Abstract
An initial efficacy test of an innovative behavioral outpatient treatment model for adolescents with problematic use of marijuana enrolled 69 adolescents, aged 14–18, and randomly assigned them to one of two treatment conditions. Both conditions received individualized Motivational Enhancement and Cognitive Behavioral Therapy (MET/CBT) and a twice-weekly drug-testing program. The experimental contingency management condition involved a clinic delivered, abstinence-based incentive program, and weekly behavioral parent training sessions that included a parent-delivered, abstinence-based, substance monitoring contract. The comparison condition included an attendance-based incentive program, and weekly psychoeducational parent sessions. Follow-up assessments were performed at 3, 6, 9 months post-treatment. The experimental condition showed greater marijuana abstinence during treatment, e.g., 7.6 vs. 5.1 continuous weeks and 50% vs. 18% achieved ≥ 10 weeks of abstinence. Improvements were found in parenting and youth psychopathology across treatment conditions, and improvements in negative parenting uniquely predicted post treatment abstinence. The outcomes observed in the experimental condition are consistent with adult substance dependence treatment literature, and suggest that integrating CM abstinence-based approaches with other empirically-based outpatient interventions provides an alternative and efficacious treatment model for adolescent substance abuse/dependence. Replication and continued development of more potent interventions remain needed to further advance the development of effective substance abuse treatments for adolescents.
Keywords: contingency management, adolescent, marijuana, cannabis, treatment
1. Introduction
Marijuana remains the most prevalent illicit substance used by adolescents, and marijuana users are at increased risk for delinquency, school failure, physical and psychological problems, and selling illegal drugs (Rey et al., 2004; Tims et al., 2002). The number of adolescents receiving treatment for marijuana abuse or dependence more than tripled from 1992 to 2002, and the majority of all adolescents in substance abuse treatment report marijuana as their primary substance (Substance Abuse and Mental Health Services Administration, 2008). Several clinical trials indicate that family-based, cognitive-behavioral, and possibly adjunct pharmacological interventions hold promise for treating adolescent substance abuse (Cornelius et al., 2005; Randall and Cunningham, 2003; Riggs et al., 2004; Waldron and Turner, 2008). Although efficacious, the low abstinence rates and the relatively low magnitude of reduction in substance use indicate much room for additional enhancement, suggesting that adolescent substance abuse treatments need to be improved and alternative treatment models explored (Compton and Pringle, 2004). Further, the adolescent treatment literature has generally focused on reductions in the frequency of use or on reductions in problem use, with fewer demonstrations of differences across treatment conditions in rates of documented abstinence.
In an effort to further enhance outcomes for adolescent substance abuse, we have developed a novel treatment that integrated a developmentally-appropriate, contingency-management based intervention (CM) with Motivational Enhancement and Cognitive Behavioral Therapy (MET/CBT). CM approaches have become one of the most thoroughly researched and effective behavioral procedures to increase drug abstinence and other treatment targets across adult substance-dependence disorders (Higgins et al., 2008; Petry and Simic, 2002). CM treatments for adolescent substance abuse have received little experimental testing. A number of studies describe use of CM-like procedures as part of their multicomponent intervention, e.g., instructing parents to provide rewards and consequences for abstinence or use (eg, Azrin et al., 1994; Henggeler et al., 2002; Liddle et al., 2001; Waldron et al., 2001). Unfortunately, none have isolated and tested such CM components. Further, in the absence of a schedule of urine drug testing of sufficient frequency to verify abstinence, it is not clear that parents can effectively implement a contingency management plan at home. Two recent trials have isolated CM procedures. Henggeler et al. (2006) found that abstinence-based incentives did not clearly enhance outcomes when added to Drug Court and a comprehensive family based therapy, although the reinforcement schedule was not reported, and all youth received incentives and consequences based on urine drug testing results through the 12 month Drug Court program. Krishnan-Sarin et al. (2006) found that youth who received an abstinence-based incentive intervention and CBT had greater rates of tobacco abstinence than youth who received CBT alone. Despite that lack of studies, recent reports describe dissemination of CM interventions in community adolescent treatment settings (Henggeler et al., 2008; Lott and Jencius, 2009).
Our CM model integrates three empirically-based interventions (Kamon et al., 2005). First, abstinence-based incentives are provided by the clinic to motivate treatment engagement and promote initial abstinence from marijuana and other substances (Budney et al., 2006; Higgins et al., 1994). Second, a parent-directed CM program is employed to further motivate initiation of abstinence, to maintain abstinence after treatment is discontinued, and to better manage other related behavior problems (Dishion and Kavanagh, 2003). Third, a CM intervention is used to motivate parent participation in and adherence to the program. Here, parents earn chances to win prizes for actively participating in treatment (Petry et al., 2000). In summary, the CM components are designed to increase adolescents’ motivation for abstinence, and enhance parents’ abilities to use effective parenting to decrease substance use and other problems.
The present trial provides a test of this experimental intervention by comparing it with a stringent comparison treatment. The primary hypotheses were that the abstinence-based CM programs would promote greater abstinence during the treatment period, and the behavioral parenting training would promote greater maintenance of drug abstinence post-treatment. Secondary hypotheses reflected changes in potential mechanisms related to the use of behavioral parent training, including greater reductions in adolescent conduct problems and greater improvements in effective parenting. Exploratory analyses also tested changes in parenting during treatment as a mediator of treatment effects on substance outcomes during follow up.
2. Methods
2.1. Participants
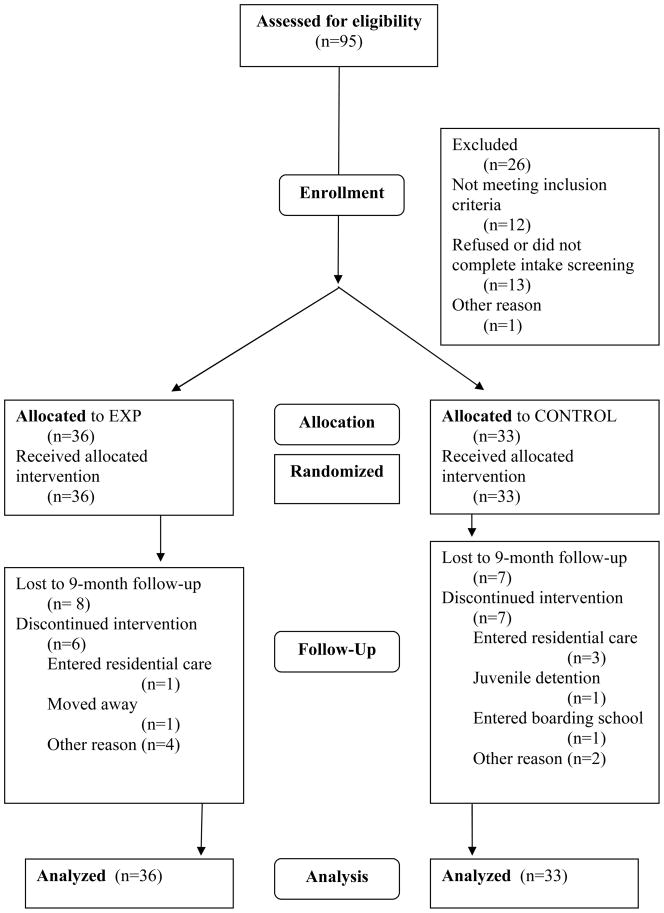
The study was conducted in compliance with the Institutional Review Board of the University of Vermont. Families living in the greater Burlington, Vermont area were referred for treatment by schools, the juvenile justice system, community therapists, physicians, or were self-referred. We advertised our treatment services in local newspapers, posted flyers in the community, and sent mailings to local schools, physicians, and counselors. Inclusion criteria were: 1) age 12–18 years; 2) reported use of marijuana during the prior 30 days or a marijuana-positive urine test; 3) living with a parent/guardian who agreed to participate; 4) residing within a 30 minute drive to the clinic. Adolescents were ineligible if they 1) displayed active psychosis or current suicidal behavior or had a severe medical illness limiting participation; or 2) had alcohol, opiate, or cocaine dependence requiring more intensive treatment. No adolescents were excluded based on these criteria. A total of 95 youth were assessed, 12 did not meet inclusion criteria, 14 refused treatment or did not complete the intake assessment or did not enroll for another reason, and 69 (57 male, 12 female) enrolled in the trial. See Figure 1 for the CONSORT participant flow diagram. Written informed consent was obtained from the parent(s) or legal guardian; assent was obtained from the adolescent. Youth were enrolled between April 2003 and April 2005, and follow-up assessments were completed by April 2006.
