The rationale for prescribing statins is well established.1 Recently there has been an increase in the rate of prescribing of lipid lowering drugs, although large variations remain between practices.2 Fewer prescriptions are written in practices in more deprived areas3; it is not clear what effect local guidelines have on such inequalities. The aim of this study was to describe changes in the rate of prescribing statins between general practices after the introduction of national and local guidelines.
Methods and results
The study population included 110 of 118 general practices in Nottingham. The main reason for excluding practices was poor quality data. Townsend scores, which measure deprivation on a scale of 4.8 (most deprived) to −3.6 (least deprived),4 were derived for practices using the weighted sum of census information from enumeration districts for patients registered with each practice. Data from prescribing and cost reports were collected over three six-month periods from 1 April to 30 September in 1996, 1997, and 1998. Average daily quantities were used to determine the daily dose of statins prescribed and were expressed as a rate (statin-years) of prescribing per 1000 patients aged 35-69. Variables were logarithmically transformed; multiple linear regression was used to examine the relation between prescribing and deprivation by adjusting for list size, practice status (training or fundholding or both), the number of general practitioners, total admissions standardised for age, rates of admissions and outpatient referrals, and the cost of all cardiovascular drugs excluding lipid lowering drugs.
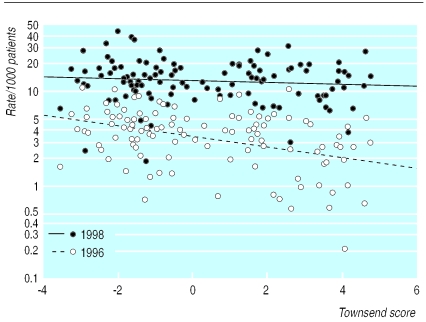
During 1996, the rates of prescribing statins varied from a median of 3.8 statin-years per 1000 adults overall and a median of 4.9 in the quintile of practices classed as least deprived to a median of 2.0 in the quintile classed as most deprived. These rates increased in 1998 to a median of 13.2 statin-years among all practices and to a median of 15.3 in the least deprived quintile and 10.8 in the most deprived. In each year practices in the most deprived areas had lower rates of prescribing than those in more affluent areas.
In 1996 there was a significant inverse relation between deprivation and rates of prescribing statins, with the Townsend score explaining 14% of the variation after adjustment for the costs of cardiovascular drugs and practice population aged 35-69 years (P<0.0005). In 1997 and 1998, proportionally larger increases in prescribing occurred among practices in more deprived areas; no significant relation between deprivation and prescribing rates was found during this time. Using Townsend scores of +3 and −3 to represent practices in deprived and more affluent areas, we found a 63% greater increase in prescribing statins among practices in deprived areas compared with those in more affluent areas between 1996 and 1997 and an 88% greater increase between 1997 and 1998 (figure).
Comment
The prescription of statins in primary care in Nottingham increased fourfold between 1996 and 1998; the greatest increase occurred in the most deprived areas. The data precluded assessment of the needs of individual patients.5 It is possible that patients in practices in deprived areas and patients in more affluent areas differed in their access to medical care, resulting in a lower level of prescribing in more deprived practices. The appropriateness of prescribing was not assessed; local guidelines on statins focused mainly on secondary prevention but we were not able to assess whether the reduction in the difference between the practices was due to the use of statins in secondary prevention.
We do not know whether the observed pattern of prescribing will change or whether the use of statins by practices in more deprived areas will continue to increase at different rates depending on the level of deprivation. A more detailed study is warranted to establish whether changes in prescribing were the result of the introduction of new guidelines in late 1996, increasing familiarity with statins, or an improved awareness of statins among practitioners in the most deprived areas.
Figure.
Relation between Townsend score of each practice and rate of statin prescribing per 1000 patients aged 35-69 in 1996 and 1998. Regression lines show unadjusted analyses
Acknowledgments
We would like to thank Nicola Alexander, pharmacy support officer, and Dr Sarah Wilson, director of public health, Nottingham Health Authority, for their help in preparing this work.
Footnotes
Funding: None.
Competing interests: None declared.
References
- 1.Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian simvastatin survival study (4S) Lancet. 1994;344:1383–1389. [PubMed] [Google Scholar]
- 2.Baxter C, Jones R, Corr L. Time trend analysis and variations in prescribing lipid lowering drugs in general practice. BMJ. 1998;317:134–135. doi: 10.1136/bmj.317.7166.1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Packham C, Robinson J, Morris J, Richards C, Marks P, Gray D. Statin prescribing in Nottingham general practices: a cross-sectional study. J Public Health Med. 1999;21:60–64. doi: 10.1093/pubmed/21.1.60. [DOI] [PubMed] [Google Scholar]
- 4.Townsend P, Phillmore P, Beattie A. Health and deprivation: inequality in the north. London: Croom Helm; 1988. [Google Scholar]
- 5.Picken DM, Payne JN, Haq IU, McCabe CJ, Ward SE, Jackson PR, et al. Statin therapy/HMG Co-A reductase inhibitor treatment in the prevention of coronary heart disease: guidance notes for purchasers 96/04. Sheffield: University of Sheffield; 1996. [Google Scholar]