Abstract
Background
There is increasing concern about discontinuity of care across transitions (e.g. from home to hospital) and how that might affect appropriate medical management. We examined the changes over time in outpatient to inpatient continuity in individuals hospitalized with advanced lung cancer and its relationship to end of life ICU use.
Methods
Retrospective analysis of the linked Surveillance, Epidemiology and End Results (SEER) – Medicare database. Subjects were 21,183 Medicare beneficiaries aged 66 years or older diagnosed with Stage IIIB or IV lung cancer between January 1, 1992 and December 31, 2002 who died within a year of diagnosis from 1992 through 2003. Outpatient to inpatient continuity is defined as an inpatient visit by the patient's usual care provider during the last hospitalization. The primary outcome measure is ICU use during the last hospitalization.
Results
Outpatient to inpatient continuity decreased from 60.1% in 1992 to 51.5% in 2002 (p<0.001). Factors associated with decreased continuity included: male gender, black race, low socioeconomic status, being unmarried, treatment by a hospitalist, and treatment in a teaching hospital. ICU use increased by 5.8% per year from 1993–2002. After adjusting for patient characteristics, patients with outpatient to inpatient continuity had a 25.1% reduced odds of spending time in an ICU during the terminal hospitalization.
Conclusion
Outpatient to inpatient continuity of care declined during the 1990s and early 2000s. Patients with terminal lung cancer who experienced continuity of care across the outpatient to hospital settings were less likely to spend time in the ICU prior to death.
Keywords: continuity of care, older adults, lung cancer, ICU use, end of life care, hospitalist
Introduction
Continuity of care is a key attribute of good medical care 1. Provider continuity is associated with improved patient satisfaction, increased use of preventive care services, fewer emergency room visits, lower hospitalization rates and reduced health care costs2–16. For cancer patients, it is a desirable attribute of a good patient-physician relationship17. Cancer patients with outpatient provider continuity have reduced emergency room visits and are more likely to die out-of-hospital during end of life18, 19.
American health care has undergone major changes over the past two decades. Some of these changes might threaten continuity of care, whereby a patient has a long-standing relationship with a physician. Such changes include: Health Maintenance Organization (HMO) networks with shifting patient eligibility and physician membership; continued growth of specialists; and the hospitalist movement20–24. One type of continuity of care is across transitions: home to hospital, hospital to home, hospital to nursing home, etc. Little is known about outpatient to inpatient continuity. Transitions between care settings jeopardize continuity of care, patient safety, and quality of care25–28. A recent study of transitions between care settings during end of life showed that 62% of patients experience one or more transitions during the last 3 months of life29. Most of this transition is from home to hospital, raising issues of continuity of care.
Lack of continuity of care may affect health care decisions, in particular, end of life decisions, when trust and values become critical17. Physicians unfamiliar with the patient may not know the patient’s wishes or values, and may not be good at discussing end of life choices, such as hospice or palliative care30.
In this study we assessed continuity of care in patients with advanced lung cancer. We addressed the following questions: did outpatient to inpatient continuity of care among advanced lung cancer patients change over time? Also, was lack of outpatient to inpatient provider continuity associated with an increased risk of an ICU stay? Finally, did the growth of hospitalists affect continuity and ICU use? We chose ICU use as an outcome because there has been general concern about its overuse during end of life care31–34.
Methods
Data Source
This is a retrospective study of lung cancer patients identified from the linked Surveillance, Epidemiology and End Results (SEER)-Medicare database for the years 1992–200235. We included the original SEER registries, encompassing 14% of the United States population from the 11 geographic regions: the states of Connecticut, Hawaii, Utah, New Mexico and Iowa, and the metropolitan areas of San Francisco/Oakland, Los Angeles, and San Jose/Monterey (California), and the municipalities of Detroit, MI; Seattle, WA; and Atlanta, GA. For all incident cancers diagnosed in these areas, the SEER registries collect information on patient demographics, tumor characteristics, stage at diagnosis, date of diagnosis, therapy received within four months of diagnosis, and date and cause of death.
Through a collaborative project between the National Cancer Institute and the Centers for Medicare and Medicaid Services (CMS), entitlement information and claims data from the Medicare program were linked to the SEER data for cancer patients aged 65 and older. Medicare eligibility could be identified for 93% of SEER patients aged 65 and older36.
Data from multiple files were used for this study: 1) the Patient Entitlement and Diagnosis File (SEER registry data and Medicare entitlement information); 2) Medicare Provider Analysis and Review file (hospital inpatient and skilled nursing facility stays), 3) Outpatient Standard Analytic File (hospital outpatient services), and 4) 100% Physician/Supplier File (physician and other medical services); and 5) a Hospital File created by NCI with information on hospital characteristics from the CMS Provider of Service (POS) survey and the Healthcare Cost Report.
