The case
Sara is a 41-year-old secretary in an autobody shop who comes to see you for evaluation of intermittent episodes of wheeze and shortness of breath that have progressed over the past 2 years. She feels that she has more “colds” than her workplace colleague, each of which lasts for 2–3 weeks, with persistent cough and dyspnea. She had wheezing and allergy symptoms in childhood, and her mother and 1 cousin have confirmed asthma. Over the past 6 months, she has noticed that because of her dyspnea, she is unable to keep up with her partner when they go salsa dancing. She is otherwise well and is taking no medications. She smokes a half package of cigarettes daily and has done so for 20 years.
Sara states that she has never received a diagnosis of asthma. However, because she often gets a stuffy nose, she has wondered if she has allergies. Her mother has told her that she had eczema as a baby, and she remembers having itchy, red rashes when she was younger. She wakes up a couple of times a week because of coughing, but she can generally get back to sleep after she coughs up some phlegm.
The first step in managing asthma is to make the correct diagnosis. Asthma may mimic other common conditions and may be either overdiagnosed1 or underdiagnosed.2 After an appropriate history has been obtained and a physical examination performed, the recommended diagnostic testing methods include spirometry (preferred), serial peak flow measurements and provocational challenges.
Asthma is the most common chronic respiratory disease in Canada, affecting about 2.2 million adults and 0.8 million children.3–5 Poor asthma control imposes a significant burden on the health care system,6,7 with the annual direct and in -direct costs estimated at between $504 million and $648 million in Canada.8 However, despite the significant expenditure of health care resources on people with asthma, as well as decades of improvements in diagnosis and treatment and regular updates of evidence-based clinical practice guidelines, asthma control at the population level remains suboptimal.6,7
Canadian guidelines for the diagnosis and treatment of asthma have existed since 1989 and were most recently updated in 2003. In this series, we are using case-based examples to highlight recent changes in recommendations for asthma management and to highlight practical aspects of diagnosis and treatment. The case used here focuses on the diagnosis of asthma in adults.
The presence of certain key symptoms may suggest the presence of asthma, but can also result from airway inflammation alone, from chronic rather than reversible airflow limitation, or from other respiratory and nonrespiratory conditions. Moreover, asthma symptoms correlate poorly with abnormalities of lung function9 and airway inflammation,10,11 and thus in isolation may suggest a less severe form of the disease than is actually present. Although many clinicians diagnose asthma on the basis of a trial of therapy, objective measurements are necessary to confirm the clinical diagnosis. Validated questionnaires may be an option in settings where objective testing is unavailable.12
Asthma is an inflammatory disease13 associated with symptoms resulting from abnormalities of airway function, in particular wide, short-term variations in airflow resistance in the intrapulmonary airways. Thus, a conclusive diagnosis of asthma is based on tests designed to detect rapid changes in the forced expiratory volume in 1 second (FEV1) or peak expiratory flow. Although this review focuses particularly on diagnosis, these tests can also be used to assess asthma control and as an aid in optimizing chronic therapy.
The chronic inflammation of asthma is associated with airway hyperresponsiveness that leads to recurrent symptoms, yet lung function may nevertheless remain normal. Identification of airway hyperresponsiveness thus has clinical value, particularly in the diagnosis of asthma in people with normal spirometry results or with symptoms uncharacteristic of asthma. Airway hyperresponsiveness is usually measured using direct stimuli, such as methacholine or histamine, that act by stimulating specific receptors on the bronchial smooth muscle to cause contraction and narrowing of the airways.
The inflammation associated with asthma is characteristically eosinophilic. Measurement of sputum eosinophilia has been proposed for clinical use in the diagnosis of asthma. However, some patients with this condition have neutrophilic inflammation, whereas, conversely, some patients without asthma have eosinophilic inflammation.
Sources of information
We identified studies for potential inclusion in this literature review using several search strategies. The main source of studies was the “Asthma and Wheez*” register of the Cochrane Airways Group, which was originally created through a comprehensive search of EMBASE, MEDLINE and CINAHL. We searched all of the register’s original research studies and reviews using the following terms: “diagnos*” or “sensitiv*” or “test*” or “challenge” or “examination” or “accuracy.” The Asthma and Wheez* register includes studies published in foreign languages. The current review encompasses records published in or added to the register between 2005 and June 2008.
We also reviewed several asthma guidelines, specifically the Canadian consensus guidelines of 199913 and 2003,14 the 2008 British Thoracic Society – Scottish Intercollegiate Guidelines Network guidelines,15 the American College of Chest Physicians’ cough guidelines,16 the National Heart, Lung, and Blood Institute guidelines17 and the 2007 and 2008 guidelines of the Global Initiative for Asthma.18,19 The recent Global Initiative for Asthma guidelines were given the most credence because they are the most recent international guidelines available and because several Canadian respirologists were leaders in the guideline-creation process. Furthermore, we searched MEDLINE and PubMed for articles on newer issues related to the diagnosis of asthma. Finally, we took into account our own clinical experience, as supported by the relevant referenced evidence.
We based our grades of evidence on those of the Canadian Task Force on Preventive Health Care (Table 1).20
Table 1.
Recommendation grades and levels of evidence for specific clinical actions*
| Grade or level† | Description |
|---|---|
| Recommendation grade | |
| A | There is good evidence to recommend the clinical action. |
| B | There is fair evidence to recommend the clinical action. |
| C | Existing evidence is conflicting and does not allow a recommendation for or against the use of the clinical action; however, other factors may influence decision-making. |
| D | There is fair evidence to recommend against the clinical action. |
| E | There is good evidence to recommend against the clinical action. |
| I | There is insufficient evidence (in terms of quantity or quality or both) to make a recommendation; however, other factors may influence decision-making. |
| Level of evidence | |
| I | Evidence from one or more randomized controlled trials. |
| II-1 | Evidence from nonrandomized controlled trials. |
| II-2 | Evidence from cohort or case–control studies, preferably from more than one centre or research group. |
| II-3 | Evidence from comparisons between times or places, with or without the intervention; dramatic results from uncontrolled experiments may be included. |
| III | Opinions of respected authorities, based on clinical experience; descriptive studies or reports of expert committees. |
Modified from the Canadian Task Force on Preventive Health Care.20
The strongest recommendations (grades A and E) are reserved for interventions whose value is supported or highly negated by level I evidence. Grade B and D recommendations are associated with level II-1 and level II-2 evidence. Grade I recommendations reflect level II-3 and level III evidence and indicate that existing evidence is of insufficient quality or quantity (or both) to support a specific recommendation.
Approach to asthma diagnosis
Asthma should be suspected in patients with recurrent respiratory symptoms, particularly cough, wheeze, chest tightness and dyspnea. Alternative diagnoses should be excluded. An objective lung function test such as spirometry can be used to confirm airway obstruction and to demonstrate reversibility of obstruction with bronchodilator medication.
History
The clinical features associated with asthma are listed in Box 1. If the history is strongly suggestive of asthma, then a trial of treatment is warranted. If the trial is successful, asthma treatment should be continued.15 Objective testing to confirm the diagnosis should be considered at a later date. If the treatment is unsuccessful, or if the history is less clearly suggestive of asthma, objective testing should be performed to confirm the diagnosis. If the spirometry results are normal in such patients, further objective confirmation of asthma by measurement of airway responsiveness will validate the presence of current asthma, although it does not exclude past or future asthma. Alternative causes of symptoms suggestive of asthma (Box 2) should also be considered in the differential diagnosis of asthma.