Figure 1.
CONSORT participant flow diagram. EXP=Experimental condition; Control=Control condition
Minimum likelihood allocation was used to randomly assign participants via computer sequentially to one of the two treatment conditions while balancing across conditions on seven baseline characteristics that may influence outcome, abstinence prior to treatment (0 vs. ≥1 day), gender, involvement with the legal system, age (≥17 or <17), tobacco smoker, prior participation in brief treatment in our clinic, and therapist.
2.2. Measures
2.2.1. Substance use
A Bachelor’s level research assistant administered the Vermont Structured Diagnostic Interview (VSDI; Hudziak et al., 2004) to assess DSM-IV substance use disorders. Interviewers were trained to administer the instruments via manual review, observation, and supervised practice interviews. The interview has demonstrated good psychometric properties (Hudziak et al., 2004). Substance use was assessed at intake and twice weekly throughout treatment using the Time-Line Follow-Back method (Sobell and Sobell, 1992), parent report, urinalysis testing, and breathalyzers. At intake, the Time-Line Follow Back assessed frequency of marijuana, alcohol and other substance use three months prior to treatment, and was administered at all visits during treatment and post-treatment.
Urine toxicology monitoring during the 14-week treatment period involved twice-weekly (e.g., Monday/Thursday or Tuesday/Friday) testing. An alcohol breath test was performed at each visit, and parents were provided with and trained to use disposable breathalyzers (AlcoPro, Inc., Knoxville) to test for alcohol use at home. Urine specimens were obtained under same-gender, staff observation and screened via an onsite Enzyme-Multiplied Immunoassay Technique (EMIT: Dade-Behring, San Jose, CA). Specimens were immediately screened for marijuana, cocaine, opioids, benzodiazepines, amphetamines, and methamphetamines, and results were provided during the clinic visit. The cannabinoid cutoff level for a positive test was 50ng/ml. If either the adolescent or parents reported substance use, or a positive urine specimen or breath test was obtained, the adolescent was considered positive for the purpose of CM implementation. Invalid specimens (creatinine below 30 mg/dl) resulted in a request to provide a replacement specimen within 4–24 hours. Failure to submit a scheduled specimen was treated as a positive result. Extensive outreach procedures were employed including: multiple phone calls, flexible scheduling, offering to go to a participant’s home or neutral site for collection, and use of excused absences in cases where legitimate conflicts (e.g., inclement weather, illness, family vacation) were discussed proactively. A maximum of 4 excused absences were granted, which resulted in lengthening the treatment period by up to 2 weeks.
2.2.2. Adolescent psychopathology
Adolescents and parents were each administered the VSDI (Hudziak et al., 2004) to assess DSM-IV disorders commonly diagnosed in adolescence. Parents and adolescents also completed the Child Behavior Checklist (CBCL) and Youth Self-Report (YSR), respectively (Achenbach and Rescorla, 2001). The CBCL and YSR yield scores on 8 syndromes and three broad scales. At intake, the CBCL and YSR assessed behaviors during the past 6 months. At treatment end and follow-up assessments, parents and adolescents reported on behaviors during the past 3 months.
2.2.3. Parenting measures
The Alabama Parenting Questionnaire (APQ) was completed by parents and scores were obtained on three factors, Positive Involvement, Ineffective Discipline, and Deficient Monitoring (Frick, 1991; Wells et al., 2000). The Positive Involvement scale measures the degree to which parents show interest towards, and offer praise, affection, and other forms of positive reinforcement to the teen. Ineffective Discipline measures the predictability and consistency of discipline practices. Deficient Monitoring measures the degree to which the child is outside parental supervision.
2.2.4. Follow-up assessments
At the end of treatment, and 3, 6, and 9 months post the end of treatment, the adolescent and parent(s) returned to the clinic for a comprehensive assessment. Research assistants not blinded to condition collected the following: urine specimen, self-reported substance use (Time-Line Follow-Back), CBCL/YSR, and the APQ.
2.3. Treatment conditions
Both treatment conditions involved one 90-minute, weekly therapy session for 14 consecutive weeks and twice-weekly drug testing. All parent(s) were informed of drug toxicology results. All adolescents received the MET/CBT12 curriculum modified for individual therapy (Sampl and Kadden, 2001; Webb et al., 2001). At the end of the 14 weeks, all families were offered an additional 12 weeks of once weekly substance testing to facilitate parental monitoring and were referred, when appropriate, to other community resources.
2.3.1. Experimental Condition (MET/CBT+Abstinence CM+Family Management)
2.3.1.1. Abstinence-based Contingency Management
Adolescents in the Experimental condition (EXP) participated in an abstinence-based contingency management program modeled from that used in previous trials for adult marijuana dependence (Budney et al., 2006), but with one major modification. Rather than receive incentives for documented marijuana abstinence, adolescents received incentives only if they provided a urine specimen and breath specimen that tested negative for all substances, and parent and self-reports indicated no substance use (including alcohol). Δ-9-THC remains detectable at 50ng/ml for up to two weeks and sometimes longer in heavy marijuana users, thus the abstinence contingency did not start until Week 3. During Weeks 1–2, participants in both conditions received $5 vouchers for each specimen provided independent of test results to encourage compliance with the program.
For each substance-negative specimen and report during Weeks 3–14, EXP participants earned vouchers with a monetary value. The voucher value started at $1.50, escalated by $1.50 with each consecutive negative specimen, and a $10 bonus was earned for each two consecutive negative results. Vouchers were reset back to their initial value if results were positive, from which they could escalate again after three consecutive negative results. An adolescent who was abstinent throughout Weeks 3–14 earned vouchers worth $570. Voucher earnings were redeemed for retail goods selected by the teen (e.g., movie pass, sports/hobby equipment, clothing). Adolescents in EXP earned a mean of $312 (SD=$237) or $22.28 per week.
