Abstract
Viral infection is associated with approximately one-half of acute exacerbations of chronic obstructive pulmonary disease (COPD), which in turn, accelerate disease progression. In this study, we infected mice exposed to a combination of elastase and LPS, a constituent of cigarette smoke and a risk factor for development of COPD, with rhinovirus serotype 1B, and examined animals for viral persistence, airway resistance, lung volume, and cytokine responses. Mice exposed to elastase and LPS once a week for 4 wk showed features of COPD such as airway inflammation and obstruction, goblet cell metaplasia, reduced lung elastance, increased total lung volume, and increased alveolar chord length. In general, mice exposed to elastase or LPS alone showed intermediate effects. Compared with rhinovirus (RV)-infected PBS-exposed mice, RV-infected elastase/LPS-exposed mice showed persistence of viral RNA, airway hyperresponsiveness, increased lung volume, and sustained increases in expression of TNFα, IL-5, IL-13, and muc5AC (up to 14 days postinfection). Furthermore, virus-induced IFNs, interferon response factor-7, and IL-10 were deficient in elastase/LPS-treated mice. Mice exposed to LPS or elastase alone cleared virus similar to PBS-treated control mice. We conclude that limited exposure of mice to elastase/LPS produces a COPD-like condition including increased persistence of RV, likely due to skewing of the immune response towards a Th2 phenotype. Similar mechanisms may be operative in COPD.
Keywords: chronic obstructive pulmonary disease, goblet cell metaplasia, IL-10, innate immunity, interferons
chronic obstructive pulmonary disease (COPD) is a progressive disease and characterized by small airway inflammation, airway obstruction due to hypersecretion of mucus, emphysema, and abnormal inflammatory response of lungs to external stimuli. Although the primary cause of COPD is smoking and chronic exposure to environmental pollutants, acute exacerbations (AE-COPD) due to infections can accelerate disease progression. One-half of all AE-COPD are associated with bacterial infection, with non-typeable Hemophilus influenzae being the most common pathogen (1). Exacerbations are also associated with the acquisition of new strains of H. influenzae, Moraxella catarrhalis and Streptococcus pneumoniae, Enterobacter, and Pseudomonas aeruginosa (11, 44). On the other hand, between 27 and 56% of AE-COPD has been associated with respiratory viral infections, with rhinovirus (RV) being the most common virus isolated (14, 39, 43). Furthermore, mild COPD patients experimentally infected with RV showed persistence of virus that was associated with increased proinflammatory cytokines in nasal lavage and significant increases in lower respiratory tract symptoms compared with normal volunteers (31). However, the underlying reasons for RV persistence and associated increased inflammatory response in COPD patients are poorly understood.
LPS is a major proinflammatory component of gram-negative bacteria that is present in cigarette smoke in appreciable amounts (19, 28, 42). LPS has also been shown to be an active component of various occupational and environmental hazards (40). Experimental inhalation of LPS evokes pulmonary and systemic inflammation in healthy human subjects (22, 33). In experimental animals, long-term intratracheal exposure to LPS (twice a week for 3 mo) causes goblet cell metaplasia, airway wall thickening, and emphysema, which persist up to 8 wk after the final LPS administration (24, 47). Recently, exposure of mice to inhaled LPS, 4 h a day for 4 wk, was shown to cause emphysema-like changes that persisted up to 4 wk (6). Thus, chronic LPS exposure mimics changes observed in human subjects with COPD, suggesting that this model could be applicable to the study of RV-induced exacerbations. To accomplish this, we augmented the LPS model by adding exposure to elastase, a well-known inducer of emphysematous lung lesions that generates proinflammatory elastin fragments (20). Addition of elastase considerably decreased the number and frequency of exposures and dose of LPS required to generate a COPD phenotype. Finally, we inoculated elastase- and LPS-exposed mice to human RV1B, a minor group virus capable of replicative lung infection in mice (37). We found that, upon infection with RV1B, elastase- and LPS-treated mice with pathological and physiological changes typical of COPD show persistence of RV in their lungs, airway hyperresponsiveness, increased lung volume, and increased airway inflammation compared with control animals. Furthermore, elastase- and LPS-exposed mice showed deficient IFN and IL-10 responses to viral infection. Mice exposed to elastase or LPS alone showed intermediate pathological and physiological changes and cleared RV from their lungs similar to PBS-treated mice.
MATERIALS AND METHODS
Animals.
Eight- to ten-week-old female C57BL/6 mice were purchased from Charles River Laboratories (Wilmington, MA) and housed in a pathogen-free facility. All experiments described herein were approved by the Animal Care and Use Committee of the University of Michigan.
Elastase and LPS exposure.
Animals were exposed by the intranasal route to 1.2 units of porcine pancreatic elastase (Elastin Products, Owensville, MO) on day 1 and 7 μg (∼70 endotoxin units) of LPS from Escherichia coli O26:B6 (Sigma-Aldrich, St. Louis, MO) on day 4 of the week for four consecutive weeks. In some experiments, mice were treated with elastase or LPS alone, once a week for 4 wk. One week after the last exposure to LPS or elastase, lung histology, volume, elasticity, cytokines, airway cholinergic responsiveness, and susceptibility to RV infection were assessed. Mice repeatedly treated with PBS instead of elastase and/or LPS were used as controls.
RV infection.
RV1B was purchased from American Type Culture Collection (ATCC; Manassas, VA). Viral stocks were generated by infecting H1 HeLa cells (ATCC) as described previously (36), and 50% tissue culture infectivity (TCID50) values of viral stock were determined by the Spearman-Karber method (23). One week after the 4-wk exposure to PBS, LPS, elastase, or elastase/LPS, mice were anesthetized briefly with isoflurane and inoculated with 50 μl (5 × 107 TCID50/mouse) of RV1B or uninfected HeLa cell supernatant (sham) by the intranasal route, as described (37).
Measurement of lung elasticity and airway cholinergic responsiveness.
Mice were anesthetized by intraperitoneal injection of ketamine (2.5–5 mg/100 g body wt). A steel cannula was inserted into the trachea and connected to a miniature computerized FlexiVent ventilator (Scireq, Montreal, Quebec, Canada). Pentobarbital sodium (2 mg/100 g body wt) was also given to provide further sedation and allow stabilization on the ventilator. To determine elastic recoil, lungs were gradually inflated to 30 cmH2O, and pressure and lung volume was measured continuously during inflation and deflation of the lungs. Elastance and compliance were recorded by inflating the lungs to full capacity. Airway responsiveness to methacholine was measured by nebulizing increasing doses of methacholine. Airway resistance was measured every 15 s for a period of 3 min, and the highest resistance recorded was considered for calculation (37).
Total lung volume, lung histology, and morphometry.
Lungs were inflated at a constant pressure of 30 cmH2O for 30 min, and the lung volume was measured by fluid displacement. For histological evaluation, inflated lungs were embedded in paraffin, and 5-μm-thick sagittal sections were stained with hematoxylin and eosin or periodic acid-Schiff (PAS) reagent. Alveolar chord length was determined using sagittal sections obtained at 5-mm intervals through the length of the lungs, and diameter of the air spaces measured in random areas was measured using NIH Image J analysis software (38). The airway wall thickness (between the basement membrane and adventitia) of non-cartilageous bronchioles (excluding terminal bronchioles) was also measured.
Lung inflammatory cells.
Mice were euthanized, and lungs were lavaged with PBS containing 5 mM EDTA. Total and differential cell counts were determined as described previously (37). Bronchoalveolar lavage cells were immunolabeled with antibodies to CD4, CD8, CD11b, CD11c, and CD19 and analyzed by flow cytometry.
Viral titers in infected animals.
Lung homogenates from mice were subjected to two freeze-thaw cycles and centrifuged. Viral titers (TCID50) in lung homogenate supernatants were determined as described previously (23), with some modifications. HeLa cells (1 × 104/well) were mixed with 10-fold serial dilutions of lung homogenates and plated in 96-well plates in DMEM containing 10% serum, 5 mM l-glutamine, and penicillin (50 U/ml)/streptomycin (50 μg/ml). Cells were incubated for 3 days, the cytopathic effect was scored, and data were presented as TCID50/ml.
