Abstract
Background
Older adults who cease driving have poorer health than those who continue to drive. However, it is unclear whether the transition to driving cessation itself results in health declines or whether driving cessation subsequently exacerbates health declines over time.
Methods
The current study addresses these questions using multilevel modeling among 690 older adults from the Advanced Cognitive Training for Independent and Vital Elderly study. Driving status and health, as indicated by the SF-36 questionnaire, self-rated health, physical performance (Turn 360° Test), and depressive symptoms were assessed at baseline and at 1-, 2-, 3-, and 5-year follow-up visits.
Results
The transition to driving cessation was accompanied by significant declines in physical and social functioning, physical performance, and physical role (ps < .05). Health declines after driving cessation were steeper for general health.
Conclusions
The transition to driving cessation is associated with health declines for older adults as measured by several indicators. Additionally, general health declines more sharply following driving cessation. These findings highlight the importance of interventions to sustain driving mobility among older adults.
Keywords: Older drivers, Driving cessation, Health
FOR older adults, remaining an active driver is important for maintaining independence and well-being. Many studies have shown that there are negative social and health consequences to driving cessation among older adults (1–5). As examples, Freeman and colleagues found that nondrivers were five times more likely to enter long-term care facilities (1). Edwards and colleagues demonstrated that older adults who ceased driving were four to six times more likely to die over the subsequent 3 years (4). Considered with prior research, these findings raise the question of whether or not there is a direct relationship between driving status and health for older adults. Specifically, this article addresses whether the transition of driving cessation is accompanied and/or followed by precipitous declines in health among older adults.
It is common for older adults to decide to cease driving due to poor health. Compared with drivers, older nondrivers report having more medical conditions as well as poorer self-ratings of health (6–8). Older adults who have ceased driving tend to be older, are more likely to be women, and usually have lower levels of education as well (7–11). Self-rated health and performance-based physical measures are predictors of subsequent driving status (9–11). Furthermore, older adults who have ceased driving are more likely to report physical difficulties (6–8). Thus, poor health is clearly associated with and often precedes driving cessation among older adults.
What remains unclear is whether or not the transition to driving cessation itself results in further health declines for older adults. While it may be that older adults who cease driving are already predisposed to declines in health, it could also be that ceasing driving further exacerbates health declines over time. Prior research has documented that when older adults cease driving, they are more likely to experience increased social isolation, decreased activity, increased depression, and decreased sense of control, all of which could negatively impact subsequent health (2,3,5,12). Interestingly, the increased social isolation and depression are not ameliorated by access to alternative transportation (5,13). It may also be the case that ceasing driving limits access to health care, which then hastens decline.
The present analyses examined data from participants in the control group of the Advanced Cognitive Training for Independent and Vital Elderly (ACTIVE) clinical trial (14). The effect of driving cessation on health trajectories was examined at the transition to cessation as well as subsequent to cessation.
METHODS
Participants
Community-dwelling adults aged 65 years and older with adequate vision (≥ 20/50 or better), relatively good health, and no evidence of substantial cognitive decline (Mini-Mental State Examination score ≥ 23) or communicative difficulties were recruited to participate in the ACTIVE study. The ACTIVE study investigated the impact of three cognitive interventions upon the subsequent functioning of older adults across a 5-year period and is detailed by Jobe and colleagues (14). We utilized data from the control group. Participants who were current or former drivers at baseline were included in the analysis (N = 690). These participants were 73.6% women and 71.8% white, with a mean baseline age of 74.1 years (SD = 6.1). Years of education ranged from sixth grade to the doctoral level, with an average level of 13.4 years (SD = 2.7), corresponding to “some college or vocational school.”
Measures
Driving status.—
The Driving Habits Questionnaire (DHQ), an 18-item measure of driving behaviors, was used to determine driving status (15,16). The DHQ ascertains whether respondents are current drivers, defined as “someone who has driven within the past 12 months and would do so today if they needed to.” Nondrivers were asked when and why they stopped driving. A total of 37 participants (5.3%) reported stopping driving at some point during the 5-year period of the study. Fifty-nine participants (8.6%) were former drivers who reported driving cessation dates before the baseline assessment, and 594 participants (86.0%) reported driving throughout the 5-year study period.