2.3.1.2. Family Management
Parents in the EXP condition received the Family Management (FMC) curriculum during weekly counseling sessions (Dishion et al., 2003). Topics covered include identifying and labeling adolescent behavior, developing incentives and consequences for change, limit-setting, monitoring, and relationship skills. The first two sessions provided an overview of FMC and a review and discussion of a feedback report summarizing assessment information regarding the adolescent’s substance use and risk factors, and parent risk factors (parenting behaviors, marital satisfaction, parent psychopathology including substance use). During Session 3, a Substance Monitoring Contract (SMC) was developed between the parent(s) and youth specifying positive and negative consequences to be implemented in response to abstinence or substance use. The therapist and parents developed lists of potential incentives for abstinence and negative consequences for substance use that could be implemented following each substance testing appointment. All subsequent FMC sessions followed a standard format. Sessions began by reviewing substance testing results and evaluating or modifying the SMC. Homework assignments were reviewed and the training from the FMC curriculum was provided.
To motivate and reinforce parent compliance with treatment, a CM procedure utilizing the Fishbowl method was implemented (Petry et al., 2000). Each week, parents were asked to complete six tasks: attend therapy, attend mid-week urine testing appointments, implement the SMC (twice per week), complete homework, and administer breathalyzers. Parents earned one draw from the Fishbowl for each task. Each draw resulted in obtaining a winning (75% chance) or non-winning slip (25% chance). Winning slips ranged in value from small ($1–$2: 68% chance), to medium ($20: 7% chance), to large prizes ($100: 1% chance). Prizes were delivered immediately and included gift certificates to restaurants, ice cream shops, movie theaters, and grocery stores. Parent earnings averaged approximately $100 or $7.22/week.
2.3.2. Control Condition (MET/CBT+Attendance CM+Parent Psychoeducation)
To encourage compliance with urine drug testing and participation in the MET/CBT sessions, adolescents in the CONTROL condition could earn $5 vouchers twice per week (maximum earnings of $140; average actual earnings=$113) for attending scheduled counseling and urinalysis appointments. Parents in the CONTROL condition received a structured psychoeducational substance use curriculum during their once-weekly session. (McCallum, 1994). During each session a topic was discussed; topics included: drug knowledge, drug use consequences, understanding reasons for drug use and for stopping use, improving communication, negotiation problems, and positive parenting strategies. These sessions differed from the FMC in that systematic training exercises and assignments were not provided, an SMC was not developed, and the session topics varied. Commonalities with the EXP intervention included: equivalent frequency and duration of counseling, review of assessment feedback report, receiving drug testing results twice per week, training in use of home breathalyzers, proactive case-management services, and reading materials on parenting.
2.4 Therapists, treatment integrity and fidelity
Three master’s level clinicians (1 male, 2 female) and 1 female postdoctoral fellow (all European American) served as therapists. Each therapist treated an equal number of EXP and CONTROL youth. Therapists had systematic training and supervised experience in MET/CBT, the Family Management Curriculum, and the Parent Drug Education curriculum for at least 6–12 months prior to participation in the trial. To maintain treatment integrity: (a) therapists followed detailed manuals for each treatment and used a checklist during each session that detailed that session’s curriculum components; (b) all treatment sessions were videotaped and one tape was randomly selected to be reviewed in weekly supervision to provide feedback to the therapists; (c) all active cases were discussed weekly in group supervision using a checklist to review each component; (d) the postdoctoral fellow reviewed one videotaped session approximately every two weeks, selecting one from each therapist on a rotating schedule. A fidelity checklist developed for this trial was used to rate and comment on the therapist’s delivery of each treatment component; (e) when need for additional training was identified based on supervision or tape reviews, weekly one-on-one remedial training was provided by the postdoctoral fellow or first or second authors. Such training involved weekly tape reviews with modeling and role-playing delivery of the problematic components. One therapist received such remedial training, which lasted for approximately 4–6 months.
2.5. Data analysis
Comparisons between conditions on baseline characteristics and primary outcome measures (longest period of documented continuous marijuana abstinence achieved during treatment and number of participants who achieved specific durations of continuous abstinence) were performed using t-tests or rank sum tests for continuous measures and chi-square tests for nominal measures. All families (N=69) who attended one or more sessions were included in all analyses consistent with an intent-to-treat model.
Generalized Estimating Equation (GEE) analyses were used to examine treatment condition differences in post treatment marijuana abstinence. These analyses were performed counting missing urine specimens as positive for marijuana to provide a conservative estimate of use, and were also performed by including missing data. As results were almost identical, results are presented treating missing samples as positive. Treatment condition differences in secondary marijuana use outcome measures (self-reports of marijuana use) and associated risk factors (youth psychopathology and parenting) were tested via mixed-model repeated measures (i.e., hierarchical linear modeling) to examine change from pre- to post-treatment. Analyses performed either including or excluding contradictory and/or incomplete self-report substance use data did not produce substantially different findings. For self-report measures, we provide the findings of the mixed-model repeated measures analysis on all available data. We also conducted exploratory structural equation modeling analyses testing relations between treatment condition, change in parenting (a hypothesized mediator), and post treatment marijuana use.
3. Results
3.1. Participants
Demographic and substance use characteristics were similar across conditions as shown in Table 1. Thirty-six youth were enrolled in EXP and 33 in CONTROL. Fifty-two families had two-parent participation and 17 had mother-only participation. Overall, 65% of youth tested positive for THC at intake. On average, adolescents reported using marijuana 1.8 (SD=1.4) times per day on 13.3 (SD=10.3) days during the month prior to intake. Thirty-one (45%) adolescents met DSM-IV criteria for Marijuana Abuse only and 30 (43%) for Marijuana Dependence. Eight (12%) adolescents were diagnostic orphans. They did not endorse sufficient symptoms to meet criteria for Marijuana Abuse or Dependence, but met all other inclusion criteria including a THC positive urine drug test and/or reported use in the 30 days prior to intake. Those not meeting DSM criteria were less likely to have a THC positive intake urine drug test but the difference was not significant (No DSM: 50% THC positive vs. DSM Abuse or Dependence: 67%, X2(1)=.34, p=.92). Those not meeting DSM criteria reported significantly fewer days of use in the 30 days prior to intake (No DSM: Mean=4.4 days, SD=5.8 vs. DSM Abuse or Dependence: Mean=14.6 days, SD=10.1, F=10.2, p<.01). Fifteen (22%) also met criteria for Alcohol Abuse, and participants reported drinking an average of 3.4 (SD=4.0) drinks per day on 1.5 (SD=2.1) days in the month prior to intake. One met criteria for Opiate Abuse and one for Sedative Abuse. Forty (58%) adolescents were regular tobacco users.
Table 1.