Box 1. Clinical features related to probability of asthma in those with episodic symptoms*
Features favouring primary diagnosis of asthma
- At least 2 of the following symptoms: wheeze, breathlessness, chest tightness or cough with or without sputum, especially:
- - if symptoms are worse at night and early in the morning
- - if symptoms occur in response to exercise, exposure to allergens or exposure to cold air
- - if symptoms occur after taking ASA or β-blockers
History of atopic disorder
Findings of widespread wheeze on auscultation
Low FEV1 or peak expiratory flow (current or historical) that is otherwise unexplained
Peripheral blood eosinophilia that is otherwise unexplained
Features not favouring primary diagnosis of asthma
Prominent dizziness, light-headedness or peripheral tingling (in the absence of wheeze)
Chronic productive cough in the absence of wheeze or breathlessness
Normal results on physical examination of the chest during symptomatic episodes
Voice disturbance
Symptoms only with colds
Significant smoking history (more than 20 pack-years)
Cardiac disease
Normal peak expiratory flow or spirometry results during symptomatic episodes (not an exclusion criterion)
Note: ASA = acetylsalicylic acid, FEV1 = forced expiratory volume in 1 second.
Box 2. Alternative causes of symptoms suggestive of asthma*
- Other obstructive lung diseases
- - Chronic obstructive pulmonary disease
- - Eosinophilic bronchitis
- - Bronchiectasis
- - Cystic fibrosis
- - Primary ciliary dyskinesia syndrome
- - Immunoglobulin deficiency
- - Bronchopulmonary dysplasia
Chronic rhinosinusitis
Gastroesophageal reflux
Hyperventilation syndrome and panic attacks
Vocal cord dysfunction21
- Infections:
- - Recurrent viral infections of the lower respiratory tract
- - Tuberculosis
- - Other respiratory infections (e.g., chronic fungal, mycobacterial or parasitic infections)
- Mechanical obstruction of the airways:
- - Tumour (benign or malignant)
- - Foreign-body aspiration
- - Congenital malformations of the airways
- - Upper airway obstruction
Medications (e.g., angiotensin-converting-enzyme inhibitors)
Nonobstructive lung diseases (e.g., diffuse parenchymal lung disease, pulmonary embolism)
Extrapulmonary diseases (e.g., left ventricular failure, congenital heart disease)
Dyspnea can have respiratory, cardiac, hematologic, neuromuscular or psychosomatic causes, but the pattern of symptoms associated with this problem may point to the specific diagnosis (Box 1). Distinguishing asthma from chronic obstructive pulmonary disease (COPD) is a common clinical challenge. Asthma is associated with variable symptoms that often worsen after exposure to triggers and with nocturnal symptoms (usually occurring between 2 am and 6 am). In contrast, patients with COPD tend to experience a gradual increase in symptoms over time, with exacerbations often being related to infectious precipitants (Table 2).22 Also, COPD is characterized by irreversible or only partially reversible airflow obstruction and results from an abnormal inflammatory response to noxious agents. Asthma and COPD can coexist, particularly in people who smoke.19,23 Validated symptom-based questionnaires and diagnostic algorithms, designed for use in countries without the capabilities to objectively measure lung function, can be used to differentiate these conditions.12
Table 2.
Differences between asthma and chronic obstructive pulmonary disease (COPD)*
| Characteristic | Asthma | COPD |
|---|---|---|
| Age at onset | Usually < 40 yr | Usually > 40 yr |
| Smoking history | Not causal, but worsens control | Usually >10 pack-years |
| Sputum production | Infrequent | Common |
| Allergies | Common | Infrequent |
| Clinical symptoms | Intermittent and variable | Persistent and progressive |
| Course of disease | Stable (with exacerbations) | Progressive worsening (with exacerbations) |
| Importance of nonrespiratory comorbid illnesses | Not usually important | Often important |
| Spirometry results | Often normalize over time | May improve, but do not normalize over time |
| Airway inflammation | Eosinophilic | Neutrophilic |
Adapted with permission from the Canadian Pharmacists Journal: 140[Suppl 3], 2007.22
Congestive heart failure may feature symptoms similar to those of asthma, including cough and breathlessness. However, heart failure most commonly occurs in patients with a known history of cardiac problems and is often associated with ankle edema and weight gain. Moreover, although nocturnal symptoms are often prominent in heart failure, they tend to occur 1 or 2 hours after the patient reclines, rather than in the early morning hours.
The classic symptoms of asthma are listed in Box 1. It is important to elicit the possible triggers of asthma symptoms, especially those that can be modified. These triggers are typically allergic but may be occupational in nature and are commonly overlooked unless specifically considered. If work-related asthma is a possibility, details of work exposures and a pattern of improvement of asthma symptoms during holidays should be explored.
Comorbidities that can aggravate asthma, such as allergic rhinitis and gastroesophageal reflux disease, should also be documented.
Asthma is 1 of the 3 main causes of chronic cough in patients with normal results on chest radiography who are not taking angiotensin-converting-enzyme inhibitors (the others being rhinosinusitis and gastroesophageal reflux disease). Cough due to asthma usually occurs at night, and hence evaluations during the day may be normal.24 In patients with a persistent cough, asthma can be diagnosed in the same manner as for those who present with dyspnea or wheeze.17,18
Physical examination
The physical examination is relatively insensitive for diagnosis of asthma. Between episodes of asthma activity, physical signs of asthma may be absent, and the results of a physical examination are often entirely normal. Thus, the absence of physical findings does not rule out asthma. For this reason, an accurate, focused history combined with objective testing is essential.
The clinician should, however, look for signs of asthma such as wheeze, a prolonged expiratory phase and use of accessory muscles. Findings on the skin (i.e., eczema) and in the upper respiratory tract (i.e., nasal congestion, nasal polyps or postnasal drip) may also relate to asthma.