General health and functioning.—
The SF-36 questionnaire was used to assess health (17). Four of the eight subscales were used in the current analyses: physical functioning, physical role, social functioning, and general health. These subscales best represent the domains of functioning that have been implicated by prior research as correlates of driving cessation. The physical functioning composite indicates the extent to which persons are limited in their physical activities due to health, while physical role indicates the extent to which respondents experience problems with work or other daily activities as a result of their physical health. The social functioning composite quantifies the extent to which social activities are affected by either physical or emotional difficulties. The general health composite reflects the respondents’ ratings of their health in general compared with others and with regard to expectations for the future. Each subscale ranges from 0 to 100 with higher scores reflecting better health and functioning.
Self-rated health.—
Participants rated their health on a 5-point Likert scale ranging from excellent—1 to poor—5.
Physical performance.—
Physical performance was measured by the Turn 360° Test (18). Participants were asked to stand and turn in two complete circles. The number of steps taken to complete each circle was recorded such that fewer steps reflected better performance. The average number of steps across both turns was used in the analyses.
Depressive symptoms.—
The 12-item short form Center for Epidemiological Studies-Depression (CES-D) scale (19) was used to quantify the frequency of depressive symptoms experienced across the prior week. Participants rated the frequency with which they experienced 12 symptoms such as feeling down or blue on a scale of 0–3, with higher total scores reflecting more depressive symptoms.
Procedure
Telephone interviews were conducted to confirm eligibility. Participants initially underwent in-person screening and baseline visits, during which tests and questionnaires were administered. Participants were then randomly assigned to a control group or a cognitive training group; a total of 2,802 individuals were randomized with 698 to the control condition. Follow-up visits were conducted 1, 2, 3, and 5 years after the baseline visit, and information about driving and health was obtained at these visits. The ACTIVE study was conducted in compliance with the ethical rules for human experimentation set forth in the Declaration of Helsinki and was approved by institutional review boards at all study sites.
Statistical Analyses
The effects of driving cessation on health across time were estimated and examined using multilevel growth curve analyses (20) as conducted using SAS Proc Mixed (21). Similar transition analyses have been previously conducted examining spouse caregiver well-being before, at, and after nursing home placement by Gaugler and colleagues (22) and evaluating older adults’ mobility before, at, and after hospitalization by Brown and colleagues (23). In our analyses, there were three time-invariant covariates (age at baseline, sex, and years of education), three time-varying predictor variables (time, driving status, and time since driving cessation), and seven outcome variables (physical functioning, physical role, social functioning, physical performance, general health, self-rated health, and depressive symptoms). Age, sex, and education level were chosen as covariates in that these factors are related to rates of driving cessation (7–11).
Multilevel analytic models were constructed with three time-varying predictor variables for each dependent variable. “Time” was calculated as the number of months from baseline to the date of each assessment for each participant. The coefficient for this time variable accounted for general linear trends in health trajectories across time. “Driving status” was coded dichotomously as 1 at all time points for those who remained drivers throughout the study and as 0 at all time points for those who ceased driving prior to the study. For those who ceased driving during the course of the study, their status was coded as 1 at time points in which they were driving and as 0 for all time points after they reported ceasing driving. The coefficient for this effect is of primary interest and indicates the amount of abrupt change that occurs at the time of driving cessation. “Time since driving cessation” was set to 0 for all assessments before driving cessation and was set to the number of months elapsed between each assessment and the date at which the participant reported driving cessation. This variable was set to 0 months for all assessments for those participants who continued to drive throughout the entire study period. The coefficient for this time since driving cessation variable indicated whether the change in health across time after driving cessation was different from the rate of change before driving cessation.
Random effects were estimated for the intercept and for the time variable, with a nonzero covariance allowed between these two random effects. Age at baseline, sex, and number of years of education were included as time-invariant covariates in all models reported in this article. All models were estimated using full maximum likelihood estimation methods as provided by SAS Proc Mixed (21).
