Abstract
Objectives
To quantify the impact of NHS Direct on the use of accident and emergency, ambulance, and general practitioner cooperative services.
Design
Observational study of trends in use of NHS Direct and other immediate care services over 24 months spanning introduction of NHS Direct.
Setting
Three areas in England in first wave of introduction of NHS Direct, and six nearby general practitioner cooperatives as controls.
Subjects
All contacts with these immediate care services.
Main outcome measures
Changes in trends in use after introduction of NHS Direct.
Results
NHS Direct received about 68 500 calls from a population of 1.3 million in its first year of operation, of which 72% were out of hours and 22% about a child aged under 5 years. Changes in trends in use of accident and emergency departments and ambulance services after introduction of NHS Direct were small and non-significant. Changes in trends in use of general practitioner cooperatives were also small but significant, from an increase of 2.0% a month before introduction of NHS Direct to −0.8% afterwards (relative change −2.9% (95% confidence interval −4.2% to −1.5%)). This reduction in trend was significant both for calls handled by telephone advice alone and for those resulting in direct contact with a doctor. In contrast, the six control cooperatives showed no evidence of change in trend; an increase of 0.8% a month before NHS Direct and 0.9% after (relative change 0.1% (−0.9% to 1.1%)).
Conclusion
In its first year NHS Direct did not reduce the pressure on NHS immediate care services, although it may have restrained increasing demand on one important part—general practitioners' out of hours services.
Introduction
NHS Direct, the national, nurse led telephone helpline, was announced in December 19971 following the recommendations in the chief medical officer's report Developing Emergency Services in the Community, which appeared three months earlier.2 The purpose of the new service was to provide “easier and faster advice and information for people about health, illness and the NHS so that they are better able to care for themselves and their families.” Although more specific objectives for NHS Direct have not been published, the chief medical officer's report expressed the hope that a national telephone helpline might “help reduce or limit the demand” on other parts of the NHS, in particular ambulance services, accident and emergency departments, and general practitioner cooperatives.2
There is little existing evidence on the effect of publicly available telephone helplines on the nature and volume of demand for health services. Although there is evidence that telephone consultations may reduce the subsequent use of health services by individual patients, at least in the short term,3–5 the effects on population demand and in the longer term are unknown. The objective of this study was to assess the effect of NHS Direct on overall demand for NHS immediate care services in its first year of operation.
Subjects and methods
Data sources
The study was confined to examining the three sites of the first wave of NHS Direct—covering Preston and Chorley, Milton Keynes, and Northumbria—which have been operational since March 1998. These sites initially provided a service to about 1.3 million people, which did not change during the period of this study. The sites have since been expanded to serve about 4.3 million people. We used the call logs created by the decision support software in use at each site to determine the number and characteristics of calls to NHS Direct.
We sought routine data on activity in the year before and year after the introduction of NHS Direct from the ambulance services, accident and emergency departments, and general practitioner cooperatives within the study areas. Data on emergency journeys were provided by each of the three ambulance services. We restricted these to journeys originating within the NHS Direct areas by means of, depending on the service, the postcode, telephone dialling code, or health authority area of the patient, with the method used constant across the study period. Data on first attendances were provided by each of the 11 accident and emergency departments, and on patient calls by four of the five general practitioner cooperatives within the study areas. Of these four, three provided services for essentially all general practitioners in their areas, while the fourth covered about 70% of general practitioners. The fifth general practitioner cooperative was not computerised and was unable to provide data for the analysis.
For each area, we sought comparator data from two neighbouring general practitioner cooperatives that were not themselves covered by NHS Direct during the study period. These six cooperatives were computerised and had been in existence since at least March 1997. In two, the number of practices and patients covered increased slightly during the study period, and the numbers of contacts were deflated to take account of this.