Quantitative real-time PCR.
Total RNA from lungs was used to quantify viral RNA, IFNα, IFNβ, IFNγ, IRF-7, TNFα, IL-5, IL-10, IL-13, muc5AC, and muc5B mRNA levels by quantitative real-time PCR using specific primers.
Lung cytokines and MPO activity.
Mice were euthanized at predetermined time points. Lungs were collected and homogenized in PBS containing complete protease inhibitors (Roche, Indianapolis, IN). Cytokine protein levels were measured either by ELISA (R&D Systems, Minneapolis, MN) or multiplex immunoassay (BioRad, Hercules, CA). MPO activity was measured by EnzCheck MPO activity kit (Invitrogen) following the manufacturer's instructions.
Immunofluorescence staining.
Deparaffinized and hydrated lung sections were heated at 120°C under pressure in 0.1 M citrate buffer (pH 6.0) to unmask antigens. Sections were blocked with 5% normal donkey serum and incubated with RV1B antiserum (ATCC). Bound antibody was recognized with second antibody conjugated with Alexa Fluor 488 (Invitrogen). Sections were counterstained with Mayer's hematoxylin (Sigma-Aldrich) and visualized by fluorescence microscopy (37).
Statistical analysis.
Results are expressed as means ± SD or geomean with complete range of data. Data were analyzed by using SigmaStat statistical software (Systat Software, San Jose, CA). One- or two-way ANOVA with Tukey-Kramer post hoc analysis was performed as appropriate to compare groups, and a P value < 0.05 was considered significant.
RESULTS
Histological evaluation of the lungs.
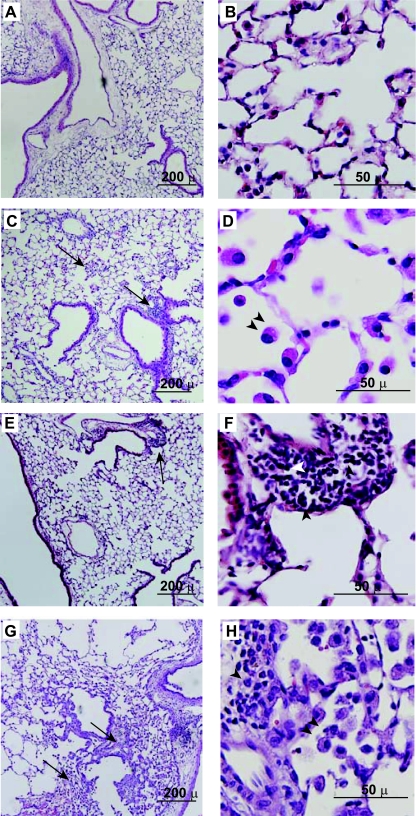
Seven days after the final treatment with LPS, elastase, elastase/LPS, or PBS, mice were euthanized for histological examination. PBS-treated mice showed normal histology with no accumulation of inflammatory cells in the alveolar space (Fig. 1, A and B). Mice treated with LPS (Fig. 1, C and D) or elastase alone (Fig. 1, E and F) showed mild peribronchiolar and perivascular inflammation, with neutrophils and lymphocytes being the major inflammatory cells in LPS-treated mice and macrophages in elastase-treated mice. In contrast, elastase/LPS-treated mice showed widespread lung inflammation (Fig. 1, G and H). Large aggregates of mononuclear inflammatory cells and neutrophils were noted in both the peribronchiolar and perivascular spaces. We also observed accumulation of mononuclear cells in the air spaces.
Fig. 1.
Elastase/LPS treatment induced parenchymal and airway inflammation. Formalin-fixed, paraffin-embedded lungs harvested from PBS, elastase, LPS, or a combination of elastase/LPS-treated mice were stained with hematoxylin and eosin (H&E). PBS-treated mice (A and B) showed no obvious inflammation. Elastase-treated mice (C and D) showed mild inflammation with macrophages (arrowheads) being the predominant cell type. LPS-treated mice (E and F) showed mild inflammation with lymphocytes and neutrophils (arrowhead) being predominant cell types. Elastase/LPS-treated mice (G and H) showing moderate widespread inflammation with neutrophils (single arrowhead) and macrophages (double arrowheads). Arrows in C, E, and G show inflammatory foci. Images shown are typical of 4–6 independent experiments.
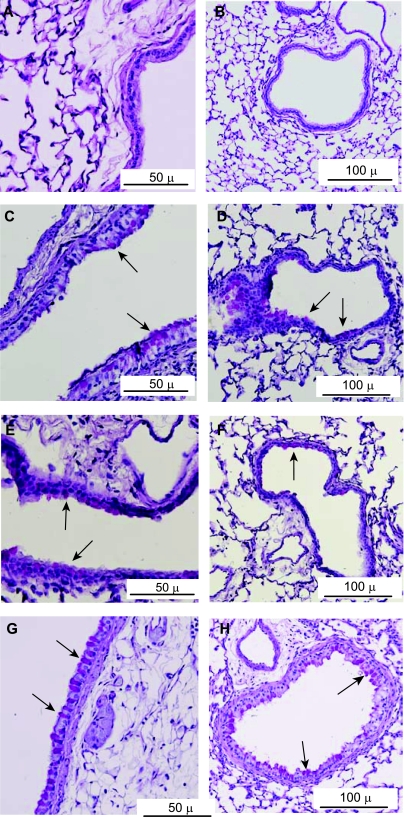
PBS-treated mice showed very few PAS-positive cells in the large airways and none in the small airways (Fig. 2, A and B). LPS- or elastase-treated mice showed more PAS-positive cells in both the large and small airways (Fig. 2, C–F). Compared with mice treated with elastase or LPS alone, mice treated with a combination of elastase and LPS showed a further increase in the number of PAS-positive cells in both the large and small airways (Fig. 2, G and H). Immunostaining of lung sections with muc5AC antibody indicated that PAS-positive cells in the airways were in fact mucin-producing goblet cells (Supplemental Fig. 1. Supplemental data for this article is available online at the AJP-Lung web site.).
Fig. 2.
Elastase/LPS treatment induced goblet cell metaplasia. Paraffin lung sections of mice were stained with periodic acid-Schiff (PAS) reagent. PBS-treated mice did not show an increase in PAS-positive cells in either large or small airways (A and B). Elastase (C and D) or LPS-treated mice show few PAS-positive cells (arrows) in both large (C and E) and small airways (D and F). Elastase/LPS-treated mice show abundant PAS-positive cells (arrows) in large (G) and small airways (H), respectively. Images shown are typical of 4–6 independent experiments.
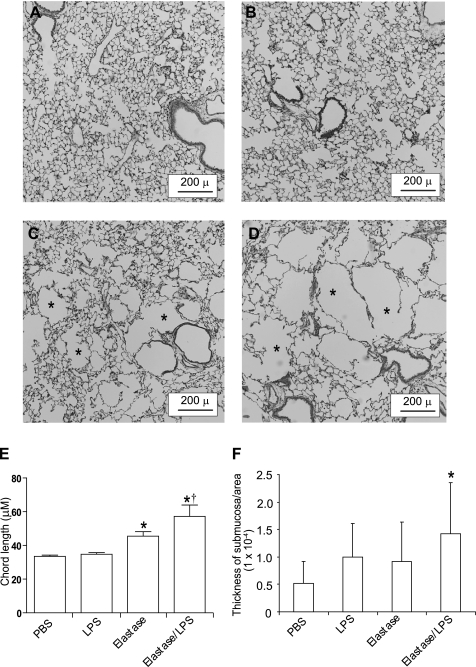
Examination of parenchyma indicated normal alveoli in mice treated with PBS or LPS (Fig. 3, A and B). By morphometric analysis, average chord length in PBS-treated mice was found to be 33 μM, similar to an earlier report (45). LPS treatment did not increase the chord length, consistent with the histological observations. In contrast, mice treated with elastase alone or elastase/LPS showed alveolar destruction, which resulted in enlarged air spaces, an indication of emphysematous change (Fig. 3, C and D). Elastase-treated mice showed a small but significant increase in mean chord length over PBS-treated control mice. Elastase/LPS mice showed almost a twofold increase in mean chord length over PBS-treated control mice, which was significantly higher than that observed in mice treated with PBS, LPS, or elastase alone (Fig. 3E). Morphometric analysis of the small airways indicated significantly increased airway wall thickness in elastase/LPS-treated mice compared with PBS-treated control mice (Fig. 3F).
