Abstract
Herpes simplex virus type-1 (HSV-1) is one of many pathogens that use the cell surface glycosaminoglycan heparan sulfate as a receptor. Heparan sulfate is highly expressed on the surface and extracellular matrix of virtually all cell types making it an ideal receptor. Heparan sulfate interacts with HSV-1 envelope glycoproteins gB and gC during the initial attachment step during HSV-1 entry. In addition, a modified form of heparan sulfate, known as 3-O-sulfated heparan sulfate, interacts with HSV-1 gD to induce fusion between the viral envelope and host cell membrane. The 3-O-sulfation of heparan sulfate is a rare modification which occurs during the biosynthesis of heparan sulfate that is carried out by a family of enzymes known as 3-O-sulfotransferases. Due to its involvement in multiple steps of the infection process, heparan sulfate has been a prime target for the development of agents to inhibit HSV entry. Understanding how heparan sulfate functions during HSV-1 infection may not only be critical for inhibiting infection by this virus, but it may also be crucial in the fight against many other pathogens as well.
Keywords: Heparan sulfate (HS), Herpesviruses, Herpes simplex virus type-1 (HSV-1), 3-O-sulfotransferases, Viral entry
HS BIOSYNTHESIS
Heparan sulfate (HS) is a highly sulfated polysaccharide composed of up to 100 repeating uronic acid (D-glucuronic acid [GlcA] or L-iduronic acid [IdoA]) and D-glucosamine (GlcN) disaccharide units. HS is ubiquitously expressed on the cell surface and extracellular matrix of almost all cell types as heparan sulfate proteoglycans (HSPGs) (17, 45, 63). HSPGs are composed of HS polysaccharide side chains covalently linked to a protein core via a tetrasaccharide linker region. HS plays a role in multiple biological processes including blood coagulation, lipid metabolism, regulation of embryonic development, neurogenesis, angiogenesis, axon guidance, cytokine/growth factor interaction, and HS can serve as a receptor for many viruses and bacteria (17, 37, 45, 63, 91). The functional diversity of HS is due to extensive modifications HS undergoes during its biosynthesis.
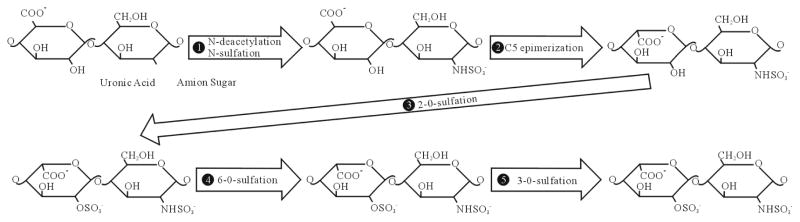
The biosynthesis of HS is a sequential, multi-step process that occurs in the Golgi apparatus. Synthesis of HS begins with the assembly of the tetrasaccharide linker region (GlcA-Gal-Gal-Xyl) on serine residues of the protein core (17, 45, 63). After the initial addition of an N-acetylated glucosamine (GlcNAc) residue to begin the HS chain, polymerization occurs by the addition of alternating GlcA and GlcNAc residues. As polymerization occurs, HS undergoes a series of modifications. The enzymes involved include glycosyltransferases, an epimerase, and sulfotransferases. First, N-deacetylation and N-sulfation of GlcNAc occurs, converting it to N-sulfoglucosamine (GlcNS). Next is the C5 epimerization of GlcA to IdoA. The next modification steps involve O-sulfation by either 2-O-sulfotransferases, 6-O-sulfotransferases, or 3-O-sulfotransferases. First is 2-O-sulfation of IdoA and GlcA, followed by 6-O-sulfation of GlcNAc and GlcNS units, and finally 3-O-sulfation of GlcN residues (17, 45, 63). The arrangement of these modified residues creates distinct binding motifs on the HS chain that are believed to regulate its functional specificity and allow HS to function in distinct biological processes including viral membrane fusion and penetration (66).
HS FUNCTIONS IN HSV-1 INFECTION
The abundant expression of HS on the surface of almost all cell types makes it an ideal receptor for viral infection. In addition, the negative charge of the highly sulfated HS makes it well suited to interact with viral proteins carrying positive charges (81). Evidence also suggests that virus can bind specifically to HS by interacting with specific saccharide sequences (66). This suggests a relationship between HS structure and viral activity. The structural specificity shown by viral infection could be critical for understanding viral activity. HS serves as a receptor for an array of viruses, including human immunodeficiency virus (HIV), hepatitis-C, human papillomavirus, and Dengue virus (5, 10, 29, 83). In addition, virtually all human herpes- viruses, with possible exception of Epstein Barr virus (EBV), use HS as an initial co-receptor for entry (67). Among the herpesviruses, interaction of HS with herpes simplex virus type-1 (HSV-1) has been most studied and therefore, it forms the focus of this review.
HSV-1 belongs to the alphaherpesvirus subfamily of the herpesviruses (67). It is a neurotropic virus that is highly prevalent among humans. HSV-1 can establish latent infection in the peripheral nervous system, allowing the virus to persist in the host causing life-long infection. HSV-1 infection can result in a number of symptoms ranging from the more common mucocutaneous lesions to more severe, life-threatening symptoms, including meningitis and encephalitis (14). Although the primary infection with HSV-1 may remain asymptomatic, it forms the starting point for the life-long recurrent episodes of symptomatic problems associated with the disease. Therefore, HS, as an entry coreceptor, has an important initial role in the pathogenesis of HSV-1.