RESULTS
Time
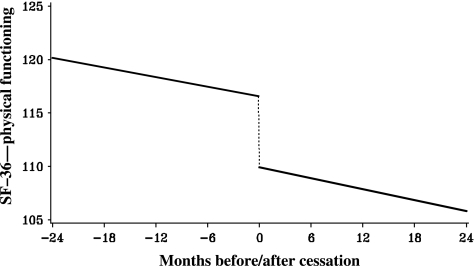
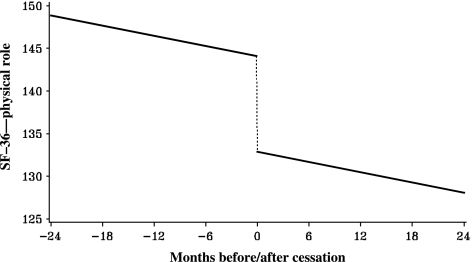
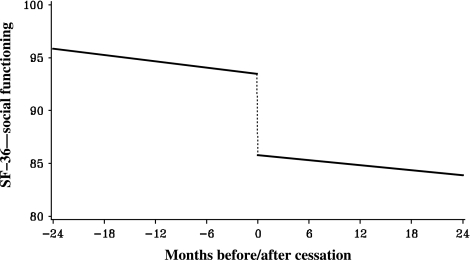
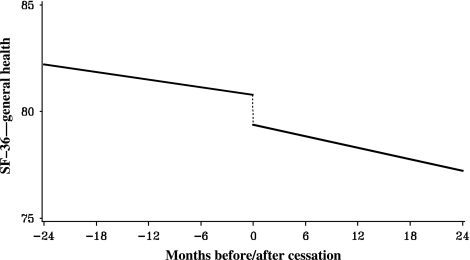
The results of multilevel growth curve analyses are summarized in Table 1 and depicted with model-based prototypical trajectories in Figures 1–4. Across all the outcome variables, there were significant effects for time. As would be expected in an older adult population, overall health and physical functioning tended to decline across the 5-year period.
Table 1.
Results of Multilevel Growth Curve Analyses Examining Effects of Driving Cessation on Health, Physical, and Social Functioning
| Effect | Estimate | Standard Error | t | Degrees of Freedom | p Value |
| Physical functioning | |||||
| Intercept | 113.51 | 12.62 | 8.99 | 685 | <.001 |
| Time | −0.15 | 0.01 | −11.01 | 605 | <.001 |
| Driving status | 6.66 | 2.03 | 3.28 | 1387 | .001 |
| Time since cessation | −0.02 | 0.01 | −1.37 | 1387 | .170 |
| Physical role | |||||
| Intercept | 137.69 | 18.25 | 7.54 | 684 | <.001 |
| Time | −0.20 | 0.03 | −7.06 | 603 | <.001 |
| Driving status | 11.17 | 3.94 | 2.84 | 1384 | .005 |
| Time since cessation | −0.0001 | 0.02 | −0.01 | 1384 | .996 |
| Social functioning | |||||
| Intercept | 88.18 | 9.64 | 9.14 | 685 | <.001 |
| Time | −0.10 | 0.02 | −6.15 | 604 | <.001 |
| Driving status | 7.68 | 2.20 | 3.49 | 1388 | <.001 |
| Time since cessation | 0.02 | 0.01 | 1.41 | 1388 | .159 |
| Physical performance | |||||
| Intercept | −0.003 | 0.95 | 0.00 | 678 | .998 |
| Time | 0.01 | 0.002 | 6.27 | 491 | <.001 |
| Driving status | −0.81 | 0.23 | −3.53 | 698 | <.001 |
| Time since cessation | −0.002 | 0.001 | −1.76 | 698 | .078 |
| General health | |||||
| Intercept | 80.83 | 9.34 | 8.65 | 685 | <.001 |
| Time | −0.06 | 0.01 | −4.86 | 601 | <.001 |
| Driving status | 1.39 | 1.74 | 0.80 | 1383 | .425 |
| Time since cessation | −0.03 | 0.01 | −2.97 | 1383 | .003 |
| Self-rated health | |||||
| Intercept | 2.62 | 0.47 | 5.59 | 684 | <.001 |
| Time | 0.002 | 0.001 | 3.24 | 565 | .001 |
| Driving status | −0.19 | 0.10 | −1.80 | 1193 | .072 |
| Time since cessation | 0.001 | 0.001 | 1.35 | 1193 | .176 |
| Depressive symptoms | |||||
| Intercept | 3.42 | 2.43 | 1.41 | 684 | .160 |
| Time | 0.01 | 0.004 | 2.05 | 565 | .041 |
| Driving status | −0.39 | 0.52 | −0.75 | 1192 | .453 |
| Time since cessation | 0.005 | 0.003 | 1.52 | 1192 | .128 |
Note: The above models controlled for baseline age, sex, and years of education.