Fig. 3.
Emphysematous changes and airway remodeling in elastase/LPS-treated mice. Lungs of PBS, elastase, or elastase/LPS-treated mice were inflated to an identical pressure, processed for paraffin embedding, and stained with H&E. A: lungs from PBS- (A) or LPS-treated (B) mice showed normal alveolar morphology. Elastase- (C) or elastase/LPS-treated (D) mice showed mild and moderate emphysema (*), respectively. Images are representative of 4–6 independent experiments. E: the diameter of the air spaces was measured in at least 10 random fields per slide and averaged to determine alveolar chord length. Lungs of elastase- and elastase/LPS-treated mice showed increased mean chord length compared with PBS- or LPS-treated mice. F: airway wall thickness was increased in elastase/LPS-treated mice compared with PBS-, elastase-, or LPS-treated mice. N = 4–6, means ± SD, *different from PBS group, P ≤ 0.05; †different from all other groups, P ≤ 0.05, 1-way ANOVA.
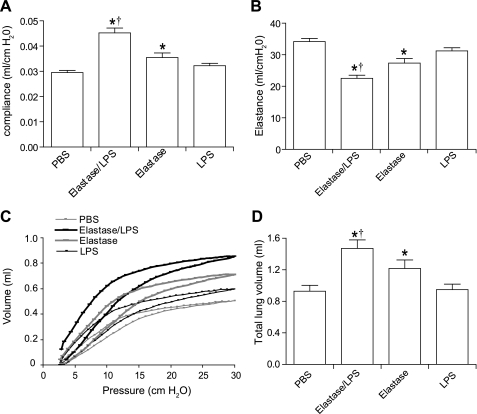
Lung function and volume.
To assess elasticity of the lungs, we determined total respiratory system compliance, elastance, and the pressure-volume (PV) relationship during air inflation for at least six mice from each group. Compared with PBS-treated control mice, compliance was significantly increased in mice treated with elastase and elastase/LPS, but not those treated with LPS alone (Fig. 4A). Mice treated with elastase alone and elastase/LPS also showed decreased elastance compared with PBS-treated mice (Fig. 4B). Consistent with these observations, elastase/LPS-treated mice always showed an upward and leftward shift in the PV relationship compared with PBS-treated mice, demonstrative of reduced elastic recoil (Fig. 4C). LPS- or elastase-treated mice showed smaller changes. Total lung volume at a constant pressure of 30 cmH2O was also significantly increased in elastase/LPS-treated mice (Fig. 4B). LPS/elastase-treated mice showed a statistically significant increase in basal airway resistance (0.84 ± 0.03 cmH2O·ml−1·s−1) compared with PBS-treated controls (0.66 ± 0.01 cmH2O·ml−1·s−1). However, there was no significant difference in airway responsiveness to methacholine challenge between the two groups (see below).
Fig. 4.
Compliance, elastance, elastic recoil, and total lung volume. Mice were anesthetized and compliance (A), elastance (B), and pressure-volume relationships were (C) measured using the Flexivent system. Elastase- and elastase/LPS-treated mice showed an increase in compliance, a decrease in elastance, and a left shift of PV-loop compared with PBS- or LPS-treated mice (gray). Data are representative of at least 6 animals per group. B: with the chest closed, lungs were instilled with buffered formalin at 30 cmH2O constant pressure for 30 min via a catheter inserted into the trachea, and total lung volume was measured by volume displacement. Elastase- and elastase/LPS-treated mice showed higher total lung volume than the PBS-treated mice. Data in A, B, and D represent means and SD calculated from 6–8 animals per group, *different from PBS group, P ≤ 0.05; †different from all other groups, P ≤ 0.05, 1-way ANOVA. A representative PV curve from 4 to 6 mice from each group is shown in C.
Lung inflammation.
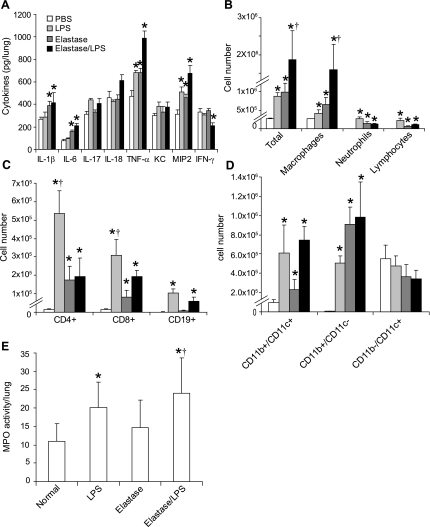
To examine whether these structural and morphological changes were associated with altered cytokine levels in the lungs, we measured the protein levels of IL-1β, IL-6, IL-17, IL-18, TNFα, KC, MIP-2/CXCL2, and IFNγ by ELISA. The proinflammatory cytokines IL-1β, IL-6, and TNFα, as well as the neutrophil chemoattractant MIP2, were significantly increased in LPS-, elastase-, and elastase/LPS-treated mice compared with PBS-treated mice (Fig. 5A). However, elastase/LPS mice showed higher increases in the aforementioned cytokine levels than the mice treated with LPS or elastase alone. Elastase/LPS-treated mice also showed a small but statistically significant decrease in IFNγ compared with mice in other groups. These results indicate that inflammatory changes in elastase/LPS-treated mice are associated with an altered expression of cytokines.
Fig. 5.
Lung inflammation. A: supernatants from lung homogenates were analyzed by Bioplex ELISA to determine cytokine levels. Elastase-, LPS-, and elastase/LPS-treated mice showed significant increases in IL-1β, IL-6, TNFα, and MIP-2, and elastase/LPS mice showed a decrease in IFNγ- compared with PBS-treated mice. B: BAL was performed in PBS-, elastase-, LPS-, and elastase/LPS-treated mice, and total and differential cell counts were determined. Compared with PBS-treated mice, LPS-, elastase-, or elastase/LPS-treated mice showed higher total cell counts and increased macrophages, lymphocytes, and neutrophils. Elastase/LPS-treated mice showed significant increases in total cell counts and macrophages compared with all other groups. C and D: immunolabeling and flow cytometric analysis of BAL cells revealed that elastase- and elastase/LPS-treated mice showed increased numbers of CD4+, CD8+, and CD19+ lymphocytes, CD11b+/CD11c− monocytes, and the CD11b+/CD11c+ mononuclear cell population compared with PBS-treated mice. LPS-treated mice showed increases in CD4+ and CD8+ lymphocytes and the CD11b+/CD11C− and CD11b+/CD11c+ cell population. E: MPO activity in the lung homogenates of elastase/LPS-treated mice was greater than in PBS-, LPS-, or elastase-treated mice. N = 6, *different from PBS group, P ≤ 0.05; †different from all other groups, P ≤ 0.05, 1-way ANOVA.