Like other enveloped viruses, HSV-1 enters cells by inducing fusion between the viral envelope and host cell membrane. HSV-1 can enter host cells by two different pathways. First, HSV-1 can trigger with fusion with the host cell plasma membrane at the cell surface. Second, the virus may enter into the cell through endocytosis using a phagocytosis-like uptake mechanism and trigger fusion with the phagosomal membrane (11, 56). In either case the interaction with HS may be of critical significance. Initially, HS was found to be involved in viral binding during the attachment phase of HSV-1 entry (86). It was previously been shown that soluble heparin, a molecule similar to HS, could bind to HSV-1 virions and inhibit their binding to host cells (54). Enzymatic removal of HS from the cell surface using heparinase led to significantly reduced binding of virions to cells and reduced infection of those cells (86). Cells defective in HS biosynthesis, but not chondroitin sulfate (CS) biosynthesis, are infected at a significantly reduced level (30, 65). Significance of HS in viral binding can also be demonstrated by a low speed centrifugation technique called spinoculation (64). HSV-1 entry into mutant cells defective in HS biosynthesis can be restored to near wild-type levels by spinoculating the virus and the mutant cells together. Spinoculation provides a stronger force to facilitate the adherence of the virus particles on the cell surface. The fact that entry can be restored to near wild-type levels by spinoculation suggests strongly that the initial interactions with HS may not be essential for entry provided an alternate mechanism can bring the virus in extreme close proximity with the plasma membrane (64).
The viral interaction with HS begins with the binding of HSV-1envelope glycoproteins gB and/or gC to HS moieties present on the cells surfaces (72). Next, a third HSV-1 envelope glycoprotein, gD, interacts with one of its receptors to trigger fusion with the host cell; a process that also requires gB, and two additional envelope glycoproteins, gH and gL. Though gC enhances viral binding via its interaction with HS, it is not essential for viral entry (71). The absence of gC results in the reduced HSV-1 binding to the cell. However, virus that does bind can still infect the cell. In the absence of both gB and gC, binding is severely reduced, even compared to when only gC is absent, and the virus is also unable to mediate infection (25, 26). Soluble forms of both gB and gC, as well as, gB and gC extracted from virions, can bind both heparin and HS (26, 74, 81). Soluble gC is able to inhibit HSV-1 binding to cells (26, 73).
Specific amino acid resides from two separate regions of gC were determined to be critical for its interaction with HS (Arg-143, Arg-145, Arg-147, Thr-150 and Gly-247) (79). These arginine residues may interact with 6-O- and 2-O-sulfate groups found on HS and they may define the minimum requirement to bind gC (18). This data correlates with a study that suggests basic and hydrophobic residues localized at the Cys127–Cys144 loop of gC compose a major HS-binding domain (51). A short lysine-rich region of the gB sequence (residues 68–76) has been identified as the HS binding domain of gB and is required for gB-mediated HSV-1 attachment (41). However, this region was not required for gB function during the fusion process of HSV-1 entry.
Attachment is not the only step in which HS is involved. HSV-1 gD can interact with three families of HSV-1 entry receptors to trigger fusion (7). These include: nectin-1 and nectin-2, which are both members of the immunoglobulin superfamily (20), herpesvirus entry mediator (HVEM) from the tumor necrosis factor receptor (TNFR) family (53), and a specially modified form of HS known as 3-O-sulfated heparan sulfate (3-OS HS) (66).
SYNTHESIS OF 3-O-S HS
The final modification step during the biosynthesis of HS (summarized in Fig. 1) is the 3-O-sulfation of HS. Sulfate from PAPS (adenosine 3′-phosphate 5′-phosphosulphate) is transferred to the 3-OH position of GlcN residues to form 3-OS HS (89). 3-O-sulfation is the final, and relatively rare, modification undergone by HS. Several proteins are able to selectively bind to the 3-OS HS motifs, including antithrombin, fibroblast growth factor 7, and, as mentioned earlier, HSV-1 gD (52, 66, 68, 69).
Fig. 1.
Biosynthesis of heparan sulfate. During its biosynthesis, HS has the potential to undergo a series of modifications. Above is a representative of a disaccharide unit consisting of a glucuronic acid (GlcA) and N-acetylated glucosamine (GlcNAc) residue. HS undergoes modifications in the following order: i.) N-deacetylation and N-sulfation of GlcNAc occurs, converting it to N-sulfoglucosamine (GlcNS), ii.) C5 epimerization of GlcA to IdoA, iii.) 2-O-sulfation of IdoA and GlcA, iv.) 6-O-sulfation of GlcNAc and GlcNS units, v.) 3-O-sulfation of GlcN residues.
3-O-sulfation is carried out by a family of enzymes called 3-O-sulfotransferases (3-OSTs). Currently, seven members of the family have been identified: 3-OST-1, -2, -3A, -3B, -4, -5, -6 (58, 76, 87, 89). 3-OST-3A and 3-OST-3B have nearly identical amino acid sequences in the sulfotransferase domain and generate the same 3-O-sulfated disaccharides (47, 68). 3-OSTs consist of a divergent N-terminal domain and a C-terminal sulfotransferase domain that is conserved among all isoforms (68). The sulfotransferase domain determines the sequence specificity of each isoform (68,90). The various isoforms are able to recognize unique saccharide sequences around the modification site (47, 68). This site-specific function of each isoform allows them to generate their own distinct 3-O-sulfated motifs. Thus, each isoform is able to produce a unique 3-OS HS chain with its own distinct function. For example, HS modified by 3-OST-1 contains anti-thrombin binding sites, while, HS modified by 3-OST -2, 3-OST-3, 3-OST-4, and 3-OST-6 interacts with HSV-1 gD and serves as an entry receptor for HSV-1 (58, 66, 76, 89). Interestingly, HS modified by 3-OST -5 has both anticoagulant activity and binds HSV-1 gD (87). The site specific function of these enzymes, along with their distinct expression pattern in cells and tissue, makes them key regulators of HS function (68).