Study Cohort
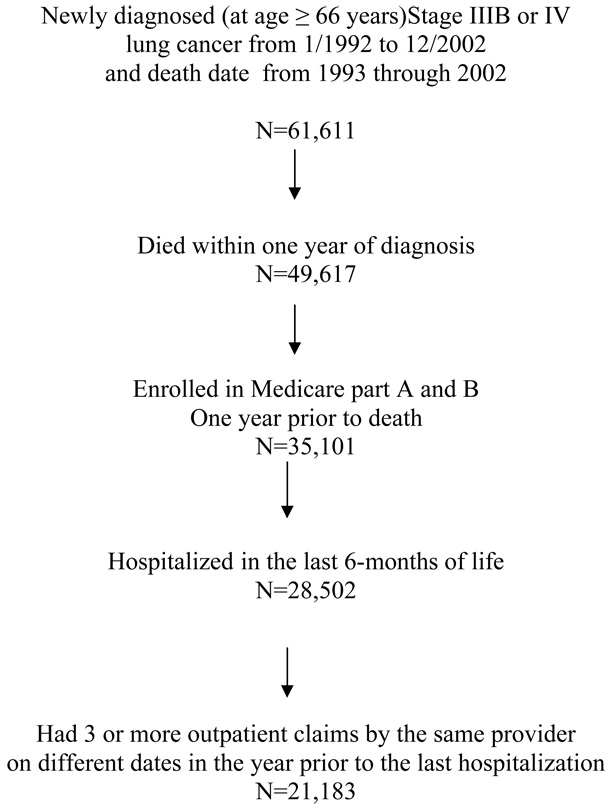
Eligible subjects were selected from the Patient Entitlement and Diagnosis File and included patients who were: 1) diagnosed with stage III B or stage IV lung cancer from 1992 – 2002, 2) 66 years or older at the time of diagnosis, 3) died within one year of diagnosis over the period 1993 – 2002, 4) enrolled in Medicare Parts A and B one year prior to death, 5) hospitalized in the last six months of life, and 6) had at least 3 or more visits to one provider in a year prior to the admitting date of the last hospitalization (Figure 1). We limit our analysis to the original SEER sites that have provided continuous data from 1992 to 2002. Individuals enrolled in an HMO at any time from date of diagnosis through date of death were excluded, because of concerns about completeness of information in the Medicare files of these patients.
Figure 1.
Establishment of study cohort who died within a year after diagnosis of advanced lung cancer, from 1992 to 2002, and who had a usual care provider
Measures
Information on patients’ socio-demographic characteristics was obtained from the SEER data: age (66–74, 75–84, ≥85), race (non-Hispanic white, Black, Hispanic, Other), gender, and marital status at the time of diagnosis (married, not married). Tumor stage, vital status, cause of death, and geographic region were also derived from SEER data. Residence was dichotomized into large metropolitan area vs. others. A large metropolitan area has an average population of over one million based on the 1990 census. Socio-economic status is based on whether the patient was eligible for state buy-in coverage provided by the Medicaid program for at least one month during the index year. Comorbidity was measured with a score developed by Klabunde et al. using all Medicare claims from the year prior to diagnosis37.
Establishment of Usual Care Provider (UCP)
HCFA Common Procedure Terminology (CPT) evaluation and management codes 99201 to 99205 (new patient) and 99221 to 99215 (established patient encounters) were used to establish outpatient visits. The individual providers were determined using the Unique Provider Identification Number (UPIN). Three or more visits to the same provider within a year prior to last hospitalization established the usual care providers for the patient. By this definition a patient could have more than one UCP. UCPs were classified as primary care physicians or others. For purposes of this study a primary care physician was a general practitioner, family physician, internist, or a geriatrician.
Definition of outpatient to inpatient continuity of care
An in-patient claim by the UCP during hospitalization established outpatient to inpatient continuity with a provider. Inpatient claims were identified using HCFA- CPT evaluation and management codes 99221 to 99223 (for initial hospital care), 99251 to 99255 (inpatient consultation) and 99231 to 99233 (for subsequent hospital follow-up).
Definition of a hospitalist
There is no provider code for a hospitalist physician in the administrative database. Therefore, we employed a functional definition of hospitalist originally proposed by Saint et al38: a physician with >50% of his or her total Medicare claims per year originating from inpatient CPT evaluation and management codes (99221–99223; 99231–99233, 99251–99255). We restricted our analyses to physicians with at least 10 inpatient claims per year and who had either internal medicine or geriatrics as their specialty.
The primary outcome was ICU use during the terminal hospitalization and was ascertained from inpatient hospital claims in the MEDPAR file. Patients with ICU room charges >0 or who had a CPT code for mechanical ventilation during hospitalization were considered as having “ICU use” during the admission.