Analysis of cells in bronchoalveolar lavage (BAL) fluid indicated an increased number of total cells in LPS-, elastase-, and elastase/LPS-treated mice compared with PBS-treated controls (Fig. 5B). However, elastase/LPS-treated mice showed almost twofold more cells than mice treated with LPS or elastase alone. The number of macrophages, neutrophils, and lymphocytes was significantly increased in LPS-, elastase-, and elastase/LPS-treated mice compared with PBS-treated controls. LPS-treated mice showed more neutrophils and lymphocytes compared with mice treated with either elastase alone or elastase/LPS. Further analysis of BAL cells by immunolabeling followed by flow cytometry revealed 10-fold or greater increases in number of CD4+ and CD8+ T lymphocytes in all three treatment groups and CD19+ B lymphocytes in only LPS- and elastase/LPS-treated mice (Fig. 5). Again, LPS-treated mice showed a larger increase in the lymphocyte population compared with the other two groups. There were also increases in the numbers of monocytes (CD11b+/CD11c−, low-autofluorescence cells) in LPS- and elastase/LPS-treated mice compared with PBS-treated controls, perhaps reflecting recruitment of monocytes from the bone marrow (17). The CD11b+/CD11c+ population (which includes inflammatory macrophages and immature dendritic cells) was also increased in LPS- and elastase/LPS-treated mice compared with PBS-treated controls, whereas numbers of mature alveolar macrophages (CD11b−/CD11c+, high-autofluorescence cells) did not differ significantly (Fig. 5). Lung homogenate MPO activity was significantly increased in LPS- and elastase/LPS-treated mice (Fig. 5) compared with PBS-treated mice, consistent with the observed increase in neutrophils. Although elastase-treated mice showed an increase in MPO activity compared with PBS mice, the difference was not statistically significant. Together, these results suggest that the combination of elastase and LPS induces more dramatic alterations in lung function and histology than either agent alone. For this reason, we focused subsequent studies on the outcome of RV infection on elastase/LPS-treated mice. For comparison, a limited number of studies were also performed in mice treated with elastase or LPS alone.
RV infection.
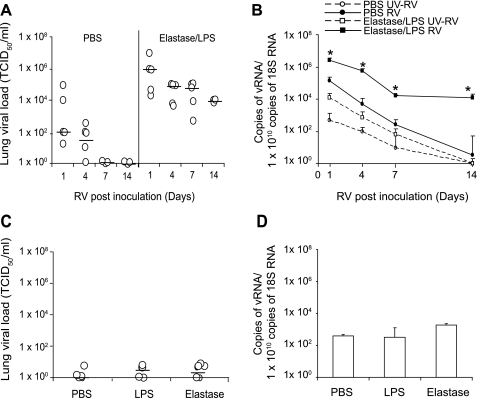
Recently, we have demonstrated the feasibility of infecting mice with RV1B, a minor group virus that binds to low-density lipoprotein family receptors (37). PBS- or elastase/LPS-treated mice were intranasally inoculated with 5 × 107 50% tissue-culture infective dose (TCID50) RV1B, replication-deficient UV-irradiated RV1B (UV-RV1B), or sham HeLa cell supernatant 1 wk after the last exposure to elastase/LPS. RV-infected PBS mice showed low levels of replicating virus up to 4 days postinfection, as measured by TCID50. In contrast, RV-infected elastase/LPS mice showed virus up to 14 days after infection (Fig. 6A), and viral titers were 4–5 log higher than corresponding RV-infected PBS mice at all time points examined. None of the mice infected with UV-RV1B or treated with sham showed replicating virus in their lungs (data not shown). We then measured levels of viral RNA (vRNA), which can also elicit inflammation (37). PBS mice showed the presence of vRNA 1 and 4 days postinfection, whereas elastase/LPS mice showed vRNA up to 14 days after inoculation, at significantly higher levels than their respective PBS-treated mice (Fig. 6B). Mice infected with UV-irradiated RV1B showed 2–3 log lower levels of vRNA compared with respective RV-infected animals. Mice treated with LPS or elastase alone before RV1B infection were examined for viral titer and viral RNA at 7 days postinfection. Both groups of mice showed negligible viral titers and vRNA in their lungs at that time point (Fig. 6, C and D), similar to PBS-treated mice.
Fig. 6.
Persistence of rhinovirus (RV) in elastase/LPS-treated mice. PBS or elastase/LPS mice were inoculated with RV1B or UV-RV1B and killed 1, 4, 7, or 14 days postinoculation. A and B: viral load and copy number in lung homogenates were determined by cytopathic assay and quantitative PCR, respectively, in PBS- or elastase/LPS-treated mice. Lung homogenates from mice infected with UV-RV1B did not show a cytopathic effect; therefore, data are not presented. C and D: mice treated with PBS, elastase, or LPS were inoculated with RV and killed 7 days later. Viral load and copy number were determined by cytopathic assay and quantitative RT-PCR, respectively. Data points in A and C indicate the range of values, and the bar represents median. B and D: data represent geometric mean and SE (n = 6, *P < 0.05, 2-way ANOVA).
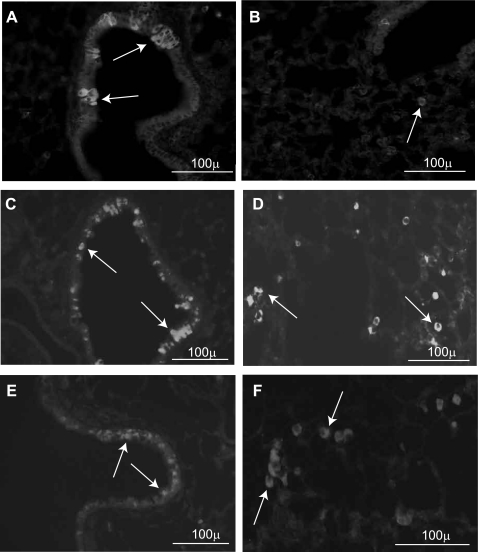
We next examined the lungs from RV-infected PBS and elastase/LPS-treated mice for the presence of virus by immunofluorescence staining. As observed previously (37), anti-RV1B immunofluorescence staining of lung sections from PBS-treated mice showed occasional RV1B-positive cells in the airway epithelium and surrounding peribronchium, likely indicating the infection of inflammatory cells (Fig. 7, A and B). Immunostaining was observed 1 but not 4 days after initial infection, consistent with viral titers. Elastase/LPS-treated mice exhibited abundant RV-positive cells in the airway epithelium (Fig. 7C) as well as in the lung parenchyma, where the signals were predominantly found in infiltrating inflammatory cells (Fig. 7D). Infection of lung cells was also observed, albeit at a lower level, in day 14 mice (Fig. 7, E and F). Together, these results indicate that RV persists at higher levels and for a longer period in elastase/LPS mice than PBS mice.
Fig. 7.
Immunolocalization of RV in mouse lungs. PBS- (A and B) and elastase/LPS-treated mice were inoculated with RV and killed 1 or 14 days later. Paraffin lung sections were immunostained with antibody to RV1B, and bound antibody was detected by anti-guinea pig IgG conjugated with Alexa Fluor 488. All panels are representative of 3 animals per group. A and B show the presence of RV in occasional airway epithelial cells and inflammatory cells in PBS-treated mice 1 day postinfection. C and D show the presence of RV in airway and alveolar inflammatory cells, respectively, 1 day postinoculation, in elastase/LPS-treated mice. E and F show the persistence of RV in small airway and alveolar inflammatory cells 14 days postinoculation in elastase/LPS-treated mice. Arrows represent examples of RV-positive cells.
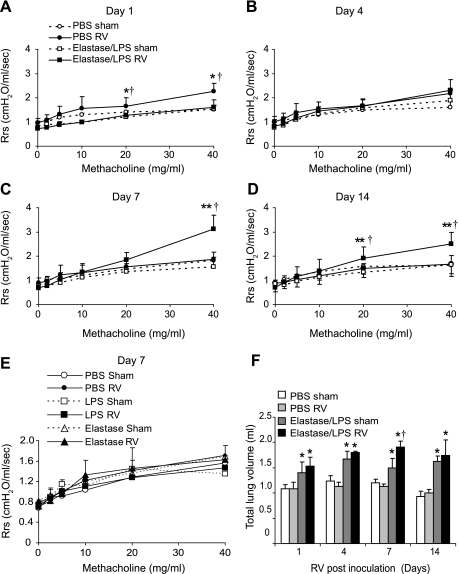
RV-induced changes in airway responsiveness and lung volume.