Figure 1.
Effects of driving cessation on physical functioning.
Figure 2.
Effects of driving cessation on limitations in work or other daily activities due to physical health.
Figure 3.
Effects of driving cessation on social functioning.
Figure 4.
Effects of driving cessation on general health.
Driving Status
Interestingly, there were also significant effects of driving status, indicating that at the point of driving cessation there were significant declines across most of the outcome variables, with the exceptions of SF-36 general health, self-rated health, and depressive symptoms. As can be seen from Table 1 and Figures 1–4, after adjusting for age, sex, and education, the transition to driving cessation was accompanied by a 6.7-point drop in physical functioning, an almost 12-point decline in performance of work or other daily activities (physical role), and an almost 8-point decrease in social functioning.
Time Since Driving Cessation
Health trajectories after driving cessation were significantly steeper in decline only for SF-36 general health. Otherwise, the linear rate of change in health trajectories did not differ significantly from before to after driving cessation across the follow-up period.
DISCUSSION
Because it is not possible to conduct an experiment and randomize older adults to driving cessation, it is difficult to discern the causal relationship between driving status and health. However, the analytic techniques used in this article allow us to examine health across the entire 5-year study period (time), at the point of driving cessation (driving status), and subsequent to driving cessation (time since driving cessation) in order to better understand the temporal relationships between these variables. These analyses indicate that among older adults, driving cessation is accompanied by significant declines in physical and social functioning (Figures 1–3). Older adults who cease driving are likely to experience accompanying increased limitations in physical functioning, increased difficulties in their daily activities as a result of physical health problems, and increased interference in social activities.
When examining health outcomes subsequent to driving cessation, we found general health tended to decline more rapidly after driving cessation (Figure 4). Although trajectories of physical and social functioning did not decline more rapidly subsequent to driving cessation, there also was no recovery or rebounding from the declines in functioning that were experienced at the transition to driving cessation. There was also a trend for older adults who ceased driving to show steeper rates of decline in physical performance subsequent to the transition. This difference was significant in base models that did not adjust for covariates. It may be that significantly steeper declines in physical performance subsequent to driving cessation, as well as in other health domains, would emerge over longer periods of time.
As previously mentioned, other studies have indicated that increased depression and social isolation are not ameliorated by the capacity to use public transportation (5,13). Thus, it is likely that the health declines associated with driving cessation observed in these analyses would also not be improved by access to alternative transportation. Overall, these and prior results indicate that maintained driving mobility is important for health and well-being among older adults.
Unlike prior studies that have found increased depression accompanying and subsequent to driving cessation (3,24), these results did not indicate significant increases in depressive symptoms at the point of driving cessation or following driving cessation. We did, however, find increased depression across time overall (p = .04). These prior studies differ in that they examined depression using the 20-item CES-D among older adults who were baseline drivers who ceased driving across the subsequent 2- to 3-year period. The present findings could be due to less sensitivity of the short form of the CES-D. Different prevalence rates of depression across study samples also could account for these differences.
Another limitation of the present analyses is that the current sample included only relatively healthy, community-dwelling older adults without significant declines in functional abilities at baseline. It is not certain whether the same results would be found among the broader spectrum of older adults in the population. At the same time, the significant decreases in health and functioning experienced in the sample at the transition to driving cessation are striking given their baseline state of health.
In summary, the results of these analyses indicate that the transition to driving cessation is accompanied by precipitous health declines for older adults, particularly with regard to social and physical functioning as well as physical performance. However, when trajectories are examined across time, driving cessation does not appear to hasten the rate of decline in physical or social functioning after cessation. On the other hand, the rate of general health decline may be exacerbated subsequent to driving cessation.
The implications of these findings as well as prior research (1,4,12) are that driving is clearly an instrumental activity of daily living important for older adults’ maintained health and well-being. Further research is needed to determine whether prolonging driving mobility among older adults could potentially avert precipitous declines in health and functioning. Fortunately, recent attempts to enhance and prolong older adults’ driving mobility through physical and cognitive interventions have been successful in enhancing on-road performance (25,26) and maintaining driving mobility (27). Interestingly, one of these interventions, cognitive speed of processing training, has also been found to result in maintained health-related quality of life (28). Although more research is needed, the present results highlight the importance and potential impact of interventions to prolong driving mobility on older adults’ health and well-being.