Demographic and Substance Use Characteristics
| Treatment Condition |
||
|---|---|---|
| EXP | CONTROL | |
| N=36 | N=33 | |
| Gender | ||
| Male | 31 (86%) | 26 (79%) |
| Ethnicity | ||
| Caucasian | 33 (92%) | 30 (91%) |
| African American | 2 (6%) | 2 (6%) |
| Hispanic | 1 (3%) | 1 (3%) |
| Mean SES (9 step scale)a | 7.1 (1.5) | 7.0 (1.7)b |
| Mean Age | 16.1 (1.1) | 15.9 (1.0) |
| Father participation | 30 (83%) | 22 (67%) |
| Legal problems | 12 (33%) | 10 (30%) |
| Tobacco user | 23 (64%) | 17 (52%) |
| Mental health services in past 12 months | 21 (58%) | 15 (46%) |
| Intake Urine Drug Test THC positive | 22 (61%) | 23 (70%) |
| Mean days used marijuana in past 30 | 11.1 (9.2) | 15.7 (11.0) |
| Mean times used marijuana per day | 1.7 (1.4) | 2.0 (1.4) |
| Mean days used alcohol in past 30 | 1.6 (2.0) | 1.5 (2.1) |
| Mean drinks per drinking day | 3.1 (3.5) | 3.8 (4.5) |
| DSM Substance Use | ||
| Marijuana Dependence | 14 (39%) | 16 (49%) |
| Marijuana Abuse | 16 (44%) | 15 (45%) |
| No Marijuana Abuse/Dependence | 6 (17%) | 2 (6%) |
| Alcohol Abuse | 8 (22%) | 7 (21%) |
| Nicotine Dependence | 2 (6%) | 5 (15%) |
| DSM Mental Health | ||
| Endorsed by either parent | ||
| ODD+/or CD | 21 (58%) | 20(61%) |
| ADHD | 15 (42%) | 18 (55%) |
| Major Depression +/or GAD | 17 (47%) | 13 (39%) |
| Endorsed by youth | ||
| ODD+/or CD | 8 (22%) | 10 (30%) |
| ADHD | 6 (17%) | 12 (36%) |
| Major Depression +/or GAD | 5 (14%) | 7(21%) |
Note. All p’s >.05 for treatment condition comparisons. EXP=Experimental Condition; CONTROL=Control Condition; SES=Socioeconomic Status; DSM=Diagnostic and Statistical Manual; THC= Tetrahydrocannabinol; ODD = Oppositional Defiant Disorder; CD = Conduct Disorder; ADHD = Attention Deficit Hyperactivity Disorder; GAD = Generalized Anxiety Disorder.
A score of 7 on the (Hollingshead, 1975) scale represents the following types of occupations: teacher, real estate broker, administrator.
Excludes one subject for whom SES could not be scored.
As shown in Table 1 rates of psychopathology were high in both conditions with rates of ODD or CD, ADHD, and Depression or GAD ranging from 39%–61% based on parent reports and from 14%–36% based on youth reports. The pattern of more psychopathology reported by parents than youth was also observed on the CBCL and YSR. Generally, EXP and CONTROL youth had similar mean CBCL and YSR internalizing, externalizing, total problems, and parenting scores at intake (all p’s >.05).
3.2. Participation and retention
Teens and mothers attended 11.3 (SD=4.0), and 10.7 (SD=3.9) of 14 sessions on average, respectively, with no between-condition differences. Fathers who attended one or more sessions (N=51) attended 9.1 (SD=4.5) sessions on average. Retention was good, as measured by attendance during the last treatment week: 77% for both conditions. Adolescents in both conditions provided a similar number of urine specimens (EXP: 23.4 (SD=8.1) vs. CONTROL: 22.6 (SD=7.4)). Participation rates for follow-ups also did not differ between EXP and CONTROL: 92% vs. 91%, 75% vs. 85%, 75% vs. 85%, and 78% vs. 79% for the discharge and 3-, 6-, and 9-month assessments, respectively. No adverse events were observed.
3.3. During-treatment abstinence
Primary marijuana use outcome measures indicated that EXP enhanced continuous abstinence outcomes. EXP youth had more mean weeks of documented continuous marijuana abstinence during treatment than CONTROL youth (EXP: 7.6 (SD=5.6) vs. CONTROL: 5.1 (SD=4.5), t=−2.1; p=.04, d=.48, medium effect). Those in the EXP condition were also more likely to achieve ≥8 weeks of continuous abstinence (53% vs. 30%, X2(1)=3.6, p=.06) and ≥10 weeks of continuous abstinence (50% vs. 18%, X2(1)=7.7, p=.006), while rates of briefer periods of abstinence were similar across the two treatment conditions (≥4 weeks: EXP 61%, CONTROL 55%; ≥6 weeks: EXP 56%, CONTROL 46%).
3.4. Post-treatment abstinence
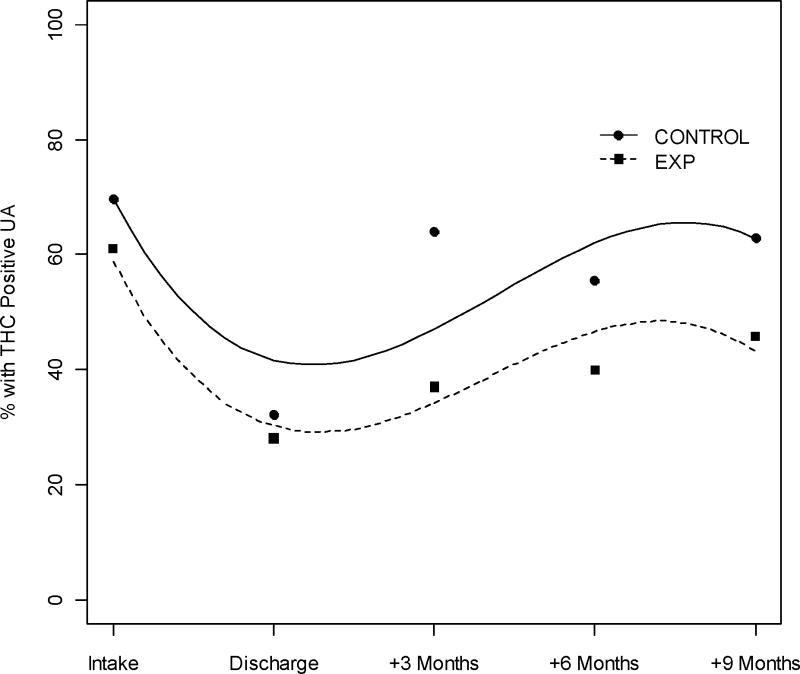
Generalized Estimating Equation (GEE) analyses comparing the point prevalence of marijuana use at intake, discharge and at 3, 6, and 9 months indicated that marijuana abstinence based on urine toxicology testing followed a cubic pattern. Marijuana use decreased during treatment (linear time effect = −1.22, p<.01), but then increased during follow-up (quadratic time effect = 0.41, p<.01) and began to level off again (cubic time effect = −0.04, p<.01). There were no significant treatment or time × treatment interaction effects, although EXP showed higher rates of abstinence at each timepoint (see Figure 2). Power was .80 to detect effect sizes of d=.40 for treatment condition and .29 for the treatment × time interaction. The observed effect sizes were .21 for treatment and <.10 for treatment × time. Results were similar whether missing urine drug tests were coded positive or included as missing values in the GEE analysis.
Figure 2.