Hospitals were dichotomized into teaching or non-teaching. Teaching hospitals were hospitals with a major medical school affiliation. Medical school affiliation was ascertained from the Provider of Services data in NCI’s Hospital File. For analyses of ICU use, patients hospitalized in hospitals that did not contain ICU beds (from the Healthcare Cost Report Information System) were deleted (1303 patients).
The study was approved by the Institutional Review Board of University of Texas Medical Branch, Galveston, TX.
Statistical Analysis
The likelihood ratio chi square statistic was used to compare rates of outpatient to inpatient continuity of care by subject characteristics. Changes in outpatient to inpatient continuity over time (year of diagnosis) were initially evaluated with the Cochran Armitage trend test. Multivariate logistic regression analysis was used to assess whether changes in ICU use over time varied by subject, outpatient to inpatient continuity of care and hospital characteristics. A p-value of <0.05 was considered significant. All statistical analyses were performed using SAS version 9.1 (SAS Institute Inc., Cary, NC).
Results
Figure 1 outlines the approach to identifying the study cohort. Of the 28,502 patients diagnosed with advanced lung cancer and hospitalized in the last 6-months of life, 21,183 (74.3%) had three or more visits to the same provider within the year prior to last hospitalization. We defined any provider who saw the patient on three or more different occasions in an outpatient setting as a usual care provider.
Table 1 describes the baseline patient characteristics of the study cohort. Of the patients with a usual care provider (n=21,183), 11,570 (54.6%) had outpatient to inpatient continuity; that is, they were seen during hospitalization by their usual care provider.
Table 1.
Baseline characteristics of the study cohort and percent with outpatient to inpatient continuity of care
| Variables | N | Percent with outpatient to inpatient continuity of care | p-value |
|---|---|---|---|
| Overall Cohort | 21,183 | 54.6 | |
| ICU use | |||
| Yes | 4,336 | 50.1 | |
| No | 16,847 | 55.7 | <0.0001 |
| Age at Diagnosis (in years) | |||
| 66–74 | 10,298 | 54.9 | |
| 75–84 | 8,879 | 54.6 | |
| ≥ 85 | 2006 | 52.8 | 0.203 |
| Gender | |||
| Male | 11,662 | 54.5 | |
| Female | 9,521 | 54.7 | 0.81 |
| Race (%) | |||
| Non-Hispanic White | 17,653 | 55.1 | |
| Black | 1,647 | 46.9 | |
| Hispanic | 674 | 53.1 | |
| Other | 1,209 | 59.6 | <0.0001 |
| Married | |||
| Yes | 11,265 | 56.1 | |
| Others | 9,918 | 52.9 | <0.0001 |
| SEER site (%) | |||
| Atlanta | 1,252 | 53.9 | |
| Connecticut | 2,772 | 59.1 | |
| Detroit | 4,258 | 50.2 | |
| Hawaii | 564 | 64.0 | |
| Iowa | 2,969 | 49.6 | |
| New Mexico | 711 | 45.0 | |
| Seattle | 2,350 | 50.8 | |
| Utah | 461 | 40.1 | |
| California* | 5,846 | 61.4 | <0.0001 |
| Low socioeconomic status | |||
| No | 17,867 | 55.3 | |
| Yes | 3,316 | 51.0 | <0.0001 |
| Comorbidity score | |||
| =0 | 10,063 | 54.0 | |
| =1 | 6,361 | 55.0 | |
| ≥2 | 4,759 | 55.4 | 0.23 |
| Cause of death | |||
| Lung cancer | 18,063 | 55.4 | |
| Others | 3,120 | 50.2 | <0.0001 |
| AJCC Stage | |||
| Stage IIIB | 6,775 | 56.0 | |
| Stage IV | 14,408 | 54.0 | 0.007 |
| Teaching Hospital | |||
| Yes | 5,868 | 49.5 | |
| No | 15,315 | 56.6 | <0.0001 |
| Residence | |||
| Large metropolitan area | 13,401 | 55.2 | |
| Others | 7,782 | 56.9 | <0.0001 |
California includes metropolitan areas of San Francisco/Oakland, Los Angeles and San Jose
Figure 2 shows the percent of patients receiving care from their usual care provider during their final hospitalization. Outpatient to inpatient continuity decreased from 60.1% in 1992 to 51.5% in 2002 (p-<0.0001). Over this same period, the number of patients who received care by a hospitalist increased from 8% to 16% (p<0.0001).
Figure 2.
Percent of patients with advanced lung cancer receiving care by their outpatient provider during their final hospitalization, from 1992 to 2002.*
*Analysis restricted to SEER sites that provided continuous data from 1992 to 2002 (n=21,183).
Cochran-Armitage trend test for 1992–2002: p<0.0001
Table 2 presents results of a multivariable analysis of factors associated with outpatient to inpatient continuity. Continuity declined over time. Patient characteristics associated with lower odds of continuity were male gender, black race, being unmarried, and having a low socioeconomic status. Treatment in an academic hospital and inpatient care provided by a hospitalist were also independently associated with a decreased odds of continuity of care.