Airway cholinergic responsiveness was measured in anesthetized tracheotomized animals (Fig. 8, A–D). PBS-treated mice inoculated with RV1B showed hyperresponsiveness to methacholine challenge on day 1 and returned to normal by day 4. In contrast, elastase/LPS-treated mice inoculated with RV1B showed a delayed increase in airway responsiveness that appeared at day 7 and persisted to day 14. Persistence of airway hyperresponsiveness after RV infection may relate in part to the observed airway remodeling (Fig. 3F). Similar to PBS-treated mice, RV1B infection of mice treated with elastase or LPS alone showed normal airway responsiveness at 7 days postinoculation (Fig. 8E).
Fig. 8.
Measurement of airway responsiveness. PBS-, elastase-, LPS-, and elastase/LPS-treated mice were inoculated with RV1B, and airway responsiveness to inhaled methacholine was measured. A–D represents airway resistance at 1, 4, 7, or 14 days postinoculation, respectively, in PBS- or elastase/LPS-treated mice. E: airway resistance in PBS-, elastase-, and LPS-treated mice at 7 days postinoculation. F: total lung volume was measured at a constant pressure of 30 cmH2O. N = 4–6; †different from respective sham-infected mice, P ≤ 0.05; *different from elastase/LPS group, P ≤ 0.05; **different from PBS group, P ≤ 0.05, 2-way ANOVA.
We also examined total lung volume at a constant distending pressure of 30 cmH2O. In PBS-treated mice, there was no change in lung volume 1–14 days after RV inoculation. In contrast, elastase/LPS mice, which demonstrated increased total lung volume under basal conditions, showed a further increase 7 days after RV inoculation (Fig. 7F). Inoculation with UV-RV1B had no effect on total lung volume in either PBS or elastase/LPS mice (not shown). These results suggest that infection with RV induces airway narrowing, with consequent hyperinflation, in elastase/LPS-treated mice, but not mice treated with PBS, elastase, or LPS alone.
IFN levels in RV-infected mice.
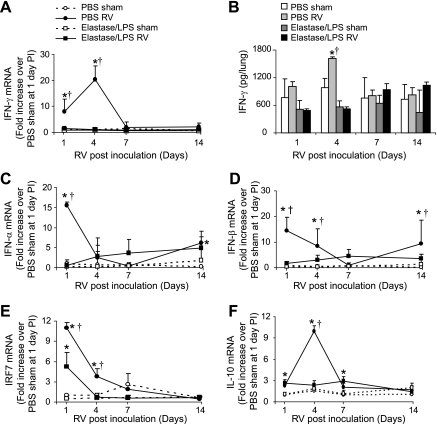
Viral clearance has been shown to depend in part on IFN production. We therefore measured IFNγ mRNA and protein levels by quantitative PCR and ELISA. PBS-treated control mice inoculated with RV1B showed increased IFNγ mRNA and protein levels on day 4 postinfection (Fig. 9, A and B), whereas elastase/LPS-treated mice inoculated with RV1B failed to show such an increase. mRNA levels of IFNα and IFNβ also did not increase in elastase/LPS-treated mice upon RV inoculation (Fig. 9, C and D). In addition, elastase/LPS-treated mice inoculated with RV showed lower expression of interferon response factor (IRF)-7 and IL-10 than similarly inoculated PBS-treated mice (Fig. 9, E and F). These results provide a partial mechanistic explanation for the failure of elastase/LPS-treated mice to clear RV from their lungs efficiently.
Fig. 9.
Expression of IFNs and IL-10. PBS or elastase/LPS mice were inoculated with RV1B and euthanized 1, 4, 7, or 14 days postinoculation (PI) by qPCR and ELISA. A and B: whole lung mRNA and protein levels, respectively, of IFNγ; mRNA levels of IFNα (C), IFNβ (D), IRF-7 (E), and IL-10 (F). N = 3–5, *different from respective sham-infected mice, P ≤ 0.05; †different from elastase/LPS group, P ≤ 0.05, 2-way ANOVA.
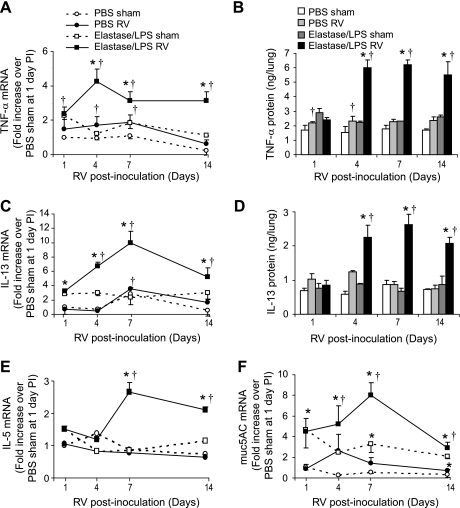
Analysis of differential cell counts and histological evaluation revealed a short-lived increase in neutrophils in both groups of mice inoculated with RV compared with their respective sham-infected animals (not shown). We examined the expression of TNFα and IL-13, each of which have been shown to increase airway responsiveness (9, 16, 27, 50). mRNA levels of both TNFα (Fig. 10A) and IL-13 (Fig. 10C) were significantly higher in RV-inoculated elastase/LPS-treated mice. Changes in mRNA were accompanied by increased protein levels of TNFα (Fig. 10B) and IL-13 (Fig. 10D) in the lung homogenates. We also observed increased mRNA expression of another Th2 cytokine, IL-5, in elastase/LPS-treated mice compared with PBS-treated mice (Fig. 10E).
Fig. 10.
Expression of IL-13, TNFα, and muc5AC. Lung mRNA levels of TNFα (A), IL-13 (C), IL-5 (E), and muc5AC (F) were measured by qRT-PCR. Lung protein levels of TNFα (B) and IL-13 (D) were measured by Bioplex ELISA. N = 5, †different from respective sham-infected mice, P ≤ 0.05; *different from elastase/LPS group, P ≤ 0.05; 2-way ANOVA.
Mucus plugging of the airways is one of the cardinal features of COPD, and RV has been shown to increase mucus secretion in vitro and in vivo (4, 21, 52). We examined expression of the mucin genes muc5B and muc5AC by real-time quantitative PCR. RV inoculation of PBS-treated mice caused a twofold increase in muc5AC expression on day 4, which returned to baseline by day 7 (Fig. 10F). Elastase/LPS-treated mice showed fourfold higher muc5AC levels than PBS-treated mice under basal conditions, which further increased after RV inoculation. This difference persisted up to 14 days after infection. No difference in expression levels of muc5B transcripts was observed between RV and sham-inoculated animals (not shown).
DISCUSSION
A growing body of evidence implicates viral upper respiratory infection as an important cause of AE-COPD. AE-COPD are more frequent during winter months when respiratory viral infections are prevalent and often preceded by clinical symptoms of the common cold. RV is the most common viral pathogen in AE-COPD (43). However, the mechanisms by which RV causes exacerbations in COPD patients are not well understood, in part due to the lack of suitable animal model. We and others recently showed that mice inoculated with RV1B, which replicates in mouse airway epithelial cells (46), show neutrophilic airway inflammation, evidence of RV replication in vivo, and hyperresponsiveness up to 4 days after inoculation (4, 37). In the present study, we show that, upon RV infection, elastase and LPS-treated mice with structural and functional lung changes reminiscent of COPD show delayed and persistent airway hyperresponsiveness, a significant increase in total lung volume and mucin expression, and viral persistence up to 14 days after infection. As far as we are aware, this is the first study examining the innate immune response to viral infection in animals with a phenotype resembling COPD. Our data parallel findings in a pilot study of experimental RV infection of COPD patients (31). In the latter study, RV infection was associated with lower respiratory tract symptoms, reduced airway function and replication, and persistence of virus up to 11 days after inoculation.
