Abstract
Aims
To examine whether need–service matching in addiction treatment leads to improvements in drug use, and whether treatment duration mediates those improvements.
Design, participants, measurements
This analysis utilizes prospective data from a US cohort of addiction treatment patients who reported service needs beyond core rehabilitative services (n = 3103). ‘Drug use improvement’ is the difference between the patient’s peak drug use frequency (in days per month) in the year before intake and in the year after treatment. Overall and primary use of the major illicit drugs (heroin, powder or crack cocaine and marijuana) are considered separately. ‘Need–service match’ means that a patient rated a service as important at intake and reported its receipt during treatment. ‘Percentage of needs matched’ indicates the proportion of five service domains (medical, mental health, family, vocational and housing) so matched.
Findings
In mixed regression models controlling for multiple factors, a greater percentage of needs matched tended to improve primary (β = 0.028, P = 0.09) and overall (β = 0.049, P = 0.05) drug use in the follow-up year. Exclusion of treatment duration as a covariate doubled the magnitude of these coefficients. The benefits of matching were concentrated among the half of patients reporting needs in four to five rather than one to three domains, and were strongest among patients in long-term residential facilities. Addressing vocational and housing needs exerted the greatest effects.
Conclusions
Matching comprehensive services to needs is a useful addiction treatment practice, especially for high-need patients. Treatment duration might partially mediate its effect.
Keywords: Health services needs and demand, housing, mental health services, needs assessment, substance abuse treatment centers, vocational rehabilitation
INTRODUCTION
Drug abuse and dependence produce adverse effects in multiple areas of life (O’Brien & McLellan 1996; Gerstein et al. 1997). These effects include family distress, unemployment, illness and homelessness. Although well-being is important of itself, problems in these areas are especially important to persons with substance problems because they increase the probability of relapse (McLellan & Weisner 1996). Family conflict, chronic medical illness, pain and affective symptoms can trigger relapse (Daley 1988). Substantial evidence suggests that drug abuse treatment effectively reduces substance use and improves outcomes in these areas (Gerstein et al. 1997; Hubbard et al. 1997). Observed differences in patient outcomes across different programs have driven the search to identify the effective components of addiction treatment. The delivery of comprehensive services to address patients’ needs is considered one potentially effective component (Gerstein & Harwood 1990).
Many substance abuse treatment programs and their staffs expend considerable resources and energy to address patients’ needs for comprehensive services. The research evidence for this practice is mixed. Some studies support the idea that delivering services to match patients’ problems improves treatment retention and outcomes (Ball & Ross 1991; Hubbard et al. 1997; Hser et al. 1999a). An investigation that randomized 94 patients to problem–service matching versus standard services found that those who received three or more service sessions matched to mental health, family or employment problems had better treatment completion and post-treatment outcomes (McLellan et al. 1997). Other investigations have had difficulty detecting similar effects (Joe, Simpson & Hubbard 1991; Fiorentine 1998).
The current study evaluates whether matching comprehensive services to patients’ needs improved drug use at follow-up in a US national sample of addiction treatment programs. It further examines whether treatment retention mediates any effect of such matching on outcomes.
Conceptual Framework
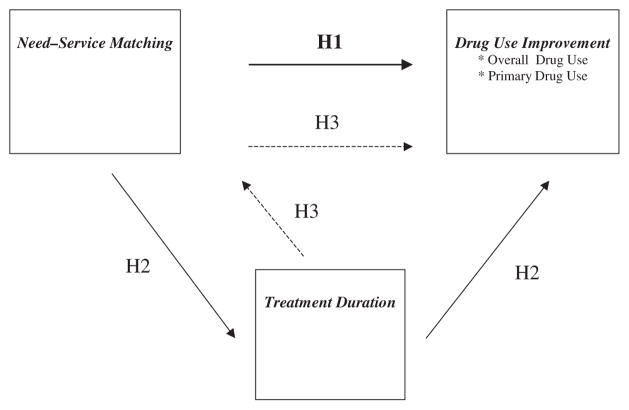
The conceptual framework posits that matching services to needs influences subsequent drug use both directly and indirectly, the latter through effects on treatment duration (Fig. 1). Domains of service need (e.g. medical, mental health, family, vocational and housing) represent problems that might induce relapse (Daley 1988). Matching services to address these needs might ameliorate these problems and directly decrease relapse risk. Thus, hypothesis 1 states:
Figure 1.
Conceptual framework showing the direct (H1) effect of need–service matching on improvements in drug use, and indirect effects in which treatment duration (H2) and need–service matching (H3) serve as mediators
H1: Matching comprehensive services to patients’ needs in treatment will directly improve drug use at follow-up.
However, even if addressing a particular service need does not decrease relapse risk directly, it might increase the patient’s perception of program responsiveness, and augment retention (Broome, Flynn & Simpson 1999). Thus, treatment retention might mediate the possible effect of need–service matching on drug use outcomes. Several studies support the important effect of longer treatment duration on drug-related outcomes (Simpson 1981; Simpson, Joe & Brown 1997; Zhang, Friedmann & Gerstein 2003). In support of a mediating effect of treatment duration, McLellan et al. (1993) found that problem–service-matched patients had significantly longer duration of treatment than patients without service matching and used fewer drugs after treatment. Thus, the second hypothesis is:
H2: Treatment duration mediates the relationship between need–service matching with respect to drug use improvement at follow-up.