Table 2.
Multivariable analysis of factors predicting whether a patient experiences continuity of care from the outpatient to the hospital setting
| Variables | Odds ratio (95% CI§) |
|---|---|
| Year of diagnosis (each increasing year) | 0.981 (0.972, 0.990) |
| Age at diagnosis (each increasing year) | 0.997 (0.933,1.002) |
| Gender | |
| Male | 1.0 |
| Female | 1.065 (1.004, 1.130) |
| Race | |
| Non-Hispanic White | 1.0 |
| Black | 0.774 (0.695, 0.861) |
| Hispanic | 0.984 (0.839, 1.153) |
| Others | 1.309 (1.154, 1.484) |
| Low socioeconomic status | |
| No | 1.0 |
| Yes | 0.830 (0.764, 0.902) |
| Teaching hospital | |
| No | 1.0 |
| Yes | 0.729 (0.685, 0.776) |
| Co-morbidity score | |
| 0 | 1.0 |
| 1 | 1. 053 (0.988, 1.123) |
| ≥2 | 1.102 (1.026, 1.183) |
| Married | |
| No | 1.0 |
| Yes | 1.122 (1.056, 1.192) |
| Hospital length of stay | 1.022 (1.018, 1.026) |
| Place of residence | |
| Non-large metropolitan area | 1.0 |
| Large metropolitan area | 1.115 (1.051, 1.182) |
| Seen hospitalist during hospitalization | |
| No | 1.0 |
| Yes | 0.935 (0.879, 0.996) |
Confidence interval
Of patients with outpatient to inpatient provider continuity, 18.7 % had an ICU stay during their last hospitalization, compared to 22.5 % of patients without provider continuity (p<0.0001). ICU use did not differ whether outpatient to inpatient continuity was by a primary care physician or a specialist, 19.1% vs. 18.5% respectively. Of those who received care by a hospitalist, 33.2% had an ICU stay during the last hospitalization, compared to 19.3% of those who received care by non-hospitalist physicians (p<0.0001).
Table 3 presents the results of a multivariable analysis of factors associated with ICU use in the final hospitalization among patients with advanced lung cancer. After controlling for other relevant factors, patients with outpatient to inpatient continuity had a 25.1% reduced odds of spending time in an ICU. Those seen by a hospitalist during the last hospitalization had 56.7% higher odds of ICU use. Odds of an ICU admission increased approximately 5.8% per year from 1993 to 2002. Higher odds of ICU use were also associated with being married, younger age, low socioeconomic status, higher comorbidity, Hispanic or other ethnicity, and living in large metropolitan areas.
Table 3.
Multivariable analyses of factors associated with ICU use during final hospitalization*
| Variables | Model 1 Odds ratio (95% CI±) | Model 2 Odds ratio (95% CI) |
|---|---|---|
| Outpatient to inpatient Continuity of care | ||
| No | 1.0 | 1.0 |
| Yes | 0.797 (0.745, 0.854) | 0.749 (0.698, 0.804) |
| Seen by a hospitalist‡ | ||
| No | 1.0 | |
| Yes | 1.567 (1.403,1.751) | |
| Year of diagnosis (each increasing year) | 1.058 (1.046, 1.071) | |
| Age at diagnosis(each increasing year) | 0.983 (0.977, 0.988) | |
| Gender | ||
| Male | 1.0 | |
| Female | 0.948 (0.879, 1.023) | |
| Race | ||
| Non-Hispanic White | 1.0 | |
| Black | 1.104 (0.972, 1.255) | |
| Hispanic | 1.289 (1.066, 1.560) | |
| Others | 1.264 (1.091, 1.463) | |
| Low socioeconomic status | ||
| No | 1.0 | |
| Yes | 1.146 (1.034, 1.271) | |
| Teaching hospital | ||
| No | 1.0 | |
| Yes | 0.959 (0.887, 1.038) | |
| Co-morbidity score | ||
| 0 | 1.0 | |
| 1 | 1.139 (1.048, 1.238) | |
| ≥2 | 1.468 (1.345, 1.603) | |
| Married | ||
| No | 1.0 | |
| Yes | 1.182 (1.093, 1.278) | |
| Hospital length of stay | 1.046 (1.041, 1.050) | |
| Place of residence | ||
| Non-large metropolitan area | 1.0 | |
| Large metropolitan area | 1.603 (1.482, 1.733) | |
Analyses restricted to the 19,880 patients hospitalized in hospitals that possessed ICU beds.
CI = Confidence interval
Discussion
For patients with advanced lung cancer, continuity of care across the outpatient to hospital setting declined during the 1990s. Continuity of care (being seen by a usual care provider during hospitalization) was associated with a lower chance of an ICU stay.