Persistence of RV was associated with deficient IFN and IL-10 responses, and augmented IL-5 and IL-13 responses, indicating at least two potential mechanisms for reduced clearance and increased severity of lung disease. IFNs play an important role in limiting viral spread in the early stages of infection. In the present study, RV-infected, elastase/LPS-treated mice failed to show significant increases in lung IFN. RV-infected elastase/LPS mice also showed reduced expression of IRF-7, which is required for maximal IFNγ expression (41). A similar deficiency in the IFN response to RV has been shown in experimentally infected asthmatic patients (8, 32, 49). Studies of BAL T cells from COPD patients tend to show a decreased percentage of IFNγ-producing cells following anti-CD3/anti-CD28 antibody stimulation (3), consistent with the notion of a deficient IFNγ response during AE-COPD.
IL-10, an immunomodulatory cytokine, blocks proinflammatory cytokine production by inhibiting T cells and preventing the maturation of dendritic cells, suggesting that IL-10 plays a role in maintaining chronicity and pathogenicity in chronic infections (12). In the present study, elastase/LPS-treated mice with increased viral loads showed reduced IL-10 responses, consistent with the notion that IL-10 production provides an element of protection against RV infection. BAL cells from atopic asthmatic subjects show a deficient IL-10 response that correlates with increased viral load, lower airway inflammation, and lung function impairment in response to experimental RV infection (32). Furthermore, lung tissue from COPD patients show decreased LPS-induced IL-10 release compared with lung tissue from patients with normal lung function (18). Together, these data suggest that differences in the production of IL-10 may have important biological implications for AE-COPD.
Recently, cigarette smoke was shown to enhance the inflammatory, remodeling, and apoptotic effects of influenza virus in the lung (25). In particular, 2 wk of cigarette smoke exposure increased the induction of IL-18, IL-12/IL-23 p40, and IFNγ caused by influenza virus. However, there was no effect on viral titer. In the present study, elastase/LPS enhanced the inflammatory effects of RV in the lung, including enhanced induction of TNFα, IL-13, and IL-5. However, in our study, IL-10 and IFNγ were decreased, and viral load increased. These differences could be attributed to disparities in the animal models used, as 2 wk of cigarette smoke exposure is insufficient to generate a COPD phenotype. It is also possible that the observed discrepancies in the response to infection could be due to differences in the viruses themselves.
In general, Th1-dominated tissue inflammation, including the increased production of IL-10 and IFNγ by activated T cells, is believed to play a central role in COPD pathogenesis, particularly in development of emphysema (10, 13, 15, 30). Most recently, administration of cigarette smoke and synthetic double-stranded RNA was shown to induce IFNγ-dependent emphysema in mice (25). On the other hand, transgenic overexpression of the Th2 cytokine IL-13 also induces emphysema (48), and Sendai virus infection induces IL-13-dependent chronic lung disease in mice (26). Increased levels of Th2 cytokines have been found in patients with COPD, especially in patients who fulfill the criteria for diagnosis of chronic bronchitis (2, 34, 35). In the present study, levels of IL-13 and IL-5 were higher in RV-inoculated elastase/LPS-treated mice. These results are compatible with a distinction between a general Th1 cytokine response underlying progression of COPD, especially of its emphysematous component, and a defective Th1/Th2 balance during AE-COPD, or in chronically infected airways.
Expression of ICAM-1, a receptor for major group RV, is increased in the airway submucosa of patients with COPD (53). Our preliminary studies suggest that ICAM-1 expression is also increased in the airway epithelial cells of these patients (D. Schneider, M. Hershenson, U. Sajjan, unpublished observations). It is therefore conceivable that an increase in the expression in viral receptors plays a role in the increased susceptibility to RV observed in elastase/LPS-treated mice. Oxidative stress is another factor that can affect responses to acute viral infections. Cigarette smoke-induced oxidative stress has been shown to attenuate IFN production in response to double-stranded RNA (5). Our ongoing studies indicate that compared with PBS-treated control mice, elastase/LPS-treated mice show increased lung levels of thiobarbituric acid reactive substances, a measure of lipid peroxidation caused by oxidative stress (Ganesan, Hershenson, and Sajjan, unpublished results), and this could contribute the observed susceptibility of these mice to RV infection.
In RV-infected elastase/LPS-treated mice, airway hyperresponsiveness 7–14 days postinoculation paralleled increases in IL-13, TNFα, and Muc5AC expression. IL-13 increases airway responsiveness and mucus secretion via the IL-4 receptor/signal transducers and activators of transcription (STAT)-6 pathway (51). TNFα acts synergistically with IL-13 to increase the smooth muscle response to cholinergic compounds (9). Recently, RV infection was shown to induce Muc5AC expression in human bronchial epithelial cells by activation of epidermal growth factor receptor (EGFR) signaling (54). Increased Muc5AC expression is present in the bronchial epithelium of COPD patients (7). IL-13 and EGFR activation may therefore contribute to RV-induced airway hyperresponsiveness.
Finally, we would like to note the similarities and differences between our mouse model of elastase and LPS exposure, other animal models of COPD, and human COPD. COPD has been modeled by exposure to cigarette smoke, chemicals, gases, proteases, and LPS, as reviewed in Ref. 29. Mice exposed to cigarette smoke for 6 mo develop pulmonary emphysema, inflammation, and accumulation of macrophages in the alveoli, but do not show small airway obstruction or goblet cell metaplasia. Intratracheal administration of tissue-degrading enzymes such as elastase also leads to emphysematous lung lesions, but without obvious remodeling of small airways. As noted above, long-term intratracheal exposure to LPS (twice a week for 3 mo) causes both airway and alveolar changes that persist up to 8 wk after the final LPS administration (47). In our model, adding elastase to LPS decreased the required exposure time to 1 mo; furthermore, intranasal rather than intratracheal installation was sufficient to induce structural and function changes typical of COPD including pulmonary emphysema, loss of lung elastic recoil, hyperinflation, diffuse lung inflammation, goblet cell metaplasia, airway remodeling, and markedly increased numbers of neutrophils, T and B lymphocytes, monocytes, and immature macrophages in the airways and alveoli. Morphological and inflammatory changes were accompanied by increases in lung IL-1β, IL-6, TNFα, and MIP-2/CXCL2, as seen in humans with COPD (8). These morphological and inflammatory changes lasted up to 8 wk after exposure (not shown). Most significantly, elastase and LPS treatment was associated with an impaired innate immune response to infection with RV, a clinically relevant viral pathogen. In contrast, mice treated with elastase or LPS alone for 4 wk showed intermediate changes in lung histology and no difference in RV clearance. On the other hand, we did not observe an increased ratio of CD8+/CD4+ cells, as observed in human COPD.
In summary, we have shown that, in elastase/LPS-treated mice with histological and functional changes typical of COPD, clearance of RV from the lungs is limited, leading to prolonged airway hyperresponsiveness and lung hyperinflation, thus contributing to disease progression. Additional studies employing this combined mouse model of COPD and RV infection may provide further insight into cellular mechanisms of COPD exacerbation.
GRANTS
This work was supported by National Institutes of Health Grants HL-81420 and HL-82550 (M. B. Hershenson), AT-004793 (U. Sajjan), and HL-082480 (J. L. Curtis) and the Biomedical and Laboratory Research and Development Service, Department of Veterans Affairs.