GEE model of marijuana positive urine drug tests from intake to 9 months post treatment. Circles and squares represent observed percentages for the CONTROL and EXP conditions, respectively. The estimated cubic curves for each treatment condition are displayed. EXP=Experimental condition; CONTROL=Control condition; UA=Urinalysis
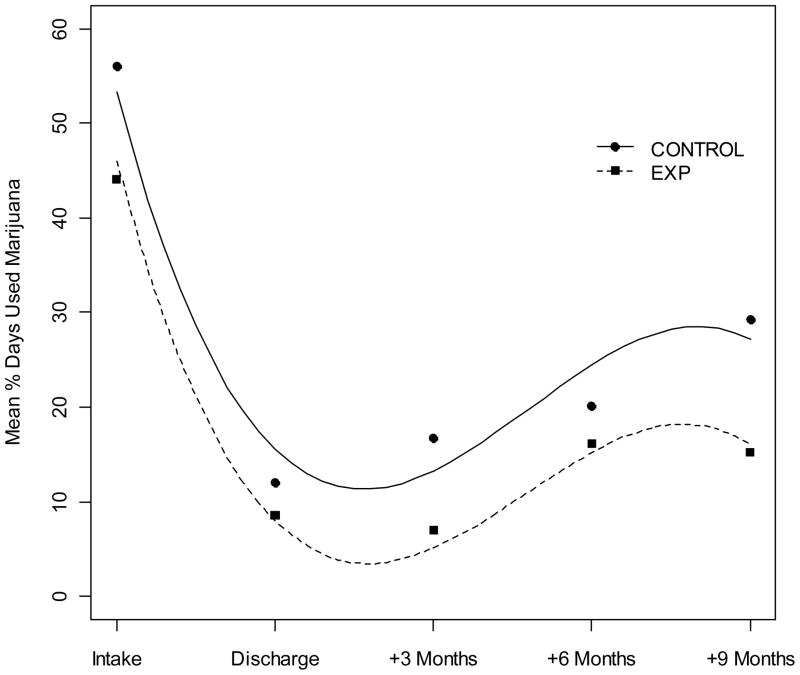
3.5 Self-reported marijuana use outcomes
The mixed-model repeated measures analysis of secondary marijuana use outcome measure (self-reports of marijuana use) did not show significant treatment or time × treatment interaction effects (see Figure 3). For these analyses, power was .80 to detect effect sizes of d=.37 for treatment condition and .26 for the treatment × time interaction. The observed effect sizes were .24 for treatment and <.10 for treatment × time. The linear, quadratic, and cubic effects of time were all significant (p<.01). Marijuana use decreased through treatment (linear time effect = −131.16), began to increase after treatment (quadratic time effect = 39.68), but stabilized at a level lower than pre-treatment (cubic time effect = −3.69). Similar results and power estimates were obtained for self-reports of alcohol use, which included a significant quadratic time effect (.80, p<.01), but no treatment or time × treatment interactions. Percent of days used alcohol declined from intake to the 3 month follow up, but increased from 6 to 9 months.
Figure 3.
Mixed model of reported percentage of days used marijuana in the 90 days prior to intake and between each subsequent assessment. Circles and squares represent observed percentages for the CONTROL and EXP conditions, respectively. The estimated cubic curves for each treatment condition are displayed. EXP=Experimental condition; CONTROL=Control condition.
3.6 Parenting and Teen Psychopathology
Significant time effects emerged for all 3 APQ parenting scales, with no significant time × treatment condition interactions. All d’s were <.10 for the interactions, with power=.80 to detect interactions ranging from d=.12 to .29 across scales. Positive Involvement showed significant linear improvement over time (B=2.8, p<.05), with mothers reporting significantly more positive involvement with their teens (B=4.7, p<.01). Deficient Monitoring showed significant quadratic change (B=.53, p<.01), with scores improving from intake to 3 months, and worsening from 3 to 9 months post treatment. Negative Discipline showed significant cubic changes (B=−.41, p<.01), with scores improving from pre- to post-treatment, increasing slightly from 3 to 6 months post-treatment, but declining again from 6 to 9 months post treatment. In addition, for Negative Discipline, there was a main effect of treatment condition (B=1.2, p<.05, d=.25), with significantly worse scores for the CONTROL condition than the EXP condition.
Significant quadratic time effects emerged for both psychopathology scales (internalizing B=.75, p<.01; externalizing B=.67, p<.01), with scores improving (decreasing) from intake to 3 months post-treatment, and rising slightly from 3 to 9 months post treatment. There were no significant time × treatment condition interactions. Both d’s were <.10 for the interactions, with power=.80 to detect interactions of d=.10. However, for Externalizing, there was a main effect of treatment condition (B=2.4, p<.05, d=.30), with significantly higher scores for the CONTROL condition than the EXP condition. Both scales also showed significant informant effects, with teens reporting significantly fewer problems than mothers on internalizing (B=−7.0, p<.01) and externalizing (B=−4.5, p<.01), and fathers reporting significantly fewer problems for teens than mothers on internalizing (B=−2.8, p<.05).
Another potential indicator of parenting change was participation in the optional weekly urine drug tests in the 12 weeks following the end of counseling. EXP families were expected to show greater attendance because they had been taught contingency contracting based on test results. A large percentage of both treatment conditions attended one or more of these appointments (70% of CONTROL, 78% of EXP). EXP teens attended more times (EXP: 5.3 vs. CONTROL: 3.9), but the difference was not significant. The number of tests attended across conditions was significantly related to marijuana abstinence at discharge (e.g., negative drug test) at discharge (t(67)=3.2, p<.01) and at 3 months (t(67)=2.2, p<.05), but not at 6 or 9 months. These results suggest that parents of youth who responded well to treatment continued with testing, and continued testing may have helped maintain abstinence while it was available.
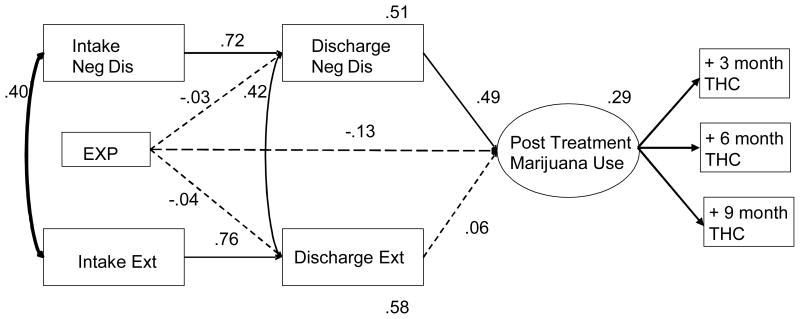
3.7 Predictors of Post Treatment Abstinence
We tested parenting, externalizing problems, and treatment condition as predictors of abstinence during the follow-up period (THC urine drug test results at 3, 6, and 9 months) in three exploratory structural models. Each model included: mean maternal and paternal CBCL externalizing ratings at intake and discharge, treatment condition, and a latent post treatment abstinence intercept construct with follow up urine test results (3,6,9 months) as indicators. Mean maternal and paternal Positive Involvement, Negative Discipline, and Poor Monitoring were each tested in a separate model. Models were tested in Mplus. The strongest results were found among parental negative discipline, adolescent externalizing problems, and post treatment substance use. As Figure 4 shows, negative discipline and adolescent externalizing were significantly correlated with each other at intake and discharge (Intake r=.40, Discharge r=.42) and showed significant stability from intake to discharge (Negative Discipline B=.72, Externalizing B=.76). Accounting for relations between intake and end of treatment allows us to interpret the end of treatment variables as reflecting during-treatment change. Consistent with the analyses presented above, treatment condition did not independently predict parenting or externalizing improvement, or marijuana use in the post-treatment period. However, changes in negative discipline (B=.49) were associated with marijuana abstinence in the follow-up period, with the model accounting for a total of 29% of variance in post treatment marijuana use. The identical pattern of results was found for Poor Monitoring, but Positive Involvement did not predict post treatment marijuana use. The final models fit well (RMSEAs=.00). These results suggest that inconsistent discipline and poor monitoring played an important role in marijuana use post treatment.