Other factors independently associated with a lower odds of outpatient to inpatient continuity of care include male gender, black race, lower socioeconomic status, being unmarried, care in a teaching hospital, and participation of a hospitalist in the care. The lower outpatient to inpatient continuity in teaching hospitals is consistent with the academic model of clinical practice, where rotating attending physicians are responsible for care of hospitalized patients. Our finding on the relationship of hospitalists to reduced continuity of care supports the concern expressed by others that the growth of the hospitalist movement may threaten continuity of care across transitions39. The other factors associated with low continuity of care are all commonly recognized to be risk factors for less than optimal medical care.
The decline in continuity of care may reflect the general trend in the United States primary care physician workforce. The number of internal medicine residents choosing primary care has declined from 54% in 1998 to 20% in 200640. The increasing pressure to improve productivity and efficiency further limits the role of primary care physicians to either "officist" or "hospitalist," jeopardizing continuity of care.
In addition to a substantial increase in end of life ICU care over time, odds of ICU care were independently associated with no outpatient to inpatient continuity, care by a hospitalist, younger age, Hispanic or other ethnicity, low socioeconomic status, higher comorbidity and living in a large metropolitan area.
Patients who received care by a hospitalist physician had higher odds of ICU stay during the last hospitalization. These findings should be interpreted in the context of our operational definition of a hospitalist physician. Moreover, we could not ascertain the timing of care provided by the hospitalist during the hospitalization in relation to ICU stay. It is possible that the hospitalist provided care to these patients while in the ICU or after an ICU stay.
Prior studies of hospitalists have shown reduced length of stay and reduced overall hospital costs and no difference or improvements in outcomes such as mortality and readmission rates41–43. A meta-analysis by Wachter and Goldman of 19 studies showed a 13.4% reduction in cost and 16.6% reduction in length of stay after initiating hospitalist programs24. Despite these improvements in efficiency, the expansion of the hospitalist movement is not without controversy. A major threat of the hospitalist model is the increasing discontinuity of care, from both outpatient-to-inpatient and inpatient-to-outpatient settings39.
Studies examining the effects of continuity of care have shown improved patient satisfaction, improved health outcomes and reduced health care costs3–9, 11, 12, 14–16, 44–47. There has been less work on the effect of continuity of care in end of life settings. Recent studies by Burge et al. showed that cancer patients with higher outpatient continuity with their primary care provider had fewer emergency room visits and were less likely to die in the hospital18, 19.
Individual patient preferences are often difficult to establish48–50. Physicians, nurses and family members differ significantly in their knowledge and understanding of a patient’s preferences for end-of-life care51. This situation is further complicated by misconceptions of the spiritual, religious and cultural needs of the patient and family members. Honoring patient preferences is critical in providing end-of-life care for terminally ill patients. Thus, familiarity with the patient should improve end-of-life choices.
In our study, the effect of outpatient to inpatient continuity of care on ICU use was similar whether the continuity of care was with a primary care physician or a specialist. This may reflect the patient population with advanced lung cancer, who may be closely followed by a specialist such as oncologist or pulmonologist.
The other factors that were associated with ICU use in our study, such as ethnicity, age, socioeconomic status and comorbidity, are consistent with numerous prior reports52–55.
Annually 540,000 Americans die using ICU services31. As the nation ages, the doubling of individuals older than 65 years of age by 2030 will require increasing demand on ICU services. Currently only 37% of ICU patients receive care from a critical care trained physician56. The current supply and projected number of trainees are not sufficient to meet the growing national need, unless better rationing and appropriate ICU use is promoted.
Our study has several limitations. First, while we found associations between lack of continuity of care and end of life ICU use, such associations found in observational data are not necessarily causal. Some unmeasured factors may be responsible for both discontinuity of care and ICU use. This study is limited to ICU use during final hospitalization for advanced lung cancer patients. Our study used administrative data that did not contain information on patient, family, or treating physician attitudes and preferences regarding end of life care. It is difficult for physicians to predict the life span of an individual with advanced lung cancer, even though the median survival of such patients has changed little over the span of the study. Cancer patients often choose treatments based on prognosis, which may be overestimated57. Only services billed by the physicians were included, and non-billable "social visits" by the usual care provider during the last hospitalization are not captured in the administrative data sets. However, this deficiency would likely decrease the estimate of association between continuity and ICU use.
We did not examine local health system characteristics that may have played a role in ICU use. It might be that the very factors associated with less continuity are also associated with less advance care planning or preferences for more aggressive care at the end of life. Patients with continuity may be more likely to have advance care planning. Future studies to examine the effect of continuity of care on advance care planning are needed.
These results reflect the Medicare population aged 66 and older with advanced lung cancer and may not be generalizable to other settings or populations. Subjects with HMO coverage were excluded from the study. A change in HMO enrollments during the study period might have affected the analysis of the time trend of outpatient to inpatient continuity of care.