ROLE OF 3-O-S HS IN HSV-1 INFECTION
The first 3-OST enzyme shown to be capable of binding HSV-1 gD and serving as an entry receptor for HSV was 3-OST-3 (66). Since then, all of the other known 3-OST enzymes have been studied for their ability to do the same. All of the enzymes, except 3-OST-1, have been shown to interact with gD and allow HSV-1 entry (58,66,76,87,89). Visual evidence has shown colocalization of 3-OS HS and HSV-1 gD during the fusion process (78). Soluble 3-SO HS was used to show that 3-OS HS was required to trigger the fusion process during HSV-1 infection, and not just required to anchor HSV-1 to specific locations on the cell surface (75–76). A similar study was performed using soluble forms of nectin-1 and nectin-2 to trigger entry into HSV-resistant cells (38). Soluble 3-OS HS, modified by 3-OST-3, functioned in a manner similar to that of the soluble nectins as it was also able to trigger entry in HSV-resistant cells (77). Cells deficient in glycosaminoglycan synthesis became susceptible to HSV-1 entry when spinoculated in the presence of 3-OS HS, further supporting the role of 3-OS HS in HSV-1 mediated fusion rather than cell attachment (77).
Besides entry, soluble 3-OS HS can also trigger cell-cell fusion (78). After entry occurs, the virus is able to spread throughout the host by a process known as cell-cell fusion. During this process, HSV-1 infected cells express the viral envelope glycoproteins required for fusion on their surface, allowing the infected cell to bind and fuse with neighboring uninfected cells. This results in the formation of large multinucleated cells called syncytia. While soluble 3-OS HS generated by 3-OST-3 can trigger cell-cell fusion, 3-OS HS generated by 3-OST-1 cannot trigger entry or cell-cell fusion. HSV-1 is able to produce polykaryocytes during HSV-1 cell-cell fusion in cultured human corneal fibroblasts (CF) using 3-OS HS (78). Polykaryocyte formation depended heavily on the expression of 3-OS HS on the receptor expressing target CF cells, but not on the HSV-1 glycoprotein expressing effector cells. Interestingly, while 3-OS HS was able to trigger cell-cell fusion, previous studies have demonstrated that unmodified HS is not required for cell-cell fusion to occur (59).
Studies have tried to determine the specific saccharide structure in 3-OS HS that allows it to bind HSV-1 gD. A study looking at the crystal structure of the HSV-1 gD-HVEM complex predicted two possible 3-OS HS binding sites on gD (8). One binding site is a deep surface pocket that is positively charged, and the second binding site is a relatively flat surface that contains numerous basic amino acid residues. It was suggested the interaction between the positively charged amino acid residues from gD and the negatively charged sulfate groups from 3-OS HS might provide the electrostatic interactions to create binding sites for 3-OS HS. An octasaccharide developed from HS modified by 3-OST-3 is able to bind gD (46). Amino acid mutations in the N-terminal region of gD that had a negative effect on its ability to interact with 3-OS HS are consistent with the proposed 3-OS HS gD-binding sites (92).
INTERACTION BETWEEN HS AND OTHER HERPESVIRUSES
Besides HSV-1, many, but not all, members of the herpesvirus family interact with HS during infection. These include members of the alphaherpesviruses: HSV-2, varicella zoster virus (VZV), pseudorabies virus (PRV), and bovine herpesvirus 1 (BHV-1). It also includes members of the beta herpesviruses: human cytomegalovirus (HCMV) and human herpesvirus 7 (HHV-7), and members of the gamma herpesviruses: BHV-4 and Kaposi’s sarcoma herpesvirus (KSHV or HHV-8) (1, 12, 31, 44, 55, 67, 70, 80, 84, 86).
Though HSV-1 and HSV-2 infection share several similarities, they do exhibit some key type-specific differences in regards to their interaction with HS. Though both interact with HS, the relative importance of their HS binding glycoproteins differs. While gC plays a key role in attachment during HSV-1 entry, HSV-2 gC is not as important for this process (28,81). HSV-2 gB is believed to play a much more critical role in attachment than HSV-1 gB (28). Difference in gC function is thought to be responsible for several differences in the biological activities of HSV-1 and HSV-2, such as affinity for cell surface HS (81), differential binding to the C3b component of complement (19), and differential sensitivity to polyanionic and polycationic substances (27,39,40). Another key difference between HSV-1 and HSV-2 is their affinity for 3-OS HS. Only HSV-1 gD, and not HSV-2 gD, interacts with 3-OS HS to trigger viral entry (66).
Like HSV-1 and HSV-2, other herpesviruses use specific viral envelope glycoproteins to bind to HS during the entry process. HCMV glycoproteins gM and gB interact with HS to mediate entry into cells by attaching the virion to the cell surface (12,55). Studies using soluble heparin and the enzymatic removal of HS have shown that KSHV also interacts with HS during entry and that interaction is critical for infection (1). Findings have suggested that KSHV gpK8.1A is the glycoprotein that specifically bins to HS to mediate attachment (85). Still, only HSV-1 has been shown to use 3-OS HS as an entry receptor.
USE OF HS AS AN ANTI-HERPETIC AGENT
The most effective and widely used treatment for HSV infection currently is acyclovir (6). However, acyclovir is not always well tolerated and drug-resistant HSV-1 strains are rapidly emerging, especially in patients that are immunocompromised (4, 16). Thus, the need for novel antiherpetic drugs is required. Due to its involvement in both attachment and entry of HSV into host cells, HS has been a prime candidate for the development of therapeutic agents to inhibit HSV infection. These agents might also have the ability to inhibit the infection of other viruses that interact with HS. Multiple approaches involving HS are being developed to inhibit HSV-1 infection using both naturally occurring and synthesized molecules. While some highly cationic molecules are being synthesized to bind HS to inhibit HSV-1 binding and infection (33, 82), othet molecules are being studied that can mimic HS.
One approach has been to identify other sulfated polysaccharides that can be used to inhibit HSV-1 infection. The idea was that these sulfated polysaccharides could mimic HS because of their similarity in structure and compete with it for the virus, to inhibit infection. Numerous sulfated molecules have been explored, most notably, heparin and chemically modified derivatives of heparin (18,23,48). Other sulfated polysaccharides shown to inhibit HSV entry include pentosan polysulfate (24), dextran sulfate (15, 24), sulfated maltoheptaose (24), sulfated fucoidans (42, 60, 61), and spirulan (22), and a low molecular weight molecule PI-88 which can inhibit entry and cell-cell spread (57).