The sound of an expiratory wheeze is identical in asthma, COPD, congestive heart failure and pneumonia and cannot be used to distinguish among these conditions. The presence of pulsus paradoxus is a potential marker of the severity of airflow obstruction during an exacerbation, but it is nonspecific in differentiating the causes of respiratory symptoms.25
Tracheal deviation, accompanied by unilateral hyperresonance to percussion, suggests the alternative diagnosis of pneumothorax. Jugular venous distension suggests congestive heart failure or pericardial effusion. Clubbing, which is not associated with asthma, suggests an alternative diagnosis such as bronchiectasis, interstitial lung disease or malignant disease.26
Definitive diagnosis of asthma
The diagnosis of asthma requires a history or current presence of respiratory signs and symptoms consistent with asthma (Box 1), combined with the objective demonstration of variable airflow obstruction. Variable airflow obstruction means that the obstruction is not necessarily present at all times, varying with time, exposure to asthma triggers and treatment. A good response to asthma treatment in a patient with a typical history of asthma supports a diagnosis of asthma.1 However, objective confirmation of the variable airflow obstruction characteristic of asthma, using spirometry or peak expiratory flow monitoring, is required, especially for patients whose response to treatment is suboptimal or whose symptoms are not highly suggestive of asthma.9,19,25–29
Spirometry is recommended for all patients to confirm the diagnosis of asthma before initiation of possibly lifelong therapy. This form of objective testing is preferred over peak flow measurement because of the wide variation in predicted values for peak flow rates (as described below). Diagnosis is consequently less accurate if it is based on peak flow monitoring or a trial of therapy. Unfortunately, many clinicians diagnose asthma without confirming the diagnosis with objective testing, and misdiagnosis and mistreatment, particularly overtreatment, are therefore common.27,30
Spirometry is commonly performed in pulmonary function laboratories, but can be performed efficiently in primary care offices as well.31 Portable hand-held spirometers allow screening for obstruction32 and may be more easily used for this purpose than laboratory-based spirometry equipment. Out-of-office spirometry may be more time-consuming and hence less desirable for patients — and, because feedback is delayed, less desirable for physicians — than spirometry done in primary care practice33–36 and specialist practice. Wherever the spirometry is done, it must be performed according to the proper protocols.37 All spirometers should be standardized after manufacture38–41 and calibrated regularly.
Spirometry measures the forced vital capacity (FVC, the maximum volume of air that can be exhaled) and the FEV1, from which the FEV1/FVC ratio can be calculated. The patient is instructed to take in as big a breath as possible, to seal his or her lips around the mouthpiece of the spirometer and to blow the air out as fast and as fully as possible. This must be done with full effort and reproducibility. Videos illustrating the proper technique for spirometry measurement can be found at www.olapep.ca.
In the normal population, the FEV1/FVC ratio is usually greater than 0.80 and possibly greater than 0.90 in children.19 Any values less than these suggest airflow obstruction.19 The Canadian COPD guidelines stipulate that an FEV1/FVC ratio of less than 0.70 after administration of a bronchodilator identifies airway obstruction associated with COPD.42
The presence of one of the following18 is required to confirm reversibility of airflow obstruction, which is the hallmark of asthma (Figure 1):
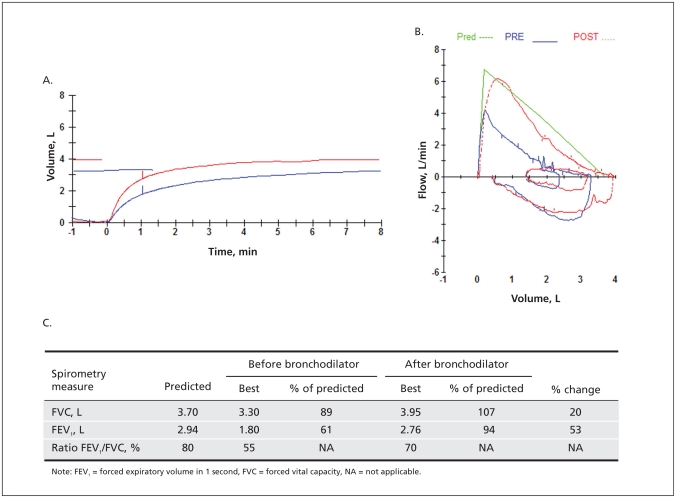
Figure 1.
Spirometry results for a patient with asthma: volume–time curves (A), flow–volume loops (B) and data table (C). Obstruction is indicated by the ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity (55%); significant reversibility is indicated by the improvement in FEV1 after administration of bronchodilator (0.96 L or 53%). These results are diagnostic for asthma.
an improvement in FEV1 of at least 12% and at least 200 mL19,43–45 15–20 minutes after administration of an inhaled rapid-acting β2-agonist, or
an improvement in FEV1 of at least 20% and at least 200 mL after 2 weeks of treatment with an anti-inflammatory agent such as an inhaled corticosteroid or a leukotriene receptor antagonist.38
Clinicians must correlate the patient’s history and the results of the physical examination with the pulmonary function test results to ensure that the diagnosis is accurate.
Work-related asthma
The diagnosis, management and prevention of work-related asthma have been addressed in a recent consensus statement46 endorsed by the Canadian Thoracic Society. Work-related asthma includes occupational asthma (de novo asthma or recurrence of previously quiescent childhood asthma caused by conditions attributable to a work environment46) and work-exacerbated asthma (asthma that is triggered by workplace factors in people who have pre-existing or concurrent asthma46).
The diagnosis of occupational asthma should be considered in all cases of new adult-onset asthma or recurrence of childhood asthma. Occupational asthma can be due to a specific sensitizing agent at work and is similar to an allergic response. Less frequently, it can be due to an acute, high-level exposure to an irritant at work. Work-exacerbated asthma may occur when there is exposure to 1 or more triggers at work that can exacerbate or aggravate asthma (such as dusts, fumes, cold air or exercise).
Although a history of asthma symptoms that are worse at work and that improve when away from work is very sensitive for both occupational asthma and work-exacerbated asthma, it is not very specific. Therefore, except if the patient experiences only a transient exacerbation of symptoms at work, the relation of asthma to the work environment must be confirmed with objective tests.
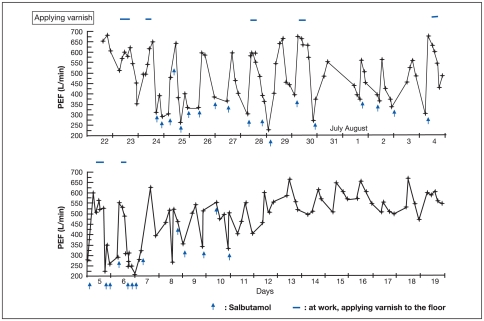
Assessing the relation of asthma to work begins with a thorough work history to determine exposures at work. Review of material safety data sheets from the workplace can assist in assessing exposure. Next, asthma should be objectively documented. As well, airway changes during periods at work compared with periods off work should be determined, by serial monitoring of peak expiratory flow at least 4 times a day for 2 weeks while the patient is working, then for a similar period when the patient is away from work (Figure 2).47 This monitoring is combined with a self-recorded diary of symptoms and use of reliever bronchodilator.43,44
Figure 2.
Serial recordings of peak expiratory flow (PEF) for a patient with occupational asthma. Measurements made during periods at work and while off work show objective improvement of PEF while off work, particularly after 3–4 days (see lower panel). The asthma was due to inhalation of toluene diisocyanate present in a varnish that the patient used at work (exposure indicated by horizontal bars at top of graph). Arrows indicate use of reliever medication (salbutamol) for asthma symptoms. Reproduced courtesy of Dr. André Cartier and Medical Resource Communications.47
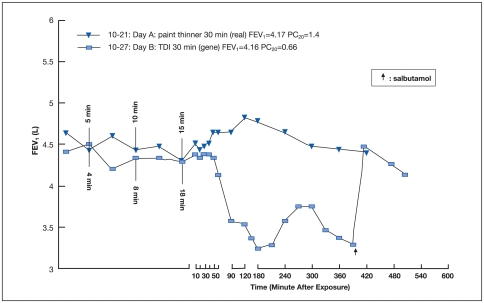
As a more objective indicator, the presence of nonspecific bronchial hyperresponsiveness at the end of a working week, with improvement when the patient has been off work for 10 days or more, is supportive of occupational asthma.44,45 Only a few centres are able to perform bronchoprovocation challenges to specific work agents (Figure 3).44,46,48,49 Documentation of sensitization to a work agent (particularly high-molecular-weight agents such as flour, animal dander or urine) by skin prick tests or serum tests for specific immunoglobulin E antibodies may also help to confirm the diagnosis. In addition, sputum cell counts, although available in only a few centres, can be measured at work and away from work. The presence of sputum eosinophilia at work and its absence away from work provides strong supportive evidence for occupational asthma.50
Figure 3.