Analysis
We examined the effects of NHS Direct on the use of ambulance, accident and emergency, and general practitioner cooperative services by fitting simple models to the data on the number of monthly contacts with each type of service. After examining the serial correlation between error terms (using the Durbin-Watson statistic), we used these models to treat the monthly counts of service contacts as independent and the month effects as simple fixed effects. These models were fitted in order to remove any systematic monthly variation in service use before we tested whether the introduction of NHS Direct was associated with a change in the linear trend in use of each service in each area, using Draper and Smith's model.6 We also tested whether any estimated changes in the trend in use of general practitioner cooperatives in the three NHS Direct areas were different from those for the six control cooperatives.
We assumed any effects of NHS Direct to be multiplicative and fitted the models to the log counts, which we assumed to be normally distributed for the purposes of testing for a change in trend. We also tested models that assumed Poisson counts and were fitted to the square root of the counts: these gave similar results, and only the multiplicative models are reported here.
Results
NHS Direct activity
In its first year of operation NHS Direct logged about 68 500 calls from the 1.3 million people served, of which 49 375 (72%) were made out of hours (between 6 pm and 8 am, or at weekends). The monthly number of calls rose steadily during this period. Of the 60 180 (88%) calls for which a patient's age was recorded, 13 447 (22%) were made on behalf of a child under 5 years old. Problems presented by callers were highly diverse, with the commonest—diarrhoea and vomiting, upper respiratory symptoms, fever, abdominal pain, skin rashes, and wounds—being those of “acute primary care.”7 For triaged calls, callers were advised to contact a general practitioner (30-49% of calls, depending on site), attend an accident and emergency department (14-27%), or use self care (30-35%) or were diverted to the emergency service (2-3%). Table 1 summarises the principal characteristics of the three sites.
Table 1.
Characteristics of NHS Direct service in the three sites for first wave of service
| Site
|
|||
|---|---|---|---|
| Milton Keynes | Preston and Chorley | Northumbria | |
| Host organisation | Ambulance service trust | Ambulance service trust | Ambulance service trust |
| Population served | 185 000 | 370 000 | 757 000 |
| Population type | Mainly urban | Mixed urban and rural | Inner city, surrounding conurbation, and large rural area |
| Staffing | Call handlers and nurses in single call centre | Call handlers in call centre, nurses in two accident and emergency departments | Call handlers and nurses in single call centre |
| Decision support software | Centramax | Telephone Advice System | Personal Health Advisor |
| No of calls in first year | 23 842 | 23 787 | 20 877 |
| Annual call rate per 1000 population | 129 | 64 | 28 |
Impact on other services
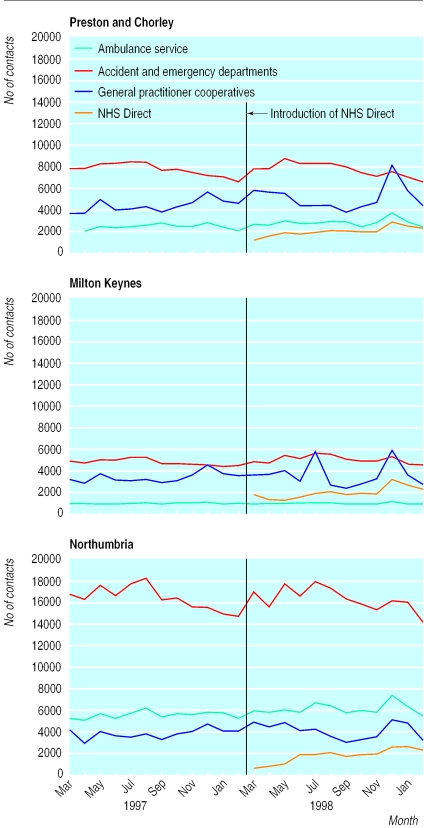
Figure 1 shows total demand for emergency ambulance journeys, first attendances at accident and emergency departments, and all calls to general practitioner cooperatives for each area, alongside the number of calls to NHS Direct. The figure shows substantial monthly variation in contacts with all services but no obvious impact of NHS Direct on the numbers of contacts. When we restricted contacts to the “least serious” for each service—ambulance category C calls, accident and emergency attendances triaged as non-urgent, and calls to cooperatives dealt with by telephone advice alone—we again found no obvious impact of NHS Direct (values not shown).8
Figure 1.