Other studies have instead looked at the ability of sulfated nonpolysaccharide compounds to inhibit HSV infection because they are relatively easy to synthesize. Recently, it was discovered that a sulfated derivative of lignin could inhibit HSV infection (62). Lignin was able to mimic HS to inhibit infection. Inhibition of HSV-1 infection was dependent on the molecular weight of lignin with the heaviest chain being able to inhibit infection the best. Several natural antimicrobial proteins and peptides have been studied for their ability to block viral entry or inhibit later stages of viral growth to inhibit infection (35). Lactoferrin and lactoferricin have been studied extensively for their antiherpetic ability. Lactoferrin (Lf) is a multifunctional iron-binding protein that is a component of the innate immune system and has antimicrobial, antiviral, and anti-inflammatory activities (32, 43). Lf has anti-HSV activity and can inhibit HSV-1 infection (21, 49). Metal complexes of bovine Lf inhibit in vitro replication of both HSV-1 and HSV-2 (50). Recently, it was shown that one of the mechanisms of anti-HSV-1 activity of Lf is its ability to compete with HSV-1 for binding to HS and CS (3, 32). Both bovine and human Lf can also inhibit cell-to-cell spread of HSV-1 and HSV-2 (36).
Lactoferricin (Lfcin) is a peptide generated by pepsin cleavage from the N-terminal part of Lf (21, 49). Both bovine and human Lfcin have been shown to exert antiviral activity against HSV-1 and HSV-2 (2, 3, 34). Like Lf, Lfcin also competes with HSV-1 for HS to inhibit infection (3). Lfcin can exhibit antiviral activity both at the cell surface and at later stages after internalization. Bovine and human Lfcin can inhibit cell-to-cell spread of HSV-1, but not HSV-2 (36).
A relatively new approach had been to use HS biosynthetic enzymes to develop biologically active polysaccharides and oligosaccharides (9, 13, 88). Recently, a 3-O-sulfated octasaccharide was synthesized, which is able to mimic the active domain of 3-OS HS (13). The 3-O-sulfated octasaccharide was synthesized by incubating a heparin octasaccharide (3-OH octasaccharide) with 3-OST-3. The results showed the 3-O-sulfated octasaccharide was able to more efficiently block HSV-1 infection than the heparin octasaccharide, suggesting may be able to inhibit both attachment and fusion. The results suggest it is possible to inhibit HSV-1 entry using specific heparan sulfate based oligosaccharides.
In summary, significant new and old information strongly implicate HS as an important co-receptor in HSV-1 entry into cells in particular and herpesvirus entry in general. Due to complexities involved in understanding HS structure it is difficult to specifically identify structural features of HS needed for viral interactions. However, the discovery of 3-O sulfated HS and its association with viral fusion mechanism has uncovered a strong new possibility that specificity within HS chains may be crucial for its function as a pathogen receptor (66, 78). More structural analysis will be needed to properly understand the true significance of HS in the entry process. Likewise, significant new work will be needed to establish the importance of HS in vivo. At present, virtually no information is available on its significance as a pathogen receptor in vivo.
Acknowledgments
Some of the work described here was supported by a NIH grant (AI 057860 to D.S).
Footnotes
Foundation item: NIH grant (AI 057860 to D.S)
References
- 1.Akula SM, Wang FZ, Vierira J, et al. Human herpesvirus 8 (HHV8/KSHV) infection of target cells involves interaction with heparan sulfate. Virology. 2001;282 (2):245–255. doi: 10.1006/viro.2000.0851. [DOI] [PubMed] [Google Scholar]
- 2.Andersen JH, Jenssen H, Gutteberg TJ. Lactoferrin and lactoferricin inhibit herpes simplex 1 and 2 infection and exhibit synergy when combined with acyclovir. Antiviral Res. 2003;58 (3):209–215. doi: 10.1016/s0166-3542(02)00214-0. [DOI] [PubMed] [Google Scholar]
- 3.Andersen JH, Jenssen H, Sandvik K, et al. Anti-HSV activity of lactoferrin and lactoferricin is dependent on the presence of heparan sulphate at the cell surface. J Med Virol. 2004;74 (2):262–271. doi: 10.1002/jmv.20171. [DOI] [PubMed] [Google Scholar]
- 4.Bacon TH, Levin MJ, Leary JL, et al. Herpes simplex virus resistance to acyclovir and penciclovir after two decades of antiviral therapy. Clin Microbiol Rev. 2003;16 (1):114–128. doi: 10.1128/CMR.16.1.114-128.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barth H, Schafer C, Adah MI, et al. Cellular binding of hepatitis C virus envelope glycoprotein E2 requires cell surface heparan sulfate. J Biol Chem. 2003;278 (42):41003–41012. doi: 10.1074/jbc.M302267200. [DOI] [PubMed] [Google Scholar]
- 6.Brady RC, Bernstein DI. Treatment of herpes simplex virus infections. Antiviral Res. 2004;61(2):73–81. doi: 10.1016/j.antiviral.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 7.Campadelli-Fiume G, Cocchi F, Menotti L, et al. The novel receptors that mediate the entry of herpes simplex viruses and animal alphaherpesviruses into cells. Rev Med Virol. 2000;10 (5):305–319. doi: 10.1002/1099-1654(200009/10)10:5<305::aid-rmv286>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 8.Carfi A, Willis SH, Whitbeck JC, et al. Herpes simplex virus glycoprotein D bound to the human receptor HveA. Mol Cell. 2001;8 (1):169–179. doi: 10.1016/s1097-2765(01)00298-2. [DOI] [PubMed] [Google Scholar]