Bronchoprovocation challenge testing for occupational asthma for the same patient as depicted in Figure 2. The decrease in forced expiratory volume in 1 second (FEV1) after a 30-minute exposure to toluene diisocyanate (TDI; day B, October 27; rectangles) but not after a 30-minute control exposure to paint thinner (day A, October 21; triangles) indicates a positive result on this specific challenge test, providing further confirmation of the diagnosis of occupational asthma due to toluene diisocyanate. Testing was performed in a single-blind manner, with multiple spirometry measurements over time before and after exposure. For day A, FEV1 = 4.17 L, PC20 (concentration of the provoking agent that causes the FEV1 to drop by 20%) = 1.4. For day B, FEV1 = 4.16 L, PC20 = 0.66. Arrow indicates use of reliever medication (salbutamol). Reproduced courtesy of Dr. André Cartier and Medical Resource Communications.47
Generally, as many of the above investigations as possible should be performed. This is because each test can be falsely negative or positive and also because there are often major implications for workplace conditions and compensation when a diagnosis of occupational asthma or frequent work-exacerbated asthma is made. Early referral to a specialist is recommended if work-related symptoms occur for more than a few days, because the tests can be difficult to interpret and hence the diagnosis can be more difficult to make if the patient has stopped working. Transient work-exacerbated asthma can usually be managed by the combination of reducing exposure and optimizing medication.
Further testing when spirometry results are nondiagnostic
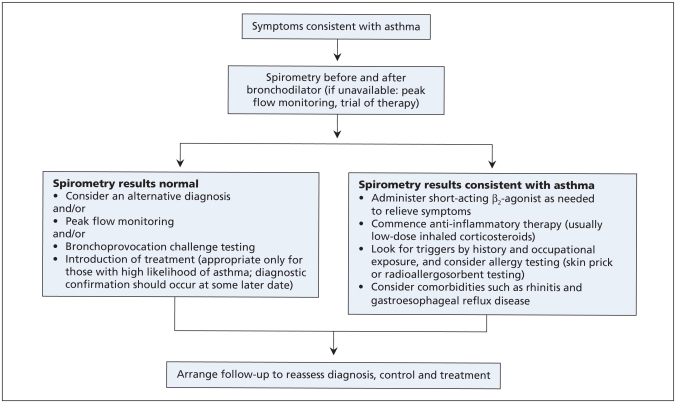
If spirometry results are normal but the clinician still suspects the patient has asthma (a common situation, because asthma is a variable disease), the diagnosis can be confirmed by other objective tests. A diagnostic algorithm for asthma is shown in Figure 4.
Figure 4.
Diagnostic algorithm for asthma.
Serial peak flow monitoring
Measurement of peak flow involves having the patient take in as deep a breath as possible and blow it out as hard and fast as possible into the measuring device (a peak flow meter). The test measures the fastest rate of expired airflow.
The following peak flow parameters support a diagnosis of asthma:19
Diurnal variation in peak expiratory flow of more than 20% (or, with twice-daily readings, of more than 10% at each reading)
An improvement of at least 60 L/min or at least 20% after inhalation of a rapid-acting bronchodilator
Peak flow measurement is much simpler and cheaper than spirometry and can be used by patients for self-monitoring at home or in the workplace. However, unlike spirometers, peak flow meters do not measure flow rates over time, nor do they measure lung volumes. Furthermore, there is great variation in readings from peak flow meters and in their reference values. Hence, they are not highly reliable for either children or adults.18 Patient compliance with self-monitoring may also be an issue. Furthermore, peak expiratory flow is less sensitive to changes in airway calibre than is FEV1. Therefore, it is preferable to use peak flow meters only for monitoring asthma, not for diagnosis.
Challenge testing
If the clinical scenario suggests asthma but spirometry results are normal, the diagnosis of asthma can be confirmed with bronchoprovocation or challenge testing. The optimal type of challenge test to use depends on local availability and physician preference, and hence the choice is best left to an asthma specialist. The choices include direct challenges with histamine or methacholine51 and indirect airway challenges with mannitol or exercise.52,53
Absolute and relative contraindications for challenge testing53 are listed in Box 3. Challenge testing should be conducted in accordance with strict protocols in a laboratory or other facility equipped to manage acute bronchospasm. An initial spirometry test should be conducted to assess baseline FEV1 and safety to proceed. This initial measurement should also be used to determine reproducibility. Inability of the patient to generate reproducible flow–volume curves is often a reason to discontinue a bronchial provocation test. Challenge testing should also be reconsidered for patients whose FEV1 has been reduced to below 70% of the normal predicted value, as bronchoprovocation could cause significant bron-chospasm in such individuals.19 To decrease the rate of false positive results, it may also be prudent to delay the test if the patient has just had an acute respiratory infection.
Box 3. Contraindications to methacholine and exercise challenge testing53
Absolute contraindications
Severe airflow limitation (FEV1 < 1.0 L)
Heart attack or stroke in the past 3 months
Uncontrolled hypertension, systolic blood pressure >200 mm Hg or diastolic blood pressure > 100 mm Hg
Known aortic aneurysm
Relative contraindications
Moderate airflow limitation (FEV1 < 1.5 L)
Inability to achieve spirometry results of acceptable quality
Pregnancy
Breastfeeding
Current use of cholinesterase inhibitor medication (for myasthenia gravis)
Note: FEV1 = forced expiratory volume in 1 second.
After completion of baseline spirometry, the inhalational challenge test begins with inhalation of saline, after which FEV1 is again recorded. If there is no change, then progressively higher doses of the provoking agent (e.g., methacholine) are given according to protocol, until the FEV1 drops by 20% or the maximum test dose is reached. An inhaled β2-agonist is then provided to reverse the obstruction.
Airway reactivity is measured in terms of the dose or concentration of the provoking agent that causes the FEV1 to drop by 20% (the PD20 or PC20, respectively). For methacholine, a PC20 value lower than the standard threshold of 8 mg/mL is considered a positive result indicative of airway hyperreactivity.
A negative result on an inhalational challenge test in a patient who is symptomatic, in the absence of corticosteroid anti-inflammatory treatment and during a time when asthma triggers are still present, is highly sensitive in ruling out asthma.54,55 An exception is patients whose only trigger for bronchospasm is exercise, including elite athletes, in whom such results may be false negatives. However a positive test result does not always mean that asthma is present. Positive results may occur with allergic rhinitis,56 cystic fibrosis,57 bronchiectasis and COPD.56 As such, the challenge test, when negative, may be most useful in ruling out asthma.