In summary, outpatient to inpatient continuity of care declined during the 1990s and early 2000s, while care by hospitalists increased. Patients with terminal lung cancer who experienced outpatient-to-hospital continuity of care were less likely to spend time in the ICU prior to death. Efforts to improve outpatient-to-inpatient continuity of care in hospitalized patients may reduce end-of-life ICU use in terminally ill patients.
Acknowledgements
The authors thank Mark Siegel M.D., Terri Fried M.D., and Amber Barnato M.D., M.P.H., M.S. for their helpful comments on an earlier version of this manuscript and Sarah Toombs Smith Ph.D. for help in manuscript preparation.
This study used the linked SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the Applied Research Program, NCI; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database.
This work was supported by grants, (P30AG024832) and (P50 CA 105631) from the National Institutes of Health.
Footnotes
Conflict of interest Statement: None of the authors has a financial relationship with a commercial entity that has an interest in the content of this manuscript.
Reference List
- 1.Institue of Medicine: National Academy of Sciences. 1st ed. Washington, DC: 1996. Committee on the future of primary care. Primary Care. America's health in new era. [Google Scholar]
- 2.Saultz JW, Lochner J. Interpersonal continuity of care and care outcomes: a critical review. Ann Fam Med. 2005 March;3(2):159–166. doi: 10.1370/afm.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gill JM, Mainous AG., III The role of provider continuity in preventing hospitalizations. Arch Fam Med. 1998 July;7(4):352–357. doi: 10.1001/archfami.7.4.352. [DOI] [PubMed] [Google Scholar]
- 4.Gill JM, Mainous AG, III, Nsereko M. The effect of continuity of care on emergency department use. Arch Fam Med. 2000 April;9(4):333–338. doi: 10.1001/archfami.9.4.333. [DOI] [PubMed] [Google Scholar]
- 5.Gill JM, Saldarriaga A, Mainous AG, III, Unger D. Does continuity between prenatal and well-child care improve childhood immunizations? Fam Med. 2002 April;34(4):274–280. [PubMed] [Google Scholar]
- 6.Gill JM, Mainous AG, III, Diamond JJ, Lenhard MJ. Impact of provider continuity on quality of care for persons with diabetes mellitus. Ann Fam Med. 2003 September;1(3):162–170. doi: 10.1370/afm.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mainous AG, III, Gill JM. The importance of continuity of care in the likelihood of future hospitalization: is site of care equivalent to a primary clinician? Am J Public Health. 1998 October;88(10):1539–1541. doi: 10.2105/ajph.88.10.1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mainous AG, III, Baker R, Love MM, Gray DP, Gill JM. Continuity of care and trust in one's physician: evidence from primary care in the United States and the United Kingdom. Fam Med. 2001 January;33(1):22–27. [PubMed] [Google Scholar]
- 9.Mainous AG, III, Kern D, Hainer B, Kneuper-Hall R, Stephens J, Geesey ME. The relationship between continuity of care and trust with stage of cancer at diagnosis. Fam Med. 2004 January;36(1):35–39. [PubMed] [Google Scholar]
- 10.Mainous AG, III, Goodwin MA, Stange KC. Patient-physician shared experiences and value patients place on continuity of care. Ann Fam Med. 2004 September;2(5):452–454. doi: 10.1370/afm.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meredith LS, Sturm R, Camp P, Wells KB. Effects of cost-containment strategies within managed care on continuity of the relationship between patients with depression and their primary care providers. Med Care. 2001 October;39(10):1075–1085. doi: 10.1097/00005650-200110000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Petersen LA, Burstin HR, O'Neil AC, Orav EJ, Brennan TA. Nonurgent emergency department visits: the effect of having a regular doctor. Med Care. 1998 August;36(8):1249–1255. doi: 10.1097/00005650-199808000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Starfield BH, Simborg DW, Horn SD, Yourtee SA. Continuity and coordination vin primary care: their achievement and utility. Med Care. 1976 July;14(7):625–636. doi: 10.1097/00005650-197607000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Wasson JH, Sauvigne AE, Mogielnicki RP, et al. Continuity of outpatient medical care in elderly men. A randomized trial. JAMA. 1984 November 2;252(17):2413–2417. [PubMed] [Google Scholar]
- 15.Weiss GL, Ramsey CA. Regular source of primary medical care and patient satisfaction. QRB Qual Rev Bull. 1989 June;15(6):180–184. doi: 10.1016/s0097-5990(16)30289-5. [DOI] [PubMed] [Google Scholar]