- 9.Chen J, Avci FY, Munoz EM, et al. Enzymatically redesigning of biologically active heparan sulfate. J Biol Chem. 2005;280 (52):42817–42825. doi: 10.1074/jbc.M504338200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen Y, Maguire T, Hileman RE, et al. Dengue virus infectivity depends on envelope protein binding to target cell heparan sulfate. Nat Med. 1997;3 (8):866–871. doi: 10.1038/nm0897-866. [DOI] [PubMed] [Google Scholar]
- 11.Clement C, Tiwari V, Scanlan PM, et al. A novel role for phagocytosis-like uptake in herpes simplex virus entry. J Cell Biol. 2006;174 (7):1009–1021. doi: 10.1083/jcb.200509155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Compton T, Nowlin DM, Cooper NR. Initiation of human cytomegalovirus infection requires initial interaction with cell surface heparan sulfate. Virology. 1993;193 (2):834–841. doi: 10.1006/viro.1993.1192. [DOI] [PubMed] [Google Scholar]
- 13.Copeland R, Balasubramaniam A, Tiwari V, et al. Using a 3-O-sulfated heparin octasaccharide to inhibit the entry of herpes simplex virus type 1. Biochemistry. 2008;47 (21):5774–5783. doi: 10.1021/bi800205t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Corey L, Spear PG. Infections with herpes simplex viruses. N Engl J Med. 1986;314 (11):686–691. doi: 10.1056/NEJM198603133141105. [DOI] [PubMed] [Google Scholar]
- 15.Dyer AP, Banfield BW, Martindale D, et al. Dextran sulfate can act as an artificial receptor to mediate a typespecific herpes simplex virus infection via glyco-protein B. J Virol. 1997;71(1):191–198. doi: 10.1128/jvi.71.1.191-198.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eizuru Y. Development of new antivirals for herpesviruses. Antivir Chem Chemother. 2003;14 (6):299–308. doi: 10.1177/095632020301400602. [DOI] [PubMed] [Google Scholar]
- 17.Esko JD, Lindahl U. Molecular diversity of heparan sulfate. J Clin Invest. 2001;108 (2):169–173. doi: 10.1172/JCI13530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feyzi E, Trybala E, Bergstrom T, et al. Structural requirement of heparan sulphate for interaction with herpes simplex virus type 1 virions and isolated glycoprotein C. J Biol Chem. 1997;272 (40):24850–24857. doi: 10.1074/jbc.272.40.24850. [DOI] [PubMed] [Google Scholar]
- 19.Friedman HM, Cohen GH, Eisenberg RJ, et al. Glycoprotein C of herpes simplex virus type 1 acts as a receptor for C3b component of complement on infected cells. Nature. 1984;309 (5969):633–635. doi: 10.1038/309633a0. [DOI] [PubMed] [Google Scholar]
- 20.Geraghty RJ, Krummenacher C, Cohen GH, et al. Entry of alphaherpesviruses mediated by poliovirus receptor-related protein 1 and poliovirus receptor. Science. 1998;280 (5369):1618–1620. doi: 10.1126/science.280.5369.1618. [DOI] [PubMed] [Google Scholar]
- 21.Hasegawa K, Motsuchi W, Tanaka S, et al. Inhibition with lactoferrin of in vitro infection with human herpes virus. Jpn J Med Sci Biol. 1994;47 (2):73–85. doi: 10.7883/yoken1952.47.73. [DOI] [PubMed] [Google Scholar]
- 22.Hayashi T, Hayashi K, Maeda M, et al. Calcium spirulan, an inhibitor of enveloped virus replication, from a blue-green alga Spirulina platensis. J Nat Prod. 1996;59 (1):83–87. doi: 10.1021/np960017o. [DOI] [PubMed] [Google Scholar]
- 23.Herold BC, Gerber SI, Polonsky T, et al. Identification of structural features of heparin required for inhibition of herpes simplex virus type 1 binding. Virology. 1995;206 (2):1108–1116. doi: 10.1006/viro.1995.1034. [DOI] [PubMed] [Google Scholar]
- 24.Herold BC, Siston A, Bremer J, et al. Sulfated carbohydrate compounds prevent microbial adherence by sexually transmitted disease pathogens. Antimicrob Agents Chemother. 1997;41 (12):2776–2780. doi: 10.1128/aac.41.12.2776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Herold BC, Visalli RJ, Susmarski N, et al. Glycoprotein C-independent binding of herpes simplex virus to cells requires cell surface heparan sulphate and glycoprotein B. J Gen Virol. 1994;75 (Pt 6):1211–1222. doi: 10.1099/0022-1317-75-6-1211. [DOI] [PubMed] [Google Scholar]
- 26.Herold BC, WuDunn D, Soltys N, et al. Glycoprotein C of herpes simplex virus type 1 plays a principal role in the adsorption of virus to cells and in infectivity. J Virol. 1991;65 (3):1090–1098. doi: 10.1128/jvi.65.3.1090-1098.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hutton RD, Ewert DL, French GR. Differentiation of types 1 and 2 of herpes simplex virus by plaque inhibition with sulfated polyanions. Proc Soc Exp Biol Med. 1973;142 (1):27–29. doi: 10.3181/00379727-142-36950. [DOI] [PubMed] [Google Scholar]
- 28.Gerber SI, Belval BJ, Herold BC. Differences in the role of glycoprotein C of HSV-1 and HSV-2 in viral binding may contribute to serotype differences in cell tropism. Virology. 1995;214 (1):29–39. doi: 10.1006/viro.1995.9957. [DOI] [PubMed] [Google Scholar]