An exercise challenge test measures the FEV1 or peak expiratory flow at rest and then again after exercise such as running on a treadmill or riding a stationary bike. Exercise-induced bronchospasm is confirmed by a 15% or greater decrease in peak flow rate or FEV1. It may be further graded as mild (15%–25% decrease), moderate (25%–40% decrease) or severe (40% or greater decrease).58 Exercise challenge is performed less frequently than methacholine challenge. This is primarily because the latter is easier to perform and more sensitive, although it is also less specific.
Ancillary tests
Chest radiography is not necessary for the diagnosis of obstructive airway disease,18 but it can help rule out other conditions such as congestive heart failure, lung cancer and bronchiectasis. Chest radiography should also be ordered in atypical cases15 or for patients with no response to asthma therapy.
Any relevant environmental allergies suggested by the history should be confirmed by skin prick tests with common allergen extracts or with specific immunoglobulin E allergen assays.59 Appropriate avoidance strategies can then be advocated. Examples of avoidance strategies are removal of pets; use of covers for mattresses, box spring, pillows and bedding; reduction of humidity (to kill house dust mites); and closing of windows during pollen seasons.
Gaps in knowledge and future directions
Other testing approaches may be part of future algorithms. Measurement of inflammatory markers such as sputum eosinophils or exhaled nitric oxide is already being used in some settings to evaluate asthma control and formulate management decisions. However, although such tests show clinical promise, they have not yet been rigorously investigated for use in the diagnosis of asthma60–62 and are currently limited to tertiary care centres and research facilities.
Tests to assess airway hyperresponsiveness with indirect stimuli — which induce the release of mediators from inflammatory cells and sensory nerves, causing contraction of bronchial smooth muscle and narrowing of the airways — are gaining attention for both identifying and monitoring asthma. Indirect stimuli include hyperpnea, hypertonic aerosols, osmotic challenges and adenosine monophosphate. Tests using indirect stimuli may be superior to those using direct stimuli, as responses to indirect challenges appear to be related to mast cells and eosinophils in the airways. Thus, indirect stimuli may better reflect the inflammatory status of the airway following treatment with inhaled corticosteroids. Also, the severity of airway hyperresponsiveness in response to an indirect stimulus is not closely related to baseline lung function. Many people with asthma who have normal lung function are very responsive to indirect stimuli. Moreover, osmotic challenge tests with mannitol have demonstrated higher specificity and greater safety for the diagnosis of asthma than traditional measures of airway hyperresponsiveness, such as methacholine challenge.63
A 10% or more fall in FEV1 from baseline is considered an abnormal response following hyperventilation with dry air, as is a fall of 15% from baseline following challenge with hypertonic aerosols. For adenosine monophosphate, a 20% or greater fall in FEV1 at a concentration of less than 400 mg/mL is considered abnormal. Furthermore, a positive response to bronchial provocation by eucapnic voluntary hyperventilation is considered acceptable confirmation of exercise-induced asthma;64–66 it is in fact the current standard of the International Olympic Committee, although it is not often used in other settings.
Tests that use indirect stimuli differ from one another in their complexity and the amount of equipment required, many being possible only in a hospital laboratory. The use of eucapnic voluntary hyperventilation, for example, should be confined to specialist centres. However, a mannitol testing kit using a dry powder inhaler has recently been developed that could allow such testing to move outside the pulmonary function laboratory and into the office setting.
In the future, genetic testing may allow individually targeted diagnostics and therapeutic decisions.67,68
Case revisited
Sara’s history of childhood atopy and allergy, together with her persistent cough and wheeze, are suggestive of asthma. Her worsening of symptoms with physical activity and her upper respiratory tract infections also support a diagnosis of asthma. Moreover, the absence of heartburn makes a diagnosis of reflux less likely,69 and there is no clinical evidence of rhinitis. Although people with asthma may display many physical signs, normal results on physical examination, such as were found in Sara’s case, are typical.
A careful environmental history is taken, covering both Sara’s home and her workplace. Objective measurement of airflow obstruction and reversibility is required to confirm the diagnosis, and spirometry before and after administration of bronchodilator is ordered. Work-related asthma is suspected because her adult symptoms began while she was working and because she may be exposed to occupational sensitizers (such as diisocyanates or amines from autobody spray paints) and irritants in her workplace. Alternatively, she may be experiencing recurrence of childhood asthma, unrelated to her work but exacerbated by exposures at work, such as to fumes and dust. Therefore, if the diagnosis of asthma is confirmed, peak flow monitoring will be initiated and she will be referred to a specialist with expertise in work-related asthma.
In the interim, Sara is started on a fast-acting bronchodilator reliever medication, and she is instructed to use it on an as-needed basis to treat symptoms and before exertion to prevent symptoms. A controller medication (a steroid or com bination steroid and long-acting bronchodilator inhaler70) is not prescribed until the diagnosis is confirmed.
Sara is encouraged to stop smoking: even a few minutes spent discussing smoking cessation can assist in changing a patient’s behaviour.71,72 Follow-up is arranged for a time when the spirometry results will be available. If Sara’s test results and clinical condition confirm persistent asthma, anti-inflammatory therapy will be appropriate for her.
Conclusions
The key messages for the diagnosis of asthma in adults are presented in Box 4. Available tests can help the clinician to make a firm diagnosis of asthma in most patients. This common condition may well require lifelong therapy, and accurate diagnosis is therefore important. For people with a high likelihood of asthma and an appropriate response to therapy, a categorical diagnosis of asthma can be made. For such patients, confirmation with spirometry should be considered at a later date. For all others, spirometry should be part of the initial diagnostic work-up. Provocation testing may be necessary if the spirometry results are normal. The diagnosis of asthma depends on the physician’s expert correlation of the patient’s history, the results of a physical examination, the patient’s clinical response and the results of pulmonary function testing.
Box 4. Key messages for the diagnosis of asthma in adults
The diagnosis of asthma should be suspected in patients with recurrent cough, wheeze and dyspnea in whom no alternative diagnosis can be found and should be confirmed by an objective measurement of lung function or, if normal, by tests for bronchial hyperresponsiveness (grade A recommendation; level II-2 evidence).
A clinical diagnosis of asthma should be prompted by symptoms such as episodic breathlessness, wheezing, cough, sputum and chest tightness (grade A recommendation; level II-2 evidence).
Measurements of lung function by spirometry or peak expiratory flow provide an assessment of the severity of airflow limitation, its reversibility and its variability, and can be used to confirm the diagnosis of asthma (grade B recommendation; level II-2 evidence).
Measurements of allergic status can help to identify risk factors that cause asthma symptoms in individual patients (grade B recommendation; level III evidence).
Because the obstruction observed in asthma is variable, it is possible (and perhaps even likely) for the spirometry results to be normal for a patient who has asthma. Options to confirm asthma include bronchial challenge tests, serial peak flow monitoring and measurements of inflammation (grade B recommendation; level II-2 evidence).
For patients with symptoms consistent with asthma who have normal lung function, measurement of airway responsiveness may help to establish the diagnosis (grade B recommendation; level II-2 evidence).
Challenge testing is potentially useful in patients with typical symptoms but normal spirometry results or atypical symptoms or possible occupational asthma (grade B recommendation; level III evidence).