- 16.Weiss LJ, Blustein J. Faithful patients: the effect of long-term physician-patient relationships on the costs and use of health care by older Americans. Am J Public Health. 1996 December;86(12):1742–1747. doi: 10.2105/ajph.86.12.1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith SD, Nicol KM, Devereux J, Cornbleet MA. Encounters with doctors: quantity and quality. Palliat Med. 1999 May;13(3):217–223. doi: 10.1191/026921699668267830. [DOI] [PubMed] [Google Scholar]
- 18.Burge F, Lawson B, Johnston G, Cummings I. Primary care continuity and location of death for those with cancer. J Palliat Med. 2003 December;6(6):911–918. doi: 10.1089/109662103322654794. [DOI] [PubMed] [Google Scholar]
- 19.Burge F, Lawson B, Johnston G. Family physician continuity of care and emergency department use in end-of-life cancer care. Med Care. 2003 August;41(8):992–1001. doi: 10.1097/00005650-200308000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Flocke SA, Stange KC, Zyzanski SJ. The impact of insurance type and forced discontinuity on the delivery of primary care. J Fam Pract. 1997 August;45(2):129–135. [PubMed] [Google Scholar]
- 21.Kahana E, Strange KC, Meehan R, Raff L. Forced disruption in continuity of primary care: the patients' prespective. Social Focus. 1997;30:177–187. [Google Scholar]
- 22.Kikano GE, Flocke SA, Gotler RS, Stange KC. 'My insurance changed': the negative effects of forced discontinuity of care. Fam Pract Manag. 2000 November;7(10):44–45. [PubMed] [Google Scholar]
- 23.Wachter RM, Goldman L. The emerging role of "hospitalists" in the American health care system. N Engl J Med. 1996 August 15;335(7):514–517. doi: 10.1056/NEJM199608153350713. [DOI] [PubMed] [Google Scholar]
- 24.Wachter RM, Goldman L. The hospitalist movement 5 years later. JAMA. 2002 January 23;287(4):487–494. doi: 10.1001/jama.287.4.487. [DOI] [PubMed] [Google Scholar]
- 25.Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004 October 5;141(7):533–536. doi: 10.7326/0003-4819-141-7-200410050-00009. [DOI] [PubMed] [Google Scholar]
- 26.Coleman EA, Min SJ, Chomiak A, Kramer AM. Posthospital care transitions: patterns, complications, and risk identification. Health Serv Res. 2004 October;39(5):1449–1465. doi: 10.1111/j.1475-6773.2004.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moore C, Wisnivesky J, Williams S, McGinn T. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003 August;18(8):646–651. doi: 10.1046/j.1525-1497.2003.20722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van WC, Mamdani M, Fang J, Austin PC. Continuity of care and patient outcomes after hospital discharge. J Gen Intern Med. 2004 June;19(6):624–631. doi: 10.1111/j.1525-1497.2004.30082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van den BL, Deschepper R, Bilsen J, Van CV, Deliens L. Transitions between care settings at the end of life in belgium. JAMA. 2007 October 10;298(14):1638–1639. doi: 10.1001/jama.298.14.1638. [DOI] [PubMed] [Google Scholar]
- 30.Brody H. The best system in the world. Hastings Cent Rep. 1995:S18–S21. [PubMed] [Google Scholar]
- 31.Angus DC, Barnato AE, Linde-Zwirble WT, et al. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med. 2004 March;32(3):638–643. doi: 10.1097/01.ccm.0000114816.62331.08. [DOI] [PubMed] [Google Scholar]
- 32.Barnatox AE, McClellan MB, Kagay CR, Garber AM. Trends in inpatient treatment intensity among Medicare beneficiaries at the end of life. Health Serv Res. 2004 April;39(2):363–375. doi: 10.1111/j.1475-6773.2004.00232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Earle CC, Neville BA, Landrum MB, Ayanian JZ, Block SD, Weeks JC. Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol. 2004 January 15;22(2):315–321. doi: 10.1200/JCO.2004.08.136. [DOI] [PubMed] [Google Scholar]
- 34.Sharma G, Freeman J, Zhang D, Goodwin JS. Trends in end-of-life ICU use among older adults with advanced lung cancer. Chest. 2008 January;133(1):72–78. doi: 10.1378/chest.07-1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF. Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care. 2002 August;40(8 Suppl):IV–18. doi: 10.1097/01.MLR.0000020942.47004.03. [DOI] [PubMed] [Google Scholar]
- 36.Potosky AL, Riley GF, Lubitz JD, Mentnech RM, Kessler LG. Potential for cancer related health services research using a linked Medicare-tumor registry database. Med Care. 1993 August;31(8):732–748. [PubMed] [Google Scholar]