- 29.Giroglou T, Florin L, Schafer F, et al. Human papillomavirus infection requires cell surface heparan sulfate. J Virol. 2001;75 (3):1565–1570. doi: 10.1128/JVI.75.3.1565-1570.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gruenheid S, Gatzke L, Meadows H, et al. Herpes simplex virus infection and propagation in a mouse L cell mutant lacking heparan sulfate proteoglycans. J Virol. 1993;67 (1):93–100. doi: 10.1128/jvi.67.1.93-100.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jacquet A, Haumont M, Chellun D, et al. The varicella zoster virus glycoprotein B (gB) plays a role in virus binding to cell surface heparan sulfate proteoglycans. Virus Res. 1998;53 (2):197–207. doi: 10.1016/s0168-1702(97)00149-4. [DOI] [PubMed] [Google Scholar]
- 32.Jenssen H. Anti herpes simplex virus activity of lactoferrin/lactoferricin-an example of antiviral activity of antimicrobial protein/peptide. Cell Mol Life Sci. 2005;62 (24):3002–3013. doi: 10.1007/s00018-005-5228-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jenssen H, Andersen JH, Mantzilas D, et al. A wide range of medium-sized, highly cationic, alpha-helical peptides show antiviral activity against herpes simplex virus. Antiviral Res. 2004;64 (2):119–26. doi: 10.1016/j.antiviral.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 34.Jenssen H, Andersen JH, Uhlin-Hansen L, et al. Anti-HSV activity of lactoferricin analogues is only partly related to their affinity for heparan sulfate. Antiviral Res. 2004;61(2):101–109. doi: 10.1016/j.antiviral.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 35.Jenssen H, Hamill P, Hancock RE. Peptide antimicrobial agents. Clin Microbiol Rev. 2006;19(3):491–511. doi: 10.1128/CMR.00056-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jenssen H, Sandvik K, Andersen JH, et al. Inhibition of HSV cell-to-cell spread by lactoferrin and lactoferricin. Antiviral Res. 2008;79 (3):192–198. doi: 10.1016/j.antiviral.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 37.Inatani M, Irie F, Plump AS, et al. Mammalian brain morphogenesis and midline axon guidance require heparan sulfate. Science. 2003;302(5647):1044–1046. doi: 10.1126/science.1090497. [DOI] [PubMed] [Google Scholar]
- 38.Kwon H, Bai Q, Baek HJ, et al. Soluble V domain of Nectin-1/HveC enables entry of herpes simplex virus type 1 (HSV-1) into HSV-resistant cells by binding to viral glycoprotein D. J Virol. 2006;80 (1):138–48. doi: 10.1128/JVI.80.1.138-148.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Langeland N, Holmsen H, Lillehaug JR, et al. Evidence that neomycin inhibits binding of herpes simplex virus type 1 to the cellular receptor. J Virol. 1987;61 (11):3388–3393. doi: 10.1128/jvi.61.11.3388-3393.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Langeland N, Moore LJ, Holmsen H, et al. Interaction of polylysine with the cellular receptor for herpes simplex virus type 1. J Gen Virol. 1998;69 (Pt 6):1137–1145. doi: 10.1099/0022-1317-69-6-1137. [DOI] [PubMed] [Google Scholar]
- 41.Laquerre S, Argnani R, Anderson DB, et al. Heparan sulfate proteoglycan binding by herpes simplex virus type 1 glycoproteins B and C, which differ in their contributions to virus attachment, penetration, and cell-to-cell spread. J Virol. 1998;72 (7):6119–6130. doi: 10.1128/jvi.72.7.6119-6130.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee JB, Hayashi K, Hashimoto M, et al. Novel antiviral fucoidan from sporophyll of Undaria pinnatifida (Mekabu) Chem Pharm Bull (Tokyo) 2004;52 (9):1091–1094. doi: 10.1248/cpb.52.1091. [DOI] [PubMed] [Google Scholar]
- 43.Legrand D, Pierce A, Elass E, et al. Lactoferrin structure and functions. Adv Exp Med Biol. 2008;606:163–194. doi: 10.1007/978-0-387-74087-4_6. [DOI] [PubMed] [Google Scholar]
- 44.Liang X, Babiuk LA, Zamb TJ. Mapping of heparin-binding structures on bovine herpesvirus 1 and pseudorabies virus gIII glycoproteins. Virology. 1993;194 (1):233–243. doi: 10.1006/viro.1993.1254. [DOI] [PubMed] [Google Scholar]
- 45.Lindahl U, Kusche-Gullberg M, Kjellén L. Regulated diversity of heparan sulfate. J Biol Chem. 1998;273 (39):24979–24982. doi: 10.1074/jbc.273.39.24979. [DOI] [PubMed] [Google Scholar]
- 46.Liu J, Shriver Z, Pope RM, et al. Characterization of a heparan sulphate octasaccharide that binds to herpes simplex viral type 1 glycoprotein D. J Biol Chem. 2002;277 (36):33456–33467. doi: 10.1074/jbc.M202034200. [DOI] [PubMed] [Google Scholar]
- 47.Liu J, Shworak NW, Sinay P, et al. Expression of heparan sulphate D glucosaminyl 3-O sulphotransferase isoforms reveals novel substrate specificities. J Biol Chem. 1999;274 (8):5185–5192. doi: 10.1074/jbc.274.8.5185. [DOI] [PubMed] [Google Scholar]
- 48.Lycke E, Johansson M, Svennerholm B, et al. Binding of herpes simplex virus to cellular heparan sulphate, an initial step in the adsorption process. J Gen Virol. 1991;72 (Pt 5):1131–1137. doi: 10.1099/0022-1317-72-5-1131. [DOI] [PubMed] [Google Scholar]
- 49.Marchetti M, Longhi C, Conte MP, et al. Lactoferrin inhibits herpes simplex virus type1 adsorption to Vero cells. Antiviral Res. 1996;29(2–3):221–231. 89–94. doi: 10.1016/0166-3542(95)00840-3. [DOI] [PubMed] [Google Scholar]
- 50.Marchetti M, Pisani S, Antonini G, et al. Metal complexes of bovine lactoferrin inhibit in vitro replication of herpes simplex virus type 1 and 2. Biometals. 1998;11(2) doi: 10.1023/a:1009217709851. [DOI] [PubMed] [Google Scholar]
- 51.Mardberg K, Trybala E, Glorioso JC, et al. Mutational analysis of the major heparan sulfate-binding domain of herpes simplex virus type 1 glycoprotein C. J Gen Virol. 2001;82 (Pt 8):1941–1950. doi: 10.1099/0022-1317-82-8-1941. [DOI] [PubMed] [Google Scholar]