Key points
A clinical diagnosis of asthma should be prompted by intermittent symptoms of breathlessness, wheezing, cough, sputum or chest tightness.
Measurements of lung function by spirometry, before and after administration of a β2-agonist, should be used to confirm the clinical diagnosis of asthma.
Occupational asthma should be considered in all cases of new-onset asthma in adults.
Challenge testing is most useful to exclude a diagnosis of asthma.
This article is the second in a 7-part case study series that was developed as a knowledge translation initiative of the Canadian Thoracic Society Asthma Committee. The series aims to educate and inform primary care providers and nonrespiratory specialists about the diagnosis and management of asthma. The key messages presented in the cases are not clinical practice guidelines but are based on a review of the most recent scientific evidence available. Financial support for the publication of this series has been provided, in part, by the Canadian Thoracic Society.
Acknowledgements
We thank the following individuals for their contributions to this article: Dr. Susan Tarlo, University of Toronto, Dr. Don Cock-roft, University of Saskatchewan, and Dr. André Cartier and Dr. Catherine Lemiere, Université de Montréal for help with the section on occupational asthma; Dr. John Brannan, for help with mannitol testing; and Rosemary Frei, for assistance with literature searches and for editorial input.
Footnotes
This article has been peer reviewed.
Competing interests: Alan Kaplan has received honoraria for talks from AstraZeneca, GlaxoSmithKline, Nycomed, Boehringer Ingelheim and Pfizer. He has served on advisory boards for Merck Frosst, Nycomed, AstraZeneca and Boehringer Ingelheim. He has received travel reimbursement to meetings of the European Respiratory Society from Merck and AstraZeneca. Meyer Balter serves on advisory boards for AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Merck, Nycomed and Pfizer and has received honoraria from each of these companies for speaking engagements. Alan Bell has been a member of AstraZeneca Canada’s National Advisory Board for Respiratory Medicine from 2003 to the present and has received travel reimbursement to attend meetings of this board. He has also received consulting contracts and speaker fees from this board. He has received compensation for conducting clinical trials in respiratory disease from the following companies: AstraZeneca Canada, Nycomed Canada and Boehringer Ingelheim Canada. Harold Kim has received speakers fees and has served on advisory boards for Merck, GlaxoSmithKline, AstraZeneca, Graceway and Nycomed. Andrew McIvor has attended advisory board meetings and provided continuing medical education for which he has received honoraria from pharmaceutical companies involved in asthma management: AstraZeneca, Boehringer Ingelheim, Graceway, GlaxoSmithKline, Novartis, Merck Frosst and Pfizer.
Contributors: All authors contributed to the development, writing and editing of the article, and all approved the final version submitted for publication.
Funding: The Canadian Thoracic Society has received funding to facilitate the knowledge translation activities of the CTS Asthma Committee from AstraZeneca Canada, GlaxoSmithKline Inc., Merck Frosst Canada and Novartis Pharmaceuticals. None of the sponsors played a role in the collection, review, analysis or interpretation of the scientific literature or in any decisions regarding the key messages presented in the case studies.
Amended from British Guideline on the Management of Asthma: A National Clinical Guideline. 15
REFERENCES
- 1.Aaron SD, Vandemheen KL, Boulet LP, et al. Overdiagnosis of asthma in obese and nonobese adults. CMAJ. 2008;179:1121–31. doi: 10.1503/cmaj.081332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stanbrook MB, Kaplan A. The error of not measuring asthma. CMAJ. 2008;179:1099–102. doi: 10.1503/cmaj.081665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Life and breath: respiratory disease in Canada. Ottawa (ON): Public Health Agency of Canada; 2007. [(accessed 2009 Jul. 24)]. Available: www.phac-aspc.gc.ca/publicat/2007/lbrdc-vsmrc/index-eng.php. [Google Scholar]
- 4.Kaplan A. Systems for the management of respiratory disease in primary care —an international series: Canada. Prim Care Respir J. 2008;17:73–8. doi: 10.3132/pcrj.2008.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Persons with asthma, by age and sex (1996/1997–2005) Ottawa (ON): Statistics Canada; 2009. [(accessed 2009 Jan. 3)]. Available: www40.statcan.ca/l01/cst01/health49a.htm. [Google Scholar]
- 6.FitzGerald JM, Boulet LP, McIvor A, et al. Asthma control in Canada remains suboptimal: The Reality of Asthma Control (TRAC) study. Can Respir J. 2006;13:253–9. doi: 10.1155/2006/753083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chapman KR, Ernst P, Grenville A. Control of asthma in Canada: patient and physician perspective. Am J Respir Crit Care Med. 2000;161(Suppl):A799. [Google Scholar]
- 8.Krahn MD, Berka C, Langlois P, et al. Direct and indirect costs of asthma in Canada, 1990. CMAJ. 1996;154:821–31. [PMC free article] [PubMed] [Google Scholar]
- 9.Cowie RL, Underwood M, Field SK. Asthma symptoms do not predict spirometry. Can Respir J. 2007;14:339–42. doi: 10.1155/2007/816132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parameswaran K, Pizzichini E, Pizzichini MMM, et al. Clinical judgement of airway inflammation versus sputum cell counts in patients with asthma. Eur Respir J. 2000;15:486–90. doi: 10.1034/j.1399-3003.2000.15.10.x. [DOI] [PubMed] [Google Scholar]
- 11.Lemiere C. Induced sputum and exhaled nitric oxide as non-invasive markers of airway inflammation from work exposures. Curr Opin Allergy Clin Immunol. 2007;7:133–7. doi: 10.1097/ACI.0b013e3280187584. [DOI] [PubMed] [Google Scholar]
- 12.International Primary Care Respiratory Group. IPCRG guidelines for the management of chronic respiratory diseases in primary care. [(accessed 2009 Jan. 3)];Prim Care Resp J. 2006 1:1–74. Available: www.thepcrj.org/journ/guidelines.php. [Google Scholar]
- 13.Boulet L–P, Becker A, Bérubé D, et al. Canadian asthma consensus report, 1999. [(accessed 2009 Jul. 24)];CMAJ. 1999 161(11 Suppl 1):S1–62. Available: www.cmaj.ca/cgi/reprint/161/11_suppl_1/s1. [PMC free article] [PubMed] [Google Scholar]
- 14.Lemiere C, Bai T, Balter M, et al. Adult asthma consensus guidelines update 2003. Can Respir J. 2004;11(Suppl A):9A–18A. doi: 10.1155/2004/271362. [DOI] [PubMed] [Google Scholar]
