high proportion of children with asthma identified in this study confirms our original conclusion that these children are worthy of careful follow up as a group at increased risk of developing asthma. It is to be expected that the prevalence of asthma will rise over time in any cohort, and adult onset wheeze is common and often missed.12 The declining temporal relation, however, supports our hypothesis that children with undiagnosed or “latent” asthma may first present with pneumonia.
Although we have shown a clear association of asthma with a history of pneumonia, this study has not considered whether the pneumonia is a predisposing factor for asthma or whether it occurs as a result of undiagnosed and untreated asthma. This research needs to be extended into primary care, where many more children with less severe respiratory infections are managed without referral to hospital
What is already known on this topic
Children admitted to hospital with pneumonia are sometimes subsequently found to be asthmatic, but no clear association has been shown
What this study adds
The cumulative prevalence of asthma after childhood pneumonia is high; therefore careful follow up is recommended to detect new cases
Childhood pneumonia may be an underrecognised presentation of asthma
A structured symptom questionnaire can facilitate recognition of symptoms
Treatment of asthma
The patient symptom questionnaire showed significantly higher symptom scores in both treated and untreated children with asthma than in those without asthma. The higher scores in children with asthma not receiving treatment suggest either a degree of undertreatment of known asthma, which has been identified as a problem for children with asthma in general,13 or that these reported symptoms reflect the level of disability which these children with asthma tolerate without seeking treatment.
Conclusions
This study shows that an appreciable proportion of children presenting to a district general hospital with a clinical and radiological diagnosis of pneumonia either already have unrecognised asthma or subsequently develop asthma. Careful follow up of such children is necessary to detect new cases of asthma and to facilitate their early treatment.
Figure.
Prevalence of asthma and treatment for asthma in 78 children admitted to hospital for pneumonia
Acknowledgments
We thank Dr Alex Ferguson for inspiring this project, Ms Frances Lobban and Mrs Jenny James for their secretarial work, our general practitioner colleagues throughout Devon for their cooperation, and our families for their support and patience.
Footnotes
Contributors: CEC gathered and analysed data from the original cohort of patients, and for this study traced patients' addresses and general practitioners, collected and analysed data, searched the literature, and helped draft the paper. DMGH originally proposed that this study be undertaken, advised on the study and questionnaire design, supervised and analysed the radiological review, and helped to draft the paper. JMC and DATS carried out the radiological review. CEC will act as guarantor for the paper.
Funding: CEC was supported by research grants from Ciba Laboratories and Boehringer Ingelheim.
References
- 1.British Thoracic Society; National Asthma Campaign; Royal College of Physicians of London; General Practitioners in Asthma Group; British Association of Accident and Emergency Medicine; British Paediatric Society; Royal College of Paediatrics and Child Health. British guidelines on asthma management. 1995 review and position statement. Thorax. 1997;52:S1–20. doi: 10.1136/thx.48.2_suppl.s1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clark CE. Is childhood pneumonia an unrecognised presentation of asthma? Asthma Gen Pract. 1997;5:9–11. [Google Scholar]
- 3.Korppi M, Kuikka L, Reijonen T, Remes K, Juntunen-Backman K, Launiala K. Bronchial asthma and hyperreactivity after early childhood bronchiolitis or pneumonia. An 8-year follow-up study. Arch Pediatr Adolesc Med. 1994;148:1079–1084. doi: 10.1001/archpedi.1994.02170100077015. [DOI] [PubMed] [Google Scholar]
- 4.Dean AG, Dean JA, Burton AH, Dicker RC. Epi-Info, Version 5: a word processing, database, and statistics program for epidemiology on microcomputers. Stone Mountain, GA: USD; 1990. [Google Scholar]
- 5.Armstrong P, Wilson AG, Dee PM, Hansell DM. Imaging of diseases of the chest. 2nd Edition. St Louis: Mosby; 1995. [Google Scholar]
- 6.Venables KM, Farrer N, Sharp L, Graneek BJ, Newman Taylor AJ. Respiratory symptoms questionnaire for asthma epidemiology: validity and reproducibility. Thorax. 1993;48:214–219. doi: 10.1136/thx.48.3.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mok JYQ, Simpson H. Outcome for acute bronchitis, bronchiolitis and pneumonia in infancy. Arch Dis Child. 1984;59:306–309. doi: 10.1136/adc.59.4.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Korppi M, Reijonen T, Pöysä L, Juntunen-Backman K. A 2- to 3-year outcome after bronchiolitis. Am J Dis Child. 1993;147:628–631. doi: 10.1001/archpedi.1993.02160300034017. [DOI] [PubMed] [Google Scholar]
- 9.Korppi M, Kuikka L, Reijonen T, Remes K, Juntunen-Backman K, Launiala K. Bronchial asthma and hyperreactivity after early childhood bronchiolitis or pneumonia. Arch Pediatr Adolesc Med. 1994;148:1079–1084. doi: 10.1001/archpedi.1994.02170100077015. [DOI] [PubMed] [Google Scholar]
- 10.Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonenen M Morgan WJ and the Group Health Medical Associates. Asthma and wheezing in the first six years of life. N Engl J Med. 1995;332:133–138. doi: 10.1056/NEJM199501193320301. [DOI] [PubMed] [Google Scholar]
- 11.Strachan DP, Butland BK, Anderson HR. Incidence and prognosis of asthma and wheezing illness from early childhood to age 33 in a national British cohort. BMJ. 1996;312:1195–1199. doi: 10.1136/bmj.312.7040.1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bodner C, Ross S, Douglas G, Little J, Legge J, Friend J, et al. The prevalence of adult onset wheeze: longitudinal study. BMJ. 1997;314:792–793. doi: 10.1136/bmj.314.7083.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Speight ANP, Lee DA, Hey EN. Underdiagnosis and undertreatment of asthma in childhood. BMJ. 1983;286:1253–1256. doi: 10.1136/bmj.286.6373.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]