Supplementary Material
REFERENCES
- 1.Bandi V, Apicella MA, Mason E, Murphy TF, Siddiqi A, Atmar RL, Greenberg SB. Nontypeable Haemophilus influenzae in the lower respiratory tract of patients with chronic bronchitis. Am J Respir Crit Care Med 164: 2114–2119, 2001 [DOI] [PubMed] [Google Scholar]
- 2.Barcelo B, Pons J, Fuster A, Sauleda J, Noguera A, Ferrer JM, Agusti AG. Intracellular cytokine profile of T lymphocytes in patients with chronic obstructive pulmonary disease. Clin Exp Immunol 145: 474–479, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barczyk A, Pierzchala W, Kon OM, Cosio B, Adcock IM, Barnes PJ. Cytokine production by bronchoalveolar lavage T lymphocytes in chronic obstructive pulmonary disease. J Allergy Clin Immunol 117: 1484–1492, 2006 [DOI] [PubMed] [Google Scholar]
- 4.Bartlett NW, Walton RP, Edwards MR, Aniscenko J, Caramori G, Zhu J, Glanville N, Choy KJ, Jourdan P, Burnet J, Tuthill TJ, Pedrick MS, Hurle MJ, Plumpton C, Sharp NA, Bussell JN, Swallow DM, Schwarze J, Guy B, Almond JW, Jeffery PK, Lloyd CM, Papi A, Killington RA, Rowlands DJ, Blair ED, Clarke NJ, Johnston SL. Mouse models of rhinovirus-induced disease and exacerbation of allergic airway inflammation. Nat Med 14: 199–204, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bauer CM, Dewitte-Orr SJ, Hornby KR, Zavitz CC, Lichty BD, Stampfli MR, Mossman KL. Cigarette smoke suppresses type I interferon-mediated antiviral immunity in lung fibroblast and epithelial cells. J Interferon Cytokine Res 28: 167–179, 2008 [DOI] [PubMed] [Google Scholar]
- 6.Brass DM, Hollingsworth JW, Cinque M, Li Z, Potts E, Toloza E, Foster WM, Schwartz DA. Chronic LPS inhalation causes emphysema-like changes in mouse lung that are associated with apoptosis. Am J Respir Cell Mol Biol 39: 584–590, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Caramori G, Di Gregorio C, Carlstedt I, Casolari P, Guzzinati I, Adcock IM, Barnes PJ, Ciaccia A, Cavallesco G, Chung KF, Papi A. Mucin expression in peripheral airways of patients with chronic obstructive pulmonary disease. Histopathology 45: 477–484, 2004 [DOI] [PubMed] [Google Scholar]
- 8.Contoli M, Message SD, Laza-Stanca V, Edwards MR, Wark PA, Bartlett NW, Kebadze T, Mallia P, Stanciu LA, Parker HL, Slater L, Lewis-Antes A, Kon OM, Holgate ST, Davies DE, Kotenko SV, Papi A, Johnston SL. Role of deficient type III interferon-lambda production in asthma exacerbations. Nat Med 12: 1023–1026, 2006 [DOI] [PubMed] [Google Scholar]
- 9.Deshpande DA, Dogan S, Walseth TF, Miller SM, Amrani Y, Panettieri RA, Kannan MS. Modulation of calcium signaling by interleukin-13 in human airway smooth muscle: role of CD38/cyclic adenosine diphosphate ribose pathway. Am J Respir Cell Mol Biol 31: 36–42, 2004 [DOI] [PubMed] [Google Scholar]
- 10.Di Stefano A, Caramori G, Capelli A, Gnemmi I, Ricciardolo FL, Oates T, Donner CF, Chung KF, Barnes PJ, Adcock IM. STAT4 activation in smokers and patients with chronic obstructive pulmonary disease. Eur Respir J 24: 78–85, 2004 [DOI] [PubMed] [Google Scholar]
- 11.Eller J, Ede A, Schaberg T, Niederman MS, Mauch H, Lode H. Infective exacerbations of chronic bronchitis: relation between bacteriologic etiology and lung function. Chest 113: 1542–1548, 1998 [DOI] [PubMed] [Google Scholar]
- 12.Filippi CM, von Herrath MG. IL-10 and the resolution of infections. J Pathol 214: 224–230, 2008 [DOI] [PubMed] [Google Scholar]
- 13.Freeman CM, Curtis JL, Chensue SW. CC chemokine receptor 5 and CXC chemokine receptor 6 expression by lung CD8+ cells correlates with chronic obstructive pulmonary disease severity. Am J Pathol 171: 767–776, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greenberg SB, Allen M, Wilson J, Atmar RL. Respiratory viral infections in adults with and without chronic obstructive pulmonary disease. Am J Respir Crit Care Med 162: 167–173, 2000 [DOI] [PubMed] [Google Scholar]
- 15.Grumelli S, Corry DB, Song LZ, Song L, Green L, Huh J, Hacken J, Espada R, Bag R, Lewis DE, Kheradmand F. An immune basis for lung parenchymal destruction in chronic obstructive pulmonary disease and emphysema. PLoS Med 1: e8, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grunig G, Warnock M, Wakil AE, Venkayya R, Brombacher F, Rennick DM, Sheppard D, Mohrs M, Donaldson DD, Locksley RM, Corry DB. Requirement for IL-13 independently of IL-4 in experimental asthma. Science 282: 2261–2263, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guth AM, Janssen WJ, Bosio CM, Crouch EC, Henson PM, Dow SW. Lung environment determines unique phenotype of alveolar macrophages. Am J Physiol Lung Cell Mol Physiol 296: L936–L946, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hackett TL, Holloway R, Holgate ST, Warner JA. Dynamics of pro-inflammatory and anti-inflammatory cytokine release during acute inflammation in chronic obstructive pulmonary disease: an ex vivo study. Respir Res 9: 47, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hasday JD, Bascom R, Costa JJ, Fitzgerald T, Dubin W. Bacterial endotoxin is an active component of cigarette smoke. Chest 115: 829–835, 1999 [DOI] [PubMed] [Google Scholar]
- 20.Houghton AM, Quintero PA, Perkins DL, Kobayashi DK, Kelley DG, Marconcini LA, Mecham RP, Senior RM, Shapiro SD. Elastin fragments drive disease progression in a murine model of emphysema. J Clin Invest 116: 753–759, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Inoue D, Yamaya M, Kubo H, Sasaki T, Hosoda M, Numasaki M, Tomioka Y, Yasuda H, Sekizawa K, Nishimura H, Sasaki H. Mechanisms of mucin production by rhinovirus infection in cultured human airway epithelial cells. Respir Physiol Neurobiol 154: 484–499, 2006 [DOI] [PubMed] [Google Scholar]
- 22.Jagielo PJ, Thorne PS, Watt JL, Frees KL, Quinn TJ, Schwartz DA. Grain dust and endotoxin inhalation challenges produce similar inflammatory responses in normal subjects. Chest 110: 263–270, 1996 [DOI] [PubMed] [Google Scholar]
- 23.Johnston SL, Tyrrell DAJ. Rhinoviruses. In: Diagnostic Procedures for Viral, Rickettsial, and Chlamydial Infections, edited by Lennette EH, Schmidt NJ.Washington, DC: American Public Health Association, 1997, p. 533–563 [Google Scholar]
- 24.Kaneko Y, Takashima K, Suzuki N, Yamana K. Effects of theophylline on chronic inflammatory lung injury induced by LPS exposure in guinea pigs. Allergol Int 56: 445–456, 2007 [DOI] [PubMed] [Google Scholar]
- 25.Kang MJ, Lee CG, Lee JY, Dela Cruz CS, Chen ZJ, Enelow R, Elias JA. Cigarette smoke selectively enhances viral PAMP- and virus-induced pulmonary innate immune and remodeling responses in mice. J Clin Invest 118: 2771–2784, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim EY, Battaile JT, Patel AC, You Y, Agapov E, Grayson MH, Benoit LA, Byers DE, Alevy Y, Tucker J, Swanson S, Tidwell R, Tyner JW, Morton JD, Castro M, Polineni D, Patterson GA, Schwendener RA, Allard JD, Peltz G, Holtzman MJ. Persistent activation of an innate immune response translates respiratory viral infection into chronic lung disease. Nat Med 14: 633–640, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kips JC, Tavernier J, Pauwels RA. Tumor necrosis factor causes bronchial hyperresponsiveness in rats. Am Rev Respir Dis 145: 332–336, 1992 [DOI] [PubMed] [Google Scholar]