- 37.Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000 December;53(12):1258–1267. doi: 10.1016/s0895-4356(00)00256-0. [DOI] [PubMed] [Google Scholar]
- 38.Saint S, Christakis DA, Baldwin LM, Rosenblat R. Is Hospitalism New? An Analysis of Medicare Data from Washington State in 1994. Effective Clinical Practice. 2000;3:35–39. [PubMed] [Google Scholar]
- 39.Manian FA. Whither continuity of care? Engl J Med. 1999 April 29;340(17):1362–1363. doi: 10.1056/NEJM199904293401712. [DOI] [PubMed] [Google Scholar]
- 40.Bodenheimer T. Primary care--will it survive? N Engl J Med. 2006 August 31;355(9):861–864. doi: 10.1056/NEJMp068155. [DOI] [PubMed] [Google Scholar]
- 41.Davis KM, Koch KE, Harvey JK, Wilson R, Englert J, Gerard PD. Effects of hospitalists on cost, outcomes, and patient satisfaction in a rural health system. Am J Med. 2000 June 1;108(8):621–626. doi: 10.1016/s0002-9343(00)00362-4. [DOI] [PubMed] [Google Scholar]
- 42.Lindenauer PK, Rothberg MB, Pekow PS, Kenwood C, Benjamin EM, Auerbach AD. Outcomes of care by hospitalists, general internists, and family physicians. N Engl J Med. 2007 December 20;357(25):2589–2600. doi: 10.1056/NEJMsa067735. [DOI] [PubMed] [Google Scholar]
- 43.Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002 December 3;137(11):866–874. doi: 10.7326/0003-4819-137-11-200212030-00007. [DOI] [PubMed] [Google Scholar]
- 44.Christakis DA, Mell L, Koepsell TD, Zimmerman FJ, Connell FA. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics. 2001 March;107(3):524–529. doi: 10.1542/peds.107.3.524. [DOI] [PubMed] [Google Scholar]
- 45.Mainous AG, III, Koopman RJ, Gill JM, Baker R, Pearson WS. Relationship between continuity of care and diabetes control: evidence from the Third National Health and Nutrition Examination Survey. Am J Public Health. 2004 January;94(1):66–70. doi: 10.2105/ajph.94.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Parchman ML, Pugh JA, Noel PH, Larme AC. Continuity of care, self-management behaviors, and glucose control in patients with type 2 diabetes. Med Care. 2002 February;40(2):137–144. doi: 10.1097/00005650-200202000-00008. [DOI] [PubMed] [Google Scholar]
- 47.Strumberg JP, Schattner P. Personal doctoring. Its impact on continuity of care as measured by the comprehensiveness of care score. Aust Fam Physician. 2001;30(5):513–518. [PubMed] [Google Scholar]
- 48.The SUPPORT Principal Investigators. A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT) JAMA. 1995 November 22;274(20):1591–1598. [PubMed] [Google Scholar]
- 49.Fried TR, Bradley EH. What matters to seriously ill older persons making end-of-life treatment decisions? A qualitative study. J Palliat Med. 2003 April;6(2):237–244. doi: 10.1089/109662103764978489. [DOI] [PubMed] [Google Scholar]
- 50.Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002 April 4;346(14):1061–1066. doi: 10.1056/NEJMsa012528. [DOI] [PubMed] [Google Scholar]
- 51.Shalowitz DI, Garrett-Mayer E, Wendler D. The accuracy of surrogate decision makers: a systematic review. Arch Intern Med. 2006 March 13;166(5):493–497. doi: 10.1001/archinte.166.5.493. [DOI] [PubMed] [Google Scholar]
- 52.Barnato AE, Berhane Z, Weissfeld LA, Chang CC, Linde-Zwirble WT, Angus DC. Racial variation in end-of-life intensive care use: a race or hospital effect? Health Serv Res. 2006 December;41(6):2219–2237. doi: 10.1111/j.1475-6773.2006.00598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Degenholtz HB, Thomas SB, Miller MJ. Race and the intensive care unit: disparities and preferences for end-of-life care. Crit Care Med. 2003 May;31(5 Suppl):S373–S378. doi: 10.1097/01.CCM.0000065121.62144.0D. [DOI] [PubMed] [Google Scholar]
- 54.Gornick ME, Eggers PW, Reilly TW, et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. N Engl J Med. 1996 September 12;335(11):791–799. doi: 10.1056/NEJM199609123351106. [DOI] [PubMed] [Google Scholar]
- 55.Virnig BA, Kind S, McBean M, Fisher E. Geographic variation in hospice use prior to death. J Am Geriatr Soc. 2000 September;48(9):1117–1125. doi: 10.1111/j.1532-5415.2000.tb04789.x. [DOI] [PubMed] [Google Scholar]
- 56.Kelley MA, Angus D, Chalfin DB, et al. The critical care crisis in the United States: a report from the profession. Chest. 2004 April;125(4):1514–1517. doi: 10.1378/chest.125.4.1514. [DOI] [PubMed] [Google Scholar]
- 57.Lamont EB, Christakis NA. Prognostic disclosure to patients with cancer near the end of life. Ann Intern Med. 2001 June 19;134(12):1096–1105. doi: 10.7326/0003-4819-134-12-200106190-00009. [DOI] [PubMed] [Google Scholar]