- 15.British Thoracic Society; Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma: a national clinical guideline. London (UK): The Society; 2008. [(accessed 2009 Jan. 3)]. Available: www.sign.ac.uk/pdf/sign101.pdf. [Google Scholar]
- 16.Irwin RS, Baumann MH, Bolser DC, et al. Diagnosis and management of cough executive summary: ACCP evidence-based clinical practice guidelines. Chest. 2006;129 (Suppl 1):1S–23S. doi: 10.1378/chest.129.1_suppl.1S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Asthma Education and Prevention Program. Expert Panel report 3: Guidelines for the diagnosis and management of asthma Full report 2007. Bethesda (MD): US Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute; 2007. [(accessed 2009 Jan. 3)]. Available: www.nhlbi.nih.gov/guidelines/asthma/asthgdln.pdf. [Google Scholar]
- 18.Global strategy for asthma management and prevention. Global Initiative for Asthma; 2007. [(accessed 2009 Jan. 3)]. Available: www.ginasthma.org/Guidelineitem.asp??l1=2&l2=1&intId=60. [Google Scholar]
- 19.Bateman ED, Hurd SS, Barnes PJ, et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008;31:143–78. doi: 10.1183/09031936.00138707. [DOI] [PubMed] [Google Scholar]
- 20.Canadian Task Force on Preventive Health Care. New grades for recommendations from the Canadian Task Force on Preventive Health Care. CMAJ. 2003;169:207–8. [PMC free article] [PubMed] [Google Scholar]
- 21.Gjevre JA, Hurst TS, Taylor-Gjevre RM, et al. The American Thoracic Society’s spirometric criteria alone is inadequate in asthma diagnosis. Can Respir J. 2006;13:433–7. doi: 10.1155/2006/198940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hodder R. Clinical differences between asthma and chronic obstructive pulmonary disease (COPD) Can Pharm J. 2007;140(Suppl 3):S8. [Google Scholar]
- 23.Jenkins CR, Thompson PJ, Gibson PG, et al. Distinguishing asthma and chronic obstructive pulmonary disease: Why, why not and how? Med J Aust. 2005;183 (Suppl 1):S35–7. doi: 10.5694/j.1326-5377.2005.tb06916.x. [DOI] [PubMed] [Google Scholar]
- 24.Corrao WM, Braman SS, Irwin RS. Chronic cough as the sole presenting manifestation of bronchial asthma. N Engl J Med. 1979;300:633–7. doi: 10.1056/NEJM197903223001201. [DOI] [PubMed] [Google Scholar]
- 25.Arnold DH, Gebretsadik T, Minton PA, et al. Clinical measures associated with FEV1 in persons with asthma requiring hospital admission. Am J Emerg Med. 2007;25:425–9. doi: 10.1016/j.ajem.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 26.Li JT, Pearlman DS, Nicklas RA, et al. Algorithm for the diagnosis and management of asthma: a practice parameter update: Joint Task Force on Practice Parameters, representing the American Academy of Allergy, Asthma and Immunology, the American College of Allergy, Asthma and Immunology, and the Joint Council of Allergy, Asthma and Immunology. Ann Allergy Asthma Immunol. 1998;81:415–20. doi: 10.1016/s1081-1206(10)63138-9. [DOI] [PubMed] [Google Scholar]
- 27.Petty TL. Simple office spirometry. Clin Chest Med. 2001;22:845–59. doi: 10.1016/s0272-5231(05)70070-8. [DOI] [PubMed] [Google Scholar]
- 28.Bellamy D. Spirometry in practice: a practical guide to using spirometry in primary care. 2nd ed. London (UK): The British Thoracic Society COPD Consortium; 2005. [(accessed 2009 Jan. 3)]. Available: www.brit-thoracic.org.uk/Portals/0/Clinical%20Information/COPD/COPD%20Consortium/spirometry_in_practice051.pdf. [Google Scholar]
- 29.National Asthma Education and Prevention Program. Expert Panel report: guidelines for the diagnosis and management of asthma update on selected topics—2002. J Allergy Clin Immunol. 2002;110 (Suppl 5):S141–219. [PubMed] [Google Scholar]
- 30.LindenSmith J, Morrison D, Deveau C, et al. Overdiagnosis of asthma in the community. Can Respir J. 2004;11:111–6. doi: 10.1155/2004/276493. [DOI] [PubMed] [Google Scholar]
- 31.Tuomisto L, Jarvinen V, Laitinen J, et al. Asthma Programme in Finland: the quality of primary care spirometry is good. Prim Care Respir J. 2008;17:226–31. doi: 10.3132/pcrj.2008.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rytila P, Helin T, Kinnula V. The use of microspirometry in detecting lowered FEV1 values in current or former smokers. Prim Care Respir J. 2008;17:232–7. doi: 10.3132/pcrj.2008.00058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Derom E, van Weel C, Liistro G, et al. Primary care spirometry. Eur Respir J. 2008;31:197–203. doi: 10.1183/09031936.00066607. [DOI] [PubMed] [Google Scholar]
- 34.Calverley P. Fulfilling the promise of primary care spirometry. Eur Respir J. 2008;31:8–10. doi: 10.1183/09031936.00124507. [DOI] [PubMed] [Google Scholar]
- 35.Pearson M, Ayres JG, Sarno M, et al. Diagnosis of airway obstruction in primary care in the UK: the CADRE (COPD and Asthma Diagnostic/management REassessment) programme 1997–2001. Int J Chron Obstruct Pulmon Dis. 2006;1:435–43. doi: 10.2147/copd.2006.1.4.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hueto J, Cebollero P, Pascal I, et al. Spirometry in primary care in Navarre, Spain [article in Spanish] Arch Bronconeumol. 2006;42:326–31. doi: 10.1016/s1579-2129(06)60541-7. [DOI] [PubMed] [Google Scholar]
- 37.Miller MR, Hankinson J, Brusasco V, et al. ATS/ERS Task Force: Standardisation of lung function testing series. Number 2. Standardisation of spirometry. Eur Respir J. 2005;26:319–38. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 38.Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948–68. doi: 10.1183/09031936.05.00035205. [DOI] [PubMed] [Google Scholar]
- 39.American Thoracic Society. Standardization of spirometry, 1994 update. Am J Respir Crit Care Med. 1995;152:1107–36. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 40.Official statement of the European Respiratory Society. Standardized lung function testing. Eur Respir J Suppl. 1993;16:1–100. [PubMed] [Google Scholar]
- 41.Sawyer G, Miles J, Lewis S, et al. Classification of asthma severity: Should the international guidelines be changed? Clin Exp Allergy. 1998;28:1565–70. doi: 10.1046/j.1365-2222.1998.00451.x. [DOI] [PubMed] [Google Scholar]
- 42.O’Donnell DE, Hernandez P, Kaplan A, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease — 2008 update — highlights for primary care. Can Respir J. 2008;15(Suppl SA):1A–8A. doi: 10.1155/2008/641965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Beach J, Russell K, Blitz S, et al. Systematic review of the diagnosis of occupational asthma. Chest. 2007;131:569–78. doi: 10.1378/chest.06-0492. [DOI] [PubMed] [Google Scholar]