The converse relationship is also plausible. That is, need–service matching could mediate the relationship between treatment duration and drug use improvement. In this circumstance, the positive effect of longer treatment duration on drug use improvement might derive in part from its allowing the program greater opportunity to address the patient’s service needs. Although we believe it likely that need–service matches are made early in treatment or not at all, the current dataset does not indicate the timing of service delivery during treatment. However, even in the absence of information about timing, the current analysis can still explore the converse hypothesis:
H3: Need–service matching mediates the relationship between treatment duration and drug use improvement.
METHOD
The National Treatment Improvement Evaluation Study (NTIES) was a multi-site longitudinal survey of administrative and clinical elements of substance abuse treatment conducted between 1992 and 1997. During the early 1990s, the US Government’s Center for Substance Abuse Treatment (CSAT) had given demonstration grants to a majority of states to distribute among approximately 800 treatment programs in order to expand services. NTIES evaluated the implementation and effectiveness of these demonstration grants.
After approval from institutional review boards at the University of Chicago and other involved institutions, the National Opinion Research Center (NORC) and the Research Triangle Institute surveyed patients in grantee programs. NTIES research staff completed intake, treatment discharge and follow-up data collection between July 1993 and November 1995. Patient interviews collected information regarding the patient’s ratings of service importance, receipt of services, drug abuse history and other characteristics. A total of 6593 patients completed intake interviews. Within 3 weeks of the last program contact—whether discharge was voluntary or involuntary, with or against advice—5274 patients (80.0%) completed treatment discharge interviews and 5388 (81.7%) completed 1 year follow-up interviews. Although targeted as a 12 month follow-up, abbreviation of the period at the tail end of the study compressed follow-up to a median of 11 months. Of the entire intake cohort, 93.1% completed either treatment discharge or follow-up interviews. Respondents were similar to the non-respondents in most characteristics except that respondents remained in treatment for a significantly longer duration than did non-respondents.
Subjects enrolled before the midpoint of the study were asked to provide a urine specimen immediately after the interview. The refusal rate was less than 1% and an additional 3% could not be completed for logistical reasons. Interviewers did not directly observe specimen collection, but the protocol did include measurement of irregularities (e.g. unusual temperature, color or other activity); such irregularities were noted in only 3% of completed samples.
Survey instruments for NTIES were constructed carefully (Gerstein et al. 1997; Gerstein & Johnson 2000). The development process involved a thorough review of existing literature, and an iterative process of pre-test and revision. Many items were taken directly from standard instruments or previous drug treatment outcomes studies. The questionnaire development team included experts in substance abuse treatment, mental health and cognitive interviewing. They performed focus groups and cognitive interviews to assure the comprehension and administrative feasibility of items. To minimize recall decay and telescoping, drug use items were designed to elicit use during clearly defined time periods anchored around the NTIES treatment episode.
Only the 4526 patients who completed all three interviews are included in these analyses. After removal of participants in the correctional modality, the sample includes 3255 patients from 63 treatment units as follows: 410 patients in eight methadone programs; 1282 in 31 out-patient non-methadone units; 578 in five short-term residential programs; and 985 patients in 19 long-term residential facilities. Most of the NTIES sample was African American, age 40 or younger, and approximately one third was female. Few were married. A slim majority had graduated high school or had health insurance (primarily Medicaid). A minority (20%) was legally employed. In the year before treatment, the average patient had received approximately $6214 from legal sources (wages, entitlements, child support, alimony, etc.). Subjects also had extensive drug use careers before the NTIES treatment episode. An average of 10 years had separated the patient’s first use of the primary drug from treatment intake. A slim majority (51%) had previous drug treatment, with an average of three previous treatment episodes among those with previous treatment. The 3103 patients (95%) who reported a need for at least one of the services of interest constituted the final analytic sample.
Dependent variables
Prior studies have measured drug use outcomes in a variety of ways, including strict abstinence (Hser et al. 1999b), drug-type-specific improvement (Gerstein & Zhang 2001) and composite improvement scores (Friedmann et al. 2003a). Following Zhang et al. (2003), this study examines baseline to follow-up change in drug use: improvement in primary drug use and improvement in overall drug use. These ordinal measures are sensitive to specific levels of frequency of use, capture the poly-drug character of contemporary substance abuse and attend to the relative importance that patients attach to different drugs. Improvement is measured as a change in the number of drug-using days during the month of most frequent use in each of two periods: the year before the baseline interview and the year since treatment, as approximated by the interval between the last day of the NTIES treatment episode and the follow-up interview (which took place an average of 11 months later).
Primary drug use improvement
We identified a patient’s primary drug(s) through response(s) to the question: ‘what is the drug or drug combination that made you come to treatment this time?’. Offered a list of 13 drug types, 99% of patients named marijuana, powder cocaine, crack cocaine, heroin or alcohol as a primary drug. Of these respondents, 81% named one or more of these four types as a primary drug and 20% indicated two or more of these four types. For the purposes of this paper, we focus on the four most commonly cited illicit drugs. Following a procedure developed by the Drug Abuse Treatment Outcome Study (DATOS; Hubbard et al. 1997), the questionnaire first asked respondents whether they had used each specified drug five times or more during the reference period. Respondents who responded ‘yes’ were subsequently asked to indicate the category of the highest level of drug use during the reference year as more than 20 days/month, 6–20 days, 1–5 days or no days. The respective frequencies might be characterized in clinically meaningful terms as heavy (daily or near-daily); recurrent or binge; sporadic; and abstinent. Drug use improvement is the difference in peak use between the baseline and follow-up periods (Zhang et al. 2003). An improvement score for one drug could thus range from +3 (from heavy use before to little or no use after) to −3 (from little or no use before to heavy use after). The primary drug use improvement measure sums improvement scores only for the primary drug(s) indicated at the baseline interview. Primary drug use improvement ranges from −5 to 9 and has a mean of 1.3 (95% CI: ±0.03). Positive values indicate reduced drug use from treatment intake to follow-up.