FUNDING
The ACTIVE study was supported by grants from the National Institute on Aging and the National Institute of Nursing Research to Hebrew Senior Life (U01 NR04507), Indiana University School of Medicine (U01 NR04508), Johns Hopkins University (U01AG14260), New England Research Institutes (U01 AG14282), Pennsylvania State University (U01 AG14263), University of Alabama at Birmingham (U01 AG14289), and University of Florida (U01AG14276). Additionally, these analyses were supported by the National Institute on Aging, Cognitive Training Gains and Mobility Outcomes in ACTIVE (5 R03 AG23078-02), Karlene Ball, PhD, (PI).
Acknowledgments
We would like to acknowledge and thank the entire ACTIVE team. The ACTIVE principal investigators include Hebrew Senior Life—John N. Morris, PhD, Indiana University School of Medicine—Frederick W. Unverzagt, PhD, Johns Hopkins University—George W. Rebok, PhD, New England Research Institutes (Data Coordinating Center)—Sharon L. Tennstedt, PhD, Pennsylvania State University—Sherry L. Willis PhD, University of Alabama at Birmingham—Karlene Ball PhD, University of Florida/Wayne State University—Michael Marsiske, PhD, National Institutes of Health—Kathy Mann-Koepke, PhD, National Institute of Nursing Research and Jonathan King, PhD, National Institute on Aging.
References
- 1.Freeman EE, Gange SJ, Munoz B, et al. Driving status and risk of entry into long-term care in older adults. Am J Public Health. 2006;96(7):1254–1259. doi: 10.2105/AJPH.2005.069146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marottoli RA, Mendes de Leon CF, Glass TA, et al. Driving cessation and increased depressive symptoms: prospective evidence from the New Haven EPESE. Established Populations for Epidemiologic Studies of the Elderly. J Am Geriatr Soc. 1997;45:202–206. doi: 10.1111/j.1532-5415.1997.tb04508.x. [DOI] [PubMed] [Google Scholar]
- 3.Windsor TD, Anstey KJ, Butterworth P, et al. The role of perceived control in explaining depressive symptoms associated with driving cessation in a longitudinal study. Gerontologist. 2007;2:215–223. doi: 10.1093/geront/47.2.215. [DOI] [PubMed] [Google Scholar]
- 4.Edwards JD, Ross LA, Perkins M. Driving status and three-year mortality among community-dwelling older. J Gerontol A Biol Sci Med Sci. 2009;64A:300–305. doi: 10.1093/gerona/gln019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mezuk B, Rebok GW. Social integration and social support among adults following driving cessation. J Gerontol B Psychol Sci Soc Sci. 2008;63B:S298–S303. doi: 10.1093/geronb/63.5.s298. [DOI] [PubMed] [Google Scholar]
- 6.Campbell MK, Bush TL, Hale WE. Medical conditions associated with driving cessation in community-dwelling, ambulatory elders. J Gerontol B Psychol Sci Soc Sci. 1993;48:S230–S234. doi: 10.1093/geronj/48.4.s230. [DOI] [PubMed] [Google Scholar]
- 7.Jette AM, Branch LG. A ten-year follow up of driving patterns among the community dwelling elderly. Hum Factors. 1992;34:25–31. doi: 10.1177/001872089203400104. [DOI] [PubMed] [Google Scholar]
- 8.Marottoli RA, Ostfeld AM, Merrill SS, et al. Driving cessation and changes in mileage driven among elderly individuals. J Gerontol B Psychol Sci Soc Sci. 1993;48:S255–S260. doi: 10.1093/geronj/48.5.s255. [DOI] [PubMed] [Google Scholar]
- 9.Dellinger AM, Sehgal M, Sleet DA, et al. Driving cessation: what former drivers tell us. J Am Geriatr Soc. 2001;49:431–435. doi: 10.1046/j.1532-5415.2001.49087.x. [DOI] [PubMed] [Google Scholar]
- 10.Campbell MK, Bush TL, Hale WE. Medical conditions associated with driving cessation in community-dwelling, ambulatory elders. J Gerontol. 1993;48:S230–S234. doi: 10.1093/geronj/48.4.s230. [DOI] [PubMed] [Google Scholar]