- 52.McKeehan WL, Wu X, Kan M. Requirement for anticoagulant heparan sulfate in the fibroblast growth factor receptor complex. J Biol Chem. 1999;274 (31):21511–21514. doi: 10.1074/jbc.274.31.21511. [DOI] [PubMed] [Google Scholar]
- 53.Montgomery RI, Warner MS, Lum BJ, et al. Herpes simplex virus-1 entry into cells mediated by a novel member of the TNF/NGF receptor family. Cell. 1996;87 (3):427–436. doi: 10.1016/s0092-8674(00)81363-x. [DOI] [PubMed] [Google Scholar]
- 54.Nahmias AJ, Kibrick S. Inhibitory effect of heparin on herpes simplex virus. J Bacteriol. 1964;87 (5):1060–1066. doi: 10.1128/jb.87.5.1060-1066.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Neyts J, Snoeck R, Schols D, et al. Sulfated polymers inhibit the interaction of human cytomegalovirus with cell surface heparan sulfate. Virology. 1992;189 (1):48–58. doi: 10.1016/0042-6822(92)90680-n. [DOI] [PubMed] [Google Scholar]
- 56.Nicola AV, McEvoy AM, Straus SE. Roles for endocytosis and low pH in herpes simplex virus entry into HeLa and Chinese hamster ovary cells. J Virol. 2003;77 (9):5324–5332. doi: 10.1128/JVI.77.9.5324-5332.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nyberg K, Ekblad M, Bergstrom T, et al. The low molecular weight heparan sulfate-mimetic, PI-88, inhibits cell-to-cell spread of herpes simplex virus. Antiviral Res. 2004;63(1):15–24. doi: 10.1016/j.antiviral.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 58.O’Donnell CD, Tiwari V, Oh MJ, et al. A role for heparan sulfate 3-O sulfotransferase isoform 2 in herpes simplex virus type 1 entry and spread. Virology. 2006;346 (2):452–459. doi: 10.1016/j.virol.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 59.Pertel PE, Fridberg A, Parish ML, et al. Cell fusion induced by herpes simplex virus glycoproteins gB, gD, and gH-gL requires a gD receptor but not necessarily heparan sulfate. Virology. 2001;279 (1):313–324. doi: 10.1006/viro.2000.0713. [DOI] [PubMed] [Google Scholar]
- 60.Ponce NM, Pujol CA, Damonte EB, et al. Fucoidans from the brown seaweed Adenocystis utricularis: extraction methods, antiviral activity and structural studies. Carbohydr Res. 2003;338 (2):153–165. doi: 10.1016/s0008-6215(02)00403-2. [DOI] [PubMed] [Google Scholar]
- 61.Preeprame S, Hayashi K, Lee J, et al. A novel antivirally active fucan sulfate derived from an edible brown alga, Sargassum horneri. Chem Pharm Bull (Tokyo) 2001;49 (4):484–485. doi: 10.1248/cpb.49.484. [DOI] [PubMed] [Google Scholar]
- 62.Raghuraman A, Tiwari V, Zhao Q, et al. Viral inhibition studies on sulfated lignin, a chemically modified biopolymer and a potential mimic of heparan sulfate. Biomacromolecules. 2007;8 (5):1759–1763. doi: 10.1021/bm0701651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rosenberg RD, Shworak NW, Liu J, et al. Heparan sulfate proteoglycans of the cardiovascular system. Specific structures emerge but how is synthesis regulated? J Clin Invest. 1997;99 (9):2062–2070. doi: 10.1172/JCI119377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Scanlan PM, Tiwari V, Bommireddy S, et al. Spinoculation of heparan sulfate deficient cells enhances HSV-1 entry, but does not abolish the need for essential glycoproteins in viral fusion. J Virol Methods. 2005;128 (1–2):104–112. doi: 10.1016/j.jviromet.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 65.Shieh MT, WuDunn D, Montgomery RI, et al. Cell surface receptors for herpes simplex virus are heparan sulphate proteoglycans. J Cell Biol. 1992;116 (5):1273–1281. doi: 10.1083/jcb.116.5.1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Shukla D, Liu J, Blaiklock P, et al. A novel role for 3-O-sulfated heparan sulfate in herpes simplex virus 1 entry. Cell. 1999;99 (1):13–22. doi: 10.1016/s0092-8674(00)80058-6. [DOI] [PubMed] [Google Scholar]
- 67.Shukla D, Spear PG. Herpesviruses and heparan sulfate: an intimate relationship in aid of viral entry. J Clin Invest. 2001;108 (4):503–10. doi: 10.1172/JCI13799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shworak NW, Liu J, Petros LM, et al. Multiple isoforms of heparan sulfate D glucosaminyl 3-O-sulfotransferase. Isolation, characterization, and expression of human cDNAs and identification of distinct genomic loci. J Biol Chem. 1999;274 (8):5170–5184. doi: 10.1074/jbc.274.8.5170. [DOI] [PubMed] [Google Scholar]
- 69.Shworak NW, HajMohammadi S, de Agostini AI, et al. Mice deficient in heparan sulfate 3-O-sulfotransferase-1: normal hemostasis with unexpected perinatal phenotypes. Glycoconj J. 2002;19(4–5):355–361. doi: 10.1023/A:1025377206600. [DOI] [PubMed] [Google Scholar]
- 70.Skrincosky D, Hocknell P, Whetter L, et al. Identification and analysis of a novel heparin-binding glycoprotein encoded by human herpesvirus 7. J Virol. 2000;74 (10):4530–4540. doi: 10.1128/jvi.74.10.4530-4540.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Spear PG, Longnecker R. Herpesvirus entry: an update. J Virol. 2003;77 (19):10179–10185. doi: 10.1128/JVI.77.19.10179-10185.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Spear PG, Shieh MT, Herold BC, et al. Heparan sulfate glycosaminoglycans as primary cell surface receptors for herpes simplex virus. Adv Exp Med Biol. 1992;313:341–353. doi: 10.1007/978-1-4899-2444-5_33. [DOI] [PubMed] [Google Scholar]