Contacts with immediate care services before and after introduction of NHS Direct in Preston and Chorley, Milton Keynes, and Northumbria
Statistical models
After allowing for systematic monthly variation in the nine time series shown in figure 1, we found no consistent evidence of any serial correlation between the monthly numbers of contacts (table 2). Based on the assumption that the monthly counts are independent, the models found no significant change in the trend in use of services in each area, with the exception of general practitioner cooperatives in Northumbria. Changes in trends in the use of ambulance and accident and emergency services were small and variable. However, estimated changes in the use of general practitioner cooperatives were more consistent, showing a change from an increase of about 2% a month before March 1998 to a decrease of between 0.2% and 1.3% a month afterwards.
Table 2.
Estimated effect of introduction of NHS Direct on changes in service use
| Service | Durbin-Watson statistic (significance*) | Estimated trend in use per month (%)
|
Change in trend (95% CI) | Test statistic† | |
|---|---|---|---|---|---|
| Before introduction | After introduction | ||||
| Ambulance services | |||||
| Milton Keynes | 1.9 (NS) | 0.7 | −0.2 | −0.9 (−2.0 to 0.2) | t=−1.61, P=0.14 |
| Preston and Chorley | 1.1 (S) | 1.0 | 0.9 | −0.1 (−1.7 to 1.6) | t=−0.11, P>0.5 |
| Northumbria | 1.6 (NS) | 0.8 | 0.6 | −0.2 (−1.2 to 0.8) | t=−0.45, P>0.5 |
| Accident and emergency departments | |||||
| Milton Keynes | 1.1 (S) | 0.2 | 0.7 | 0.5 (−0.2 to 1.3) | t=1.42, P=0.16 |
| Preston and Chorley | 2.6 (I) | 0.0 | −0.1 | −0.1 (−0.8 to 0.5) | t=−0.34, P>0.5 |
| Northumbria | 2.3 (NS) | −0.1 | 0.0 | 0.2 (−0.5 to 0.8) | t=0.52, P>0.5 |
| General practitioner cooperatives | |||||
| Milton Keynes | 2.4 (NS) | 1.9 | −0.9 | −2.8 (−6.5 to 1.1) | t=−1.42, P=0.16 |
| Preston and Chorley | 1.2 (I) | 2.2 | −0.2 | −2.3 (−5.0 to 0.4) | t=−1.71, P=0.09 |
| Northumbria | 1.6 (NS) | 2.1 | −1.3 | −3.4 (−5.7 to −1.0) | t=−2.82, P=0.02 |
S=significant at P=0.05 but not at p=0.025; NS=not significant; I=inconclusive.
All t statistics have 10 degrees of freedom except for ambulance services in Milton Keynes, which had 9 because of one missing data point.
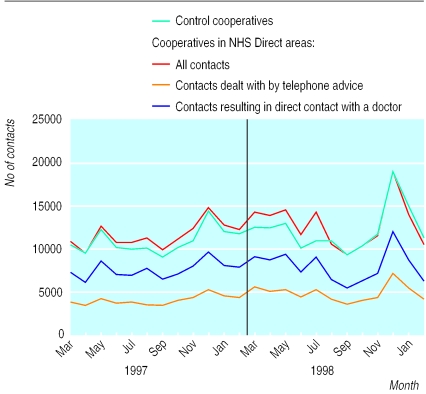
Analysis of general practitioner cooperative calls
Calls to general practitioner cooperatives may be handled by telephone advice alone or result in direct contact with a doctor, in either an out of hours treatment centre or the patient's home. The model we fitted to the data found strong statistical evidence that for both types of call there was a significant change in trend in March 1998 (table 3), so we compared these data with those from six control cooperatives. Figure 2 shows the monthly number of calls to the cooperatives in NHS Direct areas (also shown by type of call) and those to the control cooperatives. The change in trend in use in the NHS Direct areas was significantly different from that in the controls: in the three NHS Direct areas the estimated trend changed from 2.0% a month before NHS Direct to −0.8% afterwards (estimated relative change −2.9% (95% confidence interval −4.2% to −1.5%)), whereas in the six control cooperatives the trend hardly changed, from 0.8% a month before to 0.9% afterwards (relative change 0.1% (−0.9% to 1.1%)).
