Abstract
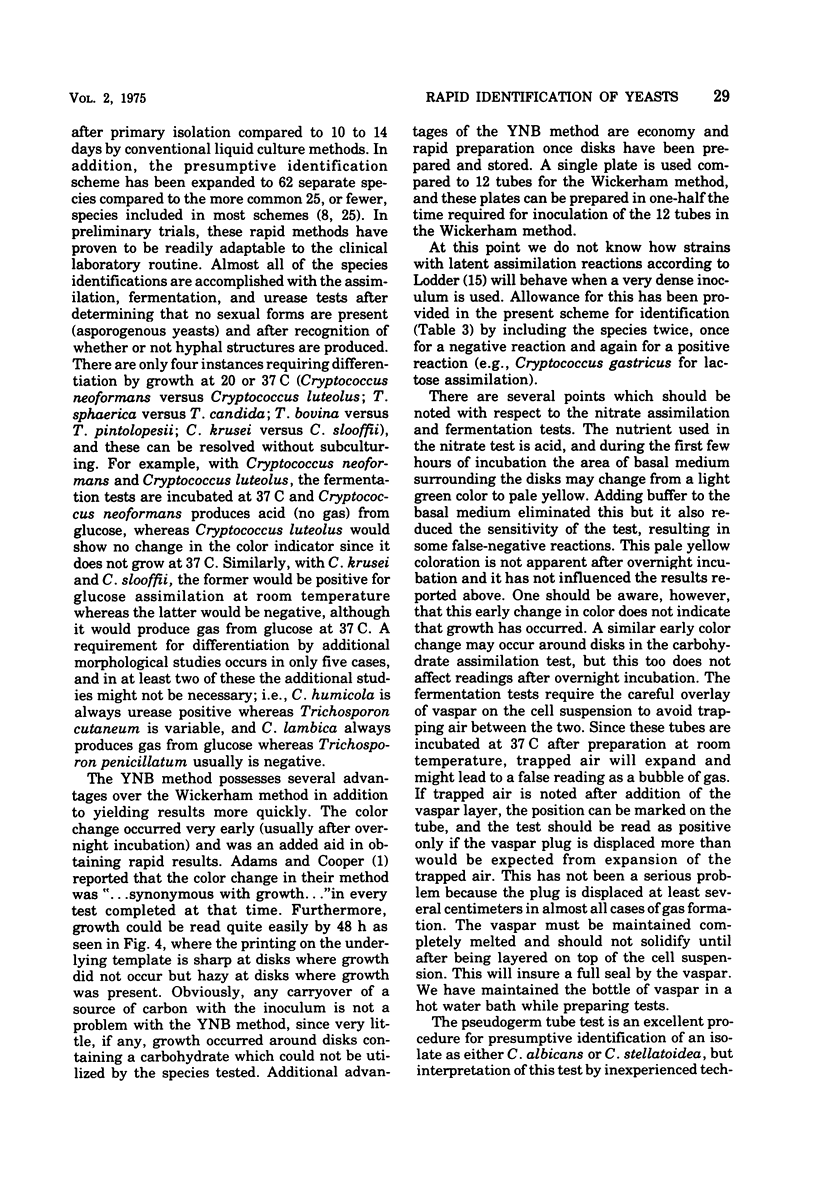
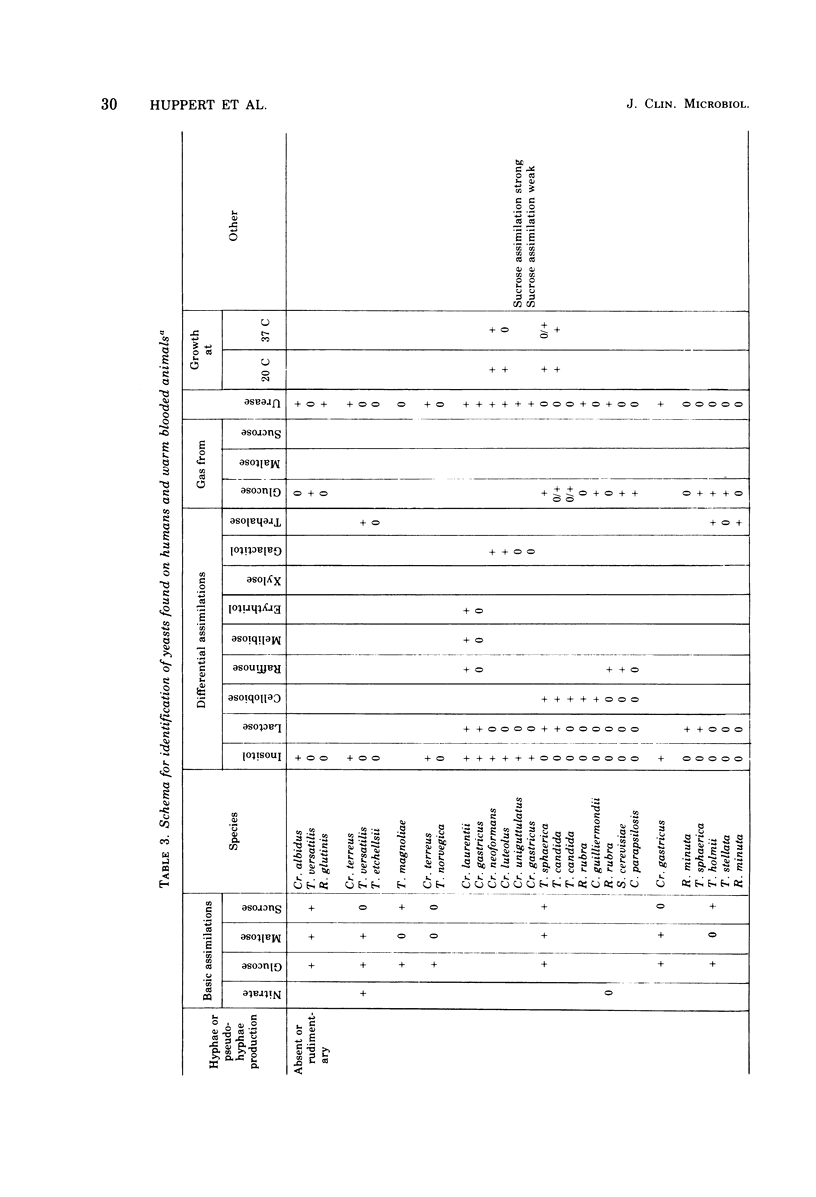
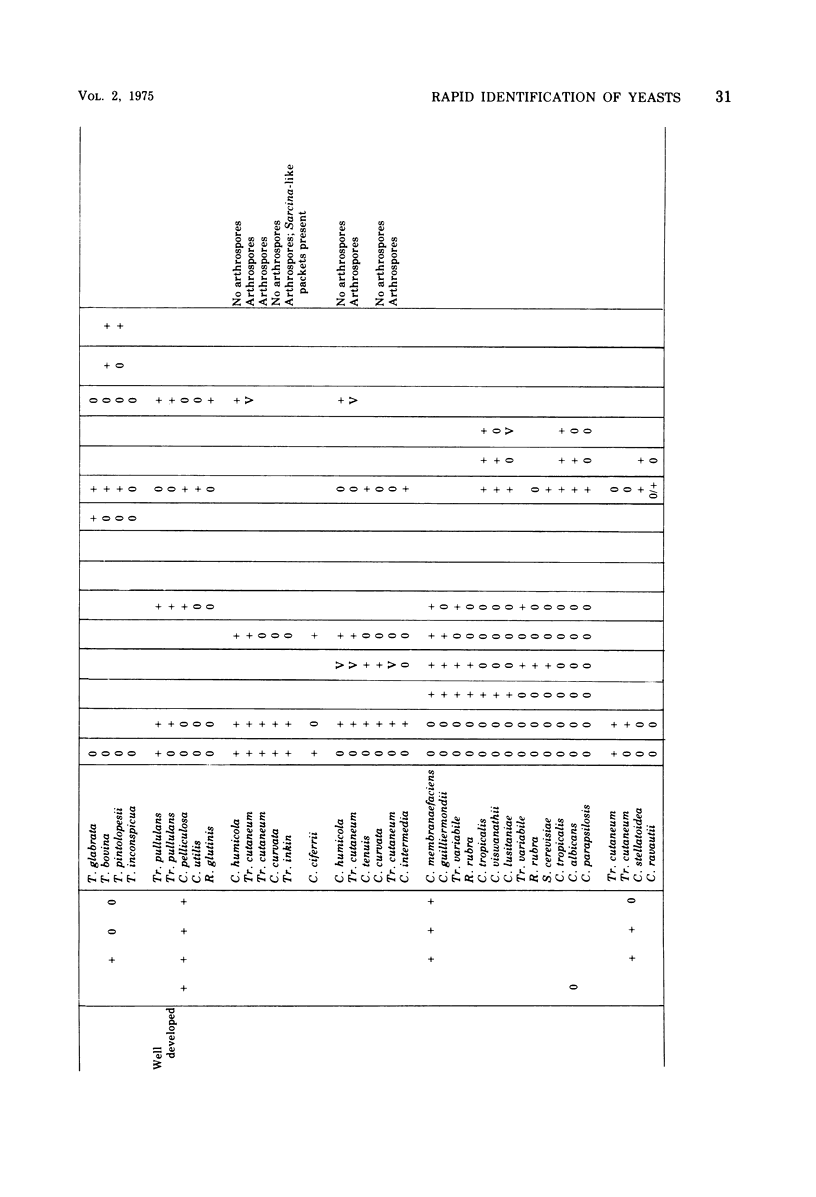
Opportunistic infections by yeasts have been implicated as one of the major causes of complications in the compromised patient. Rapid recognition and identification of these yeasts is essential for patient management, but conventional liquid medium methods for completing identification tests are cumbersome and time consuming. Rapid tests have been devised based on modifications of methods commonly used in bacteriology. These rapid methods included tests for carbohydrate and nitrate assimilation, fermentation, and urease production. These were compared with several current methods for accuracy of results, for time to final identification, and for economy of time and reagents. In addition, the usual tests for pseudogerm tube formation, for production of hyphae or pseudohyphae, and for growth temperatures were included. The rapid tests achieved 96% or better accuracy compared with expected results, and 46 species of yeasts were identified in 1 to 2 days compared with the 10 to 14 days required by conventional liquid culture methods.