- 73.Svennerholm B, Jeansson S, Vahlne A, et al. Involvement of glycoprotein C (gC) in adsorption of herpes simplex virus type 1 (HSV-1) to the cell. Arch Virol. 1991;120 (3–4):273–279. doi: 10.1007/BF01310482. [DOI] [PubMed] [Google Scholar]
- 74.Tal-Singer R, Peng C, Ponce De Leon M, et al. Interaction of herpes simplex virus glycoprotein gC with mammalian cell surface molecules. J Virol. 1995;69 (7):4471–4483. doi: 10.1128/jvi.69.7.4471-4483.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tiwari V, Clement C, Duncan MB, et al. A role for 3-O-sulphated heparan sulphate in cell fusion induced by herpes simplex virus type 1. J Gen Virol. 2004;85 (Pt 4):805–809. doi: 10.1099/vir.0.19641-0. [DOI] [PubMed] [Google Scholar]
- 76.Tiwari V, O’Donnell CD, Oh MJ, et al. A role for 3-O-sulfotransferase isoform-4 in assisting HSV-1 entry and spread. Biochem Biophys Res Commun. 2005;338 (2):930–937. doi: 10.1016/j.bbrc.2005.10.056. [DOI] [PubMed] [Google Scholar]
- 77.Tiwari V, O’Donnell C, Copeland RJ, et al. Soluble 3-O-sulfated heparan sulfate can trigger herpes simplex virus type 1 entry into resistant Chinese hamster ovary (CHO-K1) cells. J Gen Virol. 2007;88:1075–1079. doi: 10.1099/vir.0.82476-0. [DOI] [PubMed] [Google Scholar]
- 78.Tiwari V, ten Dam GB, Yue BY, et al. Role of 3-O-sulfated heparan sulfate in virus-induced polykaryocyte formation. FEBS Lett. 2007;581 (2–3):4468–4472. doi: 10.1016/j.febslet.2007.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Trybala E, Bergstrom T, Svennerholm B, et al. Localization of a functional site on herpes simplex virus type 1 glycoprotein C involved in binding to cell surface heparan sulphate. J Gen Virol. 1994;75 (Pt 4):743–752. doi: 10.1099/0022-1317-75-4-743. [DOI] [PubMed] [Google Scholar]
- 80.Trybala E, Bergstrom T, Spillmann D, et al. Interaction between pseudorabies virus and heparin/heparan sulfate. Pseudorabies virus mutants differ in their interaction with heparin/heparan sulfate when altered for specific glycoprotein C heparin-binding domain. J Biol Chem. 1998;273 (9):5047–5052. doi: 10.1074/jbc.273.9.5047. [DOI] [PubMed] [Google Scholar]
- 81.Trybala E, Liljeqvist JA, Svennerholm B, et al. Herpes simplex virus types 1 and 2 differ in their interaction with heparan sulfate. J Virol. 2000;74 (19):9106–9114. doi: 10.1128/jvi.74.19.9106-9114.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Trybala E, Olofsson S, Mardberg K, et al. Structural and functional features of the polycationic peptide required for inhibition of herpes simplex virus invasion of cells. Antiviral Res. 2004;62 (3):125–134. doi: 10.1016/j.antiviral.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 83.Tyagi M, Rusnati M, Presta M, et al. Internalization of HIV-1 Tat requires cell surface heparan sulfate proteoglycans. J Biol Chem. 2001;276 (5):3254–3261. doi: 10.1074/jbc.M006701200. [DOI] [PubMed] [Google Scholar]
- 84.Vanderplasschen A, Bublot M, Dubuisson J, et al. Attachment of the gammaherpesvirus bovine herpesvirus 4 is mediated by the interaction of gp8 glycoprotein with heparinlike moieties on the cell surface. Virology. 1993;196 (1):232–240. doi: 10.1006/viro.1993.1471. [DOI] [PubMed] [Google Scholar]
- 85.Wang FZ, Akula SM, Pramod NP, et al. Human herpesvirus 8 envelope glycoprotein K8. 1A interaction with the target cells involves heparan sulfate. J Virol. 2001;75 (16):7517–7527. doi: 10.1128/JVI.75.16.7517-7527.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.WuDunn D, Spear PG. Initial interaction of herpes simplex virus with cells is binding to heparan sulphate. J Virol. 1989;63 (1):52–58. doi: 10.1128/jvi.63.1.52-58.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Xia G, Chen J, Tiwari V, et al. Heparan sulfate 3-O-sulfotransferase isoform 5 generates both an anti-thrombin-binding site and an entry receptor for herpes simplex virus, type 1. J Biol Chem. 2002;277 (40):37912–37919. doi: 10.1074/jbc.M204209200. [DOI] [PubMed] [Google Scholar]
- 88.Xu D, Moon A, Song D, et al. Engineering sulfotransferases to modify heparan sulfate. Nat Chem Biol. 2008;4 (3):200–202. doi: 10.1038/nchembio.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Xu D, Tiwari V, Xia G, et al. Characterization of heparan sulphate 3-O sulphotransferase isoform 6 and its role in assisting the entry of herpes simplex virus type 1. Biochem J. 2005;385 (Pt 2):451–459. doi: 10.1042/BJ20040908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yabe T, Shukla D, Spear PG, et al. Portable sulphotransferase domain determines sequence specificity of heparan sulphate 3-O-sulphotransferases. Biochem J. 2001;359 (Pt 1):235–241. doi: 10.1042/0264-6021:3590235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Yamaguchi Y. Heparan sulfate proteoglycans in the nervous system: their diverse roles in neurogenesis, axon guidance, and synaptogenesis. Semin Cell Dev Biol. 2001;12:99–106. doi: 10.1006/scdb.2000.0238. [DOI] [PubMed] [Google Scholar]
- 92.Yoon M, Zago A, Shukla D, et al. Mutations in the N-termini of herpes simplex virus type 1 and 2 gDs alter functional interactions with the entry/fusion receptors HVEM, Nectin-2, and 3-O-sulphated heparan sulphate but not with Nectin-1. J Virol. 2003;77 (17):9221–9231. doi: 10.1128/JVI.77.17.9221-9231.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]