Table 3.
Estimated effect of introduction of NHS Direct on changes in use of general practitioner cooperatives
| Service | Estimated trend in use per month (%)
|
Change in trend (95% CI) | Test statistic | |
|---|---|---|---|---|
| Before introduction | After introduction | |||
| NHS Direct areas: | ||||
| Calls managed by telephone advice | 2.7 | −0.1 | −2.7 (−4.3 to −1.1) | t56=−3.38, P<0.01 |
| Calls resulting in direct contact with doctor | 1.8 | −1.3 | −3.0 (−4.7 to −1.2) | t56=−3.37, P<0.01 |
| All calls | 2.0 | −0.8 | −2.9 (−4.2 to −1.5) | t191=−4.25, P<0.01* |
| Control cooperatives | 0.8 | 0.9 | 0.1 (−0.9 to 1.1) | t191=0.17, P>0.5* |
Test statistic for difference in change in trend between NHS Direct areas and control cooperatives: F1,7=26.3, P<0.01.
Figure 2.
Contacts with general practitioner cooperatives in areas where NHS Direct was introduced and in control cooperatives
Discussion
NHS Direct represents a substantial, and growing, proportion of all contacts with immediate care services in the areas examined. However, the use of ambulance services and accident and emergency departments did not seem to have been affected by the introduction of NHS Direct in any clearly identifiable way, although in the future the least urgent (category C) ambulance calls may be transferred to NHS Direct, with the intention of relieving some of the pressure on ambulance services.9 On the other hand, we found a more consistent pattern of impact on the use of general practitioner cooperatives, and the model we fitted to the data, based on the assumption that the effect was the same in all three areas, estimated that the introduction of NHS Direct was associated with a halting of the previous trend of increasing use of cooperatives. The effect of NHS Direct was similar for cooperative contacts managed by telephone advice alone and those resulting in face to face contact with a doctor.
This picture, of little effect on overall demand for accident and emergency and ambulance services but some impact on demand for general practitioner cooperative services, is not unexpected since NHS Direct is used largely as a telephone out of hours service, with a case mix similar to that of general practitioner cooperatives rather than emergency calls or non-urgent accident and emergency cases.7 A survey of NHS Direct callers, carried out in its first year,8 found that most respondents (61%) said that without NHS Direct they would have contacted their general practitioner (unpublished data), suggesting that cooperatives might be the most likely to feel any effect of the service. Overall, our evidence suggests that a substantial number of callers to NHS Direct would otherwise have called their out of hours general practitioner cooperative and that a sufficiently large proportion of these callers were diverted to self care or other services to more than compensate for any extra demand generated by NHS Direct directing callers on to out of hours general practitioner services. However, given that up to half of callers were advised to contact their general practitioner, and many would have done so during normal surgery hours, there might have been a different effect on general practitioners' workload in working hours. We were unable to examine this in the current study.
It is perhaps surprising that the thousands of calls to NHS Direct each month did not have a more visible impact on overall demand for immediate care services. The impression, rather, is that the NHS Direct contacts simply added to the overall picture of health service use for immediate health problems. It remains possible that NHS Direct improved the appropriateness of demand for other services without having had a great impact on total demand, although the apparent stability of “least serious” demand for each service suggests that such an effect could not have been a large one.
Some have argued that NHS Direct may simply represent an “extra step” for people to access services that they would have accessed anyway. However, the evidence from the data presented here, alongside users' accounts of their intentions before and actions after a call,7 suggests that this rather simplistic view is unlikely to be the case. It is more likely, as indicated above, that several different effects are operating, the sum of which has so far resulted in only a small change in overall service demand. The fact that these effects have so far remained roughly in balance does not guarantee that this will always remain the case.