Correlative validity was examined among the 1651 subjects with urine toxicology at follow-up. The urine toxicology panel indicates the crude presence versus absence of drug metabolites at a threshold level, indicating opiate or cocaine use or the smoking of a single marijuana cigarette in the previous 2–3 days, and daily marijuana use during the previous 10 days (Wolff et al. 1999). Acknowledging differences in measurement, these analyses of correlative validity confirm that urine toxicology results have an inverse relationship with the improvement scores. For example, the primary drug use improvement score is significantly greater in subjects with negative urine for their primary drug(s) than among those with positive urine toxicology for their primary drug(s) (respective mean score, 1.45 versus 1.16) (P < 0.001). Moreover, subjects with negative urine tests for illicit drugs have mean primary drug improvement scores of 1.95, compared with 0.67 among those whose urine tests positive for drug metabolites (P < 0.0001). The respective percentages of patients whose urine tested positive for marijuana, heroin or cocaine (crack or powder) were 6%, 6% and 15% for the specified drug among patients who report using less than five times during the follow-up period, compared with 43%, 69% and 59% among those who report use five or more times (P < 0.0001). Despite differing time frames and levels of measurement, self-reported primary drug use in the follow-up year is correlated moderately with the urine toxicology results: the Spearman correlation coefficients for marijuana, heroin and cocaine are 0.50, 0.61 and 0.37, respectively.
Overall drug use improvement
The overall drug use improvement measure sums improvement scores across the four most prevalent illicit drugs: heroin, powder or crack cocaine and marijuana (Zhang et al. 2003). While overall and primary scores are well correlated (correlation table available from the authors on request), drug substitution is common. Positive scores indicate reduced overall substance use. Overall drug use improvement scores range from −11 to 12 and have a mean of 2.14 (95% CI: ±0.05) and a median between 1 and 2. In terms of correlative validity with urine toxicology results at follow-up, overall drug improvement scores are significantly higher among subjects with negative urines than among those whose urine tests positive for any drug metabolite (mean scores of 2.44 and 1.72, respectively; P < 0.0001). Urine toxicology tests are positive for any metabolite among 51% of subjects with overall improvement scores of less than 0 (i.e. a net increase in drug use), 37% of subjects with improvement scores between 0 and 3, and 28% of subjects with overall improvement scores of 4 or more.
Independent variables
Domain-specific need–service matching
This includes individual need–service matching for five domains: medical services, mental health services, family services, vocational skills counseling and housing services. We calculate five measures of matched need for services, one for each domain. Need in each service domain is measured from an item in the intake interview that asked patients: ‘how important is help with [the problem]? Would you say not at all important, somewhat important or very important?’. Responses were clustered primarily at the extremes (‘not at all’ and ‘very’). As in prior studies (Joe et al. 1991; Hser et al. 1999a), the patient is considered to need the specific service in domains for which help was rated ‘somewhat or very important’. We did examine an alternative cut-point at the level of ‘very important’; this specification did not change the results. The treatment discharge questionnaire asked patients whether they received the service; other work has validated patient report of service delivery (Ritter et al. 2001). For patients who needed a particular service, if the patient reports having received the service during treatment then the need for that service is considered matched. Patients with needs matched are coded as 1, otherwise 0.
Percentage of needs matched
The primary explanatory variable, percentage of needs matched assesses the breadth of services matched to address patients’ needs. Ranging from 0 to 100%, the percentage of needs matched is the unweighted total number of needs matched over the total number of patients’ self-reported needs multiplied by 100. Approximately 4.7% of the sample (152 patients) reported no needs and are excluded from calculations using this measure. This variable does assume equivalency of needs—for example, a patient with 50% of their needs matched could have either two reported needs with one matched, or four needs with two matched. While matching some needs might be more important than others, this specification is appropriate for evaluating the cumulative impact of need–service matching on substance abuse treatment outcomes (Hser et al. 1999a). Persons with high needs might benefit more from matched services, thus we dichotomized a high-needs group (4–5 domains, n = 1575) from a low-needs group (1–3 domains, n = 1528).
Treatment duration
This is defined in this analysis as the number of weeks elapsed between the first and last day of treatment received. It is a continuous variable ranging from 0 to 50.
Other patient-level variables
Past-year peak drug use
We used the peak frequency of drug use in the 12 months before the baseline interview as a predictor of drug use improvement. This covariate adjusts for three possible effects. First, the greater the peak level of drug use in the year prior to treatment, the greater the room for improvement. Therefore, prior-year peak use as a covariate adjusts for floor or ceiling effects. Second, prior-year peak use as a covariate captures any tendency to regress toward the mean. Finally, peak use may be a marker for the severity of pre-treatment drug use.
Reduction from past-year peak drug use
A second drug use variable incorporates the reduction in the frequency of drug use from the past-year peak period to the month immediately preceding the baseline interview (Zhang et al. 2003). If the past-year peak and past-month frequencies are equal, we code reduction from past-year peak use as 0, otherwise 1. A value of 1 indicates that the patient reduced his or her drug use just before treatment entry relative to the peak level in the year before treatment. The NTIES baseline interview was required to take place within 3 weeks of the first out-patient visit or overnight stay; generally, it occurred within a few days of initial treatment in residential and methadone programs and within a week among out-patients. Therefore, the ‘past 30 days’ indexed by the peak reduction measure covers primarily the immediate pre-treatment period, but to a lesser extent it includes short periods immediately following treatment initiation. In either event, inclusion of this marker of reduction from past-year peak among the covariates identifies how much improvement may be attributed to treatment retention beyond that initial week or two of treatment. To the extent that motivation is present on entry into treatment, this measure of reduction from past-year peak reflects ‘cutting down’ before or early in treatment, a behavioral marker of preparation or ‘realized motivation’.