- 44.Tarlo SM. Laboratory challenge testing for occupational asthma. J Allergy Clin Immunol. 2003;111:692–4. doi: 10.1067/mai.2003.1374. [DOI] [PubMed] [Google Scholar]
- 45.Bright P, Burge PS. Occupational lung disease. 8. The diagnosis of occupational asthma from serial measurements of lung function at and away from work. Thorax. 1996;51:857–63. doi: 10.1136/thx.51.8.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tarlo SM, Balmes J, Balkissoon R, et al. Diagnosis and management of work-related asthma: American College of Chest Physicians consensus statement. [(accessed 2009 Jan. 3)];Chest. 2008 134(3 Suppl):1S–41S. doi: 10.1378/chest.08-0201. Available: www.chestjournal.org/content/vol134/3_suppl/ [DOI] [PubMed] [Google Scholar]
- 47.Cartier A. What’s new in respirology? Occupation asthma. Respiratum. 2006;4 [Google Scholar]
- 48.Tarlo SM, Liss GM. Occupational asthma: an approach to diagnosis and management. CMAJ. 2003;168:867–71. [PMC free article] [PubMed] [Google Scholar]
- 49.Hoeppner VH, Murdock KY, Kooner S, et al. Severe acute “occupational asthma” caused by accidental allergen exposure in an allergen challenge laboratory. Ann Allergy. 1985;55:36–7. [PubMed] [Google Scholar]
- 50.Girard F, Charboillez S, Cartier A, et al. An effective strategy for diagnosing occupational asthma: use of induced sputum. Am J Respir Crit Care Med. 2004;170:845–50. doi: 10.1164/rccm.200403-380OC. [DOI] [PubMed] [Google Scholar]
- 51.Cockcroft DW. Bronchoprovocation methods: direct challenges. Clin Rev Allergy Immunol. 2003;24:19–26. doi: 10.1385/CRIAI:24:1:19. [DOI] [PubMed] [Google Scholar]
- 52.Brannan JD, Anderson SD, Perry CP, et al. The safety and efficacy of inhaled dry powered mannitol as a bronchial provocation test for airway hyperresponsiveness: a phase 3 comparison study with hypertonic (4.5%) saline. Respir Res. 2005;6:144. doi: 10.1186/1465-9921-6-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Crapo RO, Casaburi R, Coates AL, et al. Guidelines for methacholine and exercise challenge testing — 1999. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors July 1999. Am J Respir Crit Care Med. 2000;161:309–29. doi: 10.1164/ajrccm.161.1.ats11-99. [DOI] [PubMed] [Google Scholar]
- 54.Boulet LP. Asymptomatic airway hyperresponsiveness: a curiosity or an opportunity to prevent asthma? Am J Respir Crit Care Med. 2003;167:371–8. doi: 10.1164/rccm.200111-084PP. [DOI] [PubMed] [Google Scholar]
- 55.Cockcroft DW, Murdock KY, Berscheid BA, et al. Sensitivity and specificity of histamine PC20 determination in a random selection of young college students. J Allergy Clin Immunol. 1992;89:23–30. doi: 10.1016/s0091-6749(05)80037-5. [DOI] [PubMed] [Google Scholar]
- 56.Ramsdale EH, Morris MM, Roberts RS, et al. Asymptomatic bronchial hyperresponsiveness in rhinitis. J Allergy Clin Immunol. 1985;75:573–7. doi: 10.1016/0091-6749(85)90032-6. [DOI] [PubMed] [Google Scholar]
- 57.van Haren EH, Lammers JW, Festen J, et al. The effects of the inhaled corticosteroid budesonide on lung function and bronchial hyperresponsiveness in adult patients with cystic fibrosis. Respir Med. 1995;89:209–14. doi: 10.1016/0954-6111(95)90249-x. [DOI] [PubMed] [Google Scholar]
- 58.Safran MR, McKeag D, Van Camp SP, editors. Manual of sports medicine. Philadelphia (PA): Lippincott-Raven; 1998. [Google Scholar]
- 59.Douglass JA, O’Hehir RE. Diagnosis, treatment and prevention of allergic disease: the basics. Med J Aust. 2006;185:228–33. doi: 10.5694/j.1326-5377.2006.tb00539.x. [DOI] [PubMed] [Google Scholar]
- 60.Hargreave FE. Quantitative sputum cell counts as a marker of airway inflammation in clinical practice. Curr Opin Allergy Clin Immunol. 2007;7:102–6. 59. doi: 10.1097/ACI.0b013e328013e3c2. [DOI] [PubMed] [Google Scholar]
- 61.Parameswaran K, Pizzichini E, Pizzichini MMM, et al. Clinical judgement of airway inflammation versus sputum cell counts in patients with asthma. Eur Respir J. 2000;15:486–90. doi: 10.1034/j.1399-3003.2000.15.10.x. [DOI] [PubMed] [Google Scholar]
- 62.Lemiere C. Induced sputum and exhaled nitric oxide as non-invasive markers of airway inflammation from work exposures. Curr Opin Allergy Clin Immunol. 2007;7:133–7. doi: 10.1097/ACI.0b013e3280187584. [DOI] [PubMed] [Google Scholar]
- 63.Brannan JD, Koskela H, Anderson SD. Monitoring asthma therapy using direct bronchial provocation tests. Clin Respir J. 2007;1:3–15. doi: 10.1111/j.1752-699X.2007.00004.x. [DOI] [PubMed] [Google Scholar]
- 64.Spiering BA, Judelson DA, Rundell KW. An evaluation of standardizing target ventilation for eucapnic voluntary hyperventilation using FEV1. J Asthma. 2004;41:745–9. doi: 10.1081/jas-200028004. [DOI] [PubMed] [Google Scholar]
- 65.Haahtela T, Malmberg P, Moreira A. Mechanisms of asthma in Olympic athletes — practical implications. Allergy. 2008;63:685–94. doi: 10.1111/j.1398-9995.2008.01686.x. [DOI] [PubMed] [Google Scholar]
- 66.Anderson SD, Argyros GJ, Magnussen H, et al. Provocation by eucapnic voluntary hyperpnoea to identify exercise induced bronchoconstriction. Br J Sports Med. 2001;35:344–7. doi: 10.1136/bjsm.35.5.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Karjalainen J, Nieminen MM, Aromaa A, et al. The IL-1β genotype carries asthma susceptibility only in men. J Allergy Clin Immunol. 2002;109:514–6. doi: 10.1067/mai.2002.121948. [DOI] [PubMed] [Google Scholar]
- 68.Koppelman GH, te Meerman GJ, Postma DS. Genetic testing for asthma. Eur Respir J. 2008;32:775–82. doi: 10.1183/09031936.00093608. [DOI] [PubMed] [Google Scholar]
- 69.Irwin RS, French CL, Curley FJ, et al. Chronic cough due to gastroesophageal reflux. Clinical, diagnostic, and pathogenetic aspects. Chest. 1993;104:1511–7. doi: 10.1378/chest.104.5.1511. [DOI] [PubMed] [Google Scholar]
- 70.Lemière C, Becker A, Boulet LP, et al. Should combination therapy with inhaled corticosteroids and long-acting β2-agonists be prescribed as initial maintenance treatment for asthma? CMAJ. 2002;167:1008–9. [PMC free article] [PubMed] [Google Scholar]
- 71.Treating tobacco use and dependence: 2008 update. Washington (DC): US Department of Health and Human Services, Public Health Service; 2008. [(accessed 2009 Jan. 3)]. Available: www.surgeongeneral.gov/tobacco/treating_tobacco_use08.pdf. [Google Scholar]
- 72.Kaplan KE. Ten minute consultation: smoking cessation. BMJ. 2008;336:217. doi: 10.1136/bmj.39248.531748.47. [DOI] [PMC free article] [PubMed] [Google Scholar]