Figure 4.
Structural model predicting a post treatment marijuana use construct, defined by marijuana (THC) positive urine drug test results at 3, 6, and 9 month follow ups. Factor loadings of the THC result variables were all constrained to 1. EXP=Experimental condition; EXT=mean maternal and paternal CBCL Externalizing scores; Neg Dis=mean maternal and paternal APQ Negative Discipline scores; model p=.65, TLI=1.01, RMSEA=.00; Standardized coefficients are displayed; solid lines indicate estimates significant at p<.05.
4. Discussion
The CM-based intervention when integrated with MET/CBT (EXP) resulted in enhanced abstinence outcomes during the treatment period compared with the CONTROL intervention that integrated a participation-based incentive program and a psychoeducational parent program with MET/CBT. This finding is consistent with the growing literature on abstinence-based CM interventions with adult and young adult marijuana and other substance dependent treatment populations (Budney et al., 2007; Carroll et al., 2006; Higgins et al., 2008; Kadden et al., 2007). Previous controlled trials with adolescent substance abusers indicate that achieving abstinence during outpatient treatment is difficult. For example, “in-recovery” status at the end of treatment defined as self-reported abstinence for the prior 30 days averaged only 24% across the 5 outpatient interventions in the multi-site CYT study. In the present study, 53% in the EXP condition achieved at least 8 weeks of documented abstinence during the treatment period suggesting that this model may offer an alternative for increasing rates of extended periods of abstinence. In that regard, the CONTROL condition also performed fairly well; 55% of the adolescents in the CONTROL condition achieved at least 4 weeks of abstinence.
Despite during treatment differences in abstinence, we did not observe a robust between-group difference in documented abstinence post treatment. As Figures 2 and 3 show, there is an increase in marijuana use from discharge to the 9 month follow up, that, while not returning to intake levels, is of significant concern. The lack of significant treatment condition differences may have resulted from low power to detect differences (EXP had greater rates of abstinence at each time point, particularly at 3 months), a more potent effect of the comparison treatment than expected (rates of abstinence appear good in both conditions compared to prior treatment studies), or simply a less potent intervention effect than expected. We suggest that all three of these contributed to the findings. First, the sample size was relatively small (n=36 and 33 per condition). Effect sizes for treatment on UA results and self reports were small (ds=.21 and .24 respectively), but power was adequate to detect only medium effects in these analyses. Second, the marijuana use outcomes for the comparison condition were good relative to those reported for other efficacious interventions (e.g., Dennis et al., 2004; Waldron et al., 2001). The CONTROL intervention included incentives for participation in counseling and twice weekly urine testing; systematically provided test results to parents; and provided weekly counseling and case management to parents. Although this condition was meant to serve as an “attention control” for the CM intervention, we expect that it was active and enhanced outcomes that would have been achieved with MET/CBT alone and might be considered an alternative model warranting future study. In particular, parents in the CONTROL condition may have responded to the urine drug testing results in a similar manner to parents in the EXP condition (i.e., withdrawal of privileges or other punishment delivered contingently following positive drug tests, rewards delivered contingently following negative drug tests). The likely tendency for at least some parents to respond in this way may have served to make outcomes more similar across conditions. Third, EXP lasted only 14 weeks. With adolescents who enroll in treatment primarily because it is required by their parents, school, or the legal system, return to substance use once these contingencies and consistent monitoring are removed would seem highly probable.
4.1 Parenting and psychopathology
Across psychopathology and parenting measures, the EXP condition tended to show better outcomes, with significant main effects of treatment condition on negative discipline and externalizing. However, the treatment × time effects were not significant on any scale, indicating that adolescents in both conditions improved on measures of internalizing and externalizing psychopathology, and parents in both conditions showed parenting improvements. Similar to our findings, most adolescent substance abuse treatment studies have reported significant reductions in conduct problems, with no treatment condition differences (Henggeler et al., 2006; Liddle et al., 2001; Waldron et al., 2001). Reasons for positive changes in both externalizing and parenting for both EXP and CONTROL youth might include active intervention components in the comparison condition, as discussed above.
Despite the lack of treatment condition × time interactions on psychopathology and parenting, the structural models reflected the unique impact of parenting on adolescent marijuana use. End of treatment differences in inconsistent discipline and poor monitoring predicted post treatment marijuana use, above and beyond the effects of treatment condition. For the reasons outlined above, the comparison condition may have been more active than anticipated in producing parenting improvements. Some (but not all) studies testing family interventions for adolescent substance abuse have assessed changes in family functioning, and most of those showed improvements over time in family functioning in all treatment conditions (Azrin et al., 2001; Waldron et al., 2001). There are reports of treatment condition effects on family variables, all showing effects based on youth reports (Liddle et al., 2009; Santisteban et al., 2003) or observational measures (Liddle et al., 2001), but not parent reports. However, we could find no examples of analyses linking changes in family functioning or parenting to changes in substance use outcomes, with the exception of Dishion et al. (2003) who reported that a preventive parenting intervention influenced adolescent substance use via its impact on parental monitoring. The main mechanism explored to date has been treatment adherence and/or therapist competence (Hogue et al., 2008). Identification of mechanisms is a crucial step in the development of effective interventions, and the adolescent substance abuse treatment field suffers from the same weaknesses noted by Kazdin (2007) in the larger psychosocial treatment outcome literature. Our findings highlight parenting as an important treatment mechanism, consistent with other research supporting the key role of parental monitoring on adolescent conduct problems (Lahey et al., 2008; Laird et al., 2008) and substance use (Clark et al., 2005; Dick et al., 2007; Kamon et al., 2006). Future studies might focus on isolating and testing different methods of prompting or training parental monitoring.
4.2 Limitations
Participation required a pretreatment acknowledgment that a parent or guardian would participate each week. Hence results generalize only to adolescents that meet such treatment conditions. Note however, we believe that with outreach efforts and flexible scheduling, many families are likely to have at least one parent or guardian who will agree to participate. In addition, participating adolescents were primarily Caucasian, 75% had two-parent participation, most had parents with relatively high levels of education, lived in small metropolitan or rural communities, and reported marijuana as their primary drug of abuse. Thus, the generalizability of the tested treatment models to other populations of adolescents and to other types of substance dependence is unknown. We are currently conducting a new trial in a more diverse, lower SES population in order to assess the generalizability of this treatment model.
We accepted into treatment 8 youth who reported regular marijuana use or who provided a THC positive urine drug test but who did not meet DSM criteria for marijuana abuse or dependence. We did not have the statistical power to sufficiently explore the interaction of diagnosis with treatment condition, however, youth with vs. without a diagnosis did not show significantly different during treatment abstinence (No DSM: Mean=7.8 weeks, SD=5.2 vs. DSM Abuse/Dependence: Mean=6.2 weeks, SD=5.2, p=.44). In addition, when removing the 8 youth with no DSM diagnosis from this comparison, the magnitude of the effect was almost identical, suggesting that the inclusion of these youth had no significant impact on the findings.