- 11.O’Neill D, Bruce I, Kirby M, et al. Older drivers, driving practices and health issues. Clin Gerontol. 2000;22(1):47–55. [Google Scholar]
- 12.Marottoli RA, Mendes de Leon CF, Glass TA, et al. Consequences of driving cessation: decreased out-of-home activity levels. J Gerontol B Psychol Sci Soc Sci. 2000;55:S334–S340. doi: 10.1093/geronb/55.6.s334. [DOI] [PubMed] [Google Scholar]
- 13.Fonda SJ, Wallace RB, Herzog AR. Changes in driving patterns and worsening depressive symptoms among older adults. J Gerontol B Psychol Sci Soc Sci. 2001;56B(6):S343–S351. doi: 10.1093/geronb/56.6.s343. [DOI] [PubMed] [Google Scholar]
- 14.Jobe JB, Smith DM, Ball KK, et al. ACTIVE: a cognitive intervention trial to promote independence in older adults. Control Clin Trials. 2001;22(4):453–479. doi: 10.1016/s0197-2456(01)00139-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Owsley C, Stalvey B, Wells J, et al. Older drivers and cataract: driving habits and crash risk. J Gerontol A Biol Sci Med Sci. 1999;54A(4):M203–M211. doi: 10.1093/gerona/54.4.m203. [DOI] [PubMed] [Google Scholar]
- 16.Stalvey BT, Owsley C, Sloane ME, et al. The Life Space Questionnaire: a measure of the extent of mobility of older adults. J Appl Gerontol. 1999;18(4):460–478. [Google Scholar]
- 17.Ware JE, Jr, Sherbourne CD. The MOS 36-item short form health survey (SF-36) I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 18.Steinhagen-Thiessen E, Borchelt M. Morbidity, medication, and functional limitations in very old age. In: Baltes PB, Mayer KU, editors. The Berlin Aging Study: Aging from 70 to 100. New York, NY: Cambridge University Press; 1999. pp. 131–166. [Google Scholar]
- 19.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 20.Singer JD, Willett JB. Applied Longitudinal Data Analysis. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 21.Littell RC, Milliken GA, Stroup WW, et al. SAS for Mixed Models. 2nd ed. Cary, NC: SAS Institute; 2006. [Google Scholar]
- 22.Gaugler JE, Roth DL, Haley WE, et al. Can counseling and support reduce burden and depressive symptoms in caregivers of people with Alzehimer’s disease during the transition to institutionalization? Results from the New York University caregiver intervention study. J Am Geriatr Soc. 2008;56:421–428. doi: 10.1111/j.1532-5415.2007.01593.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brown CJ, Roth DL, Allman RM. Trajectories of life-space mobility after hospitalization. Ann Intern Med. 2009;150:372–378. doi: 10.7326/0003-4819-150-6-200903170-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ragland DR, Satariano WA, MacLeod KE. Driving cessation and increased depressive symptoms. J Gerontol A Biol Sci Med Sci. 2005;60A(3):M399–M405. doi: 10.1093/gerona/60.3.399. [DOI] [PubMed] [Google Scholar]
- 25.Marottoli RA, Allore H, Araujo KLB, et al. A randomized trial of a physical conditioning program to enhance the driving performance of older persons. J Gen Intern Med. 2007;22:590–597. doi: 10.1007/s11606-007-0134-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Roenker DL, Cissell GM, Ball KK, et al. Speed-of-processing and driving simulator training result in improved driving performance. Hum Factors. 2003;45(2):218–233. doi: 10.1518/hfes.45.2.218.27241. [DOI] [PubMed] [Google Scholar]
- 27.Edwards JD, Myers C, Ross LA. The longitudinal impact of speed of processing training upon subsequent mobility of older drivers. Gerontologist. 2009;49:485–494. doi: 10.1093/geront/gnp042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wolinsky FD, Unverzagt FW, Smith DM, et al. The ACTIVE cognitive training trial and health-related quality of life: protection that lasts for 5 years. J Gerontol A Biol Sci Med Sci. 2006;61:1324–1329. doi: 10.1093/gerona/61.12.1324. [DOI] [PubMed] [Google Scholar]