Gender
An important covariant of needs, gender is coded 1 if the patient is female and 0 if the patient is male. Other patient-level variables included health insurance, self-reported treatment motivation, race and age. Based on their lack of effect, they have been omitted for parsimony.
Program-level variables
Treatment modality
This variable is a marker for treatment approaches and populations that might influence outcomes. The sample for this analysis contains short-term residential, long-term residential, out-patient methadone and out-patient non-methadone modalities. Modality is dummy-coded with out-patient non-methadone as the referent category. All multivariate models control for modality. Other program-level variables included the program’s staff-to-patient ratio and number of active patients; they exerted no effect and are omitted for parsimony.
Statistical methods
Primary analyses examine whether need–service matching in addiction treatment leads to drug use improvement (H1), and whether treatment duration mediates those effects (H2) or vice-versa (H3). In order to prove mediation, four conditions must be met: (1) variation in levels of the independent variable must be correlated with variation in the mediator; (2) variation in the mediator must be correlated with variation in the dependent variable; (3) controlling for the mediator substantially reduces or eliminates the relationship between the independent and dependent variables; and (4) the independent variable must temporally precede the mediator, which must precede the dependent variable (Baron & Kenny 1986; Kraemer et al. 2002).
To evaluate conditions (1) and (2), Spearman correlation coefficients test bivariate relationships among the key variables. To evaluate condition (3)—whether treatment duration mediates the relationship between percentage of matched needs and drug use improvement—we compare multivariate regression model specifications that serially exclude and include treatment duration and percentage of matched needs. Given positive associations among needs-service matching, treatment duration and drug use improvement [conditions (1) and (2)], substantial diminution in the positive association between need–service matching and drug use improvement when treatment duration is included in the model is partial evidence of a mediating effect of treatment duration (Baron & Kenny 1986). These analyses use multivariate mixed models that account for the influence of patients nested within programs in error calculations (Littell et al. 1996), and adjust for multiple patient- and program-level factors. Subjects in these models are restricted to those who reported one or more service needs. We use the multivariate delta method (Sobel 1982) to estimate the standard error of mediated effects because it has been shown to perform well in simulations for testing mediation in multi-level models (Krull & MacKinnon 1999). We also estimate the effects of need–service matching separately for the low-needs and high-needs groups, and examine the interaction of needservice matching with treatment modality.
To evaluate the direct effect of domain-specific need–service matching on drug use improvement, secondary analyses generate five separate multivariate mixed models. Subjects in these five models are restricted to those who reported needing the particular service.
RESULTS
Most subjects (n = 3103) reported needing at least one service; on average, each of them reported a need for 3.22 services. Approximately two thirds of subjects considered each of the five kinds of services important, with a narrow range from 71% needing family services to 61% needing vocational services. Matching by service domain was far more variable (Table 1). On average, about one third of all service needs were matched (1.11 matched per person, with 2.11 needs unmet). In general, respondents who stated they did not need services usually did not receive them, but there were many exceptions.
Table 1.
Descriptions and distributions of service need, receipt and need–service matching variables (n and percentage of 3255).
| Service neededa |
Service not neededa |
||||
|---|---|---|---|---|---|
| Domain of service need | Description | Service received (need matched)c | Service not received | Service receiveda,b | Service not receiveda,b |
| Medical | Treatment for any medical problems | 1332 40.9% |
736 22.6% |
683 21.0% |
504 15.5% |
| Mental health | Treatment for emotions, nerves or mental health problems | 683 21.0% |
1382 42.3% |
159 4.9% |
1031 31.7% |
| Family | Treatment or counseling for family problems (other than problems raising children) | 830 25.5% |
1478 45.4% |
246 7.6% |
700 21.5% |
| Vocational | Counseling for employment problems, such as problems finding or keeping a job, or getting along with co-workers | 327 10.0% |
1670 51.4% |
129 4.0% |
1127 34.6% |
| Housing | Help with housing problems such as finding or keeping a place to live | 434 13.3% |
1616 49.4% |
85 2.6% |
1129 34.7% |
| Mean number of services | 1.11 | 2.11 | 0.40 | 1.38 | |
Service need based on patient rating of service as ‘somewhat or very important’ or not in baseline interview.
Service receipt based on self-reported service receipt during the treatment episode in treatment discharge interview.
Need and service matched, based on both service need and service receipt during the treatment episode.
In bivariate correlations, percentage of needs matched was associated with overall (β = 0.054; P < 0.01) and primary (β = 0.045; P < 0.05) drug use improvement (Table 2). As in our previous work (Zhang et al. 2003), treatment duration, past-year peak drug use and reduction from past-year peak also predicted drug use improvement. Women also demonstrated greater improvements in drug use in bivariate analyses. In terms of treatment modality, non-methadone out-patient patients demonstrated the least improvement in drug use, while long-term residential patients showed the most improvement.
Table 2.