4.3 Conclusion and future directions
The finding that the systematic application of principles of reinforcement increased abstinence among treatment seeking adolescents provides important support for the further development of programs that utilize CM to enhance abstinence outcomes in the treatment of substance use disorders. However, despite this positive effect of CM, a significant percentage of youth do not achieve abstinence during treatment and many who do achieve abstinence relapse during the first 6 months post treatment. Thus, both the initial treatment period and the post treatment period remain important targets for enhancing outcomes. Alternative positive reinforcement programs (e.g., increased magnitude, use of variable schedules, longer duration, different types of reinforcers) merit investigation. Moreover, methods to further enhance the efficacy of parent interventions particularly targeting effective monitoring and discipline practices may lead to continued improvements in outcomes.
Acknowledgments
Role of Funding Source
This work was supported by NIDA grants DA15186 and T32-DA07242, NIAAA grant AA016917, and the Arkansas Biosciences Institute, the major research component of the Arkansas Master Tobacco Settlement. There was no involvement of the sponsor in study design; collection, analysis and interpretation of data; writing of the report; nor in the decision to submit the paper for publication.
We would like to thank the staff at the Treatment Research Center at the University of Vermont, especially Heath Rocha, as well as the participating families.
Footnotes
Contributors
Catherine Stanger and Alan Budney, Department of Psychiatry, University of Arkansas for Medical Sciences; Jody L. Kamon, University of Vermont, College of Medicine; Jeffrey D. Thostenson, Department of Biostatistics, University of Arkansas for Medical Sciences. Drs. Stanger and Budney designed the study, wrote the protocol, and wrote the manuscript. Dr. Kamon assisted with statistical analyses and writing the manuscript and supervised data management. Mr. Thostenson undertook the statistical analysis. All authors contributed to and have approved the final manuscript.
Conflict of Interest
None of the authors have financial ties with any for-profit enterprises mentioned in this manuscript or relating to this study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM, Rescorla LA. Manual for ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- Azrin NH, Donohue B, Besalel VA, Kogan ES, Acierno R. Youth drug abuse treatment: A controlled outcome study. Journal of Child & Adolescent Substance Abuse. 1994;3:1–16. [Google Scholar]
- Azrin NH, Donohue B, Teichner GA, Crum T, Howell J, De Cato LA. A Controlled Evaluation and Description of Individual-Cognitive Problem Solving and Family-Behavior Therapies in Dually-Diagnosed Conduct-Disordered and Substance-Dependent Youth. Journal of Child and Adolescent Substance Abuse. 2001;11(1):1–43. [Google Scholar]
- Budney AJ, Moore BA, Rocha HL, Higgins ST. Clinical trial of abstinence-based vouchers and cognitive-behavioral therapy for cannabis dependence. J Consult Clin Psychol. 2006;74(2):307–316. doi: 10.1037/0022-006X.4.2.307. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Roffman R, Stephens RS, Walker D. Marijuana dependence and its treatment. Addict Sci Clin Pract. 2007;4(1):4–16. doi: 10.1151/ascp07414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Easton CJ, Nich C, Hunkele KA, Neavins TM, Sinha R, Ford HL, Vitolo SA, Doebrick CA, Rounsaville BJ. The use of contingency management and motivational/skills-building therapy to treat young adults with marijuana dependence. J Consult Clin Psychol. 2006;74(5):955–966. doi: 10.1037/0022-006X.74.5.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark DB, Thatcher DL, Maisto SA. Supervisory neglect and adolescent alcohol use disorders: Effects on AUD onset and treatment outcome. Addict Behav. 2005;30(9):1737–1750. doi: 10.1016/j.addbeh.2005.07.017. [DOI] [PubMed] [Google Scholar]
- Compton WM, Pringle B. Services research on adolescent drug treatment. Commentary on “The cannabis youth treatment (CYT) study: Main findings from two randomized trials”. J Subst Abuse Treat. 2004;27:195–196. doi: 10.1016/j.jsat.2004.07.003. [DOI] [PubMed] [Google Scholar]
- Cornelius JR, Clark DB, Bukstein OG, Birmaher B, Salloum IM, Brown SA. Acute phase and five-year follow-up study of fluoxetine in adolescents with major depression and a comorbid substance use disorder: A review. Addict Behav. 2005;30(9):1824–1833. doi: 10.1016/j.addbeh.2005.07.007. [DOI] [PubMed] [Google Scholar]
- Dennis M, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, Liddle H, Titus JC, Kaminer Y, Webb C, Hamilton N, Funk R. The Cannabis youth treatment (CYT) study: Main findings from two randomized trials. J Subst Abuse Treat. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Dick DM, Viken R, Purcell S, Kaprio J, Pulkkinen L, Rose RJ. Parental monitoring moderates the importance of genetic and environmental influences on adolescent smoking. J Abnorm Psychol. 2007;116(1):213–218. doi: 10.1037/0021-843X.116.1.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, Kavanagh K. Intervening in Adolescent Problem Behavior: A Family-Centered Approach. New York, NY: Guilford Press; 2003. [Google Scholar]
- Dishion TJ, Kavanagh K, Veltman M, McCartney T, Soberman L, Stormshak EA. Family Management Curriculum V2.0: Leader’s Guide. Eugene, OR: Child and Family Center Publications; 2003. [Google Scholar]
- Henggeler SW, Chapman JE, Rowland MD, Halliday-Boykins CA, Randall J, Shackelford J, Schoenwald SK. Statewide adoption and initial implementation of contingency management for substance-abusing adolescents. J Consult Clin Psychol. 2008;76(4):556–567. doi: 10.1037/0022-006X.76.4.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henggeler SW, Clingempeel WG, Brondino MJ, Pickrel SG. Four-year follow-up of multisystemic therapy with substance-abusing and substance-dependent juvenile offenders. J Am Acad Child Adolesc Psychiatry. 2002;41(7):868–874. doi: 10.1097/00004583-200207000-00021. [DOI] [PubMed] [Google Scholar]
- Henggeler SW, Halliday-Boykins CA, Cunningham PB, Randall J, Shapiro SB, Chapman JE. Juvenile drug court: Enhancing outcomes by integrating evidence-based treatments. J Consult Clin Psychol. 2006;74(1):42–54. doi: 10.1037/0022-006X.74.1.42. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Budney AJ, Bickel WK, Foerg F, Donham R, Badger G. Incentives improve outcome in outpatient behavioral treatment of cocaine dependence. Arch Gen Psychiatry. 1994;54:568–576. doi: 10.1001/archpsyc.1994.03950070060011. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Silverman K, Heil SH. Contingency management in substance abuse treatment. New York, NY: The Guilford Press; 2008. [Google Scholar]