- 28.Larsson L, Szponar B, Pehrson C. Tobacco smoking increases dramatically air concentrations of endotoxin. Indoor Air 14: 421–424, 2004 [DOI] [PubMed] [Google Scholar]
- 29.Mahadeva R, Shapiro SD. Chronic obstructive pulmonary disease 3: experimental animal models of pulmonary emphysema. Thorax 57: 908–914, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Majori M, Corradi M, Caminati A, Cacciani G, Bertacco S, Pesci A. Predominant TH1 cytokine pattern in peripheral blood from subjects with chronic obstructive pulmonary disease. J Allergy Clin Immunol 103: 458–462, 1999 [DOI] [PubMed] [Google Scholar]
- 31.Mallia P, Message SD, Kebadze T, Parker HL, Kon OM, Johnston SL. An experimental model of rhinovirus induced chronic obstructive pulmonary disease exacerbations: a pilot study. Respir Res 7: 116, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Message SD, Laza-Stanca V, Mallia P, Parker HL, Zhu J, Kebadze T, Contoli M, Sanderson G, Kon OM, Papi A, Jeffery PK, Stanciu LA, Johnston SL. Rhinovirus-induced lower respiratory illness is increased in asthma and related to virus load and Th1/2 cytokine and IL-10 production. Proc Natl Acad Sci USA 105: 13562–13567, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Michel O, Duchateau J, Plat G, Cantinieaux B, Hotimsky A, Gerain J, Sergysels R. Blood inflammatory response to inhaled endotoxin in normal subjects. Clin Exp Allergy 25: 73–79, 1995 [DOI] [PubMed] [Google Scholar]
- 34.Miotto D, Ruggieri MP, Boschetto P, Cavallesco G, Papi A, Bononi I, Piola C, Murer B, Fabbri LM, Mapp CE. Interleukin-13 and -4 expression in the central airways of smokers with chronic bronchitis. Eur Respir J 22: 602–608, 2003 [DOI] [PubMed] [Google Scholar]
- 35.Mueller R, Chanez P, Campbell AM, Bousquet J, Heusser C, Bullock GR. Different cytokine patterns in bronchial biopsies in asthma and in chronic bronchitis. Respir Med 90: 79–85, 1996 [DOI] [PubMed] [Google Scholar]
- 36.Newcomb DC, Sajjan U, Nanua S, Jia Y, Goldsmith AM, Bentley JK, Hershenson MB. Phosphatidylinositol 3-kinase is required for rhinovirus-induced airway epithelial cell interleukin-8 expression. J Biol Chem 280: 36952–36961, 2005 [DOI] [PubMed] [Google Scholar]
- 37.Newcomb DC, Sajjan US, Nagarkar DR, Wang Q, Nanua S, Zhou Y, McHenry CL, Hennrick KT, Tsai WC, Bentley JK, Lukacs NW, Johnston SL, Hershenson MB. Human rhinovirus 1B exposure induces phosphatidylinositol 3-kinase-dependent airway inflammation in mice. Am J Respir Crit Care Med 177: 1111–1121, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ray P, Tang W, Wang P, Homer R, Kuhn C, 3rd, Flavell RA, Elias JA. Regulated overexpression of interleukin 11 in the lung. Use to dissociate development-dependent and -independent phenotypes. J Clin Invest 100: 2501–2511, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rohde G, Wiethege A, Borg I, Kauth M, Bauer TT, Gillissen A, Bufe A, Schultze-Werninghaus G. Respiratory viruses in exacerbations of chronic obstructive pulmonary disease requiring hospitalisation: a case-control study. Thorax 58: 37–42, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rushton L. Occupational causes of chronic obstructive pulmonary disease. Rev Environ Health 22: 195–212, 2007 [DOI] [PubMed] [Google Scholar]
- 41.Sato M, Hata N, Asagiri M, Nakaya T, Taniguchi T, Tanaka N. Positive feedback regulation of type I IFN genes by the IFN-inducible transcription factor IRF-7. FEBS Lett 441: 106–110, 1998 [DOI] [PubMed] [Google Scholar]
- 42.Sebastian A, Pehrson C, Larsson L. Elevated concentrations of endotoxin in indoor air due to cigarette smoking. J Environ Monit 8: 519–522, 2006 [DOI] [PubMed] [Google Scholar]
- 43.Seemungal T, Harper-Owen R, Bhowmik A, Moric I, Sanderson G, Message S, Maccallum P, Meade TW, Jeffries DJ, Johnston SL, Wedzicha JA. Respiratory viruses, symptoms, and inflammatory markers in acute exacerbations and stable chronic obstructive pulmonary disease. Am J Respir Crit Care Med 164: 1618–1623, 2001 [DOI] [PubMed] [Google Scholar]
- 44.Sethi S, Evans N, Grant BJ, Murphy TF. New strains of bacteria and exacerbations of chronic obstructive pulmonary disease. N Engl J Med 347: 465–471, 2002 [DOI] [PubMed] [Google Scholar]
- 45.Soutiere SE, Mitzner W. Comparison of postnatal lung growth and development between C3H/HeJ and C57BL/6J mice. J Appl Physiol 100: 1577–1583, 2006 [DOI] [PubMed] [Google Scholar]
- 46.Tuthill TJ, Papadopoulos NG, Jourdan P, Challinor LJ, Sharp NA, Plumpton C, Shah K, Barnard S, Dash L, Burnet J, Killington RA, Rowlands DJ, Clarke NJ, Blair ED, Johnston SL. Mouse respiratory epithelial cells support efficient replication of human rhinovirus. J Gen Virol 84: 2829–2836, 2003 [DOI] [PubMed] [Google Scholar]
- 47.Vernooy JH, Dentener MA, van Suylen RJ, Buurman WA, Wouters EF. Long-term intratracheal lipopolysaccharide exposure in mice results in chronic lung inflammation and persistent pathology. Am J Respir Cell Mol Biol 26: 152–159, 2002 [DOI] [PubMed] [Google Scholar]
- 48.Wang Z, Zheng T, Zhu Z, Homer RJ, Riese RJ, Chapman HA, Jr, Shapiro SD, Elias JA. Interferon gamma induction of pulmonary emphysema in the adult murine lung. J Exp Med 192: 1587–1600, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wark PA, Johnston SL, Bucchieri F, Powell R, Puddicombe S, Laza-Stanca V, Holgate ST, Davies DE. Asthmatic bronchial epithelial cells have a deficient innate immune response to infection with rhinovirus. J Exp Med 201: 937–947, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wills-Karp M, Luyimbazi J, Xu X, Schofield B, Neben TY, Karp CL, Donaldson DD. Interleukin-13: central mediator of allergic asthma. Science 282: 2258–2261, 1998 [DOI] [PubMed] [Google Scholar]
- 51.Yang M, Hogan SP, Henry PJ, Matthaei KI, McKenzie AN, Young IG, Rothenberg ME, Foster PS. Interleukin-13 mediates airways hyperreactivity through the IL-4 receptor-alpha chain and STAT-6 independently of IL-5 and eotaxin. Am J Respir Cell Mol Biol 25: 522–530, 2001 [DOI] [PubMed] [Google Scholar]
- 52.Yuta A, Doyle WJ, Gaumond E, Ali M, Tamarkin L, Baraniuk JN, Van Deusen M, Cohen S, Skoner DP. Rhinovirus infection induces mucus hypersecretion. Am J Physiol Lung Cell Mol Physiol 274: L1017–L1023, 1998 [DOI] [PubMed] [Google Scholar]
- 53.Zandvoort A, van der Geld YM, Jonker MR, Noordhoek JA, Vos JT, Wesseling J, Kauffman HF, Timens W, Postma DS. High ICAM-1 gene expression in pulmonary fibroblasts of COPD patients: a reflection of an enhanced immunological function. Eur Respir J 28: 113–122, 2006 [DOI] [PubMed] [Google Scholar]
- 54.Zhu L, Lee PK, Lee WM, Zhao Y, Yu D, Chen Y. Rhinovirus-induced major airway mucin production involves a novel TLR3-EGFR-dependent pathway. Am J Respir Cell Mol Biol 40: 610–619, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.