Spearman correlations between key dependent and independent variables.
| Spearman correlation coefficients |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) |
| (1) Overall drug use improvement | 1.000 | 0.782c | 0.054b | 0.040a | 0.693c | 0.043a | 0.053b | 0.028 | −0.228c | 0.042a | 0.187c |
| (2) Primary drug use improvement | 1.000 | 0.045a | 0.062c | 0.534c | 0.078c | 0.074c | 0.075c | −0.232c | 0.015 | 0.181c | |
| (3) Percent of needs service matched | 1.000 | 0.176c | −0.030 | 0.086c | 0.056b | −0.115c | −0.053b | −0.033 | 0.166c | ||
| (4) Treatment duration, per week | 1.000 | −0.048b | −0.033 | −0.024 | 0.264c | 0.184c | −0.531c | 0.055b | |||
| (5) Past-year peak level of drug use | 1.000 | −0.047b | 0.020 | 0.254c | −0.360c | 0.060c | 0.149c | ||||
| (6) Reduction from past-year peak use | 1.000 | 0.018 | −0.307c | 0.131c | 0.053b | 0.038a | |||||
| (7) Female gender | 1.000 | −0.019 | −0.113c | −0.016 | 0.148c | ||||||
| (8) Methadone modality | 1.000 | d | d | d | |||||||
| (9) Non-methadone out-patient modality | 1.000 | d | d | ||||||||
| (10) Short-term residential modality | 1.000 | d | |||||||||
| (11) Long-term residential modality | 1.000 | ||||||||||
P < 0.05;
P < 0.01;
P < 0.001;
dummy variable, correlations not meaningful.
Multivariate effect of matched need for services
Matching vocational counseling and housing services to needs in those domains significantly improved overall and primary drug use (Table 3). Matching medical services to need showed a strong trend toward improving overall (P = 0.057) and primary (P = 0.076) drug use. Family services matching tended to improve overall drug use (P = 0.056) and significantly improved primary drug use. Of the five service domains examined, only mental health services matching did not appear to improve drug use.
Table 3.
Effect of matching services to needs on overall and primary drug use improvement among patients with service need.
| Parameter estimate (standard error)a |
||
|---|---|---|
| Domain of service need | Overall drug use improvement | Primary drug use improvement |
| Medical | 0.174 (0.091) [P = 0.057] | 0.125 (0.070) [P = 0.076] |
| Mental health | 0.134 (0.088) | 0.000 (0.067) |
| Family | 0.162 (0.084) [P = 0.056] | 0.140 (0.065)b |
| Vocational | 0.427 (0.121)d | 0.284 (0.092)c |
| Housing | 0.472 (0.105)d | 0.233 (0.081)c |
From multivariate mixed model regressions controlling for past-year peak level of drug use, reduction from past-year peak in the month prior to treatment entry, gender and program treatment modality and clustering patients within programs.
P < 0.05;
P < 0.01;
P < 0.001.
Multivariate effects of percentage of needs matched and treatment duration
Multivariate models examined both the direct influence of percentage of needs service matched on drug use improvement and the role of treatment duration as a potential mediator (Table 4). After controlling for treatment duration and other covariates, the positive relationships between the percentage of needs matched and both overall (P < 0.05) and primary (P = 0.09) improvement support the hypothesis that need–service matching in treatment directly improves drug use at follow-up (H1). Two additional observations suggest that treatment duration might partially mediate the influence of need–service matching on drug use improvement (H2): (1) treatment duration significantly predicts drug use improvement in all models; and (2) the coefficient for need–service matching diminishes by half with the inclusion of treatment duration in the full models. This partial mediating effect was significant for both overall (Z = 6.52, P < 0.0001) and primary drug use improvement (Z = 5.95, P < 0.0001). We could detect no similar evidence for need–service matching as a mediator of the effect of treatment duration on drug use improvement (H3).
Table 4.
Effect of need–service matching and treatment duration on overall and primary drug use improvement.a
| Parameter estimate (standard error) |
||||||
|---|---|---|---|---|---|---|
| Overall drug use improvement |
Primary drug use improvement |
|||||
| Full model | Without treatment duration | Without needs service-matched | Full model | Without treatment duration | Without needs service-matched | |
| Percent of needs service-matched | 0.049 (0.021)b | 0.086 (0.021)d | – | 0.028 (0.016) [P = 0.09] | 0.050 (0.016)c | – |
| Treatment duration, per week | 0.024 (0.003)d | – | 0.025 (0.003)d | 0.014 (0.002)d | – | 0.015 (0.002)d |
| Past-year peak level of drug use | 0.452 (0.008)d | 0.448 (0.008)d | 0.451 (0.008)d | 0.204 (0.006)d | 0.202 (0.006)d | 0.203 (0.006)d |
| Reduction from past-year peak use | 0.247 (0.073)d | 0.276 (0.074)d | 0.267 (0.070)d | 0.373 (0.056)d | 0.393 (0.056)d | 0.374 (0.054)d |
| Female gender | 0.092 (0.077) | 0.094 (0.078) | 0.092 (0.075) | 0.093 (0.059) | 0.092 (0.060) | 0.102 (0.058) |
| Program treatment modality | ||||||
| Methadone | −1.363 (0.205)d | −1.173 (0.225)d | −1.375 (0.202)d | −0.167 (0.152) | −0.054 (0.163) | −0.175 (0.149) |
| Non-methadone out-patient | Referent | Referent | Referent | Referent | Referent | Referent |
| Short-term residential | 0.402 (0.214) | 0.011 (0.234) | 0.427 (0.210)b | 0.344 (0.156)b | 0.111 (0.168) | 0.363 (0.154)b |
| Long-term residential | 0.166 (0.148) | 0.099 (0.163) | 0.192 (0.145) | 0.320 (0.110)c | 0.280 (0.118)b | 0.343 (0.107)c |
Among 3103 patients with any service need. From multivariate mixed model regressions clustering patients within programs.