- Hogue A, Henderson CE, Dauber S, Barajas PC, Fried A, Liddle HA. Treatment adherence, competence, and outcome in individual and family therapy for adolescent behavior problems. J Consult Clin Psychol. 2008;76(4):544–555. doi: 10.1037/0022-006X.76.4.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB. Four Factor Index of Social Status. Department of Sociology, Yale University; 1975. [Google Scholar]
- Hudziak JJ, Copeland W, Stanger C, Wadsworth M. Screening for DSM-IV externalizing disorders with the Child Behavior Checklist: A receiver-operating characteristic analysis. J Child Psychol Psychiatry. 2004;45(7):1299–1307. doi: 10.1111/j.1469-7610.2004.00314.x. [DOI] [PubMed] [Google Scholar]
- Kadden RM, Litt MD, Kabela-Cormier E, Petry NM. Abstinence rates following behavioral treatments for marijuana dependence. Addict Behav. 2007;32(6):1220–1236. doi: 10.1016/j.addbeh.2006.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamon JL, Budney AJ, Stanger C. A contingency management intervention for adolescent marijuana abuse and conduct problems. J Am Acad Child Adolesc Psychiatry. 2005;44(6):513–521. doi: 10.1097/01.chi.0000159949.82759.64. [DOI] [PubMed] [Google Scholar]
- Kamon JL, Stanger C, Budney AJ, Dumenci L. Relations between parent and adolescent problems among adolescents presenting for family-based substance abuse treatment. Drug Alcohol Depend. 2006;85(3):244–254. doi: 10.1016/j.drugalcdep.2006.05.015. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annu Rev Clin Psychol. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Duhig AM, McKee SA, McMahon TJ, Liss T, McFetridge A, Cavallo DA. Contingency management for smoking cessation in adolescent smokers. Exp Clin Psychopharmacol. 2006;14(3):306–310. doi: 10.1037/1064-1297.14.3.306. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Van Hulle CA, D’Onofrio BM, Rodgers JL, Waldman ID. Is parental knowledge of their adolescent offspring’s whereabouts and peer associations spuriously associated with offspring delinquency? J Abnorm Child Psychol. 2008;36(6):807–823. doi: 10.1007/s10802-008-9214-z. [DOI] [PubMed] [Google Scholar]
- Laird RD, Criss MM, Pettit GS, Dodge KA, Bates JE. Parents’ monitoring knowledge attenuates the link between antisocial friends and adolescent delinquent behavior. J Abnorm Child Psychol. 2008;36(3):299–310. doi: 10.1007/s10802-007-9178-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liddle HA, Dakof GA, Parker K, Diamond GS, Barrett K, Tejeda M. Multidimensional family therapy for adolescent drug abuse: Results of a randomized clinical trial. Am J Drug Alcohol Abuse. 2001;27(4):651–688. doi: 10.1081/ada-100107661. [DOI] [PubMed] [Google Scholar]
- Liddle HA, Rowe CL, Dakof GA, Henderson CE, Greenbaum PE. Multidimensional family therapy for young adolescent substance abuse: twelve-month outcomes of a randomized controlled trial. J Consult Clin Psychol. 2009;77(1):12–25. doi: 10.1037/a0014160. [DOI] [PubMed] [Google Scholar]
- Lott DC, Jencius S. Effectiveness of very low-cost contingency management in a community adolescent treatment program. Drug Alcohol Depend. 2009;102(1–3):162–165. doi: 10.1016/j.drugalcdep.2009.01.010. [DOI] [PubMed] [Google Scholar]
- McCallum T. Drugs: Parents and young people. Sydney: Health Education Unit, the University of Sydney; 1994. [Google Scholar]
- Petry NM, Martin B, Cooney JL, Kranzler HR. Give them prizes, and they will come: Contingency management for treatment of alcohol dependence. J Consult Clin Psychol. 2000;68:250–257. doi: 10.1037//0022-006x.68.2.250. [DOI] [PubMed] [Google Scholar]
- Petry NM, Simic F. Recent advances in the dissemination of contingency management techniques: Clinical and research perspectives. J Subst Abuse Treat. 2002;23:81–86. doi: 10.1016/s0740-5472(02)00251-9. [DOI] [PubMed] [Google Scholar]
- Randall J, Cunningham PB. Multisystemic therapy: A treatment for violent substance-abusing and substance-dependent juvenile offenders. Addict Behav. 2003;28:1731–1739. doi: 10.1016/j.addbeh.2003.08.045. [DOI] [PubMed] [Google Scholar]
- Rey JM, Martin A, Krabman P. Is the party over? Cannabis and juvenile psychiatric disorder: The past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(10):1194–1205. doi: 10.1097/01.chi.0000135623.12843.60. [DOI] [PubMed] [Google Scholar]
- Riggs PD, Hall SK, Mikulich-Gilbertson SK, Lohman M, Kayser A. A randomized controlled trial of pemoline for attention-deficit/hyperactivity disorder in substance-abusing adolescents. J Am Acad Child Adolesc Psychiatry. 2004;43(4):420–429. doi: 10.1097/00004583-200404000-00008. [DOI] [PubMed] [Google Scholar]
- Sampl S, Kadden R. Motivational Enhancement Therapy and Cognitive Behavioral Therapy for Adolescent Cannabis Users: 5 Sessions. Vol. 1. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 2001. [Google Scholar]
- Santisteban DA, Coatsworth JD, Perez-Vidal A, Kurines WM, Schwartz SJ, LaPerriere A, Szapocznik J. Efficacy of brief strategic family therapy in modifying hispanic adolescent behavior problems and substance abuse. Journal of Family Psychology. 2003;17(1):121–133. doi: 10.1037/0893-3200.17.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: Psychosocial and biological methods. Human Press; Totowa, NJ: 1992. pp. 41–72. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Treatment Episode Data Set (TEDS), 2006. Rockville, MD: United States Department of Health and Human Services; 2008. [Google Scholar]
- Tims FM, Dennis ML, Hamilton N, Buchan BJ, Diamond G, Funk R, Brantley LB. Characteristics and problems of 600 adolescent cannabis abusers in outpatient treatment. Addiction. 2002;97(Suppl 1):46–57. doi: 10.1046/j.1360-0443.97.s01.7.x. [DOI] [PubMed] [Google Scholar]
- Waldron HB, Slesnick N, Brody JL, Turner CW, Peterson TR. Treatment outcomes for adolescent substance abuse at 4- and 7-month assessments. J Consult Clin Psychol. 2001;69:802–813. [PubMed] [Google Scholar]
- Waldron HB, Turner CW. Evidence-based psychosocial treatments for adolescent substance abuse. J Clin Child Adolesc Psychol. 2008;37(1):238–261. doi: 10.1080/15374410701820133. [DOI] [PubMed] [Google Scholar]
- Webb CPM, Scudder M, Kaminer Y, Kadden R. The Motivational Enhancement Therapy and Cognitive Behavioral Therapy for Adolescent Cannabis Users. Vol. 2. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 2001. [Google Scholar]
- Wells KC, Epstein JN, Hinshaw SP, Conners CK, Klaric J, Abikoff HB, Abramowitz A, Arnold LE, Elliott G, Greenhill LI, Hechtman L, Hoza B, Jensen PS, March JS, Pelham W, Pfiffner L, Severe J, Swanson JM, Vitiello B, Wigal T. Parenting and family stress treatment outcomes in Attention Deficit Hyperactivity Disorder (ADHD): An empirical analysis in the MTA study. J Abnorm Child Psychol. 2000;28:543–553. doi: 10.1023/a:1005131131159. [DOI] [PubMed] [Google Scholar]