Limitations of study
Evidence from observational before and after studies such as this is open to different interpretations, and attribution to specific causes must always be speculative. The routine data on which this study is based are also of uncertain quality, although they should be comparable across the short period we have examined. Nevertheless, the data provide some evidence that NHS Direct has had little impact on accident and emergency and ambulance services but a modest impact on general practitioner cooperatives. The fact that this evidence is consistent with what we know about how NHS Direct is being used supports this conclusion. Our findings relate to first wave services in their first year of operation, which may not be typical of later NHS Direct organisation or activity. Whether the observed effects will be sustained or change in the future, particularly as use of NHS Direct grows, the service develops, and other services such as walk in centres are introduced, is unclear.
Conclusions
Overall, evidence from the first year of NHS Direct suggests that it has not “reduced the pressure” on the NHS, although it may have restrained the increasing pressure on one important part—general practitioner out of hours services. On the other hand, we can also say that there is no evidence that NHS Direct has been associated with any increase in demand for immediate care. If it turns out to be the case that NHS Direct has provided “easier and faster advice and information,” and has improved access to health care for those who need it, then the fact that this has been achieved without increasing demand on other services seems encouraging.
What is already known on this topic
Telephone consultations may reduce subsequent use of health services by individuals in the short term, but the effect on overall population demand in the longer term is unknown
What this study adds
In its first year, NHS Direct had no discernible effect on use of emergency ambulances or accident and emergency departments
NHS Direct was associated with a halt in the upward trend in use of general practitioner cooperatives, although the effect on overall demand for out of hours general practice was small
Overall, during its first year of operation NHS Direct had little impact on the demand for urgent health care
Acknowledgments
We thank the many individuals, including staff of NHS Direct sites, local services, the software companies, and the NHS Executive, who kindly provided data for our analyses, and Professor Mike Campbell for statistical advice.
Footnotes
Funding: This work was funded by the Department of Health. The views expressed are those of the authors and not necessarily those of the Department of Health
Competing interests: None declared
References
- 1.Department of Health. The New NHS: modern, dependable. Cmd 3807. London: Stationery Office; 1997. [Google Scholar]
- 2.Calman K. Developing emergency services in the community. The final report. London: NHS Executive; 1997. [Google Scholar]
- 3.Balas EA, Jaffrey F, Kuperman GJ, Boren SA, Brown GD, Pinciroli F, Mitchell JA, et al. Electronic communication with patients. Evaluation of distance medicine technology. JAMA. 1997;278:152–159. [PubMed] [Google Scholar]
- 4.Lattimer V, George S, Thompson F, Thomas E, Mullee M, Turnbull J, et al. Safety and effectiveness of nurse telephone consultation in out of hours primary care: randomised controlled trial. BMJ. 1998;317:1054–1059. doi: 10.1136/bmj.317.7165.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gallagher M, Huddart T, Henderson B. Telephone triage of acute illness by a practice nurse in general practice: outcomes of care. Br J Gen Pract. 1998;48:1141–1145. [PMC free article] [PubMed] [Google Scholar]
- 6.Draper NR, Smith H. Applied regression analysis. 2nd ed. Chichester: John Wiley and Sons; 1981. [Google Scholar]
- 7.Munro J, Nicholl J, O'Cathain A, Knowles E. Evaluation of NHS Direct first wave sites: second interim report to the Department of Health. Sheffield: Medical Care Research Unit; 2000. [Google Scholar]
- 8.Munro J, Nicholl J, O'Cathain A, Knowles E. Evaluation of NHS Direct first wave sites: first interim report to the Department of Health. Sheffield: Medical Care Research Unit; 1999. [Google Scholar]
- 9.Watt N. NHS advice line to handle some 999 calls. Guardian 2000 Mar 20:1.