P < 0.05;
P < 0.01;
P < 0.001.
The statistical significance of the matching effect is near the conventional threshold for a two-tailed test. In view of the large sample size, this finding indicates relatively high variability. Although the estimated effect may seem small, the following calculations based on the parameter estimates provide some context. The average patient expressed need for 3.22 services, and 1.11 of these needs were matched, a mean need–service match rate of about 34%. According to the coefficients for need–service matching (β = 0.049 per percentage point change) and for treatment duration (β = 0.024 per week), a modest 6% increase in the rate of need–service matching (to 40%) would have a similar effect on overall drug use improvement as a 12 week increase in average treatment duration, all other things being equal.
Effects of need–service matching in different treatment modalities
In a series of models (available from the authors on request), interaction terms examined whether need–service matching has different effects on outcomes in the different modalities. The interaction term coefficients were significant (P < 0.05) and opposite in direction for overall drug use improvement in methadone (β = −0.14) and for primary drug use improvement in long-term residential programs (β = 0.06). The pattern of coefficients across the models suggested that the effects of need–service matching ranged from weakest to strongest in methadone, non-methadone out-patient, short-term residential and long-term residential programs.
Effects of need–service matching in patients with high and low needs
In another series of models available on request, the authors estimated the multivariate models represented in Table 4 separately for patients with high needs (needs at intake in four to five domains) and low needs (needs in one to three domains). The magnitudes of the ‘percentage of needs matched’ coefficients were greater in the high-needs group than in the complete sample (for overall improvement, high-needs group β = 0.083, P < 0.05 versus β = 0.049, P < 0.05 in Table 4; for primary improvement, high-needs group β = 0.080, P < 0.01 versus 0.028, P = 0.09 in Table 4). In addition, for both overall and primary drug use improvement in the high-needs group, as in Table 4, the results supported the mediating effect of treatment duration (H2) and did not support the competing hypothesis that needs-matching mediates duration (H3). In the low-needs group, the needs-matched coefficients were of lower magnitude than in Table 4 and were not significant.
DISCUSSION
Among patients who reported needs in all or nearly all of the five major service domains, matching comprehensive services to needs during treatment improved their drug use outcomes in the year following treatment relative to the year before. Need–service matching appears to have both a direct effect on improvements in drug use and an indirect effect mediated by treatment duration. Treatment duration might mediate the effect of needs matching on drug use improvement because meeting needs might cause patients to stay longer in treatment. Hser et al. (1999a) found a small but significant relationship between the proportion of addressed needs and treatment retention in a treatment population. Alternatively, patients whose needs were met over a longer duration might have gained greater benefit from the matched services, a possibility not captured by our dichotomous measure (matched or not).
The significant diminution by treatment duration of the effect of need–service matching is necessary but insufficient to prove mediation (Baron & Kenny 1986; Kraemer et al. 2002). Temporal precedence of need–service matching vis-à-vis treatment duration is also required (Kraemer et al. 2002). This study cannot establish temporal precedence because NTIES did not directly assess the timing of needs assessment and service delivery during the treatment episode. Although we believe it highly likely that needs are assessed at intake and service matches are made early in treatment or not at all, any inference with regard to causal direction must be deemed exploratory. In order to characterize the mediational relationships among need–service matching, treatment duration and drug use outcomes more fully, future evaluations should measure the timing of needs assessment and service delivery daily or weekly through the use of patient diaries, detailed chart abstraction or repeated interviewing during treatment.
Given the retrospective cross-sectional nature of the NTIES treatment discharge data, we explored the notion that the mediating relationship might be reversed. That is, longer time of treatment contact might have allowed greater opportunity to match patients’ needs or to address a matched need more fully. However, the lack of change in the treatment duration coefficient in models with and without the matching variable does not support a mediating role for need–service matching. Taken with our other findings, this result suggests that treatment duration partially mediates the effect of need–service matching, but not vice-versa.
In terms of the individual service domains, the strongest effects on drug use improvement were from matching needs for vocational and housing services. These findings are consistent with the concept that a structured and supportive recovery environment produces the best drug treatment outcomes, because work is perhaps the most important source of daily structure and stable housing is essential to a supportive environment (ASAM Working Group on PPC-2 1996). The vocational results are consistent with research that demonstrates positive effects of vocational rehabilitation on drug use outcomes (Platt 1995). However, vocational and housing needs were least likely to be service-matched. They were most likely to be matched in long-term residential programs and least likely to be matched in methadone (Gerstein et al. 1997), which may partially account for relatively stronger and weaker matching effects in these modalities.
This study has a number of measurement limitations. Patients’ ratings of the importance of treatment in a particular domain are subjective, and may reflect motivational states in addition to actual needs. However, insofar as most clinical assessments of need for services are based on self-report, this measure makes clinical sense. Although one might put greater trust in self-report measures based on reports (e.g. number of prior treatments) rather than ratings (e.g. rating of need for treatment on a Likert-type scale), reports are similarly subject to reporting errors and cognitive distortions. Although the measures of drug use improvement have face validity and correlate moderately with urine toxicology, they have not been fully tested for validity against established measures. It is also uncertain whether patients accurately report their receipt of services, although other research has validated self-reports of service utilization (Ritter 2001).
This study has some advantages over other investigations of need–service matching. Previous research has examined patients from single modalities or cities (Joe et al. 1991; Fiorentine 1998; Hser et al. 1999a). Idiosyncrasies in local treatment practices, funding and administrative structures might thus have constrained external validity. In contrast, the NTIES sample includes a diversity of modalities and geographic regions, and achieved a favorable rate of attrition. However, the purposive sample of the NTIES may limit its generalizability, especially since it includes treatment units that had received funding to expand service delivery.