Full text
PDF








Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adams E. D., Jr, Cooper B. H. Evaluation of a modified Wickerham medium for identifying medically important yeasts. Am J Med Technol. 1974 Sep;40(9):377–388. [PubMed] [Google Scholar]
- Dolan C. T. A practical approach to identification of yeast-like organisms. Am J Clin Pathol. 1971 May;55(5):580–590. doi: 10.1093/ajcp/55.5.580. [DOI] [PubMed] [Google Scholar]
- Dolan C. T., Woodward M. R. Identification of Cryptococcus species in the diagnostic laboratory. Am J Clin Pathol. 1971 May;55(5):591–595. doi: 10.1093/ajcp/55.5.591. [DOI] [PubMed] [Google Scholar]
- Gaines J. D., Remington J. S. Disseminated candidiasis in the surgical patient. Surgery. 1972 Nov;72(5):730–736. [PubMed] [Google Scholar]
- HUTER R. V., COLLINS H. S. The occurrence of opportunistic fungus infections in a cancer hospital. Lab Invest. 1962 Nov;11:1035–1045. [PubMed] [Google Scholar]
- Kahanpä A. Bronchopulmonary occurrence of fungi in adults especially according to cultivation material. Acta Pathol Microbiol Scand B Microbiol Immunol. 1972;227:1–147. [PubMed] [Google Scholar]
- Kauffman C. A., Tan J. S. Torulopsis glabrata renal infection. Am J Med. 1974 Aug;57(2):217–224. doi: 10.1016/0002-9343(74)90446-x. [DOI] [PubMed] [Google Scholar]
- Klainer A. S., Beisel W. R. Opportunistic infection: a review. Am J Med Sci. 1969 Dec;258(6):431–456. doi: 10.1097/00000441-196912000-00007. [DOI] [PubMed] [Google Scholar]
- Law E. J., Kim O. J., Stieritz D. D., MacMillan B. G. Experience with systemic candidiasis in the burned patient. J Trauma. 1972 Jul;12(7):543–552. doi: 10.1097/00005373-197207000-00001. [DOI] [PubMed] [Google Scholar]
- Louria D. B., Blevins A., Armstrong D., Burdick R., Lieberman P. Fungemia caused by "nonpathogenic" yeasts. Arch Intern Med. 1967 Mar;119(3):247–252. [PubMed] [Google Scholar]
- MacMillan B. G., Law E. J., Holder I. A. Experience with Candida infections in the burn patient. Arch Surg. 1972 Apr;104(4):509–514. doi: 10.1001/archsurg.1972.04180040123021. [DOI] [PubMed] [Google Scholar]
- Mackenzie D. W. Morphogenesis of Candida albicans in vivo. Sabouraudia. 1964 Jun;3(3):225–232. [PubMed] [Google Scholar]
- Mackenzie D. W. Studies on the morphogenesis of Candida albicans. II. Growth in organ extract. Sabouraudia. 1965 Jun;4(2):126–130. [PubMed] [Google Scholar]
- Miller R. M., Polakavetz S. H., Hornick R. B., Cowley R. A. Analysis of infections acquired by the severely injured patient. Surg Gynecol Obstet. 1973 Jul;137(1):7–10. [PubMed] [Google Scholar]
- Painter B. G., Isenberg H. D. Isolation of Candida parapsilosis: report of two cases. Am J Clin Pathol. 1973 Jan;59(1):62–65. doi: 10.1093/ajcp/59.1.62. [DOI] [PubMed] [Google Scholar]
- Pankey G. A., Daloviso J. R. Fungemia caused by torulopsis glabrata. Medicine (Baltimore) 1973 Sep;52(5):395–403. doi: 10.1097/00005792-197309000-00003. [DOI] [PubMed] [Google Scholar]
- Quie P. G., Chilgren R. A. Acute disseminated and chronic mucocutaneous candidiasis. Semin Hematol. 1971 Jul;8(3):227–242. [PubMed] [Google Scholar]
- Rifkind D., Marchioro T. L., Schneck S. A., Hill R. B., Jr Systemic fungal infections complicating renal transplantation and immunosuppressive therapy. Clinical, microbiologic, neurologic and pathologic features. Am J Med. 1967 Jul;43(1):28–38. doi: 10.1016/0002-9343(67)90146-5. [DOI] [PubMed] [Google Scholar]
- TASCHDJIAN C. L., BURCHALL J. J., KOZINN P. J. Rapid identification of Candida albicans by filamentation on serum and serum substitutes. AMA J Dis Child. 1960 Feb;99:212–215. doi: 10.1001/archpedi.1960.02070030214011. [DOI] [PubMed] [Google Scholar]