An alternative hypothesis posits that linking patients to services that address their needs might ameliorate problems that could lead to relapse (Daley 1988; McLellan et al. 1997). ‘Matching’ needs in this study suggests that the patient received the service, but not necessarily that the problem was resolved or even improved. In this respect, the quality and quantity of services may have been insufficient. However, other research has suggested that few service sessions covering a problem area are necessary to affect outcomes (McLellan et al. 1997). In general, determining the extent to which needs are resolved by service delivery represents a level of detailed measurement that is not available in NTIES. Finally, patients presenting themselves for drug treatment often have a wide variety of needs beyond the five domains examined in this study (Hser et al. 1999a). For example, women entering treatment often need transportation and child care (Smith & Marsh 2002), and these services do improve treatment retention and outcomes (Marsh, D’Aunno & Smith 2000; Friedmann, Lemon & Stein 2001). The current study cannot comment about matching services to these other important needs.
We nonetheless conclude that matching comprehensive services to needs is a useful addiction treatment practice among patients with a high burden of service needs. Treatment duration might partially mediate its effect on improvements in drug use. These findings are important given the increasing level of patients’ needs and the stagnant state of comprehensive service delivery in substance abuse treatment programs (Durkin 2002; Friedmann et al. 2003b). This context for the findings of the current study implies that comprehensive service delivery, especially involving housing and employment services among high-needs patients, should be given greater emphasis in policies, initiatives and block grants that seek to improve addiction treatment outcomes. These results also provide impetus for the consideration of patients’ needs assessment and comprehensive service delivery in performance measures for substance abuse treatment services (Garnick et al. 2002).
Acknowledgments
The authors thank Jennifer Rose, PhD for her assistance with significance testing for the mediation analysis. Additional thanks to Felicia Cerbone and Marianna Gerstein at NORC’s Washington DC office for their helpful comments on earlier drafts of this manuscript, and to the anonymous reviewers at Addiction whose critical insights led to valuable re-thinking and re-analysis of the data. This research was supported by National Institute on Drug Abuse (NIDA) grants K08-DA00320 and R01 DA13615 and grant number 014673 from the Robert Wood Johnson Foundation (RWJF) Substance Abuse Policy Research Program. Dr Friedmann is an RWJF Generalist Physician Faculty Scholar. The National Opinion Research Center at the University of Chicago carried out the NTIES project under Contract number ADM 270-92-0002 from the Substance Abuse and Mental Health Services Administration’s Center for Substance Abuse Treatment (CSAT). The views expressed in this article are the authors’ and are not necessarily those of RWJF, NIDA, CSAT or any affiliated agencies.
References
- ASAM Working Group on PPC-2. ASAM Patient Placement Criteria for Substance-related Disorders. 2. Chevy Chase, MD: American Society of Addiction Medicine; 1996. PPC-2. [Google Scholar]
- Ball JC, Ross A. The Effectiveness of Methadone Maintenance Treatment. New York: Springer-Verlag; 1991. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Broome KM, Flynn PM, Simpson DD. Psychiatric comorbidity measures as predictors of retention in drug abuse treatment programs. Health Services Research. 1999;34:791–806. [PMC free article] [PubMed] [Google Scholar]
- Daley DC. Five perspectives on relapse in chemical dependency. In: Daley DC, editor. Relapse: Conceptual, Research and Clinical Perspectives. New York: Haworth Press; 1988. pp. 3–26. [Google Scholar]
- Durkin EM. An organizational analysis of psychosocial and medical services in drug abuse treatment programs. Social Service Review. 2002;76:406–429. [Google Scholar]
- Fiorentine R. Effective drug treatment. Testing the distal needs hypothesis. Journal of Substance Abuse Treatment. 1998;15:281–289. doi: 10.1016/s0740-5472(97)00194-3. [DOI] [PubMed] [Google Scholar]
- Friedmann PD, Zhang Z, Hendrickson J, Stein MD, Gerstein DR. Effect of primary medical care on addiction and medical severity in substance abuse treatment programs. Journal of General Internal Medicine. 2003a;18:1–8. doi: 10.1046/j.1525-1497.2003.10601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedmann PD, Lemon S, Durkin E, D’Aunno TA. Trends in comprehensive service availability in out-patient drug abuse treatment. Journal of Substance Abuse Treatment. 2003b;24:81–88. doi: 10.1016/s0740-5472(02)00323-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedmann PD, Lemon SC, Stein MD. Transportation and retention in outpatient drug abuse treatment programs. Journal of Substance Abuse Treatment. 2001;21:97–103. doi: 10.1016/s0740-5472(01)00185-4. [DOI] [PubMed] [Google Scholar]
- Garnick DW, Lee MT, Chalk M, Gastfriend D, Horgan CM, McCorry F, McLellan AT, Merrick EL. Establishing the feasibility of performance measures for alcohol and other drugs. Journal of Substance Abuse Treatment. 2002;23:375–385. doi: 10.1016/s0740-5472(02)00303-3. [DOI] [PubMed] [Google Scholar]
- Gerstein DR, Datta AR, Ingels JS, Johnson RA, Rasinski KA, Schildhaus S, Talley K, Jordan K, Phillips DB, Anderson DW, Condelli WG, Collins JS. NTIES. National Treatment Improvement Evaluation Study. Final Report. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 1997. [Google Scholar]
- Gerstein DR, Harwood HJ. Report of the Committee for the Substance Abuse Coverage Study, Division of Health Care Services, Institute of Medicine. Washington, DC: National Academy Press; 1990. Treating Drug Problems: a Study of the Evolution, Effectiveness and Financing of Public and Private Drug Treatment Systems. [PubMed] [Google Scholar]
- Gerstein DR, Johnson RA. Non-response and selection bias in treatment follow-up studies. Substance Use and Misuse. 2000;35:971–1014. doi: 10.3109/10826080009148429. [DOI] [PubMed] [Google Scholar]
- Gerstein DR, Zhang Z. Treatment Outcomes for Different Types of Substance Abuse. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Treatment, Department of Health and Human Services; 2001. Caliber/NED Contract no. 270-97-7016. [Google Scholar]
- Hser YI, Polinsky ML, Maglione M, Anglin MD. Matching clients’ needs with drug treatment services. Journal of Substance Abuse Treatment. 1999a;16:299–305. doi: 10.1016/s0740-5472(98)00037-3. [DOI] [PubMed] [Google Scholar]
- Hser YI, Grella CE, Hsieh S, Anglin MD, Brown BS. Prior treatment experience related to process and outcomes in DATOS. Drug and Alcohol Dependence. 1999b;57:137–150. doi: 10.1016/s0376-8716(99)00081-2. [DOI] [PubMed] [Google Scholar]
- Hubbard RL, Craddock SG, Flynn PM, Anderson J, Etheridge RM. Overview of 1 year follow-up outcomes in the Drug Abuse Treatment Outcome Study. Psychology of Addictive Behaviors. 1997;11:261–278. [Google Scholar]
- Joe GW, Simpson DD, Hubbard RL. Treatment predictors of tenure in methadone maintenance. Journal of Substance Abuse. 1991;3:73–84. doi: 10.1016/s0899-3289(05)80007-0. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Krull JL, MacKinnon DP. Multilevel mediation modeling in group-based intervention studies. Evaluation Review. 1999;23:418–444. doi: 10.1177/0193841X9902300404. [DOI] [PubMed] [Google Scholar]
- Littell RC, Milliken GA, Stroup W, Wolfinger RD. SAS System for Mixed Models. Cary, NC: SAS Institute, Inc; 1996. [Google Scholar]
- Marsh JC, D’Aunno TA, Smith BD. Increasing access and providing social services to improve drug abuse treatment for women with children. Addiction. 2000;95:1237–1247. doi: 10.1046/j.1360-0443.2000.958123710.x. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Grissom GR, Brill P, Durell J, Metzger DS, O’Brien CP. Private substance abuse treatments: are some programs more effective than others? Journal of Substance Abuse Treatment. 1993;10:243–254. doi: 10.1016/0740-5472(93)90071-9. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Weisner C. Achieving the public health and safety potential of substance abuse treatment: implications for patient referral, treatment ‘matching’, and outcome evaluation. In: Bickel WK, DeGrandpre RJ, editors. Drug Policy and Human Nature: Psychological Perspectives on the Prevention, Management, and Treatment of Illicit Drug Abuse. New York: Plenum Press; 1996. pp. 127–154. [Google Scholar]
- McLellan AT, Grissom GR, Zanis D, Randall M, Brill P, O’Brien CP. Problem-service ‘matching’ in addiction treatment. A prospective study in 4 programs. Archives of General Psychiatry. 1997;54:730–735. doi: 10.1001/archpsyc.1997.01830200062008. [DOI] [PubMed] [Google Scholar]
- O’Brien CP, McLellan AT. Myths about the treatment of addiction. Lancet. 1996;347:237–240. doi: 10.1016/s0140-6736(96)90409-2. [DOI] [PubMed] [Google Scholar]
- Platt JJ. Vocational rehabilitation of drug abusers. Psychology Bulletin. 1995;117:416–433. doi: 10.1037/0033-2909.117.3.416. [DOI] [PubMed] [Google Scholar]
- Ritter PL, Stewart AL, Kaymaz H, Sobel DS, Block DA, Lorig KR. Self-reports of health care utilization compared to provider records. Journal of Clinical Epidemiology. 2001;54:136–141. doi: 10.1016/s0895-4356(00)00261-4. [DOI] [PubMed] [Google Scholar]
- Simpson DD. Treatment for drug abuse: follow-up outcomes and length of time spent. Archives of General Psychiatry. 1981;38:875–880. doi: 10.1001/archpsyc.1981.01780330033003. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Joe GW, Brown BS. Treatment retention and follow-up outcomes in the drug abuse treatment outcome study (DATOS) Psychology of Addictive Behaviors. 1997;11:294–307. [Google Scholar]
- Smith BD, Marsh JC. Clientservice matching in substance abuse treatment for women with children. Journal of Substance Abuse Treatment. 2002;22:161–168. doi: 10.1016/s0740-5472(02)00229-5. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhardt S, editor. Sociological Methodology. Washington, DC: American Sociological Association; 1982. pp. 290–312. [Google Scholar]
- Wolff K, Farrell M, Marsden J, Monteiro MG, Ali R, Welch S, Strang J. A review of biological indicators of illicit drug use, practical considerations and clinical usefulness. Addiction. 1999;94:1279–1298. doi: 10.1046/j.1360-0443.1999.94912792.x. [DOI] [PubMed] [Google Scholar]
- Zhang Z, Friedmann PD, Gerstein DR. Does retention matter? Treatment duration and improvement in drug use. Addiction. 2003;98:673–684. doi: 10.1046/j.1360-0443.2003.00354.x. [DOI] [PubMed] [Google Scholar]